Introduction
Cancer of larynx was the second most common cancer
in head and neck following oral cavity cancer, as well as the
second most frequently cancer occurred in respiratory tract except
lung cancer. According to GLOBOCAN 2012, there were an estimate of
156,877 new cases and 83,376 deaths in the world, and the adjusted
incidence and mortality rates were 2.1/100,000 and 1.1/100,000,
respectively (1). For patients with
laryngeal cancer, surgical treatment provides the best therapeutic
effects. Even with a partial laryngectomy, patients may recover at
least a certain degree of laryngeal function, and return to society
and enjoy life almost immediately after treatment. Direct
laryngoscopy must be performed prior to the aryepiglottoplasty to
decide what amount of tissue to resect. Endoscopic
aryepiglottoplasty with use of microlaryngeal instruments is an
effective and safe method of the treatment of severe form of
laryngomalacia. It is better to perform this procedure in general
anesthesia without intubation (2)
Concurrent chemoradiotherapy has been applied to
treat patients with stage III and IV oropharyngeal, hypopharyngeal
or laryngeal cancer. Notably, based on clinical outcomes, certain
chemotherapy and radiotherapy practitioners have even suggested
that concurrent chemoradiotherapy may replace surgery to treat
laryngeal cancer (3). This is
contrary to the viewpoint of the majority of otolaryngologists, as
sole treatment by chemoradiology has not provided superior clinical
outcomes to laryngeal cancer patients in the past decades (4,5).
The arytenoids, aryepiglottic folds and epiglottis
work together to close the laryngeal inlet during swallowing, so as
to prevent aspiration (6). Following
the resection of arytenoid cartilage, the glottis cannot close
completely without proper reconstruction. Head and neck surgeons
should carefully consider the preservation of laryngeal function,
particularly in patients with late-stage laryngeal cancer. In the
present study, a novel reconstruction technique for arytenoid
region defects is investigated, which not only avoid the
complications of aspiration and laryngeal stenosis, but also
preserves sound quality post-recovery.
Materials and methods
Patients
A total of 26 laryngeal cancer patients, 25 males
and 1 female, from the Beijing Shijitan Hospital (Capital Medical
University, Beijing, China) were included in the present study. The
age of the cohort ranged between 44 and 78 years old, with a median
age of 61 years old. All cases were diagnosed as glottic carcinoma,
with 9 cases staged as T3N1aM0, 4 cases as T3N2bM0, 7 cases as
T3N0M0 and 3 cases as T2N0M0. Additionally, 3 cases encountered
recurrent diseases following initial treatment in other hospitals.
Pre-operative laryngeal endoscopy showed vocal cord fixation in 23
cases, including 3 cases of arytenoid area recurrence after initial
therapy, and impaired vocal cord movement in another 3 cases. The
vocal cartilage or arytenoid area was involved in all cases, with
anterior commissure involvement in 15 patients and tumors
approaching the posterior commissure in 3 patients. None of the
patients exhibited contralateral vocal cord involvement. : The
study was approved by the ethics committee of Capital Medical
University (Beijing, China).
Treatment
While 3 patients with tumors approaching the
posterior commissure were treated with 50 Gy pre-operative
radiation followed by surgery in 2–3 weeks, the remaining 23
patients were managed by extended vertical partial laryngectomy
without radiation or chemotherapy.
