Introduction
Schwannomas are tumors derived from Schwann cells,
generally affecting the subcutaneous tissue of the distal
extremities and/or the head and neck region. Schwannomas are
generally benign neoplasias, and are extremely rare in the
gastrointestinal tract (1).
The stomach is the most common site for schwannomas
in the gastrointestinal tract, occurring primarily in the gastric
submucosa, followed by the colon (2,3). The most
infrequently affected sites are the small intestine and esophagus
(4,5).
The peculiar morphology and localization of gastric
schwannomas often causes problems in the differential diagnosis
between gastrointestinal stromal tumors (GISTs) and other
mesenchymal tumors typically located in the stomach.
The typical histological features of gastric
schwannoma consist of focally atypical spindle cells that are
usually arranged in a microtrabecular-microfascicular pattern and a
peritumoral lymphoid cuff, often with germinal centers. S100
protein positivity, a frequent but variable immunoreactivity for
GFAP, and negativity for c-Kit and smooth muscle markers have been
described in immunohistochemical studies (6,7). For the
differential diagnosis of gastric schwannomas from GISTs, the
determination of certain genetic characteristics, such as a lack of
c-Kit and PDGFRA mutations (8) are
extremely useful. For the differential diagnosis from soft-tissue
schwannomas the analysis of somatic NF2 gene mutations, which are
common in sporadic soft-tissue schwannomas, but rare in gastric
schwannomas, is necessary (9). The
genetic features of gastric schwannoma also include chromosome 22
monosomy and polyploidy of chromosome 2 and 18 (10).
Gastric schwannoma appears to exhibit a good
prognosis, with no recurrence or metastasis, and previous follow-up
studies have not found any malignant variants (11).
The present study describes the case of a
61-year-old male who presented with a clinical diagnosis of a GIST,
and was subsequently diagnosed with gastric schwannoma following
