Introduction
Primary vascular tumors of the lymph nodes other
than Kaposi’s sarcoma are rare (1).
Nodal tumors presenting features of tumors of lymphatic endothelial
lineage are even more uncommon (2).
They occur more commonly in soft tissue and bones, rather than in
lymph nodes. Papillary intralymphatic angioendothelioma affect
individuals of all ages; however, they are rare in older patients.
The present study reports a case of vascular neoplasia with
papillation supervening within a cervical lymph node. The tumoral
elements exhibited an immunophenotype with characteristics of
lymphatic endothelial cells. Other immunohistochemical and clinical
findings indicated a new hypothesis for the pathogenesis of this
type of rare lesion. Written informed consent was obtained from the
patient.
Case report
A 59-year-old male presented with a painless, slowly
growing swelling on the right side of the neck. The clinical
examination revealed a 2.0×3.0-cm soft and movable mass, with
intact overlying skin of normal color on the upper part of the
anterior edge of the sternocleidomastoid muscle.
The patient had a medical history of a
moderately-differentiated adenocarcinoma of the sigmoid colon
infiltrating the mesorectum in September 2007. The patient received
an anterior resection of the rectum and chemotherapy following the
folinic acid (200 mg/m2), fluorouracil (400
mg/m2) and oxaliplatin (85 mg/m2) regimen for
12 cycles.
In 2011, the patient presented with lung metastasis,
which was treated by left inferior atypical lobectomy and
chemotherapy following the folinic acid (200 mg/m2),
fluorouracil (400 mg/m2) and irinotecan (180
mg/m2) regimen for 12 cycles.
In January 2012, during chemotherapeutic treatment,
a cervical swelling appeared on a whole-body computed tomography
(CT) scan, appearing as a nodular mass of ~3.5×2 cm in the right
cervical space between the sternocleidomastoid and scalene muscles
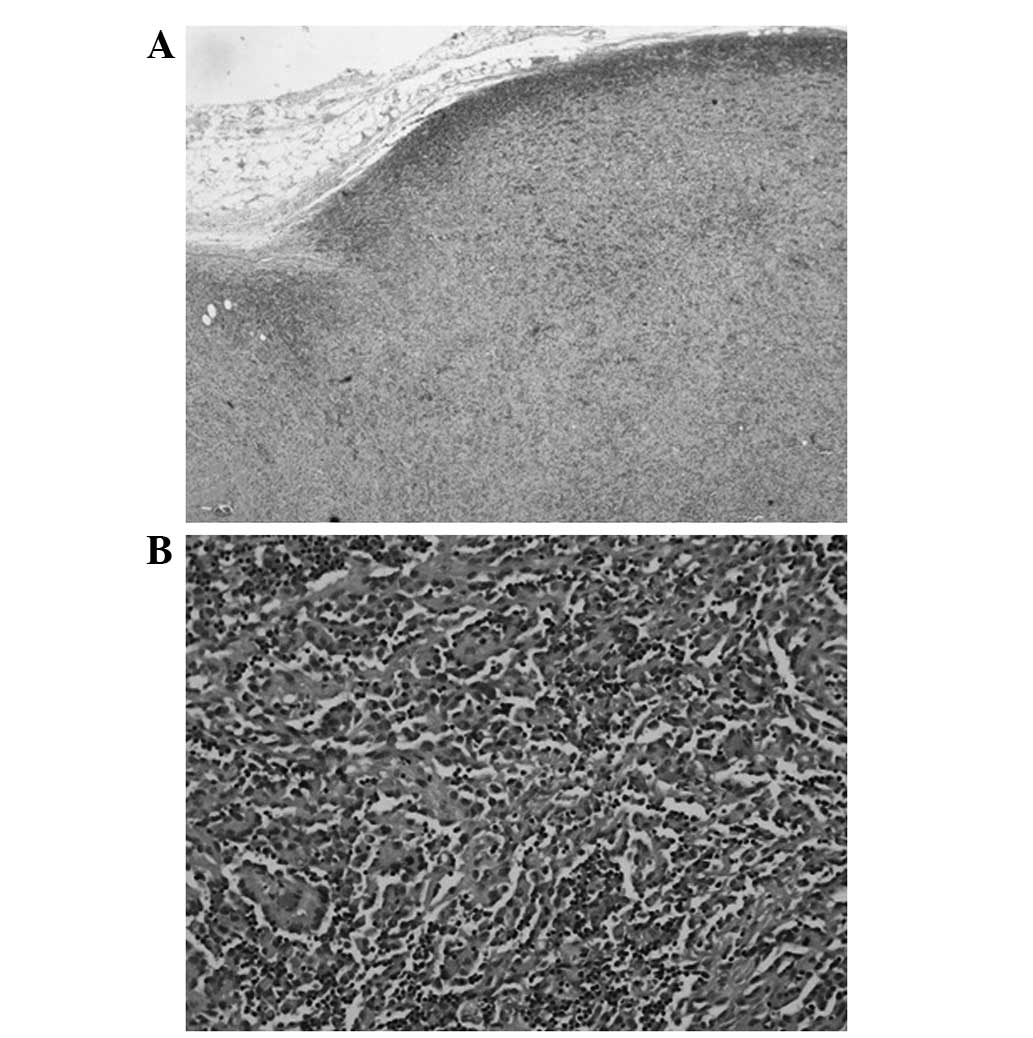
(Fig. 1). The remaining areas of
the body examined by CT were oncologically negative.
The mass was localized in the neck and was suspected
to be a lateral cervical lymph node metastasis. The patient then
underwent a neck dissection (levels II–IV) in the Department of
