Introduction
Myeloproliferative neoplasms (MPNs) correspond to a
clonal proliferation of hematopoietic cells, resulting in expansion
of ≥1 lineages (1). Molecular markers
aid to characterize these disorders, and are useful for diagnosis
and follow-up of MPNs, since they enable the detection of minimal
residual disease, such as breakpoint cluster region-Abelson
(BCR-ABL) rearrangement in chronic myeloid leukemia (CML) (1). The Janus kinase 2 (JAK2) V617F mutation
is present in 95% of patients with polycythemia vera (PV) and in
~50% of patients with essential thrombocythemia (ET) and idiopathic
myelofibrosis (MF) (2–5). The association of CML with other forms
of MPN, in particular with the JAK2 V617F mutation, is very
uncommon, and there are limited cases reported in the literature
(6–8).
Pieri et al (9) performed a
screening of 314 patients with CML and identified 8 cases (2.55%)
with concomitant JAK2 V617F mutation.
Despite the rarity of the concomitant detection of
BCR-ABL and JAK2 V617F mutation, it is of great importance to
recognize and investigate this association, particularly when the
disease has an unusual course and the diagnosis of other MPNs may
have practical therapeutic consequences. Therefore, in the present
study, the case of a patient diagnosed with CML, in whom an ET with
JAK2 V617F mutation was detected during the course of CML
follow-up, is reported.
Case report
In March 2003, a 73-year-old male patient was
referred to the Hematology and Hemotherapy Center of the University
of Campinas (Campinas, Brazil) for a hematological evaluation, due
to leukocytosis detected in a routine exam. The patient had no
clinical symptoms, and presented a white blood cell count of
49.4×109 cells/l [normal range, 5.2–12.4×109
cells/l; 2% eosinophils (normal range, 0–7%), 4.0% basophils
(normal range, 0–1.5%), 1% blasts (normal range, 0%) and 2%
promyelocytes (normal range, 0%)], a platelets count of
607.0×109 platelets/l (normal range, 150–450×109/l) and
hemoglobin levels of 12.2 g/dl (normal range, 13.5–17.5 g/dl).
Diagnosis of CML was confirmed by conventional cytogenetic
