Introduction
Breast cancer is the second largest cause of
mortality in women worldwide (1,2). Compared
with western countries, the incidence in China has increased
greatly since the 1990s (3,4). Breast cancer is a heterogeneous disease,
with five molecular subtypes, including luminal A, luminal B
HER2-negative, luminal B HER2-positive, HER2-positive and triple
negative. Furthermore, the incidence, treatment and prognosis vary
greatly among these five molecular subtypes (5).
A recent epidemiological study demonstrated that the
luminal B HER2-negative breast cancer had the highest incidence
among these five molecular subtypes, and >40% patients are
Chinese women (6). Although luminal B
HER2-negative breast cancer expresses hormone receptors, the
curative effect of hormone therapy and conventional chemotherapy is
unsatisfactory (7). Therefore, it is
important to identify new targets for the treatment of luminal B
HER2-negative breast cancer.
Cytotoxic T lymphocyte associated antigen 4
(CTLA-4), a CD28 homologue, consists of a short cytoplasmic tail, a
signal peptide, a transmembrane domain and a cellular extracellular
ligand-binding domain (8). CTLA-4 can
be a competitive inhibitor for CD28, where it binds to the ligands;
CD80 or CD86, resulting in inhibition of T cell activation and
raising the response threshold of T cells (9). In fact, CTLA-4 has a stronger binding
affinity with the two ligands compared with CD28, thus high
expression of CTLA-4 may lead to inhibition of anti-tumor immune
response (8). CTLA-4 may be expressed
on the surface of T cells (10).
However, there are some reports supporting the notion that CTLA-4
is also expressed on non-T cells, such as solid tumors (11–14). A
recent study demonstrated that patients overexpressing CTLA-4 in
esophageal cancer cells tend to have a poor prognosis (15).
Recent studies have also demonstrated that CTLA-4 is
overexpressed in breast cancer cells (10,11).
However, the association between CTLA-4 expression and prognosis in
breast cancer patients is not fully elucidated, particularly for
luminal B HER2-negative breast cancer. Therefore, the present study
aimed to answer such questions and provide a basis for new
therapeutic targets for the treatment of luminal B HER2-negative
breast cancer.
Materials and methods
Patients
A total of 102 cases of patients with stage I–III
luminal B HER2-negative breast cancer who underwent radical surgery
between January 2008 and December 2012 at Fuzhou General Hospital
of Nanjing Military Command (Fuzhou, China) were selected for the
present study. The study protocol was approved by the Medical
Ethics Committee of the Fuzhou General Hospital. The
clinicopathological characteristics of 102 patients were collected,
which included age, histological grade, lymph node, menopausal
status, tumor size and stage. The selection of clinicopathological
characteristics was determined by the recurrence risk factors,
which are recommended by the breast cancer prognosis guideline
(16). The inclusion criteria were as
follows: (i) Pathologically confirmed diagnosis of luminal B
HER2-negative breast cancer according to the St Gallen
International Expert Consensus 2013 (17); (ii) no chemotherapy or hormone therapy
prior to surgery; (iii) paraffin-embedded specimens of tumor
tissues were available, (iv) informed consent was obtained; (v)
follow-up was available. The median follow-up time was 43.5 months
(range, 1–96 months), which included 28 patients where metastasis
or local recurrence was present. The disease-free survival (DFS)
rate was 72.5%. The median DFS rate was not obtained.
Immunohistochemistry (IHC)
The surgical resection specimens of 102 patients
were fixed with formalin and embedded by paraffin. Continuous
paraffin section (thickness, 4 µm) were deparaffinized using 100%
xylene, 100% ethanol, 95% ethanol and 80% ethanol. The tissue
sections were used for antigen retrieval by high-pressure with 0.01
mol/l ethylenediaminetetraacetic acid, and endogenous peroxidase
activity was blocked by hydrogen peroxide at room temperature for
10 min. The tissue sections were washed in PBS three times, and
then primary antibodies anti-CTLA-4 IgG (dilution, 1:200; catalog
no. bs-1179R; Beijing Biosynthesis Biotechnology Co., Ltd.,
Beijing, China) and anti-Ki-67 antibody (dilution, 1:200; catalog
no. bs-23105R; Beijing Biosynthesis Biotechnology Co., Ltd.) were
added to the tissue sections for 60 min at room temperature.
