Introduction
Hodgkin's lymphoma (HL) is a unique type of lymphoma
that is one of the most common malignant tumors in young
individuals. HL is an uncommon malignancy, with 7,000-7,500 novel
cases diagnosed annually in the USA; however, the incidence of the
disease in China is lower compared with the global average
(1,2).
The majority of HL patients present with early stage disease
(3). Pathology is an important means
of diagnosis and classification. Primary ABVD combination
chemotherapy [25 mg/m2 intravenous (i.v.) pirarubicin,
10 mg/m2 i.v. bleomycin, 375 mg/m2 i.v.
dacarbazine and 1.4 mg/m2 i.v. vincristine; days 1 and
5], followed by involved-field irradiation is the standard
treatment for patients with early-stage HL, with an overall
survival (OS) >95% (4).
Multiple myeloma (MM) is a tumor that generally
effects in the elderly; it is a neoplastic plasma-cell disorder
that may be distinguished by the clonal proliferation of malignant
plasma cells in the bone marrow and the presence of monoclonal
protein in the blood or urine (5).
The disease is associated with organ dysfunction. MM accounts for
~1% of neoplasms and 13% of hematological cancers. In western
countries, the annual age-adjusted incidence is 5.6 cases per
100,000 population (6). Eventually,
numerous complications tend to appear alongside the disease,
including bone destruction, anemia, renal insufficiency,
hypercalcemia and susceptibility to infection (5). In recent years, the OS and
progression-free survival of MM has been increasing due to the
application of targeted drugs, including bortezomib, thalidomide
and lenalidomide (7). The coexistence
of HL and MM is rare (8–10). The current study reports the case of a
patient who presented with HL and MM at the same time, for which a
good outcome was achieved using chemotherapy.
Case report
A 45-year-old man was admitted to The Fourth
Hospital of Hebei Medical University (Shijiazhuang, Hebei, China)
in May 2012 due to lumbago and intermittent fever that had been
apparent since March 2012. The patient's temperature was ~39°C,
without the symptoms of chills, coughing, abdominal pain or
diarrhea. Since the symptoms first occurred, the patient had
experienced no night sweats or weight loss. The patient was
previously healthy with no relevant family medical history. Upon
physical examination, the patient's temperature was 38.5°C (normal
range, 36–37°C), with a pulse rate of 108 beats/min (normal range,
60–100 beats/min), a respiratory rate of 20 breaths/min (normal
range, 16–20 breaths/min), and a blood pressure of 134/90 mmHg
(normal range, 90–140/60–90 mmHg). Two lymph nodes, ~1 cm in
diameter, were palpable in the left supraclavicular region, and one
lymph node, ~3 cm in diameter, was palpable in the left armpit. The
patient experienced pain upon percussion over the fourth and fifth
lumbar vertebrae.
The complete blood count revealed a white blood cell
count of 9.64×109/l (normal range,
4–10×109/l), a hemoglobin level of 107.4 g/l (normal
range, 120–160 g/l) and a platelet count of 177.7×109/l
(normal range, 100–300×109/l), and the erythrocyte
sedimentation rate was 111 mm/h (normal range, <15 mm/h).
Routine blood biochemical examination revealed the following: Total
serum protein, 123.1 g/l (normal range, 65–85 g/l); albumin, 28.5
g/l (normal range, 40–55 g/l); globulin, 40.3 g/l (normal range,
20–40 g/l); immunoglobulin G (IgG), 14.2 g/l (normal range, 8–16
g/l); IgA, 10 g/l (normal range, 0.5–2.2 g/l); and IgM, 1.1 g/l
(normal range, 0.7–3.3 g/l). The lactate dehydrogenase level was
4.157 units/l (normal range, 80–250 units/l), and the β2
microglobulin (β2-MG) and C-reactive protein levels were 3.68
(normal range, 0.8–2.80 mg/l) and 84.4 mg/l (normal range, 0–8
mg/l), respectively.
