Sex determining region Y-box 2 (SOX2) is a
transcription factor that is involved in the maintenance of
embryonic stem cell pluripotency and in multiple developmental
processes (1,2). Increasing numbers of studies regarding
the association between SOX2 and malignant tumors have been
reported. Numerous studies have indicated that SOX2 is involved in
in tumorigenesis, including in skin squamous cell carcinoma,
gastric cancer, glioblastoma, colorectal cancer, lung cancer and
breast cancer (3–8). SOX2 has demonstrated a pro-oncogenic
function in the majority of the various types of malignant tumor,
including breast, colorectal and lung cancer and glioblastoma, but
not gastric cancer. The expression of SOX2 in oral squamous cell
carcinomas (OSCC) has also been reported, and SOX2 nuclear
expression is closely associated with a poor prognosis in oral
tongue squamous cell carcinoma (OTSCC) (9). In addition, the increased expression of
SOX2 in OSCC is associated with lymph node metastasis (10).
Oral cancer is a growing problem in the world and
demonstrates a high prevalence among men in Asia, particularly in
India, as oral cancer is the most prevalent type of cancer in
Indian men (11–13). The overall 5-year survival rate of
patients following a surgical resection or other treatment has not
markedly improved during the past three decades, and remains at
~50% (14). The presence of lymph
node metastasis is considered to be an important indicator of
predicting an adverse outcome (15,16).
However, certain OSCC patients that do not possess node metastasis
continue to suffer from tumor relapses subsequent to complete
surgical resections, and then poor prognoses (9,17). Novel
treatment strategies are required. In previous studies, SOX2 has
been indicated to act as a prognostic factor in various types of
tumors and as a link between malignancy and stemness (3,18,19). Novel studies indicate that cancer stem
cells (CSCs) may be responsible for the genesis, growth and
metastatic spread of the tumor (20,21). The
poor survival outcomes for OSCC patients may be attributable to a
poor selection of target cells for treatment, as current oral
cancer therapies are generally aimed at the overall mass of the
tumor. Therefore, the consideration that novel approaches to oral
cancer may be targeted using SOX2 and CSCs appears reasonable.
In order to better understand the oncogenic roles
and corresponding signal transduction pathways of the SOX2 protein,
the present study emphasizes the role of SOX2 and the associated
proteins in OSCC, and reviews the literature on the role of SOX2 in
lymph node metastasis. The aim of the present study is to provide a
reference for future studies that engage in research on the
aforementioned subject.
SOX2 is an amplified gene in OSCC, which is
established as one of the hallmark participants throughout the
developmental process in cancer. SOX2 is mainly expressed in CSCs.
In order to study the role of SOX2 in OSCC, the concept and
identification of CSC must be understood.
The major characteristic that defines stem cells is
self-renewal, whereby stem cells result in numerous types of mature
cells and lead to organogenesis (22). Similar cells that exist in cancer,
termed CSCs, have been previously documented (22). In addition to the ability to
self-renew, CSCs may result in phenotypically varied tumor cell
populations through a process of aberrant differentiation. CSCs
may, therefore, be responsible for driving tumorigenesis and tumor
growth. The theory that tumorigenesis is based exclusively on the
aberrant activity of CSCs derives from the heterogeneous nature of
OSCCs and other tumors (23). The
structural similarity of well-differentiated tumors with the
epithelium of origin may also confirm the existence of CSCs. In
particular, a well-differentiated OSCC may reproduce the
proliferation pattern and histological appearance of the oral
epithelium. Due to the lack of reliable specific markers of CSCs
(24), there are numerous unresolved
issues regarding OSCCs (25).
Numerous distinct models attempt to explain the
origin of CSCs. The most important hypothesis regarding the origin
of CSCs is that they develop from the transformation of stem cells
(SCs). This hypothesis is compelling for several reasons. The
malignant transformation of a normal cell requires 3–6 oncogenic
events, and the long life of SCs increases the risk of accumulating
the multiple mutations (26). SCs and
CSCs possessing the capacity for self-renewal is an additional
reason to consider that the origin of CSCs is normal SCs, as the
dysregulation of the self-renewal process is an early and important
event in carcinogenesis. Although the hypothesis that CSCs derive
from normal adult SCs appears to be the most plausible, other
origins may also be possible. A CSC may originate from the fusion
of a hemopoietic stem cell (HSC) with a mutated epithelial somatic
cell. In 2004, Wagers and Weissman and Houghton et al
demonstrated that the fusion of HSCs with epithelial cells has been
shown in vitro and in vivo in animal models of
stomach cancer (27,28). At present, the fusion of HSCs with
epithelial cells has not been demonstrated in OSCC. A CSC may also
result from the de-differentiation of a mature cell (29). Previous studies demonstrate that
differentiated cancer cells may achieve a CSC-like state through
epithelial mesenchymal transition (EMT). EMT is involved in the
acquisition by differentiated cells of the properties of SCs,
including in nasopharyngeal (30),
breast (31) and head and neck
squamous cell carcinomas (HNSCC) (32). A sparsely proliferative basal layer
with highly proliferative parabasal cell layers in premalignant
epithelia is another frequently observed proliferation pattern. The
aforementioned observation may indicate that the tumor did not
originate exclusively from a normal basal SC, but also from an
amplifying transitory cell (33).
