Introduction
Ophthalmic lymphomas account for 5–10% of extranodal
lymphomas, and extranodal marginal zone B-cell lymphomas of
mucosa-associated lymphoid tissue (MALT) are the leading subtype
among ophthalmic lymphomas (1,2). However,
only a few cases of sinonasal MALT lymphomas were reported in the
past 20 years (3,4). The present study reports a rare case of
a MALT lymphoma in the conjunctiva, lacrimal sac and nasal cavity,
which occurred 4 years following the spontaneous regression of
conjunctival atypical lymphoid hyperplasia. The pathological
features, imaging study and a gene arrangement test were used to
diagnose a single-clone MALT lymphoma in the conjunctiva and nasal
cavity. The role of the immunoglobulin heavy chain (IgH) gene
rearrangement and atypical infection in MALT lymphoma was also
discussed. A successful combination treatment, with local
radiotherapy and topical antibiotics plus steroid for a
disseminated MALT lymphoma, was also demonstrated in the present
study.
Case report
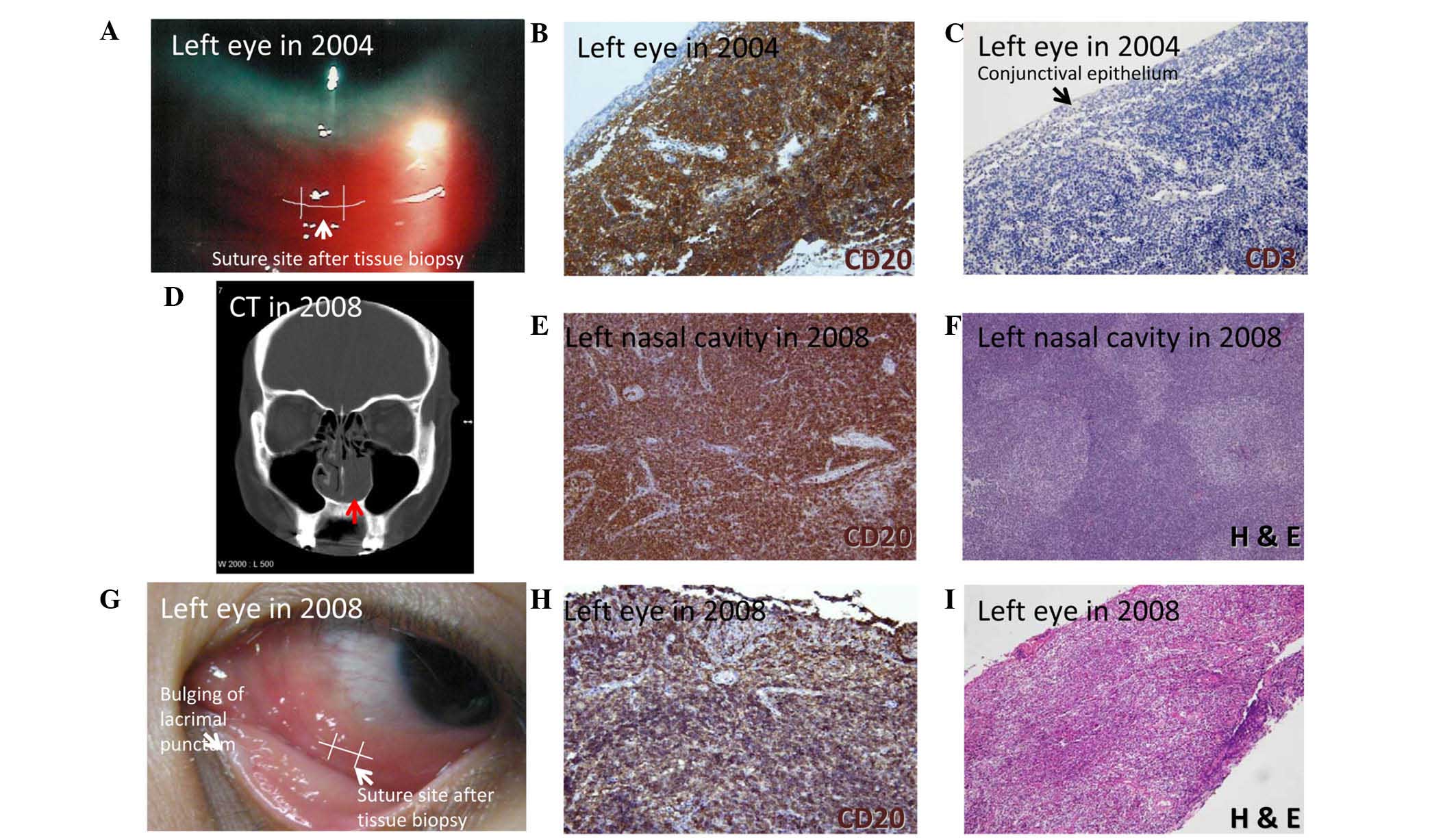
A 24-year-old female initially presented to the
Department of Ophthalmology, Wan Fang Medical Center, Taipei
Medical University (Taipei, Taiwan) in November 2004 with a painful
salmon pink-like lesion in the left inferior conjunctiva that had
lasted for several months (Fig. 1A).
