Introduction
Osteoid osteoma is a type of benign bone-forming
tumor, which is characterized as a well-demarcated osteoblastic
mass, called a nidus, surrounded by a distinct zone of reactive
bone sclerosis; these tumors have limited growth potential and
exhibit disproportionate pain (1). In
the majority of osteoid osteoma cases, typical radiographic
features demonstrate a sclerotic cortical lesion and contain a
small lucency that represents a nidus (2,3). However,
contrary to the expected presentation of osteoid osteoma, different
radiographic findings may be encountered that provide a diagnostic
dilemma for the physicians concerned. Prior to the introduction of
magnetic resonance imaging (MRI), diagnoses were made using plain
radiograph images, bone scans and computed tomography (CT) scans
(2–4).
However, MRI evaluation is now commonly preferred, particularly
when the lesions are located close to a joint or spinal area, and
may not be easily detected on plain radiographs. However, it was
suggested that there may be a high possibility of false positive
results in the diagnosis of osteoid osteoma using MRI (5); therefore, delayed diagnosis of osteoid
osteoma is a common issue. The present study aimed to investigate
the potential role of radionuclide imaging for the diagnosis of
osteoid osteoma, as radionuclide imaging has been reported to be a
more sensitive diagnostic modality in osteoid osteoma.
Patients and methods
In the present study, 18 patients with surgically
and histologically proven osteoid osteoma were retrospectively
enrolled and reviewed at Korea University Anam Hospital (Seoul,
Korea) between January 2006 and December 2013. The study was
approved by the ethics committee of Korea University Anam Hospital.
The ratio of males to females was 10:8 and mean patient age was
18.2 years (range, 4–50 years). The characteristics of the 18 cases
of osteoid osteoma were analyzed based on diagnostic imaging and
the time from initial recognition of symptoms by the patient to
diagnosis. Diagnostic modalities included plain radiograph imaging,
CT, MRI and radionuclide imaging.
Case report
Two cases of osteoid osteoma are presented. In these
patients, plain radiographs and MRI were unable to provide
sufficient findings for diagnosis of osteoid osteoma. However,
radionuclide imaging and CT revealed the characteristics of osteoid
