Introduction
Breast cancer is one of the most commonly occurring
cancers in females, with ~1.7 million new cases diagnosed and 0.5
million mortalities reported annually, worldwide (1). The main treatments for breast cancer
include hormonal therapy, chemotherapy, radiotherapy and surgery
(1,2).
The survival rates for breast cancer are dependent on the stage at
which the tumor is diagnosed. According to the National Cancer
Institute's Surveillance, Epidemiology, and End Results 2015
database, the relative 5-year survival rates of breast cancer
stages I, II, III and IV, are 100, 93, 72 and 22%, respectively
(3). If breast cancer is not
appropriately diagnosed and treated, numerous complications may
develop, such as psychological, nervous, lymph and circulatory
disorders. Furthermore, advanced breast cancer may lead to
life-threatening metastasis of the tumor to numerous organs,
including the liver, kidney, bone, skin and lung, ultimately
leading to patient mortality (4).
Variations in host genetic factors are emerging as key determinants
for breast cancer risk and responsiveness to chemotherapeutic
agents (5). Among these variations,
polymorphisms in antioxidant enzymes and innate immune receptors
have been demonstrated to play major roles in the development of
malignancies (6).
Glutathione S-transferase is a phase II detoxifying
enzyme that catalyzes the conjunction of reduced glutathione with a
wide variety of electrophilic substrates and reactive oxygen
species (7). Polymorphisms consisting
of single-nucleotide substitutions in the coding sequence of the
glutathione S-transferase π 1 gene (GSTP1; 1578A>G) give
rise to the Ile105Val amino acid substitution; this lies
within the substrate-binding site of GSTP1 (8). Patients with homozygous isoleucine
(Ile/Ile) have the highest level of GSTP1 activity. The
GSTP1 105Val variant is associated with a lower
thermal stability and altered catalytic activity in response to a
variety of substrates compared with GSTP1 105Ile
(9). GSTP1 activity is somewhat
reduced in heterozygotes (Ile/Val) and further diminished for those
with two copies of valine (Val/Val) (10).
Toll-like receptors (TLRs) are important members of
the host innate immune response and their genes have been found to
be polymorphic (11). TLR2
stimulation on the surface of breast cancer cells has been
demonstrated to increase the invasive potential of the disease
through NF-κB signaling (12).
Furthermore, emerging evidence suggests that TLR2 signaling may aid
tumor cells in overcoming immune surveillance and avoiding attack
by the host immune system (13).
Genetic studies on the TLR2 gene have identified a
polymorphism that causes a 22-bp nucleotide deletion (−196 to −174
del) in its promoter. This substitution may significantly alter the
function of the promoter, likely leading to decreased transcription
of TLR2 (14). This
polymorphism is reported to be associated with increased
susceptibility to hepatocellular carcinoma and gastric cancer
(15,16).
TLR9 is a well-known mediator of innate immunity
that is capable of detecting DNA from microbial and endogenous
sources (17,18). In addition to its role in innate
immunity, TLR9 has been demonstrated to be widely expressed in
breast cancers, and its stimulation has been implicated in breast
cancer cell invasion (19). However,
the complete role of TLR9 in breast pathophysiology has not been
clearly established. Recent data indicate that polymorphisms in the
TLR9 gene (rs352144, rs187084, rs352139, rs352140 and
rs445676) may cause an imbalance between pro- and anti-inflammatory
cytokines, resulting in chronic inflammation and cancer development
(20–22). The majority of studies have focused on
three common single nucleotide polymorphisms (SNPs): rs352140,
rs5743836 and rs187084. Nevertheless, data regarding the rs187084
genetic variant of TLR9 and its link to breast cancer
development are still lacking.
To the best of our knowledge, there is extremely
little data in the literature regarding TLR2 and TLR9
polymorphisms in patients with breast cancer. Therefore, the aim of
the present study was to assess whether an association exists
between the development of breast cancer in Egyptian females and
genetic polymorphisms of GSTP1, TLR2 and TLR9.
Subjects and methods
Subjects
The present study was conducted on 72 patients
diagnosed with breast cancer at the Oncology Center of Mansoura
University (Mansoura, Egypt) between September 2013 and December
2013. Prior to commencing treatment, relevant information was
obtained from each patient regarding age, menopausal status, number
of children, lactation history and family history of breast cancer.
Patients with chronic diseases (such as diabetes mellitus, liver
dysfunction or rheumatoid arthritis) were excluded from the study.
All pathological data were recorded following surgery (Table I). The control group included 100
healthy female volunteers. Each study participant provided written
informed consent. The study was approved by the ethics committee of
the Faculty of Medicine of Mansoura University.
 | Table I.Clinicopathological characteristics
of the studied patients (n=72). |
Table I.
