Introduction
Lung cancer is the most lethal malignancy worldwide.
Chemotherapy is one of the most commonly used treatments (1). Even though chemotherapy has improved the
survival rate of patients with lung cancer, the 5-year survival
rate in the last 25 years has remained at 15% (2). Multidrug resistance is the primary
reason for the low survival rates (3). Cisplatin is widely used as first-line
therapy for the treatment of lung cancer; however, drug resistance
presents a major concern (2).
Cisplatin is a non-specific cytotoxic drug causing
cell cycle arrest. Currently, Cisplatin possesses anticancer
effects, promotes DNA shearing and changes in regulating protein
expression associated with regulatory signal pathways (4). However, drug resistance mechanisms of
lung cancer cells are not fully understood. Therefore, it is
important to further investigate drug resistance mechanisms and
identify novel molecular targets aiming at improving the effects of
chemotherapy for lung cancer (1).
It is well established that the p53 protein is not
stable and is liable to be degraded. The half-life of the protein
is only a few minutes (5). The main
functions of p53 are cell cycle inhibition and induction of
apoptosis through caspase activation. There are three critical
steps leading to the activation of the p53 signaling pathway and
subsequent induction of p53-mediated apoptosis; transcriptional
induction of redox-associated genes, formation of reactive oxygen
species (ROS) and oxidative degradation of mitochondria (6). p53 regulates pro-apoptotic proteins,
such as B-cell lymphoma 2-associated X-protein (Bax), phorbol
12-myristate 13-acetate-induced protein 1 (Noxa) and
apoptosis-inducing factor (AIF), activates oxidation of oxygen
radicals, and restrains reductive expression of clearing ROS, so as
to induce apoptosis (7).
Miltirone is a commonly used compound in traditional
Chinese medicine (8). A number of
biological and pharmacological activities have been attributed to
it, including anti-inflammatory, antioxidant and pain-relieving
mechanisms, regulation of menstruation (8). It has been demonstrated that miltirone
exhibits multiple pharmacological actions, such as coronal flow
increase, myocardial ischemic injury protection, microcirculation
improvement, antisepsis, renal function improvement, anti-ischemic
and protection of brain tissue (9).
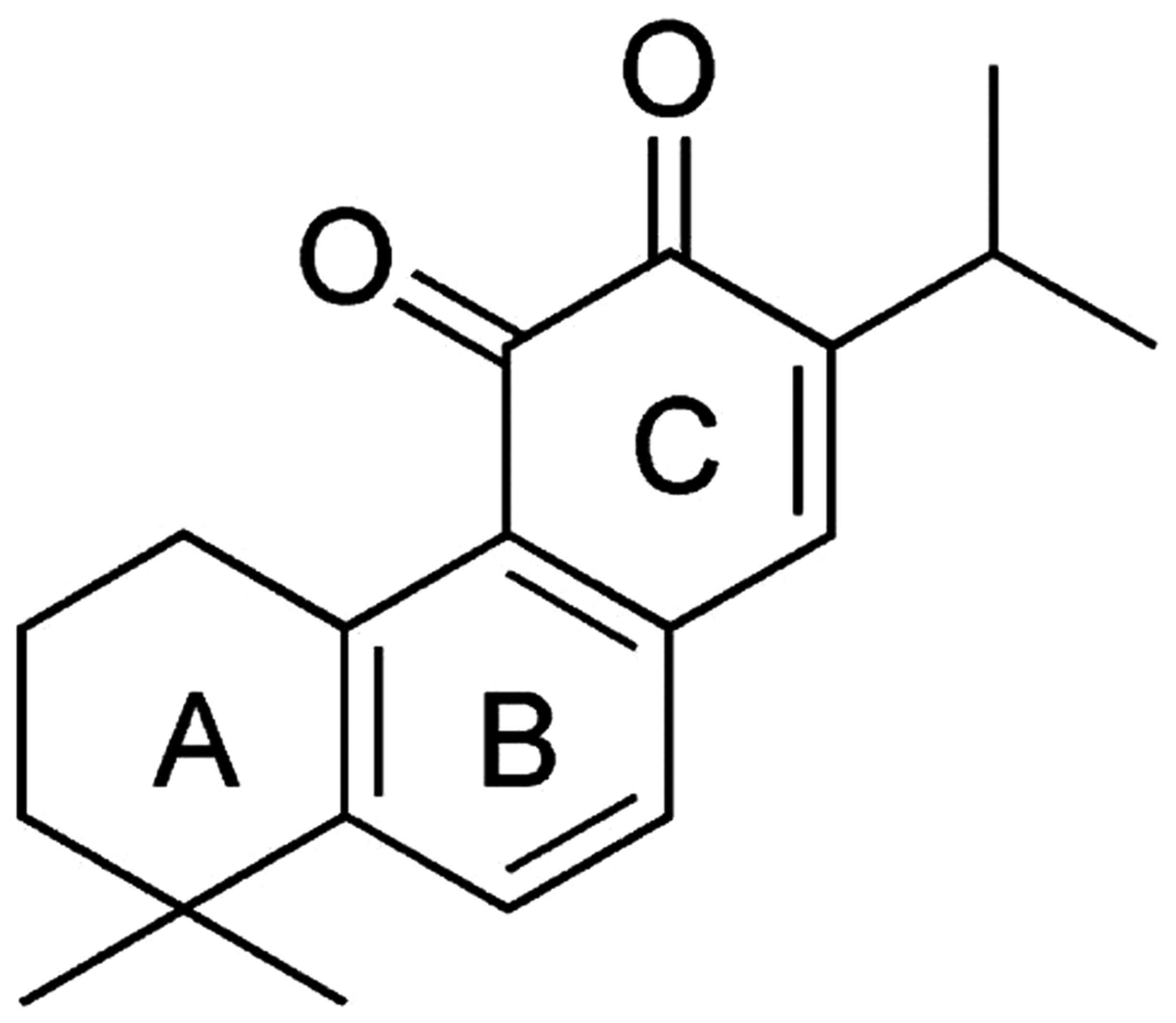
Miltirone has a molecular formula of
C19H22O2 and a melting point of
100°C. Miltirone reduces the platelet aggregation induced by
collagen and the central nervous system (10). A number of in vitro studies
have demonstrated that miltirone has antineoplastic activity over a
range of cancer types and inhibits cancer cell proliferation
(11). In the present study, the
effect of miltirone on cisplatin-resistant lung cancer cells and
the underlying molecular mechanism of action were investigated.
