Introduction
Malignant fibrous histiocytoma (MFH), also known as
undifferentiated pleomorphic sarcoma, is the most common type of
sarcoma in adults aged ≥50 years (1). Although MFH can occur almost anywhere,
including in the bone, due to its mesenchymal origin, it normally
occurs in the deep planes of proximal extremities, in the
retroperitoneum and in the torso (1–5).
Retroperitoneal involvement is relatively uncommon however, and the
presence of MFH in a visceral organ is exceedingly rare. Primary
MFH of the liver is an unusual condition, accounting for <1% of
primary hepatic malignancies (2).
Two cases with primary MFH of the liver occurred in The 302nd
Hospital (Beijing, China). The present study reports those two
novel cases, with particular emphasis on the magnetic resonance
imaging (MRI) findings. Written informed consent was obtained from
both patients.
Case report
The present study reports two cases of primary
hepatic MFH, with analysis of the ultrasound and MRI findings. The
first case was of a 67-year-old male who had no symptoms or
abnormal physical signs on routine physical examination. Other
possible significant laboratory abnormalities, which included
changes in serum transaminase (aspartate transaminase, 20 units/l;
normal range, 8–40 units/l; alanine transaminase, 32 units/l;
normal range, 5–40 units/l), serum bilirubin (total bilirubin, 18.6
μmol/l; normal range, 3.4–20.5 μmol/l; direct bilirubin, 6.8
μmol/l; normal range, 0–6.8 μmol/l) and serum α-fetoprotein (2.0
ng/ml; normal range, 0–20 ng/ml) concentrations, were not present.
The patient was referred to the Department of Surgery (The 302nd
Hospital) for further investigation of a hepatic tumor detected by
a B-scan ultrasound.
The second case was of a 35-year-old male who was
serologically positive for hepatitis B surface antigen and was
admitted to the Department of Surgery with a history of persistent
epigastric abdominal pain and weight loss. The serum concentrations
of alkaline phosphatase and fibrinogen were increased to 259 U/l
(normal range; 40–150 U/l) and 4.65g/l (normal range; 2.0–4.5 g/l),
respectively. Serum α-fetoprotein (14.8 ng/ml; normal range,
0.00–20.00 ng/ml) concentrations were also normal. The patient
underwent a liver ultrasonogram, which revealed a large hypoechoic
lesion occupying the greater portion of the right lobe.
The two patients underwent MRI prior to therapy. MRI
was performed using a 1.5-T MRI system (Signa HDx 1.5T; GE
Healthcare, Cleveland, OH, USA). Overall, the imaging examinations
performed consisted of axial T1 and T2 weighted imaging (WI) with
fat suppression, in and out phase imaging, diffusion weighted
imaging (b=0.800 sec/mm2) and use of post-contrast liver
acquisition volume acceleration sequences, including arterial,
portal venous, delayed phase and coronal T1WI with fat
suppression.