Surgical procedure
The surgical procedure consisted of the following:
i) Intubation and general anesthesia were performed following
conventional tracheotomy. ii) The surgical incision was designed
according to the tumor (T) and node (N) classification, and skin
striae. The flap was lifted to expose the surgical area. Selective
neck dissections of ipsilateral level II, III and IV sections were
performed for N-positive patients and ipsilateral I and III neck
dissections were performed for N0 patients. The ipsilateral
superior thyroid artery and vein, and the superior laryngeal artery
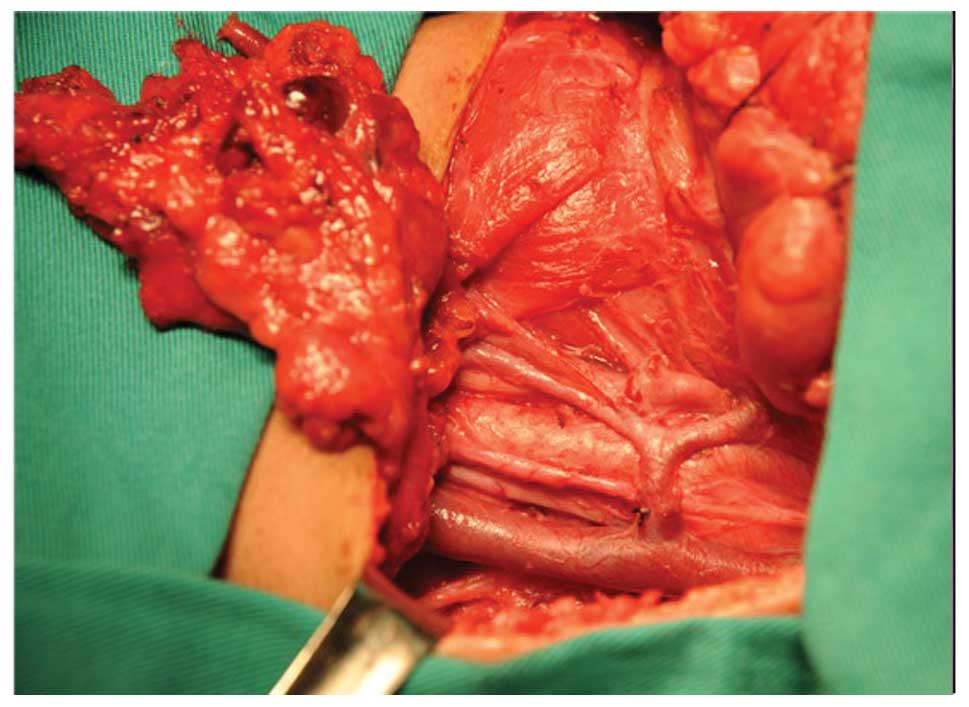
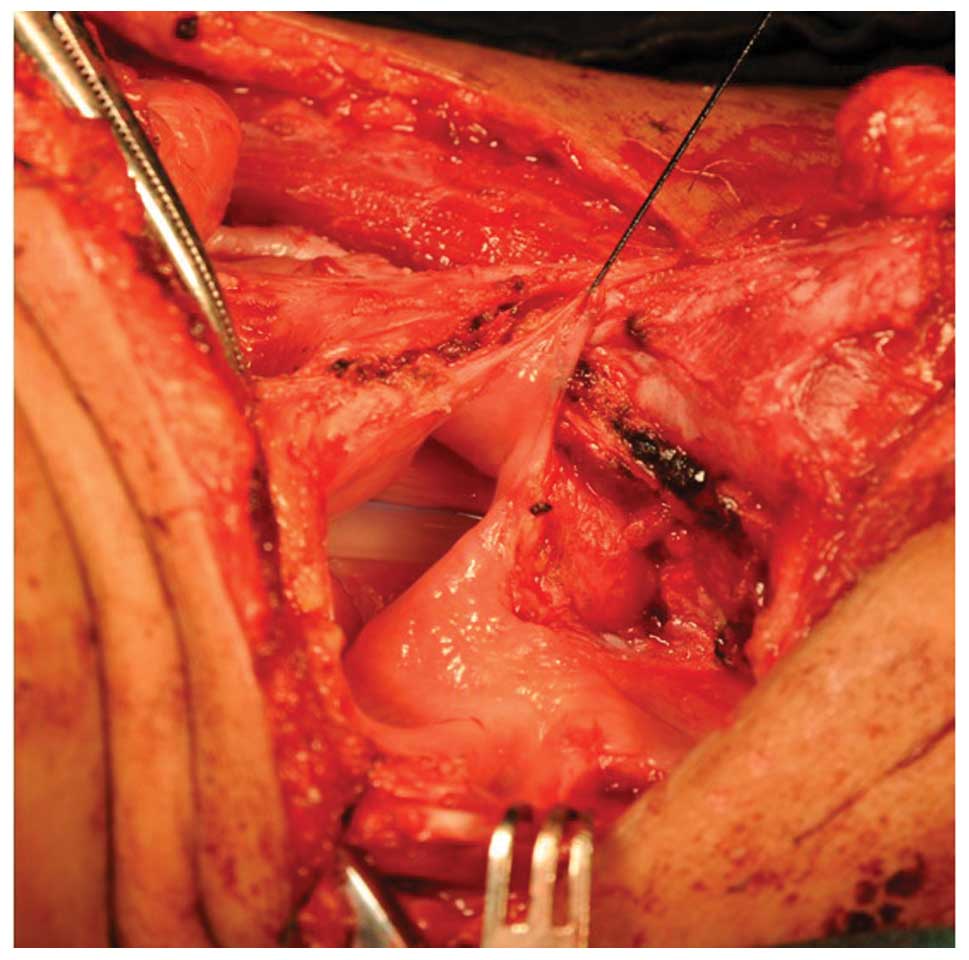
and its branches into strap muscles were preserved (Fig. 1). iii) The ipsilateral arytenoid
cartilage, vocal cords, laryngeal ventricle, ventricular fold and
anterior two-thirds of the thyroid cartilage were resected
(Fig. 2). If the anterior commissure
was involved, the anterior regions of the contralateral vocal cord
and ventricular fold were removed. Surgical margins were confirmed
upon frozen sections. iv) The lingual artery and hypoglossal nerve
were then secured. The supra-hyoid muscle group was cut off and a
section of the hyoid bone was intercepted as the graft. The bone
graft was flipped anteriorly downwards with the strap muscles to
the laryngeal space. The fascia of the strap muscles, the external
perichondrium of the thyroid cartilage and the thyrohyoid membrane
were all preserved. v) The bone graft was then tailored by
measuring the defect and thinned to meet the thickness of the
thyroid cartilage. If the cartilage of the anterior commissure was
resected, the bone graft was carved into an inverted V shape so