Materials and methods
Cell lines and cisplatin
chemoresistance assay
The HCC827 and A549 lung tumor cells were purchased
from the Shanghai Cell Bank of the Chinese Academy of Sciences
(Shanghai, China) and were maintained in RPMI-1640 medium (Thermo
Fisher Scientific, Inc., Waltham, MA, USA) supplemented with 10%
fetal bovine serum (FBS; Gibco; Thermo Fisher Scientific, Inc.) and
incubated at 37°C in 5% CO2. Miltirone (chemical
structure presented in Fig. 1) and
cisplatin were purchased from Sigma-Aldrich; Merck KGaA (Darmstadt,
Germany). HCC827 and A549 cells were maintained with 10, 100 µM, 1,
5, 10, 25 and 50 mM of cisplatin at 37°C for 3–5 days until they
were chemoresistant.
Cell viability assay
HCC827 and A549 cells were seeded in duplicate in
96-well plates at a density of 5×103 cells per well and
treated with 10, 20 or 40 µM miltirone for 0.5, 1 or 2 days. Cell
viability was determined using an MTT assay (Thermo Fisher
Scientific, Inc.). MTT incubation was performed at 37°C for 4 h,
the formazan crystals were dissolved in dimethyl sulfoxide and the
absorbance at 570 nm was determined using a microplate reader
(model 550; Bio-Rad Laboratories, Inc., Hercules, CA, USA).
Activation of caspases
HCC827 and A549 cells were seeded in duplicate in
96-well plates at a density of 5×103 cells per well and
treated with 10, 20 or 40 µM miltirone for 48 h. Cells were
incubated with N-acetyl-Asp-Glu-Val-Asp-p-nitroanilide or
N-acetyl-Ile-Glu-Thr-Asp-p-nitroanilide (both from Beyotime
Institute of Biotechnology, Haimen, China) for 2 h at 37°C.
Absorbance at 405 nm was determined using the model 550 microplate
reader.
Flow cytometric analysis of
apoptosis
HCC827 and A549 cells were seeded in duplicate in
6-well plates at a density of 2×105 cells per well and
treated with 10, 20 or 40 µM miltirone for 48 h. HCC827 and A549
cells were then harvested and resuspended in 0.5 ml binding buffer
containing Annexin V and propidium iodide (PI) (both from Nanjing
KeyGen Biotech Co., Ltd., Nanjing, China) for 30 min at 37°C in the
dark. Apoptotic cells were analyzed using a flow cytometer (BD
FASCanto C6; BD Biosciences, Franklin Lakes, NJ, USA) and FlowJo
7.6.1. software (FlowJo, LLC, Ashland, OR, USA).
Western blot analysis
HCC827 and A549 cells were lysed with a
radioimmunoprecipitation assay (Sigma-Aldrich; Merck KGaA) for 30
min on ice. Total protein concentration was determined using the
Bradford protein assay (Beyotime Institute of Biotechnology) and 50
µg protein was separated using SDS-PAGE on 8–15% polyacrylamide
gels. The separated proteins were then transferred onto a
polyvinylidene difluoride membrane (Sigma-Aldrich; Merck KGaA) and
blocked with 5% skimmed milk powder in Tris-buffered saline with
Tween-20 (TBST) for 1 h at 37°C. The membranes were incubated with
primary antibodies against Bax (cat. no. sc-6236, 1:500), AIF
(sc-5586, 1:500), p53 (cat. no. sc-6243, 1:500), matrix
metalloproteinase 2 (MMP2) (cat. no. sc-10736, 1:500), MMP9 (cat.
no. sc-10737, 1:500) (all from Santa Cruz Biotechnology, Inc.,
Dallas, TX, USA)and GAPDH (cat. no. AF1186, 1:2,000; Beyotime
Institute of Biotechnology) at 4°C overnight. Then, membranes were
washed with TBST and incubated with horseradish peroxidase-labeled
anti-rabbit secondary antibodies (cat. no. sc-2030, 1:5,000; Santa
Cruz Biotechnology, Inc.) for 1 h at 37°C. Protein bands were
visualized using the Amersham ECL Western Blotting Detection kit
(GE Healthcare Life Sciences, Shanghai, China) and analyzed using
Image Lab 3.0 (Bio-Rad Laboratories, Inc.).
Mitochondrial labelling assay
Cells were incubated for 45 min under growth
conditions in the dark at 37°C and 5% CO2. Cells were
incubated with the Mitotracker® Red CM-H2XRos (0.5
ng/µl) for 20 min in the dark at 37°C. Following incubation, the
absorbance at 525 nm was determined using the model 550 microplate
reader.
Statistical analysis
Results are expressed as the mean ± standard
deviation. Comparison between two or more groups was performed by
one-way analysis of variance followed by a Dunnett test, Tukey's
test or a Newman-Keuls test. P<0.05 (two-tailed) was considered
to indicate a statistically significant difference.