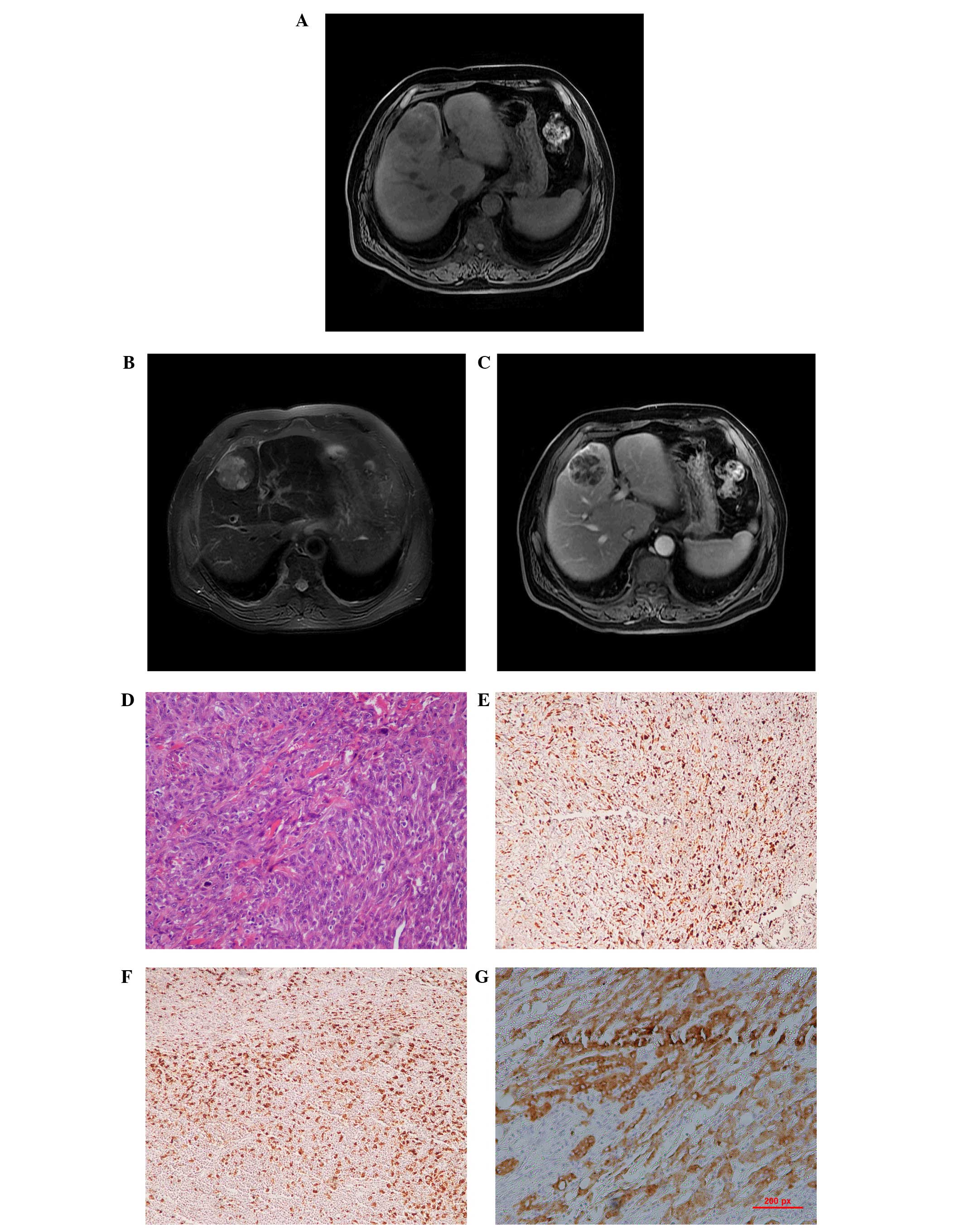
The first case with MFH in the current study
presented with a heterogeneous, low-attenuated lesion measuring
5.6×5.0×4.7 cm in the medial segment of the left lobe of the liver.
The tumor was well-delineated from the surrounding liver parenchyma
and the main signal intensity of the mass was hypointense compared
with the liver, providing a result similar to that of skeletal
muscle on T1WI. The main signal intensity of the mass on T2WI was
high compared with that in the liver, and necrotic areas with a
high signal intensity were found in the central tumor. The
enhancement was mild and heterogeneous (Fig. 1A–C).