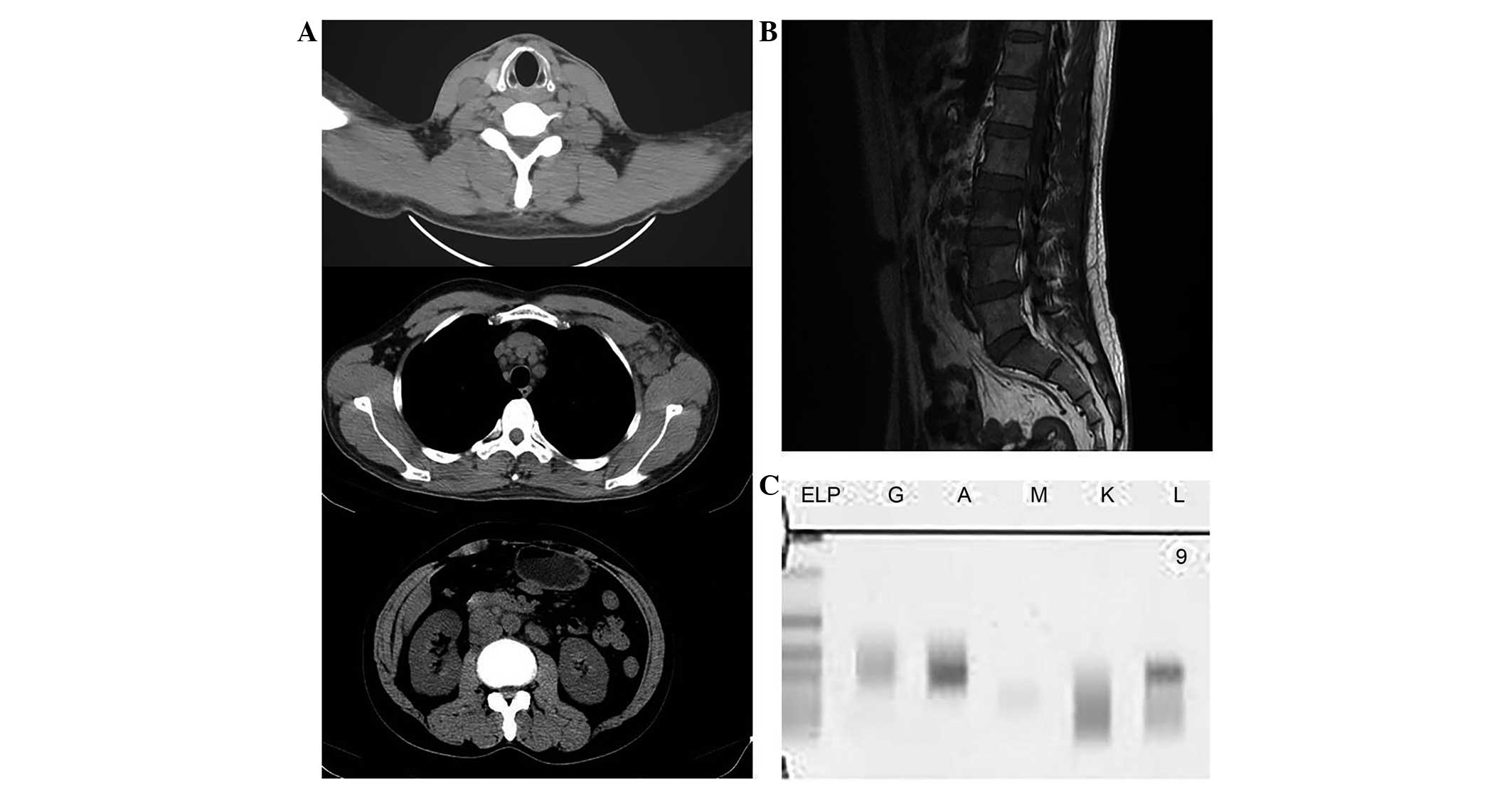
The routine whole-body scan showed diffuse lymph
node enlargement and a small amount of fluid accumulation in the
pelvic cavity (Fig. 1A). The lumbar
magnetic resonance imaging showed multiple low signals in the
thoracic, lumbar and sacral spine (Fig.
