Introduction
Hereditary hemorrhagic telangiectasia (HHT), also
known as Osler-Weber-Rendu disease, is an autosomal dominant
disorder characterized by cutaneous and/or mucosal telangiectasias
and arteriovenous malformations (AVMs), with a prevalence rate of
1–2 patients per 10,000 individuals worldwide (1). HHT is clinically diagnosed using the
Curaçao criteria, which was established in 1999 (2). Approximately 80% of HHT patients exhibit
a mutation in endoglin or activin A receptor-like kinase 1 genes.
Repeated nosebleeds due to the mucosal telangiectasias are the most
common somatic symptom and present a major HHT-related health
concern that affects patient quality of life (3). At present, an optimal treatment strategy
for HHT has not yet been established. However, in patients that
exhibit severe bleeding, infection and hypoxia, surgery is usually
required (3,4). The prognosis of HHT patients depends on
the presence of the infection associated with AVMs, including organ
abscesses and sepsis (1). Notably,
the mean lifespan of HHT patients has been found to be shortened
when compared with controls (63.2 vs. 70.0 years) (4). To date, only a few cases of tumors
arising in the small bowel have been reported (5,6). In this
study, the first case of a patient with HHT to develop cancer of
the jejunum following surgical removal of multiple colonic adenomas
is presented.
Case report
A 32-year-old female underwent a
laparoscopy-assisted ileocecal resection for multiple polyps in the
cecum and appendix veriforme at the University of Tokyo Hospital,
(Tokyo, Japan), as reported in a previous study (7). The patient was subsequently diagnosed
with HHT. Five years later, she visited a local practitioner
complaining of appetite loss which had lasted for two months,
recent abdominal pain, and intermittent vomiting. Shortly