Subsequently, the tissue sections were washed with PBS three times
and incubated with EliVision™ plus Polyer horseradish peroxidase
(Mouse/Rabbit) IHC kit (ready-to-use dilution; catalog no. KIT
9901; Fuzhou Maixin Biotechnology Co. Ltd., Fuzhou, China) at room
temperature for 30 min. Subsequently, the tissue sections were
stained with 3,3-diaminobenzidine (Fuzhou Maixin Biotechnology Co.
Ltd.) at room temperature for 3 min. The sections were
counterstained with hematoxylin at room temperature for 15 sec, and
the slides were counterstained with neutral resin for subsequent
observation with an optical microscope (magnification, ×100).
Evaluation of IHC staining
A total of two independent pathologists, who were
blinded to patient characteristics and clinical outcomes, evaluated
results of IHC staining. The expression of CTLA-4 was evaluated
with the percentage and intensity of positive tumor cells. The
scores of percentage of positive tumor cells were recorded as: 0
(0–25%), 1 (26–50%), 2 (51–75%) or 3 (76–100%). The scores of
intensity of positive tumor cells were recorded as: 0 (negative), 1
(weak), 2 (moderate) or 3 (strong). The scores for percentage and
intensity were multiplied together to attain a final histochemical
score (H-score). Then, the mean H-score was calculated from all
patient samples and determined as CTLA-4 positivity (tumor
CTLA-4+). The CTLA-4 positivity in interstitial
lymphocytes (interstitial CTLA-4+), which was in
interstitial areas adjacent to tumor nests, was evaluated as
aforementioned. Ki-67 was negative if there was less than 14% of
nuclei staining and positive if ≥14%, in accordance with previous
studies (17,18).
Statistical analysis
The data was analyzed using SPSS (version 16.0;
SPSS, Inc., Chicago, IL, USA). The association between CTLA-4
expression and various clinicopathologic parameters were analyzed
by the χ2 test. The survival probability was estimated
