Introduction
Villoglandular papillary adenocarcinoma (VGPA) was
first reported by Young and Scully in 1989 (1) and was classified as a histopathological
entity of cervical cancer by the World Health Organization in 1994
(2). VGPA is a specific type of
adenocarcinoma that is rarely identified by clinical diagnosis. To
the best of our knowledge, >150 cases of VGPA of the cervix have
been reported in the relevant literature. Human papillomavirus
infection and oral contraceptive use are considered to be
associated with VGPA (3,4). The final diagnosis of VGPA depends on
pathological confirmation. Histologically, VGPA is characterized by
exophytic proliferation with long and slender papillary structures
and a mild to moderate cellular atypia (5). There is no standard treatment for VGPA.
It has been reported that fertility-preserving surgery may be
considered if the tumor is at an early International Federation of
Gynecology and Obstetrics (FIGO) stage, and if it not a mixed type
adenocarcinoma of the uterine cervix that includes a villoglandular
component (6,7). Compared with ordinary adenocarcinoma,
VGPA is associated with a lower incidence, younger age and better
prognosis. These features have caused VGPA to gain more attention
clinically. Treatment with fertility-preserving surgery is also now
possible. In the present study, the clinical and pathological
features of this neoplasm are retrospectively reviewed using cases
from one institute, and the associated literature is also
discussed.
Patients and methods
Clinical profiles of VGPA
patients
All cases of VGPA identified by pre-operative biopsy
or post-operative surgical pathology at The Second Hospital of
Jilin University (Changchun, Jilin, China) between January 2010 and
December 2014 were retrieved. A total of 11 cases were selected,
however, patients whose post-operative diagnosis was of another
type of adenocarcinoma or ordinary adenocarcinoma associated with
VGPA were excluded. Therefore, 4 patients were excluded due to a
pre-operative diagnosis of VGPA, but a final surgical pathological
diagnosis of another type of adenocarcinoma or ordinary
adenocarcinoma associated with VGPA. Only 7 cases were included in
the present study. Among the 7 patients, 6 (54.5%; 6/11) were
diagnosed with VGPA in the pre-operative and post-operative
diagnoses. The remaining patient was pre-operatively diagnosed with
another type of adenocarcinoma. The clinical profiles included data
on patient age, presenting symptoms, history of oral contraceptive
(OCP) use, human papillomavirus (HPV) infection, International
Federation of Gynecology and Obstetrics (FIGO) staging, biopsy
pathology, treatment, post-operative pathology, adjuvant therapy,
lymph node (LN) metastasis, poor prognostic factors, follow-up and
outcome.
Results
Clinical characteristics
The median age of the patients whose pathology was
confirmed post-operatively was 36 years (range, 29–42 years). None
of the patients had a history of smoking or OCP use. The most
common symptom was contact bleeding (6 patients) and 1 patient
exhibited abnormal vaginal bleeding. All patients underwent a
pre-operative cervical biopsy. The predominant histological
features of VGPA include a villoglandular architecture and mild to
moderate cytological atypia and thus, VGPA was diagnosed in 6
patients and ordinary cervical adenocarcinoma in 1 patient.
However, the post-operative diagnosis of all 7 patients was of
VGPA, and all patients were positive for HPV.
In total, 6 patients (85.7%) presented with FIGO
stage IB1 disease and 1 with FIGO stage IIA1 disease (7). As all 7 patients were married with no
desire for further fertility, a radical hysterectomy was performed,
resulting in only 3 patients being left with one or both ovaries.
Of the 7 patients, 2 possessed poor prognostic factors; 1 patient
presented with invasive vascular infiltration, and the other with
endometrial involvement and right ovarian borderline serous gonadal
fibroma. Adjuvant therapy was being provided for 5 of the 7
patients. The follow-up time ranged from 7–57 months, with an
average time of 29 months. There was no evidence of recurrence in
any of the patients, and all patients remained alive at the time of
writing this study. The details of the patients' characteristics,
the pathology of the tumors and the management of the disease are
shown in Table I.
 | Table I.Characteristics of the patients with a
final histology of VGPA. |
Table I.