thereafter, the patient was referred back to the University of
Tokyo Hospital to receive treatment for obstructive ileus, which
was managed by intravenous hydration without oral intake. A
decompression tube was not inserted through the nose in order to
avoid nosebleeds.
Laboratory examinations performed on admission
revealed normal findings, with the exception of anemia (hemoglobin,
8.3 g/dl) and malnutrition (serum protein, 4.7 g/dl; albumin, 2.3
g/dl). Progressive anemia due to frequent nosebleeds and melena
originating from the tumor necessitated a blood transfusion prior
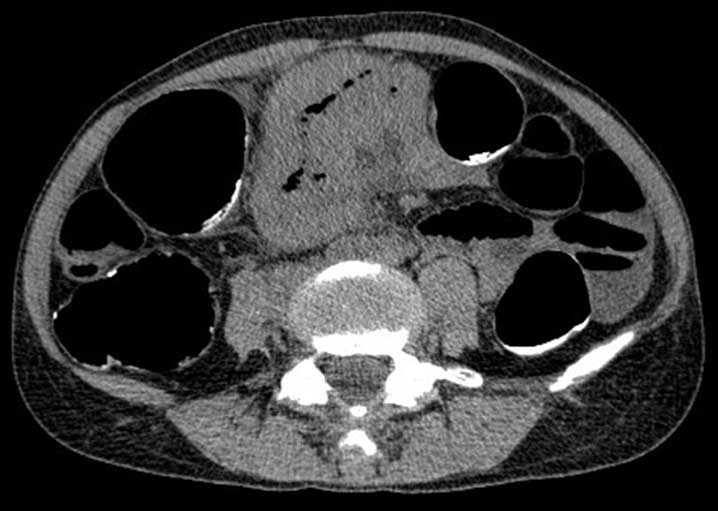
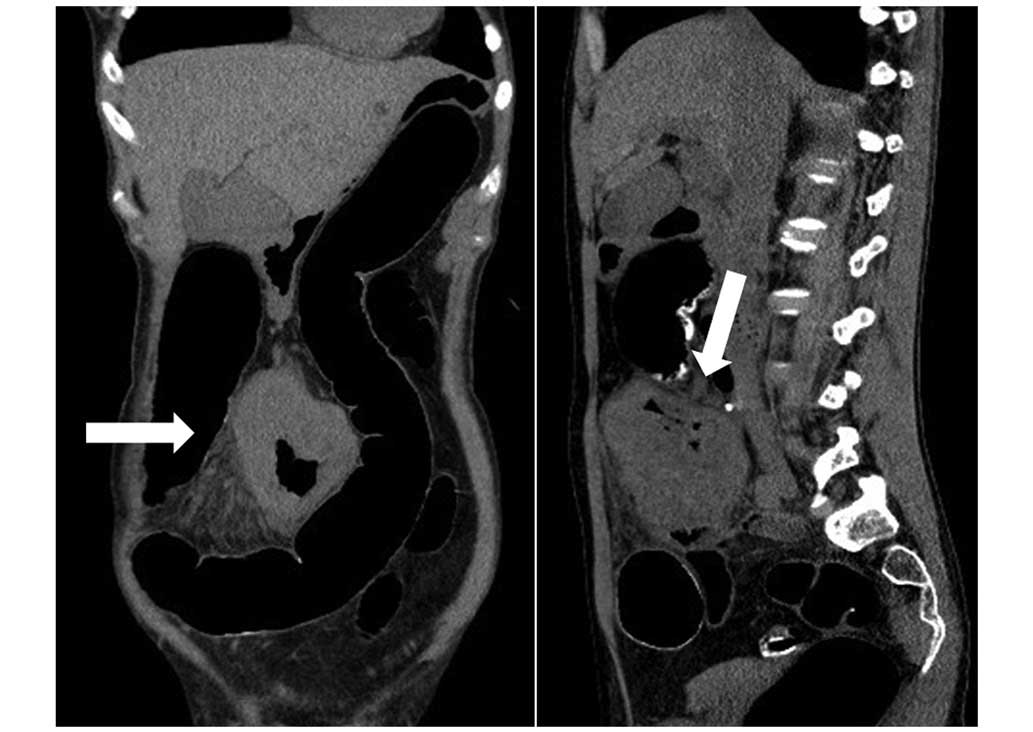
to surgery. An abdominal computed tomography (CT) scan revealed a
small bowel tumor, ~10 cm in diameter, directly behind the
transverse mesocolon (Figs. 1 and
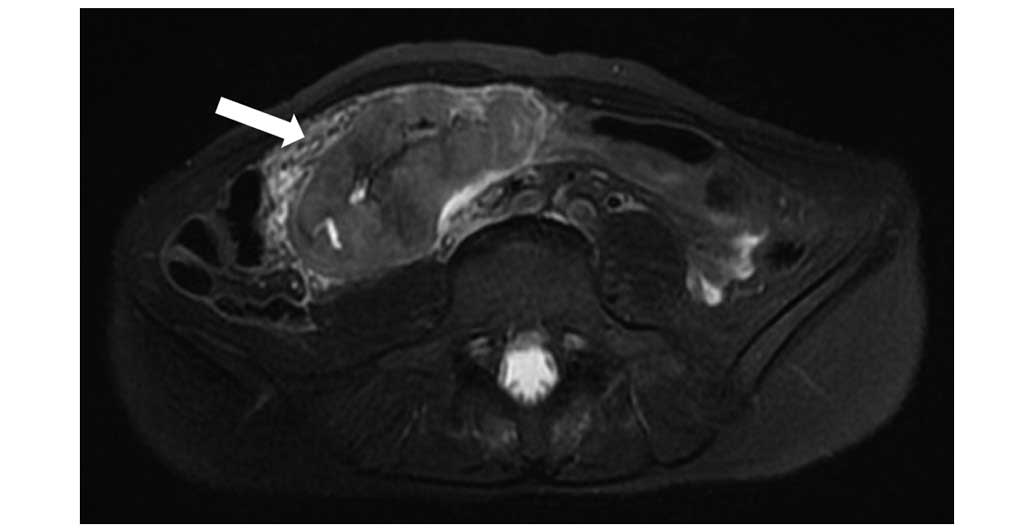
2). Magnetic resonance imaging
revealed a tumor whose border was highly enhanced by contrast and
which demonstrated high intensity in diffusion-weighted imaging
(Fig. 3). Positron emission CT
revealed a maximum standardized uptake value of 14.9 in the lesion,
suggestive of a malignant tumor. No distant organ metastasis was
demonstrated (image not shown).
The patient experienced loss of consciousness twice
when the infusion bag for hyper-alimentation was changed, which was
accessed from the right internal jugular vein. Image studies of the
patient's head did not reveal significant ischemic changes or
metastatic lesions. Considering the presence of arteriovenous
fistulas in the patient's lungs (7),
it was notable that micro air bubbles from the infusion line had
passed through the shunts to the cerebral arteries, causing
transient ischemic attack. The patient was free from ischemic
episodes after stopping central vein hyper-alimentation.