Otolaryngology, University Magna Graecia (Catanzaro, Italy).
The patient had no other vascular lesions and
continued the previous chemotherapy regimen one month later. The
patient subsequently finished the chemotherapy for colon cancer and
was oncologically negative at the last follow-up.
The neck lymphadenectomy specimen was accurately
sampled. Sections were fixed in 10% neutral-buffered formalin and
processed for light microscopy via conventional methods. Routine
processing for histological examination included paraffin
embedding, sectioning and staining with hematoxylin and eosin.
Sections prepared from the formalin-fixed,
paraffin-embedded tissue blocks were used for immunohistochemical
analysis. The sections were tested for von Willebrand factor (clone
F8/86, 1:50 dilution), CD31 (clone JC70A, 1:40 dilution), CD34
(clone QBEnd10, 1:250 dilution) (all from Dako, Glostrup, Denmark),
vascular endothelial growth factor receptor-3 (VEGFR-3; clone KLT9,
1:50 dilution; Leica Microsystems, Wetzlar, Germany), VEGF (clone
VG1, 1:50 dilution), podoplanin (clone D2-40, 1:200 dilution),
epithelial membrane antigen (clone E29, 1:100 dilution), S-100
protein (polyclonal, 1:2,000 dilution) (all from Dako), CK-AE1/AE3
(clone AE1/AE3, 1:100 dilution; Leica Microsystems) and desmin
(clone D33, 1:200 dilution; Dako) using an automated immunostainer
(Bond-Max™ Leica Microsystem, Melbourne, Australia).
Sections from tissues samples known to express the
detected proteins and sections from tissue samples known not to
express the proteins were used as the controls for each
immunohistochemical stain.
Of all the regional lymph node chains examined, only
the enlarged node shown on the CT-scan revealed the presence of a
tumoral infiltration.
Microscopically, the structure of the lymph node was
completely substituted by tumoral proliferation, with an
architectural pattern consisting of anastomosing vascular channels,
a number of which contained papillary projections or tuft-like
structures (Fig. 2).
The papillary sprouts had a hyaline core. The cells
exhibiting the papillations were large, with abundant,
eosinophilic, cytoplasm; the nuclei were partially crumpled, and
their size and shape varied. The chromatin was light and the
nucleoli were medium-sized (Fig.
2B).