Characteristics of the patients with a
final histology of VGPA.
| Patient no. | Age, years | Presenting
symptom | OCP history | HPV status | FIGO stage | Pre-operative
diagnosis | Treatment | Adjuvant
treatment | LN metastasis | Poor prognostic
factor | Follow-up,
months | Outcome |
|---|
| 1 | 42 | AVB | − | + | IB1 | VGPA | RVH+PLND+BSO | + | − | Vascular invasion
infiltration | 10 | NED |
| 2 | 35 | CB | − | + | IB1 | VGPA | RVH+PLND+BSO | + | − | Endometrial
involvement | 30 | NED |
| 3 | 42 | CB | − | + | IB1 | VGPA | RVH+PLND+BSO | − | − | − | 8 | NED |
| 4 | 31 | CB | − | + | IB1 | CA | RVH+PLND+RO | + | − | − | 7 | NED |
| 5 | 32 | CB | − | + | IB1 | VGPA | RVH+PLND+RO | + | − | − | 57 | NED |
| 6 | 29 | CB | − | + | IIA1 | VGPA | RVH+PLND+RO | + | − | − | 55 | NED |
| 7 | 42 | CB | − | + | IB1 | VGPA | RVH+PLND+BSO | − | − | − | 37 | NED |
The 4 women who were excluded from the present study
were diagnosed with VGPA pre-operatively, but the final
histological examination yielded a different diagnosis. These 4
patients (aged 44, 37, 48 and 47 years old) presented with abnormal
vaginal bleeding or contact bleeding, and a punch biopsy was
performed. The histological diagnosis was of VGPA (FIGO stages IB1,
IB1, IB2 and IIA1). As the tumor was large and the women did not
desire the preservation of fertility, all the patients underwent a
radical hysterectomy with a double salpingo-oophorectomy and LN
dissection. The final histology yielded a diagnosis of ordinary
adenocarcinoma with negative nodes, not VGPA.
Discussion
VGPA of the uterine cervix is a rare subtype of
cervical adenocarcinoma that accounts for 3.7–4.8% of all cervical
AC (1,8). Compared with other malignant cervical
tumors, VGPA tends to occur in younger women, particularly those of
reproductive age. Young and Scully (1) first reported 13 cases of VGPA with an
average age of only 33 years old. The etiology of VGA remains
unknown. Certain studies (3,4) suggest a role for HPV infection in the
pathogenesis of VGPA. Jones et al (3) reported a study in which 15 (62.5%) out
of 24 VGPA patients were taking OCP, with a duration of use (when
known) ranging between 5 and 20 years; OCPs were considered to be
associated with VGPA. In the present study, the median age of the 7
patients was 36.1 years, with a range of 29–42 years. None of the
patients had a history of OCP use, but each case was positive for
HPV infection. This test result indicates that HPV infection is
more likely to be the cause of VGPA. The clinical manifestation of
VGPA is similar to other types of cervical cancer with regard to
abnormal vaginal bleeding, contact bleeding or abnormal vaginal
secretion (1).
The final diagnosis of VGPA depends on pathological
confirmation. As Young and Scully (1)
reported that conservative treatment is feasible for VGPA, an
accurate pre-operative diagnosis allows the opportunity for a
number of VGPA-affected women to preserve their fertility. The main
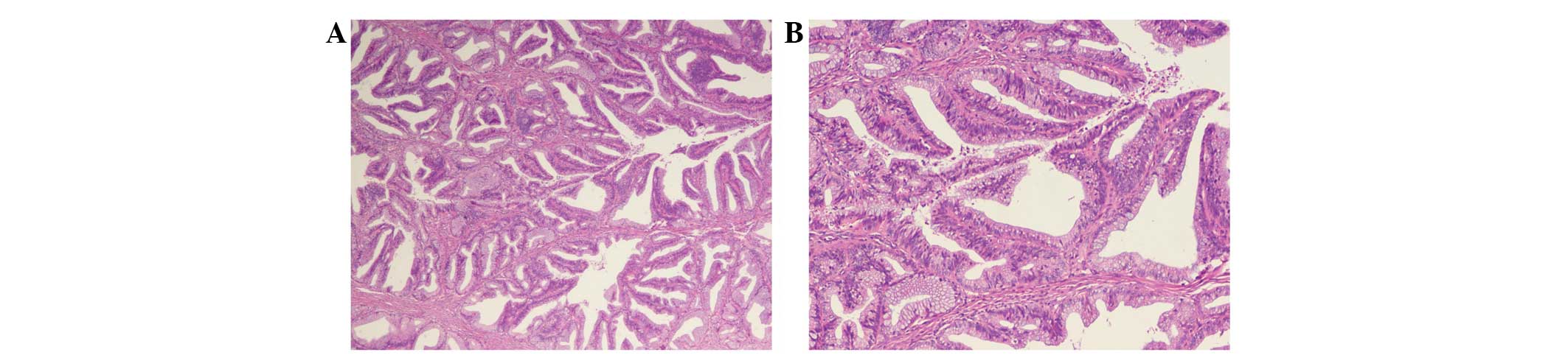
feature of VGPA is its villoglandular architecture. Each papilla in
the villoglandular structures has a central pedicle that ranges in
size and shape from short and thick to long and thin. The central
pedicle contains a number of inflammatory cells (Fig. 1). The villoglandular structures are
composed of stratified glandular cells, with mild to moderate
nuclear atypia, and mitotic figures, with little or no budding from
the villoglandular structures (9). A
study by Macdonald et al (10)
advised following the more recent changes in the definition of a
villoglandular tumor rather than continuing to conform to a limited
and conservative definition stating the presence of only
villoglandular components, with no standard adenomatous or squamous
features and no high-grade nuclear abnormalities.