analysis, using the Giemsa-trypsin-Wright stain banding technique,
which revealed the presence of the translocation t(9;22)(q34;q11)
in 20/20 metaphases examined, and by reverse
transcription-polymerase chain reaction (RT-PCR), which detected
the BCR-ABL rearrangement (b3a2) (10).
In consequence, the patient was treated with
interferon alfa-2a (6 million units/day; subcutaneous; Roche
Diagnostics, Basel, Switzerland) between April and May 2003, with
no hematological response. Thus, treatment with imatinib (400
mg/day; oral; Glivec; Novartis, Basel, Switzerland) was initiated
in May 2003. Subsequently, the white blood cell count returned to
the normal range, but the platelet count remained elevated. The
patient did not achieve a normal platelet count, despite increasing
the dose of imatinib to 700 mg/day, but achieved complete
cytogenetic remission 6 months later. However, his platelet count
increased progressively. Therefore other causes of thrombocytosis
were investigated. Ferritin levels were normal and the patient
showed increased prostate-specific antigen (PSA) levels (6.7 ng/ml;
normal range, 0–4 ng/ml), which suggested prostate cancer. Prostate
cancer was diagnosed by prostate biopsy. The patient was treated
with local radiotherapy with complete remission. Despite the
normalization observed in the PSA levels, the thrombocytosis
persisted. In November 2006, the patient achieved a major molecular
response (MR) in BCR-ABL levels, but platelets counts remained
increased (622×109 platelets/l). To further investigate whether
other MPNs were involved, the JAK2 V617F mutation was investigated
and detected by restriction fragment length polymorphism analysis,
as described previously (3), and
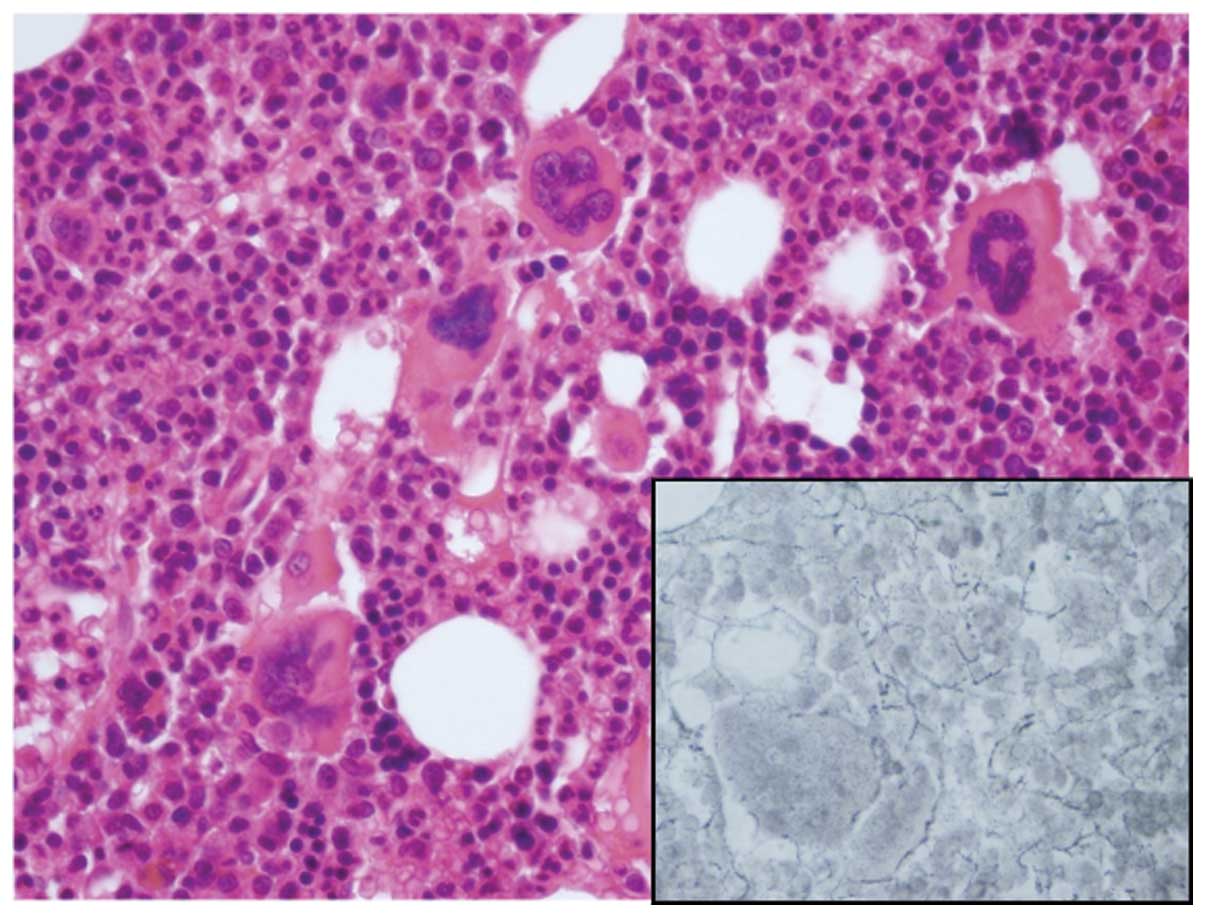
confirmed by direct Sanger sequencing. The bone marrow biopsies
conducted at the time of diagnosis and following treatment for CML
were reanalyzed, (Figs. 1 and
2, respectively). The post-treatment
biopsy displayed global hypercellularity, increased
myeloid:erythroid ratio and hyperplasia of atypical megakaryocytes,
with no fibrosis. The morphology of the megakaryocytes was
consistent with ET.