that the anteroposterior diameter of the glottis could be restored.
vi) The posterolateral end of the bone graft was placed at the
defective site of the arytenoid cartilage and sutured to the
adjacent soft tissue. It was ensured that the inside edge of the
bone graft did not exceed the midline and that the muscle pedicle
did not exceed the inside edge of the bone graft. The posterior end
of the bone graft was covered by hypopharyngeal mucosa and sutured
with the posterior commissure. vii) Next, the anterior end of the
bone graft was fixed to the edge of the contralateral thyroid
cartilage, ensuring the correct alignment of membrane to membrane
and bone to cartilage, and confirming that the end of the bone
graft was not exposed. viii) The pharynx was then closed, a
drainage tube was placed and the incision was closed.
Post-operative treatment
Conventional tracheotomy and continuous wound
drainage were performed. Drainage tubes were removed once the
drainage fluid level reached <15 ml over 24 h. Nasogastric
feeding was applied on the first post-operative day. Patients were
provided with oral intake on the seventh post-operative day and
nasal feeding tubes were removed if no evident aspiration was
observed. The tracheotomy tubes were plugged if no dyspnea was
observed. Endoscopic evaluations were then applied after one month.
If no granulation was found, the tracheal tubes were then removed.
If granulation was present, this was removed by a second surgery
and the patients were kept under observation for an additional
month. All patients were periodically reviewed by laryngeal
endoscopy, ultrasound of the neck and computed tomography of the
throat and chest.