The scarcity of markers for identifying CSCs
restricts the knowledge that studies may gain regarding the role of
CSCs in carcinogenesis; therefore, the perfect identification
technique does not yet exist. The most frequently applied method
for identifying CSCs is flow cytometry, which detects cells with
the ability to excrete the vital DNA dye Hoechst 33342 (34–38). A
distinctive small non-dyed population of cells, termed the side
population (SP), has been detected in numerous tumors, and is
highly tumorigenic (39–44). SP cells express SCs markers, including
cluster of differentiation (CD)44 (45), ATP-binding cassette sub-family G
member 2 (44), octamer-binding
transcription factor (Oct)4 (35) and
B cell-specific Moloney murine leukemia virus integration site 1
proto-oncogene (45). The SP
population ranges between 0.2–10.0% of the cancer cell population
(35). Flow cytometry does not permit
CSCs to be topographically localized in healthy or tumorous tissues
for the assessment of proliferative activity or spatial
associations with progeny. The transcription factors SOX2 (46,47),
Oct3/4 (45), β-1 integrin (48), CD133 (49) and CD44 (50) demonstrate promise for the
topographical localization of CSCs. The transcription factors SOX2
and Oct3/4 are essential for maintaining the self-renewal capacity
and pluripotency of embryonic and adult SCs. CD133+
cells in OSCC form holoclones and possess self-renewal capacity
(51), and CD44+ cells in
HNSCC possess the capacity for self-renewal and differentiation
(52). However, the usefulness of
CD44 as a marker of CSCs in OSCC is questionable as CD44 is
expressed by normal oral epithelial cells (53,54). The
value of CD44 as a marker of OSCC progression and prognosis is also
controversial. Certain studies in HNSCC have reported aldehyde
dehydrogenase (ALDH)+ cells with typical CSC behavior,
in particular the tumorigenic ability (55–58). The
specificity of CD44 as a marker of CSCs in HNSCC is reported to be
increased in combination with ALDH (55,56).
Although a small number of ALDH+/CD44− CSCs
exist (56). In addition, E-cadherin,
CD97, CD117, CD147, CK19 and epithelial-specific antigen have been
used in attempts to identify oral SCs/CSCs; however the antigens
were not adequately specific (59–62).
Notably, Miranda-Lorenzoan et al identified an intrinsic
autoflorescent phenotype in CSCs from diverse epithelial cancers,
and used the marker to isolate and characterize the CSCs (63).
SOX2 is an important stem cell marker that is
crucial for embryonic development and to maintain the
differentiation potential of stem cells. SOX2 is one of the key
transcription factors involved in inducing pluripotent stem cells.
In the past decade, SOX2 has been established as one of the
hallmark participants of the developmental process in cancer,
including in skin squamous cell carcinoma, gastric cancer,
glioblastoma, colorectal cancer, lung cancer, breast cancer and
OSCC (3–9).
SOX2 is an amplified gene in OSCC, and the key role
of SOX2 is to maintain the stemness of the cells. Nadja et
al demonstrated that SOX2 amplifications are common in OSCC and
the detection of SOX2 amplifications in the early stages of disease
may be crucial for early disease detection and a more accurate
prognosis (64). He et al
revealed that the expression of SOX2 was amplified in OSCC and was
significantly associated with the pathological grade (65). In addition, a significant difference
in SOX2 staining was demonstrated between OSCC, oral epithelial
dysplasia and normal oral mucosa. Previous studies showed that SOX2
was overexpressed in OSCCs, the expression of SOX2 was decreased in
the CAL27 and UMSCC74A cell lines that were treated with cationic
lipid nanoparticles to deliver pre-miR-107, and the tumorsphere
formation efficiency and size were decreased (66–68).
However, the mechanism by which miR-107 regulates SOX2 expression
in HNSCC is unclear. Studies indicate that SOX2 is amplified in
numerous types of tumors, which is associated with the indicators
of a favorable prognosis (69). SOX2
overexpression has been demonstrated to deregulate genes in
malignant processes, cellular migration and anchorage-independent
growth (70).
SOX2 performs a similar role in CSCs to that in
embryonic stem cells. In a previous study, SOX2 was preferentially
expressed in cancer cells with a basal-like phenotype, and is,
therefore, likely to contribute to defining the characteristics of
less differentiated stem cell phenotypes (71). A similar phenomenon existed in studies
on OSCCs and HNSCCs, as SOX2 was mainly expressed in the stratum
basale, co-localizing with the region that contained stem cells
(68,72). In addition to the application of SOX2
in identifying various subsets of tumor cells, SOX2 also maintains
the stemness of tumor-initiating cells (TICs) and CSCs.
In a previous study, SOX2 knockdown in CSCs led to
the inhibition of proliferation and loss of tumorigenicity in
immunodeficient mice, indicating that SOX2 was crucial for
maintaining the self-renewal capacity of CSCs (73). The role of SOX2 in maintaining the
self-renewal capacity of CSCs in HNSCC and breast cancer has been
previously confirmed (74,75). The findings of these studies indicate
that SOX2 expression promotes and maintains the stemness of CSCs.