1B).
Serum protein electrophoresis was performed by
capillary zone electrophoresis (Paragon CZE 2000; Beckman Coulter
Inc., Brea, CA, USA). The antiserum of IgG, IgA, IgM, κ and λ light
chain proteins were tested and serum immunofixation electrophoresis
demonstrated a spike in IgA λ chains (Fig. 1C).
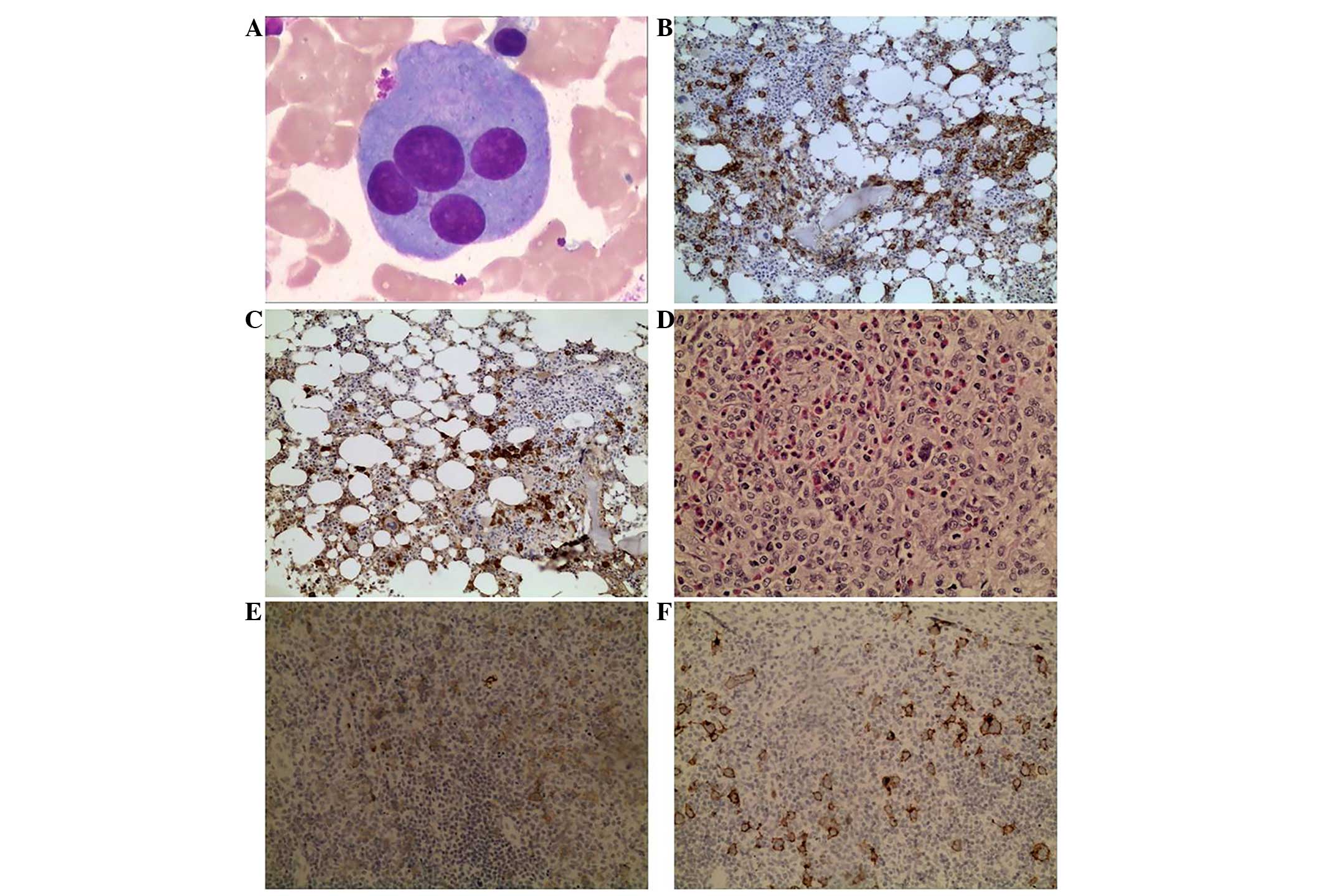
The bone marrow aspiration showed that MM cells
accounted for 20% of the nucleated cells (Fig. 2A). The lymph node and bone marrow
biopsies were 4% formalin-fixed, paraffin-embedded and sectioned
(4–5 µm thick) for staining. Routine hematoxylin and eosin staining
and necessary immunohistochemical (IHC) staining were performed
using the polymer-enhanced two-step IHC method (11). For the IHC analysis of the
paraffin-embedded sections, the antibodies that were selected
included: Mouse anti-human monoclonal antibodies, cluster of
differentiation (CD)20 (dilution, 1:100; catalog no., Kit-0001),
Ki67 (dilution, 1:200; catalog no., Kit-0005), CD4 (dilution,
1:200; catalog no., MAB-0251), CD15 (dilution, 1:200; catalog no.,
MAB-0015), CD21 follicular dendritic cells (dilution, 1:200;
catalog no., MAB-0339), CD30 (dilution, 1:200; catalog no.,
MAB-0023), CD38 (dilution, 1:200; catalog no., MAB-0341), CD56
(dilution, 1:200; catalog no., Kit-0028), CD138 (dilution, 1:200;
catalog no., MAB-0200), CD163 (dilution, 1:200; catalog no.,
MAB-0206), κ light chain (dilution, 1:200; catalog no., MAB-0356),
λ light chain (dilution, 1:200; catalog no., MAB-0357), CD45
leucocyte common antigen (LCA) (dilution, 1:200; catalog no.,
Kit-0024) and melanoma associated antigen (mutated) 1 (MUM1)
(dilution, 1:200; catalog no., MAB-0339); mouse anti-virus
monoclonal Epstein-Barr encoded RNA (EBER) antibody (dilution,
