Introduction
Although maternal mortality due to obstetric causes
has declined, there has been a relative increase in non-obstetric
causes of maternal mortality and morbidity (1). Central nervous system diseases,
including intracranial tumors, particularly malignant brain tumors
[odds ratio (OR), 143] (2) and
trauma, remain a leading cause of indirect maternal mortality.
Primary central nervous system tumors occur in ∼6 in 100,000
females (3), but are rare during
pregnancy. A study reported the incidence of maternal malignant
brain tumors at 3.6 per 1 million live births (4). The management of women with malignant
brain tumors during pregnancy has not been well evaluated.
The present study reports two cases of pregnant
women in the third trimester with gliomas. The patients underwent
caesarean section (CS) followed by craniotomy for brain tumor
resection under the same general anesthesia at 34 weeks’ gestation
and were managed successfully. At present, the management of
gliomas has been widely established in the literature, but those
occurring in pregnancy have been poorly discussed. The present
study discusses the management of the two cases with a review of
the literature.
Case report
Case 1
A 25-year-old primipara patient was admitted to
hospital at 32 weeks of pregnancy due to a headache for 1 month and
blurred vision for 20 days. The patient was in the third trimester
of pregnancy. Ultrasonography (USG) showed a single intrauterine
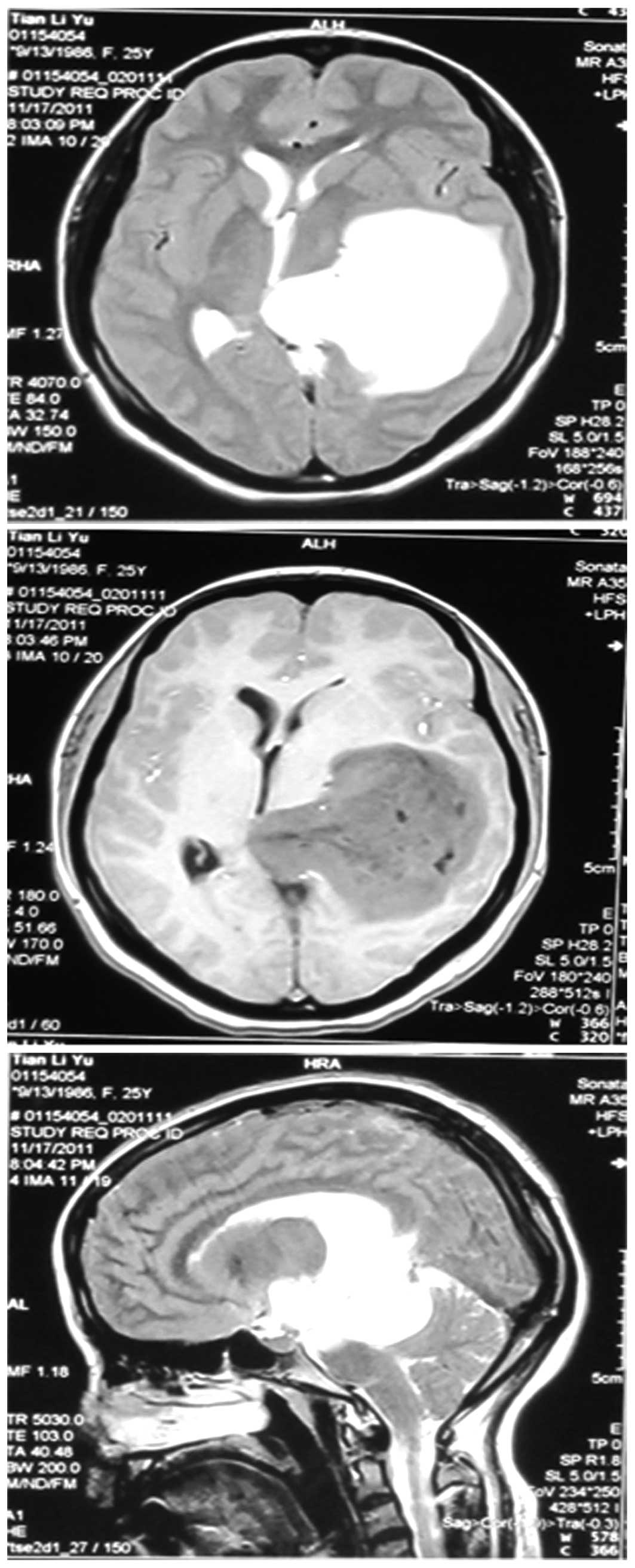
live pregnancy with occiput presentation. A magnetic resonance
imaging (MRI) scan showed a left frontoparietal mass (size: 6x5x5
cm) with peripheral enhancement (Fig.