A tissue biopsy was performed by an ophthalmologist and sent to the
Department of Pathology, Wan Fang Medical Center, Taipei Medical
University, where it was formalin-fixed and paraffin-embedded.
Immunohistochemical staining was performed using an automated
stainer (BenchMark XT, Ventana Medical Systems, Inc., Tucson, AZ,
USA) with 4-µm thick sections from formalin-fixed and
paraffin-embedded tissues. Tissue sections were deparaffinised and
rehydrated in graded alcohols and xylene. After retrieval by the
autoclave retrieval technique (10 mM citric acid buffer; 10–20 min)
and inhibition by endogenous peroxidase activity (0.3%
H2O2; 5 min), sections were incubated with
primary antibodies. The primary antibodies used were CD20
monoclonal mouse (dilution, 1:200; catalog no., CM004; Biocare
Medical, Concord, CA, USA) and CD3 monoclonal mouse (dilution,
1:200; catalog no., NCL-L-CD3-565; Leica Microsystems GmbH,
Wetzlar, Germany). Negative controls were performed by omitting
primary antibodies. After washing with Tris buffer, sections were
incubated for 30 min with a polyclonal secondary antibody against
mouse and rabbit from the ultraView Universal DAB Detection Kit
(dilution, 1:100; catalog no., 760-500; Ventana Medical Systems,
Inc.), re-incubated with 100 µg/ml peroxidase-conjugated
streptavidin, and colonized with 0.02% 3,3′-diaminobenzidine
tetrahydrochloride (0.05M Tris-HCL buffer with 0.03%
H2O2). The sections were counterstained with
hematoxylin, dehydrated and mounted. The surgical specimens
revealed atypical B-lymphoid hyperplasia (Fig. 1B and C). Spontaneous tumor regression
was observed in the following 6 months.
The patient visited the Department of
Otolaryngology, Wan Fang Medical Center, Taipei Medical University
in October 2008 complaining of left nasal pain that had lasted for
2 months. A lobulated left nasal tumor (18.8×24.6×37.4 mm in size)
with a bony destruction was noted on a sinus computed tomography
(CT) scan (Fig. 1D). Two incisional
biopsies performed by an otolaryngologist and sent to the
Department of Pathology, Wan Fang Medical Center, Taipei Medical
University confirmed a stage II mucosa-associated lymphoid tissue
(MALT) lymphoma with B-cell origin (Fig.