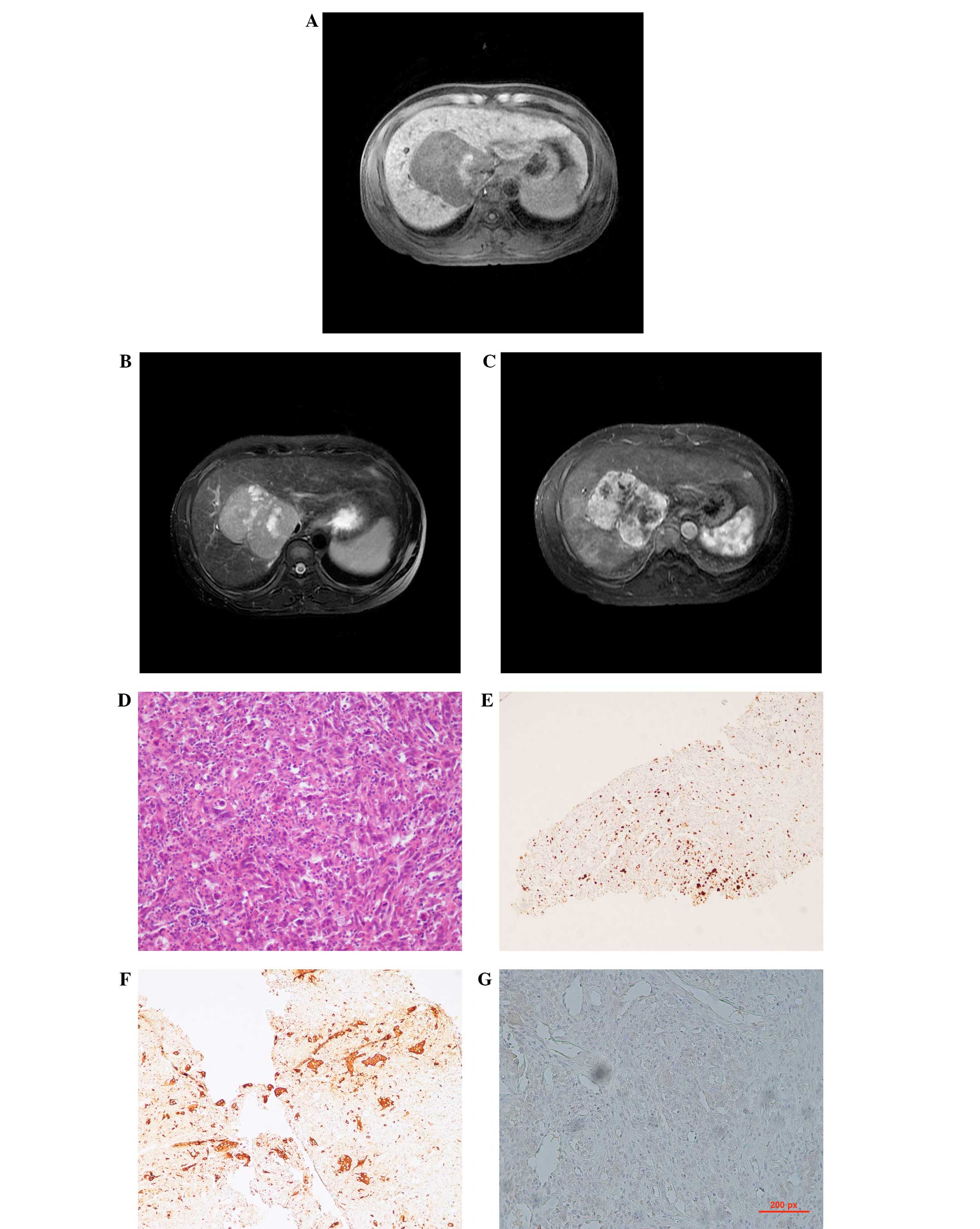
Case two presented with a 10.9×8.9×7.1-cm tumor in
the right lobe of the liver. This lesion had irregular geographical
margins, with a minor bulge into the hepatic capsule. The tumor
extended from the hepatic hilum to the liver bed and appeared to
involve the gallbladder. The main signal intensity of the mass was
hypointense on T1WI and was similar to the spleen. Multiple tiny
foci of high signal intensity were visible on the post-contrast
image, and marked enhancement and abundant blood vessels could be
found surrounding the tumor mass (Fig.
2A–C). Neither patient had any other systemic tumors.