Results
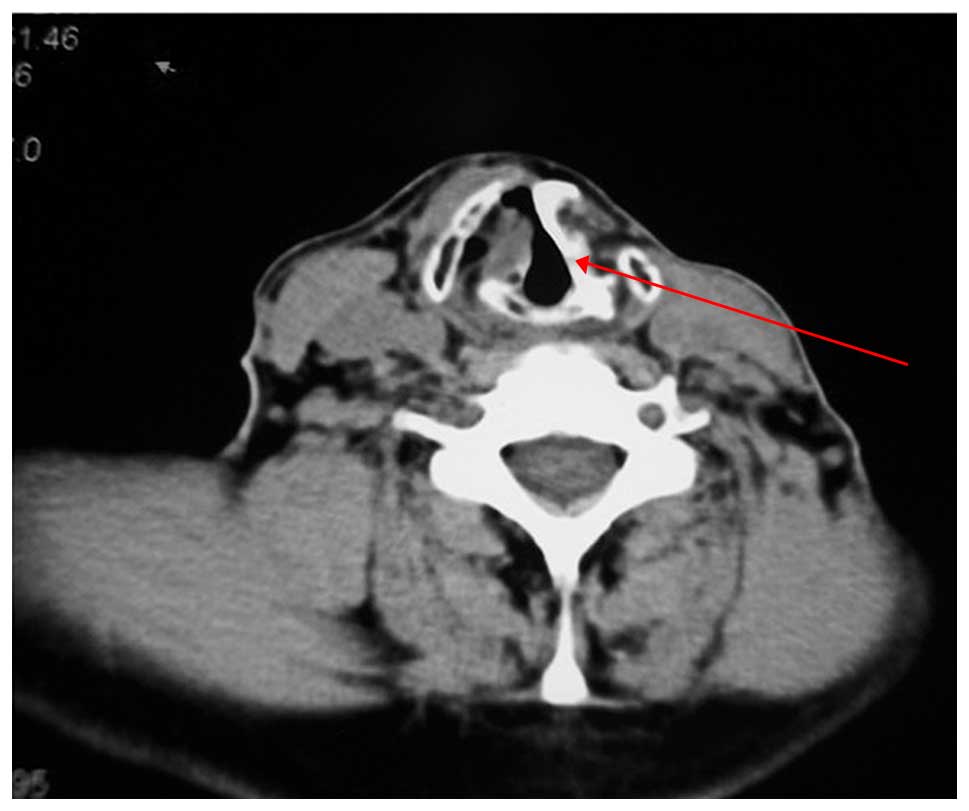
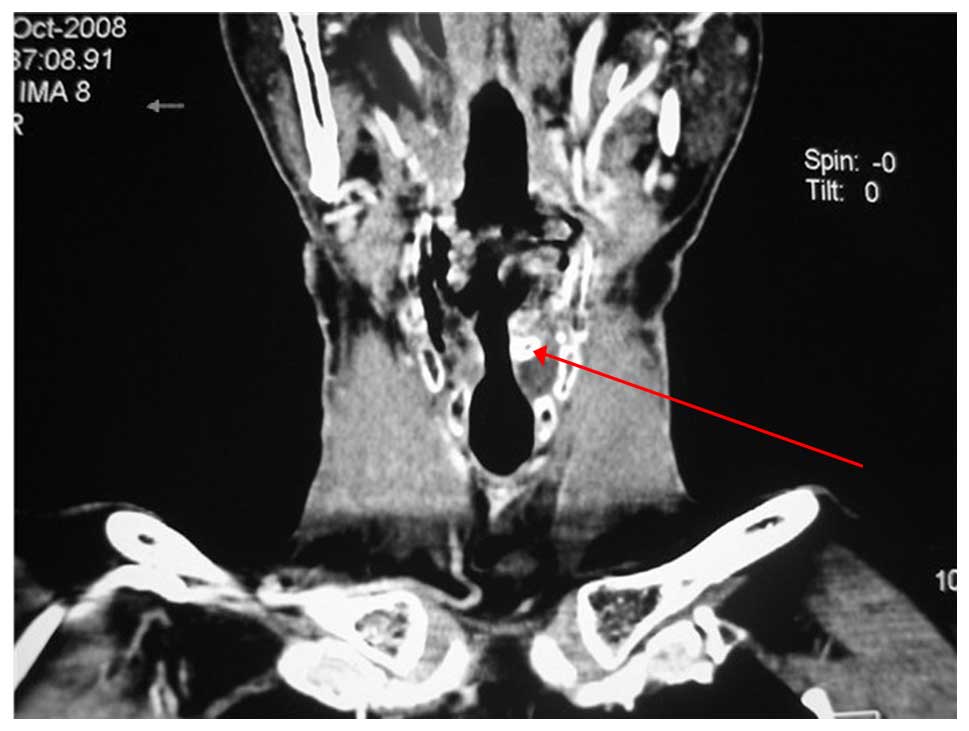
Pathological examination showed invasion of the
thyroid cartilage perichondrium in 12 cases and lymph nodes
metastases in 11 cases. Negative surgical margins were achieved in
all cases. Nasal feeding tubes were removed from 19 patients within
10 days post-surgery and in 6 patients within 3 weeks. A pharyngeal
fistula was recorded in one patient; recovery from this
complication was observed following 3 weeks of conservative
treatment, consisting of drainage and cleaning the fistula. The
extubation rate of the tracheostomy tube was 100%. In total, 18
patients were extubated within 1 month post-surgery and 6 patients
within 2 months. In addition, 2 patients underwent secondary
surgical procedures to remove granulation tissue of the anterior
commissure, and were then observed for 1 month to confirm no
granulation prior to extubation. No aspiration pneumonia or throat
adhesions were observed. The glottides of all patients were almost
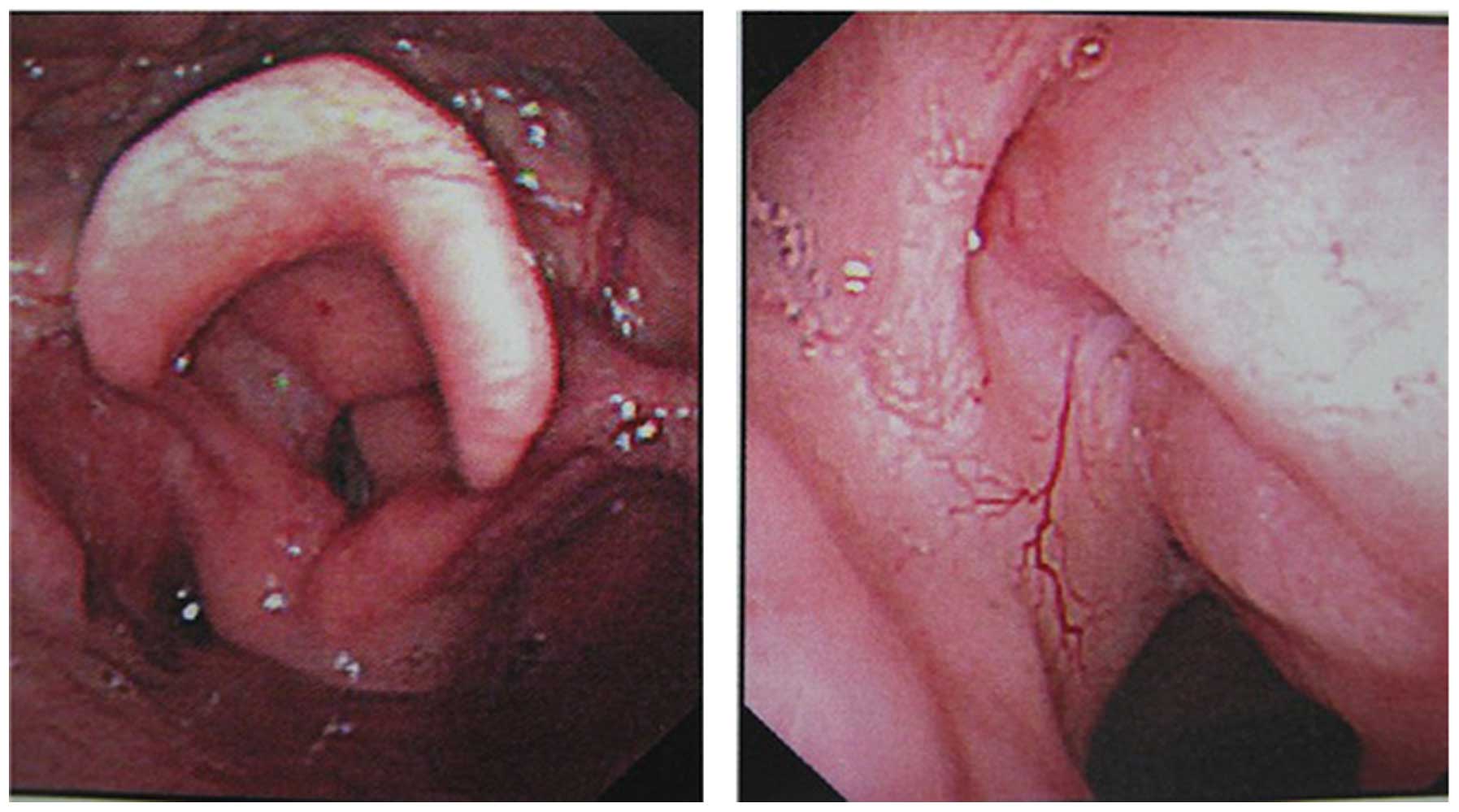
symmetrical (Figs. 3 and 4), and were able to open fully and close
well (Fig. 5). Follow-up visits were
scheduled after 2–7 years. One patient developed local recurrence,
ipsilateral regional recurrence, contralateral regional recurrence
and lung metastasis, respectively. The 3-year disease-free survival
rate was 100% (20/20) and the 5-year disease-free survival rate was
79% (11/14).
Discussion
The complications of partial laryngectomy include
laryngeal stenosis, aspiration and poor pronunciation (7,8). The
removal of arytenoid cartilage increases the incidence and grade of
