Introduction
Endometrial stromal sarcoma (ESS) is a rare
malignancy and accounts for <1% of all uterine malignancies and
~15% of all uterine sarcomas (1).
In general, ESS occurs in perimenopausal and postmenopausal females
(2,3), and <25% of ESS patients are
premenopausal (4). The mainstay of
treatment for ESS is total hysterectomy and bilateral
salpingo-oophorectomy, and adjuvant treatments include
chemotherapy, radiation and endocrine therapy. ESS is classified
into two subtypes, high- and low-grade ESS, mainly on the basis of
pathological mitotic index and cytologic atypia (4). Considering that low-grade ESS is
associated with a markedly more favorable prognosis compared with
other uterine sarcomas, fertility-preserving treatment in young
nulliparous females is feasible. However, due to the rarity of the
disease, experience of conservative management in low-grade ESS is
limited (5).
The current report presents a case of low-grade ESS
which was initially misdiagnosed as submucous myoma according to
the ultrasonic examination. The patient was diagnosed with an
endometrial stromal nodule following primary hysteroscopic surgery
and was eventually diagnosed with low-grade ESS at the subsequent
laparotomy. A desired outcome was achieved; the patient
successfully conceived and delivered a healthy baby following the
second local excision and endocrine therapy.
Case report
A 25-year-old female was admitted to the Qilu
Hospital of Shandong University (Jinan, China) complaining of
menorrhagia and shortened menstrual cycles of three months and
acute lower abdominal pain lasting for 10 h. The patient had a
surgical history of right breast fibroadenoma removal at 23 years
of age. The patient’s medical history was unremarkable. A previous
B ultrasound examination demonstrated a hypoechoic lesion
(6.1×5.2×5.9 cm) with a clear borderline on the left posterior wall
of the uterus. Physical examination of the external genitalia,
vagina and cervix showed no abnormalities. Pelvic examination
revealed a regularly enlarged uterus, the size of 70 days
pregnancy. No adnexal masses were palpated. Primary diagnosis was
determined as submucous myoma and a myomectomy was performed by
hysteroscopy. During surgery, a submucous mass that resembled type
II myoma was found in the left posterior wall of the patient’s
uterus, with a hemorrhagic and necrotic surface. Due to the
incomplete resection, as a section of the mass was in the wall,
subsequent surgery was suggested. One week later, histological
results of the formalin-fixed resected mass confirmed a submucous
endometrial stromal nodule, immunohistochemically positive for
CD10. The patient recovered satisfactorily and was discharged from
hospital six days later.
Three months later, the patient returned to the
hospital for a laparotomy in order to resect the residual lesions.
The surgery was performed on May 31, 2010. During surgical
