Introduction
Local treatment of early breast cancer has changed
during the last decade. Although the detection of small
non-palpable tumors is becoming more and more frequent, recent
literature reports that rates of unilateral and contralateral
prophylactic mastectomy (CPM) are increasing in patients who are
candidates to breast conserving surgery (1–4). The
present case study details a recently observed case at our
institution, with the aim of focusing on several important issues
in the setting of CPM in patients with unilateral breast
cancer.
Case report
A 52-year-old woman was referred to our institution
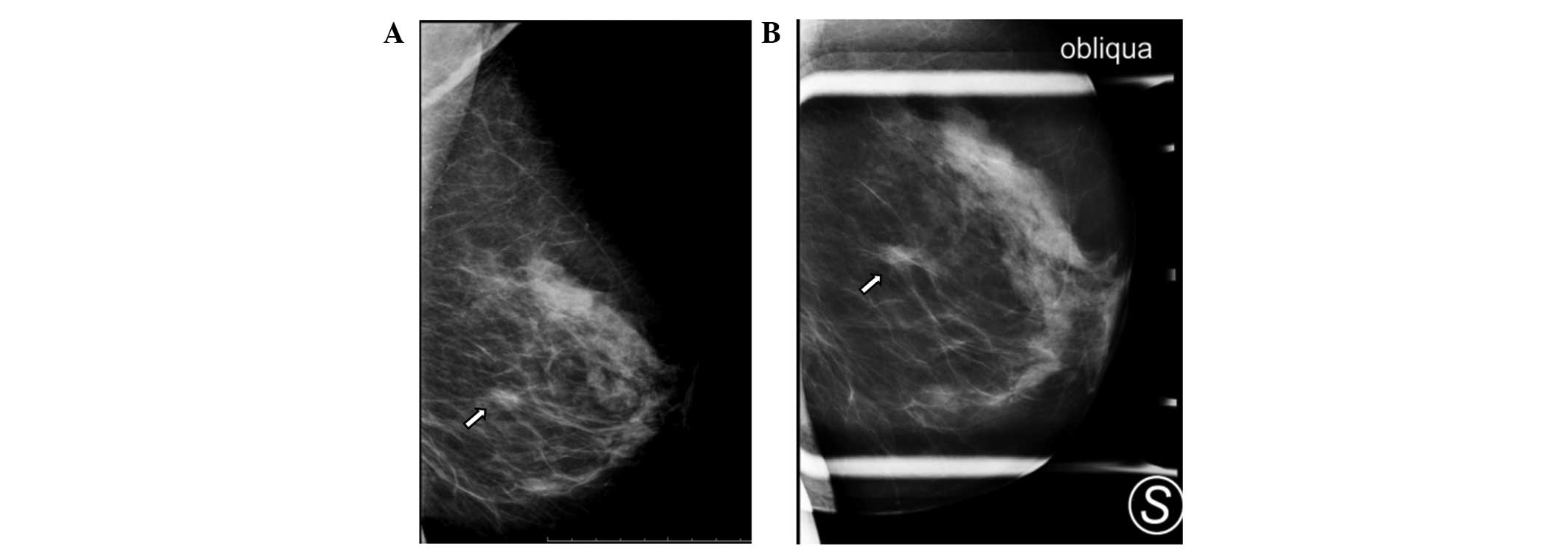
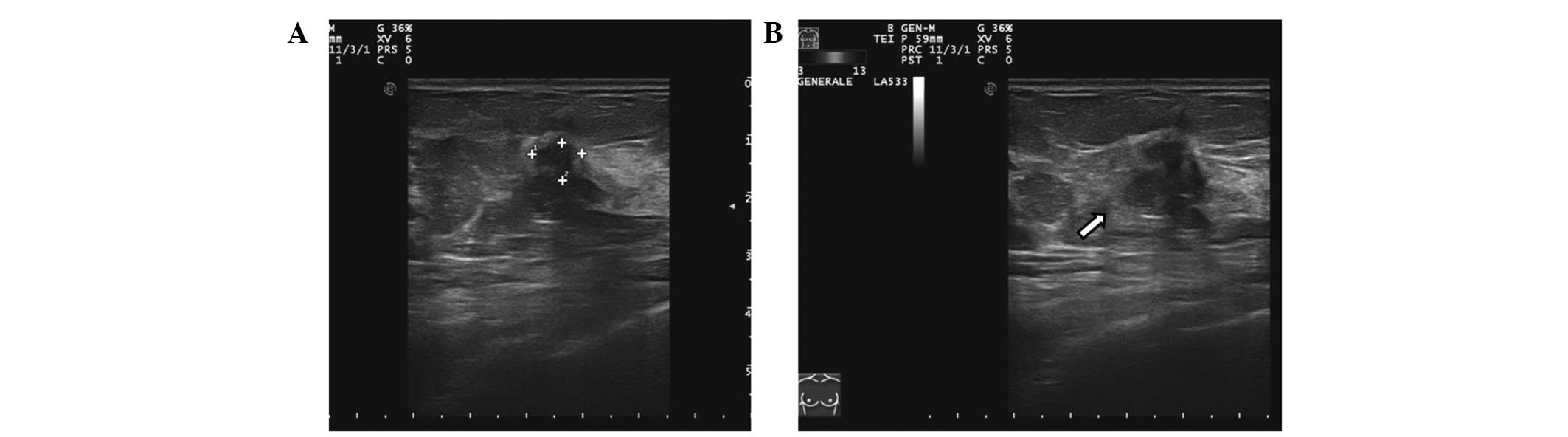
following a diagnosis of screen-detected breast cancer. Mammography
and ultrasonography demonstrated a 0.8 cm spiculated mass in the
lower outer quadrant of her left breast (Figs. 1 and 2).
