Introduction
Hyperthermia is a promising approach for cancer
therapy. Various methods, including the use of hot water,
capacitive heating and magnetic nanoparticles with an alternating
magnetic field, have been reported to induce hyperthermia (1). Magnetic nanoparticles generate heat
under an alternating magnetic field by hysteresis loss. The
advantages of magnetic particles for hyperthermia induction are
biocompatibility, injectability, lack of toxicity, effective energy
absorption of the alternating magnetic field and high-level
accumulation in the target tumor (2). Typically, there are 2 ranges of
targeting temperature used in hyperthermic treatment. High
temperatures are ≥50°C and low temperatures are from 40–43°C
(2). High temperatures are usually
supposed to kill targeted tissue directly (3–5).
However, focal hyperthermia has been reported to induce an
anti-tumor reaction, independent of the initial thermal effects
(6). In addition, the
hyperthermia-induced inhibition of angiogenesis may contribute to
the anti-tumor reaction.
Angiogenesis, an essential component of pathological
and physiological processes, is the formation of new blood vessels
from existing vasculature. The predominant stimulator of
angiogenesis is vascular endothelial growth factor (VEGF)-A
(7). In the majority of cancer
types, under pathological conditions, VEGF is secreted by tumor
cells and promotes the formation of new blood vessels by acting on
the endothelial cells of existing vessels (7,8). The
growth and malignant dissemination of solid tumors is dependent on
pathological angiogenesis (9). VEGF
binds to two associated receptors, VEGF receptor 1 (Flt-1) and 2
(Flk-1 or KDR) (10). Inhibition of
VEGF or its signaling via these receptors is a promising strategy
to block angiogenesis and the subsequent tumor growth and
metastases (8).
Angiogenesis has been reported to be blocked by
hyperthermia (11,12). However, the effect of hyperthermic
magnetic nanoparticles on the expression of VEGF and VEGF receptors
and on angiogenesis has not been elucidated. In the present study,
the effect of hyperthermic magnetic nanoparticles on tumor growth,
and the expression of VEGF and its receptors were investigated.
Materials and methods
Animals
All animal experiments were conducted in accordance
with the ‘Guide for the care and use of laboratory animals of the
School of Medicine, Tsinghua University’ in Tsinghua University
(Beijing, China). Wistar rats with a body weight of ~130 g were
purchased from the Institute of Laboratory Animal Sciences, Chinese
Academy of Medical Sciences (Beijing, China). This study was
approved by the ethics committee of Tsinghua University (Beijing,
China).
Tumor inoculation and treatment
The Walker-256 tumor cells were obtained from the
Institute of Materia Medica, Chinese Academy of Medical Sciences
(Beijing, China). The rats were injected in the right flanks with
2×106 Walker-256 tumor cells, obtained from an ascitic
Walker-256 tumor-bearing rat. Following inoculation, the diameter
of the tumors at 8 days ranged between 0.5 and 0.8 cm. Saline or
62.5 mg/ml magnetic nanoparticle fluid, with a volume at 50% of
each tumor, was intratumorally injected, as described previously
(13). Magnetic
Fe3O4 nanoparticles with a mean diameter of
20 nm were prepared, as previously described (14). The rats were randomly allocated to 5
groups of 24 rats each, including rats injected with saline without
magnetic field treatment (NS group), rats injected with magnetic
nanoparticle fluid without magnetic field treatment (MF group) and
rats injected with magnetic nanoparticle fluid with magnetic field
treatment performed once (MFH1 group), twice (MFH2 group) or three
times (MFH3 group). The animals were treated with an alternating
current magnetic field at a frequency of 180 kHz, 55 GS for 30 min,
and the temperatures inside the tumors were monitored with a
temperature probe and manually adjusted to 50–55°C, similar to
previously described (13). In the
MFH2 and MFH3 groups, the subsequent treatment was performed 24 h
after the previous treatment.
Tumor volume measurement
The size of the tumors was measured every 2 days
with a caliper. The tumor volume was then calculated with the
following formula: Tumor volume = 0.5 × (length ×
width2).
Immunohistochemistry
For the immunohistochemical staining, the tumors
were resected and fixed in a 10% formalin solution 4 days after the
hyperthermia treatment. The tumor tissues were sectioned to a 5-μm
thickness and fixed to slides. The slides were deparaffinized and
incubated with 10% normal serum for 30 min to block background
staining. The slides were then incubated for 60 min at 37°C with a
rabbit anti-VEGF polyclonal antibody (Santa Cruz Biotechnology,
Inc., Santa Cruz, CA, USA) or a rabbit anti-cluster of
differentiation (CD)34 polyclonal antibody (Boster Biological
Technology, Ltd., Wuhan, China), and subsequently incubated with
horseradish peroxidase-conjugated secondary antibodies. Each step
was followed by washing with phosphate-buffered saline three times.
