Introduction
Gastrointestinal stromal tumor (GIST) is the most
common mesenchymal neoplasm of the gastrointestinal tract and is
defined by the expression of the mast/stem cell growth factor
receptor, also termed cluster of differentiation (CD)117, a
tyrosine kinase growth factor receptor (1). The incidence of GIST is estimated to be
14–20 cases per million population. The most common site of GIST
involvement is the stomach, followed by the small intestine
(2). It is rarely located in
extra-gastrointestinal sites, such as the omentum and mesentery.
Tumors located in these regions are known as extra-gastrointestinal
stromal tumors (3). The peak
incidence of GIST is in adulthood (median age, 63 years) with no
evident gender predilection (4). GIST
may vary considerably in size and tumors >10 cm in size are
considered to be giant GISTs. GISTs >5 cm in size with ≥10
mitotic cells per 50 high-power fields (10/50 HPF) may become
malignant and are considered to be high-risk tumors (5). The incidence of GIST is estimated to be
<20 cases per million population (6). The standard treatment for GIST is
surgery with a complete resection of the tumor. The prognosis is
strictly associated with the size of the tumor and the completeness
of the surgical resection.
Case report
A 66-year-old man that presented with metastatic
pain in the right lower quadrant was admitted to the Clinical
Medical College of Yangtze University (Jingzhou, Hubei, China) in