1:200; catalog no., MAB-0339); programmed cell death 1 (dilution,
1:50; catalog no., MAB-0654) and Vs38c (dilution, 1:200; catalog
no., MAB-0296) antibodies; rabbit anti-human monoclonal CD3ε
(dilution, 1:200; catalog no., Kit-0003) and paired box 5 (Pax5)
(dilution, 1:200; catalog no., RMA-0611) antibodies; rabbit
anti-human polyclonal IgM antibody (dilution, 1:200; catalog no.,
RAB-0103); and goat anti-human polyclonal chemokine (C-X-C motif)
ligand 13 (CXCL13) antibody (dilution, 1:200; catalog no.,
GAB-0616). All primary antibodies were purchased from Fuzhou Maixin
Biotech. Co., Ltd. (Fuzhou, China). Secondary antibodies used were
from ultraView Universal DAB Detection kit (Roche Diagnostics,
Mannheim, Germany). Primary antibodies were incubated for 2 h at
37°C and secondary antibodies were incubated for 24 h at 4°C.
The IHC results of the bone marrow biopsy showed
positive staining for CD138, CD38, Ki-67, MUM1 and the κ and λ
light chains, and negative staining for CD3ε, CD30, Pax5, CD20,
EBER, CD56, IgM and Vs38c (Fig. 2B and
C). Excisional lymph node biopsy showed enlarged lymph nodes
with effaced nodal architecture, which was replaced by a mixed
inflammatory infiltrate with scattered large-sized classical
Reed-Sternberg cells (Fig. 2D). The
immunohistochemical analysis showed positive staining of the cells
for CD163, Pax5, CD30, CD15, CD3ε, CD4, CD21 follicular dendritic
cells, programmed cell death 1 and Ki-67 (40%), and negative
staining of the cells for CD20, EBER, CD45 LCA and CXCL13 (Fig. 2E and F). The patient was subsequently
diagnosed with mixed cellularity HL, stage IIIB, according to the
Ann Arbor System (12), combined with
MM (IgA λ), stage IIIA, according to the Durie-Salmon System
(13).