1), with a shift of the median line.
After multidisciplinary consultation with the
neurosurgery, obstetrics and anesthesiology departments, the
initial decision was to delay the neurosurgery until after
delivery. The patient and her family agreed with this strategy. The
decision was made to treat the patient with dexamethasone to
control the cerebral edema and accelerate fetal lung maturity.
However, the patient’s visual acuity rapidly worsened. Therefore,
the patient was scheduled for a CS and neurosurgical resection of
the tumor under general anesthesia at 34 weeks’ gestation.
A live 1,900-g female was delivered 6 min after the
skin incision. The neonate’s Apgar score at 1 min was 8 and after 2
min, the Apgar score sharply decreased to 3. The neonate was
resuscitated immediately with intermittent positive pressure
breathing and 0.04 mg naloxone was administered intramuscularly 5
min later. The Apgar score returned 8. The neonate was then
admitted to the neonatal intensive care unit.
Oxytocin (10 units) was administered i.v. to improve
the uterine contraction. Following delivery, the neurosurgical
resection of the tumor was performed uneventfully. The patient
recovered quickly from anesthesia without any neurological deficit
and was extubated in the operating room.
The pathology laboratory revealed an astrocytoma,
which was WHO grade III. The positive expression of glial
fibrillary acidic protein (GFAP), CD34, p53, Olig-2, vimentin and
isocitrate dehydrogenase-1 (IDH-1) were observed by
immunohistochemical staining techniques. The patient was discharged
7 days after surgery. Adjuvant therapy was initiated 2 weeks after
surgery. The patient completed radiotherapy and chemotherapy by
taking temozolomide for 6 months post-craniectomy. The mother
remained in a good condition and the baby was observed to develop
normally throughout the 12-month follow-up period.
Case 2
A 42-year-old, gravida 4, para 3, patient was
hospitalized at 34 weeks’ gestation due to a severe headache and
vomiting for 15 days. The patient was admitted to the Xuanwu
Hospital and was hemodynamically stable, with bilaterally reactive
pupils. The patient’s previous obstetric history included three
full-term pregnancies with two vaginal births and one CS. A
physical examination confirmed weakness in the faculty of memory,
indifference of facial expression and a Glasgow Coma Scale score of
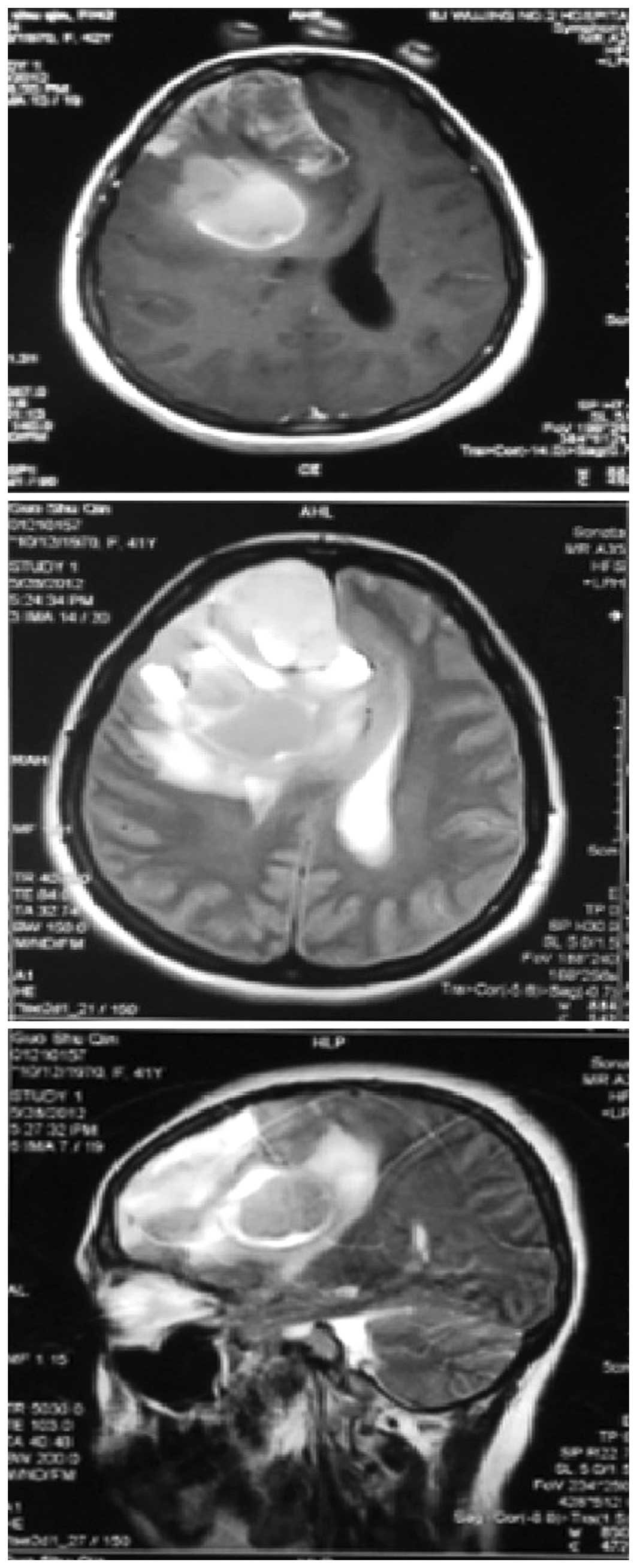
13/15. An MRI scan showed a right frontal lobe tumor with an
intratumoral hemorrhage (Fig. 2),
causing a significant midline and brain shift toward the left side.