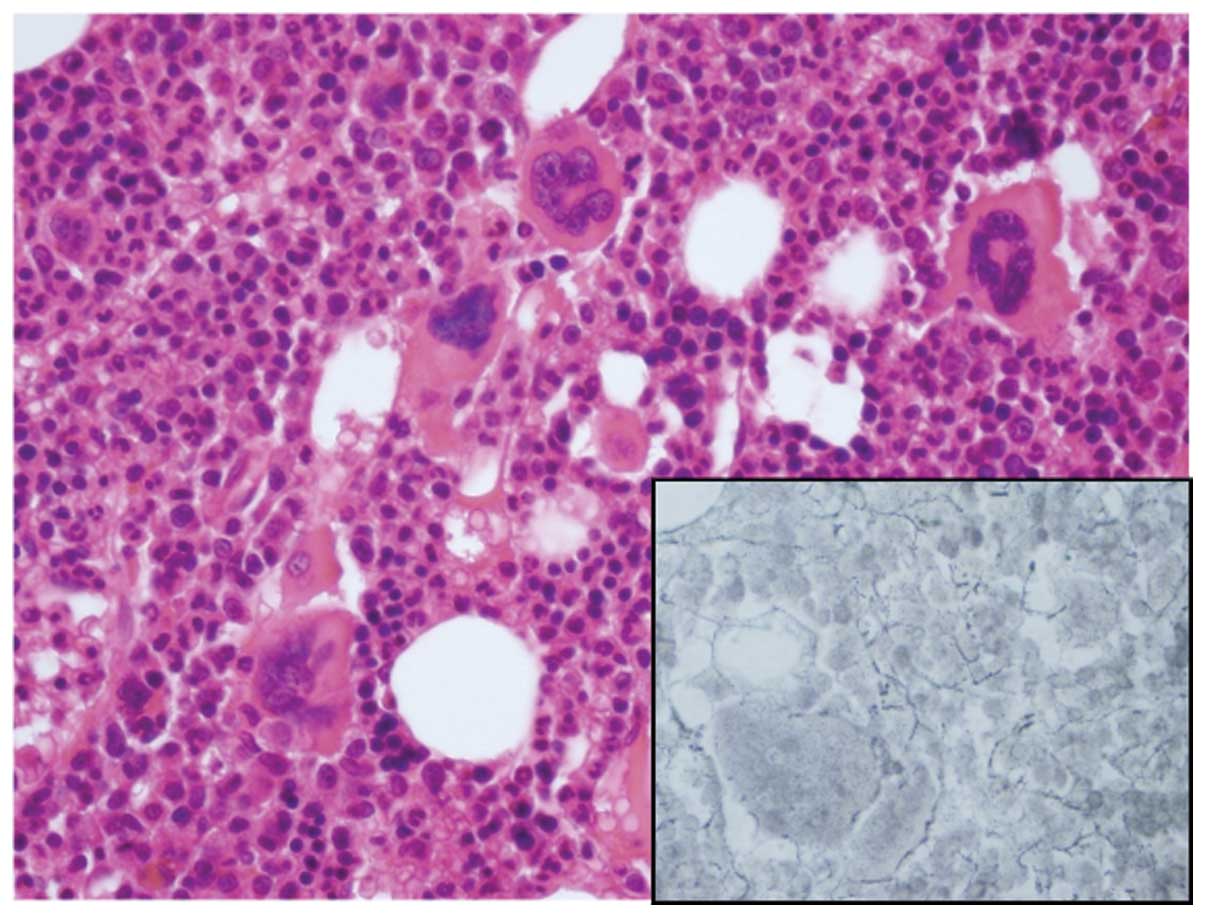 | Figure 2.Bone marrow histology following
treatment of chronic myeloid leukemia revealed features of
essential thrombocythemia, such as proliferation of pleomorphic,
hyperlobated megakaryocytes. Erythroblasts and myeloid elements
with normal morphology were also present. Hematoxylin and eosin
staining (Merck Millipore, Darmstadt, Germany); magnification, ×400
(Olympus CX31 optical microscope; Olympus America, Inc., Center
Valley, PA, USA). A mild increase in reticulin fibers
(Easypath-Erviegas, São Paulo, Brazil) was observed (inset; silver
impregnation; magnification, ×400) |
The imatinib dose was then decreased to 400 mg/day,
as the thrombocytosis was associated with ET and not due to
resistant CML. Since then, hydroxyurea (500 mg/day; oral; Hydrea;
Bristol Myers-Squibb, New York City, NY, USA), has been
administered concomitantly to control thrombocytosis. In the last
follow-up, in December 2015, >10 years following the start of
imatinib treatment, the patient maintains a complete cytogenetic
response and a deep molecular response [MR 4.5, according to the
international scale (11)], in the
BCR-ABL transcripts levels detected by RT-PCR, using a previously
described technique (12). No
thrombotic or hemorrhagic events has occurred.