Clinicopathological characteristics
of the studied patients (n=72).
| Patient
characteristics | n | % |
|---|
| Age, years (range,
27–76) |
|
|
|
≤45 | 19 | 26.4 |
|
46–55 | 31 | 43.1 |
|
>55 | 22 | 30.6 |
| Menopausal
status |
|
|
|
Premenopausal | 28 | 38.9 |
|
Postmenopausal | 44 | 61.1 |
| Number of
children |
|
|
| 0 | 2 |
2.8 |
| 1 | 2 |
2.8 |
| 2 | 10 | 13.9 |
| 3 | 30 | 41.7 |
| 4 | 23 | 31.9 |
| 5 | 1 |
1.4 |
| 6 | 3 |
4.2 |
| 7 | 1 |
1.4 |
| Lactation
history |
|
|
|
Positive | 69 | 95.8 |
|
Negative | 3 |
4.2 |
| Family history of
breast cancer |
|
|
|
Positive | 6 |
8.3 |
|
Negative | 66 | 91.7 |
| Pathology |
|
|
|
Infiltrating ductal
carcinoma | 64 | 88.9 |
|
Infiltrating lobular
carcinoma | 6 |
8.3 |
| Paget
disease | 2 |
2.8 |
| Grade |
|
|
| I | 6 |
8.3 |
| II | 47 | 65.3 |
|
III | 19 | 26.4 |
| Number of
infiltrated lymph nodes |
|
|
|
0–10 | 61 | 84.7 |
|
11–20 | 8 | 11.1 |
|
21–30 | 3 |
4.2 |
| Lymphovascular
invasion |
|
|
|
Positive | 52 | 72.2 |
|
Negative | 20 | 27.8 |
| T stage |
|
|
| 1 | 11 | 15.3 |
| 2 | 42 | 58.3 |
| 3 | 15 | 20.8 |
| 4 | 4 |
5.6 |
| N stage |
|
|
| 0 | 20 | 27.8 |
| 1 | 20 | 27.8 |
| 2 | 19 | 26.4 |
| 3 | 13 | 18.1 |
| M stage |
|
|
| 0 | 57 | 79.2 |
| 1 | 15 | 20.8 |
| ER-positive cases,
%a |
|
|
| 0 | 9 | 12.5 |
|
10–20 | 12 | 16.7 |
|
30–40 | 17 | 23.6 |
|
50–60 | 12 | 16.7 |
|
70–80 | 17 | 23.6 |
|
90–100 | 5 |
6.9 |
| PR-positive cases,
%a |
|
|
| 0 | 6 |
8.3 |
|
10–20 | 13 | 18.1 |
|
30–40 | 21 | 29.2 |
|
50–60 | 15 | 20.8 |
|
70–80 | 13 | 18.1 |
|
90–100 | 4 |
5.6 |
| HER2
expression |
|
|
|
Positive | 17 | 23.6 |
|
Negative | 55 | 76.4 |
Specimen collection
For the assessment of GSTP1, TLR2 and TLR9 genetic
polymorphisms, 5 ml blood was drawn from each subject enrolled in
the study following an overnight fast, and was collected in EDTA
tubes (BD Vacutainer Systems, Plymouth, UK) for DNA extraction. DNA
was extracted from EDTA-anticoagulated blood using a Gentra
Puregene Blood Kit for DNA purification (Qiagen, Inc., Valencia,
CA, USA).
Histopathological and
immunohistochemical examination
Tumor evaluation and grading were assessed
histopathologically, as previously described (23). Tumor size, regional lymph nodes and
distant metastasis were also evaluated and staged according to the
American Joint Committee on Cancer Staging Manual (6th edition)
(24). For immunohistochemical
staining, samples were fixed with 10% neutral-buffered formalin and
routinely processed to paraffin blocks. Next, 4-µm sections were
cut from the blocks and mounted on poly-L-lysine pre-coated glass
slides. Antigen retrieval was performed in a pressure cooker for 20
min at 120°C followed by incubation with blocking 6%
H2O2 for 3 min to block endogenous peroxidase
activity. The sections were then incubated with the Lab Vision™
Avidin Biotin Blocking Solution (cat. no. TA-015-BB (Thermo Fisher
Scientific, Pittsburgh, PA, USA) to block nonspecific protein
binding. Following antigen retrieval, the sections were incubated
for 1 h at room temperature with primary antibodies, followed by
horseradish peroxidase-conjugated secondary antibodies (Dako,
Glostrup, Denmark) for 30 min at room temperature. The primary
antibodies used were as follows: Monoclonal rabbit anti-human
estrogen receptor (ER) antibody (clone SP1; cat. no. MA1-39540;
1:200; Thermo Fisher Scientific, Waltham, MA, USA), monoclonal
mouse anti-human progesterone receptor (PR) antibody (clone PgR
636; 1:50; cat. no. M3569; Dako) and monoclonal mouse anti-human
human epidermal growth factor receptor 2 (HER2) antibody (clone
CB11; 1:10; cat. no. 18-7107; Thermo Fisher Scientific). The
secondary antibodies used were as follows: Polyclonal goat
anti-rabbit IgG antibody (1:200; cat. no. P0448; Dako) or
polyclonal rabbit anti-mouse IgG antibody (1:200; cat. no. P0260;
Dako). 3,3′-diaminobenzidine (Thermo Fisher Scientific) was then
added as a chromogen for color development. The expression of the
ER and PR were assessed immunohistochemically, as described
previously (25). Scoring for both ER
and PR expression was based on the proportion of cells in a given
tumor specimen exhibiting distinct nuclear immunopositivity, as
well as the intensity of staining (0, 5, 10, 20, 30, 40, 50, 60,
70, 80, 90 or 100%). Positive immunostaining for ER/PR expression
was defined as >10% of cells with positively stained nuclei of
any intensity. Samples exhibiting >10% immunoexpression were
considered positive. HER 2-positivity was defined
immunohistochemically, according to the Food and Drug
Administration-approved criteria, as uniform and intense
circumferential membrane staining in >10% of invasive tumor
cells (26).