Obstetric USG showed a single intrauterine live pregnancy with
breech presentation which was concordant with its gestational age.
The patient was otherwise healthy and denied any previous history
of disease. The laboratory results were within the normal ranges.
Due to the presence of an intratumoral hemorrhage, termination of
the pregnancy was recommended. Following mannitol and steroid
infusion, the patient was taken to the operation room for CS
followed by neurosurgical resection of the tumor.
CS and craniotomy in the supine position were
performed under general anesthesia. A healthy 2,450-g female was
delivered by CS 5 min after the skin incision. The female neonate
had an Apgar score of 9 at 1 min and 10 at 5 min after delivery and
was taken to the neonatal intensive care unit for observation.
Ten units of oxytocin were administered
intravenously to improve the uterine contraction after clipping the
umbilical cord. The obstetrician massaged the uterus regularly to
improve uterine tone during the neurosurgical procedure, which was
performed uneventfully. At the completion of craniotomy for
resection of the brain tumor, the patient was extubated while fully
awake in the operating room and then transported to the intensive
care unit.
The pathology laboratory reported an anaplastic
oligodendroglioma, WHO grade III. Immunohistochemistry of the tumor
cells revealed positive p53, IDH-1 and Ki-67 (40%) expression and
partially positive GFAP, CD34 and EMA expression. The patient was
discharged 8 days after surgery. The patient received radiotherapy
25 times and treatment with chemotherapy using temozolomide was
administered in another hospital.
At follow-up 6 months after discharge, the mother
was observed to have an adequate condition and the newborn was
observed to be in a good neurological and behavioral state of
development.
Discussion
Intracranial tumors are extremely rare in pregnancy
and the prevalence in pregnancy is unknown. Several types of brain
tumors are associated with pregnancy, including meningiomas,
gliomas, pituitary adenomas and acoustic neurinomas. Although a few
studies have reported cases of women with gliomas during pregnancy,
this situation remains exceptional. A French study on gliomas
reported eight cases between 1992 and 2007; five patients had
gliomas prior to pregnancy and three developed gliomas during
pregnancy and diffuse gliomas were diagnosed (5). Ducray et al(6) reported four cases of gliomas, Lynch
et al(7) five cases and
Cutura and Soldo (8) one case. The
present study reports two cases of glioma in the third
trimester.