Peroxidase activity was visualized by treatment with 0.02%
diaminobenzidine tetrahydrochloride solution containing 0.005%
hydrogen peroxide at room temperature for 5–10 min. The sections
were also counterstained with hematoxylin and eosin. Iron in the
magnetic nanoparticles was stained with prussian blue. Protein
quantification was performed by Imagepro-plus 6.0 software (Media
Cybernetics, Rockville, MD, USA), and the intensity values were
normalized to the background.
Reverse transcription polymerase chain
reaction (RT-PCR)
Total RNA was extracted using TRIzol (Invitrogen,
Carlsbad, CA, USA), as described by the manufacturer. mRNA was
reverse transcribed with RevertAid (MBI Fermentas, Inc.,
Burlington, ON, Canada) at 42°C for 60 min, and the resulting cDNA
was subjected to PCR (94°C for 1 min followed by 20–25 cycles at
94°C for 30 sec, 60°C for 30 sec, 68°C for 1 min and an extension
for 10 min at 68°C). The PCR products were separated on 1.0%
agarose gels and visualized with ethidium bromide. The forward (F)
and reverse (R) primer pairs are listed (5′ to 3′) as follows:
VEGF-F, CCTGGTGGACATCTTCCAGGAGTACC and VEGF-R,
GAAGCTCATCTCTCCTATGTGCTGGC; Flt-1-F, CGGGATCCAAGGGACTCTACACTTGTC
and Flt-1-R, GGAATTCCCGAATAGCGAGCAGATTT; Flk-1-F,
CATTGTGTCCTGCATCCGGGATAACCT and Flk-1-R,
TGTACACGATGCCATGCTCGTCACTGA; 18S-RNA-F, GCCCGAAGCGTTTACTTTGAA and
18S-RNA-R, GGTGAGGTTTCCCGTGTTGA. The quantification of gene
expression was performed by Imagepro-plus 6.0 software, and the
intensity values were normalized to 18S RNA.
Statistical analysis
All experiments were performed at least three times