exploration, a convex mass with a diameter of 5 cm was detected on
the posterior wall of the enlarged uterus and the decision was made
to perform resection. The mass, which was detected to be
trans-endometrial and well-circumscribed from the surrounding
myometrium, was completely resected. Histological examination of
frozen sections of the resected mass during the surgery suggested
low-grade ESS. Thus, radical hysterectomy was proposed to the
patient’s family, but the family rejected and expressed a desire
for fertility preservation since the patient was nulliparous. As
there were no signs of tumor infiltration and metastasis, the
surgical procedure was changed to preserve and reconstruct the
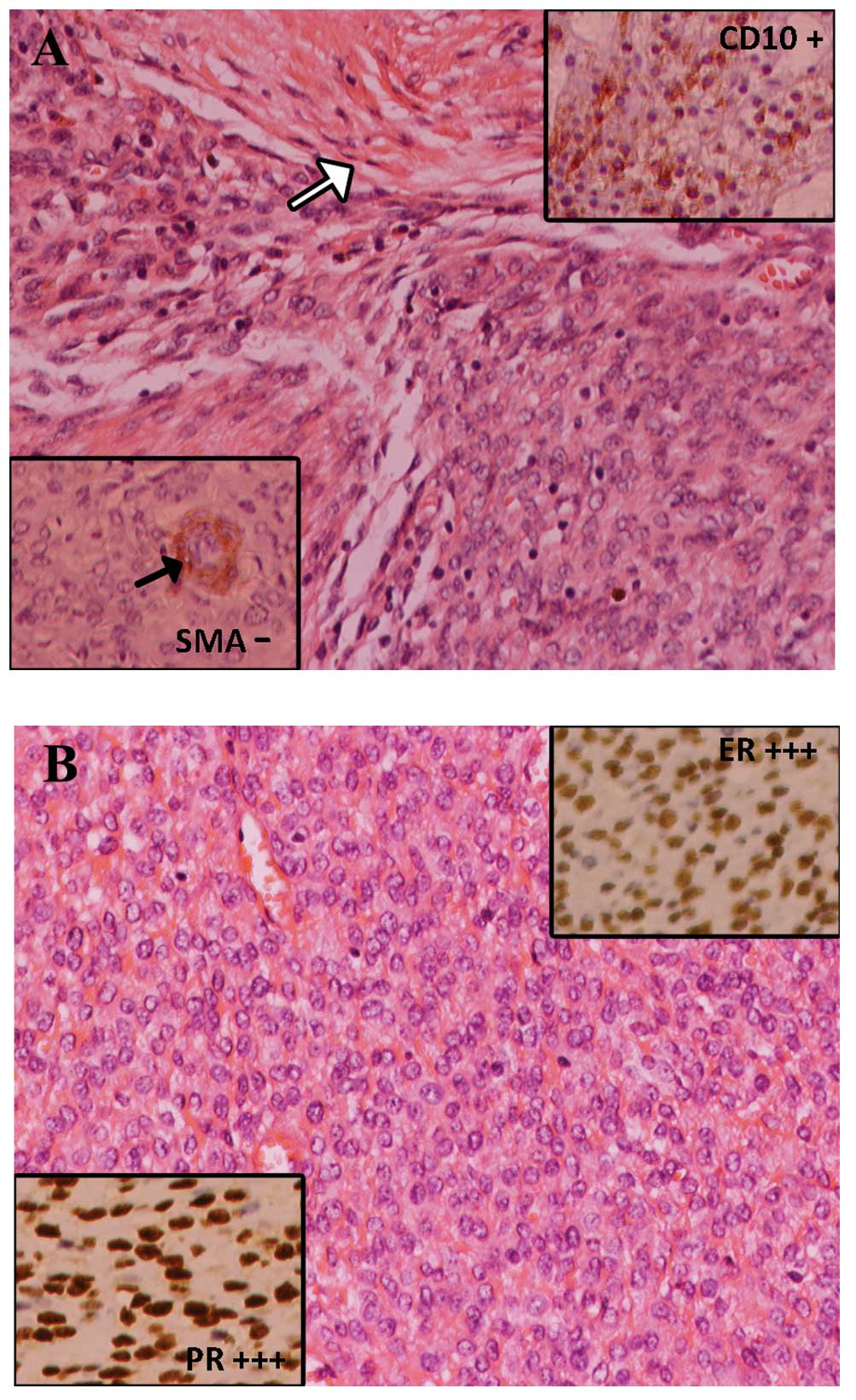
uterus, which was successfully accomplished. Final pathological
examination of the formalin-fixed resected tissue (4.5×3.3 cm)
confirmed the diagnosis of low-grade ESS. Various levels of
staining intensity are indicated by −, +, ++ and +++; negative,
weak, moderate and strong, respectively Immunohistochemistry showed
CD10(+), desmin(+), smooth muscle actin (SMA)(−) and 30% Ki67(+).
Further detection of estrogen receptor (ER), progesterone receptor
(PR) and p53 by immunohistochemistry showed ER(+++), PR(+++) and
p53(−) (Fig. 1).
Chemotherapy and endocrine therapy were suggested as
adjuvant treatments, but the patient declined chemotherapy
considering its side effects and the patient’s desire for
fertility. Medroxyprogesterone (250 mg) was administered daily for
one year to inhibit tumor recurrence. No abnormal abdominal or
pelvic observations were identified.
Following six months of medroxyprogesterone
withdrawal, the patient conceived naturally. Pregnancy was
uncomplicated and the patient delivered a healthy baby of 3,300 g
at 42 weeks’ gestation by cesarean section on November 22, 2012. On
January 9, 2013, the patient returned to the gynecological clinic
of the hospital for a general check-up and no signs of tumor
recurrence were identified. Written informed consent was
obtained.
Discussion
ESS is a rare malignant disease with an overall
five-year survival rate of ~30% (6). ESS accounts for only 15% of uterine
sarcomas. Due to its infrequency, ESS is commonly mistaken for
leiomyomas (7). Common clinical
signs of ESS include abnormal uterine bleeding, menorrhagia and
pelvic pain, which were all present in the current case report. ESS
is usually classified into low- and high-grades and the latter
generally involves perimenopausal and postmenopausal females who
exhibit blood metastasis at an early stage and relatively poor
prognosis. Compared with high-grade ESS in which mitotic figures
are common by microscopic examination, low-grade ESS has a tendency
of local recurrence with an indolent growth and its mitotic figures
are usually less than five per 10 high-power fields. The median
time of recurrence is 65 months for patients with low-grade ESS at
stage I (8).