Intracranial hypertension usually occurs secondary
to malignant brain tumors. The most common clinical manifestations
of intracranial hypertension are headaches and vomiting, which were
observed in the present patients. Intracranial hypertension may be
misdiagnosed due to confusion with pregnancy. Headaches also occur
in pregnancy, but a persistent headache is particularly associated
with hyperemesis or neurological deficits in patients with brain
tumors. In the two present cases, the patients complained of
headaches, which occurred several weeks prior to hospital
admission. A detailed history and MRI are likely to aid
diagnosis.
Management of these cases presents a medical
dilemma. A multidisciplinary group, including a neurosurgeon,
obstetrician, anesthesiologist and neonatologist should evaluate
whether the mother’s and the fetus’s lives are threatened. A
multidisciplinary team recommends the optimal timing for the
termination of pregnancy, as determined by the fetus maturity and
mother’s neurological condition. The various treatment modalities
in pregnant women with glioma are associated with histology and
gestational age (6). The two
present cases exhibited neurological deterioration or signs of
severe intracranial hypertension. If the condition had progressed
it may have threatened the mothers’ lives. Therefore, timely
interventions were important for the two patients.
Neurosurgical procedures remain the major therapy
for gliomas. Most craniotomy procedures are performed during
pregnancy and after delivery in stable patients (5,9,10).
Since the maternal intravascular volume increases with advancing
gestational age, tumor resection is at risk of causing significant
hemorrhaging. If the lesion is not large and the mother does not
have intracranial hypertension, the tumor may be removed postpartum
or its removal may be deferred until the fetus comes to term.
However, if the prognosis of maternal survival is poor, craniotomy
may be immediately performed (11,12).
In the present cases exhibiting neurological deterioration, we
considered that postoperative premature labor and fetus distress,
which may lead to fetal deaths (13), were likely. In view of the condition
of the two pregnant patients at 34 weeks’ gestation, with the aim
of reducing morbidity and mortality (11), the decision was made to perform CS
and craniotomy under the same anesthesia following the evaluation
of fetal viability by an obstetrician. Since synthetic oxytocin has
been used in patients with intracranial tumors without any adverse
effects (3), oxytocin and regular
uterine massage, which enhance uterine contraction, were
administered to the patients to reduce postpartum hemorrhaging
during the subsequent neurosurgery.
Adjuvant therapies, including radiotherapy and
chemotherapy, appear to be effective for patients with gliomas.
Early radiotherapy and chemotherapy significantly improves the
quality of life of the patients. However, radiotherapy during
pregnancy may cause harm to the developing fetus. Although the
threshold dose of 0.1–0.2 Gy is low and is not sufficient for
curative radiotherapy during pregnancy, radiation effects may
appear (14). All chemotherapy
drugs are capable of crossing the placenta and may induce fetal
toxicity, particularly in the first trimester. In general, pregnant
women with gliomas are advised to delay radiotherapy and
chemotherapy until after delivery. If the CS is performed earlier,
this allows more time to undergo further adjuvant treatment. In the
present patients, CS followed by craniotomy was performed at 34
weeks’ gestation. The patients started early radiotherapy and
chemotherapy with temozolomide, according to the regimen that is
currently considered to be the standard care for glioblastomas
(15).
Delivery by CS followed by neurosurgery is almost
always performed under general anesthesia. Studies have shown that
general anesthesia is safe and well tolerated for neuro-anesthesia
during pregnancy (16). Airway
management must address the avoidance of increases in intracranial
pressure, the presence of a potentially full stomach,
pregnancy-induced changes to the airway and enlarged breasts, which
increase the incidence of a difficult intubation (12). It is important to preserve cerebral
and uteroplacental perfusion by maintaining hemodynamic stability.
Extubation should be delayed until the patient is sufficiently
awake for the patient’s airway to be protected from regurgitation
and pulmonary aspiration. The postoperative management of pregnant
patients following neurosurgical intervention is similar to that of
non-pregnant patients.
Malignant brain tumors are associated with adverse
outcomes in pregnancy (2). Tewari
et al(17) reviewed a case
series of pregnancy-associated malignant brain tumors for two
decades between 1978 and 1998 at five hospitals. This review
reported that six out of eight patients delivered under emergency
conditions. Of these six mothers, four died and two had significant
neurological deficits. However, the outcomes for the women and
their neonates reported in the present study were generally
good.