and the representative results are shown. Results are expressed as
the mean ± standard deviation. The differences between groups were
examined for statistical significance using Student’s t-test,
except where indicated. Survival rate was assessed using the
Kaplan-Meier method and log-rank test. P≤0.05 was considered to
indicate a statistically significant difference.
Results
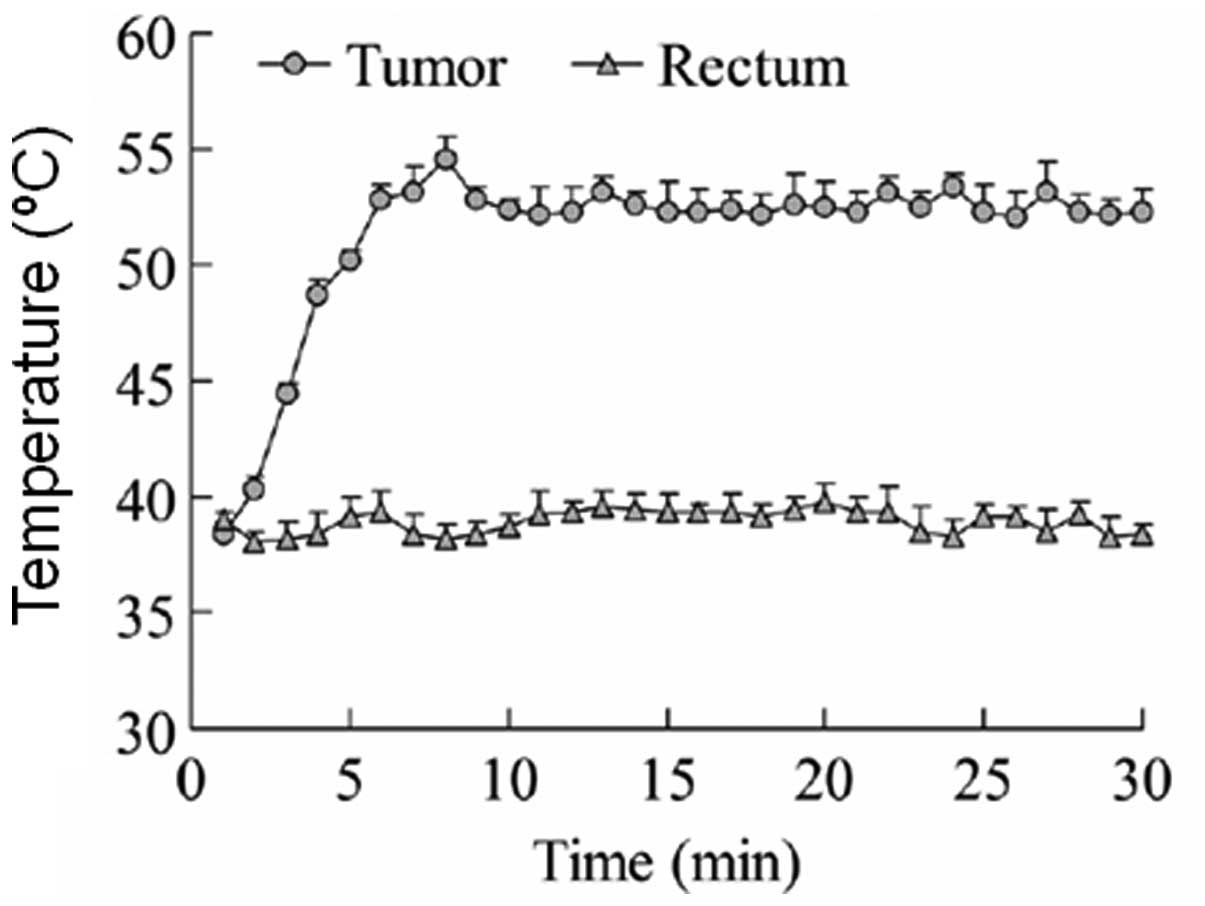
Intratumoral administration of MFH
induces a high temperature inside Walker-256 tumors
First, the rat breast carcinoma models were
established by inoculation of Walker-256 tumor cells in the right
flanks of the rats. When the tumor reached 0.5–0.8 cm in diameter,
hyperthermia treatment was performed by the intratumoral
administration of MFH, and the temperature in the tumors were
measured to determine whether a high temperature had been induced.
Fig. 1 shows the mean temperature
inside the tumor tissues after hyperthermia treatment, and the
temperature inside the rectum as a control. The temperature inside
the tumor tissues was increased to 52.5°C rapidly with the MFH
treatment, and was maintained within ±2.5°C for the remainder of
the treatment. In the controls, the rectal temperature remained
normal following the alternating magnetic field treatment. These
results indicate that a high temperature was induced successfully
in the tumor tissues by MFH.
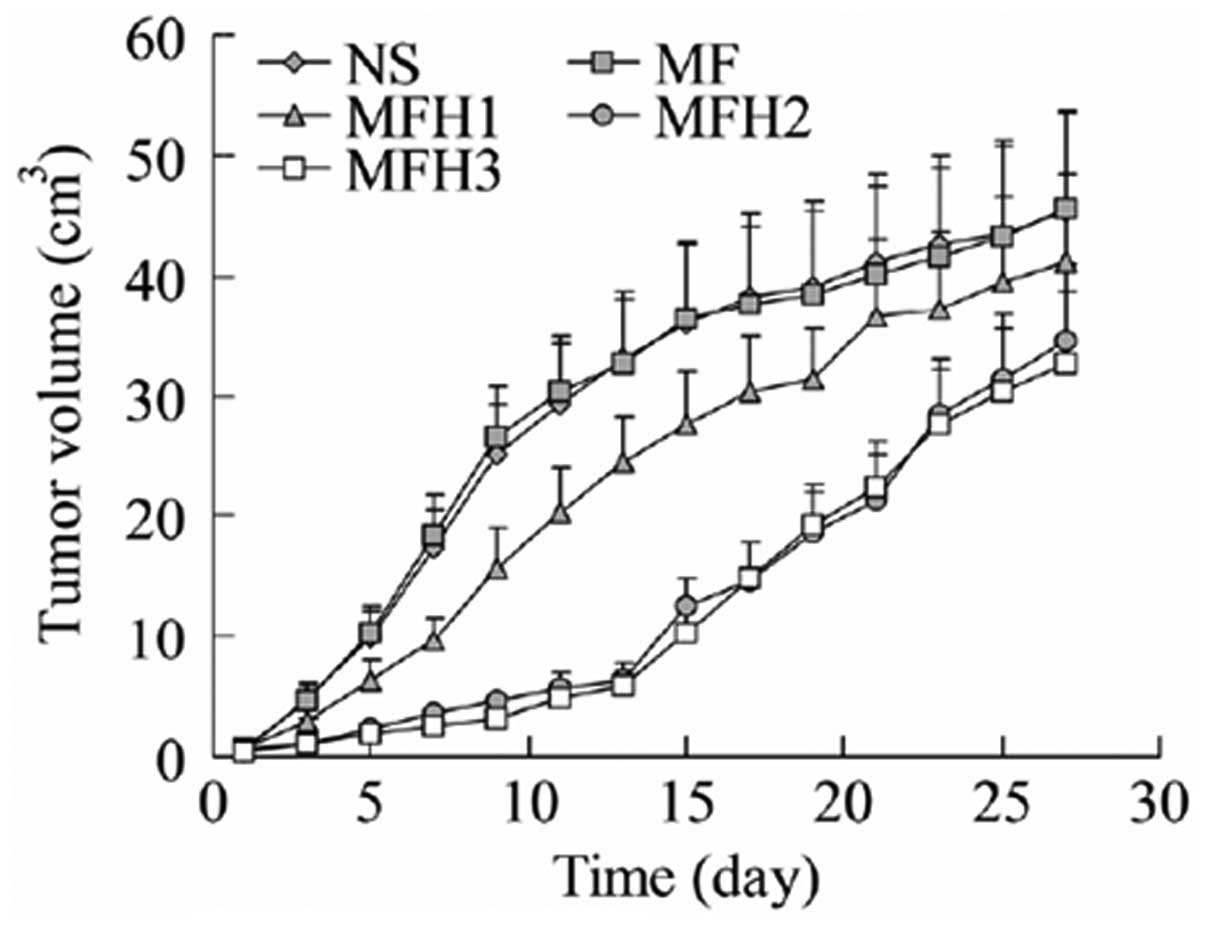
MFH treatment using magnetic
nanoparticles inhibits tumor growth
MFH has been reported to be feasible for tumor
therapy in several cancer types (15–20).