The mainstay treatment for ESS is total abdominal
hysterectomy and bilateral salpingo-oophorectomy. Due to the rarity
of ESS in young nulliparous females, the occasional cases of ESS in
young patients are usually identified in histological examinations
of resected presumed leiomyomas of the uterus (3,9). The
current report presents a case of the local resection of a
low-grade ESS, in which fertility was preserved for the young
nulliparous female. Histopathologically, ESS is frequently
misdiagnosed with myoma. CD10 and SMA have been used as
immunohistochemical markers for distinguishing between ESS and
uterine smooth muscle tumors (10,11).
In the current report, it was via the results of
immunohistochemical staining (CD10-positive and SMA-negative) that
the diagnosis of ESS was determined. Adjuvant treatments of
low-grade ESS include chemotherapy, radiation and endocrine
therapy, among which endocrine therapy, particularly progestin
therapy, is considered the most effective for curing and preventing
local recurrence. Endocrine therapy is recommended as a routine
adjuvant management for primary and recurrent ESS (12). Considering the high expression
levels of ER and PR revealed in the current case report by
immunohistological examination, the patient was administered
medroxyprogesterone for one year following fertility-preserving
surgery. The therapeutic efficacy of medroxyprogesterone was
satisfactory. Following six months of drug withdrawal, the patient
successfully conceived and delivered a healthy baby at 42 weeks’
gestation.
Previous relevant literature concerning ESS were
extensively reviewed. Indeed, fertility-preserving surgery in young
nulliparous females had been proposed in several cases (2–5) and
successful pregnancy following such management had been reported,
shown in detail in Table I
(2,3). For patients who present with a
confined uterus mass and no signs of tumor metastasis or
infiltration, it is, in theory, feasible to preserve the patient’s
uterus. However, Koskas et al previously reported a case of
a 34-year-old female with a diagnosis of low-grade ESS who
underwent a severe peritoneal recurrence following the successful
delivery of a healthy baby (13).
Li et al also identified that surgery sparing ovarian
function increased the risk of recurrence of ESS compared with
those without the preservation of ovarian function (14). In addition, Amant et al
(15) and Picker et al
(16) each reported a case of ESS
during pregnancy. Although aggressive treatments were performed in
the two patients, the patients succumbed to their diseases six days
and two years following diagnosis, respectively. A possible
explanation was that high levels of circulating estrogen enhanced
the progression of the tumor. A previous study also reported that
the treatment outcome has a significant association with stage,
histological subtype, tumor size and positivity from cytologic
biopsy (17). Therefore,
conservative management must be performed with caution in young
nulliparous patients with ESS. The risk of preserving the uterus
must be sufficiently evaluated prior to fertility-preserving
surgery and consent of the patient must be obtained preoperatively.
Local resection of the uterus mass is inevitable and adjuvant
treatment, particularly endocrine treatment, also appears to be
necessary as illustrated by current evidence. Thereafter, strict
follow-up is required to monitor recurrence.
 | Table ISystematic review of ESS followed by
pregnancy. |
Table I
Systematic review of ESS followed by
pregnancy.
| Authors
(reference) | Age, years | Clinical
manifestation/initial symptoms | Surgery | Pathology | Adjuvant therapy | Time to
pregnancy | Recurrence | Treatment following
recurrence |
|---|
| Delaney et al
(2) | 16 | Menorrhagia and
abdominal distension | Local resection and
uterine construction | Low-grade ESS | Endocrine therapy
(megestrol acetate) | 8 years | No | NA |
| Yan et al
(3) | 25 | Menorrhagia | Local resection and
uterine construction | High-grade ESS | Chemotherapy
(etoposide and cisplatin) | 40 months | No | NA |
| Koskas et al
(13) | 34 | Infertility | Resection by
hysteroscopy | Low-grade ESS | No | 6 months | Severe peritoneal
resection | Endocrine therapy
(non-steroidal aromatase inhibitors |
Although ESS is a rare uterine malignancy with poor
prognosis, in selected cases with a local uterus mass and no signs
of metastasis and infiltration, conservative management, including
local surgical resection and adjuvant treatment, may be performed
to preserve fertility. The present case report suggests that
fertility preservation by local resection and uterine
reconstruction may be a viable option for young females with
low-grade ESS.