osteoma.
Case I
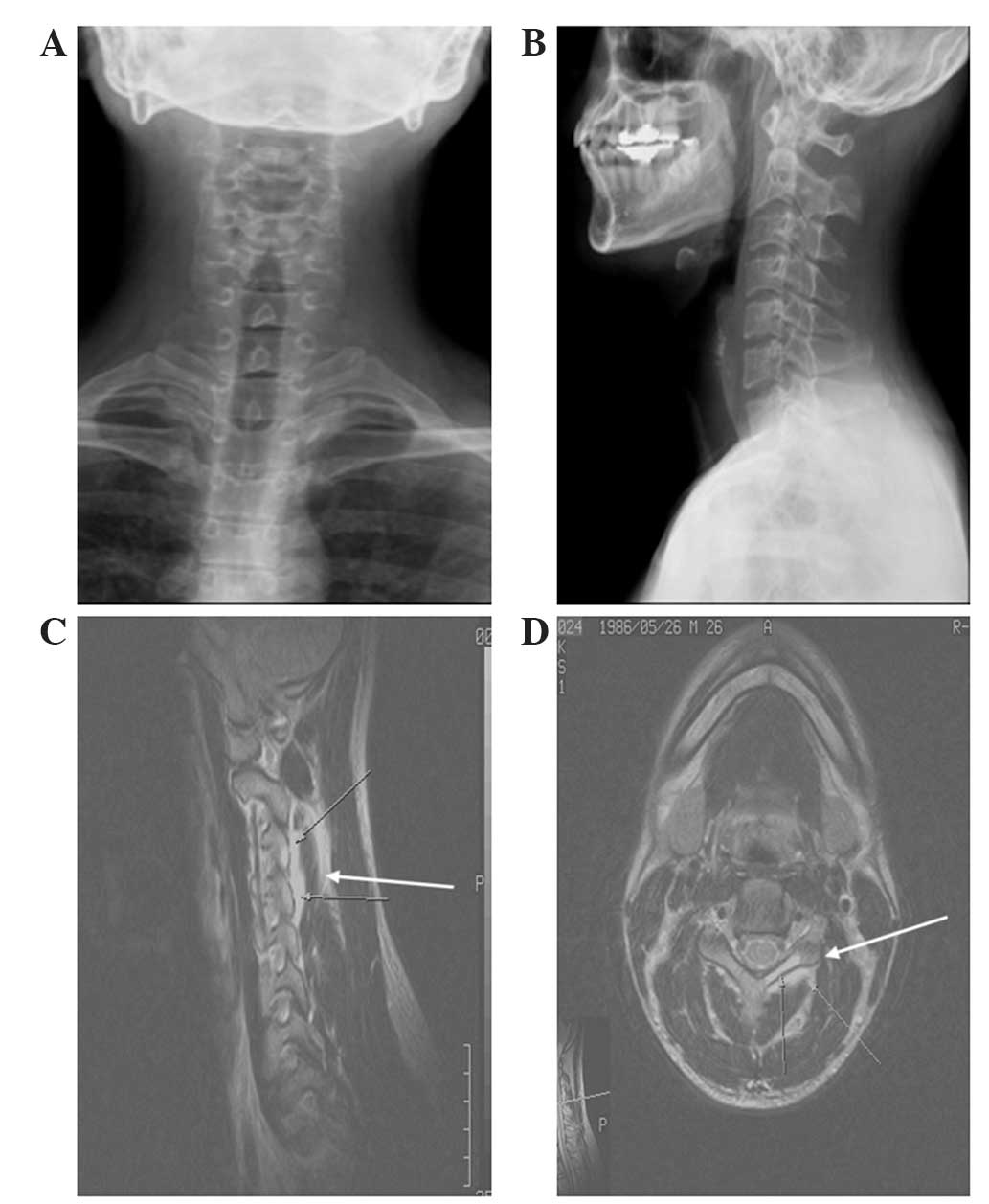
A 26-year-old male presented with severe upper neck
pain that had been ongoing for one year. The patient had previously
been treated using non-steroidal anti-inflammatory drugs (Naproxen;
200 mg, twice daily), analgesic drugs and physiotherapy in another
hospital. However, his symptom had not been relieved and so an MRI
study was recommended by the patient's physician, the results of
which revealed a non-specific inflammatory lesion on the left third
cervical spine (C3) (Fig. 1). The
laboratory findings of the patient's blood chemistry revealed an
elevated erythrocyte sedimentation rate and supported the MRI
results. When the patient was admitted to Korea University Anam
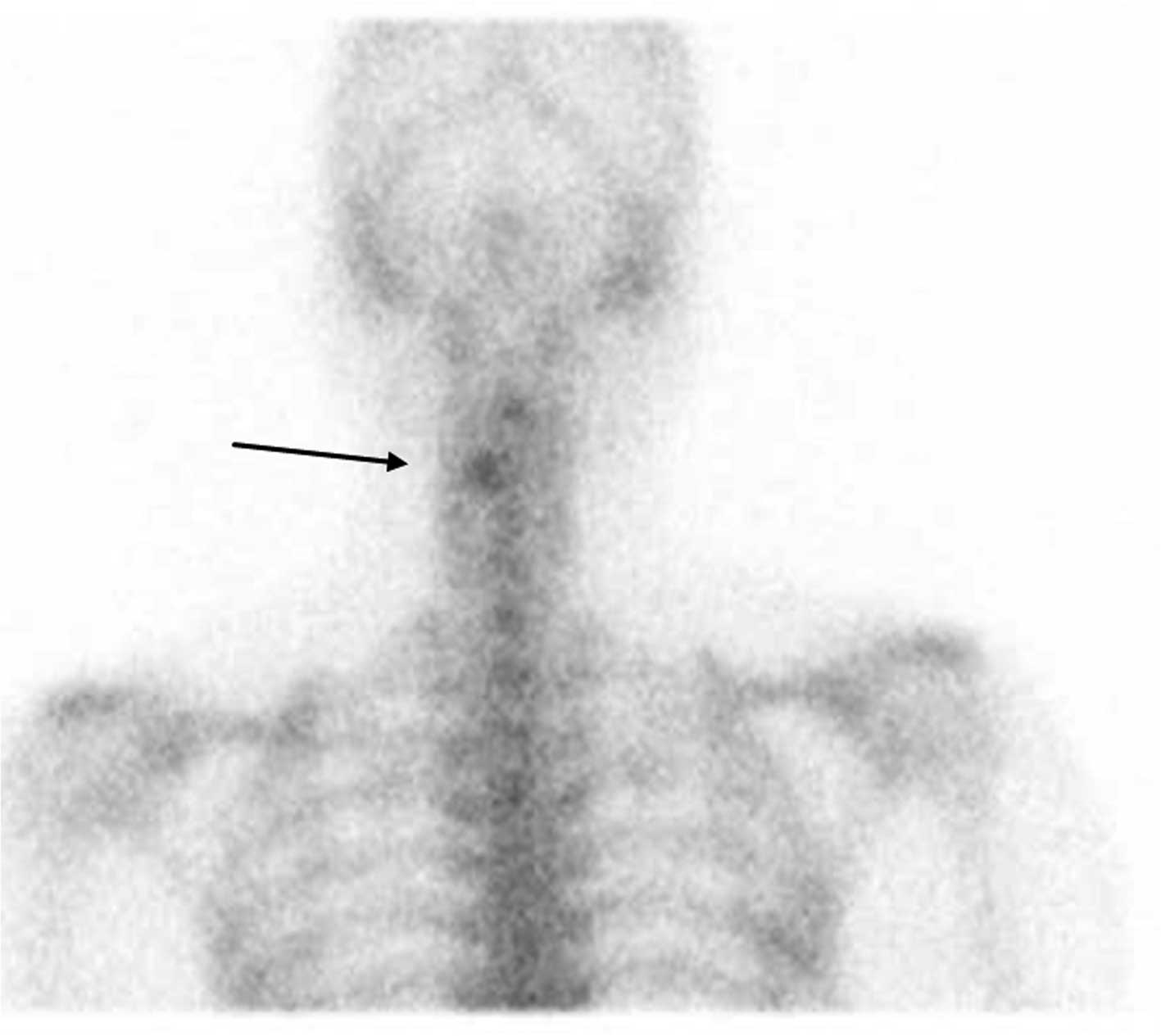
Hospital, a bone scintigraphy was performed using
99mTc-methylene diphosphonate (MDP) and the bone scan
image revealed increased focal uptake in the cervical spine
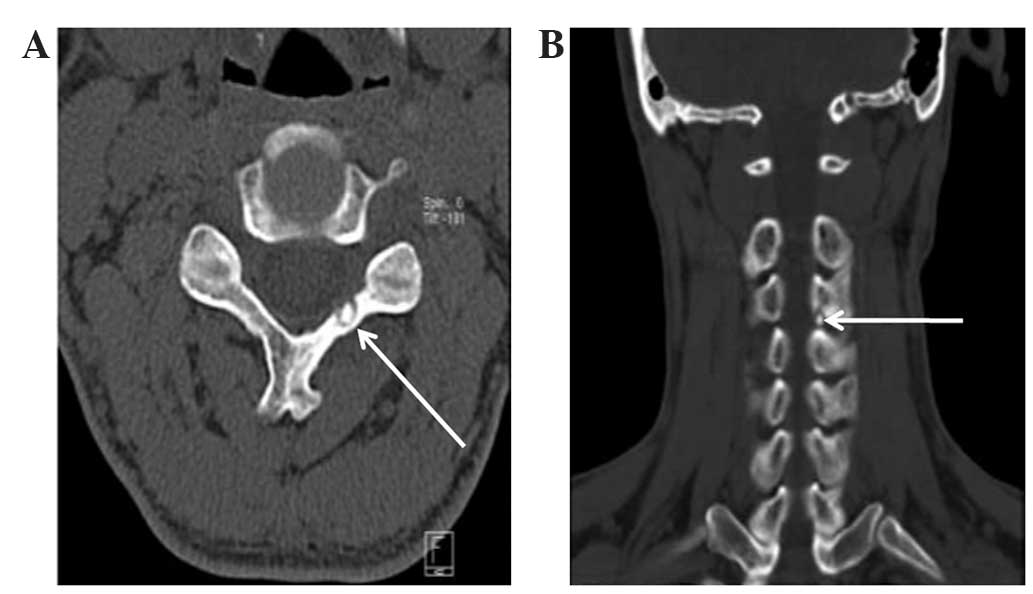
(Fig. 2). Therefore, a CT scan was
performed (Fig. 3) and a diagnosis of
an osteoid osteoma in the left C3 lamina was confirmed. The
duration from first onset of symptoms to diagnosis of osteoid