by the Kaplan-Meier test, and the statistical significance was
performed using the log-rank test. The multivariate analysis for
clinicopathological characteristics features was analyzed using the
Cox regression model. All tests were two sided. P<0.05 was
considered to indicate a statistically significant difference.
Results
CTLA-4 expression in luminal B
HER2-negative breast cancer tissues and interstitial tissues
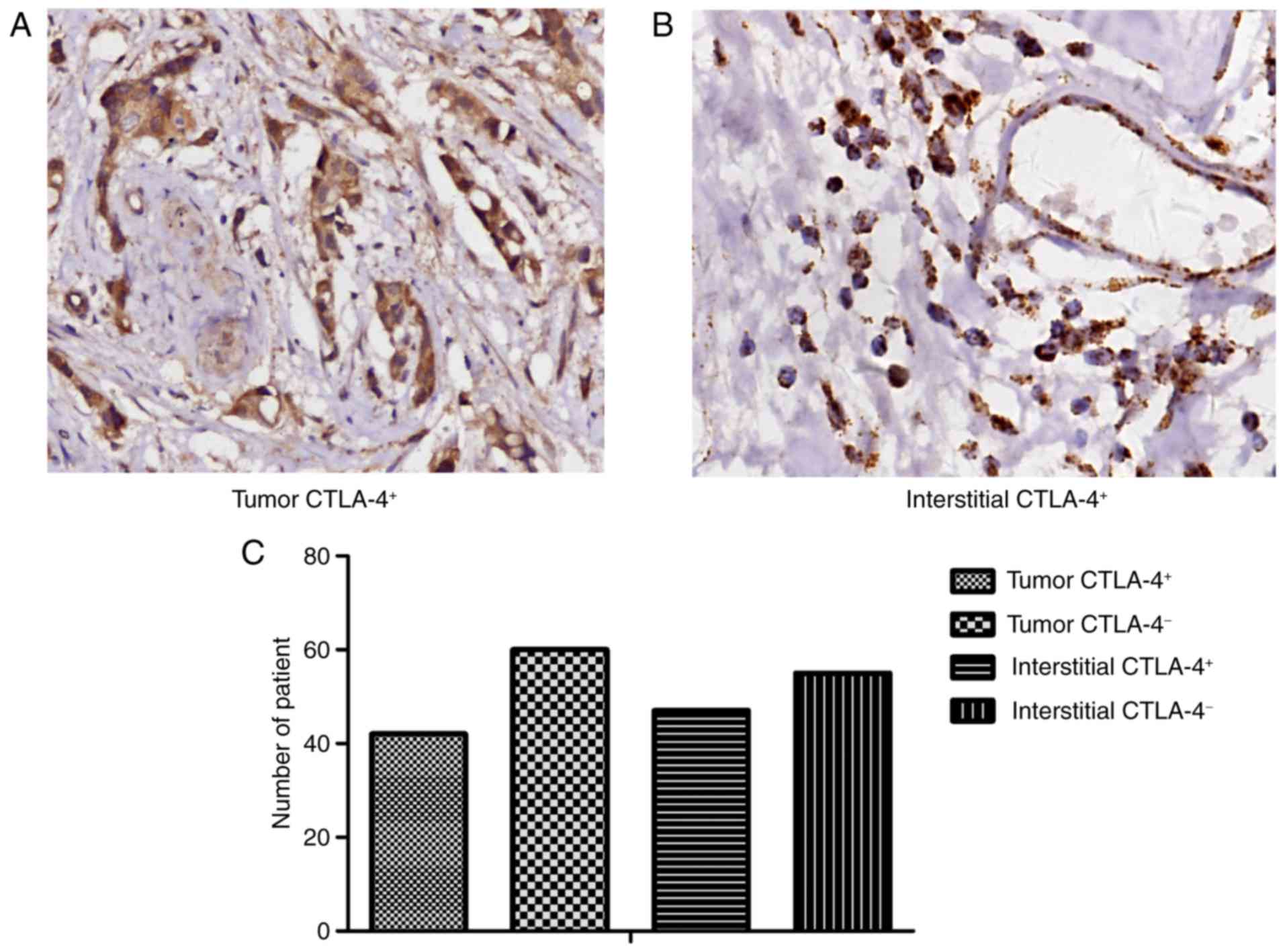
To investigate the function of CTLA-4 in progression
of luminal B HER2-negative breast cancer, IHC was conducted to
detect the expression of CTLA-4 in tumor and interstitial tissues.
CTLA-4 was expressed in the cell membrane and cytoplasm of T
lymphocytes and tumor cells (Fig. 1A and
B, respectively). The percentage of patients with tumor
CTLA-4+ was 41.2% (42/102), while the percentage of
patients with interstitial CTLA-4+ was 46.1% (47/102;
Fig. 1C). In addition, to investigate
whether there is an association between the expression of tumor and
interstitial CTLA-4, the χ2 test was used to demonstrate
that there was a strong positive association between tumor and
interstitial CTLA-4 expression (P<0.05).
Association between CTLA-4 expression
and clinicopathological characteristics
The χ2 test was performed to examine the
association between CTLA-4 expression and clinicopathological
characteristics in luminal B HER2-negative breast cancer tissues.
However, neither the expression of tumor CTLA-4 nor interstitial
CTLA-4 was associated with any clinical characteristics of the
patients in the present cohort, including age, histological grade,
lymph node, menopausal status, tumor size and stage and Ki-67
expression (all P>0.05; Table
I).
 | Table I.Association between CTLA-4 expression
and clinicopathological characteristics. |
Table I.
Association between CTLA-4 expression
and clinicopathological characteristics.
