Introduction
Uterine leiomyoma is the most common type of
gynecological tumor, and is estimated to be present in 20–30% of
women aged 30 and 40% of women aged >40. Uterine leiomyoma is
more frequent in multiparous compared with in nulliparous women.
Since laparoscopic surgery was introduced in 1979, it has
increasingly replaced abdominal and vaginal approaches to operative
treatments of uterine leiomyoma (1).
However, in April 2014, the US Food and Drug Administration (FDA)
issued a statement warning against the use of laparoscopic power
morcellators for the majority of females undergoing a hysterectomy
or myomectomy for uterine smooth muscle tumors due to the risk of
spreading the cancerous tissue intraperitoneally if the tumors were
malignant (2). Since this warning was
issued, North American gynecologists have been reluctant to perform
laparoscopic surgery on these types of tumor (3). Methods for the preoperative diagnosis of
uterine myometrial lesions is a topic of discussion for Japanese
gynecologists (4). Magnetic resonance
imaging (MRI) scans are the most useful type of method for
establishing a preoperative diagnosis of smooth muscle tumors.
However, MRIs may be inaccurate when used as the sole diagnostic
method. Since 1994, transcervical needle biopsies have been
performed to differentiate between uterine leiomyomas and
leiomyosarcomas (5).
In the present study, 331 patients with uterine
smooth muscle tumors who underwent transcervical needle biopsies
and possessed known subsequent outcomes were retrospectively
reviewed. The aim of the present study was to assess the safety of
laparoscopic excision of these types of tumors subsequent to
transcervical needle biopsy and to evaluate the association between
cytological atypia, mitotic activity and the presence of
coagulative tumor cell necrosis in biopsy specimens and final
diagnoses.
Materials and methods
Patients
Between June 1994 and May 2015, transcervical needle
biopsies were performed in 626 patients in Osaka City University
(Osaka, Japan) with written informed consent provided, subsequent
to the necessity, risks and limitations of the diagnostic accuracy
of this procedure having been explained. Outcomes were assessed in
the 331 of the 626 patients who exhibited smooth muscle tumors and
high intensity regions on T1 weighted images (T1WI) and/or T2 WI
MRI scans. Of the 331 patients, the final diagnoses were:
Leiomyosarcoma in 10 patients; smooth muscle tumor of uncertain
malignant potential in 7 patients; and leiomyoma in 314 patients.
All cases of leiomyosarcoma met the Stanford criteria of Bell et
al (6). Smooth muscle tumors of
uncertain malignant potential were defined as those that could not
be classified reliably as benign or malignant on the basis of
generally applied criteria (7). Due
to the fact that none of the tumors initially diagnosed as smooth
muscle tumors of uncertain malignant potential in the present study
met the Stanford criteria for leiomyosarcoma, but they did exhibit
moderate to severe atypia, they were classified as atypical
leiomyomas. In the present study, 76 of the 314 leiomyomas were
diagnosed using specimens obtained from surgery performed
subsequent to needle biopsy, whereas the remaining 238 leiomyomas
were diagnosed using biopsy specimens and these latter patients did
not undergo surgery. As the present study was a retrospective study
of records from patients, the Ethics Committee of Osaka City
University (Osaka, Japan) waived the requirement for informed
consent.