The patient received 3 cycles of chemotherapy,
consisting of 25 mg/m2 i.v. pirarubicin, 10
mg/m2 i.v. bleomycin, 375 mg/m2 i.v.
dacarbazine and 1.4 mg/m2 i.v. vincristine on days 1 and
15, and 100 mg oral (p.o.) thalidomide on days 1–28 (ABVDT
regimen). This resulted in a complete response (CR) for the HL and
partial remission for the MM. Following 3 further cycles of ABVDT
chemotherapy, a CR was maintained for the HL and a stable disease
(SD) state was achieved for the MM. The patient subsequently
received 2 cycles of chemotherapy consisting of 0.5 mg/day i.v.
vincristine, 10 mg/m2 i.v. pirarubicin and 10
mg/m2 i.v. dexamethasone on days 1–4 and 9–12, and 100
mg p.o. thalidomide on days 1–28). The patient refused autologous
stem cell transplantation, but was administered maintenance
treatment consisting of weekly dexamethasone (7.5 mg) and daily
thalidomide (100 mg) tablets, with dexamethasone alternated with
thalidomide every 3 months. During 2 years of follow-up, the
patient has maintained a CR for the HL and a SD state for the MM,
and continues to be followed up every 6 months.
Discussion
HL is a malignant tumor that is derived from the
lymphoid tissues; the incidence rate of HL is 1.4–6.5 cases/100,000
individuals in China (14). In 2013,
~9,000 cases of HL were diagnosed in the United States and 1,180
individuals were predicted to succumb to the disease (8). Nodular sclerosing HL is more common in
the developed countries of Europe and America, while mixed
cellularity HL is more common in China. Classic HL represents ~10%
of all lymphomas diagnosed annually in the developing world
(8). MM is a clonal B-cell disorder
with characteristic B-lymphocyte and plasma cell proliferation and
accumulation. The annual incidence of the disease is 6
cases/100,000 individuals in Western countries, thus representing
the second most frequently occurring hematological malignancy
following non-HLs. In China, the annual incidence of MM is ~1
case/100,000 individuals (9,10). The simultaneous occurrence of two
types of lymphatic system malignant tumor within the same patient
is extremely rare, with an occurrence rate of 1.4–6.5
cases/1,000,000 individuals (15).
The pathogenesis of this simultaneous occurrence are
not yet clear. Previous studies have also reported the simultaneous
occurrence of HL and chronic lymphocytic leukemia, peripheral
T-cell lymphoma or diffuse large B-cell lymphoma (16–18).
Furthermore, certain patients have developed plasmocytoma (15,19), MM
(20,21) or monotypic plasma cell proliferations
of unknown significance (22)
following therapy for HL; it is unclear whether such secondary
tumors are associated with the side effects of the first cancer
treatment. Hasskarl et al (23) suggested that MM is associated with
hematological neoplasms. A total of 589 consecutive cases of MM
were reviewed, and 13 (2.2%) were found with different
hematological neoplasms. Those MM patients with prior or
synchronously (p/s) different neoplasms exhibited a hazard ratio
(HR) of 1.2 [95% confidence interval (CI), 0.8–2.0) for impaired
OS, whereas those with subsequent neoplasms exhibited an HR of 2.5
(95% CI, 1.4–4.4). These results indicated that p/s different
neoplasms occur more frequently than subsequent different
neoplasms, and that a worse prognosis is associated with subsequent
different neoplasms. However, the simultaneous occurrence of HL and
MM is extremely rare, with only a few reported cases. One of these
studies from 1999 (24) described the
case of a 37-year-old man who presented with a 10×8-cm, right
cervical tumor that was found by the patient 6 months previously.