February 2013. Ultrasound and computed tomography (CT) scans
revealed a large mass in the lower abdominal and pelvic cavity.
Histopathological examination suggested a diagnosis of spindle cell
tumor. Following an initial improvement in the clinical symptoms,
the patient discontinued the treatment regimen (imatnib, 400 mg/d).
Subsequent to discontinuation of medication, the patient
experienced enlargement of the abdomen, emaciation, fever,
hyperhidrosis and frequent and urgent micturition. The patient was
re-admitted to hospital in May 2014. Clinical examination revealed
that the abdomen was soft and enlarged with superficial abdominal
varicose veins. A large mass was palpated that covered the entire
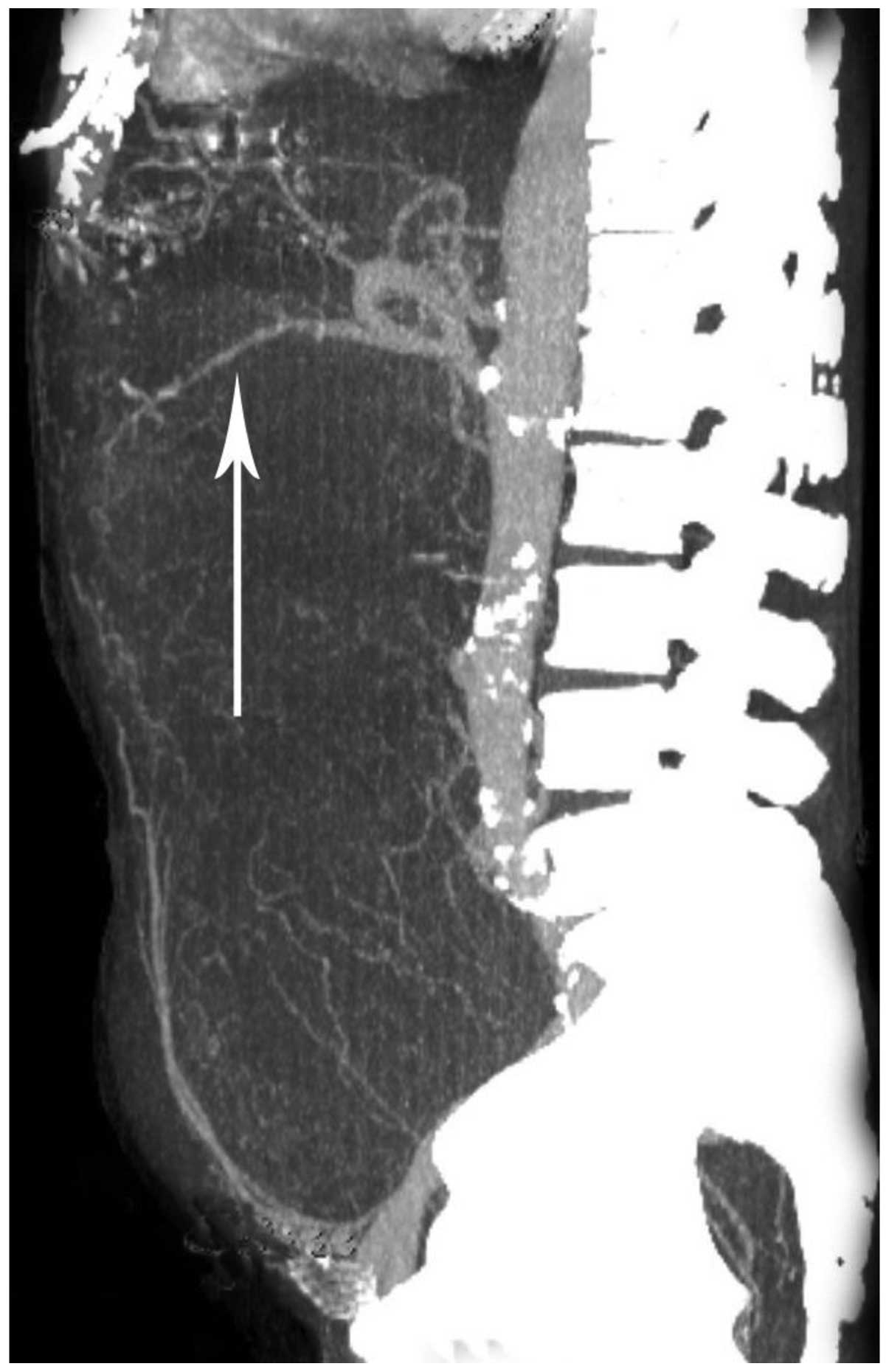
abdomen. The liver and spleen were not palpable. A CT scan revealed
the presence of a large soft tissue mass, which occupied almost the
entire abdomino-pelvic cavity (Fig.
1), and measured 34×19.1×28.6 cm in size. The intestines were
observed to be gathered at the back of the abdominal cavity, and a
large segment of the bowel was embedded inside the mass. The mass
was heterogeneous and possessed a slightly lower density than the
liver. Certain strip-like lower density areas were also observed
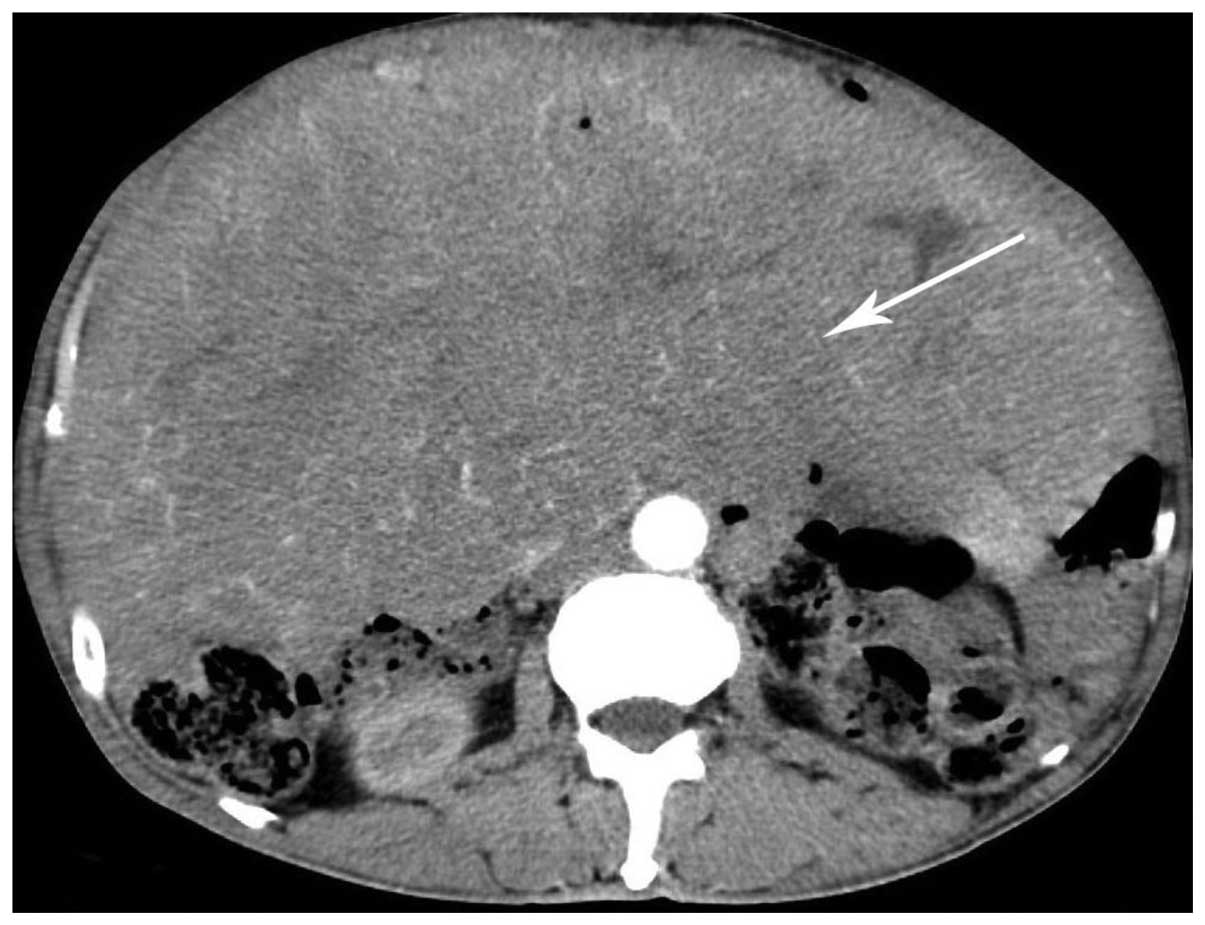
within the mass. The boundary of the mass was defined. A contrast
enhanced CT scan demonstrated that the mass was slightly enhanced,