Results
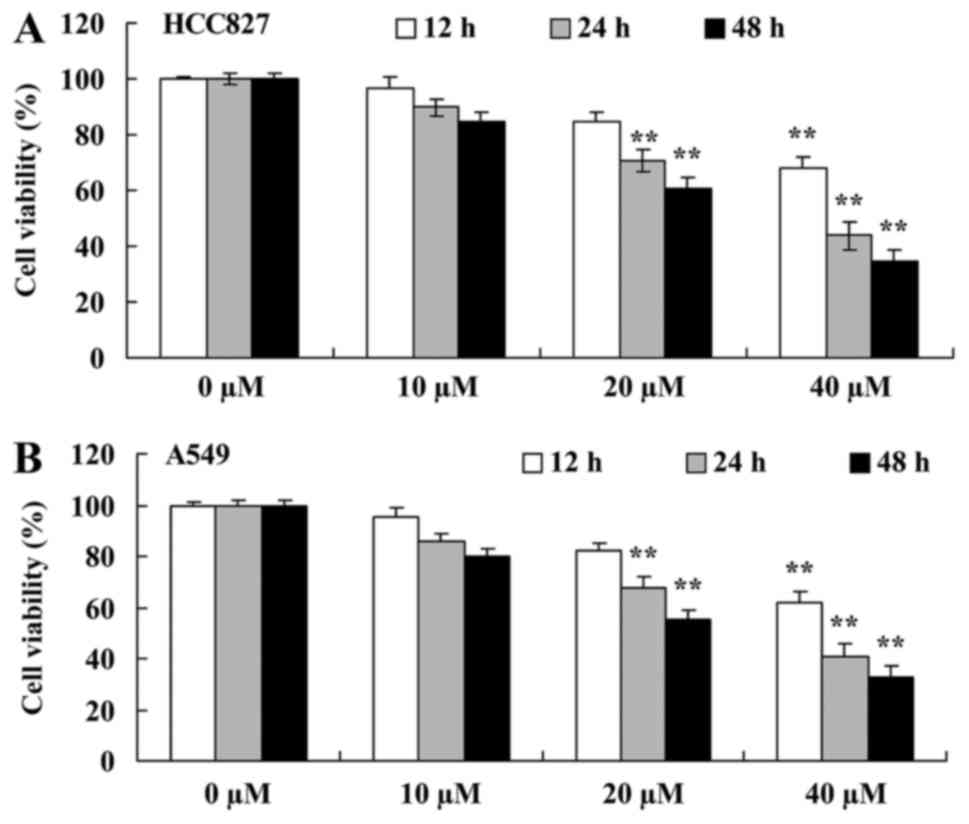
Miltirone inhibits the viability of
cisplatin-resistant HCC827 and A549 lung cancer cells
To examine the effect of miltirone on the viability
of cisplatin-resistant HCC827 and A549 lung cancer cells maintained
in 50 mM cisplatin, cell viability was determined using the MTT
assay. Treatment with miltirone inhibited the viability of HCC827
and A549 cisplatin-resistant cells in a time- and dose-dependent
manner (Fig. 2). As presented in
Fig. 2, 20 and 40 µM miltirone
significantly inhibited cell viability of HCC827 and A549
cisplatin-resistant cells, compared with the untreated control.
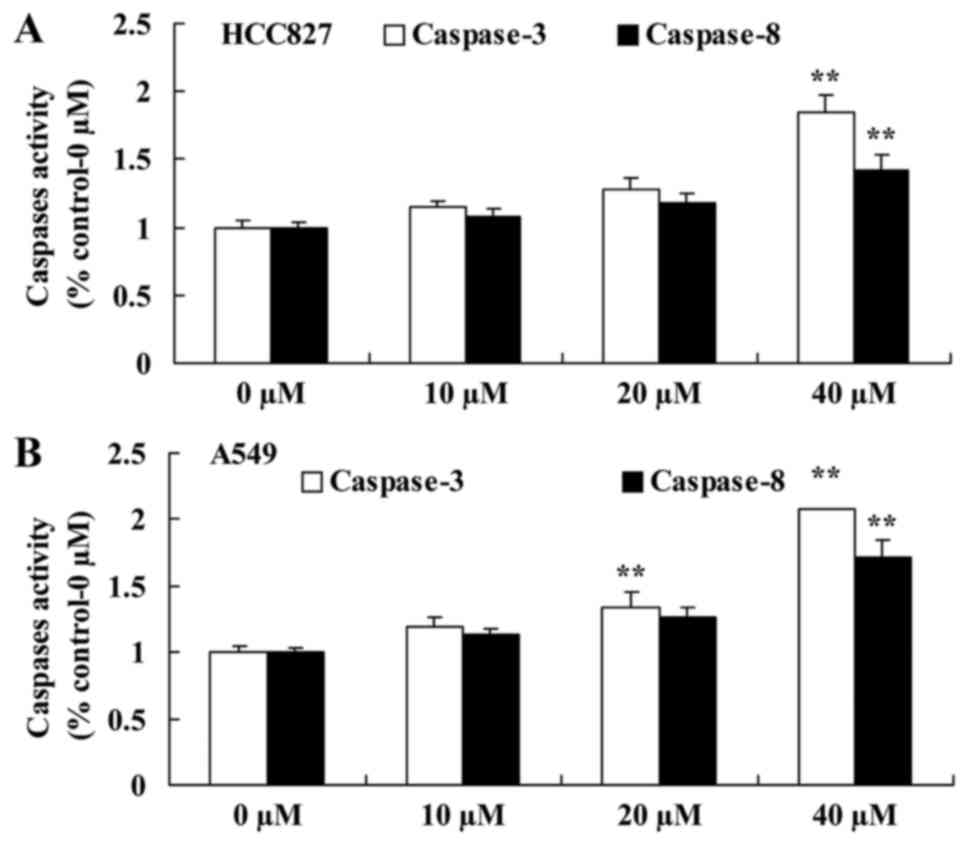
Miltirone increases caspase-3/8
activity in HCC827 and A549 cisplatin-resistant lung cancer
cells
To further investigate the anticancer effect of
miltirone on the induction of apoptosis in HCC827 and A549
cisplatin-resistant lung cancer cells, caspase-3 and caspase-8
activities were examined using commercial kits. As presented in
Fig. 3A, 40 µM miltirone
significantly increased caspase-3 and caspase-8 activities in
cisplatin-resistant HCC827 cells, compared with the untreated
control. Additionally, as presented in Fig. 3B, 20 or 40 µM miltirone significantly
increased caspase-3 and caspase-8 activities in cisplatin-resistant
A549 cells, compared with the untreated control.