morphological, immunohistochemical and molecular
investigations.
Case report
A 61-year-old Caucasian male, without comorbidities,
but affected by dyspepsia and symptoms associated with gastro
esophageal reflux disease, underwent a diagnostic
esophagogastroduodenoscopy (EGD) revealing a 4-cm bulky mass of the
gastric antrum and a 3-cm mass of the first portion of the
duodenum. Endoscopic biopsies of the two lesions were inconclusive.
In May 2012, the patient was admitted to INT Fondazione Pascale
Hospital (Naples, Italy) and underwent a new EGD with endoscopic
ultrasound, which highlighted a unique sub-mucosal heteroplasia
protruding into the gastric antrum and duodenal bulb, with images
suggestive of a diagnosis of a GIST. Blood tests including CEA,
CA19-9, chromogranin, gastrin and NSE (Neuron Specific Enolase)
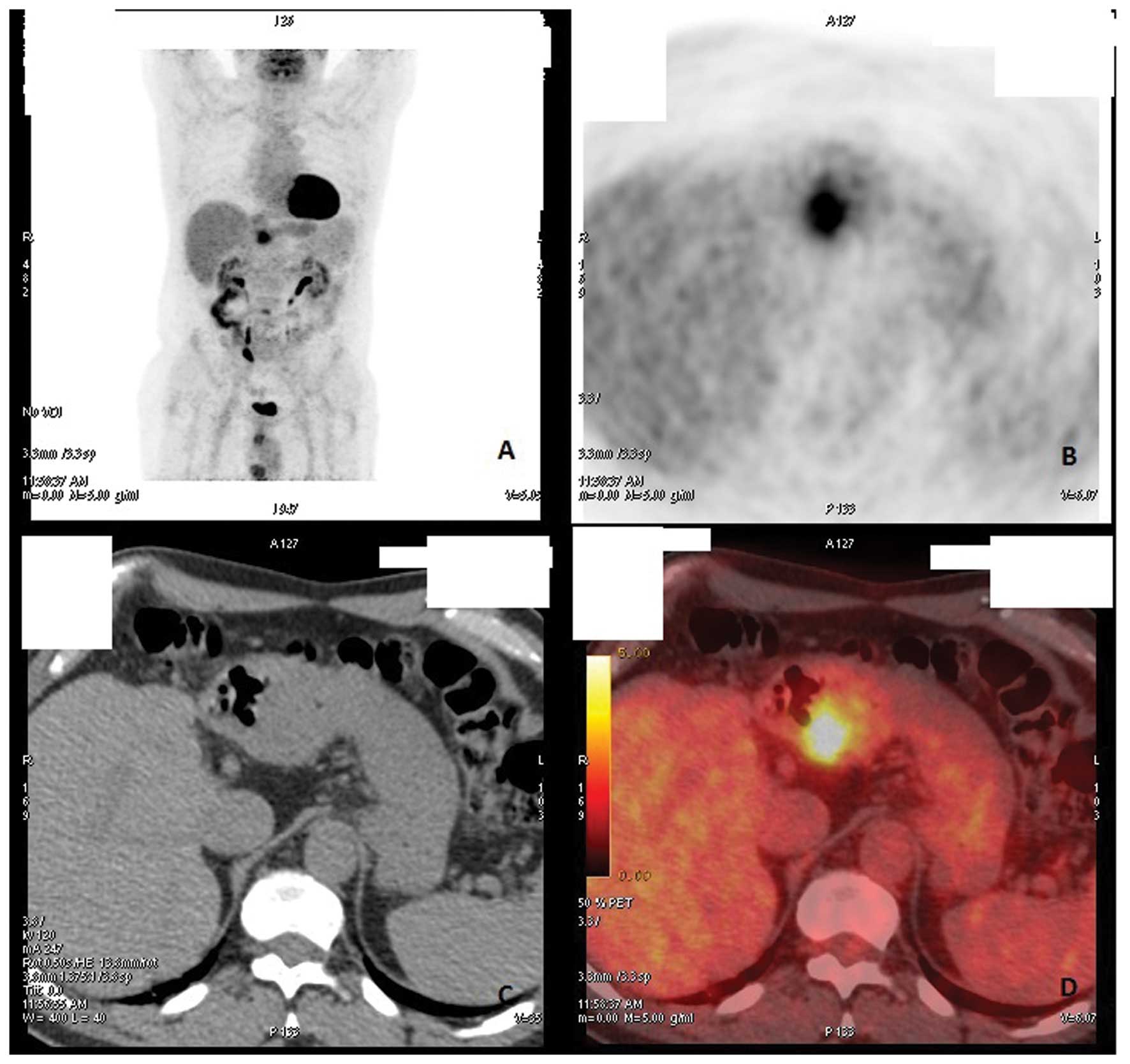
were within normal values. A total body CT scan confirmed the
presence of aforementioned lesion with images suggestive of
infiltration of perigastric fat and evidence of regional
lymphadenopathies (Fig. 1). The
patient underwent to a subtotal gastrectomy with D2
lymphadenectomy. The post-operative course was uneventful, with the
patient discharged on post-operative day 7.
The surgery constituted of subtotal
omento-gastrectomy, with stomach of 16×13 cm (great curvature ×
lesser curvature) and omentum of 50×38 cm.
At the gastric corpus, an exophytic, round lesion
(3.5 cm in maximum diameter) was present covered by normal mucosa,
with a fasciculated section surface. The omentum was
macroscopically normal.
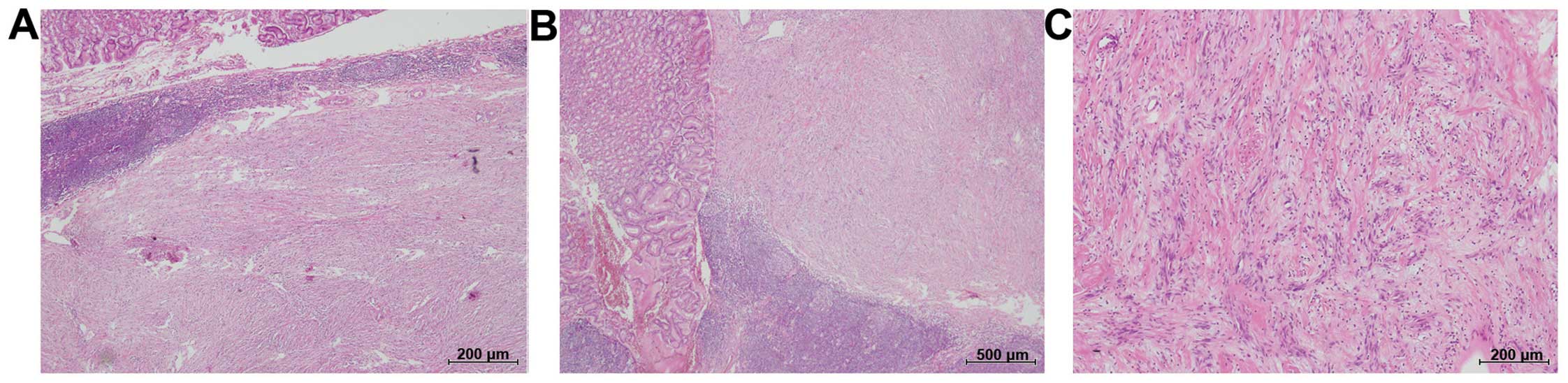
Under microscopic observation, the lesion was mainly
composed of spindle cells nests and cords, and rare epithelioid
cells, with a fasciculated/storiform growth pattern; the cytoplasm
was eosinophilic, and the nuclei were dark and occasionally
polymorphic (Fig. 2). Mitotic
activity was almost absent (<5/50 high-power fields). The Ki-67
proliferation index was low (3%) and cellular atypia was
absent.