In the present study, following the induction of a high temperature
in the tumor tissues, attention was paid to the effect of
hyperthermia on tumor growth. As shown in Fig. 2, the treatment of tumors with MFH
downregulated tumor growth. When compared with the rats injected
with saline without the magnetic field treatment (NS group), the
rats injected with the magnetic nanoparticle fluid without magnetic
field treatment (MF group) had extremely similar tumor growth
profiles. These results indicated that the magnetic nanoparticle
fluid itself did not affect tumor growth. The rats injected with
the magnetic nanoparticle fluid with the magnetic field treatment
performed once (MFH1 group) had significantly reduced tumor growth
compared with the rats in the NS or MF groups. The rats injected
with the magnetic nanoparticle fluid with the magnetic field
treatment performed twice (MFH2 group) or three times (MFH3 group)
had dramatically reduced tumor growth. The inhibition of tumor
growth induced by the MFH treatment lasted for ~2 weeks. The speed
of the tumor growth in the MFH2 and MFH3 groups was gradually
recovered to that of the NS or MF groups two weeks later.
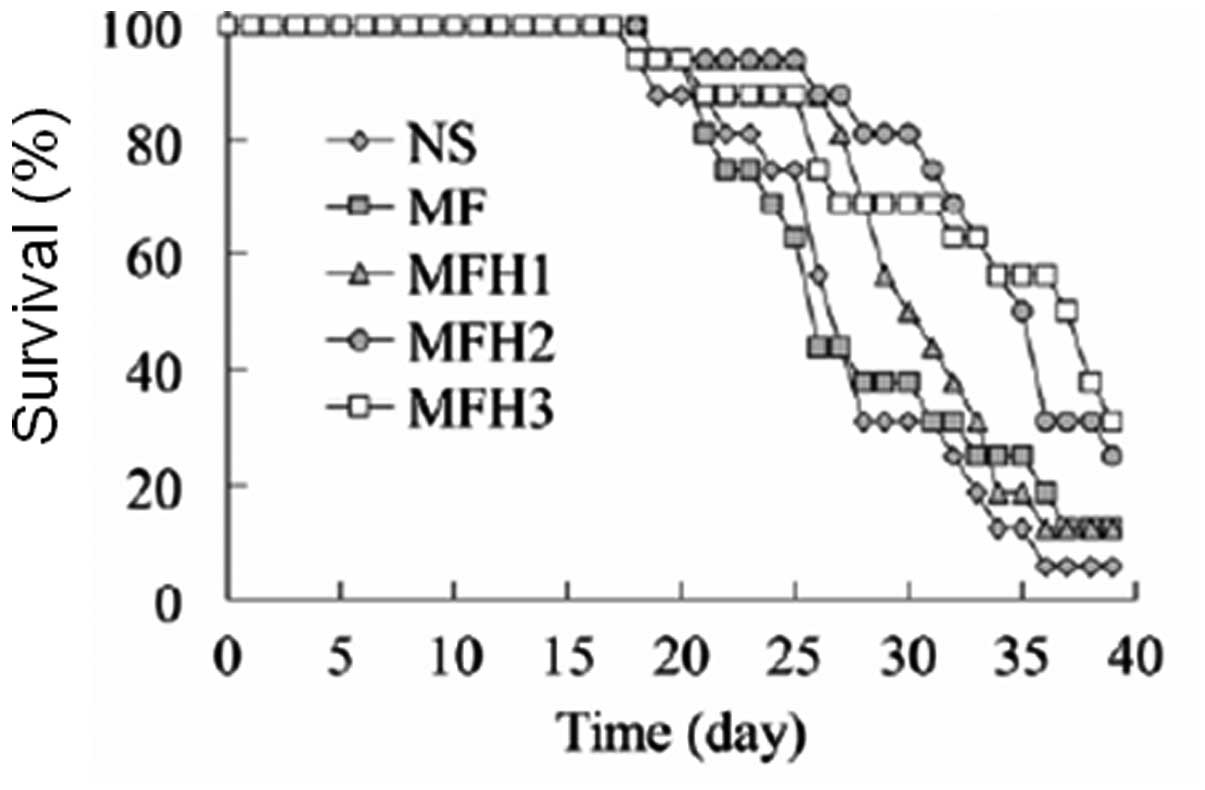
MFH treatment promotes survival of
tumor-bearing rats
As it was found that MFH treatment inhibited tumor
growth in vivo, attention was paid to the effect of MFH on
the survival rate of the tumor-bearing rats. The results in
Fig. 3 show that consistent with
the effect of the MFH treatment on tumor growth, the rats injected
with the magnetic nanoparticle fluid with the magnetic field
treatment performed twice (MFH2 group) or three times (MFH3 group)
had a significantly increased survival rate compared with the rats
injected with saline (NS group) or with the magnetic nanoparticle
fluid without the magnetic field treatment (MF group)
(P<0.05).