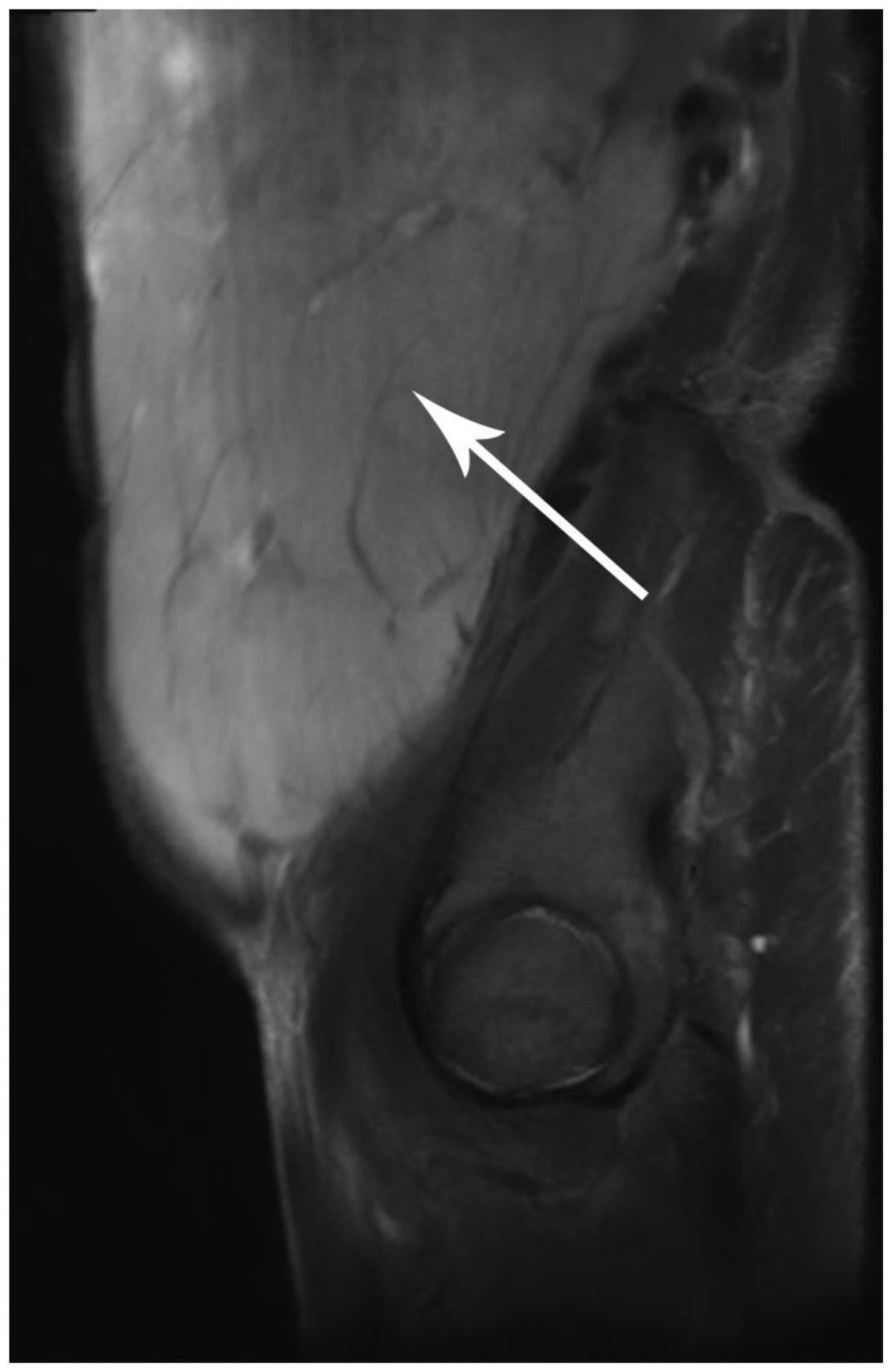
with numerous serpiginous small vessels within the mass (Fig. 2). A computed tomography angiography
scan revealed that the mass was supplied by the mesenteric artery
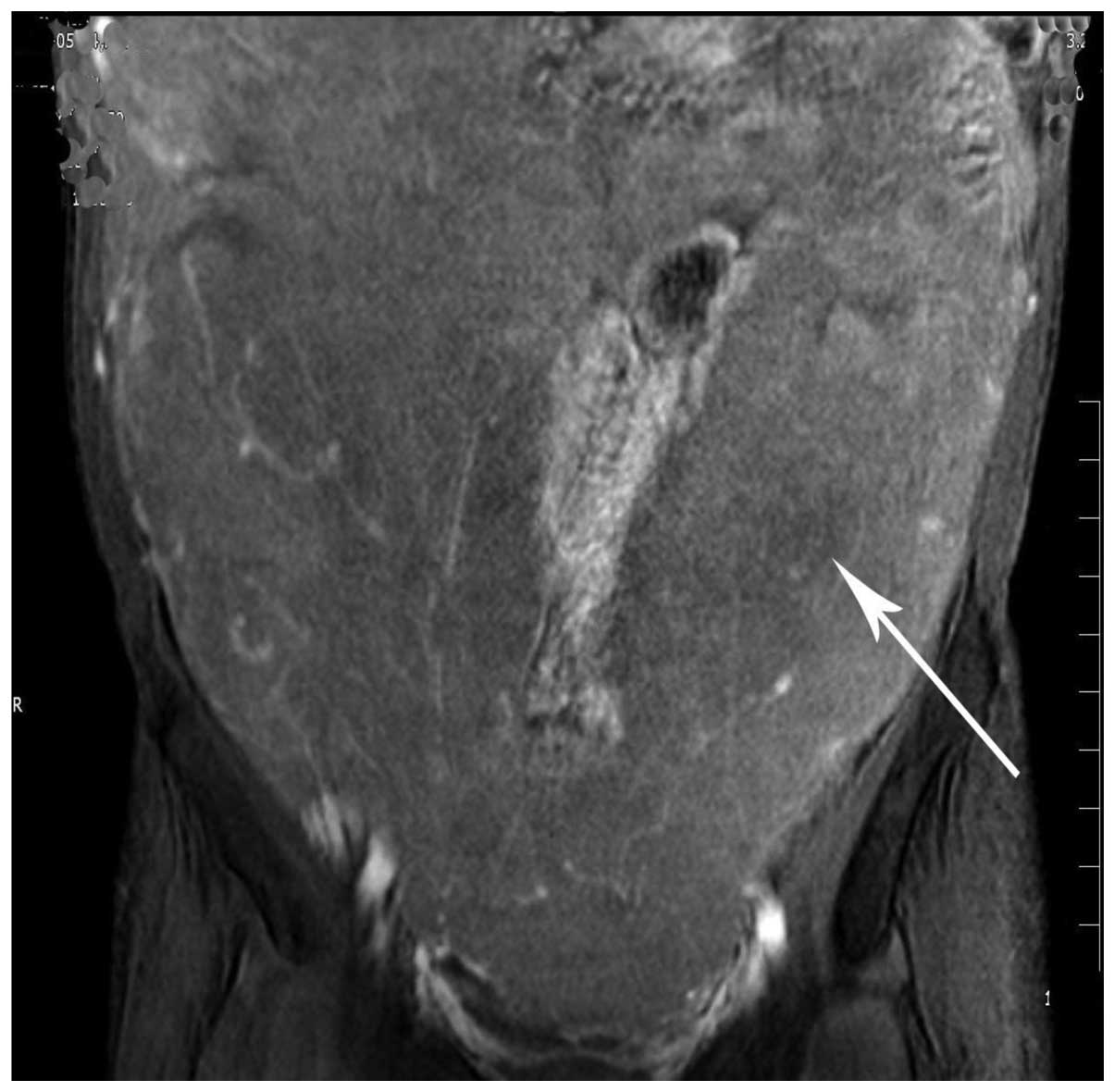
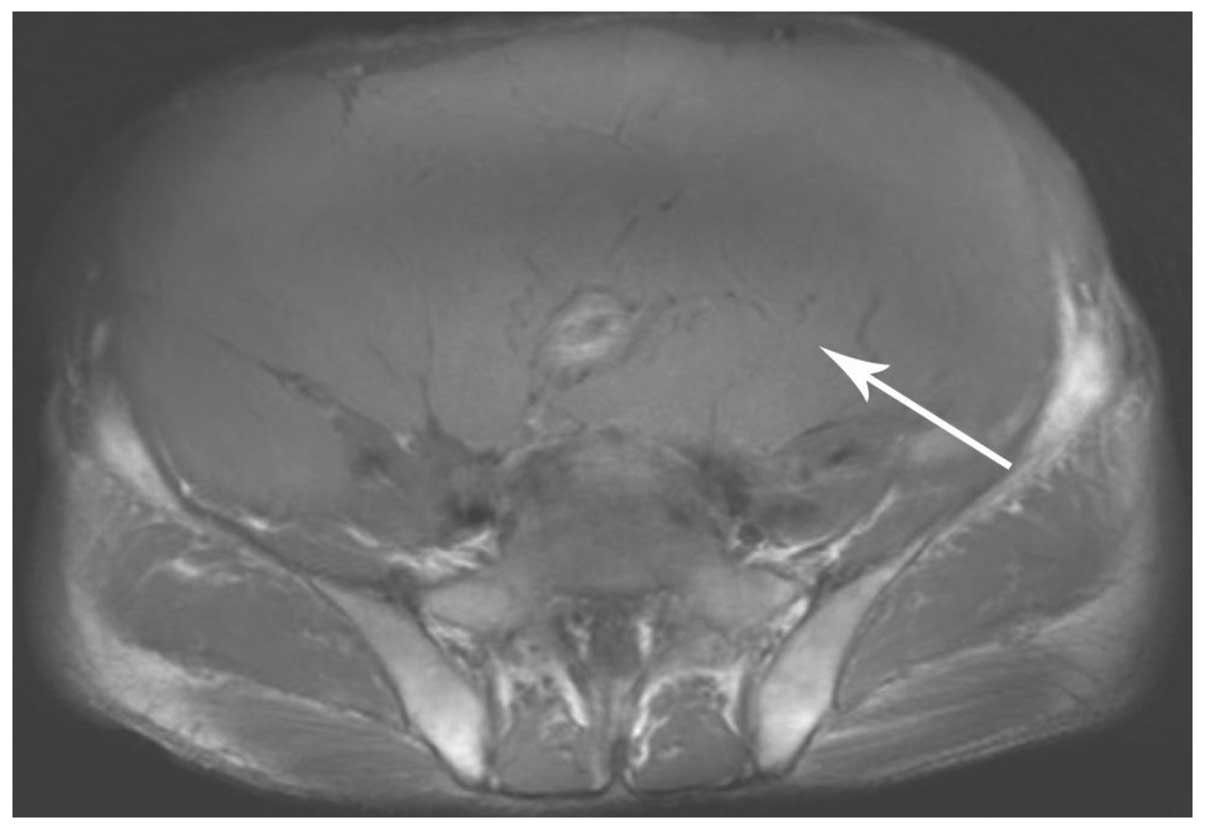
(Fig. 3). A magnetic resonance
imaging (MRI) scan revealed that the tumor possessed an equal
signal on the T1 weighted image and a high signal on the T2
weighted image (Figs. 4 and 5). The enhancement pattern of the mass was
similar between the MRI and CT scans (Fig. 6).
The CT and MRI results lead to a diagnosis of giant
abdomino-pelvic hypervascular tumor. Following a biopsy, the
diagnosis was altered to abdominal spindle cell tumor.