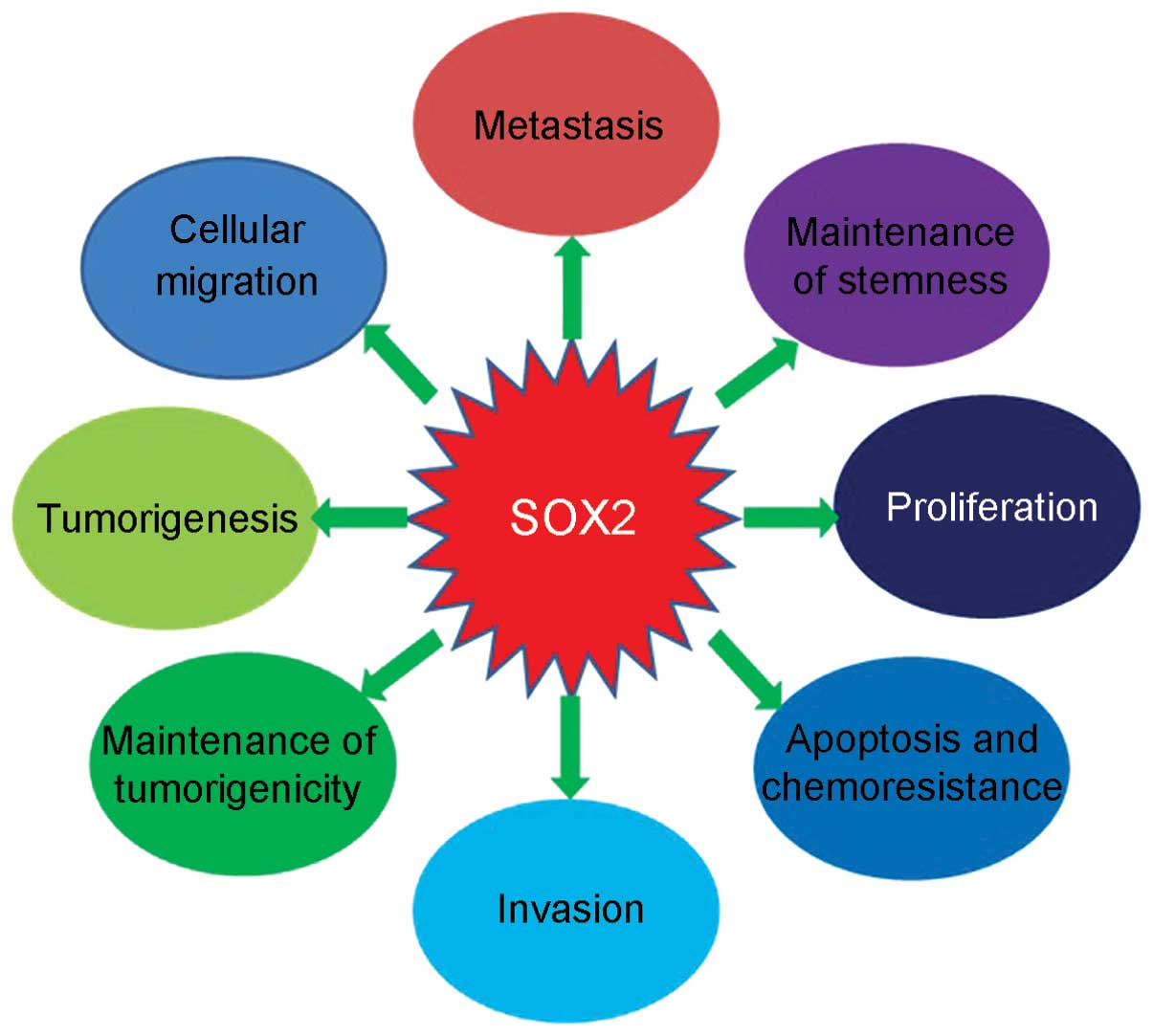
Other important roles of SOX2 in cancer progression include the
contribution to the physiological or pathophysiological process of
cancer cells. The proliferation of HNSC CSCs was inhibited in
vitro and in vivo, as SOX2 was suppressed by
all-trans-retinoic acid (76). SOX2
expression has been demonstrated to improve the ability of invasion
and migration of tumor cells in tongue squamous cell carcinoma
(TSCC) (77). Other properties of
cancer cells in OSCC or HNSCC that involve the SOX2 protein include
apoptosis (74,78), chemoresistance (79), metastasis and tumorigenesis (10,79).
SOX2 is a key regulator of development and
carcinogenesis and exhibited close associations with several
microRNAs. In a previous study, the activities of SOX2 were
indicated to be controlled by numerous microRNAs; therefore,
certain microRNAs may also be regulated by SOX2, including
microRNA-145 (80,81), microRNA-107 (67) and microRNA-302 (74). Bourguignon et al demonstrated
that the stimulation of miR-302 expression by hyaluronan-CD44 is
Oct4-SOX2-Nanog-dependent in HNSCC-specific CSCs, and that
microRNA-302 expression was the underlying mechanism of
self-renewal, clonal formation and cisplatin resistance in CSCs in
HNSCC (74). The roles of SOX2 in
cancers are summarized in Fig. 1.
At present, several studies have revealed that SOX2
overexpression in cancer cells exhibited a deleterious outcome, and
resulted in lower survival rates of patients. Several studies have
revealed that the SOX2 proteins were overexpressed in the TSCC, and
demonstrated that SOX2, recurrence and distant metastasis were
independent prognostic factors of overall survival in patients with
TSCC. Therefore the studies concluded that the expression of SOX2
may be used as a prognostic indicator of TSCC (82). SOX2 was exclusively expressed in the
CSCs of OSCC patients and the expression of SOX2 was significantly
associated with a poor prognosis of OSCC and lymph node status,
which indicates the potential prognostic value of SOX2 in OSCC.
SOX2 may also act as a promising marker for directing OSCC
diagnosis and therapy (65). The
evidence that SOX2 overexpression was oncogenic was also
demonstrated in HNSCC patients, and SOX2 was indicated to be
associated with a worse prognosis. These findings are valuable in
providing useful information for developing a novel classification
system and therapeutic strategies for HNSCC (64). However, the opposite viewpoint from
certain studies supported that increased levels of SOX2 was
significantly associated with better prognosis in the patients of
OSCC and squamous cell lung cancer (69,79).
SOX2 was amplified in numerous types of cancer,
including OSCC. However, the role of SOX2 in cancer is
controversial. The vast majority of studies show that SOX2
overexpression may promote cancer progression, hypothesizing that
SOX2 may act as a potential target for cancer therapy. However,
certain studies hypothesized that SOX2 may suppress tumors and that
SOX2 overexpression inhibits the cell proliferation. In addition,
the opposite views of the association between SOX2 and the survival
rate of patient were stated in other studies. The vast majority of
studies showed that the survival rate of OSCC patients possessing
low levels of SOX2 is increased compared with those with high
levels of SOX2. However, the opposite view was indicated by Züllig
et al, who supported that low level SOX2 expression was
significantly associated with worse survival (79). Additional studies are required in
order to understand the conflicting opinions. In conclusion, the
overexpression of SOX2 derived from amplification promotes cancer
progression and tumor formation. SOX2 may provide a novel
diagnostic marker for OSCC, be used as a therapeutic stratification
marker, or target molecules for therapeutic interference; however,
the underlying molecular mechanism remains unclear (83).
Tumor metastasis is the key factor that compromises
the prognosis of tumor patients, which accounts for 90% of
tumor-associated mortalities (84,85).