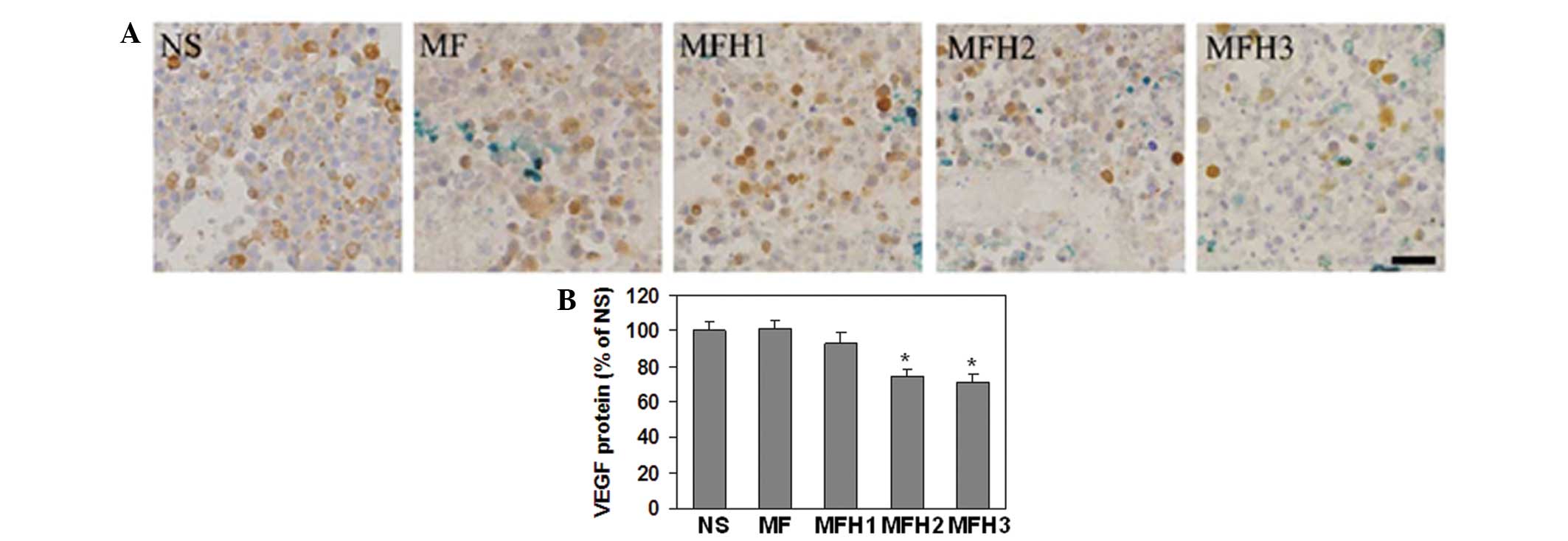
VEGF expression is reduced by
hyperthermia treatment
Hyperthermia has been reported to inhibit tumor
growth by the downregulation of angiogenesis (11,12).
To confirm whether angiogenesis was affected in the present rat
breast carcinoma model, the VEGF protein in the tumor tissues 4
days after MFH treatment was detected by immunohistochemistry. As
shown in Fig. 4A and B, the VEGF
protein level in the MFH2 or MFH3 groups was significantly reduced
by the MFH treatment compared with that in the NS or MF groups.
These results indicate that hyperthermia treatment may affect
angiogenesis by the downregulation of VEGF expression.