References
|
1
|
Nam JH: Surgical treatment of uterine
sarcoma. Best Pract Res Clin Obstet Gynaecol. 25:751–760. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Delaney AA, Gubbels AL, Remmenga S, Tomich
P and Molpus K: Successful pregnancy after fertility-sparing local
resection and uterine reconstruction for low-grade endometrial
stromal sarcoma. Obstet Gynecol. 120:486–489. 2012. View Article : Google Scholar
|
|
3
|
Yan L, Tian Y, Fu Y and Zhao X: Successful
pregnancy after fertility-preserving surgery for endometrial
stromal sarcoma. Fertil Steril. 93:269.e1–e3. 2010.PubMed/NCBI
|
|
4
|
Chang KL, Crabtree GS, Lim-Tan SK, Kempson
RL and Hendrickson MR: Primary uterine endometrial stromal
neoplasms. A clinicopathologic study of 117 cases. Am J Surg
Pathol. 14:415–438. 1990. View Article : Google Scholar
|
|
5
|
Stadsvold JL, Molpus KL, Baker JJ, Michael
K and Remmenga SW: Conservative management of a myxoid endometrial
stromal sarcoma in a 16-year-old nulliparous woman. Gynecol Oncol.
99:243–245. 2005.PubMed/NCBI
|
|
6
|
Oláh KS, Gee H, Blunt S, Dunn JA, Kelly K
and Chan KK: Retrospective analysis of 318 cases of uterine
sarcoma. Eur J Cancer. 27:1095–1099. 1991.
|
|
7
|
Jayakrishnan K, Koshy AK, Manjula P, Nair
AM, Ramachandran A and Kattoor J: Endometrial stromal sarcoma
mimicking a myoma. Fertil Steril. 92:1744–1746. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Amant F, Coosemans A, Debiec-Rychter M,
Timmerman D and Vergote I: Clinical management of uterine sarcomas.
Lancet Oncol. 10:1188–1198. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Parker WH, Fu YS and Berek JS: Uterine
sarcoma in patients operated on for presumed leiomyoma and rapidly
growing leiomyoma. Obstet Gynecol. 83:414–418. 1994.
|
|
10
|
Abeler VM and Nenodovic M: Diagnostic
immunohistochemistry in uterine sarcomas: a study of 397 cases. Int
J Gynecol Pathol. 30:236–243. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chu PG, Arber DA, Weiss LM and Chang KL:
Utility of CD10 in distinguishing between endometrial stromal
sarcoma and uterine smooth muscle tumors: an immunohistochemical
comparison of 34 cases. Mod Pathol. 14:465–471. 2001. View Article : Google Scholar
|
|
12
|
Chu MC, Mor G, Lim C, Zheng W, Parkash V
and Schwartz PE: Low-grade endometrial stromal sarcoma: hormonal
aspects. Gynecol Oncol. 90:170–176. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Koskas M, Morice P, Yazbeck C, Duvillard
P, Walker F and Madelenat P: Conservative management of low-grade
endometrial stromal sarcoma followed by pregnancy and severe
recurrence. Anticancer Res. 29:4147–4150. 2009.PubMed/NCBI
|
|
14
|
Li N, Wu LY, Zhang HT, An JS, Li XG and Ma
SK: Treatment options in stage I endometrial stromal sarcoma: a
retrospective analysis of 53 cases. Gynecol Oncol. 108:306–311.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Amant F, Van Calsteren K, Debiec-Rychter
M, Heyns L, De Beeck KO, Sagaert X, et al: High-grade endometrial
stromal sarcoma presenting in a 28-year-old woman during pregnancy:
a case report. J Med Case Rep. 4:2432010.
|
|
16
|
Picker RH, Pfanner DW, Payne W and
Coupland GE: Stromal sarcoma of the endometrium complicated by
pregnancy. Aust NZJ Obstet Gynaecol. 15:177–182. 1975. View Article : Google Scholar
|
|
17
|
Yalman D, Ozsaran Z, Baltalarli B, Demir
O, Ozdemir N and Aras A: Results of postoperative radiotherapy in
the treatment of uterine sarcomas: a retrospective analysis of 46
patients. Eur J Gynaecol Oncol. 29:46–51. 2008.PubMed/NCBI
|