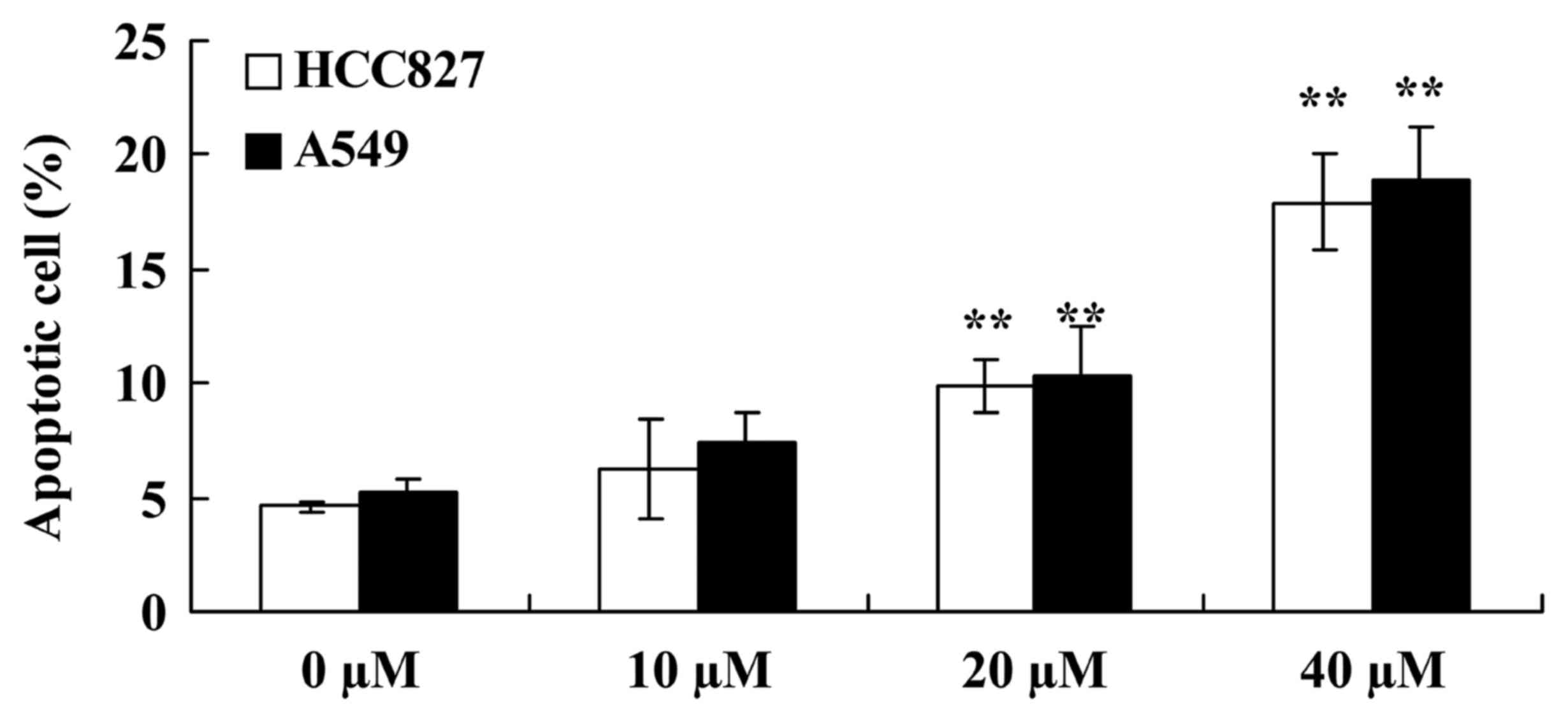
Miltirone induces apoptosis in HCC827
and A549 cisplatin-resistant lung cancer cells
Flow cytometric analysis was performed to
investigate the effect of miltirone on the induction of apoptosis
in HCC827 and A549 cisplatin-resistant lung cancer cells. As
presented in Fig. 4, 20 or 40 µM
miltirone significantly increased the proportion of apoptotic cells
in HCC827 and A549 cisplatin-resistant cells, compared with the
untreated control.