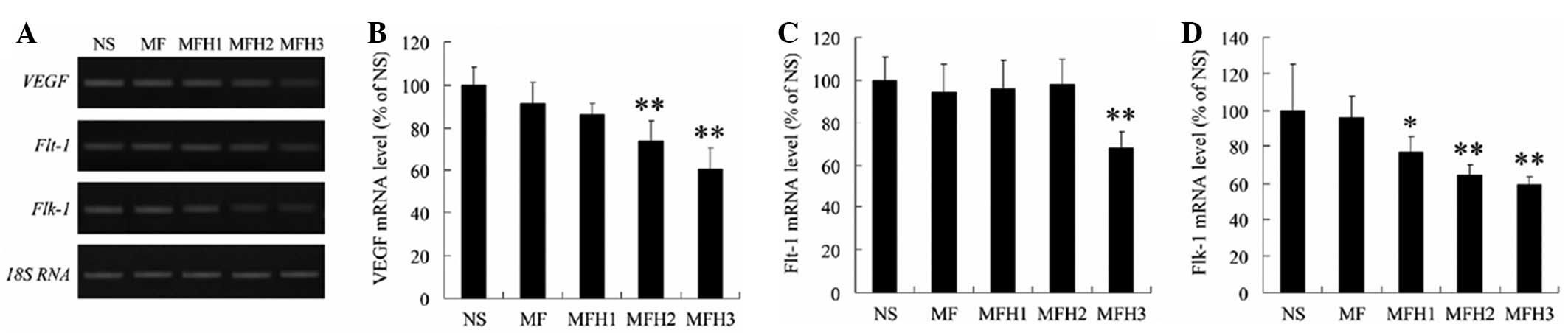
MFH downregulates the gene expression of
VEGF and its receptors, Flt-1 and Flk-1
To further confirm the effect of the MFH treatment
on VEGF expression, the gene expression of VEGF and its receptors,
Flt-1 and Flk-1, was measured by RT-PCR, and 18S RNA was amplified
as the internal control. As shown in Fig. 5A and B, the VEGF mRNA level in the
MFH2 or MFH3 groups was significantly reduced by the MFH treatment
compared with that in the NS or MF groups, which is consistent with
the protein expression of VEGF affected by the MFH treatment.
Similarly, the mRNA level of Flt-1 was significantly reduced in the
MFH3 group (Fig. 5A and C), and the
mRNA level of Flk-1 was slightly reduced in the MFH1 group and
markedly downregulated in the MFH2 and MFH3 groups (Fig. 5A and D). These results also indicate
that MFH treatment may inhibit angiogenesis by downregulation of
VEGF and its receptors, Flt-1 and Flk-1.
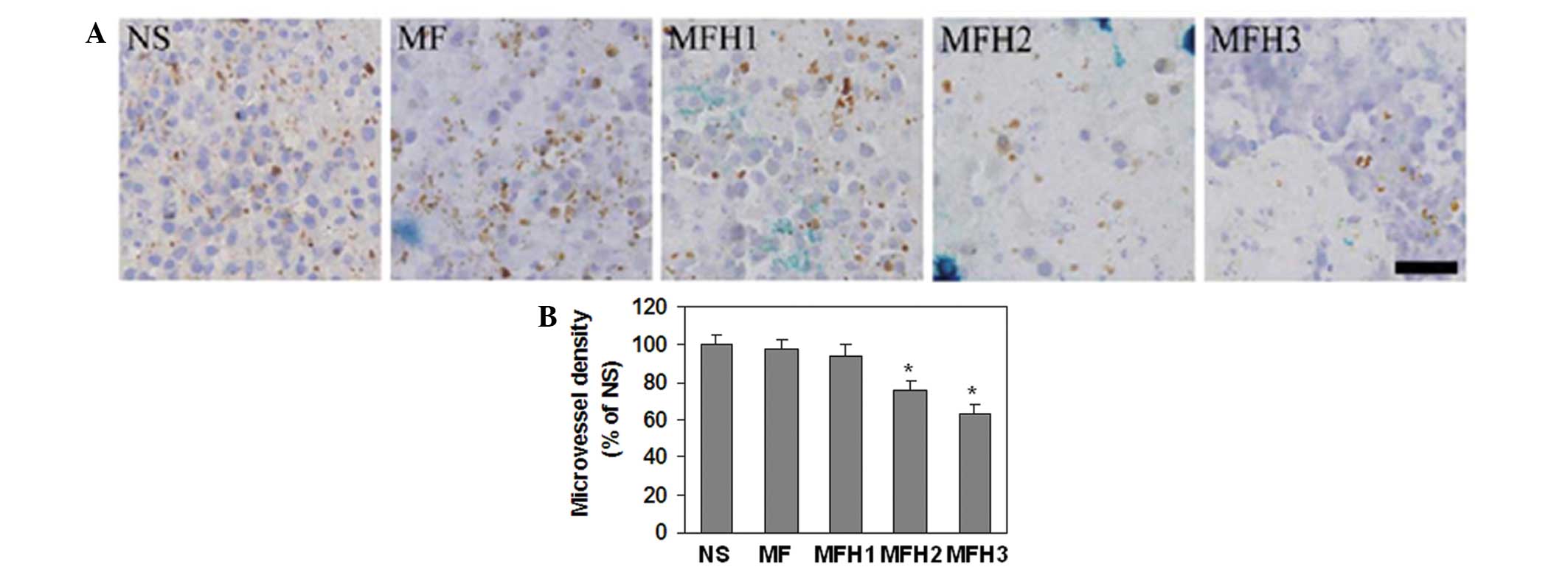
MFH treatment significantly decreases the
microvessel density
CD34 has been reported to be a marker for
microvessel density (21–22). Therefore, the microvessel density
was detected using immunohistochemistry with the anti-CD34 antibody
(Fig. 6), as described previously
(23). As expected, the microvessel
density in the MFH2 and MFH3 groups was significantly reduced by
the MFH treatment compared with that in the NS and MF groups
(Fig. 6). The microvessel density
in the MFH1 group was not significantly different compared with
that in the NS or MF groups (Fig.