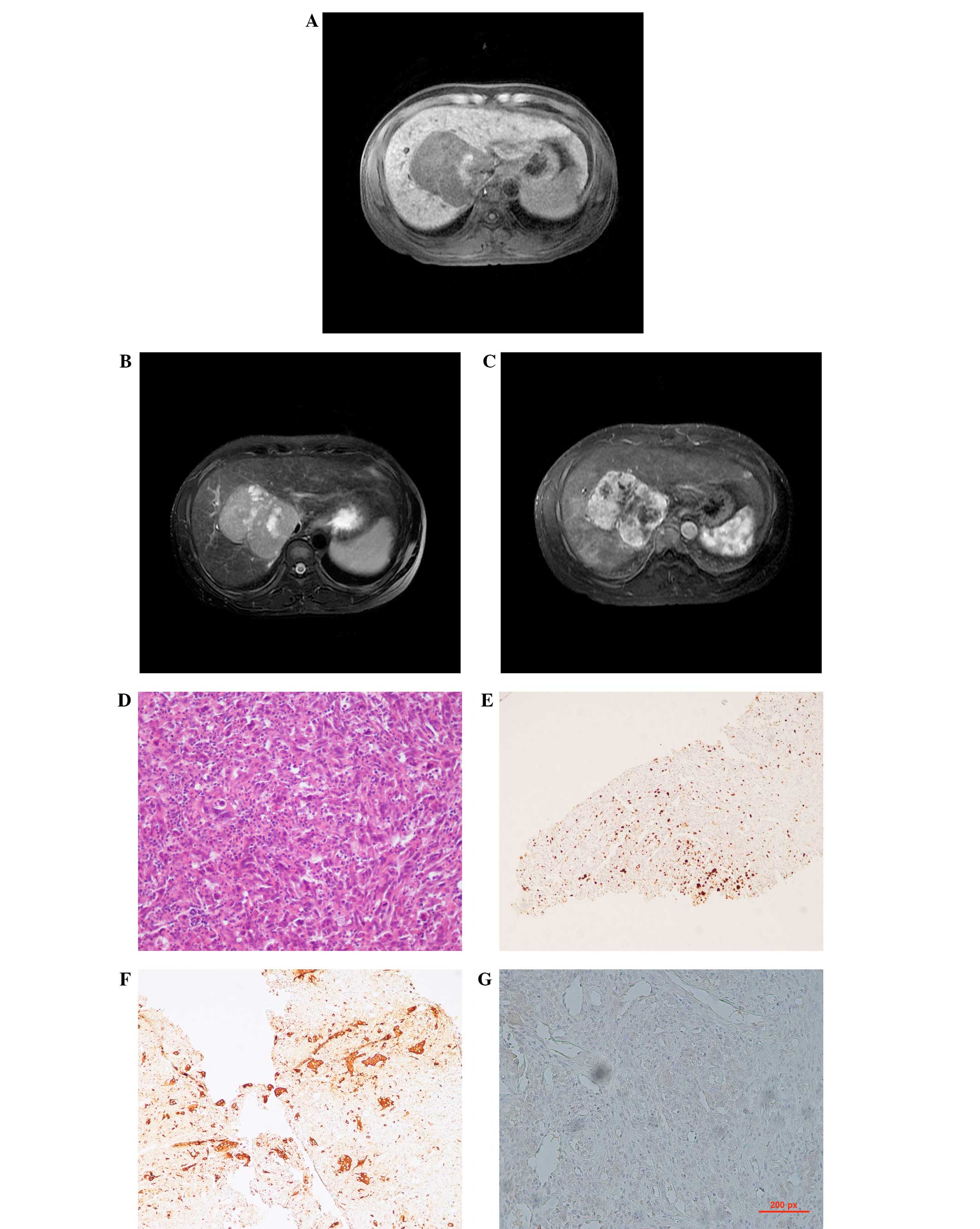 | Figure 2Case two: A 35-year-old male with
liver cirrhosis due to hepatitis B virus infection and a tumor of
the right lobe, confirmed to be a primary malignant fibrous
histiocytoma of the liver. (A) The lesion is inhomogeneous on
unenhanced T1WI and is mainly hypointense, with an irregular high
intensity area in the left section of the mass. (B) The lesion
possesses a well-defined margin and is inhomogeneously hyperintense
on T2-weighted spin-echo magnetic resonance imaging, with numerous
round- or oval-shaped patchy hyperintensity areas in the lesion.