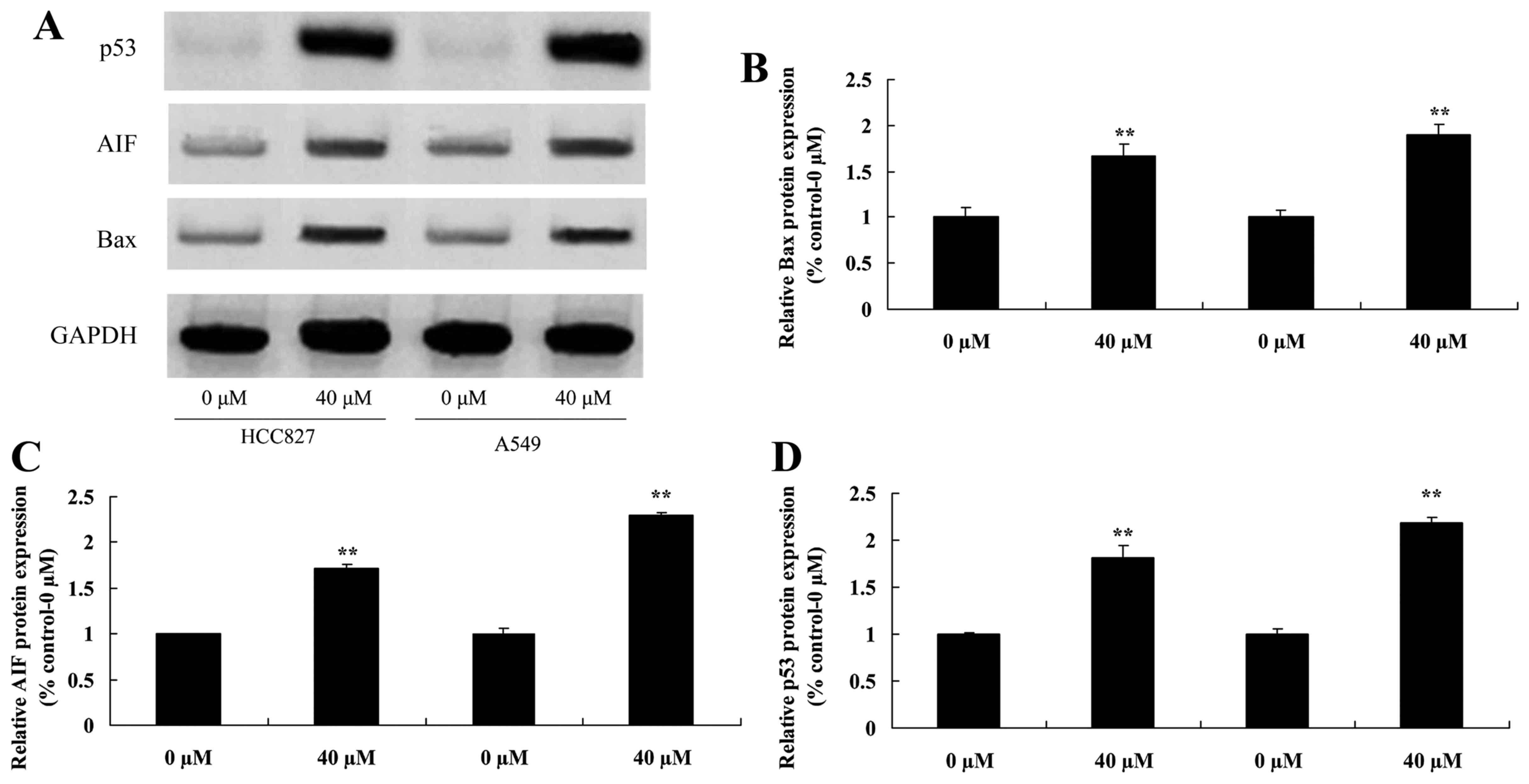
Miltirone increases Bax, AIF and p53
protein expression in HCC827 and A549 cisplatin-resistant lung
cancer cells
To investigate the regulatory effects of miltirone
on HCC827 and A549 cisplatin-resistant lung cancer cells, Bax, AIF
and p53 protein expression was examined using Western blotting. As
presented in Fig. 5, 40 µM miltirone
significantly increased the expression of Bax, AIF and p53 protein
in HCC827 and A549 cisplatin-resistant lung cancer cells, compared
with the untreated control.
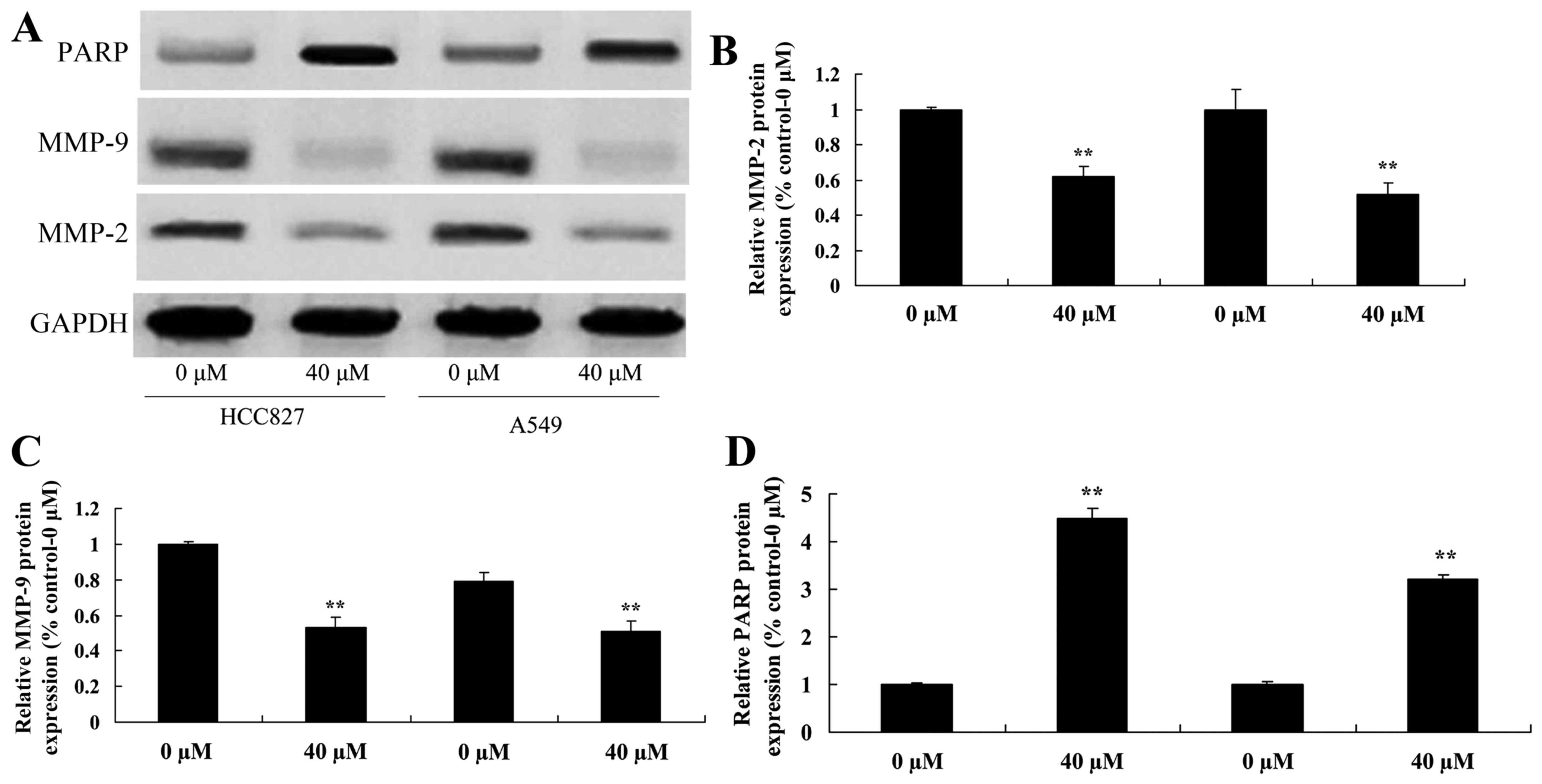
Miltirone suppresses MMP2/9 and
increases PARP protein expression in HCC827 and A549
cisplatin-resistant lung cancer cells
To further investigate the underlying molecular
mechanism of miltirone treatment on HCC827 and A549
cisplatin-resistant lung cancer cells, MMP2/9 and PARP protein
expression was examined using western blotting. As presented in
Fig. 6, 40 µM miltirone significantly
suppressed the expression of MMP2/9 protein and significantly
increased the expression of PARP protein in HCC827 and A549
cisplatin-resistant lung cancer cells, compared with the untreated
control.
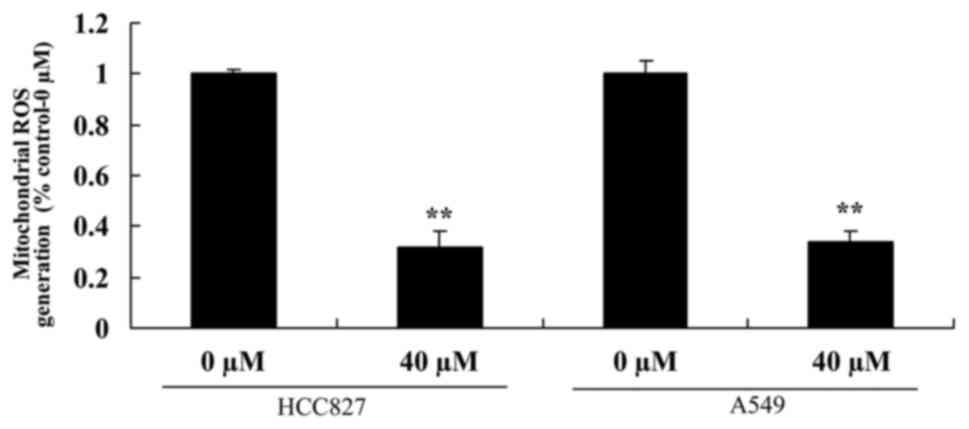
Miltirone inhibits mitochondrial ROS
generation in HCC827 and A549 cisplatin-resistant lung cancer
cells
The effect of miltirone on mitochondrial ROS
generation in HCC827 and A549 cisplatin-resistant lung cancer cells
was examined. As presented in Fig. 7,
40 µM miltirone significantly inhibited ROS generation in HCC827
and A549 cisplatin-resistant lung cancer cells, compared with the
untreated control.
Discussion
Lung cancer is the most lethal malignancy worldwide
characterized by the highest mortality rate. It is estimated that
>40% of patients with lung cancer are diagnosed with
advanced-stage disease (12). Only
~25% of patients are diagnosed with Phase I disease. For patients
diagnosed at an advanced stage, chemotherapy is the first-line
treatment following surgery (13).
Even though there has been progress in chemotherapy of lung cancer,
5-year survival rates have not improved in the last 25 years and