1E and F). Tissues were formalin-fixed and paraffin-embedded to
be used for immunohistochemistry and routine hematoxylin-eosin
staining. A histological diagnosis was performed according to the
WHO classification (5). In addition,
a relapse of the salmon pink-like lesion of the left inferior
conjunctiva was also found (Fig. 1G),
and MALT lymphoma was diagnosed by histopathological findings
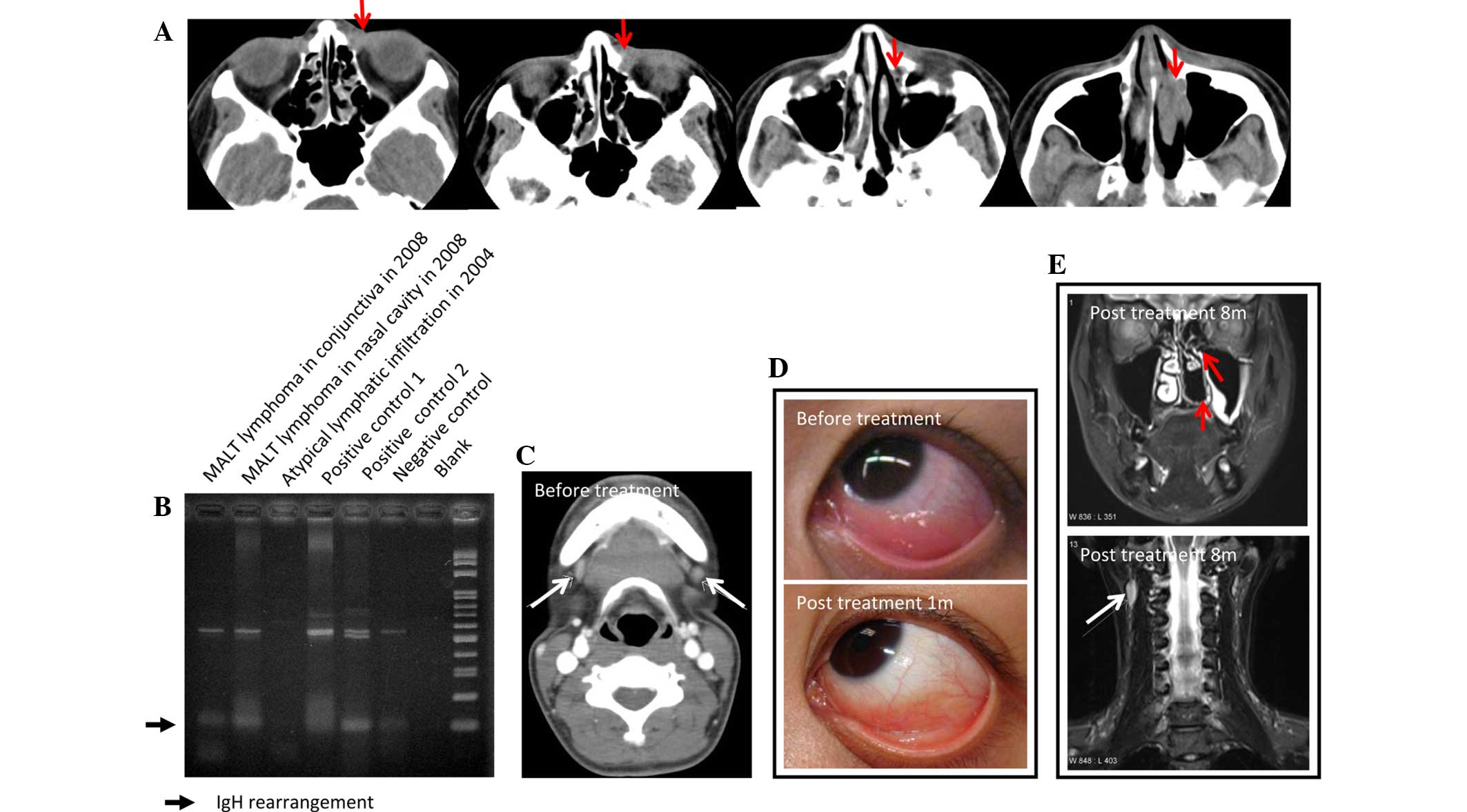
(Fig. 1H and I). Continuous imaging
sections on the sinus CT scan revealed a soft-tissue mass filled
lacrimal duct and sac (Fig. 2A; red
arrows). The homology of the MALT lymphoma in the nasal cavity and
conjunctiva was confirmed using polymerase chain reaction (PCR) and
evidenced by the sharing of the same IgH gene rearrangement.
IgH-rearrangement was not present in the conjunctival lesion in
2004 (Fig. 2B).
A series of systemic surveys revealed several
visible lymph nodes in the bilateral submanibular spaces and neck
region (Fig. 2C; white arrows). The
blood examination revealed elevated IgG for cytomegalovirus and
Epstein-Barr virus. In addition, specimens from the conjunctival
and nasal MALT lymphoma were negative for Helicobacter
pylori and Chlamydia by staining (data not shown). To
avoid radiation-related complications and for the conjunctival
mass, topical ciloxan (0.3% ciprofloxacin; 4 times a day; Alcon,
Fort Worth, TX, USA) and betamethasone eye ointment (for use before
sleep; Shionogi & Co., Ltd., Tokyo, Japan) were provided, and
the mass had regressed 1 month later (Fig. 2D). For the nasolacrimal mass and
enlarged lymph nodes, the patient received two phases of
radiotherapy with a total dosage of 46.8 Gray (Gy) (phase I, 180
cGyx10 covering the left lacrimal sac, nasal cavity and neck; phase
II, 180 cGyx16 over the bilateral neck region). Subsequent to
radiotherapy, the nasal cavity and lacrimal sac were noted to be
tumor free (Fig. 2E; upper; red
arrows), and one stationary neck lymph node (Fig. 2E; lower; white arrow) regressed the
following year. The patient was regularly followed up at the
outpatient Departments of Ophthalmology, Otolaryngology and
Oncology of Wan Fang Medical Center, Taipei Medical University. The
frequency of visits was every 3 months. No recurrence was found in
the subsequent 3 years.