complications. Serious aspiration not only affects the patient's
quality of life, but also increases the risk of patient mortality.
Patients with serious aspiration often require surgical repair of
the non-functioning glottis, with certain patients being required
to undergo a total laryngectomy. Therefore, the repair of the
laryngeal defect following the removal of the arytenoid cartilage
and the minimization of post-operative aspiration is a focus of
attention. Although a high decannulation rate may be obtained
without repair, a severe hoarseness would result from this. Thus,
it has been suggested that no reconstruction of arytenoid area
defects should be conducted at all (9). Single or double pedicle sternohyoid
muscle flaps are therefore a good option for surgery (10). Clinicians have previously successfully
restored the arytenoid defect with pedicle hyoid bone and improved
the reconstruction quality, with a post-operative extubation rate
of up to 87.9% (11). Notably, the
grafted muscle tissues in the glottic area have a different degree
of atrophy after reconstruction, and severe atrophy of the muscle
could lead to marked hoarseness, while inadequate atrophy may
affect extubation. It is therefore more difficult to determine the
ideal thickness of the muscle flap. Moreover, the preserved
contralateral thyroid cartilage will be displaced
anterioposteriorly following the loss of support from the other
half, thus shortening the anteroposterior diameter of the glottis.
The supracricoid subtotal laryngectomy has simple steps and a high
extubation rate, but provides poor sound quality (12,13).