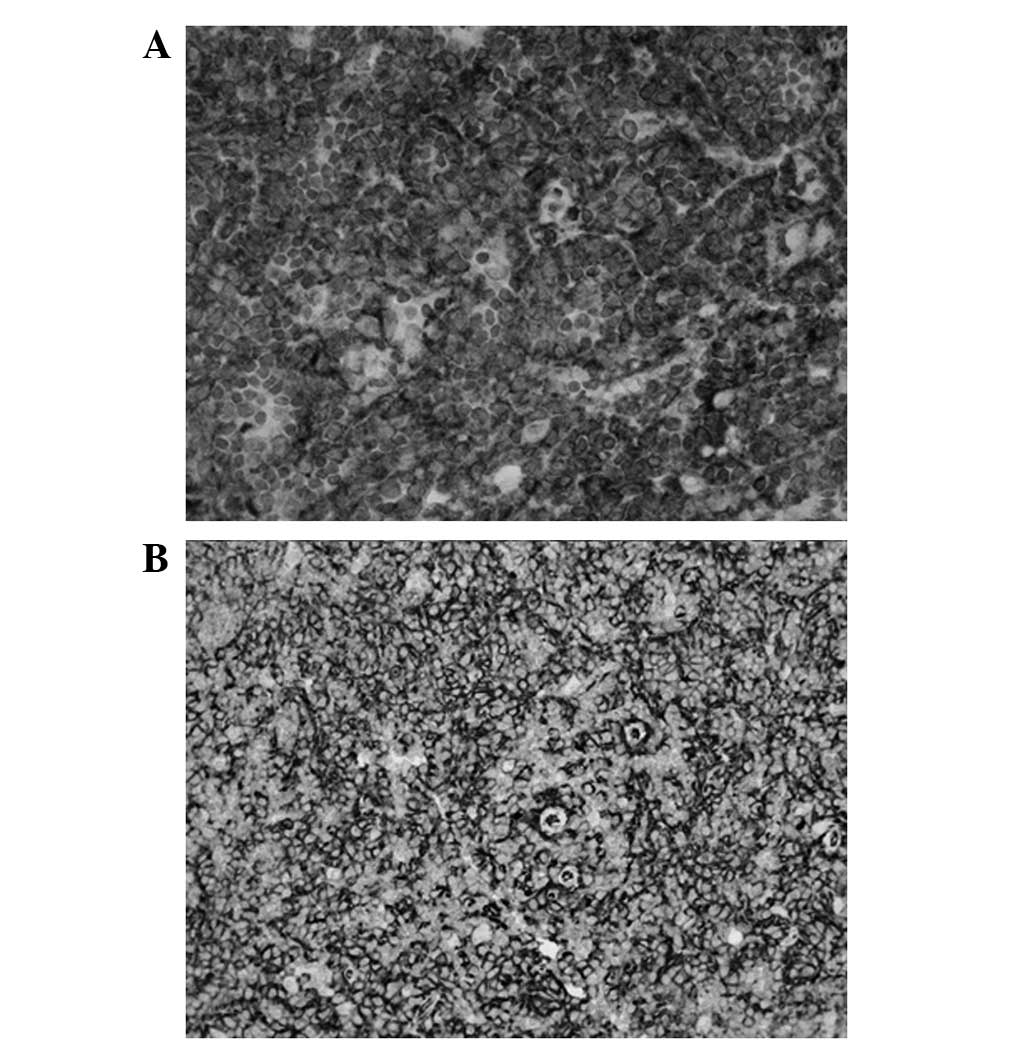
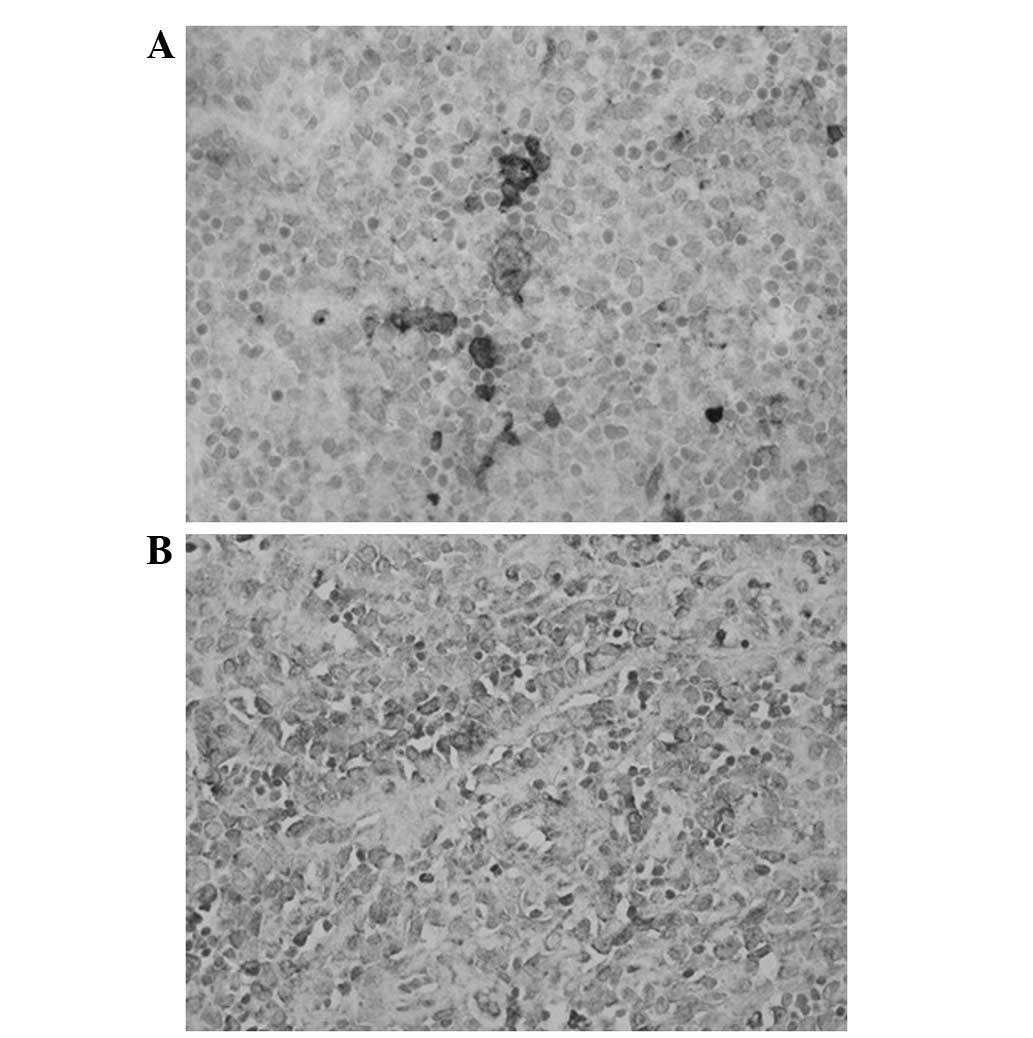
The tumor cells were positive immunohistochemically
for vimentin, von Willebrand factor, D2-40 (Fig. 3A), CD31 (Fig. 3B), VEGFR3 (Fig. 4A) and focally for CD34 and VEGF
(Fig. 4B). The tumoral elements
were negative for keratins, epithelial membrane antigen, S-100
protein and desmin. The final diagnosis was that of a
hemangioendothelioma.
Discussion
There are various types of lesions of the head and
neck regions that may occur in regional lymph node chains (3). Clinically, non-neoplastic
lymphadenopathy has to be differentiated from malignant lymphomas,
including Hodgkin’s, peripheral T-cell and non-Hodgkin’s B-cell
lymphomas. Patients affected by malignant neoplasms other than
lymphomas are often suspected as having metastases when a cervical
lymph node is enlarged. The patient examined in the present study
was suffering from a carcinoma of the colon with lung metastasis,
and a lymph node biopsy was considered necessary for further
evaluation of the stage of the disease and the effect of
chemotherapy. This patient is the second case in the literature of
a primary vascular lesion with Dabska-like features occurring in a
lymph node and is also the second case in a patient with a
carcinoma of the colon (2). Such an
association may be casual, however, other cases have to be
described in order to exclude the presence of a link.