Among the 11 cases initially selected in the present
study, only 54.5% (6/11) had the same pre-operative and
post-operative diagnosis. Similarly, in a study by Korach et
al (6), data were reviewed from
the outpatient files of 12 patients who had been diagnosed with
VGPA. The final pathology results confirmed a diagnosis of VGPA in
only 9 of the patients. Of these 9, only 2 had been correctly
pre-operatively diagnosed, while in 3, a benign or pre-malignant
initial biopsy result had been determined, and in the remaining 4
patients, an invasive malignant tumor had been diagnosed,
consequently necessitating a hysterectomy. The 3 non-VGPA patients
were diagnosed with invasive cervical adenocarcinoma on the final
histological report. Following integration of the data from the
literature review and the results of the present study cases, it
may be concluded that pre-treatment punch biopsy diagnosis has a
low rate of diagnostic accuracy when compared with the final
histological report. This may be attributed to two reasons:
Firstly, forming an accurate pre-operative pathological diagnosis
is difficult for VGPA. In 30% of cases, VGPA is associated with
other types of invasive cancer (1,11–14), which may have a significant impact on
its prognosis. It is therefore important to remember that ordinary
adenocarcinomas, including deeply invasive tumors, may have a
papillary component and that VGPA should only be diagnosed in those
lesions that are exclusively grade 1 and unassociated with an
underlying conventional adenocarcinoma component. Secondly, the
scope of a biopsy is limited, as it is unable to determine whether
the entire tumor contains other invasive adenocarcinoma tissues or
not. In addition, it is not easy to get to the basement membrane
while taking a biopsy, so infiltration cannot be completely ruled
out. Therefore, an excision or cone biopsy is occasionally required
to establish a VGPA diagnosis when a punch biopsy is not
sufficient.
Yamazawa et al (15) suggested that the recommendation of no
further treatment may be acceptable for patients who require
fertility preservation if the tumor is superficial with no
involvement of the vascular space, or if the cone margins exhibit
no residual disease. To date, only 6 cases of pregnancy associated
with VGPA of the cervix have been reported (Table II). In 3 of these cases, successful
conception was achieved following a conservative treatment for VGPA
(6,12,14). The 3
remaining cases were diagnosed during the pregnancy (16–18).
Nonetheless, the management of cervical VGPA is considered to be a
significant challenge. To date, >150 cases of VGA of the cervix
have been reported in the English literature, with 12 cases of
recurrence and 8 mortalities (Table
III) (3,6,19–21). In the clinical analysis of background
data, the patients who experienced a poor outcome were closely
associated with an advanced FIGO stage and LN metastasis. Of the
mortalities, 5 patients had VGPA of stage IIB or greater. LN
metastasis was reported in 5 patients, with 3 of these cases
developing recurrence (2 patients succumbed to recurrence). As the
current follow-up time of VGPA is short, a lack of data is
available on the 5-year survival rate.
 | Table II.Profile of patients with
villoglandular papillary adenocarcinoma associated with
pregnancy. |
Table II.