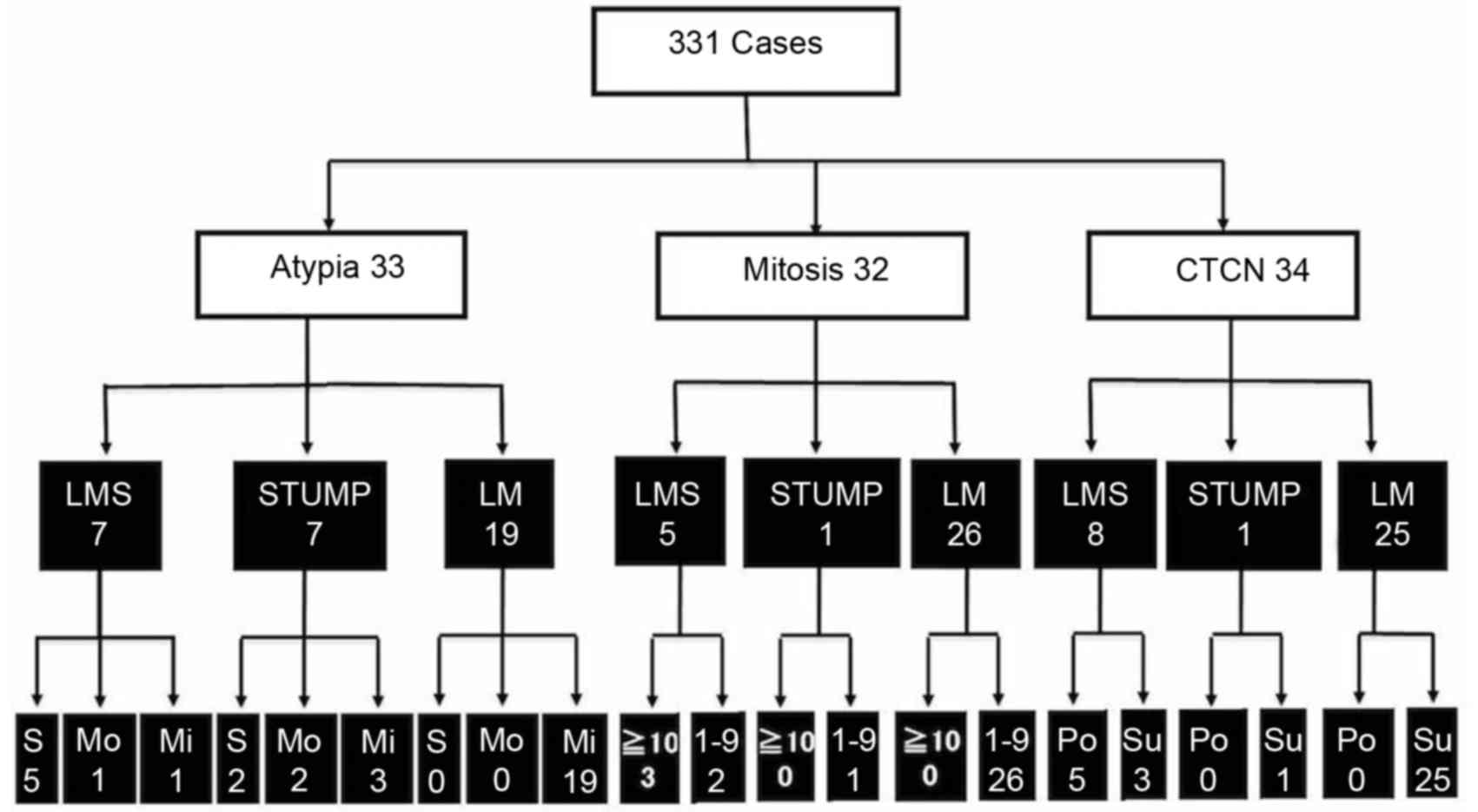
The retrospective assessment of hematoxylin and
eosin (HE)-stained transcervical needle biopsy specimens from 331
patients determined whether the Stanford criteria of Bell et
al (6): The presence of
cytological atypia, the number of mitotic figures and the presence
of coagulative tumor cell necrosis, which may be used to construct
an algorithm to perform laparoscopic surgery with histopathological
safety. Patients with any combination of cytological atypia,
mitotic figures and coagulative tumor cell necrosis were identified
and classified according to their final diagnoses, as presented in
Fig. 1. Patients exhibiting
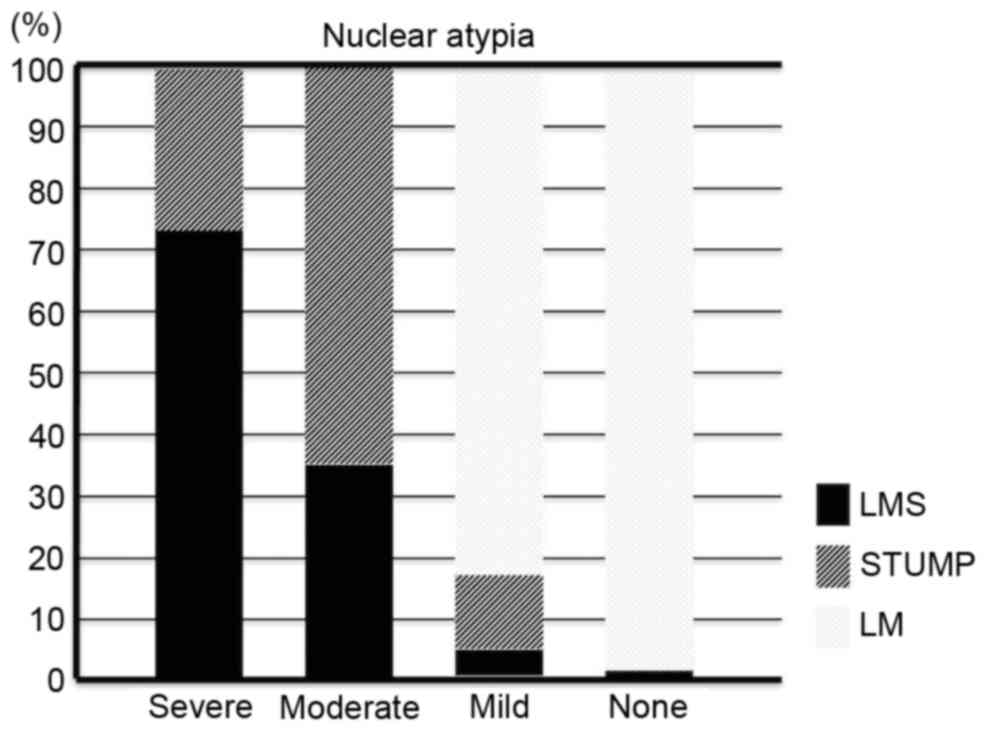
cytological atypia were allocated into 4 groups based on the degree
of atypia and the ratio of these groups was plotted, as presented
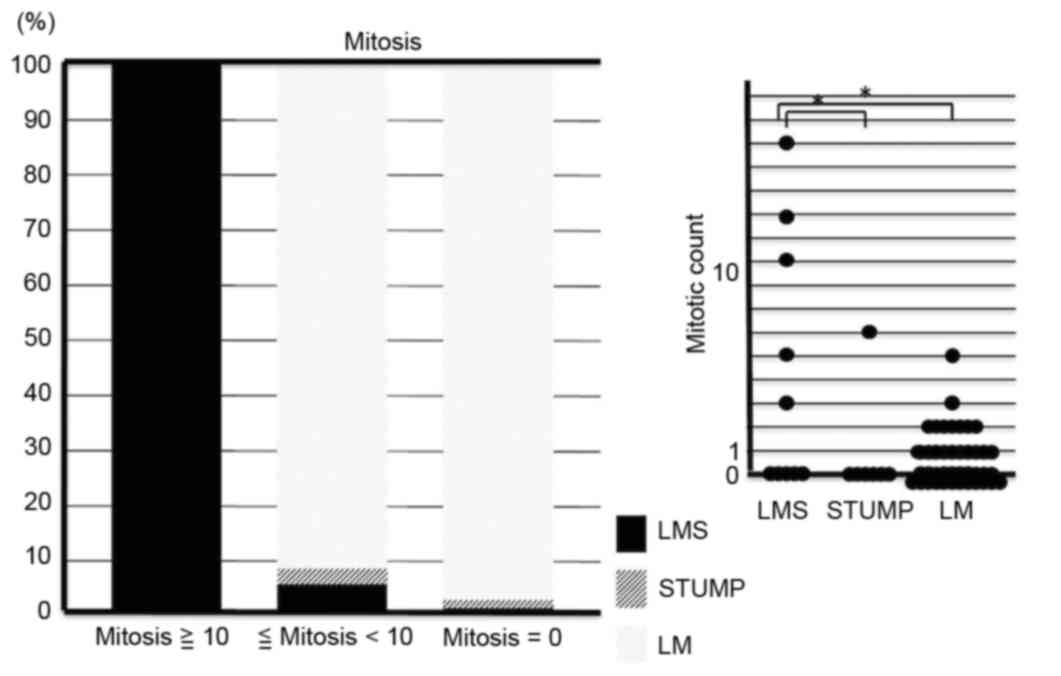
in Fig. 2. The procedure was repeated
and used to construct plots based on the number of mitotic figures
and the presence of coagulative tumor cell necrosis, as presented
in Figs. 3 and 4. A Mann-Whitney U test was performed to
ascertain the significance of the mitotic counts, as presented in
Fig. 3. P<0.05 was considered to
indicate a statistically significant difference.
Needle biopsy
The transcervical needle biopsies of smooth muscle
tumors were performed using an automatic 25-cm long, 16-gauge,
17-mm notch cutting needle and a 20-cm long straight stainless
steel guide pipe with a 4 mm maximum external dimension and a 3 mm
maximum internal dimension (Honest Medical Co., Ltd., Tokyo,
Japan), under transabdominal guidance using a Pro-Mag Ultra Biopsy
(Argon Medical Devices, Plano, TX, USA) or a Pro-Mag 2.2 biopsy
system (Argon Medical Devices). Analgesics (25 or 50 mg diclofenac
sodium suppositories in almost all cases) were administered prior
to biopsy as required. The patients were then placed in the
lithotomy position and a guide pipe was inserted transcervically
into the uterine cavity. The operator manipulated the uterine
corpus and guided the pipe using transabdominal ultrasonic
guidance, to align the pipe with the lesion to be biopsied. The
biopsy needle was then inserted through the guide pipe into the
uterine tumor. Subsequent to confirming that the tip of the needle
was within the lesion, the biopsy gun (Argon Medical Devices) was
used to obtain a tissue sample (5).