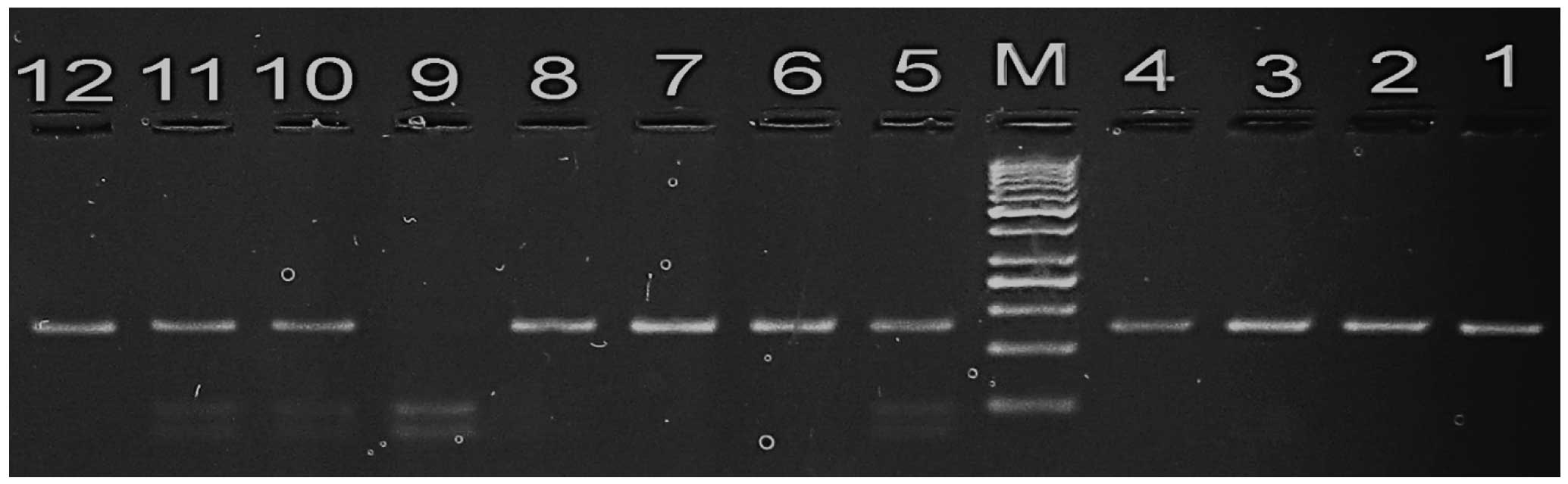
Detection of GSTP1 polymorphism
The GSTP1 105 Ile/Val polymorphism was investigated
using a polymerase chain reaction (PCR)-restriction fragment length
polymorphism (RFLP) method with the following primers (27): p105 forward,
5′-ACCCCAGGGCTCTATGGGAA-3′; and p105 reverse,
5′-TGAGGGCACAAGAAGCCCCT-3′ (Biosearch Technologies, Petaluma, CA,
USA). PCR was performed using DreamTaq Green PCR Master Mix (Thermo
Fisher Scientific). The procedure was conducted in a total reaction
volume of 40 µl. containing 1.5 mM MgCl2, 1 unit of Taq
DNA polymerase, 200 ng of each primer and 10 µl DNA as template.
PCR cycling conditions were as follows: Initial denaturation at
95°C for 5 min; 30 cycles of denaturation at 95°C for 30 sec,
primer annealing at 55°C for 30 sec and extension at 72°C for 1
min; and a final polymerization step of 72°C for 5 min to complete
the elongation processes. The PCR products (20 µl) were then
digested using 5 units of Alw261 restriction enzyme (Thermo
Fisher Scientific) in a total volume of 25 µl, and subsequently
separated on a 3.5% agarose gel (Bio Basic Inc., Markham, ON,
Canada) prior to staining with ethidium bromide (10 mg/ml; Bio
Basic Inc.) to visualize the bands (Fig.
1). Individuals with the wild genotype (Ile/Ile) exhibit a
single band (176 bp), whereas those with the mutant homozygote
(Val/Val) exhibit two bands (85 and 91 bp). Individuals with the
variant allele (Ile/Val) exhibit three bands (176 bp corresponding
to Ile; and 91 and 85 bp corresponding to Val).