remain at ~15%. Multidrug resistance is a critical reason for the
poor survival rates of lung cancer (14). The strategy mainly used for the
treatment of lung cancer is platinum-based combinational
chemotherapy (14). To the best of
our knowledge, the present study is the first to provide evidence
that miltirone significantly inhibited cell proliferation and
induced apoptosis in HCC827 and A549 cisplatin-resistant lung
cancer cells.
In the treatment of lung cancer, cisplatin is an
effective and widely used first-line agent. However, drug
resistance presents a major concern (15). Therefore, it is important to
investigate the drug resistance mechanisms and identify novel
molecular targets aiming to reverse drug resistance and improve the
curative effects of chemotherapy for lung cancer. The results of
the present study suggest that miltirone significantly increased
caspase-3/8 activities and Bax protein expression in HCC827 and
A549 cisplatin-resistant cells.
Drug resistance of lung cancer cells is mainly
attributed to resistance to apoptotic cell death. Induction of
apoptotic cell death is the main mechanism of action of agents used
for the treatment of lung cancer (16). The redox status of cells may determine
their viability. Two oxidation-reduction systems have been
described in normal cells: the non-enzyme system peroxide and the
enzyme system peroxide (17). The
former includes glycine peptide and thioredoxin reductase. The
latter includes superoxide dismutase, catalase and glutathione
peroxidase. They maintain ROS generated from oxidative stress in a
relatively stable level. A number of studies have demonstrated that
ROS in cells and alterations in the redox status are associated
with apoptosis (18). The results of
the present study suggest that miltirone significantly inhibited
ROS generation and MMP2/9 protein expression in HCC827 and A549
cisplatin-resistant lung cancer cells. In agreement with these
results, Wang et al (11)
demonstrated that miltirone induced mitochondrial dysfunction and
ROS- and p53-dependent apoptosis through MMP, AIF and activation of
caspases in colon cancer cells.