To minimize sampling error, 3 biopsy specimens/patient were
obtained.
Histopathological analysis
A total of 3 biopsy specimens from each patient were
evaluated using hematoxylin & eosin staining. Specimens were
fixed in 10% formalin at 20°C for 24 h, paraffin-embedded and cut
into 4 µm sections. Samples were deparaffinized using 99% xylene
and alcohol dehydration of graded series from 100 to 70% ethanol.
Finally, samples were stained with 0.15% hematoxylin solution
diluted 4 times for 4.5 min at 20°C, followed by 0.33% Eosin for 4
min at 20°C. The degree of cytological atypia was recorded as
follows: Severe atypia, detectable at low magnification
(magnification, ×4, light microscope); moderate atypia
(magnification, ×10-20); mild atypia (magnification, ×40) and no
atypia. The mitotic figures were counted under a light microscope
in all high-power fields for the 3 specimens using ×40 objective
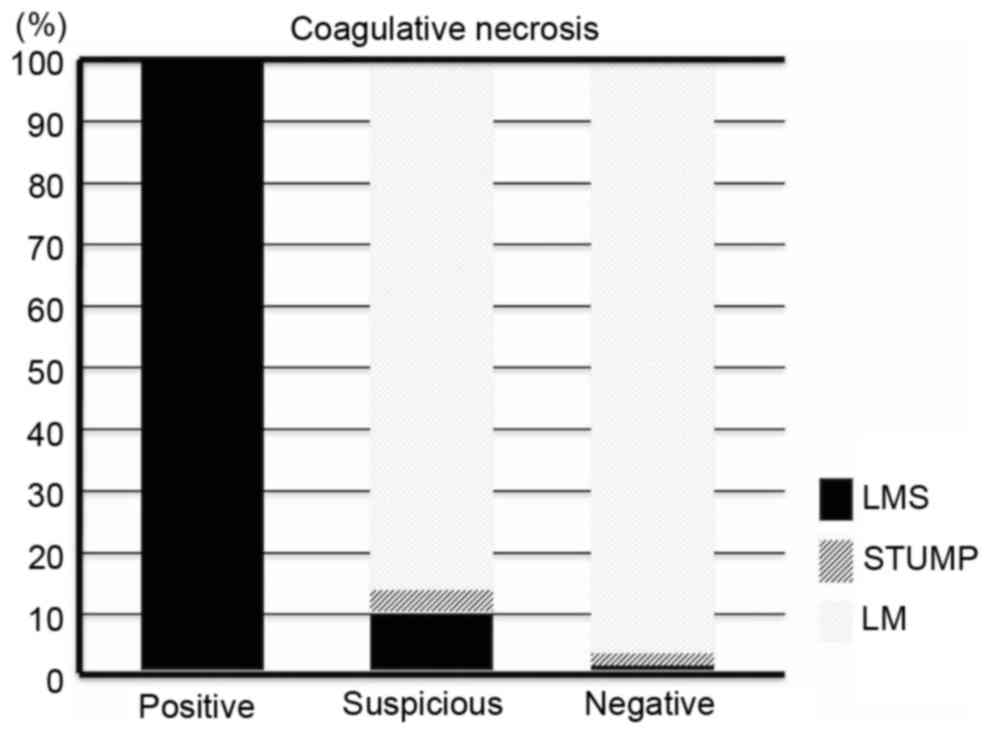
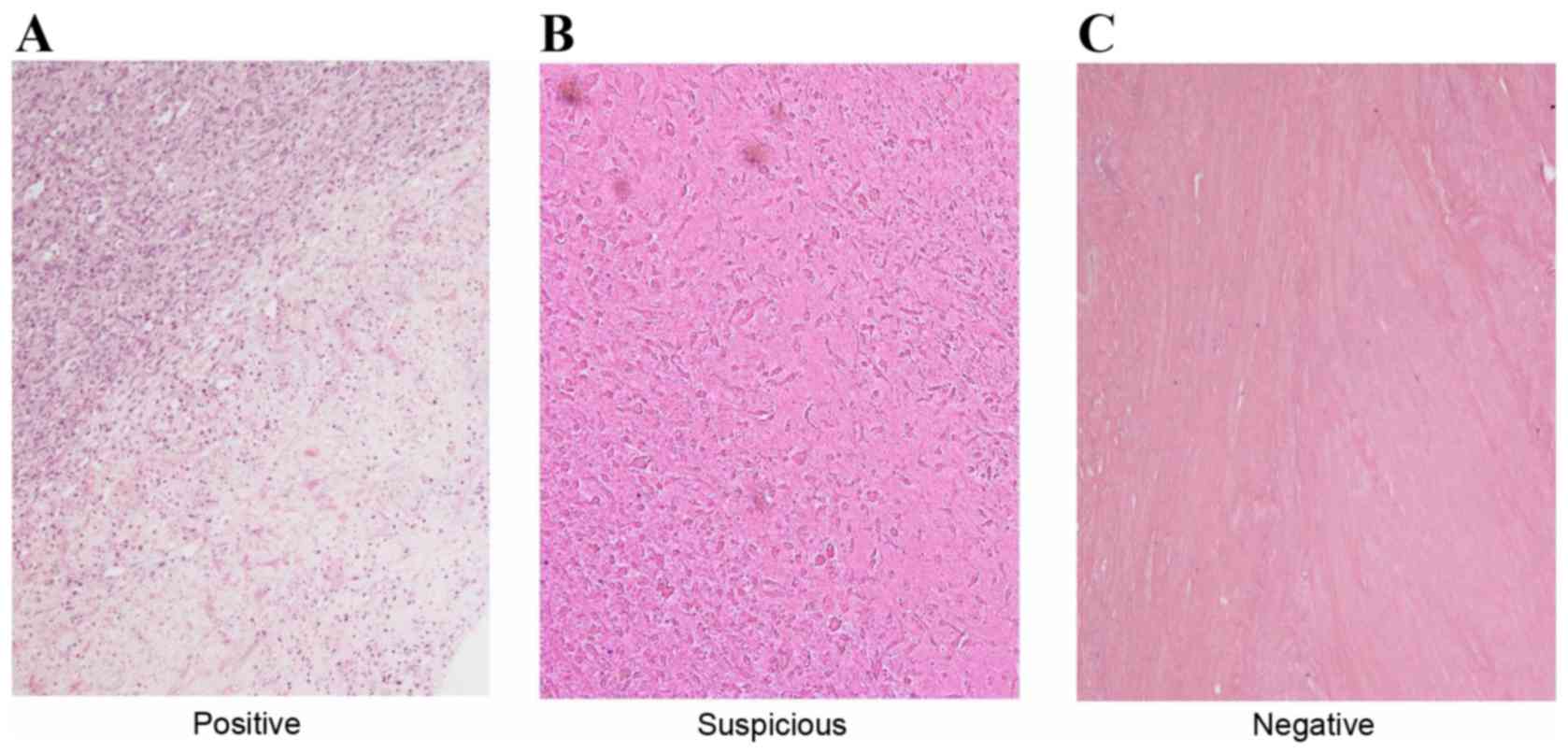
lens. Levels of coagulative tumor cell necrosis were recorded as
follows: Positive, which was confirmed by presence of ghost cells
and abrupt transition, as presented in Fig. 5; suspected, which was defined as the
presence of ghost cells with unclear abrupt transition; and
negative, which was confirmed by evidence of hyalinization only
(5). The patients with particular
variants of leiomyoma, such as epithelioid leiomyoma or
lipoleiomyoma, were excluded from additional analyses.
Results
A total of 33 patients exhibited cytological atypia
in their biopsy specimens; 7 with a diagnosis of leiomyosarcoma, 7
with a smooth muscle tumor of uncertain malignant potential and 19
with a diagnosis of leiomyoma. Thus, the final diagnosis was
leiomyoma in ~58% (19/33) of the patients with cytological atypia,
as presented in Fig. 1. Of the 10
patients with moderate or severe cytological atypia, 4 exhibited
smooth muscle tumors of uncertain malignant potential and 6
exhibited leiomyosarcomas. No cytological atypia was found in 298
patients, 99% of whom exhibited leiomyomas. However, the final
diagnosis of 3 patients with no cytological atypia in their biopsy
specimens, was leiomyosarcoma, as presented in Fig. 2.