Endovascular papillary angioendotheliomas, or Dabska
tumors, were first described in 1969 by Dabska (4). These tumors primarily affect the skin
of children (5), however, in recent
years it has been demonstrated that such a lesion may be present in
a wider age range and in more organs than originally described
(6). The literature describes a
category of ‘similar lesions’ (7),
which have two distinctive qualities, namely papillary growth and a
lymphatic immunophenotype with positivity for D2-40 (8) and VEGFR-3 (7,9). The
pathogenesis of such neoplasms remains obscure. The present study
documented immunohistochemically a focal production of VEGF from
tumoral cells and the presence of VEGFR-3 in the elements of the
neoplasia, so a VEGF/VEGFR-3 autocrine loop may have been activated
in the present case, as it is able to occur in several types of
solid tumors (10). Differential
diagnosis of node tumors should also include rare tumors, including
hemangioendotheliomas, particularly when the lymph node structure
is substituted by anastomosing vascular channels.
References
|
1
|
Chan JK, Frizzera G, Fletcher CD and Rosai
J: Primary vascular tumors of lymph nodes other than Kaposi’s
sarcoma. Analysis of 39 cases and delineation of two new entities.
Am J Surg Pathol. 16:335–350. 1992.
|
|
2
|
de Saint-Maur PP, Audouin J, Cazier A, Le
Tourneau A, Molina T and Diebold J: Nodal intralymphatic papillary
endothelial tumour with Dabska-like features: report of a case in
two mesenteric lymph nodes. Histopathology. 59:1027–1029.
2011.PubMed/NCBI
|
|
3
|
Greaves WO and Wang SA: Selected topics on
lymphoid lesions in the head and neck regions. Head Neck Pathol.
5:41–50. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dabska M: Malignant endovascular papillary
angioendothelioma of the skin in childhood. Clinicopathologic study
of 6 cases. Cancer. 24:503–510. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Schwartz RA, Dabski C and Dąbska M: The
Dabska tumor: a thirty-year retrospect. Dermatology. 201:1–5.
2000.PubMed/NCBI
|
|
6
|
Ward KA, Ecker PM, White RR, Melnik TE,
Gulbahce EH, Wilke MS and Sangueza OP: Papillary intralymphatic
angioendothelioma of the thigh: A case report and review of the
literature. Dermatol Online J. 16:42010.
|
|
7
|
Fanburg-Smith JC, Michal M, Partanen TA,
Alitalo K and Miettinen M: Papillary intralymphatic
angioendothelioma (PILA): a report of twelve cases of a distinctive
vascular tumor with phenotypic features of lymphatic vessels. Am J
Surg Pathol. 23:1004–1010. 1999. View Article : Google Scholar
|
|
8
|
Fukunaga M: Expression of D2–40 in
lymphatic endothelium of normal tissues and in vascular tumours.
Histopathology. 46:396–402. 2005.
|
|
9
|
Folpe AL, Veikkola T, Valtola R and Weiss
SW: Vascular endothelial growth factor receptor-3 (VEGFR-3): a
marker of vascular tumors with presumed lymphatic differentiation,
including Kaposi’s sarcoma, kaposiform and Dabska-type
hemangioendotheliomas, and a subset of angiosarcomas. Mod Pathol.
13:180–185. 2000.PubMed/NCBI
|
|
10
|
Su JL, Yen CJ, Chen PS, Chuang SE, Hong
CC, Kuo IH, Chen HY, Hung MC and Kuo ML: The role of the
VEGF-C/VEGFR-3 axis in cancer progression. Br J Cancer. 96:541–545.
2007. View Article : Google Scholar : PubMed/NCBI
|