Extensive rehabilitation following surgery is also commonly
required in supracricoid subtotal laryngectomy patients.
The use of a hyoid flap repairs defects in the
glottis and arytenoid areas, and restores the laryngeal frame and
anteroposterior diameter. The technique also has additional
advantages, including reducing aspiration, as the thickness of
hyoid is suitable for defects of the arytenoid area and the
structure of hypopharynx can be restored, epiglottis functionally
preserved, and pharynx and larynx successfully separated during
swallowing. If there is huge defect of the cricoid, it can be
compensated for by a corresponding increase in the amount of muscle
attached to the hyoid. Therefore, post-operative aspiration
develops with a lower occurrence rate, less severity and a quick
patient recovery.
The hyoid bone is large enough to restore different
types of laryngeal frame defects. If the thyroid cartilage at the
anterior commissure and the anterior region of the contralateral
vocal cord is removed, the diameter of the glottis can be restored
by carving the hyoid bone into an inverted V shape. It also
prevents the deflection of the glottis following reconstruction
with soft tissue alone. There is enough periosteum of hyoid to be
used for fixation. There is no displacement and hardly any atrophy
of the bone graft after fixation. Thus, the diameter of the glottis
is restored well and in a long-standing manner. The interior tissue
of the hyoid is ligament-like membrane that can be easily sutured
and epithelialized. All these are favorable factors for the
prevention of laryngeal stenosis and an increase in the extubation
rate.