Profile of patients with
villoglandular papillary adenocarcinoma associated with
pregnancy.
| First author,
year | Age, years | FIGO stage | Follow-up | Outcome | Ref. |
|---|
| Takai et al,
2010 | 28 | IB1 | 44 months | NED | (18) |
| Hurteau et al,
1995 | 22 | IB | 14 months | NED | (16) |
| Lavie et al,
2008 | 31 | IB1 | 18 months | NED | (17) |
| Hoffman et al,
2001 | 28 | – | 24 months | NED | (12) |
| Falcon et al,
2006 | 34 | IB1 | 8
years | NED | (14) |
| Korach et al,
2009 | 34 | IA1 | 10 years | NED | (6) |
 | Table III.Incidence of lymph capillary space
invasion and/or LN metastasis in the English literature. |
Table III.
Incidence of lymph capillary space
invasion and/or LN metastasis in the English literature.
|
|
|
|
| Cases of
mortality |
|
|---|
|
|
|
|
|
|
|
|---|
| First author,
year | Total cases, n | Cases of LN
metastasis, n | Cases of recurrence,
n | Cases, n | Stage | Follow-up | Ref. |
|---|
| Kaku et al
1997 | 7 | 2 | 1 | 1 | IIB | 46
months | (19) |
| Jones et al
2000 | 12 | – | 2 | 1 | – | 79
months | (3) |
| Korach et al
2009 | 9 | – | 1 | 1 | IB1 | 2 years | (6) |
| Lataifeh et
al 2013 | 28 | 2 | 5 | 5 | IB2, IB, IIB, IIIB,
IIIB | 22.4
monthsa | (20) |
| Kim et al
2014 | 15 | 1 | 3 | 0 | – | – | (21) |
In the present study, the 7 patients with VGPA had
no fertility requirements and exhibited a clinical stage of between
IB1-IIA1; therefore, all the patients underwent a radical
hysterectomy with or without adjuvant therapy. The follow-up time
ranged from 7–57 months, with an average time of 28 months. All
patients were alive with no evidence of recurrence at the time of
writing this study.
In conclusion, VGPA usually occurs in females of
reproductive age. Reproductive and endocrine treatment options are
factors that must be considered in the treatment of affected
patients, while the proposed conservative treatment for these women
allows maintenance of fertility in patients who are young and wish
to have children. However, as the number of studies reporting cases
of VGPA remains small, and as all are retrospective analyses with a
short follow-up time, more prospective randomized controlled trials
are required to confirm the prognosis of the disease. Therefore,
while choosing treatment options for patients with VGPA, data for
disease stage, fertility requirements, follow-up conditions, and
the presence of vascular and lymphatic metastasis should be
integrated, which for a range of aspects, would aid in prudent
decision-making.
Acknowledgements
The present study was supported by grants from the
National Natural Science Foundation of China (nos. 81272875 and
81302242), the Outstanding PhD program of Norman Bethune College of
medicine, Jilin University (no. 2013), the Jilin Science and
Technology Fund (nos. 20110755, 20130102094JC and 20140204022YY)
and the Basic Science Research Fund of Jilin University (no.
20142116).
References
|
1
|
Young RH and Scully RE: Villoglandular
papillary adenocarcinoma of the uterine cervix. A clinicopathologic
analysis of 13 cases. Cancer. 63:1773–1779. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Scully RE, Bonfiglio TA, Kurman RJ,
Silverberg SG and Wilkinson EJ: Uterine cervix. In: Histological
Typing of Female Genital Tract Tumors. World Health Organization
International Histological Classification of Tumors (2nd). (New
York, NY). Springer-Verlag. 1994.
|
|
3
|
Jones MW, Kounelis S, Papadaki H, Bakker
A, Swalsky PA, Woods J and Finkelstein SD: Well-differentiated
villoglandular adenocarcinoma of the uterine cervix: Oncogene/tumor
suppressor gene alterations and human papillomavirus genotyping.
Int J Gynecol Pathol. 19:110–117. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
An HJ, Kim KR, Kim IS, Kim DW, Park MH,
Park IA, Suh KS, Seo EJ, Sung SH, Sohn JH, et al: Prevalence of
human papillomavirus DNA in various histological subtypes of
cervical adenocarcinoma: A population-based study. Mod Pathol.