The intrahepatic biliary ducts are dilated. (C) Following IV
administration of gadopenate dimeglumine, the heterogeneous
enhancement of the tumor, with central hypointense sections, is
clearly visible. (D) Hematoxylin and eosin staining of the
pathological specimen (×100 magnification) reveals the spindle to
consist of oval tumor cells arranged in a criss-cross fashion.
(E–G) Immunohistological staining for vimentin (×100
magnification), cluster of differentiation 68 (×100 magnification)
and for cytokeratin 8 (×100 magnification), respectively,
demonstrating a positive reaction in the tumor cells. WI, weighted
imaging. |
Pathological results were obtained by a
hepatolobectomy in the first case and by a needle biopsy in the
second case. Microscopically, the tumors of the two cases were
similar and demonstrated proliferation of atypical cells, including
spindle, pleomorphic and multi-nucleated giant cells arranged in
storiform, sheet and/or fascicle patterns, with scattered foci of
inflammatory cells, indicating the presence of MFH (Figs. 1D and 2D). Immunohistochemical examination
revealed the tumors to be positive for vimentin, cluster of
differentiation 68 and cytokeratin (CK)8 (Figs. 1E–G and 2E–G). Upon immunohistochemical staining of
tissue from case one, the tumor was found to be negative for CK8
and vascular endothelial growth factor expression. A negative
reaction for CK10 was revealed in the tissue from the second
patient.
The post-operative period was uneventful in case
one. However, the tumor of the second patient was unresectable and
the patient was then referred to the oncology service for
palliative chemotherapy (cisplatin, 75 mg/m2, d1–3 and
actinomycin D, 60 mg/m2, d1). Following three cycles of
chemotherapy the tumor increased in size. The patient then received
cyroablation treatment, however the patient succumbed to a bleeding
complication.
Discussion
Malignant fibrous histiocytoma (MFH), considered to
be a rarely occurring soft-tissue sarcoma of the liver in adults,
has previously been defined as a pleomorphic malignant spindle cell
neoplasm exhibiting fibroblastic and facultative histiocytic
differentiation. However, the pre-operative diagnosis of hepatic
MFH is made extremely challenging by the lack of clearly
characteristic features. In order to diagnose primary hepatic MFH,
two notable characteristics are necessary. The first involves the
histopathology of the hepatic tumor. The second is that the
clinicopathological criteria that define the tumor as hepatic in
origin must be met. Li et al (5) proposed novel criteria for primary
hepatic MFH in a review of seven cases. The criteria stated that
the MFH must be a solitary or multifocal liver neoplasm without
evidence of a pre-existing, co-existing or subsequently identified
primary lesion at any location in the body. The essential point in
establishing that the origin is hepatic is the exclusion of the
possibility that the tumor is due to metastasis or direct invasion
of MFH arising in other sites. Radiological imaging examinations
and intraoperative gross examination at the time of the initial
surgery revealed no additional tumors at any alternative site or
organ in the present patients.
The imaging features of the tumors in the two cases
were within the extent of the soft-tissue MFH classification. It
has been reported that MFH appears as a well-defined mass that
shows hypoechoic, mixed or hyperechoic patterns with variable
anechoic areas. The complex internal pattern of MFH depends on the
solid portion of high cellularity and the necrotic regions on the
ultrasonogram (1). The features of
hepatic MFH on unenhanced computed tomography vary and the scan may
reveal a poorly-separated or well-delineated, large or
multi-nodular mass, with a heterogeneous low attenuation density
and numerous areas of necrosis. It has been reported that smaller
tumors may prsent as a solid mass without prominent internal
necrosis (4). However, in the
present study, the smaller tumor exhibited an increased necrotic
area compared with the larger tumor. Following contrast injection,
the solid component demonstrated variable enhancement on delayed
post-contrast scans, dependent on the tumor vascularity and the
extent of the tumor necrosis.