The patient experienced fatigue and a loss of appetite. Following a
biopsy of the cervical lymph node, a histological diagnosis was
formed of nodular sclerosing HL with a Langerhans cell focus in an
affected node. Serum electrophoresis revealed an IgA κ paraprotein
level of 3,200 mg and a β2-MG level of 7.6 mg/l. Free
immunoglobulin κ light chains were detected in the urine. X-ray
examination of the skeleton revealed osteolytic lesions in the
ribs, the calvarium, the dorsolumbar region of the vertebral
column, the pelvis and the femoral metaphyses. Computed tomography
revealed enlargement of the bilateral cervical lymph nodes without
enlargement of the spleen, liver or other lymph nodes. Bone marrow
examination demonstrated extensive infiltration by atypical plasma
cells. MM without bone marrow HL infiltration was considered as the
final diagnosis, and 3 cycles of ABVD led to complete remission of
the HL.
In 2000, Lalayanni et al (25) reported the case of a 52-year-old male
who was diagnosed with simultaneous MM and HL in the absence of any
prior treatment. Autonomous progression of plasma cell dyscrasia
did not occur, but was instead associated with HL. In June 1993,
the patient presented with a relapsing-remitting fever that had
persisted for 3 months. Physical and laboratory findings were
normal, with the exception of anemia (hemoglobin, 9 g/dl), an
erythrocyte sedimentation rate of 102 mm/h and the presence of an
IgG-κ monoclonal component with Bence-Jones protein in the urine.
Up to 60% plasma cell infiltration of the bone marrow was
determined, but a bone X-ray was normal. A diagnosis of MM was
formed and the patient was administered melphalan-prednisolone.
After 2 months, all the findings remained unchanged and left
axillary lymphadenopathy developed. Mixed cellularity HL (stage
IIB) was revealed upon biopsy. The patient achieved complete
remission of each malignancy following 6 courses of
cyclophosphamide, vincristine, procarbazine and prednisone/ABVD and
involved-field radiotherapy. The HL (stage IIIB) relapsed 1 year
later. Complete remission was achieved again for 4 months with a
chlorambucil, vinblastine, procarbazine and prednisolone regimen,
however, following this, relapse of the two diseases was noted. Two
courses of intermediate-dose melphalan were not successful in
achieving control of either disease. Infiltration of the bone
marrow by Hodgkin and plasma cells was demonstrated on biopsy.
These findings were more compatible with constitutional mosaicism.
Another 3 courses of ABVD led to complete remission of the HL and
MM for the third time, however, the patient succumbed to acute
hepatitis B and hepatic failure.
It has been suggested that certain HL cases are of
B-cell origin (26,27). Malignant HL cells could be a
consequence of the arrest of maturation in the B-cell series, and,
by contrast, plasma cell neoplasms could be a consequence of the
complete differentiation of these cells (28). A decrease in cell-mediated immunity in
HL may also explain the presence of other neoplasms, such as MM,
and similar abnormalities in karyotype have been found within them
(29). Cytokines, such as interleukin
6 (IL-6), may be important in the formation of each disease. In
addition to acting as a factor for plasma cell growth and apoptosis
(30), IL-6 mRNA is also expressed in
Reed-Sternberg cells (infiltrating the marrow), and high IL-6
levels are found in advanced HL (31). Although this stimulus does not appear
to be sufficient enough for the promotion of monoclonality, excess
IL-6 in the marrow microenvironment may be able to directly
stimulate the long-living plasma cells located there (28).
The coexistence of HL and MM is rare, and the
pathogenesis is unclear, with few cases reported in the literature;
however, the present literature review indicates that the two
tumors may be associated. The management therapy for this entity is
not standardized, as studies in the literature are confined to a
small number of case reports and small case series. The current
study reports a rare case in which two types of low-incidence
hematological neoplasm occurred simultaneously in the same patient.