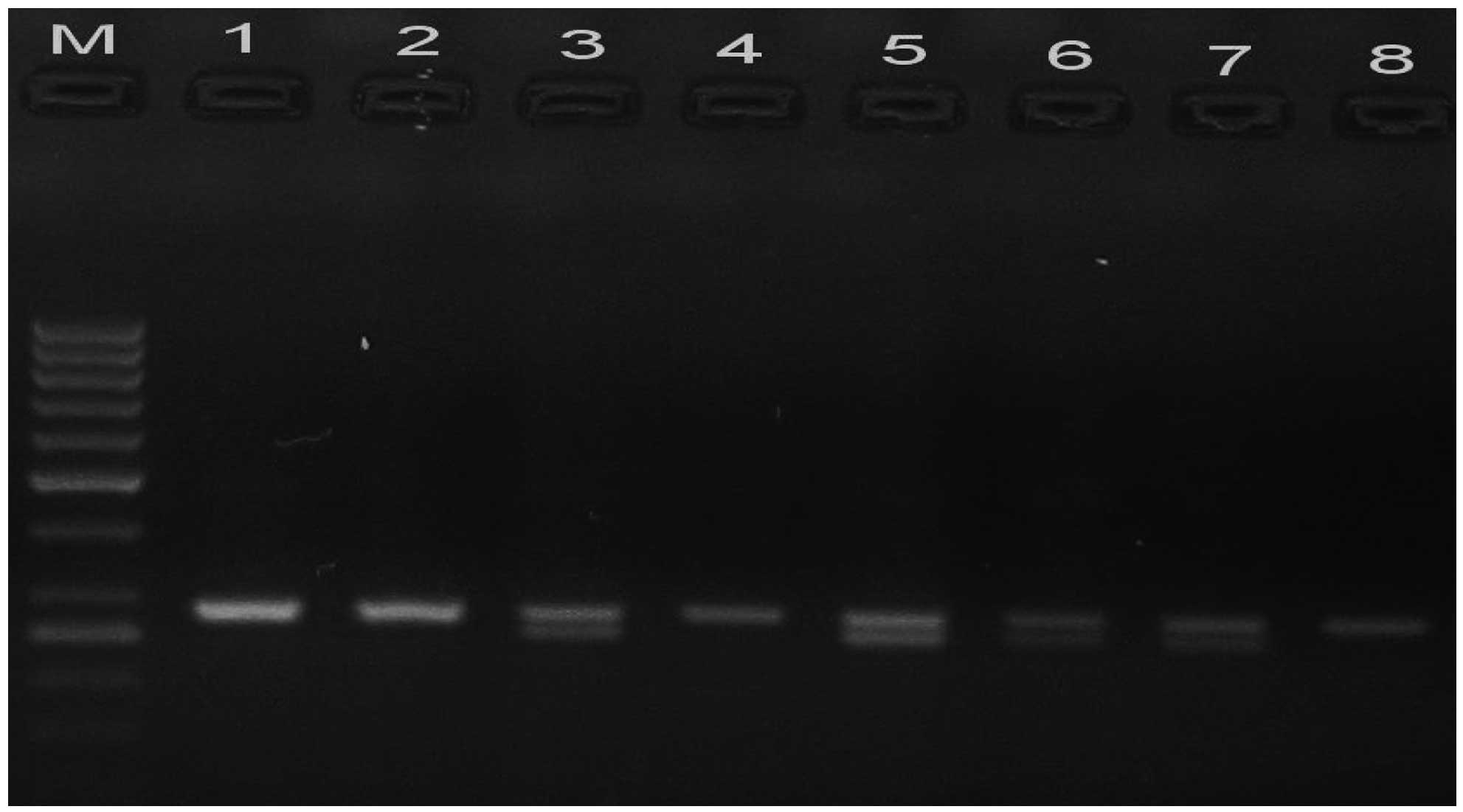
Assessment of TLR2 polymorphism
The TLR2 −196 to −174 del/ins polymorphism
was assessed using an allele-specific PCR method with the following
primers (28): forward,
5′-CACGGAGGCAGCGAGAAA-3′; and reverse, 5′-CTGGGCCGTGCAAAGAAG-3′
(Biosearch Technologies). The procedure was conducted in a total
reaction volume of 25 µl, containing 2.5 µl 10X PCR buffer, 2 µl
dNTPs (1.25 µmol/l), 0.5 µl MgCl2 (25 mmol/l), 1.25 µl
of each primer (25 mmol/l; Sigma-Aldrich, St. Louis, MO, USA), 15.3
µl dH2O, 2 µl DNA (100 ng/µl), and 0.2 µl Taq DNA
polymerase (5 U/µl; Invitrogen Life Technologies, Carlsbad, CA,
USA). PCR cycling conditions were as follows: Initial denaturation
step at 95°C for 5 min; amplification at 95°C for 30 sec, 60°C for
40 sec and 72°C for 40 sec, for 35 cycles; and a final elongation
step at 72°C for 7 min. Fig. 2 shows
the resulting homozygous (ins/ins; band at 286 bp) and heterozygous
(ins/del; bands at 286 and 264 bp) genotypes following 3.5% agarose
gel electrophoresis and ethidium bromide staining of the PCR
products.