Metastasis is a multistep process by which a percentage of primary
tumor cells acquire the ability to spread between the initial site
and secondary tissues or organs, or the surrounding normal tissues
(86–88). Failure at any stage may restrict the
entire metastatic process. Since metastasis is responsible for the
majority of mortalities of cancer patients, an improved
understanding of the molecular mechanism involved in the tumor
spreading process is crucial for preventing tumor metastasis and
improving the prognosis of patients.
SOX2 has recently been shown to be a putative CSC
marker in several malignancies, including glioblastoma (5) and gastric (3), colorectal (6), breast (8),
oral (9) and lung (7,89) cancers.
In addition, the importance of SOX2 in cancer metastasis has also
been addressed. Previously, several studies demonstrated that SOX2
expression was closely associated with lymph node metastasis,
distant spread and poor prognosis in colorectal carcinoma patients
(6,90,91).
Certain data suggested that SOX2 knockdown may induce
mesenchymal-epithelial transition (MET). MET is the reverse process
of EMT. Epithelial cells gain polarity and motility during EMT,
which are necessary for tumor invasion and metastasis in various
types of epithelial carcinomas. Notably, studies have identified
that knocking down SOX2 promoted MET and resulted in the
translocation of β-catenin, which is critical in the WNT pathway
(92). Studies indicated that all
SOX2-positive primary tumors retained a SOX2-expressing phenotype
during lymph node metastasis. This finding may indicate that
SOX2-bearing cancer cells have an increased probability and ability
to metastasize to the lymph node and supports the notion that SOX2
is crucial for breast cancer invasiveness and spread. Notably, a
significantly increased SOX2 expression in lymph node metastasis
compared with respective primary tumors was indicated (93). A similar finding was also reported in
the study conducted by Lengerke et al, in which the data
suggest that SOX2 is important in early breast carcinogenesis and
that increased expression may promote metastatic potential
(8). Downregulation of SOX2
significantly decreased angiogenesis and lymphomagenesis of breast
cancer. Additionally, the promotion effect of SOX2 on tumor cell
metastasis was observed in vitro and in the tumor bearing
mice in vivo. SOX2 also promoted the EMT process in the
tumor cells in breast cancer by regulating the WNT/β-catenin signal
pathway (94,95). A previous study on lung cancer
indicated that the overexpression of SOX2 was also positively
associated with the tumor-node-metastasis stage and lymph node
metastasis (96).
SOX2 protein expression was indicated to be
significantly associated with lymph node metastasis and recurrence
in HNSCC patients (97). However, in
numerous HNSCC patients, SOX2 expression was not associated with
disease stage, lymph node metastasis or distant metastasis
(98,99). The contradictory results may be
associated with methodological variations in the SOX2
immunopositivity scoring (99).
Therefore, additional studies on the oncogenic function of SOX2 in
HNSCC and the underlying molecular mechanisms accounting for the
association of SOX2 with progression remain to be elucidated.
Similarly to HNSCC, the studies on the association
between SOX2 and lymph node metastasis in OSCC are inadequate.
Certain data showed that the SOX2 may be classified into diffuse
staining patterns and peripheral staining patterns, and that the
SOX2 diffuse staining pattern was associated with lymph node
metastasis of OSCC (10). Even in
OTSCCs without lymph node metastasis, SOX2 expression has been
demonstrated to be involved in tumor progression (9). An additional study indicated that the
poor prognosis associated with lymph node metastasis was
significantly associated with the high expression of SOX2 in the
primary sites of OSCCs (10). Qiao
et al supported the finding that SOX2 expression was
significantly associated with lymph node metastasis (100). However, the study conducted by
Züllig et al showed that increased expression levels of SOX2
were significantly associated with a lack of lymph node metastasis,
which implies a good prognosis in OSCC patients, and indicated that
the heterogeneity of primary tumors may be one of the reasons for
controversial results (79). This
result is consistent with certain findings in lung cancer (101). According to the data in the study by
Züllig et al, SOX2 is a potential predictive marker for the
lack of metastasis to the sentinel lymph nodes of the neck in early
SCC of the oral cavity (79).
Overall, based on the phenomenon of overexpression
of SOX2 in several types of cancer and the role of SOX2 in
promoting cancer progression, the application of SOX2 is
hypothesized to aid decisions on cancer diagnosis and therapy, and
may even predict the prognosis of patients. However, underlying
molecular mechanisms of SOX2 in OSCC remain to be elucidated. The
association between the expression of SOX2 in OSCC and lymph node
metastasis is remains unclear. The molecular mechanisms underlying
the association between SOX2 and lymph node metastasis require
additional studies.
|
1
|
Ivanova N, Dobrin R, Lu R, Kotenko I,
Levorse J, DeCoste C, Schafer X, Lun Y and Lemischka IR: Dissecting
self-renewal in stem cells with RNA interference. Nature.
442:533–538. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wang J, Rao S, Chu J, Shen X, Levasseur
DN, Theunissen TW and Orkin SH: A protein interaction network for
pluripotency of embryonic stem cells. Nature. 444:364–368. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Boumahdi S, Driessens G, Lapouge G, Rorive
S, Nassar D, Le Mercier M, Delatte B, Caauwe A, Lenglez S, Nkusi E,
et al: SOX2 controls tumour initiation and cancer stem-cell
functions in squamous-cell carcinoma. Nature. 511:246–250. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Power DG, Kelsen DP and Shah MA: Advanced
gastric cancer - slow but steady progress. Cancer Treat Rev.
36:384–392. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Koyama-Nasu R, Haruta R, Nasu-Nishimura Y,
Taniue K, Katou Y, Shirahige K, Todo T, Ino Y, Mukasa A, Saito N,
et al: The pleiotrophin-ALK axis is required for tumorigenicity of
glioblastoma stem cells. Oncogene. 33:2236–2244. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Neumann J, Bahr F, Horst D, Kriegl L,
Engel J, Luque RM, Gerhard M, Kirchner T and Jung A: SOX2
expression correlates with lymph-node metastases and distant spread
in right-sided colon cancer. BMC Cancer. 11:5182011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Drilon A, Rekhtman N, Ladanyi M and Paik
P: Squamous-cell carcinomas of the lung: Emerging biology,
controversies, and the promise of targeted therapy. Lancet Oncol.