The neoplastic proliferation affected the
sub-mucosal layers and was covered by normal gastric mucosa.
The lesion showed a peripheral covering of small
lymphocytes confluent in lymphoid aggregates with a few germinal
centers.
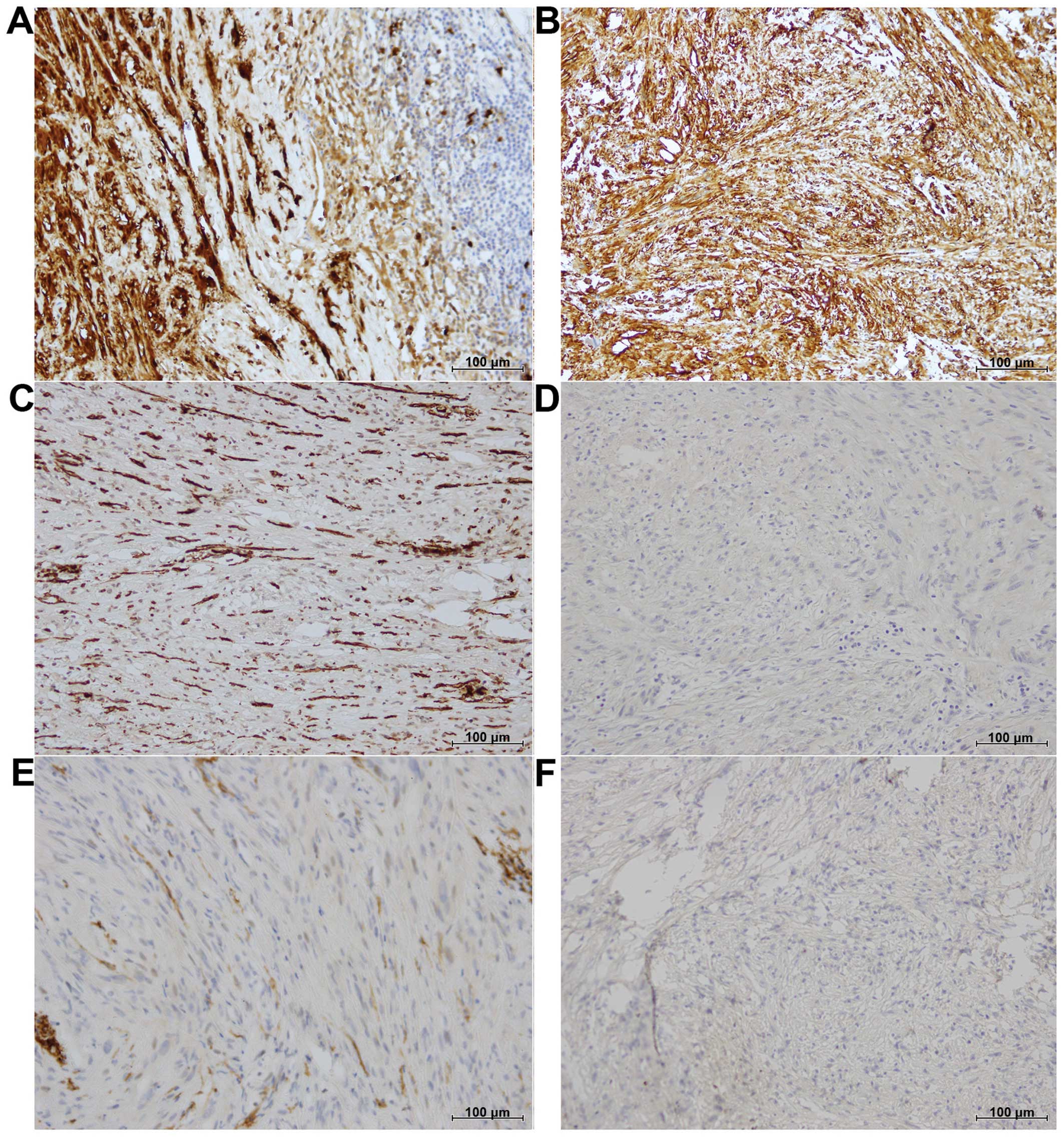
The panel of IHC markers used showed a negative
cellular reaction for cluster of differentiation (CD)117/c-Kit
(CD117, 1:50; Dako, Carpinteria, CA, USA), CD34 (QBEnd/10, 1:40;
BioGenex, San Ramon, CA, USA), SMA (1A4, 1:800; Sigma Chemicals,
St. Louis, MO, USA) and desmin (D33, 1:40; Dako) (Fig. 3).