In the present study, the post-operative voices of 6
patients were significantly improved, while 13 patients had nearly
the same quality of voice pre- and post-operatively. Hoarseness was
aggravated post-operatively in seven patients, but their daily
communication was not affected. The 3 cases that underwent
pre-operative radiotherapy were successfully reconstructed.
In summary, the present study demonstrated that a
hyoid osteomuscular flap characterized by hard bone and soft muscle
tissue can be applied to achieve restoration of laryngeal function
and structure. This technique is suitable for the reconstruction
after partial laryngectomy in patients with laryngeal cancer.
References
|
1
|
van Dijk BA, Karim-Kos HE, Coebergh JW,
Marres HA and de Vries E: Progress against laryngeal cancer in The
Netherlands between 1989 and 2010. Int J Cancer. 134:674–681. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pucher B and Grzegorowski M: Surgical
treatment of laryngomalacia in children. Otolaryngol Pol.
60:349–354. 2006.(Article in Polish). PubMed/NCBI
|
|
3
|
Forastiere AA, Goepfert H, Maor M, et al:
Concurrent chemotherapy and radiotherapy for organ preservation in
advanced laryngeal cancer. N Engl J Med. 349:2091–2098. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hoffman HT, Porter K, Karnell LH, et al:
Laryngeal cancer in the United States: changes in demographics,
patterns of care and survival. Laryngoscope. 116:(Suppl 111). 1–13.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Silver CE, Beitler JJ, Shaha AR, et al:
Current trends in initial management of laryngeal cancer: the
declining use of open surgery. Eur Arch Otorhinolaryngol.
266:1333–1352. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Liu B, Pan Z and Ji W: Reconstruction of
laryngeal defect in vertical partial laryngectomy with resection of
arytenoid cartilage. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi.
40:52–55. 2005.(In Chinese). PubMed/NCBI
|
|
7
|
Ulualp SO: Mapping regional
laryngopharyngeal mechanoreceptor response. Clin Exp
Otorhinolaryngol. 7:319–323. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ouyang D1, Liu TR, Liu XW, Chen YF, Wang
J, Su X and Yang AK: Combined hyoid bone flap in laryngeal
reconstruction after extensive partial laryngectomy for laryngeal
cancer. Eur Arch Otorhinolaryngol. 270:1455–1462. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Diab S, Pascoe J, Shahriar M, Read D,
Kinde H, Moore J, Odani J and Uzal F: Study of laryngopharyngeal
pathology in Thoroughbred horses in southern california. Equine Vet
J. 41:903–907. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jia S, Sun B and Shang L: Extended
vertical partial laryngectomy for treatment of the glottic cancer
with T3 category. Zhonghua Er Bi Yan Hou Ke Za Zhi. 31:365–367.
1996.(In Chinese). PubMed/NCBI
|
|
11
|
Tu G, Tang P and He Y: The use of hyoid
osteomuscular flap in extended partial laryngectomy. Zhonghua Er Bi
Yan Hou Ke Za Zhi. 31:39–42. 1996.(In Chinese). PubMed/NCBI
|
|
12
|
Yan D, Zhang B, Qi Y, et al: Supracricoid
partial laryngectomy versus other traditional partial laryngectomy
for selected laryngeal cancers. Lin Chung Er Bi Yan Hou Tou Jing
Wai Ke Za Zhi. 24:828–831. 2010.(In Chinese). PubMed/NCBI
|
|
13
|
Zhang SY, Lu ZM, Chen LS, et al:
Supracricoid partial laryngectomy cricohyoidoepiglottopexy
(SCPL-CHEP) versus vertical partial laryngectomy for the treatment
of glottic carcinoma. Eur Arch Otorhinolaryngol. 270:1027–1034.
2013. View Article : Google Scholar : PubMed/NCBI
|