A total of 32 patients exhibited between 1 and 9
mitotic figures in all high-power fields: 5 patients with
leiomyosarcoma, 1 patient with a smooth muscle tumor of uncertain
malignant potential, and 26 with leiomyoma. In 3 of the patients
with ≥10 mitotic figures in all high-power fields, the final
diagnosis was leiomyosarcoma, as presented in Fig. 1. A total of 26 patients with leiomyoma
that exhibited mitotic figures on biopsy specimens possessed <10
mitotic figures in all high-power fields. The median number of
mitotic figures differed significantly between incidences of
leiomyosarcoma and smooth muscle tumors of uncertain malignant
potential, and between leiomyosarcoma and leiomyoma, as presented
in Fig. 3.
A total of 34 patients exhibited a confirmed
positive result or suspected coagulative tumor cell necrosis, 8
with leiomyosarcoma, 1 with a smooth muscle tumor of uncertain
malignant potential, and 25 with leiomyoma, as presented in
Fig. 1. A total of 5 patients with
coagulative tumor cell necrosis had final diagnoses of
leiomyosarcoma. Coagulative tumor cell necrosis was not exhibited
in 297 patients, 97% of whom exhibited leiomyomas. Of the patients
with suspected coagulative tumor cell necrosis, 86% exhibited
leiomyomas and 10% exhibited leiomyosarcomas, as presented in
Fig. 4.
In the present study, no patients without
cytological atypia, mitotic figures or coagulative tumor cell
necrosis were diagnosed with either leiomyosarcomas or smooth
muscle tumors of uncertain malignant potential. The 238 patients
with leiomyomas who did not undergo surgery were followed up for
>2 years, during which time they exhibited no symptoms of
leiomyosarcoma, such as a rapid increase in the size of lesions or
an increase in lesion size subsequent to menopause.
Discussion
A previous study estimated that 1/350 women who
undergo a hysterectomy develop malignant uterine tumors (2). Since then, North American gynecologists
have been reluctant to perform laparoscopic surgery for uterine
smooth muscle tumors (3), and methods
for the preoperative diagnosis of uterine myometrial lesions is a
topic of debate amongst Japanese gynecologists (4).
MRI scans are the most useful technique of
preoperatively diagnosing smooth muscle tumors. Leiomyosarcomas
typically exhibit a high intensity with T2WI, which reflects the
growth of cells, and high intensity with T1 and T2WI, which
reflects hemorrhage. However, as some uterine leiomyomas exhibit
high intensity on T1 and/or T2WI images and some leiomyosarcomas do
not exhibit clear high intensity region on T1WI images, smooth
muscle tumors cannot be reliably diagnosed using MRI scans alone
(5). Since 1994, transcervical needle
biopsies have been performed in addition to MRIs, to accurately
exclude the diagnosis of malignant diseases such as leiomyosarcoma.