|
|
| Tumor CTLA-4 |
| Interstitial
CTLA-4 |
|
|---|
|
|
|
|
|
|
|
|---|
| Clinicopathological
characteristics | n | (+) | (−) | P-value | (+) | (−) | P-value |
|---|
| Age (years) |
|
|
| 0.099 |
|
| 0.845 |
|
<35 | 8 | 6 | 2 |
| 5 | 3 |
|
| ≥35 | 94 | 36 | 58 |
| 49 | 45 |
|
| Menopausal
status |
|
|
| 0.868 |
|
| 0.560 |
|
Premenopausal | 52 | 21 | 31 |
| 29 | 23 |
|
|
Postmenopausal | 50 | 21 | 29 |
| 25 | 25 |
|
| Histological
grade |
|
|
| 0.422 |
|
| 0.148 |
| I | 16 | 6 | 10 |
| 11 | 5 |
|
| II | 58 | 27 | 31 |
| 32 | 26 |
|
| III | 28 | 9 | 19 |
| 11 | 17 |
|
| Tumor size (cm) |
|
|
| 0.636 |
|
| 0.243 |
| ≤2 | 49 | 19 | 30 |
| 23 | 26 |
|
|
>2 | 53 | 23 | 30 |
| 31 | 22 |
|
| Lymph node |
|
|
| 0.332 |
|
| 0.161 |
|
Negative | 52 | 19 | 33 |
| 24 | 28 |
|
|
Positive | 50 | 23 | 27 |
| 30 | 20 |
|
| Tumor stage |
|
|
| 0.298 |
|
| 0.114 |
| I | 29 | 10 | 19 |
| 11 | 18 |
|
| II | 47 | 18 | 29 |
| 26 | 21 |
|
|
III | 26 | 14 | 12 |
| 17 | 9 |
|
| Ki-67 |
|
|
| 0.884 |
|
| 0.376 |
|
<14 | 9 | 3 | 6 |
| 3 | 6 |
|
|
≥14 | 93 | 39 | 54 |
| 51 | 42 |
|
Association between tumor/interstitial
CTLA-4 expression and clinical outcomes of patients with luminal B
HER2-negative breast cancer tissues
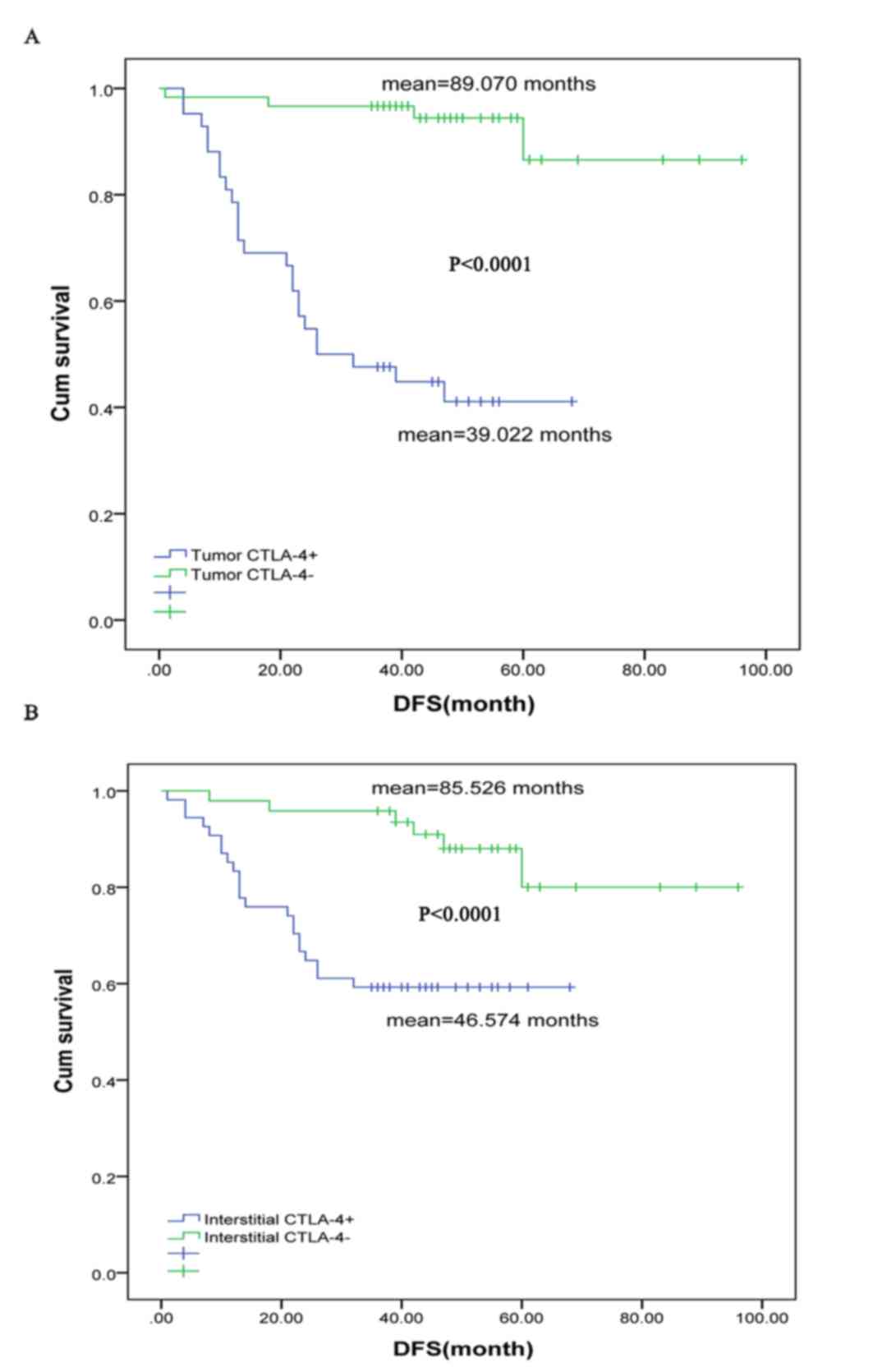
The Kaplan-Meier method was performed to examine the
association between the expression of tumor/interstitial CTLA-4 and
the survival of patients with luminal B HER2-negative breast
cancer. In the present study, the DFS rate of patients with tumor
CTLA-4+ was significantly shorter compared with patients
with tumor CTLA-4− (mean, 89.070 vs. 39.022 months;
P<0.0001; Fig. 2A). Additionally,
the DFS rate of the patients with interstitial CTLA-4+
was considerably shorter compared with patients with interstitial