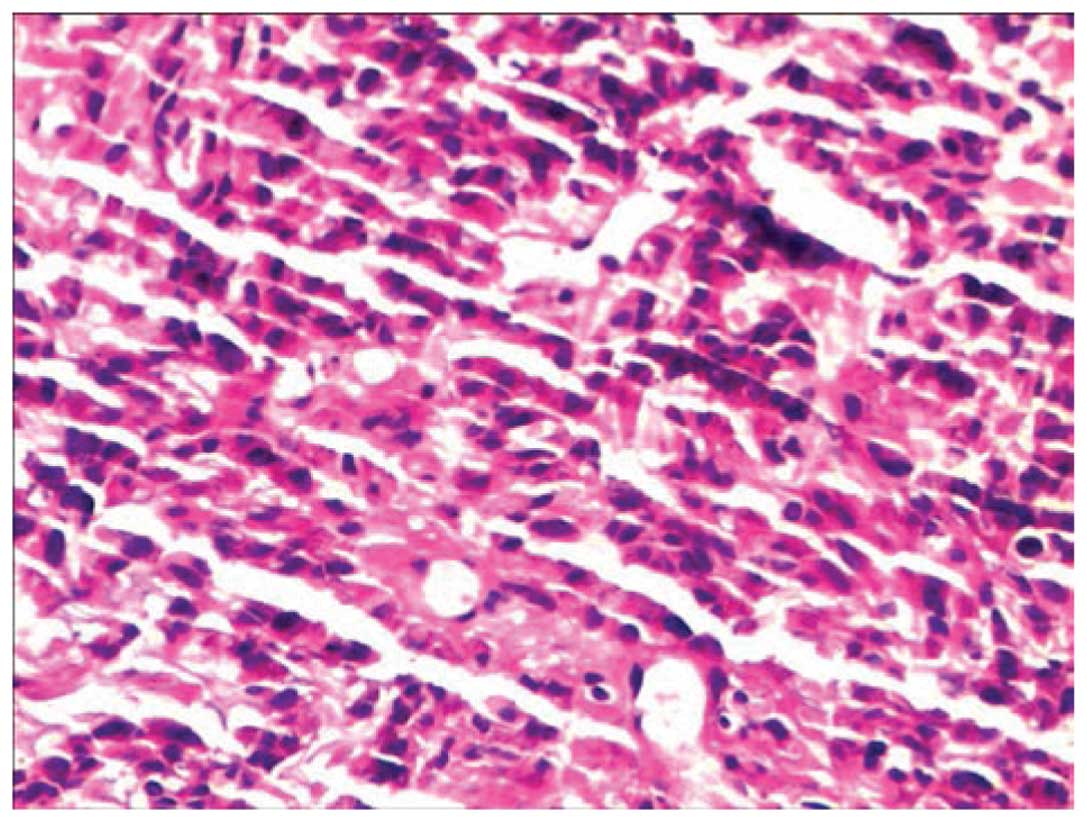
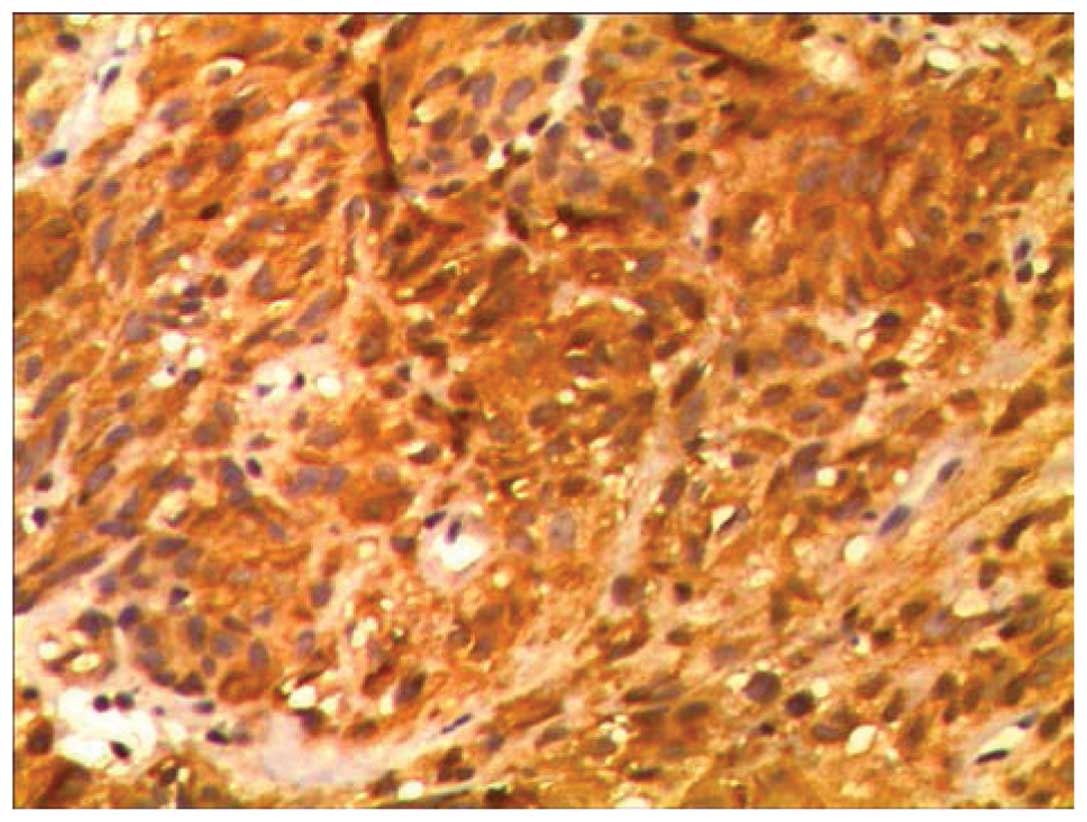
Immunohistochemical tests were performed, the results of which were
as follows: Expression of CD117, discovered on GIST-1, smooth
muscle actin, human melanoma black 45; partial expression of
protein S-100; no expression of cluster of differentiation-34,
pancytokeratin, melanoma antigen and C-reactive protein; and a Ki67
index of 5–10% (Figs. 7 and 8). A mitosis count of <5/50 HPF was
observed. Overall, the results from the clinical and
immunohistochemical tests lead to a final diagnosis of high-risk
GIST. The final surgical results confirmed these findings.