18:528–534. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Khunamornpong S, Siriaunkgul S and
Suprasert P: Well-differentiated villoglandular adenocarcinoma of
the uterine cervix Cytomorphologic observation of five cases. Diagn
Cytopathol. 26:10–14. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Korach J, Machtinger R, Perri T, Vicus D,
Segal J, Fridman E and Ben-Baruch G: Villoglandular papillary
adenocarcinoma of the uterine cervix: A diagnostic challenge. Acta
Obstet Gynecol Scand. 88:355–358. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pecorelli S: Revised FIGO staging for
carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol
Obstet. 105:103–104. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Heatley MK: Villoglandular adenocarcinoma
of the uterine cervix-a systematic review of the literature.
Histopathology. 51:268–269. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nagai N, Hirata E, Kusuda T, Mukai K,
Arihiro K and Ohama K: Villoglandular papillary adenocarcinoma of
the uterine cervix responding to neoadjuvant chemotherapy with
docetaxel and cisplatin: A case report. Int J Gynecol Cancer.
15:1187–1190. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Macdonald RD, Kirwan J, Hayat K,
Herrington CS and Shawki H: Villoglandular adenocarcinoma of the
cervix: Clarity is needed on the histological definition for this
difficult diagnosis. Gynecol Oncol. 100:192–194. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jones MW, Silverberg SG and Kurman RJ:
Well-differentiated villoglandular adenocarcinoma of the uterine
cervix: A clinicopathological study of 24 cases. Int J Gynecol
Pathol. 12:1–7. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hoffman JS, Bazzurini L, Laird L, Murphy
JC, Magriples U and Lewis J: Term delivery following conservative
treatment for villoglandular papillary adenocarcinoma of the
uterine cervix: Report of a case and analysis of the literature.
Gynecol Oncol. 81:310–313. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dede M, Deveci G, Deveci MS, Yenen MC,
Goktolga U, Dilek S and Gunhan O: Villoglandular papillary
adenocarcinoma of the uterine cervix in a pregnant woman: A case
report and review of literature. Tohoku J Exp Med. 202:305–310.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Falcon O, Garcia R, Lubrano A, Morín JC
and Andujar M: Successful term delivery following conservative
management for villoglandular papillary adenocarcinoma of the
uterine cervix: A case report. Gynecol Oncol. 101:168–171. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yamazawa K, Matsui H, Seki K, Mitsuhashi
A, Kawamata Y, Shirasawa H and Sekiya S: Human
papillomavirus-positive well-differentiated villoglandular
adenocarcinoma of the uterine cervix: A case report and review of
the literature. Gynecol Oncol. 77:473–477. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hurteau JA, Rodriguez GC, Kay HH, Bentley
RC and Clarke-Pearson D: Villoglandular adenocarcinoma of the
cervix: A case report. Obstet Gynecol. 85:906–908. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lavie O, Segev Y, Peer G, Gutterman E,
Sagie S and Auslnader R: Conservative management for villoglandular
papillary adenocarcinoma of the cervix diagnosed during pregnancy
followed by a successful term delivery: A case report and a review
of the literature. Eur J Surg Oncol. 34:606–608. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Takai N, Hayashita C, Nakamura S, Narahara
H and Matsumoto H: A case of villoglandular papillary
adenocarcinoma of the uterine cervix diagnosed during early
pregnancy followed by successful term delivery. Case Rep Med.
2010:3145472010.PubMed/NCBI
|
|
19
|
Kaku T, Kamura T, Shigematsu T, Sakai K,
Nakanami N, Uehira K, Amada S, Kobayashi H, Saito T and Nakano H:
Adenocarcinoma of the uterine cervix with predominantly
villogladular papillary growth pattern. Gynecol Oncol. 64:147–152.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lataifeh IM, Al-Hussaini M, Uzan C,
Jaradat I, Duvillard P and Morice P: Villoglandular papillary
adenocarcinoma of the cervix: A series of 28 cases including two
with lymph node metastasis. Int J Gynecol Cancer. 23:900–905. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kim HJ, Sung JH, Lee E, Ahn S, Song SY,
Choi CH, Kim TJ, Kim BG, Bae DS and Lee JW: Prognostic factors
influencing decisions about surgical treatment of villoglandular
adenocarcinoma of the uterine cervix. Int J Gynecol Cancer.
24:1299–1305. 2014. View Article : Google Scholar : PubMed/NCBI
|