CTLA-4− (mean, 85.526 vs. 46.574 months; P<0.0001;
Fig. 2B). Furthermore, the
multivariate cox regression analysis demonstrated that tumor
CTLA-4+ was an independent predictor of shorter DFS when
factors, including age, menopausal status, histological grade,
tumor size, the number of lymph nodes, clinical stage, Ki-67 and
interstitial CTLA-4, are controlled (P<0.001; Table II).
 | Table II.Multivariate analysis of patient
survival. |
Table II.
Multivariate analysis of patient
survival.
| Clinicopathological
characteristics | HR | 95% CI | P-value |
|---|
| Tumor CTLA-4 | 0.058 | 0.015–0.224 | <0.001 |
| Ki-67 | 4.406 | 0.528–36.756 | 0.171 |
| Tumor stage | 2.769 | 1.181–6.488 | 0.019 |
| Lymph node | 0.425 | 0.128–1.413 | 0.163 |
| Tumor size | 0.842 | 0.349–2.034 | 0.702 |
| Years | 2.337 | 0.471–11.591 | 0.299 |
| Menopausal
status | 1.420 | 0.610–3.308 | 0.416 |
| Histological
grade | 1.086 | 0.559–2.111 | 0.807 |
| Interstitial
CTLA-4 | 1.413 | 0.430–4.637 | 0.569 |
Discussion
Tumor-derived immune deregulation is a common
characteristic in the majority of solid tumors, particularly for
breast cancer (10). The
immunosuppressive microenvironment primarily includes cytokines and
immune checkpoint molecules, which leads to the blocking of
anti-tumor immunity (19–21). One of these immune checkpoint
molecules is the cytotoxic T lymphocyte antigen 4 (CTLA-4; CD152),
a CD28 homologue which has two common ligands with CD28: B7-1
(CD80) and B7-2 (CD86). Notably, CTLA-4 has a stronger binding
affinity with these two ligands compared with CD28 (8). The investigation of CTLA-4 is crucial
for understanding tumor-derived immune deregulation and may give
rise to novel immune therapy for breast cancer.