A B lymphocyte tumor and plasma cell neoplasm were present in the
patient, which provided more information to enable the future
optimization of treatment. Further study of such cases will aim to
explain the associations between these two tumors and provide
improved treatment selection.
References
|
1.
|
Townsend W and Linch D: Hodgkin's lymphoma
in adults. Lancet. 380:836–847. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Glaser SL and Hsu JL: Hodgkin's disease in
Asians: Incidence patterns and risk factors in population-based
data. Leuk Res. 26:261–269. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Gobbi PG, Ferreri AJ, Ponzoni M and Levis
A: Hodgkin lymphoma. Crit Rev Oncol Hematol. 85:216–237. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Klasa RJ, Connors JM, Fairey R, Gascoyne
R, Hoskins P, O'Reilly S, Shenkier T, Voss K and Wilson K: British
Columbia Cancer Agency (BCCA): Treatment of early stage Hodgkin's
disease: Improved outcome with brief chemotherapy and radiotherapy
without staging laparotomy. Annal Oncol. 7(Suppl 3): 211996.
|
|
5.
|
Raab MS, Podar K, Breitkreutz I,
Richardson PG and Anderson KC: Multiple myeloma. Lancet.
374:324–339. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Palumbo A and Anderson K: Multiple
myeloma: N Engl J Med. 364:1046–1060. 2011.
|
|
7.
|
Sonneveld P, Schmidt-Wolf IG, van der Holt
B, El Jarari L, Bertsch U, Salwender H, Zweegman S, Vellenga E,
Broyl A, Blau IW, et al: Bortezomib induction and maintenance
treatment in patients with newly diagnosed multiple myeloma:
Results of the randomized phase III HOVON-65/ GMMG-HD4 trial. J
Clin Oncol. 30:2946–2955. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Diefenbach C and Advani R: Customized
targeted therapy in Hodgkin lymphoma: Hype or hope? Hematol Oncol
Clin North Am. 28:105–122. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Tosi P: Diagnosis and treatment of bone
disease in multiple myeloma: Spotlight on spinal involvement.
Scientifica (Cairo). 2013:1045462013.PubMed/NCBI
|
|
10.
|
Jemal A, Siegel R, Xu J and Ward E: Cancer
statistics, 2010. CA Cancer J Clin. 60:277–300. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Sabattini E, Bisgaard K, Ascani S, Poggi
S, Piccioli M, Ceccarelli C, Pieri F, Fraternali-Orcioni G and
Pileri SA: The EnVision++ system: A new immunohistochemical method
for diagnostics and research. Critical comparisonwith the APAAP,
ChemMate, CSA, LABC, and SABC techniques. J Clin Pathol.
51:506–511. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Durie BG and Salmon SE: A clinical staging
system for multiple myeloma. Correlation of measured myeloma cell
mass with presentingclinical features, response to treatment, and
survival. Cancer. 36:842–854. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Smithers DW: Summary of papers delivered
at the Conference on Staging in Hodgkin's Disease (Ann Arbor).
Cancer Res. 31:1869–1870. 1971.PubMed/NCBI
|
|
14.
|
Yang QP, Zhang WY, Yu JB, Zhao S, Xu H,
Wang WY, Bi CF, Zuo Z, Wang XQ, Huang J, et al: Subtype
distribution of lymphomas in Southwest China: Analysis of 6,382
cases using WHO classification in a single institution. Diagn
Pathol. 6:772011. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Gherlinzoni F, Cavo M, Pileri S, Rivano
MT, Boriani S, Biagini R and Emiliani E: Solitary plasmocytoma of
the bone in a case of Hodgkin's disease. Acta Haematol. 76:178–180.
1986. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Weisenberg E, Anastasi J, Adeyanju M,
Variakojis D and Vardiman JW: Hodgkin's disease associated with
chronic lymphocytic leukemia. Eight additional cases, including two
of the nodular lymphocyte predominant type. Am J Clin Pathol.