Through DNA damage, ROS are important activating
agents of p53 (7). ROS regulate p53
activity and DNA damage, promoting transcriptional activation of
p53 (6). In addition, ROS generation
may be regulated by p53. p53 is able to transcriptionally activate
genes regulating the production of reactive oxygen radicals.
Furthermore, reactive oxygen radicals may induce apoptosis
(19). The stability of p53 regulates
the induction of apoptosis by promoting pro-apoptotic proteins,
such as Bax, Noxa or p53-upregulated modulator of apoptosis. In
addition, stable p53 generates increased levels of ROS and
contributes to apoptosis induction (20). The results of the present study
identified that miltirone significantly induces p53 protein
expression in HCC827 and A549 cisplatin-resistant lung cancer
cells.
Miltirone is a flavoprotein in mitochondria and has
dual functions, acting as an oxidoreductive and pro-apoptotic
molecule. Following stimulation of pro-apoptotic signals, AIF moves
from the mitochondrial inner membrane by proteolysis (21). When the mitochondrion is damaged, the
mitochondrial permeability transition pore is open, resulting in
the release of AIF to the cytosol and its translocation to the cell
nucleus (22). AIF may cause
chromatin condensation and DNA fragmentation in the nucleus, but is
caspase-independent. Therefore, it is considered to be a
caspase-independent death effector. A previous in vitro
study has demonstrated that cisplatin induces AIF translocation
from mitochondria to the nucleus in renal tubular epithelial cells
through a p53 and caspase-3-dependent mechanism, leading to
apoptosis (23). In the present
study, it was demonstrated that miltirone significantly induced AIF
protein expression in HCC827 and A549 cisplatin-resistant lung
cancer cells.
Recently, a number of studies indicated an important
regulatory role of AIF for upstream activation of nuclear PARP.
PARP is a family of proteins involved in a number of distinct roles
including DNA damage repair and induction of apoptosis (24). On the one hand, PAR mediates DNA
damage repair in cells (25). On the
other hand, when PARP is activated following serious injury,
NAD+ in cells is increased (26). Thus, ATP levels are decreased,
impairing normal cellular functions. Previous research has
indicated that AIF activates PARP leading to apoptosis induction
(27). In the present study, it was
demonstrated that miltirone significantly induced PARP protein
expression in HCC827 and A549 cisplatin-resistant lung cancer
cells. Similarly, Wu et al (28) demonstrated that miltirone induced
apoptosis in leukemia cells through activation of caspases and
PARP.
The results of the present study indicate that
miltirone suppressed cisplatin-resistant cell viability and induced
apoptosis in HCC827 and A549 lung cancer cells through ROS-p53,
AIF, PARP and MMP2/9 signaling pathways. The results of the present
study provide novel insights into the effect of miltirone on
cisplatin-resistant lung cancer cell apoptosis that may have
clinical implications.
References
|
1
|
Senan S, Cardenal F, Vansteenkiste J,
Stigt J, Akyol F, De Neve W, Bakker J, Dupont JM, Scagliotti GV,
Ricardi U and van Meerbeeck JP: A randomized phase II study
comparing induction or consolidation chemotherapy with
cisplatin-docetaxel, plus radical concurrent chemoradiotherapy with
cisplatin-docetaxel, in patients with unresectable locally advanced
non-small-cell lung cancer. Ann Oncol. 22:553–558. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sekine I, Nokihara H, Takeda K, Nishiwaki
Y, Nakagawa K, Isobe H, Mori K, Matsui K, Saijo N and Tamura T:
Randomised phase II trial of irinotecan plus cisplatin vs
irinotecan, cisplatin plus etoposide repeated every 3 weeks in
patients with extensive-disease small-cell lung cancer. Br J
Cancer. 98:693–696. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tai CJ, Wang CK, Tai CJ, Tzao C, Lien YC,
Hsieh CC, Hsieh CI, Wu HC, Wu CH, Chang CC, et al: Evaluation of
safety and efficacy of salvage therapy with sunitinib, docetaxel
(Tyxane) and cisplatinum followed by maintenance vinorelbine for
unresectable/metastatic nonsmall cell lung cancer: Stage 1 of a
simon 2 stage clinical trial. Medicine (Baltimore). 94:e23032015.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jiang CP, Wu BH, Chen SP, Fu MY, Yang M,
Liu F and Wang BQ: High COL4A3 expression correlates with poor
prognosis after cisplatin plus gemcitabine chemotherapy in
non-small cell lung cancer. Tumour Biol. 34:415–420. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wang R, Ma L, Weng D, Yao J, Liu X and Jin
F: Gallic acid induces apoptosis and enhances the anticancer
effects of cisplatin in human small cell lung cancer H446 cell line
via the ROS-dependent mitochondrial apoptotic pathway. Oncol Rep.
35:3075–3083. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhou W, Tian D, He J, Wang Y, Zhang L, Cui
L, Jia L, Zhang L, Li L, Shu Y, et al: Repeated PM2.5 exposure
inhibits BEAS-2B cell P53 expression through ROS-Akt-DNMT3B
pathway-mediated promoter hypermethylation. Oncotarget.