Previous studies have indicated that CTLA-4 was
overexpressed in breast cancer cells. However, these studies did
not investigate the function of CTLA-4 in different types of breast
cancer, particularly luminal B HER2-negative breast cancer, which
has a high incidence in Chinese women (11). In the present study, the expression of
CTLA-4 was detected by IHC, and 41.2% (42/102) and 46.1% (47/102)
were patients with tumor and interstitial CTLA-4+,
respectively. Furthermore, the association between tumor CTLA-4 and
interstitial CTLA-4 was assessed. It was demonstrated that there
was a positive association of tumor CTLA-4 and interstitial CTLA-4.
Subsequently, a χ2 test was performed to analyze the
association between the expression of CTLA-4 and
clinicopathological characteristics of the selected patients.
However, the results demonstrated that the expression of neither
tumor nor interstitial CTLA-4 was associated with any of the
clinical characteristics assessed, including age, menopausal
status, histological grade, tumor size, lymph node, tumor stage and
Ki-67 expression level.
Previous studies reported that patients exhibiting
positive tumor CTLA-4 expression had a better prognosis in NSCLC
and gastric cancer (12,13). However, previous studies also
demonstrated that CTLA-4 was a poor prognosis factor in esophageal
carcinoma and breast cancer (10,19).
Therefore, we hypothesized that CTLA-4 expression may be associated
with the prognosis of patients with luminal B HER2-negative breast
cancer. Furthermore, tumor CTLA-4+ was an independent
risk factor for the prognosis of patients with breast cancer.
The results of a clinical trial for a CTLA-4
blocker, tremelimumab, for the treatment of breast cancer
demonstrated that in the majority of patients, peripheral blood
immune function was improved (22).
Therefore, CTLA-4 may be a novel target for the treatment of
luminal B HER2-negative breast cancer. However, the study by
Vonderheide et al (22)
demonstrated that there was no association between peripheral blood
immune function and clinical outcomes (22). Tumor microenvironment may serve a
greater role than immune status of the peripheral blood in
anti-tumor immunotherapy. Tumor microenvironment may be taken into
account when CTLA-4 becomes an immunotherapy target for breast
cancer.
The present study has some limitations. More
patients are required in future studies in order to confirm that
CTLA-4 can be a biomarker for assessing the clinical outcomes of
anti-CTLA-4 treatment in luminal B HER2-negative breast cancer.
Furthermore, the association between tumor and interstitial CTLA-4,
and the mechanism by which CTLA-4 enters the tumor cells were not
investigated
In conclusion, the present study demonstrated a
positive association between the expression of tumor and
interstitial CTLA-4, which was associated with poor prognosis in
luminal B HER2-negative breast cancer. The present study may
provide novel therapeutic targets for patients with luminal B
HER2-negative breast cancer. However, further studies are required
to confirm these findings.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
DeSantis C, Ma J, Bryan L and Jemal A:
Breast cancer statistics, 2013. CA Cancer J Clin. 64:52–62. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Siegel R, Miller K and Jemal A: Cancer
statistics, 2015. CA Cancer J Clin. 65:5–29. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chen W, Zheng R, Baade PD, Zhang S, Zeng
H, Bray F, Jemal A, Yu XQ and He J: Cancer statistics in China,
2015. CA Cancer J Clin. 66:115–132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhang ML, Huang ZZ and Zheng Y: Estimates
and prediction on indidence, mortality and prevalence of breast
cancer in China, 2008. Zhonghua Liu Xing Bing Xue Za Zhi.
33:1049–1051. 2012.(In Chinese). PubMed/NCBI
|
|
5
|
Cancer Genome Atlas Network, .
Comprehensive molecular portraits of human breast tumors. Nature.
490:61–70. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Si W, Li Y, Han Y, Zhang F, Wang Y, Li Y,
Linghu RX, Zhang X and Yang J: Epidemiological and
clinicopathological trends of breast cancer in chinese patients
during 1993 to 2013: A retrospective study. Medicine (Baltimore).
94:e8202015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tran B and Bedard PL: Luminal-B breast
cancer and novel therapeutic targets. Breast Cancer Res.