103:479–484. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Chan WC, Griem ML, Grozea PN, Freel RJ and
Variakojis D: Mycosis fungoides and Hodgkin's disease occurring in
the same patient. Report of three cases. Cancer. 44:1408–1413.
1979. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Harris NL: The relationship between
Hodgkin's disease and non-Hodgkin's lymphoma. Semin Diagn Pathol.
9:304–310. 1992.PubMed/NCBI
|
|
19.
|
Loutayf Ranea JJ: Lymph node plasmacytoma
as the 2d tumor in a patient with Hodgkin's disease. Medicina (B
Aires). 46:2521986.(In Spanish).
|
|
20.
|
Berkessy S, Radványi G, Nagy Z and Takács
I: A case of multiple myeloma, associated with terminal plasma cell
leukemia following recovery from Hodgkin's disease. Orv Hetil.
129:1053–1055. 1988.(In Hungarian). PubMed/NCBI
|
|
21.
|
Greenberg BB, Stats D and Goldberg M: The
simultaneous occurrence of plasma cell multiple myeloma and
Hodgkin's disease. N Y State J Med. 50:305–307. 1950.PubMed/NCBI
|
|
22.
|
Gelmann EP and Dennis LH: Plasma-cell
dyscrasia after alkylating-agent therapy for Hodgkin's disease. N
Engl J Med. 305:13501981. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Hasskarl J, Ihorst G, De Pasquale D,
Schröttner P, Zerweck A, Wäsch R and Engelhardt M: Association of
multiple myeloma with different neoplasms: Systematic analysis in
consecutive patients with myeloma. Leuk Lymphoma. 52:247–259. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
de Ibarrola Andrés C, Toscano R, Lahuerta
JJ and Martínez-González MA: Simultaneous occurrence of Hodgkin's
disease, nodal Langerhans' cell histiocytosis and multiple myeloma
IgA (kappa). Virchows Arch. 434:259–262. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Lalayanni C, Theodoridou S, Athanasiadou
A, Saloum R and Tsatalas C: Simultaneous occurrence of multiple
myeloma and Hodgkin's disease. A case report. Haematologica.
85:772–773. 2000.PubMed/NCBI
|
|
26.
|
Sundeen J, Lipford E, Uppenkamp M, Sussman
E, Wahl L, Raffeld M and Cossman J: Rearranged antigen receptor
genes in Hodgkin's disease. Blood. 70:96–103. 1987.PubMed/NCBI
|
|
27.
|
Bräuninger A, Hansmann ML, Strickler JG,
Dummer R, Burg G, Rajewsky K and Küppers R: Identification of
common germinal center B-cell precursors in two patients with both
Hodgkin's disease and non-Hodgkin's lymphoma. N Engl J Med.
340:1239–1247. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
Ibbotson RM, Revell PA, Molland EA and
Minton MJ: The simultaneous presence of Hodgkin's disease and
myeloma. Postgrad Med J. 53:52–53. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
Tilly H, Bastard C, Delastre T, Duval C,
Bizet M, Lenormand B, Daucé JP, Monconduit M and Piguet H:
Cytogenetic studies in untreated Hodgkin's disease. Blood.
77:1298–1304. 1991.PubMed/NCBI
|
|
30.
|
Lu ZY, Brailly H, Wijdenes J, Bataille R,
Rossi JF and Klein B: Measurement of whole body interleukin-6
(IL-6) production: Prediction of the efficacy of anti-IL-6
treatments. Blood. 86:3123–3131. 1995.PubMed/NCBI
|
|
31.
|
Seymour JF, Talpaz M, Hagermeister FB,
Cabanillas F and Kurzrock R: Clinical correlates of elevated serum
levels of interleukin-6 in patients with untreated Hodgkin's
disease. Am J Med. 102:21–28. 1997. View Article : Google Scholar : PubMed/NCBI
|