13:e418–e426. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lengerke C, Fehm T, Kurth R, Neubauer H,
Scheble V, Müller F, Schneider F, Petersen K, Wallwiener D, Kanz L,
et al: Expression of the embryonic stem cell marker SOX2 in
early-stage breast carcinoma. BMC Cancer. 11:422011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Du L, Yang Y, Xiao X, Wang C, Zhang X,
Wang L, Zhang X, Li W, Zheng G, Wang S and Dong Z: SOX2 nuclear
expression is closely associated with poor prognosis in patients
with histologically node-negative oral tongue squamous cell
carcinoma. Oral Oncol. 47:709–713. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Michifuri Y, Hirohashi Y, Torigoe T,
Miyazaki A, Kobayashi J, Sasaki T, Fujino J, Asanuma H, Tamura Y,
Nakamori K, et al: High expression of ALDH1 and SOX2 diffuse
staining pattern of oral squamous cell carcinomas correlates to
lymph node metastasis. Pathol Int. 62:684–689. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bray F, Ren JS, Masuyer E and Ferlay J:
Global estimates of cancer prevalence for 27 sites in the adult
population in 2008. Int J Cancer. 132:1133–1145. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ren ZH, Wu HJ, Zhang S, Wang K, Gong ZJ,
He ZJ and Peng J: A new surgical strategy for treatment of tongue
squamous cell carcinoma based on anatomic study with preliminary
clinical evaluation. J Craniomaxillofac Surg. 43:1577–1582. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ren ZH, Wu HJ, Wang K, Zhang S, Tan HY and
Gong ZJ: Anterolateral thigh myocutaneous flaps as the preferred
flaps for reconstruction of oral and maxillofacial defects. J
Craniomaxillofac Surg. 42:1583–1589. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Brinkman BM and Wong DT: Disease mechanism
and biomarkers of oral squamous cell carcinoma. Curr Opin Oncol.
18:228–233. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Guo BH, Feng Y, Zhang R, Xu LH, Li MZ,
Kung HF, Song LB and Zeng MS: Bmi-1 promotes invasion and
metastasis, and its elevated expression is correlated with an
advanced stage of breast cancer. Mol Cancer. 10:102011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ren ZH and Wu HJ: Extracapsular spread in
cervical lymph nodes. Shiyong Kou Qiang Yi Xue Za Zhi. 28:514–517.
2012.(In Chinese).
|
|
17
|
El-Naaj IA, Leiser Y, Shveis M, Sabo E and
Peled M: Incidence of oral cancer occult metastasis and survival of
T1-T2N0 oral cancer patients. J Oral Maxillofac Surg. 69:2674–2679.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bass AJ, Watanabe H, Mermel CH, Yu S,
Perner S, Verhaak RG, Kim SY, Wardwell L, Tamayo P, Gat-Viks I, et
al: SOX2 is an amplified lineage-survival oncogene in lung and
esophageal squamous cell carcinomas. Nat Genet. 41:1238–1242. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kitamura H, Torigoe T, Hirohashi Y,
Asanuma H, Inoue R, Nishida S, Tanaka T, Fukuta F, Masumori N, Sato
N and Tsukamoto T: Prognostic impact of the expression of ALDH1 and
SOX2 in urothelial cancer of the upper urinary tract. Mod Pathol.
26:117–124. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Teodorczyk M, Kleber S, Wollny D, Sefrin
JP, Aykut B, Mateos A, Herhaus P, Sancho-Martinez I, Hill O,
Gieffers C, et al: CD95 promotes metastatic spread via Sck in
pancreatic ductal adenocarcinoma. Cell Death Differ. 22:1192–1202.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Goel HL, Gritsko T, Pursell B, Chang C,
Shultz LD, Greiner DL, Norum JH, Toftgard R, Shaw LM and Mercurio
AM: Regulated splicing of the α6 integrin cytoplasmic domain
determines the fate of breastcancer stem cells. Cell Rep.
7:747–761. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Reya T, Morrison SJ, Clarke MF and
Weissman IL: Stem cells, cancer, and cancer stem cells. Nature.
414:105–111. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
23
|
Pardal R, Clarke MF and Morrison SJ:
Applying the principles of stem-cell biology to cancer. Nat Rev
Cancer. 3:895–902. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
24
|
González-Moles MA, Scully C, Ruiz-Ávila I
and Plaza-Campillo JJ: The cancer stem cell hypothesis applied to
oral carcinoma. Oral Oncol. 49:738–746. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Boman BM and Wicha MS: Cancer stem cells:
A step toward the cure. J Clin Oncol. 26:2795–2799. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hahn WC and Weinberg RA: Rules for making
human tumor cells. N Engl J Med. 347:1593–1603. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wagers AJ and Weissman IL: Plasticity of
adult stem cells. Cell. 116:639–648. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Houghton J, Stoicov C, Nomura S, Rogers
AB, Carlson J, Li H, Cai X, Fox JG, Goldenring JR and Wang TC:
Gastric cancer originating from bone marrow-derived cells. Science.
306:1568–1571. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zhu AJ and Watt FM: Beta-catenin
signalling modulates proliferative potential of human epidermal
keratinocytes independently of intercellular adhesion. Development.
126:2285–2298. 1999.PubMed/NCBI
|
|
30
|
Cheng Y, Cheung AK, Ko JM, Phoon YP, Chiu
PM, Lo PH, Waterman ML and Lung ML: Physiological β-catenin
signaling controls self-renewal networks and generation of
stem-like cells from nasopharyngeal carcinoma. BMC Cell Biol.
14:442013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Morel AP, Lièvre M, Thomas C, Hinkal G,
Ansieau S and Puisieux A: Generation of breast cancer stem cells
through epithelial-mesenchymal transition. PLoS One. 3:e28882008.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Zhang Z, Filho MS and Nör JE: The biology
of head and neck cancer stem cells. Oral Oncol. 48:1–9. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
González-Moles MA, Bravo M, Ruiz-Avila I,
Acebal F, Gil-Montoya JA, Brener S and Esteban F: Ki-67 expression
in non-tumour epithelium adjacent to oral cancer as risk marker for
multiple oral tumours. Oral Dis. 16:68–75. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Yu S, Zhang R, Liu F, Wang H, Wu J and
Wang Y: Notch inhibition suppresses nasopharyngeal carcinoma by
depleting cancer stem-like side population cells. Oncol Rep.