A moderate positive cellular reaction for vimentin
(D9, 1:1,000; NeoMarkers, Westinghouse, CA, USA) and a strong
cellular reaction for S100 (1:3,000; Dako) were present (Fig. 3).
The microscopic features, particularly with respect
to the pattern of growth and the presence of peripheral lymphoid
tissue with germinal centers, and the association with the
immunohistochemical features, were conclusive for a final
histological diagnosis of a gastric tumor with Schwann cells or a
gastric schwannoma.
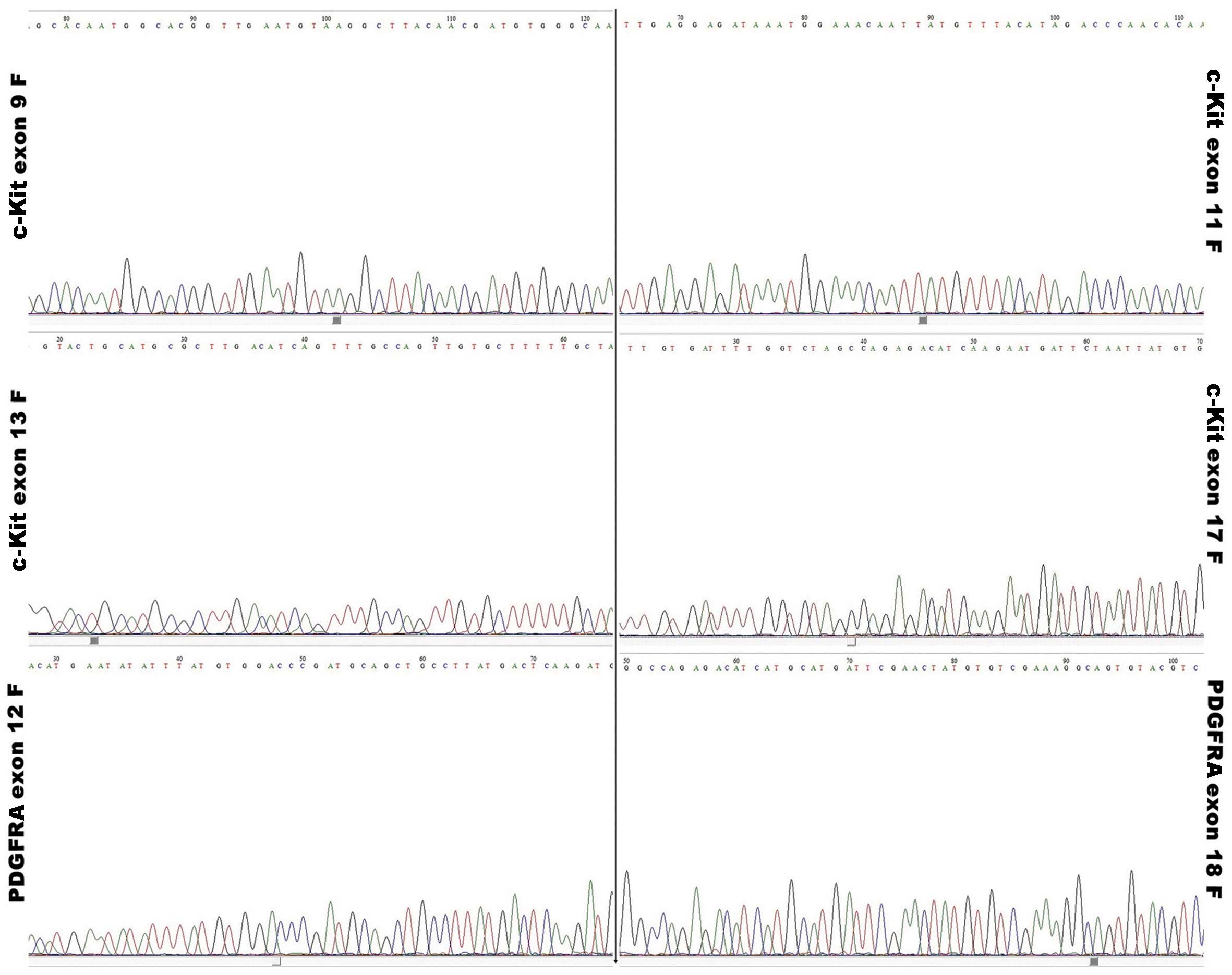
Finally, following the histological diagnosis, in
order to completely solve the problem of the differential diagnosis
with a GIST, a mutational analysis of the c-Kit and PDGFRA genes
was performed. A representative formalin-fixed, paraffin-embedded
(FFPE) sample of the case was selected and following DNA
purification (QIAamp DNA FFPE Tissue kit; Qiagen, Valencia, CA,
USA), polymerase chain reaction (PCR) was performed on 25–50 ng of
isolated genomic DNA in a 9700 Thermal Cycler (Applied Biosystems,
Foster City, CA, USA). All PCR-amplified products were directly
sequenced using an automated fluorescence-cycle sequencer (ABI
PRISM 3130; Applied Biosystems). No c-Kit or PDGFRA mutations were
detected in the sample (Fig. 4).
Written informed consent was obtained from the
patient for publication of this study and the accompanying images.
Currently the patient is well and is still undergoing follow-up at
INT Fondazione Pascale Hospital.
Discussion
Gastric schwannomas are rare stromal tumors that
consist of spindle cells of the gastrointestinal tract and arise
from the Schwann cells of the gastrointestinal neural plexus. The
stomach is the preferential site of localization and schwannomas
represent ~0.2% of all gastric neoplasms (12).
The differential diagnosis for this neoplasm is
difficult due to the macroscopic and microscopic similarities with
other typical lesions of the stomach. In particular, the presence
of spindle cells that are slow growing and covered with normal