osteoma was 18 months.
Case II
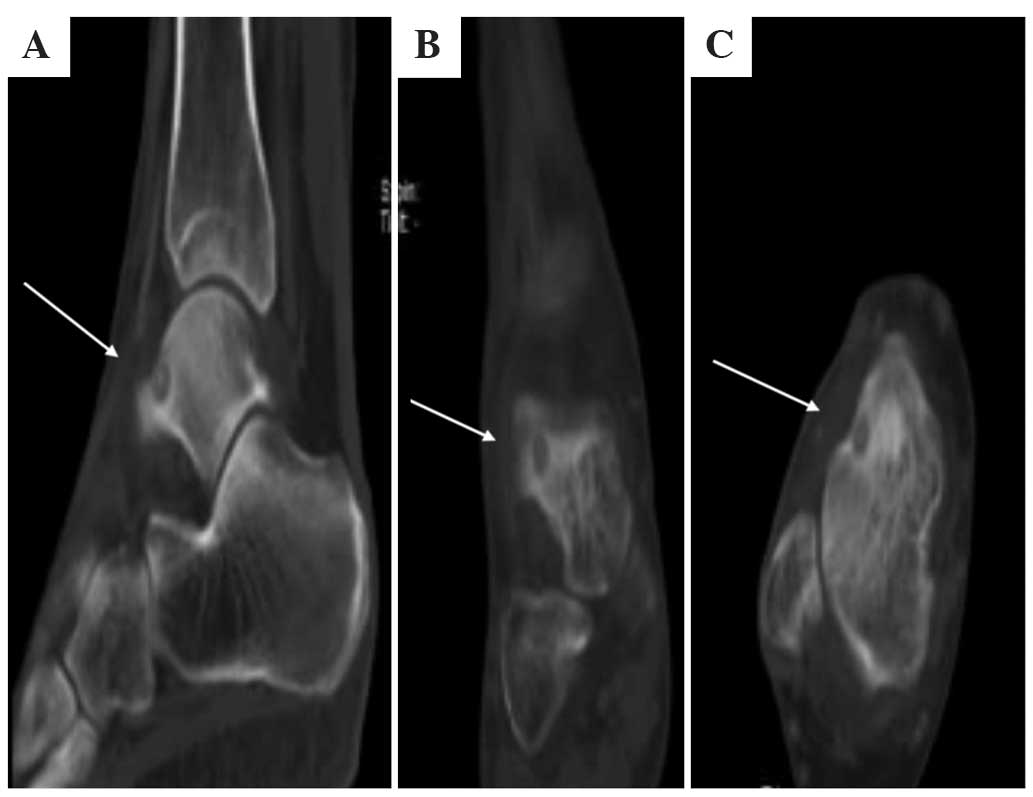
A 46-year-old female presented with right ankle
pain, which worsened at night. The patient's symptoms had lasted
for one year and were treated as an ankle sprain at another
hospital based on the results of plain radiographs, which revealed
no specific bony abnormalities (Fig. 4A
and B). The patient then underwent an MRI examination at
another hospital and was diagnosed with a tumorous lesion on the
talus, with inflammatory changes (Fig. 4C
and D). The patient was recommended to visit a specialist
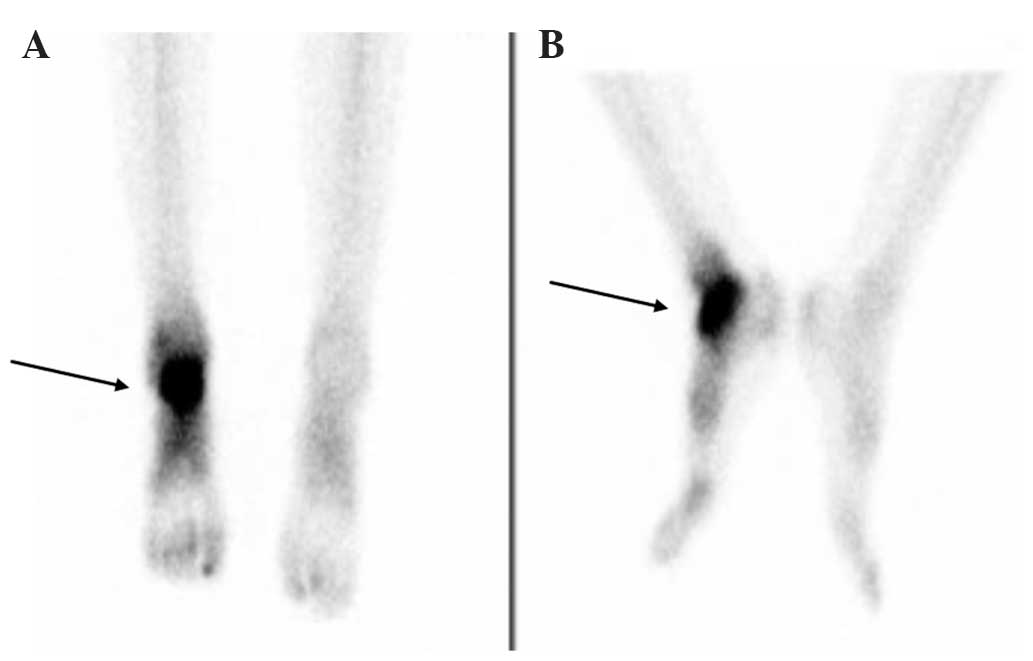
institute for bone tumors. The patient was admitted to Korea
University Anam Hospital, where bone scintigraphy (Fig. 5) and CT (Fig. 6) scans were performed. These scans
confirmed the diagnosis of an osteoid osteoma. The duration from
first onset of symptoms to diagnosis of osteoid osteoma was 20
months.
Results
A total of 18 cases of osteoid osteoma were
retrospectively reviewed in the present study. Among these 18
patients, 14 patients exhibited unique positive findings suggestive
of osteoid osteoma on plain radiographs, with a mean time between
initial recognition of symptoms by the patient and diagnosis of 5.2
months (range, 3.8–9.3 months). Of these patients, 5 cases were
identified in the femur, 5 cases were located in the tibia, 2 cases
were in the humerus and the remaining cases were in the calcaneus
and T12 spine. All of these 14 cases underwent MRI and CT scans.
However, 2 patients did not undergo radionuclide imaging as it was
not required. Out of the total 18 patients, 4 patients exhibited no
radiographic abnormalities in the initial plain radiographs: 2
cases were located in the spine (1 cervical and 1 lumbar), another
in the talus and another in the capitate. These 4 patients were
diagnosed a mean of 18.5 months (range, 17–20 months) following the
onset of symptoms. In addition, radionuclide imaging or CT scans
were not performed on these patients during the early stage of
symptoms; initially, they were treated as an ankle sprain, back and
neck sprains and a wrist sprain in each case. Following long term
medical treatment and physiotherapy, these patients underwent an
MRI study, following which 4 cases were diagnosed as an
inflammatory disease and required further CT and bone scans.