A core-biopsy showed an infiltrating ductal carcinoma of grade 2.
The tumor was non-palpable on physical examination, and there were
neither palpable masses of the contralateral breast nor axillary
lymph node enlargement.
The patient was a mother of two sons who underwent
natural menopause at the age of 49. She had an unremarkable medical
history. The patient did not have any prior family history of
breast or ovarian cancer and was being medically treated for
hypertension. In response to the diagnosis of breast cancer, the
patient requested a bilateral mastectomy. After having visited the
patient and assessing her medical records, breast-conservation
surgery plus sentinel node biopsy followed by radiation therapy was
recommended for the patient, clarifying for her that, in the
considered opinion of the surgeon, the patient had a very low
probability of subsequently developing a contralateral breast
cancer.
The patient maintained that she considered bilateral
mastectomy and immediate reconstruction would be her preferred
option. In response to her appeal, after multidisciplinary team
discussions, breast-conserving surgery was again proposed as the
course of treatment; bilateral mastectomy was not considered to be
viable as an option.
In response to the recommendation from our medical
team, the patient elected to ask for a second, independent opinion
from another surgeon working at a different institution. The
patient then underwent a bilateral nipple-sparing mastectomy, with
sentinel node biopsy and immediate implant reconstruction. An
histological examination revealed no additional foci of cancer in
the ipsi- or contralateral breast, other than the index tumor. The
sentinel node biopsy was negative.
Subsequently, the patient returned to our
institution for wound care and postoperative oncological
consultation. The patient commenced endocrine therapy, and was
initially satisfied with the cosmetic results of the bilateral
reconstruction. At six months following the surgery, the patient
returned for a follow-up visit, complaining of occasional bilateral
breast pain and an almost complete loss of sensation in her
nipples. At the one-year follow-up visit, the patient disclosed a
general sense of discomfort linked to the surgical operation, and
complained of difficulties with her sexual life. The patient
expressed an opinion that she had begun to doubt the necessity of
having undergone a bilateral mastectomy, and considered that
breast-conserving surgery may been preferable as the treatment
option.
Discussion
For breast surgeons and their patients, the
decision-making process has become more and more complex in the
last decade. Rates of mastectomy are growing in patients with
breast cancer who are eligible for breast conservation (2–5). In
addition, rates of CPM are also on the rise for both invasive and
in situ cancer (1,6,7). There are
several reasons for these phenomena, including the increasing use
of preoperative MRI, the growing employment of immediate
post-mastectomy reconstruction, improvements in cosmetic results
with the relatively new techniques of skin- and nipple-sparing
mastectomy, the increasing use of genetic testing, and last but not
least, the patients' entitlement to choose their preferred surgery
option (6–12).
In the present case study, the recommended surgical
option was to perform breast-conserving surgery followed by
radiation therapy. A bilateral mastectomy was considered to be an
unnecessary and excessive intervention. In fact, it should be
recognized that the annual lifetime risk of contralateral breast
cancer is ~0.5–1%, and the cumulative 10 year risk is ~4–5%
(2,5).
Furthermore, the risk of developing a second, fatal breast cancer
is even lower. In a recent large series study, occult breast cancer
was identified in 6% of patients undergoing CPM (12). In particular, there are specific
situations in which the risk of developing a contralateral cancer
is higher than that reported above, such as familiarity for breast
cancer, axillary lymph node involvement, being under 50 years of
age at the time of diagnosis, previous chest wall irradiation, and
the presence of genetic mutations linked with hereditary breast
cancer (1,3–5).
Furthermore, it is known that patients with BRCA1/2 mutations have
a substantially higher risk of contralateral cancer compared with
sporadic counterparts, accounting for 12–20% within 5 years of
initial diagnosis (1,13).
In the present case study, the patient had none of
those risk factors. Our multidisciplinary breast cancer team
considered that they had explained exhaustively to the patient the
benefits and risks of bilateral mastectomy, focusing on the issue
that the risk of a second breast neoplasm was very low. It is
paradoxical that an increasing number of women are choosing to
undergo bilateral mastectomy in a setting in which rates of
contralateral breast cancer are decreasing, largely as a
consequence of adjuvant endocrine therapy (5,14).