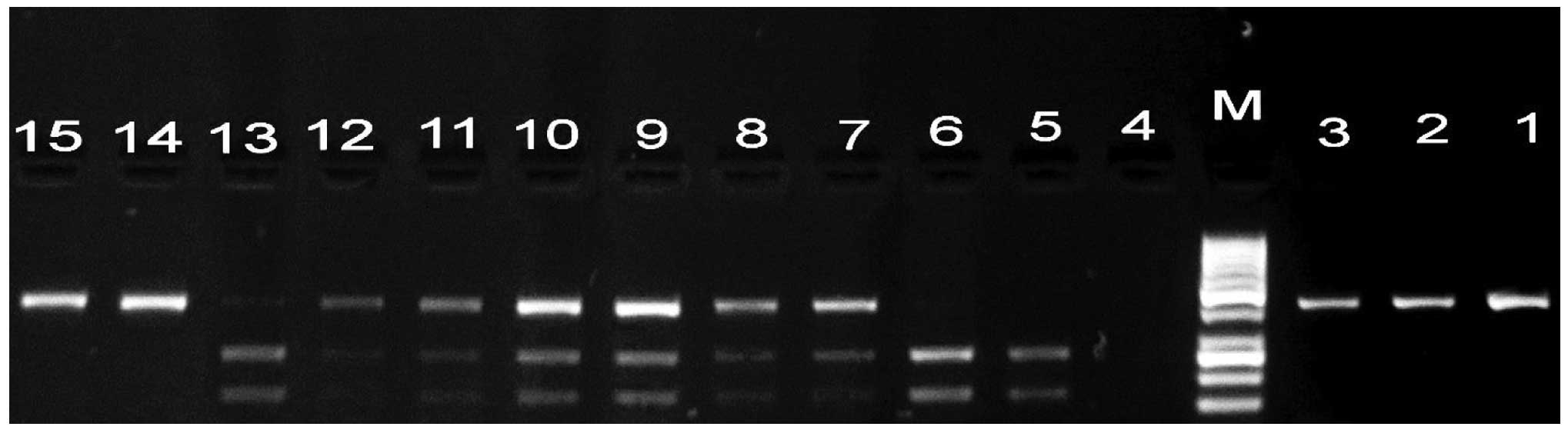
Detection of TLR9 polymorphism
Genotyping of TLR9 was conducted using PCR-RFLP, as
previously described (29). PCR
reactions consisted of an initial step of 95°C for 5 min, followed
by 35 cycles at 95°C 30 sec, 60°C for 30 sec and 72°C for 30 sec,
and a final incubation at 72°C for 5 min. Briefly, PCR mixtures (30
µl final volume) contained 20 ng of genomic DNA, 20 pmol of each
primer (25 pmol/ml; Intergrated DNA Technologies, Coralville, IA,
USA), 3 µl ml of dNTPs (2.5 nM; Thermo Fisher Scientific), 3 µl
MgCl2 (25 mM; Thermo Fisher Scientific), 1 ml of
NH4 buffer and 0.2 µl of Taq polymerase (Thermo Fisher
Scientific). The following primers for TLR9-rs187084 (1237T/C) were
used: forward, 5′-ACTATCGAGCCTGCCTGCCATGATACC-3′; and reverse,
5′-ATCCAGCCTTCTTACAAACCTCCCACCC-3′ (Biosearch Technologies). A
15-µl aliquot of each product was digested with 0.5 units of
BspTI (Thermo Fisher Scientific). PCR products were
subjected to electrophoresis on a 2% agarose gel and visualized by
ethidium bromide staining (Fig. 3).
The presence of a wild type allele (C allele) for TLR9 resulted in
an intact 423-bp band, whereas the RFLP profile of the T variant
was characterized by two bands of 172 and 251 bp.
Statistical analysis
The χ2 test was employed to examine
differences in genotypic and allelic distribution between breast
cancer patients and controls. The odds ratio (OR) and 95%
confidence intervals (CI) were calculated. P<0.05 was considered
to indicate statistically significant differences. Statistical
tests were performed with GraphPad Prism software version 5.0
(GraphPad Software, Inc, La Jolla, CA, USA).
Results
Patient characteristics
The breast cancer group (n=72) had a median age of
46.2 years (range, 27–76 years), with postmenopausal status in
61.1%, positive lactation history in 95.8%, positive family history
of breast cancer in 8.3% and metastasis in 20.8%. The staging and
other clinical and pathological characteristics are shown in
Table I.
GSTP1 genotype distribution
The distribution of the different genotypes of
GSTP1 is presented in Table
II. A significantly lower percentage of the GSTP1
Ile/Val (heterozygous) genotype was observed in women with breast
cancer compared with healthy individuals (26.4 vs. 41%,
respectively; P=0.0297; OR=2.112). There was also a significant
decrease in the combined number of Val/Val and Ile/Val genotypes
frequencies in breast cancer patients compared with controls, at
rates of 36.1 and 51%, respectively (P=0.0283; OR=1.995).
Furthermore, the GSTP1 Val allele frequency was decreased in breast
cancer patients relative to controls, at rates of 22.9 and 32.5%,
respectively.
 | Table II.GSTP1 genotypes and allele
distribution in breast cancer patients and control subjects. |
Table II.