mucosa is common to a large series of gastric tumors defined
generically as ‘spindle cell tumors of the gastrointestinal tract’
(13).
However, immunohistochemical staining is useful in
these cases, as S100 protein staining can be applied for
differentiating schwannomas from other spindle cell tumors of the
stomach (7). Generally, S100
protein-positive and smooth muscle actin- and c-Kit-negative tumor
cells support the diagnosis of a schwannoma (11).
The patient in the present study came to our
attention due to a presumptive diagnosis of a GIST, based solely on
radiographic and endoscopic investigations. The tumor sample
exhibited sub-mucosal layers, covered by normal gastric mucosa, and
was morphologically characterized by spindle cells nests and cords,
and rare epithelioid cells, with a fasciculated/storiform growth
pattern.
An immunohistochemical study was performed to
correctly define the histomorphological features of the lesion. The
IHC panel showed strong positivity for S100 and negativity for
c-Kit, CD34, SMA and desmin. These observations alone could be
sufficient to exclude a diagnosis of GIST, however, GISTs are also
characterized by several activating mutations in the c-Kit and
PDGFRA genes (8). The majority of the
mutations are located in the juxtamembrane domain (exon 11),
followed by the extracellular domain (exon 9) and less commonly,
the kinase domains (exon 13 and 17). The most common mutations in
PDGFRA are located in exons 12, 14 and 18. c-Kit and PDGFRA
mutations appear to be mutually exclusive oncogenic events in GISTs
(8).
For this reason, a mutational analysis was performed
in the present study to detect c-Kit and PDGFRA mutations in the
tumor sample, but no gene alterations were found.
Therefore, molecular analysis appears to be
extremely useful, even if it is more expensive than in situ
analyses and the response times are much longer. In any case, the
IHC evaluation may be indicative of the presence of activating
mutations of the two genes.