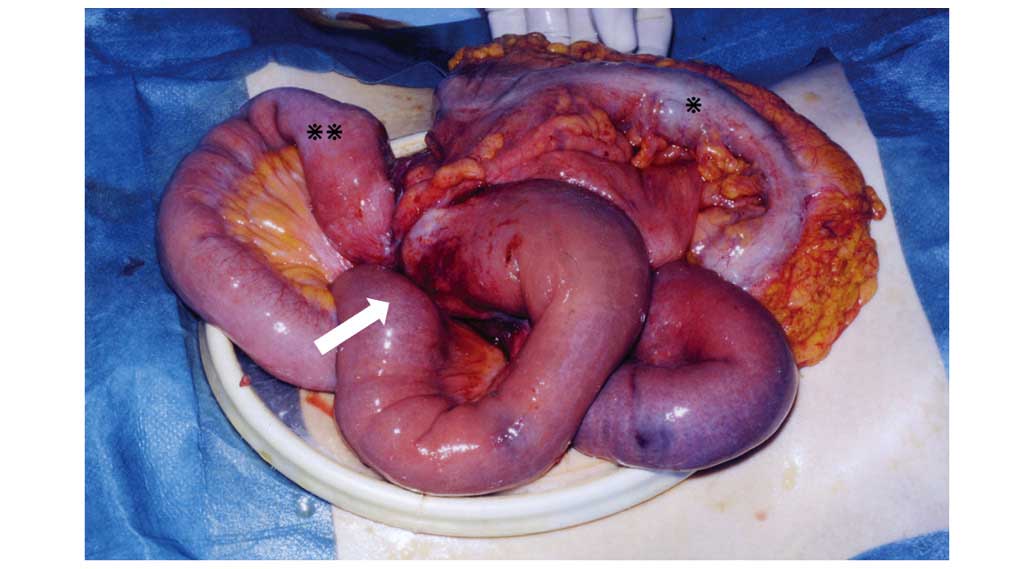
Resection of the tumor-bearing segment of the
jejunum (30 cm from the Treitz ligament) as well as right
hemicolectomy was performed since the tumor had invaded the
terminal ileum as well as the mesenterium of the transverse colon
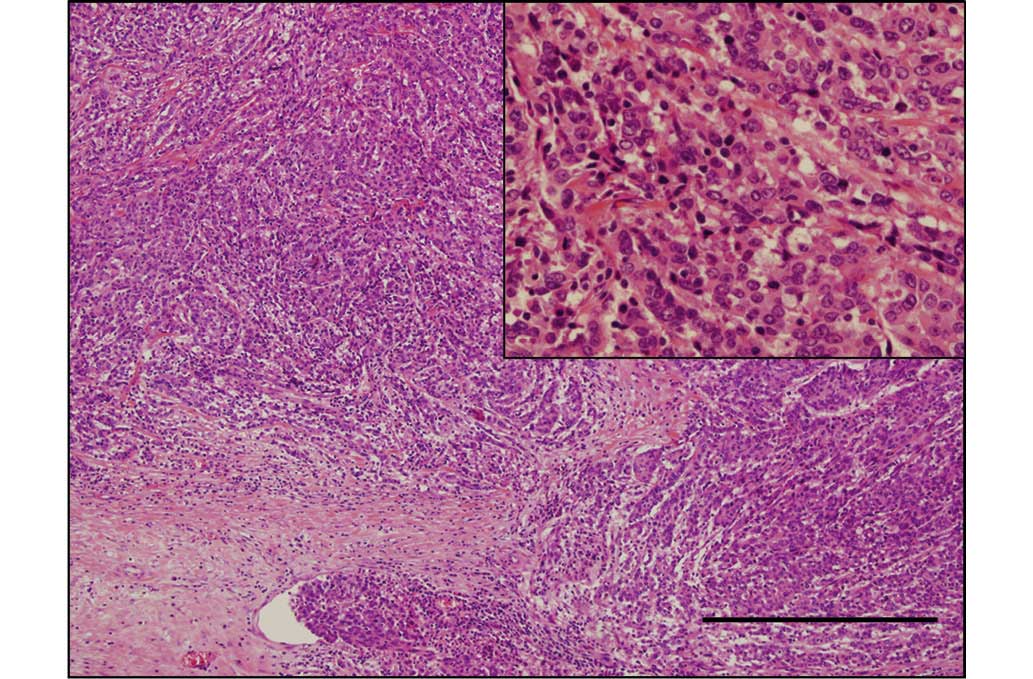
(Fig. 4). The resected specimen was
histologically diagnosed as poorly differentiated adenocarcinoma
(Fig. 5) with prominent lymphatic and
venous infiltration. One of the twelve regional lymph nodes
dissected was affected by cancer.