MFH has been reported as inhomogeneously
hyperintense on T2WI and inhomogeneously enhanced on gadobenate
dimeglumine-enhanced T1-weighted gradient-recalled echo imaging
(6,7), which is similar to the present case
findings. In case two, cirrhosis was indicated by a diffuse nodular
hyperintense signal on T1WI and a low-intensity nodule surrounded
by high-intensity septa on T2WI. Hepatic MFH associated with
advanced liver cirrhosis is extremely rare. Hwang et al
reported a case of the simultaneous occurrence of MFH and
hepatocellular carcinoma in a patient with a cirrhotic liver
(8). Although the present study is
too small to contribute any definitive diagnostic features of
hepatic histiocytomas, the present cases exhibited variable and
non-specific morphological findings on MRI. However, signs
suggestive of malignancy were always present in the two patients,
including heterogeneous intensity, necrotic areas and heterogeneous
vascular enhancement.
MFH of the liver is generally recognized as having a
high local recurrence rate and a significant metastasis rate. The
risk of local recurrence and distant metastasis correlates with the
depth and size of the primary tumor. Recurrence of the tumor is not
uncommon, even when the resection margin is tumor-free (6). Distant metastases may spread via the
circulatory (30%) and lymphatic (12%) systems (9).
The size and location of the tumor and the efficacy
of the initial surgical removal all contribute markedly towards the
prognosis of a patient with soft-tissue MFH (10). The tumor size is considered to be a
clinically significant prognostic factor in hepatic MFH.
Additionally, the histopathological grade is considered to be
closely associated with the prognosis (11).
In conclusion, the present case study described two
cases of rare MFH in the liver, which tended to appear as
hepatocellular carcinoma. MRI of a primary liver MFH may reveal a
well-encapsulated, inhomogeneously enhancing mass. Although MFH is
a rare entity, the possibility of hepatic MFH should be
acknowledged during differential diagnosis, even in cirrhotic
patients, and hepatic spindle cell tumors require comprehensive
tissue sampling and immunohistochemical analyses in order to be
diagnosed.
References
|
1
|
Weiss SW and Enzinger FM: Malignant
fibrous histiocytoma: an analysis of 200 cases. Cancer.
41:2250–2266. 1978.
|
|
2
|
Liver Cancer Study Group of Japan. Primary
liver cancer in Japan. Clinicopathologic features and results of
surgical treatment. Ann Surg. 211:277–287. 1990.
|
|
3
|
Kearney MM, Soule EH and Ivins JC:
Malignant fibrous histiocytoma: a retrospective study of 167 cases.
Cancer. 45:167–178. 1980.
|
|
4
|
Yu JS, Kim KW, Kim CS, et al: Primary
malignant fibrous histiocytoma of the liver: imaging features of
five surgically confirmed cases. Abdom Imaging. 24:386–391.
1999.
|
|
5
|
Li YR, Akbari E, Tretiakova MS, et al:
Primary hepatic malignant fibrous histiocytoma: clinicopathologic
characteristics and prognostic value of ezrin expression. Am J Surg
Pathol. 32:1144–1158. 2008.
|
|
6
|
Lee YT: Leiomyosarcoma of the
gastro-intestinal tract: general pattern of metastasis and
recurrence. Cancer Treat Rev. 10:91–101. 1983.
|
|
7
|
Wunderbaldinger P, Schima W, Harisinghani
M and Saini S: Primary malignant fibrous histiocytoma of the liver:
CT and MR findings. AJR Am J Roentgenol. 171:900–901. 1998.
|
|
8
|
Hwang HS, Ha ND, Jeong YK, et al:
Simultaneous occurrence of malignant fibrous histiocytoma and
hepatocellular carcinoma in cirrhotic liver: A case report. World J
Hepatol. 27:256–261. 2011.
|
|
9
|
Atmatzidis KS, Pavlidis TE, Galanis IN, et
al: Malignant fibrous histiocytoma of the abdominal cavity: report
of a case. Surg Today. 33:794–796. 2003.
|
|
10
|
Rydholm A and Syk I: Malignant fibrous
histiocytoma of soft tissue. Correlation between clinical variables
and histologic malignancy grade. Cancer. 57:2323–2324. 1986.
|
|
11
|
Ding GH, Wu MC, Yang JH, et al: Primary
hepatic malignant fibrous histiocytoma mimicking
cystadenocarcinoma: a case report. Hepatobiliary Pancreat Dis Int.
5:620–623. 2006.
|