Discussion
The association of JAK2 mutations and BCR-ABL
rearrangement is infrequent, and was recently reported in
association with MF (6,7,13,14) and PV (8,15,16). In a previous report by the present
authors, the presence of the JAK2 V617F mutation in CML was
reported to be rare, with the present case being the only one
detected among 55 cases of CML analyzed (17).
Bee et al (8)
reported a case of PV with JAK2 V617F mutation and BCR-ABL
rearrangement at diagnosis. In that report, the patient presented a
decrease in V617F alleles when the burden of BCR-ABL messenger RNA
increased, and reappearance of V617F clones following the
administration of imatinib. A similar case was reported by Ursuleac
et al (16), where a patient
with PV developed CML following 7 years of PV diagnosis. Wahlin
et al (18) described a case
of ET with emergence of CML during treatment with hydroxyurea. A
recent study by Mizutani et al (19) reported the emergence of CML during
treatment for ET in a patient following 9 years of diagnosis. By
contrast, Véronèse et al (6)
reported a case of CML developing ET upon achieving BCR-ABL major
MR, similarly to the present findings. In that case, the JAK2 clone
was present at low levels at CML diagnosis, while in the present
patient, the bone marrow histology was consistent with ET when the
mutation was detected, although molecular data regarding the JAK2
mutation was not available at the time of diagnosis.
In conclusion, the present report emphasizes that
the presence of persistent or increasing thrombocytosis in CML,
which is not responsive to treatment, should always be further
investigated. Bone marrow histology may be useful to exclude other
malignant diseases or to confirm other MPNs. In the present case,
JAK2 V617F mutation analysis was determinant in the final
characterization of ET associated with CML. Molecular
characterization of MPN at the time of diagnosis is necessary to
establish a correct diagnosis and to detect concomitant clones.
Although rare, the association of ET with CML may be identified at
diagnosis or may appear during treatment, and may require to alter
the therapeutic approach.
References
|
1
|
Swerdlow HS, Campo E, Harris NL, Jaffe ES,
Pileri SA, Stein H, Thiele J and Vardiman JW: WHO Classification of
Tumors of Haematopoietics and Lymphoid Tissues. 2:(4th). IARC.
Lyon: 23–25. 2008.
|
|
2
|
Baxter EJ, Scott LM, Campbell PJ, East C,
Fourouclas N, Swanton S, Vassiliou GS, Bench AJ, Boyd EM, Curtin N,
et al: Cancer Genome Project: Acquired mutation of the tyrosine
kinase JAK2 in human myeloproliferative disorders. Lancet.
365:1054–1061. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Monte-Mór BDCR, da Cunha AF, Pagnano KBB,
Saad ST, Lorand-Metze I and Costa FF: JAK V617F prevalence in
Brazilian patients with polycythemia vera, idiopathic myelofibrosis
and essential thrombocythemia. Genet Mol Biol. 30:336–338. 2007.