In addition to epistaxis, the patient experienced
wound infection postoperatively, which could be treated
conservatively. Her postoperative recovery was otherwise
uneventful. She received an intravenous infusion of oxaliplatin
(123 mg/m2) on day 1 plus oral capecitabine (920
mg/m2) (CapeOx) twice daily for 2 weeks in a 3-week
cycle as adjuvant chemotherapy for 6 months (a total of 8 cycles);
chemotherapy-related peripheral neurotoxicity and neutropenia could
be managed. Due to severe neuropathy the dosage of oxaliplatin was
reduced by 20% for the final two cycles. The patient is currently
alive without evidence of recurrence 12 months after the surgery.
Written informed consent was obtained from the patient for
publication of the present study.
Discussion
Small bowel adenocarcinomas (SBAs) account for
<5% of gastrointestinal cancers worldwide (8). Genetic predisposition to SBAs has been
indicated; patients with familial adenomatous polyposis, Lynch
syndrome and Peutz-Jeghers syndrome have a relatively higher risk
of SBA than the general population, suggesting genetic alterations
predisposed to cancer development (9).
Genetic analyses have revealed that abnormalities in
endoglin family genes cause HHT (10). In an in vivo experiment, the
overexpression of endoglins in prostate cancer cells revealed
growth-inhibiting effects on tumor cells (11–14).
However, other animal studies have revealed that protein promotes
angiogenesis in a tumor microenvironment, causing accelerated
metastasis (15). Therefore, it is an
interesting question of whether HHT manifests cancer-prone
phenotypes or not. A clinical observational study demonstrated that
reduced endoglin expression in HHT is associated with a lower
frequency of common malignancies, including lung, prostate and
colorectal cancer, and a more favorable cancer-specific survival
(10). Based on these findings, the
current patient's case is rare. To the best of our knowledge, this
is the first HHT patient to develop cancer of the small intestine,
excluding the duodenum (5).
The current case illustrates several significant
points in the perioperative care of patients with HHT. First, in
the surgical treatment of a gastrointestinal malignancy, frequent
nosebleeds may hinder the appropriate management of a possible
perioperative ileus since the insertion of a nasogastric or long
tube may exacerbate anemia. In addition, the existence of an
arteriovenous shunt easily causes an arterial embolism during
intravenous infusion, particularly when using the central vein. In
the current case, significant infarction was avoided by switching
to peripheral vein nutrition. Therefore, special management is
required for HHT patients who undergo gastrointestinal surgery.
In general, SBA exhibits a poor prognosis (9). In addition, poorly differentiated
adenocarcinoma, as in the current case, is one of the predictors of
poor outcome (8). There have been
only a limited number of studies on the subject of adjuvant
chemotherapy for SBAs, most of which are retrospective (16,17).
Similarly, the majority of published studies pertaining to
palliative chemotherapy for advanced SBAs are retrospective and
limited in number. The best outcome was a median overall survival
of 20 months achieved in a phase II trial of CapeOx in patients
with advanced SBAs (18). Adjuvant
CapeOx treatment was selected in the current case based on the
results of the above-mentioned study as well as by extrapolating
from relapse-preventing effects of CapeOx for colon cancer
(19). Furthermore, CapeOx is
advantageous in terms of minimizing the infusion time of
chemotherapeutic drugs, and appears to be an ideal regimen for
cancer patients with HHT.
In conclusion, the present study reported the case
of an HHT patient diagnosed with jejunum cancer, an extremely
uncommon condition according to epidemiological studies. This study
shows that HHT is a disorder that may cause clinically significant
complications due to peripheral artery dilatation and arteriovenous
malformation, thereby suggesting the necessity of cautious
management during perioperative care.
Glossary
Abbreviations
Abbreviations:
|
HHT
|
hereditary hemorrhagic
telangiectasia
|
|
CT
|
computed tomography
|
|
SBA
|
small bowel adenocarcinoma
|
|
FAP
|
familial adenomatous polyposis
|
References
|
1
|
Guttmacher AE, Marchuk DA and White RI Jr:
Hereditary hemorrhagic telangiectasia. N Engl J Med. 333:918–924.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Shovlin CL, Guttmacher AE, Buscarini E,
Faughnan ME, Hyland RH, Westermann CJ, Kjeldsen AD and Plauchu H:
Diagnostic criteria for hereditary hemorrhagic telangiectasia
(Rendu-Osler-Weber syndrome). Am J Med Genet. 91:66–67. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Arthur H, Geisthoff U, Gossage JR, Hughes
CC, Lacombe P, Meek ME, Oh P, Roman BL, Trerotola SO, Velthuis S
and Wooderchak-Donahue W: Executive summary of the 11th HHT
international scientific conference. Angiogenesis. 18:511–524.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sabbà C, Pasculli G, Suppressa P, D'Ovidio
F, Lenato GM, Resta F, Assennato G and Guanti G: Life expectancy in
patients with hereditary haemorrhagic telangiectasia. QJM.