13:2212011. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Grosso JF and Jure-Kunkel MN: CTLA-4
blockade in tumor models: An overview of preclinical and
translational research. Cancer Immun. 13:52013.PubMed/NCBI
|
|
9
|
Schwartz JC, Zhang X, Fedorov AA,
Nathenson SG and Almo SC: Structural basis for co-stimulation by
the human CTLA-4/B7-2 complex. Nature. 410:604–608. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yu H, Yang J, Jiao S, Li Y, Zhang W and
Wang J: Cytotoxic T lymphocyte antigen 4 expression in human breast
cancer: Implications for prognosis. Cancer Immunol Immunother.
64:853–860. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mao H, Zhang L, Yang Y, Zuo W, Bi Y, Gao
W, Deng B, Sun J, Shao Q and Qu X: New Insights of CTLA-4 into its
biological function in breast cancer. Curr Cancer Drug Targets.
10:728–736. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Salvi S, Fontana V, Boccardo S, Merlo DF,
Margallo E, Laurent S, Morabito A, Rijavec E, Dal Bello MG, Mora M,
et al: Evaluation of CTLA-4 expression and relevance as a novel
prognostic factor in patients with non-small cell lung cancer.
Cancer Immunol Immunother. 61:1463–1472. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim JW, Nam KH, Ahn SH, Park DJ, Kim HH,
Kim SH, Chang H, Lee JO, Kim YJ, Lee HS, et al: Prognostic
implications of immunosuppressive protein expression in tumors as
well as immune cell infiltration within the tumor microenvironment
in gastric cancer. Gastric Cancer. 19:42–52. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Laurent S, Carrega P, Saverino D, Piccioli
P, Camoriano M, Morabito A, Dozin B, Fontana V, Simone R, Mortara
L, et al: CTLA-4 is expressed by human monocyte-derived dendritic
cells and regulates their functions. Hum Immunol. 71:934–941. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhang XF, Pan K, Weng DS, Chen CL, Wang
QJ, Zhao JJ, Pan QZ, Liu Q, Jiang SS, Li YQ, et al: Cytotoxic T
lymphocyte antigen-4 expression in esophageal carcinoma:
Implications for prognosis. Oncotarget. 7:26670–26679.
2016.PubMed/NCBI
|
|
16
|
Ehinger A, Malmström P, Bendahl PO, Elston
CW, Falck AK, Forsare C, Grabau D, Rydén L, Stål O and Fernö M;
South and South-East Swedish Breast Cancer Groups, : Histological
grade provides significant prognostic information in addition to
breast cancer subtypes defined according to St Gallen 2013. Acta
Oncol. 56:68–74. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Goldhirsch A, Winer EP, Coates AS, Gelber
RD, Piccart-Gebhart M, Thürlimann B and Senn HJ; Panel members, :
Personalizing the treatment of women with early breast cancer:
Highlights of the St Gallen international expert consensus on the
primary therapy of early breast cancer 2013. Ann Oncol.
24:2206–2223. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Prihantono P, Hatta M, Binekada C,
Sampepajung D, Haryasena H, Nelwan B, Asadul Islam A and Nilawati
Usman A: Ki-67 expression by immunohistochemistry and quantitative
real-time polymerase chain reaction as predictor of clinical
response to neoadjuvant chemotherapy in locally advanced breast
cancer. J Oncol. 2017:62098492017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Emens LA: Breast cancer immunobiology
driving immunotherapy: Vaccines and immune checkpoint blockade.
Expert Rev Anticancer Ther. 12:1597–1611. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Koch MA, Thomas KN, Perdue NR, Smigiel KS,
Srivastava S and Campbell DJ: T-bet(+) Treg cells undergo abortive
Th1 cell differentiation due to impaired expression of IL-12
receptor β2. Immunity. 37:501–510. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yu HM, Yang JL, Jiao SC, Wang JD and Li Y:
TGF-β1 precursor and CD8 are potential prognostic and predictive
markers in operated breast cancer. J Huazhong Univ Sci Technolog
Med Sci. 34:51–58. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Vonderheide RH, LoRusso PM, Khalil M,
Gartner EM, Khaira D, Soulieres D, Dorazio P, Trosko JA, Rüter J,
Mariani GL, et al: Tremelimumab in combination with exemestane in
patients with advanced breast cancer and treatment-associated
modulation of inducible costimulator expression on patient T cells.
Clin Cancer Res. 16:3485–3494. 2010. View Article : Google Scholar : PubMed/NCBI
|