28:561–566. 2012.PubMed/NCBI
|
|
35
|
Zhang P, Zhang Y, Mao L, Zhang Z and Chen
W: Side population in oral squamous cell carcinoma possesses tumor
stem cell phenotypes. Cancer Lett. 277:227–234. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Song J, Chang I, Chen Z, Kang M and Wang
CY: Characterization of side populations in HNSCC Highly invasive,
chemoresistant and abnormal Wnt signaling. PLoS One. 5:e114562010.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Yanamoto S, Kawasaki G, Yamada S,
Yoshitomi I, Kawano T, Yonezawa H, Rokutanda S, Naruse T and Umeda
M: Isolation and characterization of cancer stem-like side
population cells in human oral cancer cells. Oral Oncol.
47:855–860. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Richard V, Nair MG, Santhosh Kumar TR and
Pillai MR: Side population cells as prototype of chemoresistant,
tumor-initiating cells. Biomed Res Int. 2013:5172372013. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Zhai JM, Yin XY, Hou X, Hao XY, Cai JP,
Liang LJ and Zhang LJ: Analysis of the genome-wide DNA methylation
profile of side population cells in hepatocellular carcinoma. Dig
Dis Sci. 58:1934–1947. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Broadley KW, Hunn MK, Farrand KJ, Price
KM, Grasso C, Miller RJ, Hermans IF and McConnell MJ: Side
population is not necessary or sufficient for a cancer stem cell
phenotype in glioblastoma multiforme. Stem Cells. 29:452–461. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Guo D, Xu BL, Zhang XH and Dong MM: Cancer
stem-like side population cells in the human nasopharyngeal
carcinoma cell line cne-2 possess epithelial mesenchymal transition
properties in association with metastasis. Oncol Rep. 28:241–247.
2012.PubMed/NCBI
|
|
42
|
Wei X, Dombkowski D, Meirelles K,
Pieretti-Vanmarcke R, Szotek PP, Chang HL, Preffer FI, Mueller PR,
Teixeira J, MacLaughlin DT and Donahoe PK: Mullerian inhibiting
substance preferentially inhibits stem/progenitors in human ovarian
cancer cell lines compared with chemotherapeutics. Proc Natl Acad
Sci USA. 107:18874–18879. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Wu CP, Zhou L, Xie M, Du HD, Tian J, Sun S
and Li JY: Identification of cancer stem-like side population cells
in purified primary cultured human laryngeal squamous cell
carcinoma epithelia. PLoS One. 8:e657502013. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Tabor MH, Clay MR, Owen JH, Bradford CR,
Carey TE, Wolf GT and Prince ME: Head and neck cancer stem cells:
The side population. Laryngoscope. 121:527–533. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Mack B and Gires O: CD44s and CD44v6
expression in head and neck epithelia. PLoS One. 3:e33602008.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Keramari M, Razavi J, Ingman KA, Patsch C,
Edenhofer F, Ward CM and Kimber SJ: SOX2 is essential for formation
of trophectoderm in the preimplantation embryo. PLoS One.
5:e139522010. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Okumura-Nakanishi S, Saito M, Niwa H and
Ishikawa F: Oct-3/4 and SOX2 regulate Oct-3/4 gene in embryonic
stem cells. J Biol Chem. 280:5307–5317. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Evans RD, Perkins VC, Henry A, Stephens
PE, Robinson MK and Watt FM: A tumor-associated beta 1 integrin
mutation that abrogates epithelial dfferentiation control. J Cell
Biol. 160:589–596. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Yin AH, Miraglia S, Zanjani ED,
Almeida-Porada G, Ogawa M, Leary AG, Olweus J, Kearney J and Buck
DW: AC133, a novel marker for human hematopoietic stem and
progenitor cells. Blood. 90:5002–5012. 1997.PubMed/NCBI
|
|
50
|
Aruffo A, Stamenkovic I, Melnick M,
Underhill CB and Seed B: CD44 is the principal cell surface
receptor for hyaluronate. Cell. 61:1303–1313. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Felthaus O, Ettl T, Gosau M, Driemel O,
Brockhoff G, Reck A, Zeitler K, Hautmann M, Reichert TE, Schmalz G
and Morsczeck C: Cancer stem cell-like cells from a single cell of
oral squamous carcinoma cell lines. Biochem Biophys Res Commun.
407:28–33. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Faber A, Barth C, Hörmann K, Kassner S,
Schultz JD, Sommer U, Stern-Straeter J, Thorn C and Goessler UR:
CD44 as a stem cell marker in head and neck squamous cell
carcinoma. Oncol Rep. 26:321–326. 2011.PubMed/NCBI
|
|
53
|
Oliveira LR, Oliveira-Costa JP, Araujo IM,
Soave DF, Zanetti JS, Soares FA, Zucoloto S and Ribeiro-Silva A:
Cancer stem cell immunophenotypes in oral squamous cell carcinoma.