Benefits of contralateral mastectomy include the diminishing need
for clinical and imaging surveillance, cosmetic symmetry in
selected cases, and a decreased risk of developing contralateral
breast cancer (1). However, the
latter should not be considered as an outcome from an oncological
point of view. In fact, novel techniques or approaches in surgical
oncology should be directed towards survival benefits rather than a
simple risk reduction. It is important to highlight that no studies
in the literature have demonstrated an advantage in terms of
survival by performing a contralateral mastectomy in patients with
unilateral breast cancer, except (probably) in the scenario of
germline mutations in breast-cancer susceptibility genes (1,2,6,15).
In conclusion, in the setting of unilateral breast
cancer eligible for breast conservation, bilateral mastectomy
should be attentively evaluated as an option only in patients with
a higher-than-average risk of developing a contralateral breast
cancer.
References
|
1
|
Tracy MS, Rosenberg SM, Dominici L and
Partridge AH: Contralateral prophylactic mastectomy in women with
breast cancer: Trends, predictors, and areas for future research.
Breast Cancer Res Treat. 140:447–452. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Stucky CC, Gray RJ, Wasif N, Dueck AC and
Pockaj BA: Increase in contralateral prophylactic mastectomy:
Echoes of a bygone era? Surgical trends for unilateral breast
cancer. Ann Surg Oncol. 17(Suppl 3): S330–S337. 2010. View Article : Google Scholar
|
|
3
|
Kummerow KL, Du L, Penson DF, Shyr Y and
Hooks MA: Nationwide trends in mastectomy for early-stage breast
cancer. JAMA Surg. 150:9–16. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Adkisson CD, Bagaria SP, Parker AS, Bray
JM, Gibson T, Thomas CS, Heckman MG and McLaughlin SA: Which
eligible breast conservation patients choose mastectomy in the
setting of newly diagnosed breast cancer? Ann Surg Oncol.
19:1129–1136. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Portschy PR and Tuttle TM: Rise of
mastectomy. J Surg Oncol. 107:563–564. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Soran A, Kamali Polat A, Johnson R and
McGuire KP: Increasing trend of contralateral prophylactic
mastectomy: What are the factors behind this phenomenon? Surgeon.
12:316–322. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Janssen S, Holz-Sapra E, Rades D, Moser A
and Studer G: Nipple-sparing mastectomy in breast cancer patients:
The role of adjuvant radiotherapy (Review). Oncol Lett.
9:2435–2441. 2015.PubMed/NCBI
|
|
8
|
Fancellu A, Soro D, Castiglia P, Marras V,
Melis M, Cottu P, Cherchi A, Spanu A, Mulas S, Pusceddu C, et al:
Usefulness of magnetic resonance in patients with invasive cancer
eligible for breast conservation: A comparative study. Clin Breast
Cancer. 14:114–121. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fancellu A, Turner RM, Dixon JM, Pinna A,
Cottu P and Houssami N: Meta-analysis of the effect of preoperative
breast MRI on the surgical management of ductal carcinoma in
situ. Br J Surg. 102:883–893. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Agarwal S, Agarwal S, Neumayer L and
Agarwal JP: Therapeutic nipple-sparing mastectomy: Trends based on
a national cancer database. Am J Surg. 208:93–98. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
King TA, Sakr R, Patil S, Gurevich I,
Stempel M, Sampson M and Morrow M: Clinical management factors
contribute to the decision for contralateral prophylactic
mastectomy. J Clin Oncol. 29:2158–2164. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
King TA, Gurevich I, Sakr R, Patil S,
Stempel M and Morrow M: Occult malignancy in patients undergoing
contralateral prophylactic mastectomy. Ann Surg. 254:2–7. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Verhoog LC, Brekelmans CT, Seynaeve C, van
den Bosch LM, Dahmen G, van Geel AN, Tilanus-Linthorst MM, Bartels
CC, Wagner A, van den Ouweland A, et al: Survival and tumour
characteristics of breast cancer patients with germline mutations
of BRCA1. Lancet. 351:316–321. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rosenberg SM, Sepucha K, Ruddy KJ, Tamimi
RM, Gelber S, Meyer ME, Schapira L, Come SE, Borges VF, Golshan M,
et al: Local therapy decision-making and contralateral prophylactic
mastectomy in young women with early-stage breast cancer. Ann Surg
Oncol. 22:3809–3815. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chung A, Huynh K, Lawrence C, Sim MS and
Giuliano A: Comparison of patient characteristics and outcomes of
contralateral prophylactic mastectomy and unilateral total
mastectomy in breast cancer patients. Ann Surg Oncol. 19:2600–2606.
2012. View Article : Google Scholar : PubMed/NCBI
|