However, a previous study showed that in a small
percentage of GISTs, immunohistochemistry was negative for c-Kit
protein staining, negative for desmin and S100 protein in the
majority of cases, and positive for smooth muscle actin in ~50% of
cases (14).
The present IHC panel and the molecular analysis
supported the gastric schwannoma diagnosis. The correct diagnosis
is also crucial in order to determine the correct therapeutic
strategies. In fact, while gastric schwannoma has a good prognosis
and the post-operative prognosis is excellent, recurrent disease is
in fact generally associated only with an incomplete surgical
margin. The prognosis of patients with GISTs is poor owing to the
frequent recurrence, and the resistance to chemotherapy and
radiotherapy regimens (15). GISTs
with several point mutations in the c-Kit gene may benefit from the
use of specific receptor tyrosine kinase inhibitors, such as
imatinib mesylate (Gleevec) (15).
In conclusion, the correct histomorphological
revision, supported by specific IHC panel and molecular
investigations, to exclude in particular the diagnosis of GISTs, is
fundamental, as misdiagnosis may prevent the patient from
benefiting from specific target therapies.
References
|
1
|
Melvin WS and Wilkinson MG: Gastric
schwannoma. Clinical and pathologic considerations. Am Surg.
59:293–296. 1993.PubMed/NCBI
|
|
2
|
Braumann C, Guenther N, Menenakos C and
Junghans T: Schwannoma of the colon mimicking carcinoma: A case
report and literature review. Int J Colorectal Dis. 22:1547–1548.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jacobson BC, Hirsch MS, Lee JH, Van Dam J,
Shoji B and Farraye FA: Multiple asymptomatic plexiform schwannomas
of the sigmoid colon: A case report and review. Gastrointest
Endosc. 53:801–804. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tokunaga T, Takeda S, Sumimura J and Maeda
H: Esophageal schwannoma: Report of a case. Surg Today. 37:500–502.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kitada M, Matsuda Y, Hayashi S, Ishibashi
K, Oikawa K and Miyokawa N: Esophageal schwannoma: A case report.
World J Surg Oncol. 11:2532013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hirose T, Ishizawa K, Sakaki M and Fujii
Y: Retroperitoneal schwannoma is characterized by a high incidence
of cellular type and GFAP-immunoreactivity. Pathol Int. 62:456–462.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sarlomo-Rikala M and Miettinen M: Gastric
schwannoma - a clinicopathological analysis of six cases.
Histopathology. 27:355–360. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lasota J and Miettinen M: Clinical
significance of oncogenic KIT and PDGFRA mutations in
gastrointestinal stromal tumours. Histopathology. 53:245–266. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ogasawara N, Sasaki M, Ishiguro H, Itoh Y,
Nojiri S, Kubota E, Wada T, Kataoka H, Kuwabara Y and Joh T:
Gastric schwannoma with adjacent external progression harbored
aberrant NF2 gene. Dig Endosc. 21:192–195. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
de Díaz Ståhl T, Hansson CM, de Bustos C,
Mantripragada KK, Piotrowski A, Benetkiewicz M, Jarbo C, Wiklund L,
Mathiesen T, Nyberg G, et al: High-resolution array-CGH profiling
of germline and tumor-specific copy number alterations on
chromosome 22 in patients affected with schwannomas. Hum Genet.
118:35–44. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Voltaggio L, Murray R, Lasota J and
Miettinen M: Gastric schwannoma: A clinicopathologic study of 51
cases and critical review of the literature. Hum Pathol.
43:650–659. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Snyder RA, Harris E, Hansen EN, Merchant
NB and Parikh AA: Gastric schwannoma. Am Surg. 74:753–756.
2008.PubMed/NCBI
|
|
13
|
Miettinen M and Lasota J: Histopathology
of gastrointestinal stromal tumor. J Surg Oncol. 104:865–873. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Miettinen M, Sobin LH and Sarlomo-Rikala
M: Immunohistochemical spectrum of GISTs at different sites and
their differential diagnosis with a reference to CD117 (KIT). Mod
Pathol. 13:1134–1142. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Papaetis GS and Syrigos KN: Targeted
therapy for gastrointestinal stromal tumors: Current status and
future perspectives. Cancer Metastasis Rev. 29:151–170. 2010.
View Article : Google Scholar : PubMed/NCBI
|