J Oral Pathol Med. 40:135–142. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Grimm M, Alexander D, Munz A, Hoffmann J
and Reinert S: Is 1,25-dihydroxyvitamin D3 receptor expression a
potential Achilles' heel of CD44+ oral squamous cell
carcinoma cells? Target Oncol. 8:189–201. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Nishikawa S, Konno M, Hamabe A, Hasegawa
S, Kano Y, Ohta K, Fukusumi T, Sakai D, Kudo T, Haraguchi N, et al:
Aldehyde dehydrogenase high gastric cancer stem cells are resistant
to chemotherapy. Int J Oncol. 42:1437–1442. 2013.PubMed/NCBI
|
|
56
|
Clay MR, Tabor M, Owen JH, Carey TE,
Bradford CR, Wolf GT, Wicha MS and Prince ME: Single-marker
identification of head and neck squamous cell carcinoma cancer stem
cells with aldehyde dehydrogenase. Head Neck. 32:1195–1201. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Krishnamurthy S, Dong Z, Vodopyanov D,
Imai A, Helman JI, Prince ME, Wicha MS and Nör JE: Endothelial
cell-initiated signaling promotes the survival and self-renewal of
cancer stem cells. Cancer Res. 70:9969–9978. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Zhang Z, Dong Z, Lauxen IS, Filho MS and
Nör JE: Endothelial cell-secreted EGF induces epithelial to
mesenchymal transition and endows head and neck cancer cells with
stem-like phenotype. Cancer Res. 74:2869–2881. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Richard V and Pillai MR: The stem cell
code in oral epithelial tumorigenesis: 'The cancer stem cell shift
hypothesis'. Biochim Biophys Acta. 1806:146–162. 2010.PubMed/NCBI
|
|
60
|
Allegra E, Trapasso S, Pisani D and Puzzo
L: The role of BMI1 as a biomarker of cancer stem cells in head and
neck cancer: A review. Oncology. 86:199–205. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Zhou ZT and Jiang WW: Cancer stem cell
model in oral squamous cell carcinoma. Curr Stem Cell Res Ther.
3:17–20. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Hayashi S, Tanaka J, Okada S, Isobe T,
Yamamoto G, Yasuhara R, Irie T, Akiyama C, Kohno Y, Tachikawa T and
Mishima K: Lin28a is a putative factor in regulating cancer stem
cell-like properties in side population cells of oral squamous cell
carcinoma. Exp Cell Res. 319:1220–1228. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Miranda-Lorenzo I, Dorado J, Lonardo E,
Alcala S, Serrano AG, Clausell-Tormos J, Cioffi M, Megias D,
Zagorac S, Balic A, et al: Intracellular autofluorescence: A
biomarker for epithelial cancer stem cells. Nat Methods.
11:1161–1169. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Kokalj Vokač N, Cizmarević B, Zagorac A,
Zagradišnik B and Lanišnik B: An evaluation of SOX2 and hTERC gene
amplifications as screening markers in oral and oropharyngeal
squamous cell carcinomas. Mol Cytogenet. 7:52014. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
He KF, Zhang L, Huang CF, Ma SR, Wang YF,
Wang WM, Zhao ZL, Liu B, Zhao YF, Zhang WF and Sun ZJ:
CD163+ tumor-associated macrophages correlated with poor
prognosis and cancer stem cells in oral squamous cell carcinoma.
Biomed Res Int. 2014:8386322014. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Chen C, Wei Y, Hummel M, Hoffmann TK,
Gross M, Kaufmann AM and Albers AE: Evidence for
epithelial-mesenchymal transition in cancer stem cells of head and
neck squamous cell carcinoma. PLoS One. 6:e164662011. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Piao L, Zhang M, Datta J, Xie X, Su T, Li
H, Teknos TN and Pan Q: Lipid-based nanoparticle delivery of
Pre-miR-107 inhibits the tumorigenicity of head and neck squamous
cell carcinoma. Mol Ther. 20:1261–1269. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Walter V, Yin X, Wilkerson MD, Cabanski
CR, Zhao N, Du Y, Ang MK, Hayward MC, Salazar AH, Hoadley KA, et
al: Correction: Molecular subtypes in head and neck cancer exhibit
distinct patterns of chromosomal gain and loss of canonical cancer
genes. PLoS One. 8:e568232014. View Article : Google Scholar
|
|
69
|
Wilbertz T, Wagner P, Petersen K, Stiedl
AC, Scheble VJ, Maier S, Reischl M, Mikut R, Altorki NK, Moch H, et
al: SOX2 gene amplification and protein overexpression are
associated with better outcome in squamous cell lung cancer. Mod
Pathol. 24:944–953. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Hussenet T, Dali S, Exinger J, et al: SOX2
is an oncogene activated by recurrent 3q26.3 amplifications in
human lung squamous cell carcinomas. PLoS One. 5:e89602010.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Rodriguez-Pinilla SM, Sarrio D,
Moreno-Bueno G, Rodriguez-Gil Y, Martinez MA, Hernandez L,
Hardisson D, Reis-Filho JS and Palacios J: Sox2: A possible driver
of the basal-like phenotype in sporadic breast cancer. Mod Pathol.
20:474–481. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Lu W, Feng F, Xu J, et al: QKI impairs
self-renewal and tumorigenicity of oral cancer cells via repression
of SOX2. Cancer Biol Ther. 15:1174–1184. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Hägerstrand D, He X, Bradic Lindh M, Hoefs
S, Hesselager G, Ostman A and Nistér M: Identification of a
SOX2-dependent subset of tumor - and sphere-forming glioblastoma
cells with a distinct tyrosine kinase inhibitor sensitivity
profile. Neuro Oncol. 13:1178–1191. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Bourguignon LY, Wong G, Earle C and Chen
L: Hyaluronan-CD44v3 interaction with Oct4-Sox2-Nanog promotes
miR-302 expression leading to self-renewal, clonal formation, and
cisplatin resistance in cancer stem cells from head and neck
squamous cell carcinoma. J Biol Chem. 287:32800–32824. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Leis O, Eguiara A, Lopez-Arribillaga E,
Alberdi MJ, Hernandez-Garcia S, Elorriaga K, Pandiella A, Rezola R
and Martin AG: SOX2 expression in breast tumours and activation in
breast cancer stem cells. Oncogene. 31:1354–1365. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Lim YC, Kang HJ, Kim YS and Choi EC:
All-trans-retinoic acid inhibits growth of head and neck cancer
stem cells by suppression of Wnt/β-catenin pathway. Eur J Cancer.
48:3310–3318. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Sun Y, Han J, Lu Y, Yang X and Fan M:
Biological characteristics of a cell subpopulation in tongue
squamous cell carcinoma. Oral Dis. 18:169–177. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Lee SH, Nam HJ, Kang HJ, Kwon HW and Lim
YC: Epigallocatechin-3-gallate attenuates head and neck cancer stem
cell traits through suppression of Notch pathway. Eur J Cancer.