Radionuclide imaging was later performed in these cases and the
results were strongly positive for osteoid osteoma. Overall,
radionuclide imaging was performed on 16 patients and all of the
cases were positively identified as osteoid osteoma.
Discussion
Osteoid osteoma is a type of benign bone-forming
tumor, which accounts for 10–12% of all benign bone tumors
(6). Osteoid osteoma is characterized
by a well-demarcated osteoblastic mass, called a nidus, surrounded
by a distinct zone of reactive bone sclerosis (7). It was reported that >50% of osteoid
osteomas occur in the long bones of the lower extremities; in
addition, they are often present in the small bones of the hand and
feet. However, these tumors rarely occur on the axial skeleton
(8). Osteoid osteoma has unique and
quite often diagnostic symptoms; the typical clinical symptom is
long term pain of increasing severity (9). This pain is often referred to the
nearest joint when the tumor is located in the proximity of a
joint, which physicians may confuse with arthritic pain (10). The well-known radiographic features of
osteoid osteoma are characteristic and diagnostic (7); however, due to localized bone and joint
pain without significant abnormality on plain radiographs, patients
may be initially referred to a rheumatologist for evaluation. In
this situation, the diagnosis is not readily apparent and
inflammatory arthritis, degenerative arthritis, gouty arthritis and
even septic arthritis may be considered as the diagnosis rather
than osteoid osteoma (11).
The typical radiographic and clinical features of
osteoid osteoma are not always distinguishable. Intracortical
lesions of long bones produce extensive fusiform thickening of the
cortex with dense radiopacity, which may obscure the nidus of
osteoid osteoma (12). In cases of
osteoid osteoma in small bones and the spine, the nidus may not be
visible on plain radiographs; therefore, additional imaging
studies, including CT, MRI and radionuclide imaging, may be
required for the confirmation of diagnosis (13). In general, physicians may prefer to
use MRI rather than CT scans, as MRI exaggerates the inflammatory
changes around osteoid osteomas (14). However, according to the way images
are captured during testing, small surroundings of the nidus may be
excluded from examined area, resulting in a misdiagnosis. The
present study reported examples of cases of the talus and cervical
spine, which demonstrated how misdiagnosis resulted from the
exaggerative tendency of MRI. In Case I, a 26-year-old male
suffered from severe neck pain ongoing for one year. An MRI of the
cervical spine revealed edematous signal change in the left C3
lamina, which was diagnosed as a non-specific inflammatory lesion
in C3 lamina and the patient was treated using anti-inflammatory
agents. However, when the patient was admitted to Korea University
Anam Hospital, bone scintigraphy using 99mTc-MDP was
performed, which revealed small increased focal uptake on the C3
lamina; therefore, an accurate diagnosis was confirmed using CT.
According to Swee et al (4),
plain radiograph images and clinical history were sufficient for
the accurate diagnosis of osteoid osteoma in 75% of cases. In such
circumstances, no further work-up is necessary, though CT scans may
assist the localization of the tumors nidus. It was therefore
advised that if the plain radiograph was equivocal, tomography
should be directed to the area in question, whereas if the plain
radiograph was normal with high index of suspicion, radionuclide
imaging should be performed (4).
However, at the time of the study by Swee et al, MRI was not
popular as a diagnostic modality and so only plain x-ray,
tomography and radionuclide imaging were considered as diagnostic
modalities. Following the introduction of MRI as a diagnostic tool,
physicians may tend to consider MRI as the first choice technique,
rather than CT, in cases of ambiguous pain patients (15). However, CT is an effective modality
for the diagnosis of osteoid osteoma; although if the plain
radiograph is normal, a selection of CT scans as a first choice of
radiologic examination is not often obvious.