View Article : Google Scholar
|
|
4
|
Jones AV, Kreil S, Zoi K, Waghorn K,
Curtis C, Zhang L, Score J, Seear R, Chase AJ, Grand FH, et al:
Widespread occurrence of the JAK2 V617F mutation in chronic
myeloproliferative disorders. Blood. 106:2162–2168. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Levine RL, Wadleigh M, Cools J, Ebert BL,
Wernig G, Huntly BJ, Boggon TJ, Wlodarska I, Clark JJ, Moore S, et
al: Activating mutation in the tyrosine kinase JAK2 in polycythemia
vera, essential thrombocythemia, and myeloid metaplasia with
myelofibrosis. Cancer Cell. 7:387–397. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Véronèse L, Tchirkov A, Richard-Pebrel C,
Ledoux-Pilon A, Fleury J, Chaleteix C, Goumy C, Gouas L, Berger MG,
Vago P, et al: A thrombocytosis occurring in Philadelphia positive
CML in molecular response to imatinib can reveal an underlying
JAK2(V617F) myeloproliferative neoplasm. Leuk Res. 34:e94–e96.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Conchon MR, Costa JL, Novaes MM,
Dorlhiac-Llacer PE, de Alencar Fischer, Chamone D and Bendit I:
Simultaneous detection of JAK2 V617F mutation and Bcr-Abl
translocation in a patient with chronic myelogenous leukemia. Int J
Hematol. 88:243–245. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bee PC, Gan GG, Nadarajan VS, Latiff NA
and Menaka N: A man with concomitant polycythaemia vera and chronic
myeloid leukemia: The dynamics of the two disorders. Int J Hematol.
91:136–139. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pieri L, Spolverini A, Scappini B, Occhini
U, Birtolo S, Bosi A, Albano F, Fava C and Vannucchi AM:
Concomitant occurrence of BCR-ABL and JAK2V617F mutation. Blood.
118:344–346. 2011. View Article : Google Scholar
|
|
10
|
Cross NC, Melo JV, Feng L and Goldman JM:
(1994) An optimized multiplex polymerase chain reaction (PCR) for
detection of BCR-ABL fusion mRNAs in haematological disorders.
Leukemia. 8:186–189. 1994.PubMed/NCBI
|
|
11
|
Cross NC, White HE, Müller MC, Saglio G
and Hochhaus A: Standardized definitions of molecular response in
chronic myeloid leukemia. Leukemia. 26:2172–2175. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ribeiro BF, Vergílio BR, Miranda EC,
Almeida MH, Delamain MT, da Silveira RA, de Souza CA, Albuquerque
DM, Dos Santos A, Duarte VO, et al: BCR-ABL1 transcript levels at 3
and 6 months are better for identifying chronic myeloid leukemia
patients with poor outcome in response to second-line
second-generation tyrosine kinase inhibitors after imatinib
failure: A report from a single institution. Acta Haematol.
134:248–254. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jallades L, Hayette S, Tigaud I, Johnston
A, Coiffier B, Magaud JP and Ffrench M: Emergence of
therapy-unrelated CML on a background of BCR-ABL-negative JAK2
V617F-positive chronic idiopathic myelofibrosis. Leuk Res.
32:1608–1610. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pingali SR, Mathiason MA, Lovrich SD and
Go RS: Emergence of chronic myelogenous leukemia from a background
of myeloproliferative disorder: JAK2 V617F as a potential risk
factor for BCR-ABL translocation. Clin Lymphoma Myeloma. 9:E25–E29.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Toogeh G, Ferdowsi S, Naadali F,
Alimoghaddam K, Ghavamzadeh A, Shirkoohi R and Ghaffari SH:
Concomitant presence of JAK2 V617F mutation and BCR-ABL
translocation in a pregnant woman with polycythemia vera. Med
Oncol. 28:1555–1558. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ursuleac I, Colita A, Adam T, Jardan C,
Ilea A and Coriu D: The concomitant occurrence of JAK2 V617F
mutation and BCR/ABL transcript with phenotypic expression - an
overlapping myeloproliferative disorder or two distinct diseases? -
case report. J Med Life. 6:34–37. 2013.PubMed/NCBI
|
|
17
|
Pagnano KBB, Almeida D, Delamain MT, De
Souza AC and Lorand-Metze I: JAK2 V617F mutation evaluation of
chronic myeloid leukemia and acute myeloid leukemia. Rev Bras
Hematol Hemoter. 31:1692009.(In Portuguese).
|
|
18
|
Wahlin A and Golovleva I: Emergence of
Philadelphia positive chronic myeloid leukaemia during treatment
with hydroxyurea for Philadelphia negative essential
thrombocythaemia. Eur J Haematol. 70:240–241. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mizutani S, Kuroda J, Shimizu D, Horiike S
and Taniwaki M: Emergence of chronic myelogenous leukemia during
treatment for essential thrombocythemia. Int J Hematol. 91:516–521.
2010.
|