To determine whether transcervical needle biopsies are useful for
performing laparoscopic surgeries for uterine smooth muscle tumors
with histopathological safety, the present study retrospectively
assessed 331 patients with smooth muscle tumors who had undergone
the aforementioned procedure.
Of the 331 patients in the present study, all 250
that did not exhibit the 3 Stanford criteria: Cytological atypia,
mitotic figures and coagulative tumor cell necrosis, and exhibited
high intensity regions on MRI scans were diagnosed with leiomyoma.
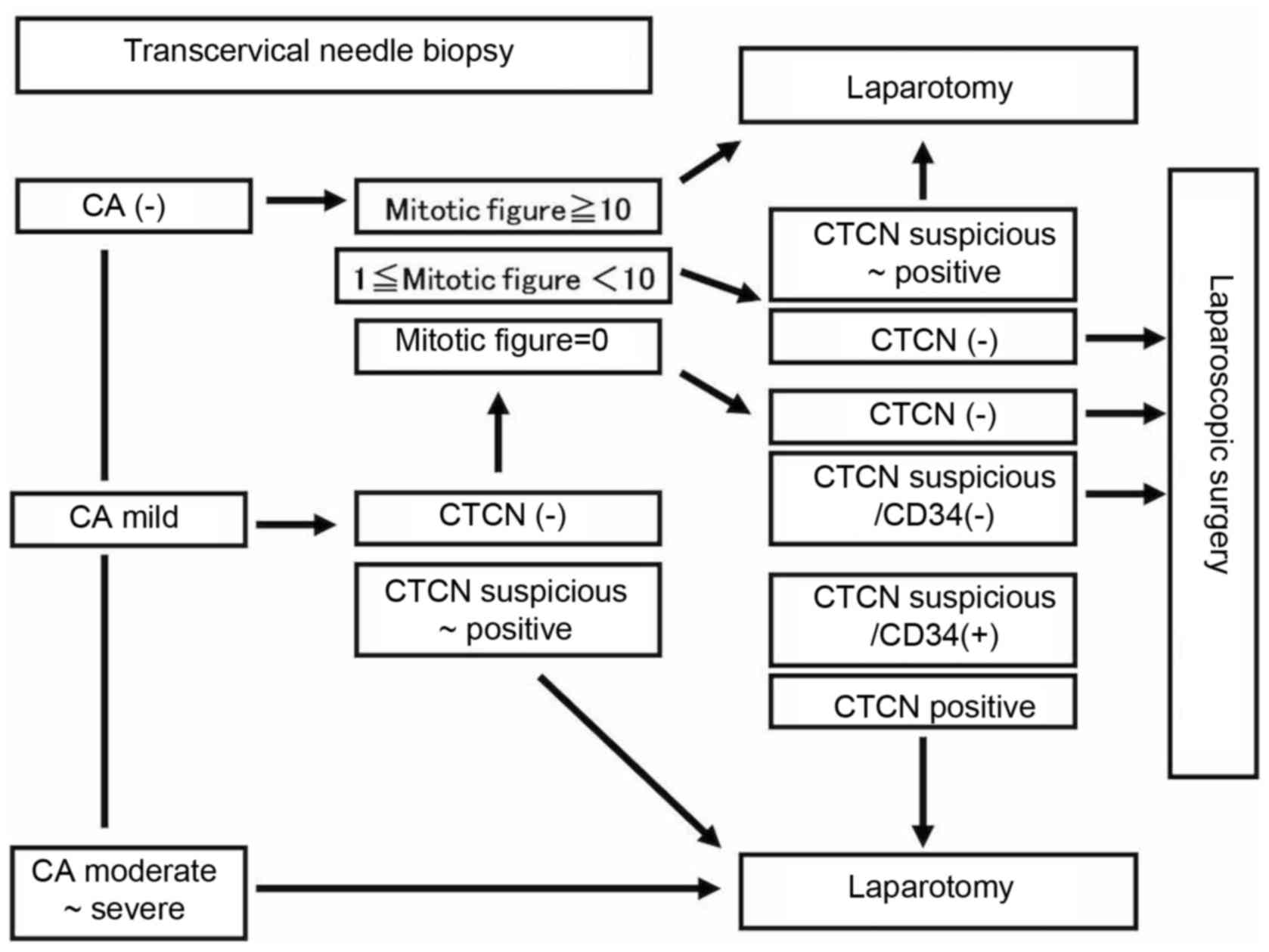
Thus, laparoscopic surgery is histopathologically safe when these 3
factors are negative in the transcervical needle biopsy specimens.
However, if moderate or severe cytological atypia is found in
transcervical needle biopsy specimens, the tumor is likely to be a
smooth muscle tumor of uncertain malignant potential or
leiomyosarcoma, and laparoscopic surgery is therefore not
recommended. Additionally, in the present study, leiomyosarcoma was
the final diagnosis in 1 patient with mild cytological atypia and
in 3 patients with no cytological atypia. The specimens of these
patients (1 patient with mild cytological atypia and 3 patients
with no cytological atypia) comprised mainly necrotic areas with
few viable cells. As biopsies target the parts of tumors with
abnormal MRI findings, necrotic tissue is often obtained in
patients with leiomyosarcoma. When a specimen contains areas with
suspected or positive coagulative tumor cell necrosis, laparoscopic
surgery is not recommended, due to the limited number of cells
available from viable areas leading to an underestimation of the
degree of cytological atypia.
Laparoscopic surgery is not recommended in patients
with tumors that exhibit ≥10 mitotic figures in all fields
examined, as such tumors are likely to be leiomyosarcomas. The
patients with biopsy specimens that contained 1–9 mitotic figures
received final diagnoses of leiomyosarcoma. However, in all such
cases, the biopsy specimens exhibited areas with suspected or
positive coagulative tumor cell necrosis regions and a limited
number of viable cells. Therefore, when mitotic figures in
transcervical needle biopsy specimens containing necrotic regions
are identified, laparoscopic surgery is considered contraindicated
in these patients for the same reasons as it is in patients with
cytological atypia, mainly due to the limited number of cells
available from viable areas leading to an underestimation of the
degree of mitotic figures.
As the possibility of leiomyosarcoma is high when
coagulative tumor cell necrosis is present, laparoscopic surgery is
not recommended in such patients. Of patients with suspected
coagulative tumor cell necrosis, ~10% exhibit leiomyosarcoma.