Following conservative treatment with imatnib (400 mg, daily) for 6
months, the tumor became smaller and was suitable for surgery,
which the patient received in December 2014. The final surgery
confirmed the high-risk GIST. Subsequent to the surgery, the
patient was recommended to continue the use of imatnib and receives
regular CT or MRI reexaminations every 3 months, which are planned
to continue for 3 years.
Discussion
GISTs are rare mesenchymal tumors that arise
predominantly in the gastrointestinal tract, and may occur at any
location between the esophagus and the rectum (7). The most common regions of the
gastrointestinal tract affected are the stomach (60%) and small
intestine (30%) (8,9). In total, >90% of GISTs occur in
adults >40 years old (median age, 63 years); however, GISTs have
been identified in all age groups, including children (10). The majority of GISTs remain
asymptomatic until they have reached a large size (11). Symptoms vary according to location and
size of the tumor, and patients generally present with non-specific
symptoms, such as abdominal pain, fatigue, dyspepsia, nausea,
anorexia, weight loss, fever and obstruction of the intestines
(12). GIST may be classified into
five categories, according to the growth pattern of the tumor. The
categories consist of the cross-wall, internal-wall, external-wall,
intracavity and extra-gastrointestinal tract types (13). GISTs range in size of diameter between
a few millimeters and >30 cm (14). When the size of the mass measures
>10 cm, the GIST is referred to as giant GIST (15,16). The
risk of malignancy of GISTs varies between very low and high based
on the mitotic rate and size; GISTs >5 cm with a mitotic rate of
>5/50 HPF are considered to be high-risk tumors (8). The risk of malignancy is calculated
according to the modified National Institutes of Health criteria
(17), which classifies GIST tumors
into 4 categories: Extremely low, low, intermediate and high-risk
(18).
Multislice spiral computer tomography (MCST) is
considered to be the optimal imaging method for the detection of
GISTs (19). On CT and MRI, GISTs
appear as large heterogeneous masses with areas of low attenuation
from hemorrhage, necrosis or cyst formation. Severe hemorrhage and
calcification within the mass is occasionally revealed, but
lymphadenopathy is not a common finding. A malignant stromal tumor
is observed on a CT scan as a mass >5 cm, possessing a lobulated
contour and heterogeneity, with central necrosis or liquefaction,
mesenteric infiltration, regional lymphadenopathy and exophytic
growth. GISTs demonstrate conspicuous uniform or non-uniform
enhancement on a contrast-enhanced scan. GISTs may be composed of
thin, elongated spindle cells or plumper epithelioid cells. The
most useful diagnostic marker for GIST is CD117, a cell-surface
transmembrane tyrosine kinase, also known as c-Kit, which is
immunohistochemically detectable in 95% of GISTs (20).
The current patient presented with characteristic
features of GIST, which is demonstrated by the clinical features of
the patient, CT and MRI imaging, biopsy findings and
immunohistochemical staining. The mass was large and occupied
almost the entire abdominal and pelvic cavity. No association
between the mass and the adjacent gastrointestinal structure was
observed on the CT scan. As the mass was large and did not exhibit
any symptoms of intestinal obstruction, it was concluded that the
mass was extra-gastrointestinal in origin. In addition, the mass
was a hypervascular tumor, as certain tortuous enhanced vessels
were observed within the mass in a contrast-enhanced CT scan.
However, the tumor parenchyma did not clearly enhance in every
stage of the contrast enhanced scan. Therefore, whether this
inconsistent appearance is a characteristic feature of GIST
requires clarification by additional studies of patients with
similar characterisitcs to the present patient.