GSTP1 genotypes and allele
distribution in breast cancer patients and control subjects.
|
| Breast cancer
patients (n=72) | Controls
(n=100) |
|
|
|
|---|
|
|
|
|
|
|
|
|---|
| GSTP1
genotype | n | % | n | % | OR | 95% CI | P-value |
|---|
| Ile/Ile | 46 | 63.9 | 47 | 47.0 | Reference |
|
|
| Ile/Val | 19 | 26.4 | 41 | 41.0 | 2.112 |
1.071–4.165 |
0.0297 |
| Val/Val |
7 |
9.7 | 12 | 12.0 | 1.678 |
0.607–4.639 | 0.315 |
| Ile/Val +
Val/Val | 26 | 36.1 | 53 | 53.0 | 1.995 |
1.073–3.712 |
0.0283 |
| Ile frequency | 111 | 77.1 | 135 | 67.5 |
|
|
|
| Val frequency | 33 | 22.9 | 65 | 32.5 | 1.619 | 0.994–2.64 | 0.052 |
TLR genotype distribution
The genotype and allele frequencies of TLR2
did not differ significantly between breast cancer patients and
controls (Table III). However, the
frequency of the TLR9 CC and CT genotypes were significantly
lower in women with breast cancer compared with healthy individuals
[CC, 12.5% vs. 20%, respectively (P=0.0016; OR=0.316); CT, 47.2%
vs. 63%, respectively (P=0.0069; OR=0.264)]. A significant decrease
was also observed in the overall TLR9 C allele frequency in
breast cancer patients compared with controls, at rates of 36.1 and
51.5%, respectively (P=0.0047; OR=0.532).
 | Table III.Genotypes and alleles distribution of
TLR2 and TLR9 in breast cancer patients and control
subjects. |
Table III.
Genotypes and alleles distribution of
TLR2 and TLR9 in breast cancer patients and control
subjects.
|
| Breast cancer
patients (n=72) | Controls
(n=100) |
|
|
|
|---|
|
|
|
|
|
|
|
|---|
| Genotypes | n | % | n | % | OR | 95% CI | P-value |
|---|
| TLR2 |
|
|
|
|
|
|
|
|
Ins/Ins | 44 | 61.1 | 61 | 61.0 | Reference |
|
|
|
Del/Ins | 22 | 30.6 | 33 | 33.0 | 1.082 | 0.557–2.103 | 0.8667 |
|
Del/Del | 6 |
8.3 |
6 |
6.0 | 0.721 | 0.218–2.386 | 0.7956 |
| Ins
frequency | 110 | 76.4 | 155 | 77.5 |
|
|
|
| Del
frequency | 34 | 23.6 | 45 | 22.5 | 0.939 | 0.565–1.561 | 0.809 |
| TLR9 |
|
|
|
|
|
|
|
| TT | 29 | 40.3 | 17 | 17.0 | Reference |
|
|
| CT | 34 | 47.2 | 63 | 63.0 | 0.316 | 0.153–0.656 | 0.0016 |
| CC | 9 | 12.5 | 20 | 20.0 | 0.264 | 0.098–0.709 | 0.0069 |
| T
frequency | 92 | 63.9 | 97 | 48.5 |
|
|
|
| C
frequency | 52 | 36.1 | 103 | 51.5 | 0.532 | 0.343–0.825 | 0.0047 |
Discussion
The present study investigated whether polymorphisms
of GSTP1, TLR2 and TLR9 are associated with
the development of breast cancer in the Egyptian population. The
results of the GSTP1 105 Ile/Val genetic polymorphism
assessment revealed a decreased frequency of the Val allele among
breast cancer patients relative to that of control subjects. In
disagreement with the current results, Shea et al (30) observed no association between
GSTP1 genotypes and breast cancer susceptibility in the
American population. This discordance of data may be partly
attributed to unknown genetic or environmental exposures that may
modify the effects of GSTP1 genes in a certain population
(31). This result may be suggestive
of the differential effect of GSTP1 genotypes on cellular
proliferation and apoptosis, which may be translated into cell
viability (32). Adler and Pincus
(33) reported that peptides covering
amino acid residues 99–121 influence the binding of GSTP1 to c-Jun
N-terminal kinase (JNK) 1, suggesting that the Ile105Val
substitution has no effect on cell proliferation, but protects
cells from apoptosis through a JNK-dependent mechanism.
The present investigation into the TLR2 −174
to −196 del polymorphism indicated that the insertion/deletion
(ins/del) and del/del genotypes (d allele) are not associated with
breast cancer. In agreement with these findings, Etokebe et
al (34) failed to demonstrate
any correlation between the TLR2 d allele and breast cancer
development. However, a study by Theodoropoulos et al
(35) reported a positive association
between this polymorphism and an increased risk of breast cancer in
the Greek population. The reason for this discordance may be
attributed to different genetic backgrounds between the studied
populations, varying sample sizes and heterogeneity of the tumors
examined (36).
The results of the current study indicated that the
TLR9 rs187084 (1237T/C) polymorphism was associated with an
increased risk of breast cancer in women, based on an Egyptian
patient population. To date, no functional data is available
regarding the rs187084 polymorphism, however, due to its location
in the promoter region of the gene, it may alter the function of
the promoter (37). The variant
alleles of this TLR9 polymorphism may alter the response to
DNA from both microbial and endogenous sources, and thereby
influence the production of more pro-inflammatory mediators. A
recent study revealed that the high activity T allele of rs187084
appears to be a risk factor for the development of endometrial
cancer (38). By contrast, the C
allele of the rs187084 and T allele of the rs352140 TLR9
polymorphisms were recently reported to be associated with an
increased risk of cervical cancer in Poland (19).