The present study was approved by the Joint
Institutional Review Board of Taipei Medical University and written
informed consent was obtained from the patient for participation in
the study.
Discussion
To the best of our knowledge, the current study
presents the first case report of an IgH-rearranged conjunctival
MALT lymphoma with nasal cavity spread through the nasolacrimal
duct. It was reported in the literature that 92% of ophthalmic MALT
lymphoma patients have a primary ocular adnexal lymphoma, 60% of
which are primarily localized in the orbit and 33% of which in the
conjunctiva with a salmon-colored appearance (1,2).
Conjunctival MALT lymphoma derived from lymphoid hyperplasia is
rare due to the benign course of lymphoid hyperplasia (2,6). In the
present case, although the conjunctival MALT lymphoma (Fig. 1G-I) appeared following a spontaneous
regressed atypical lymphoid hyperplasia (Fig. 1A-C), PCR demonstrated a discordant
lymphoproliferative tumor of the left conjunctiva in November 2004
and October 2008 (Fig. 2B).
Genetic rearrangement (7,8) and
chronic infectious stimulation (8,9) result in
the activation of nuclear factor κ-light-chain-enhancer of
activated B-cells, and subsequently contributes to the malignant
transformation of MALT lymphomas (10). Chromosomal abnormalities involving IgH
gene translocation, including t(1;14)(p22;q32), t(14;18)(q32;q21),
and t(3;14)(p14;q32), are frequently associated with gastric or
pulmonary MALT lymphomas but seldom found in conjunctival MALT
lymphomas (1,8). In contrast with IgH rearrangement,
infectious agents associated with MALT lymphomas are more common
including H. pylori, Chlamydia and hepatitis C virus.
Infection with these pathogens and infectious antigen stimulation
of conjunctival tissue is not uncommon during life (9). Different from gastric MALT lymphomas,
the prevalence of H. pylori infection is relatively low in
the conjunctiva (11); however,
Chlamydia and hepatitis C virus infections are frequently
associated with conjunctival MALT lymphomas (9,12). In the
present study, the patient suffered a rare conjunctival MALT
lymphoma with IgH rearrangement (Fig.
2B), but tested negative for H. pylori and
Chlamydia infection. Notably, although H. pylori and
Chlamydia were undetectable in the conjunctival and nasal
MALT lymphomas, the conjunctival tumor lesion showed a good
response to topical antibiotics therapy (Fig. 2D), indicating that an atypical
infection played a role in the present case.
Ophthalmic MALT lymphoma is a malignancy with a
indolent course, and neither the clinical stage, ocular region
localization, nor therapeutic strategy affects the 5-year survival
or progression-free survival rate, with the exception of IgH
translocation involvement (1,2). For an IgH-translocated ophthalmic MALT
lymphoma, aggressive treatment is necessary due to the high-risk of
tumor progression (13). MALT
lymphomas are sensitive to external beam radiation, chemotherapy,
cryotherapy and oral doxycycline for Chlamydia infection
(1,9),
and the systemic anti-CD20 antibody, rituximab, is reserved for
refractory MALT lymphomas (14). In
the present case, to avoid radiation-related ocular complications,
a topical ciprofloxacin and steroid were chosen to treat the
conjunctival MALT lymphoma, and radiotherapy was given covering
bilateral neck, left nasal cavity, and left lacrimal sac.
Ciprofloxacin is a broad-spectrum antibiotic covering atypical
infections with a low resistance rate, chosen for the present
patient, who was negative for H. pylori and Chlamydia
infection. The current study demonstrated that a combination of
radiation therapy, topical ciprofloxacin and a topical steroid was
an effective therapeutic strategy for an IgH-rearranged
conjunctival MALT lymphoma with nasal cavity dissemination
(Fig. 2D and E).
In summary, a single-clone MALT lymphoma in the
conjunctiva with nasal cavity dissemination is rare, but possible.
In patients diagnosed with conjunctival MALT lymphoma, thorough
clinical examination should be performed to exclude the possibility
of conjunctival tumor spreading via the nasolacrimal duct.