49:3210–3218. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Züllig L, Roessle M, Weber C, Graf N,
Haerle SK, Jochum W, Stoeckli SJ, Moch H and Huber GF: High sex
determining region Y-box 2 expression is a negative predictor of
occult lymph node metastasis in early squamous cell carcinomas of
the oral cavity. Eur J Cancer. 49:1915–1922. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Xu N, Papagiannakopoulos T, Pan G, Thomson
JA and Kosik KS: MicroRNA-145 regulates OCT4, SOX2, and KLF4 and
represses pluripotency in human embryonic stem cells. Cell.
137:647–658. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Liu T, Cheng W, Huang Y, Huang Q, Jiang L
and Guo L: Human amniotic epithelial cell feeder layers maintain
human iPS cell pluripotency via inhibited endogenous microRNA-145
and increased SOX2 expression. Exp Cell Res. 318:424–434. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Huang CF, Xu XR, Wu TF, Sun ZJ and Zhang
WF: Correlation of ALDH1, CD44, OCT4 and SOX2 in tongue squamous
cell carcinoma and their association with disease progression and
prognosis. J Oral Pathol Med. 43:492–498. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Liu K, Lin B, Zhao M, Yang X, Chen M, Gao
A, Liu F, Que J and Lan X: The multiple roles for SOX2 in stem cell
maintenance and tumorigenesis. Cell Signal. 25:1264–1271. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Floor SL, Dumont JE, Maenhaut C and Raspe
E: Hallmarks of cancer: Of all cancer cells, all the time? Trends
Mol Med. 18:509–515. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Christofori G: New signals from the
invasive front. Nature. 441:444–450. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Langley RR and Fidler IJ: The seed and
soil hypothesis revisited - the role of tumor-stroma interactions
in metastasis to different organs. Int J Cancer. 128:2527–2535.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Comen EA: Tracking the seed and tending
the soil: Evolving concepts in metastatic breast cancer. Discov
Med. 14:97–104. 2012.PubMed/NCBI
|
|
88
|
Comen E, Norton L and Massagué J: Clinical
implications of cancer self-seeding. Nat Rev Clin Oncol. 8:369–377.
2011.PubMed/NCBI
|
|
89
|
Nakatsugawa M, Takahashi A, Hirohashi Y,
Torigoe T, Inoda S, Murase M, Asanuma H, Tamura Y, Morita R,
Michifuri Y, et al: SOX2 is overexpressed in stem-like cells of
human lung adenocarcinoma and augments the tumorigenicity. Lab
Invest. 91:1796–1804. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Lee HJ, Eom DW, Kang GH, Han SH, Cheon GJ,
Oh HS, Han KH, Ahn HJ, Jang HJ and Han MS: Colorectal
micropapillary carcinomas are associated with poor prognosis and
enriched in markers of stem cells. Mod Pathol. 26:1123–1131. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Hu H, Chang DT, Nikiforova MN, Kuan SF and
Pai RK: Clinicopathologic features of synchronous colorectal
carcinoma: A distinct subset arising from multiple sessile serrated
adenomas and associated with high levels of microsatellite
instability and favorable prognosis. Am J Surg Pathol.
37:1660–1670. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Han X, Fang X, Lou X, Hua D, Ding W, Foltz
G, Hood L, Yuan Y and Lin B: Silencing SOX2 induced
mesenchymal-epithelial transition and its expression predicts liver
and lymph node metastasis of CRC patients. PLoS One. 7:e413352012.
View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Abd El-Maqsoud NM and Abd El-Rehim DM:
Clinicopathologic implications of EpCAM and SOX2 expression in
breast cancer. Clin Breast Cancer. 14:e1–e9. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Li X, Xu Y, Chen Y, Chen S, Jia X, Sun T,
Liu Y, Li X, Xiang R and Li N: SOX2 promotes tumor metastasis by
stimulating epithelial-to-mesenchymal transition via regulation of
WNT/β-catenin signal network. Cancer Lett. 336:379–389. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Li X, Chen S, Sun T, Xu Y, Chen Y, Liu Y,
Xiang R and Li N: The transcriptional regulation of SOX2 on FOXA1
gene and its application in diagnosis of human breast and lung
cancers. Clin Lab. 60:909–918. 2014.PubMed/NCBI
|
|
96
|
Yang F, Gao Y, Geng J, Qu D, Han Q, Qi J
and Chen G: Elevated expression of SOX2 and FGFR1 in correlation
with poor prognosis in patients with small cell lung cancer. Int J
Clin Exp Pathol. 6:2846–2854. 2013.PubMed/NCBI
|
|
97
|
Tang XB, Shen XH, Li L, Zhang YF and Chen
GQ: SOX2 overexpression correlates with poor prognosis in laryngeal
squamous cell carcinoma. Auris Nasus Larynx. 40:481–486. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Schröck A, Göke F, Wagner P, Bode M,
Franzen A, Braun M, Huss S, Agaimy A, Ihrler S, Menon R, et al: Sex
determining region Y-box 2 (SOX2) amplification is an independent
indicator of disease recurrence in sinonasal cancer. PLoS One.
8:e592012013. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
González-Márquez R, Llorente JL, Rodrigo
JP, García-Pedrero JM, Álvarez-Marcos C, Suárez C and Hermsen MA:
SOX2 expression in hypopharyngeal, laryngeal, and sinonasal
squamous cell carcinoma. Hum Pathol. 45:851–857. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Qiao B, He B, Cai J and Yang W: The
expression profile of Oct4 and SOX2 in the carcinogenesis of oral
mucosa. Int J Clin Exp Pathol. 7:28–37. 2014.PubMed/NCBI
|
|
101
|
Lu Y, Futtner C, Rock JR, Xu X, Whitworth
W, Hogan BL and Onaitis MW: Evidence that SOX2 overexpression is
oncogenic in the lung. PLoS One. 5:e110222010. View Article : Google Scholar : PubMed/NCBI
|