In conclusion, the current findings indicate
significant roles for TLR9 rs187084 (1237T/C) and
GSTP1 (Ile/Val) polymorphic variants in the susceptibility
to breast cancer of an Egyptian female population, whilst no
association was observed for the TLR2 −196 to −174 del/ins
polymorphism. Thus, polymorphisms in GSTP1 and TLR9,
but not TLR2, may be important in the development of breast
cancer.
Acknowledgements
The authors wish to acknowledge the laboratory
support of the Clinical Immunology Unit, Clinical Pathology
Department, Faculty of Medicine of Mansoura University for
facilitating the molecular genetic studies.
References
|
1
|
Ferlay J, Soerjomataram I, Dikshit R, Eser
S, Mathers C, Rebelo M, Parkin DM, Forman D and Bray F: Cancer
incidence and mortality worldwide: Sources, methods and major
patterns in GLOBOCAN 2012. Int J Cancer. 136:E359–E386. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Howard JH and Bland KI: Current management
and treatment strategies for breast cancer. Curr Opin Obstet
Gynecol. 24:44–48. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Itano JK, Brant J, Conde F and Saria M:
Breast Cancer. Core Curriculum for Oncology Nursing (5th).
(Philadelphia, PA). Elsevier Health Sciences. 752015.
|
|
4
|
Weigelt B, Peterse JL and van't Veer LJ:
Breast cancer metastasis: Markers and models. Nat Rev Cancer.
5:591–602. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ulrich CM, Robien K and McLeod HL: Cancer
pharmacogenetics: Polymorphisms, pathways and beyond. Nat Rev
Cancer. 3:912–920. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Klaunig JE, Kamendulis LM and Hocevar BA:
Oxidative stress and oxidative damage in carcinogenesis. Toxicol
Pathol. 38:96–109. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hayes JD and Pulford DJ: The glutathione
S-transferase supergene family: Regulation of GST and the
contribution of the isoenzymes to cancer chemoprotection and drug
resistance. Crit Rev Biochem Mol Biol. 30:445–600. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yang G, Shu XO, Ruan ZX, Cai QY, Jin F,
Gao YT and Zheng W: Genetic polymorphisms in
glutathione-S-transferase genes (GSTM1, GSTT1, GSTP1) and survival
after chemotherapy for invasive breast carcinoma. Cancer.
103:52–58. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Johansson AS, Stenberg G, Widersten M and
Mannervik B: Structure-activity relationships and thermal stability
of human glutathione transferase P1-1 governed by the H-site
residue 105. J Mol Biol. 278:687–698. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhang BL, Sun T, Zhang BN, Zheng S, Lü N,
Xu BH, Wang X, Chen GJ, Yu DK and Lin DX: Polymorphisms of GSTP1 is
associated with differences of chemotherapy response and toxicity
in breast cancer. Chin Med J (Engl). 124:199–204. 2011.PubMed/NCBI
|
|
11
|
Medvedev AE: Toll-like receptor
polymorphisms, inflammatory and infectious diseases, allergies, and
cancer. J Interferon Cytokine Res. 33:467–484. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Xie W, Wang Y, Huang Y, Yang H, Wang J and
Hu Z: Toll-like receptor 2 mediates invasion via activating
NF-kappaB in MDA-MB-231 breast cancer cells. Biochem Biophys Res
Commun. 379:1027–1032. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Huang B, Zhao J, Unkeless JC, Feng ZH and
Xiong H: TLR signaling by tumor and immune cells: A double-edged
sword. Oncogene. 27:218–224. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Noguchi E, Nishimura F, Fukai H, Kim J,
Ichikawa K, Shibasaki M and Arinami T: An association study of
asthma and total serum immunoglobin E levels for Toll-like receptor
polymorphisms in a Japanese population. Clin Exp Allergy.
34:177–183. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Nischalke HD, Coenen M, Berger C,
Aldenhoff K, Müller T, Berg T, Krämer B, Körner C, Odenthal M,
Schulze F, et al: The toll-like receptor 2 (TLR2) −196 to −174 del
ins polymorphism affects viral loads and susceptibility to
hepatocellular carcinoma in chronic hepatitis C. Int J Cancer.
130:1470–1475. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tahara T, Arisawa T, Wang F, Shibata T,
Nakamura M, Sakata M, Hirata I and Nakano H: Toll-like receptor
2–196 to 174del polymorphism influences the susceptibility of
Japanese people to gastric cancer. Cancer Sci. 98:1790–1794. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Latz E, Schoenemeyer A, Visintin A,
Fitzgerald KA, Monks BG, Knetter CF, Lien E, Nilsen NJ, Espevik T
and Golenbock DT: TLR9 signals after translocating from the ER to
CpG DNA in the lysosome. Nat Immunol. 5:190–198. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tian J, Avalos AM, Mao SY, Chen B, Senthil
K, Wu H, Parroche P, Drabic S, Golenbock D, Sirois C, et al:
Toll-like receptor 9-dependent activation by DNA-containing immune
complexes is mediated by HMGB1 and RAGE. Nat Immunol. 8:487–496.
2007. View
Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ilvesaro JM, Merrell MA, Li L, Wakchoure
S, Graves D, Brooks S, Rahko E, Jukkola-Vuorinen A, Vuopala KS,
Harris KW and Selander KS: Toll-like receptor 9 mediates CpG
oligonucleotide-induced cellular invasion. Mol Cancer Res.