Otolaryngologist may play a role in nasal examination. The
nasolacrimal duct may serve as a channel for conjunctival tumor
spreading. IgH-involved translocation is a disease progression
factor, and combination therapeutic approach, including topical
antibiotics for conjunctival tumor and radiotherapy for extra
conjunctival lesions, may successfully control high-risk,
disseminated MALT lymphomas.
Acknowledgements
The authors acknowledge Dr Chia-Che Wu (Ear, Nose,
Throat consultant), Dr Jo-Ting Tsai (Oncologist), Dr Gia-Yaun Chen
(Radiologist) and Dr Phui-Ly Liew (Pathologist) as clinical
consultants at Wan Fang Medical Center, Taipei Medical
University.
References
|
1
|
Sjö LD: Ophthalmic lymphoma: Epidemiology
and pathogenesis. Acta Ophthalmol 87 Thesis. 1:1–20. 2009.
View Article : Google Scholar
|
|
2
|
Ferry JA, Fung CY, Zukerberg L, Lucarelli
MJ, Hasserjian RP, Preffer FI and Harris NL: Lymphoma of the ocular
adnexa: A study of 353 cases. Am J Surg Pathol. 31:170–184. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cuadra-Garcia I, Proulx GM, Wu CL, Wang
CC, Pilch BZ, Harris NL and Ferry JA: Sinonasal lymphoma: A
clinicopathologic analysis of 58 cases from the massachusetts
general hospital. Am J Surg Pathol. 23:1356–1369. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yang QP, Zhang WY, Yu JB, Zhao S, Xu H,
Wang WY, Bi CF, Zuo Z, Wang XQ, Huang J, et al: Subtype
distribution of lymphomas in southwest China: Analysis of 6,382
cases using WHO classification in a single institution. Diagn
Pathol. 6:772011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Swerdlow SH, Campo E, Harris NL, Jaffe ES,
Pileri SA, Stein H, Thiele J and Vardiman JW: WHO Classification of
Tumours of Haematopoietic and Lymphoid Tissues (4th). IARC Press.
Lyon: 2008.
|
|
6
|
Demirci H, Shields CL, Karatza EC and
Shields JA: Orbital lymphoproliferative tumors: Analysis of
clinical features and systemic involvement in 160 cases.
Ophthalmology. 115:1626–1631. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kossakowska AE, Eyton-Jones S and Urbanski
SJ: Immunoglobulin and T-cell receptor gene rearrangements in
lesions of mucosa-associated lymphoid tissue. Diagn Mol Pathol.
2:233–240. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ferreri AJ, Dolcetti R, Du MQ, Doglioni C,
Resti AG, Politi LS, De Conciliis C, Radford J, Bertoni F, Zucca E,
et al: Ocular adnexal MALT lymphoma: An intriguing model for
antigen-driven lymphomagenesis and microbial-targeted therapy. Ann
Oncol. 19:835–846. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Verma V, Shen D, Sieving PC and Chan CC:
The role of infectious agents in the etiology of ocular adnexal
neoplasia. Surv Ophthalmol. 53:312–331. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Isaacson PG and Du MQ: MALT lymphoma: From
morphology to molecules. Nat Rev Cancer. 4:644–653. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ferreri AJ, Ponzoni M, Viale E, Guidoboni
M, Conciliis CD, Resti AG, Politi L, Lettini AA, Sacchetti F,
Dognini G, et al: Association between Helicobacter pylori infection
and MALTtype lymphoma of the ocular adnexa: Clinical and
therapeutic implications. Hematol Oncol. 24:33–37. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ferreri AJ, Guidoboni M, Ponzoni M, De
Conciliis C, Dell'Oro S, Fleischhauer K, Caggiari L, Lettini AA,
Dal Cin E, Ieri R, et al: Evidence for an association between
Chlamydia psittaci and ocular adnexal lymphomas. J Natl
Cancer Inst. 96:586–594. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Matsuo T and Yoshino T: Long-term
follow-up results of observation or radiation for conjunctival
malignant lymphoma. Ophthalmology. 111:1233–1237. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Salepci T, Seker M, Kurnaz E, Guler DO,
Bilici A, Dane F, Aliustaoglu M, Atesoglu EB, Gumus M and Yaylaci
M: Conjunctival malt lymphoma successfully treated with single
agent rituximab therapy. Leuk Res. 33:e10–e13. 2009. View Article : Google Scholar : PubMed/NCBI
|