99:327–334. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Korzenik J, Chung DC, Digumarthy S and
Badizadegan K: Case records of the Massachusetts General Hospital.
Case 33–2005. A 43-year-old man with lower gastrointestinal
bleeding. N Engl J Med. 353:1836–1844. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kato S and Ichihara K: Hereditary
hemorrhagic telangiectasia with malignant lymphoma. An autopsy
case. Acta Pathol Jpn. 38:383–391. 1988.PubMed/NCBI
|
|
7
|
Kaneko M, Nozawa H, Kitayama J, Sunami E,
Akahane M, Yamauchi N, Furukawa Y and Nagawa H: A case of
hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu disease)
with multiple polyps arising in the cecum and appendix. Acta
Gastroenterol Belg. 74:352–354. 2011.PubMed/NCBI
|
|
8
|
Neugut AI, Jacobson JS, Suh S, Mukherjee R
and Arber N: The epidemiology of cancer of the small bowel. Cancer
Epidemiol Biomarkers Prev. 7:243–251. 1998.PubMed/NCBI
|
|
9
|
Aparicio T, Zaanan A, Svrcek M,
Laurent-Puig P, Carrere N, Manfredi S, Locher C and Afchain P:
Small bowel adenocarcinoma: epidemiology, risk factors, diagnosis
and treatment. Dig Liver Dis. 46:97–104. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Duarte CW, Murray K, Lucas FL, Fairfield
K, Miller H, Brooks P and Vary CP: Improved survival outcomes in
cancer patients with hereditary hemorrhagic telangiectasia. Cancer
Epidemiol Biomarkers Prev. 23:117–125. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liu Y, Jovanovic B, Pins M, Lee C and
Bergan RC: Over expression of endoglin in human prostate cancer
suppresses cell detachment, migration and invasion. Oncogene.
21:8272–8281. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lakshman M, Huang X, Ananthanarayanan V,
Jovanovic B, Liu Y, Craft CS, Romero D, Vary CP and Bergan RC:
Endoglin suppresses human prostate cancer metastasis. Clin Exp
Metastasis. 28:39–53. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Craft CS, Romero D, Vary CP and Bergan RC:
Endoglin inhibits prostate cancer motility via activation of the
ALK2-Smad1 pathway. Oncogene. 26:7240–7250. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Romero D, Terzic A, Conley BA, Craft CS,
Jovanovic B, Bergan RC and Vary CP: Endoglin phosphorylation by
ALK2 contributes to the regulation of prostate cancer cell
migration. Carcinogenesis. 31:359–366. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Romero D, O'Neill C, Terzic A, Contois L,
Young K, Comley BA, Bergan RC, Brooks PC and Vary CP: Endoglin
regulates cancer-stromal cell interactions in prostate tumors.
Cancer Res. 71:3482–3493. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Koo DH, Yun SC, Hong YS, Ryu MH, Lee JL,
Chang HM, Kang YK, Kim SC, Han DJ, Lee YJ and Kim TW: Adjuvant
chemotherapy for small bowel adenocarcinoma after curative surgery.
Oncology. 80:208–213. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Overman MJ, Lopetz S, Lin E, Abbruzzese JL
and Wolff RA: Is there a role for adjuvant therapy in resected
adenocarcinoma of the small intestine. Acta Oncol. 49:474–479.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Overman MJ, Varadhachary GR, Kopetz S,
Adinin R, Lin E, Morris JS, Eng C, Abbruzzese JL and Wolff RA:
Phase II study of capecitabine and oxaliplatin for advanced
adenocarcinoma of the small bowel and ampulla of vater. J Clin
Oncol. 27:2598–2603. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Haller DG, Tabernero J, Maroun J, de Braud
F, Price T, Van Cutsem E, Hill M, Gilberg F, Rittweger K and
Schmoll HJ: Capecitabine plus oxaliplatin compared with
fluorouracil and folinic acid as adjuvant therapy for stage III
colon cancer. J Clin Oncol. 29:1465–1471. 2011. View Article : Google Scholar : PubMed/NCBI
|