Patients with a final diagnosis that is not leiomyosarcoma but who
exhibit suspected coagulative tumor cell necrosis, also
occasionally exhibit hyaline necrosis in leiomyoma or smooth muscle
tumors of uncertain malignant potential. The presence of hyaline
necrosis does not contraindicate laparoscopic surgery. However, it
may be difficult to differentiate between coagulative tumor cell
necrosis and hyaline necrosis on HE-stained specimens. We
previously reported that coagulative tumor cell necrosis and
hyaline necrosis contain significantly different numbers of
anti-cluster of differentiation (CD)34 antibody-positive vessels.
Vessels in the areas of coagulative tumor cell necrosis appear to
retain immunostaining by the anti-CD34 antibody. In the present
study, CD34-stained vessels were counted for each specimen at
high-power fields (magnification, ×40) and the highest number of
positive vessels was recorded. We found that ~80% of
leiomyosarcomas exhibit >10 CD34-stained vessels in necrotic
areas and that the highest combined sensitivity and specificity is
achieved by setting the cut-off score at 10 CD34-stained vessels
(8). None of the smooth muscle tumors
of uncertain malignant potential examined in the hospital of Osaka
City University have exhibited coagulative tumor cell necrosis,
thus, this combination is likely to be rare. Laparoscopic surgery
is considered acceptable in patients with biopsies that are
negative for coagulative tumor cell necrosis, or in patients with
<10 CD34-positive vessels in lesions with suspected coagulative
tumor cell necrosis. Based on the data obtained in the present
study, the proposed algorithm for the indications for laparoscopic
surgery is presented in Fig. 6.
Laparoscopic surgery for smooth muscle tumors is
considered histopathologically safe when HE-stained specimens,
obtained by transcervical needle biopsy of areas in tumors
exhibiting high intensity on MRI scans, are negative for all 3 of
the following criteria: Cytological atypia, mitotic figures and
coagulative tumor cell necrosis. However, if any combination of
moderate or severe cytological atypia, >10 mitotic figures and
coagulative tumor cell necrosis is identified in the transcervical
needle biopsy specimens, laparoscopic surgery is not
recommended.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
MMu designed the study and wrote the initial draft
of the manuscript. TI, MK, MMa and NK contributed to analysis and
interpretation of data, and assisted in the preparation of the
manuscript. TF and TS contributed to data collection and
interpretation and critically reviewed the manuscript. All authors
approved the final version of the manuscript, and agreed to be
accountable for all aspects of the work in ensuring that questions
related to the accuracy or integrity of any part of the work are
appropriately investigated and resolved.
Ethics approval and consent to
participate
As the present study was retrospective, the Ethics
Committee of Osaka City University (Osaka, Japan) waived the
requirement for informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
MRI
|
magnetic resonance imaging
|
|
HE
|
hematoxylin and eosin
|
References
|
1
|
Semm K: New methods of pelviscopy
(gynecologic laparoscopy) for myomectomy, ovariectomy, tubectomy
and adrenectomy. Endoscopy. 11:85–93. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
U.S. Food and Drug Administration:
Laparoscopic uterine power morcellation in hysterectomy and
myomectomy: FDA safety communication. http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm393576.htmNovember.
2014
|
|
3
|
Ton R, Kilic GS and Phelps JY: A
medical-legal review of power morcellation in the face of the
recent FDA warning and litigation. J Minim Invasive Gynecol.
22:564–572. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tanaka O, Nishida M, Tsunoda H, Okamoto Y
and Yoshikawa H: Smooth muscle tumors of uncertain malignant
potential and leiomyosarcomas of the uterus: MR findings. J Magn
Reson Imaging. 20:998–1007. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kawamura N, Ichimura T, Ito F, Shibata S,
Takahashi K, Tsujimura A, Ishiko O, Haba T, Wakasa K and Ogita S:
Transcervical needle biopsy for the differential diagnosis between
uterine sarcoma and leiomyoma. Cancer. 94:1713–1720. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bell SW, Kempson RL and Hendrickson MR:
Problematic uterine smooth muscle neoplasms. A clinicopathologic
study of 213 cases. Am J Surg Pathol. 18:535–538. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
International Agency for Research on
Cancer (IARC): WHO Classification of Tumours of Female Reproductive
Organs. Kurman RJ, Carcangiu ML, Herrington CS and Young RH: 4th
edition. IARC; Lyon: pp. 238–239. 2014
|
|
8
|
Yoshida C, Ichimura T, Kawamura N, Nakano
A, Kasai M, Sumi T and Ishiko O: A scoring system for
histopathologic and immunohistochemical evaluations of uterine
leiomyosarcomas. Oncol Rep. 22:725–731. 2009. View Article : Google Scholar : PubMed/NCBI
|