6). These results further demonstrated that the MFH treatment
with magnetic nanoparticles inhibited angiogenesis.
Discussion
Similar to the results of a previous study, which
showed that hyperthermia treatment with magnetic nanoparticle fluid
at ~54°C significantly inhibited tumor growth in a rat tumor model
induced by implantation of MatLyLu-cells into the prostates of rats
(13), the present study also
observed that hyperthermia treatment at 52.5±2.5°C reduced
Walker-256 tumor growth. However, following relatively long-term
observation, it was found that 2 weeks after hyperthermia
treatment, the tumor growth recovered partly to the levels in the
control groups. In addition, it was also found that performing the
MFH treatment once did not inhibit tumor growth significantly, but
that repeating the MFH treatment two or three times inhibited tumor
growth and also promoted the survival of the tumor-bearing rats.
These results indicate that in order to properly control tumor
growth, repeated and lasting MFH treatment is required.
VEGF and its downstream signaling play a significant
role in angiogenesis and tumor progression (7,8).
Hyperthermia has been reported to inhibit the expression of VEGF
and its receptors, which downregulates angiogenesis and thus
facilitates the inhibition of tumor growth. For example,
hyperthermia at 42°C was shown to suppress the gene and protein
expression of VEGF in human fibrosarcoma HT-1080 cells, and the
level of VEGF in sera from cancer patients was significantly
diminished 2–3 weeks after treatment with whole-body hyperthermia
at 42°C (24). In addition, it was
reported that heat exposures between 41 and 45°C also directly
inhibited angiogenesis in mice (11,12).
In the present study, it was shown that hyperthermia treatment at
52.5±2.5°C inhibited the expression of VEGF, Flt-1 and Flk-1 and
inhibited angiogenesis. As magnetic nanoparticles alone did not
affect the expression of VEGF, Flt-1 and Flk-1 and angiogenesis, it
was concluded that the effect of magnetic nanoparticle-induced
hyperthermia on angiogenesis is similar to that induced by other
heat exposures.
Taken together, the present study results showed
that hyperthermia treatment at 52.5±2.5°C using magnetic
nanoparticles inhibited tumor growth, promoted the survival of the
tumor-bearing rats and inhibited angiogenesis potentially by the
downregulation of the expression of VEGF and its receptors,
including Flt-1 and Flk-1. These results indicate that the
hyperthermia-induced inhibition of VEGF and its receptors may be
involved in tumor thermotherapy.
Acknowledgements
This study was supported by grants from the National
Natural Science Foundation of China (30571779 and 10775085), the
Yuyuan Medical Science Foundation Program of Tsinghua University
and the Science and Technology Commission of Beijing Municipality
(Z07000200540704).
References
|
1
|
Ito A, Shinkai M, Honda H and Kobayashi T:
Medical application of functionalized magnetic nanoparticles. J
Biosci Bioeng. 100:1–11. 2005. View Article : Google Scholar
|
|
2
|
Motoyama J, Yamashita N, Morino T, Tanaka
M, Kobayashi T and Honda H: Hyperthermic treatment of DMBA-induced
rat mammary cancer using magnetic nanoparticles. Biomagn Res
Technol. 6:22008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Muralidharan V, Malcontenti-Wilson C and
Christophi C: Interstitial laser hyperthermia for colorectal liver
metastases: the effect of thermal sensitization and the use of a
cylindrical diffuser tip on tumor necrosis. J Clin Laser Med Surg.