6:1534–1543. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Roszak A, Lianeri M, Sowińska A and
Jagodziński PP: Involvement of Toll-like receptor 9 polymorphism in
cervical cancer development. Mol Biol Rep. 39:8425–8430. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kutikhin AG: Association of polymorphisms
in TLR genes and in genes of the Toll-like receptor signaling
pathway with cancer risk. Hum Immunol. 72:1095–1116. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhang L, Qin H, Guan X, Zhang K and Liu Z:
The TLR9 gene polymorphisms and the risk of cancer: Evidence from a
meta-analysis. PLoS One. 8:e717852013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Robinson IA, McKee G, Nicholson A, D'Arcy
J, Jackson PA, Cook MG and Kissin MW: Prognostic value of
cytological grading of fine-needle aspirates from breast
carcinomas. Lancet. 343:947–949. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Singletary SE and Connolly JL: Breast
cancer staging: Working with the sixth edition of the AJCC Cancer
Staging Manual. CA Cancer J. Clin. 56:37–47. 2006.
|
|
25
|
Høgdall EV, Christensen L, Høgdall CK,
Blaakaer J, Gayther S, Jacobs IJ, Christensen IJ and Kjaer SK:
Prognostic value of estrogen receptor and progesterone receptor
tumor expression in Danish ovarian cancer patients: From the
'MALOVA' ovarian cancer study. Oncol Rep. 18:1051–1059.
2007.PubMed/NCBI
|
|
26
|
Wolff AC, Hammond ME, Hicks DG, Dowsett M,
McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M,
Fitzgibbons P, et al: American Society of Clinical Oncology;
College of American Pathologists: Recommendations for human
epidermal growth factor receptor 2 testing in breast cancer:
American Society of Clinical Oncology/College of American
Pathologists clinical practice guideline update. J. Clin Oncol.
31:3997–4013. 2013. View Article : Google Scholar
|
|
27
|
Harries LW, Stubbins MJ, Forman D, Howard
G and Wolf CR: Identification of genetic polymorphisms at the
glutathione S-transferase Pi locus and association with
susceptibility to bladder, testicular and prostate cancer.
Carcinogenesis. 18:641–644. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
de Oliveira JG and Silva AE: Polymorphisms
of the TLR2 and TLR4 genes are associated with risk of gastric
cancer in a Brazilian population. World J Gastroenterol.
18:1235–1242. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Etem EO, Elyas H, Ozgocmen S, Yildirim A
and Godekmerdan A: The investigation of toll-like receptor 3, 9 and
10 gene polymorphisms in Turkish rheumatoid arthritis patients.
Rheumatol Int. 31:1369–1374. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Shea TC, Claflin G, Comstock KE, Sanderson
BJ, Burstein NA, Keenan EJ, Mannervik B and Henner WD: Glutathione
transferase activity and isoenzyme composition in primary human
breast cancers. Cancer Res. 50:6848–6853. 1990.PubMed/NCBI
|
|
31
|
Sharma A, Pandey A, Sharma S, Chatterjee
I, Mehrotra R, Sehgal A and Sharma JK: Genetic polymorphism of
glutathione S-transferase P1 (GSTP1) in Delhi population and
comparison with other global populations. Meta Gene. 2:134–142.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Holley SL, Fryer AA, Haycock JW, Grubb SE,
Strange RC and Hoban PR: Differential effects of glutathione
S-transferase pi (GSTP1) haplotypes on cell proliferation and
apoptosis. Carcinogenesis. 28:2268–2273. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Adler V and Pincus MR: Effector peptides
from glutathione-S-transferase-pi affect the activation of jun by
jun-N-terminal kinase. Ann Clin Lab Sci. 34:35–46. 2004.PubMed/NCBI
|
|
34
|
Etokebe GE, Knezević J, Petricević B,
Pavelić J, Vrbanec D and Dembić Z: Single-nucleotide polymorphisms
in genes encoding toll-like receptor −2,-3,-4 and −9 in
case-control study with breast cancer. Genet Test Mol Biomarkers.
13:729–734. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Theodoropoulos GE, Saridakis V, Karantanos
T, Michalopoulos NV, Zagouri F, Kontogianni P, Lymperi M, Gazouli M
and Zografos GC: Toll-like receptors gene polymorphisms may confer
increased susceptibility to breast cancer development. Breast.
21:534–538. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Ng CK, Pemberton HN and Reis-Filho JS:
Breast cancer intratumor genetic heterogeneity: Causes and
implications. Expert Rev Anticancer Ther. 12:1021–1032. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Novak N, Yu CF, Bussmann C, Maintz L, Peng
WM, Hart J, Hagemann T, Diaz-Lacava A, Baurecht HJ, Klopp N, et al:
Putative association of a TLR9 promoter polymorphism with atopic
eczema. Allergy. 62:766–772. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ashton KA, Proietto A, Otton G, Symonds I,
McEvoy M, Attia J and Scott RJ: Toll-like receptor (TLR) and
nucleosome-binding oligomerization domain (NOD) gene polymorphisms
and endometrial cancer risk. BMC Cancer. 10:3822010. View Article : Google Scholar : PubMed/NCBI
|