In conclusion, the results of the present study
demonstrated that 28.6% of osteoid osteoma cases with clinical
indications revealed no abnormal findings in plain radiographs.
However, all radionuclide imaging results in the present study
accurately identified positive cases of osteoid osteoma. Therefore,
in such situations where plain radiographs are not conclusive,
radionuclide imaging may provide a useful tool for diagnosis. In
addition, these results suggested that if the radionuclide imaging
is positive, CT scans may be more valuable for diagnosis of osteoid
osteoma compared with MRI; however, if the radionuclide imaging is
negative, MRI should be recommended for the diagnosis of other
undiscovered disease entities.
References
|
1
|
Klein MJ, Parisien MV and Schneider-Stock
R: Osteoid osteomaWorld Health Organization Classification of
Tumours, International Agency for Research on Cancer (IARC),
Pathology and Genetics of Tumours of Soft Tissue and Bone. Fletcher
CDM, Unni KK and Mertens F: IARC Press; Lyon: pp. 260–261. 2002
|
|
2
|
Schajowicz F and Lemos C: Osteoid osteoma
and osteoblastoma. Closely related entities of osteoblastic
derivation. Acta Orthop Scand. 41:272–291. 1970. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sim FH, Dahlin CD and Beabout JW:
Osteoid-osteoma: Diagnostic problems. J Bone Joint Surg Am.
57:154–159. 1975.PubMed/NCBI
|
|
4
|
Swee RG, McLeod RA and Beabout JW: Osteoid
osteoma. Detection, diagnosis and localization. Radiology.
130:117–123. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hosalkar HS, Garg S, Moroz L, Pollack A
and Dormans JP: The diagnostic accuracy of MRI versus CT imaging
for osteoid osteoma in children. Clin Orthop Relat Res.
433:171–177. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kransdorf MJ, Stull MA, Gilkey FW and
Moser RP Jr: Osteoid osteoma. Radiographics. 11:671–696. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Greenspan A: Benign bone-forming lesions:
Osteoma, osteoid osteoma and osteoblastoma. Clinical, imaging,
pathologic and differential considerations. Skeletal Radiol.
22:485–500. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sabanas AO, Bickel WH and Moe JH: Natural
history of osteoid osteoma of the spine; review of the literature
and report of three cases. Am J Surg. 91:880–889. 1956. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ebrahimzadeh MH, Ahmadzadeh-Chabock H and
Ebrahimzadeh AR: Osteoid osteoma: A diagnosis for radicular pain of
extremities. Orthopedics. 32:8212009.PubMed/NCBI
|
|
10
|
Georgoulis AD, Papageorgiou CD, Moebius
UG, Rossis J, Papadnikolakis A and Soucacos PN: The diagnostic
dilemma created by osteoid osteoma that presents as knee pain.
Arthroscopy. 18:32–37. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Greenspan A, Jundt G and Remagen W: Bone
forming (osteogenic) lesionsDifferential Diagnosis in Orthopaedic
Oncology. 2nd. Lippincott Williams & Wilkins; Philadelphia, PA:
pp. 40–157. 2006
|
|
12
|
Chai JW, Hong SH, Choi JY, Koh YH, Lee JW,
Choi JA and Kang HS: Radiologic diagnosis of osteoid osteoma: From
simple to challenging findings. Radiographics. 30:737–749. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Helms CA, Hattner RS and Vogler JB III:
Osteoid osteoma: Radionuclide diagnosis. Radiology. 151:779–784.
1984. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Davies M, Cassar-Pullicino VN, Davies AM,
et al: The diagnostic accuracy of MR imaging in osteoid osteoma.
Skeletal Radiol. 31:559–569. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Emery DJ, Shojania KG, Forster AJ,
Mojaverian N and Feasby TE: Overuse of magnetic resonance imaging.
JAMA Intern Med. 13:823–825. 2013. View Article : Google Scholar
|