7:20691–20703. 2016.PubMed/NCBI
|
|
7
|
Matsumoto M, Nakajima W, Seike M, Gemma A
and Tanaka N: Cisplatin-induced apoptosis in non-small-cell lung
cancer cells is dependent on Bax- and Bak-induction pathway and
synergistically activated by BH3-mimetic ABT-263 in p53 wild-type
and mutant cells. Biochem Biophys Res Commun. 473:490–496. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhou L, Jiang L, Xu M, Liu Q, Gao N, Li P
and Liu EH: Miltirone exhibits antileukemic activity by
ROS-mediated endoplasmic reticulum stress and mitochondrial
dysfunction pathways. Sci Rep. 6:205852016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mostallino MC, Mascia MP, Pisu MG,
Busonero F, Talani G and Biggio G: Inhibition by miltirone of
up-regulation of GABAA receptor alpha4 subunit mRNA by ethanol
withdrawal in hippocampal neurons. Eur J Pharmacol. 494:83–90.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhou X, Wang Y, Hu T, Or PM, Wong J, Kwan
YW, Wan DC, Hoi PM, Lai PB and Yeung JH: Enzyme kinetic and
molecular docking studies for the inhibitions of miltirone on major
human cytochrome P450 isozymes. Phytomedicine. 20:367–374. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang L, Hu T, Shen J, Zhang L, Li LF, Chan
RL, Li MX, Wu WK and Cho CH: Miltirone induced mitochondrial
dysfunction and ROS-dependent apoptosis in colon cancer cells. Life
Sci. 151:224–234. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Watanabe S, Inoue A, Nukiwa T and
Kobayashi K: Comparison of Gefitinib Versus Chemotherapy in
Patients with Non-small Cell Lung Cancer with Exon 19 Deletion.
Anticancer Res. 35:6957–6961. 2015.PubMed/NCBI
|
|
13
|
Shukuya T, Yamanaka T, Seto T, Daga H,
Goto K, Saka H, Sugawara S, Takahashi T, Yokota S, Kaneda H, et al:
Nedaplatin plus docetaxel versus cisplatin plus docetaxel for
advanced or relapsed squamous cell carcinoma of the lung
(WJOG5208L): A randomised, open-label, phase 3 trial. Lancet Oncol.
16:1630–1638. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tsunoda T, Koizumi T, Hayasaka M, Hirai K,
Koyama S, Takabayashi Y, Fujimoto K and Kubo K: Phase II study of
weekly docetaxel combined with cisplatin in patients with advanced
non-small-cell lung cancer. Cancer Chemother Pharmacol. 54:173–177.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tiseo M, Boni L, Ambrosio F, Camerini A,
Vitale MG, Baldini E, Cinieri S, Zanelli F, Defraia E, Passalacqua
R, et al: Italian multicenter phase III randomized study of
cisplatin-etoposide with or without bevacizumab as first-line
treatment in extensive stage small cell lung cancer: Treatment
rationale and protocol design of the GOIRC-AIFA FARM6PMFJM trial.
Clin Lung Cancer. 16:67–70. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yun HS, Baek JH, Yim JH, Lee SJ, Lee CW,
Song JY, Um HD, Park JK, Park IC and Hwang SG: Knockdown of
hepatoma-derived growth factor-related protein-3 induces apoptosis
of H1299 cells via ROS-dependent and p53-independent NF-κB
activation. Biochem Biophys Res Commun. 449:471–476. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
He L, Lai H and Chen T: Dual-function
nanosystem for synergetic cancer chemo-/radiotherapy through
ROS-mediated signaling pathways. Biomaterials. 51:30–42. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hong Y, Sengupta S, Hur W and Sim T:
Identification of Novel ROS Inducers: Quinone derivatives tethered
to long hydrocarbon Chains. J Med Chem. 58:3739–3750. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hu Z, Zeng Q, Zhang B, Liu H and Wang W:
Promotion of p53 expression and reactive oxidative stress
production is involved in zerumbone-induced cisplatin sensitization
of non-small cell lung cancer cells. Biochimie. 107:Pt B. 257–262.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Meijer A, Kruyt FA, van der Zee AG,
Hollema H, Le P, ten Hoor KA, Groothuis GM, Quax WJ, de Vries EG
and de Jong S: Nutlin-3 preferentially sensitises wild-type
p53-expressing cancer cells to DR5-selective TRAIL over rhTRAIL. Br
J Cancer. 109:2685–2695. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hunter TB, Manimala NJ, Luddy KA, Catlin T
and Antonia SJ: Paclitaxel and TRAIL synergize to kill
paclitaxel-resistant small cell lung cancer cells through a
caspase-independent mechanism mediated through AIF. Anticancer Res.
31:3193–3204. 2011.PubMed/NCBI
|
|
22
|
Zhang W, Wang X and Chen T: Resveratrol
induces mitochondria-mediated AIF and to a lesser extent
caspase-9-dependent apoptosis in human lung adenocarcinoma ASTC-a-1
cells. Mol Cell Biochem. 354:29–37. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chen JT, Huang CY, Chiang YY, Chen WH,
Chiou SH, Chen CY and Chow KC: HGF increases cisplatin resistance
via down-regulation of AIF in lung cancer cells. Am J Respir Cell
Mol Biol. 38:559–565. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cardnell RJ, Feng Y, Mukherjee S, Diao L,
Tong P, Stewart CA, Masrorpour F, Fan Y, Nilsson M, Shen Y, et al:
Activation of the PI3K/mTOR pathway following PARP inhibition in
small cell lung cancer. PLoS One. 11:e01525842016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Tangutoori S, Baldwin P and Sridhar S:
PARP inhibitors: A new era of targeted therapy. Maturitas. 81:5–9.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Gangopadhyay NN, Luketich JD, Opest A,
Landreneau R and Schuchert MJ: PARP inhibitor activates the
intrinsic pathway of apoptosis in primary lung cancer cells. Cancer
Invest. 32:339–348. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Cardnell RJ and Byers LA: Proteomic
markers of DNA repair and PI3K pathway activation predict response
to the PARP inhibitor BMN 673 in small cell lung cancer - response.
Clin Cancer Res. 20:22372014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wu CF and Efferth T: Miltirone induces
G2/M cell cycle arrest and apoptosis in CCRF-CEM acute
lymphoblastic leukemia cells. J Nat Prod. 78:1339–1347. 2015.
View Article : Google Scholar : PubMed/NCBI
|