20:189–196. 2002. View Article : Google Scholar
|
|
4
|
Patrício MB, Soares J and Vilhena M:
Morphologic and morphometric studies on tumor necrosis produced by
radiotherapy, and hyperthermia singly and in combination. J Surg
Oncol. 42:5–10. 1989.PubMed/NCBI
|
|
5
|
Tschoep-Lechner KE, Milani V, Berger F, et
al: Gemcitabine and cisplatin combined with regional hyperthermia
as second-line treatment in patients with gemcitabine-refractory
advanced pancreatic cancer. Int J Hyperthermia. 29:8–16. 2013.
View Article : Google Scholar
|
|
6
|
Nikfarjam M, Malcontenti-Wilson C and
Christophi C: Focal hyperthermia produces progressive tumor
necrosis independent of the initial thermal effects. J Gastrointest
Surg. 9:410–417. 2005. View Article : Google Scholar
|
|
7
|
Ferrara N, Gerber HP and LeCouter J: The
biology of VEGF and its receptors. Nat Med. 9:669–676. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tabernero J: The role of VEGF and EGFR
inhibition: implications for combining anti-VEGF and anti-EGFR
agents. Mol Cancer Res. 5:203–220. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bergers G and Benjamin LE: Tumorigenesis
and the angiogenic switch. Nat Rev Cancer. 3:401–410. 2003.
View Article : Google Scholar
|
|
10
|
Olsson AK, Dimberg A, Kreuger J and
Claesson-Welsh L: VEGF receptor signalling - in control of vascular
function. Nat Rev Mol Cell Biol. 7:359–371. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fajardo LF, Prionas SD, Kowalski J and
Kwan HH: Hyperthermia inhibits angiogenesis. Radiat Res.
114:297–306. 1988. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Roca C, Primo L, Valdembri D, et al:
Hyperthermia inhibits angiogenesis by a plasminogen activator
inhibitor 1-dependent mechanism. Cancer Res. 63:1500–1507.
2003.PubMed/NCBI
|
|
13
|
Johannsen M, Thiesen B, Jordan A, et al:
Magnetic fluid hyperthermia (MFH) reduces prostate cancer growth in
the orthotopic Dunning R3327 rat model. Prostate. 64:283–292. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhang S, Bian Z, Gu C, et al: Preparation
of anti-human cardiac troponin I immunomagnetic nanoparticles and
biological activity assays. Colloids Surf B Biointerfaces.
55:143–148. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang ZY, Song J and Zhang DS: Nanosized
As2O3/Fe2O3 complexes combined with magnetic fluid hyperthermia
selectively target liver cancer cells. World J Gastroenterol.
15:2995–3002. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Müller S: Magnetic fluid hyperthermia
therapy for malignant brain tumors - an ethical discussion.
Nanomedicine. 5:387–393. 2009.PubMed/NCBI
|
|
17
|
Yan S, Zhang D, Gu N, et al: Therapeutic
effect of Fe2O3 nanoparticles combined with magnetic fluid
hyperthermia on cultured liver cancer cells and xenograft liver
cancers. J Nanosci Nanotechnol. 5:1185–1192. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Johannsen M, Thiesen B, Gneveckow U, et
al: Thermotherapy using magnetic nanoparticles combined with
external radiation in an orthotopic rat model of prostate cancer.
Prostate. 66:97–104. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Johannsen M, Jordan A, Scholz R, et al:
Evaluation of magnetic fluid hyperthermia in a standard rat model
of prostate cancer. J Endourol. 18:495–500. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jordan A, Scholz R, Wust P, et al: Effects
of magnetic fluid hyperthermia (MFH) on C3H mammary carcinoma in
vivo. Int J Hyperthermia. 13:587–605. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bottini A, Berruti A, Bersiga A, et al:
Changes in microvessel density as assessed by CD34 antibodies after
primary chemotherapy in human breast cancer. Clin Cancer Res.
8:1816–1821. 2002.PubMed/NCBI
|
|
22
|
de la Taille A, Katz AE, Bagiella E, et
al: Microvessel density as a predictor of PSA recurrence after
radical prostatectomy. A comparison of CD34 and CD31. Am J Clin
Pathol. 113:555–562. 2000.PubMed/NCBI
|
|
23
|
Ruan J, Hyjek E, Kermani P, et al:
Magnitude of stromal hemangiogenesis correlates with histologic
subtype of non-Hodgkin’s lymphoma. Clin Cancer Res. 12:5622–5631.
2006.PubMed/NCBI
|
|
24
|
Sawaji Y, Sato T, Takeuchi A, Hirata M and
Ito A: Anti-angiogenic action of hyperthermia by suppressing gene
expression and production of tumour-derived vascular endothelial
growth factor in vivo and in vitro. Br J Cancer. 86:1597–1603.
2002. View Article : Google Scholar : PubMed/NCBI
|