References
|
1
|
Novelli M, Rossi S, Rodriguez-Justo M,
Taniere P, Seddon B, Toffolatti L, Sartor C, Hogendoorn PC, Sciot
R, Van Glabbeke M, et al: DOG1 and CD117 are the antibodies of
choice in the diagnosis of gastrointestinal stromal tumours.
Histopathology. 57:259–270. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Su YY, Chiang NJ, Wu CC and Chen LT:
Primary gastrointestinal stromal tumor of the liver in an anorectal
melanoma survivor: A case report. Oncol Lett. 10:2366–2370.
2015.PubMed/NCBI
|
|
3
|
Bár T, Sankot J, Adamová Z and Mičulka P:
Extraintestinal GIST - case report. Rozhl Chir. 94:383–386.
2015.(In Czech). PubMed/NCBI
|
|
4
|
Suryawanshi KH, Patil TB, Damle RP, Dravid
NV and Surana A: Gastrointestinal stromal tumour of small intestine
presenting as a mesenteric mass. J Clin Diagn Res. 8:FD14–FD16.
2014.PubMed/NCBI
|
|
5
|
Sashidharan P, Matele A, Matele U, Al
Felahi N and Kassem KF: Gastrointestinal stromal tumors: A case
report. Oman Med J. 29:138–141. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Liang X, Yu H, Zhu LH, Wang XF and Cai XJ:
Gastrointestinal stromal tumors of the duodenum: Surgical
management and survival results. World J Gastroenterol.
19:6000–6010. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Salari M, Ahadi M, Hoseini SM, Mokhtari E,
Gafarzadehgan K, Hashemian HR, Esmaeili B and Vossoughinia H:
Gastrointestinal Stromal Tumors in Northeastern Iran: 46 Cases
During 2003-2012. Middle East J Dig Dis. 7:161–165. 2015.PubMed/NCBI
|
|
8
|
Rammohan A, Sathyanesan J, Rajendran K,
Pitchaimuthu A, Perumal SK, Srinivasan U, Ramasamy R, Palaniappan R
and Govindan M: A gist of gastrointestinal stromal tumors: A
review. World J Gastrointest Oncol. 5:102–112. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Antonopoulos P, Leonardou P, Barbagiannis
N, Alexiou K, Demonakou M and Economou N: Gastrointestinal and
extragastrointestinal stromal tumors: Report of two cases and
review of the literature. Case Rep Gastroenterol. 8:61–66. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Stamatakos M, Douzinas E, Stefanaki C,
Safioleas P, Polyzou E, Levidou G and Safioleas M: Gastrointestinal
stromal tumor. World J Surg Oncol. 7:61–70. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sorour MA, Kassem MI, Ghazal A-H,
El-Riwini MT and Abu Nasr A: Gastrointestinal stromal tumors (GIST)
related emergencies. Int J Surg. 12:269–280. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhao X and Yue C: Gastrointestinal stromal
tumor. J Gastrointest Oncol. 3:189–208. 2012.PubMed/NCBI
|
|
13
|
Beham AW, Schaefer I-M, Schüler P, Cameron
S and Ghadimi BM: Gastrointestinal stromal tumors. Int J Colorectal
Dis. 27:689–700. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Giuliani J and Bonetti A: The occurrence
of gastrointestinal stromal tumors and second malignancies. J
Gastrointest Cancer. 46:408–412. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gerrish ST and Smith JW: Gastrointestinal
stromal tumors - diagnosis and management: A brief review. Ochsner
J. 8:197–204. 2008.PubMed/NCBI
|
|
16
|
Dickhoff C, Leguit RJ, Slors JF, Vervenne
WL and Bemelman WA: Giant rectal gastrointestinal stromal tumors: A
report of two cases. Case Rep Gastroenterol. 2:54–69. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
de Oliveira RP, Portari Filho PE, Iglesias
AC, de Oliveira CA and Pannain VL: Comparative study of the
different degrees of risk of gastrointestinal stromal tumor. Rev
Col Bras Cir. 42:32–36. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhao WY, Xu J, Wang M, Zhang ZZ, Tu L,
Wang CJ, Cao H and Zhang ZG: Evaluation of high-risk
clinicopathological indicators in gastrointestinal stromal tumors
for prognosis and imatinib treatment outcome. BMC Gastroenterol.
14:105–113. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cai PQ, Lv XF, Tian L, Luo ZP, Mitteer RA
Jr, Fan Y and Wu YP: CT characterization of duodenal
gastrointestinal stromal tumors. AJR Am J Roentgenol. 204:988–993.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Serrano C and George S: Recent advances in
the treatment of gastrointestinal stromal tumors. Ther Adv Med
Oncol. 6:115–127. 2014. View Article : Google Scholar : PubMed/NCBI
|