Gliomas in patients during pregnancy are rare. The
aim of treatment is to minimize maternal and fetal mortality and
morbidity. A multidisciplinary approach, including obstetricians,
anesthesiologists, neurosurgeons and neonatologists, is essential
to achieve the optimal timing of neurosurgery and delivery. The
findings from the present cases suggest that CS and craniotomy may
be performed under the same general anesthesia at 34 weeks’
gestation. Further adjuvant treatment started soon after surgery
may facilitate improved outcomes for the mother and newborn.
Acknowledgements
The authors would like to thank Geng
Xu, Jiankun Xu and Xiaotong Fan at the Department of Neurosurgical
Oncology, Xuanwu Hospital, Capital Medical University for providing
assistance.
References
|
1
|
Cantwell R, Clutton-Brock T, Cooper G, et
al: Saving Mothers’ Lives: Reviewing maternal deaths to make
motherhood safer: 2006–2008. The Eighth Report of Confidential
Enquiries into Maternal Deaths in the United Kingdom. BJOG.
118(Suppl 1): 1–203. 2011.
|
|
2
|
Terry AR, Barker FG 2nd, Leffert L,
Bateman BT, Souter I and Plotkin SR: Outcomes of hospitalization in
pregnant women with CNS neoplasms: a population-based study. Neuro
Oncol. 14:768–776. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chang L, Looi-Lyons L, Bartosik L and
Tindal S: Anesthesia for cesarean section in two patients with
brain tumours. Can J Anaesth. 46:61–65. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Haas JF, Jänisch W and Staneczek W: Newly
diagnosed primary intracranial neoplasms in pregnant women: a
population-based assessment. J Neurol Neurosurg Psychiatry.
49:874–880. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pallud J, Duffau H, Razak RA, et al:
Influence of pregnancy in the behavior of diffuse gliomas: clinical
cases of a French glioma study group. J Neurol. 256:2014–2020.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ducray F, Colin P, Cartalat-Carel S, et
al: Management of malignant gliomas diagnosed during pregnancy. Rev
Neurol (Paris). 162:322–329. 2006.(In French).
|
|
7
|
Lynch JC, Gouvêa F, Emmerich JC,
Kokinovrachos G, Pereira C, Welling L and Kislanov S: Management
strategy for brain tumour diagnosed during pregnancy. Br J
Neurosurg. 25:225–230. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cutura N and Soldo V: Preterm delivery in
a patient with frontal lobe brain tumor. Vojnosanit Pregl.
66:830–832. 2009.(In Serbian).
|
|
9
|
Chaudhuri P and Wallenburg HC: Brain
tumors and pregnancy. Presentation of a case and a review of the
literature. Eur J Obstet Gynecol Reprod Biol. 11:109–114. 1980.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nossek E, Ekstein M, Rimon E, Kupferminc
MJ and Ram Z: Neurosurgery and pregnancy. Acta Neurochir (Wien).
153:1727–1735. 2011. View Article : Google Scholar
|
|
11
|
Ng J and Kitchen N: Neurosurgery and
pregnancy. J Neurol Neurosurg Psychiatry. 79:745–752. 2008.
View Article : Google Scholar
|
|
12
|
Goldschlager T, Steyn M, Loh V,
Selvanathan S, Vonau M and Campbell S: Simultaneous craniotomy and
caesarean section for trauma. J Trauma. 66:E50–E51. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Morris JA Jr, Rosenbower TJ, Jurkovich GJ,
et al: Infant survival after cesarean section for trauma. Ann Surg.
223:481–491. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kal HB and Struikmans H: Radiotherapy
during pregnancy: fact and fiction. Lancet Oncol. 6:328–333. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang LP and Paech MJ: Neuroanesthesia for
the pregnant woman. Anesth Analg. 107:193–200. 2008. View Article : Google Scholar
|
|
16
|
Stupp R, Mason WP, van den Bent MJ, et al:
Radiotherapy plus concomitant and adjuvant temozolomide for
glioblastoma. N Engl J Med. 352:987–996. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tewari KS, Cappuccini F, Asrat T, Flamm
BL, Carpenter SE, Disaia PJ and Quilligan EJ: Obstetric emergencies
precipitated by malignant brain tumors. Am J Obstet Gynecol.
182:1215–1221. 2000. View Article : Google Scholar : PubMed/NCBI
|