Introduction
Chemoradiation therapy (CRT) as a treatment for
laryngeal cancer (LC) and hypopharyngeal cancer (HPC) has gained
widespread acceptance as it has produced high rates of laryngeal
preservation without compromising survival rates when compared with
total laryngectomy (TL) (1–3). However, different conclusions (such as
better results in terms of survival and/or local control achieved
by surgery) were additionally drawn from other studies (4–6). Salvage
laryngectomy was required in >50% of all patients with T4
[American Joint Committee on Cancer (AJCC) or Union for
International Cancer Control] cancer (2,7). However,
salvage laryngectomy may result in the loss of normal speech
function and higher rates of postoperative complications (8). Strategies to preserve the larynx are not
recommended for patients with T4a LC or T4a HPC, particularly those
with cartilage invasion, and initial surgery is generally employed
as the primary treatment method (9–11). A
number of studies have revealed poorer local control and survival
when treating LC or HPC with cartilage invasion by CRT compared
with that when treated by initial surgery (9,12). High
overall survival (OS) and laryngeal preservation rates have been
reported for patients with T4 tumor with cartilage invasion treated
with CRT (13), but the number of
cases is small.
The most common location of HPC is the pyriform
sinus (14). With regards to the
anatomic structure, the incidence rates of thyroid or cricoid
cartilage invasion in HPC should be higher compared with those in
LC as HPC is often located or even concealed between the thyroid
and cricoid cartilages (15). The
treatment modalities for HPC and LC, therefore, should be
different. In literature, various treatment modalities for partial
laryngectomy were established for LC, but few were developed for
HPC to avoid employing TL, including vertical
hemilaryngopharyngectomy (VHLP) (16–18),
supracricoid hemilaryngopharyngectomy (SCHLP) (19,20),
extended supraglottic laryngectomy (ESGL) (21) and near-total laryngectomy (22). However, the oncologic and functional
outcomes of these surgical techniques have seldom been reported.
Furthermore, HPC with simultaneous invasion of thyroid and cricoid
cartilages is not infrequent from our clinical experiences (~39% of
cartilage invasion in our series) (15). Additionally, the majority of open
partial laryngectomy (OPL) procedures are usually used for
non-extensive thyroid cartilage invasion (18–21), and
there are a limited number of previous studies on the simultaneous
invasion of thyroid and cricoid cartilages. TL and CRT are the
procedures most often used for HPC with cartilage invasion, and
these frequently cause unsatisfactory (either oncologic or
functional) outcomes (9–11).
Long-term tube-free tracheostomy (TFT) results in a
self-sustaining passage, which is established by a side-to-skin
stoma between the trachea and the anterior neck skin (23). A side-to-skin tracheotomy may maintain
adequate airway and allow the patient to phonate via remnants of
laryngeal structures, simply by occluding the tracheal stoma
(24–26). The present study aimed to identify a
feasible treatment strategy for HPC invading the thyroid and/or
cricoid cartilage by comparing the oncologic and functional
outcomes and quality of life between OPL with TFT and TL with an
artificial larynx (pneumatic tube).
Materials and methods
Patients
Between June 2008 and December 2014, patients with
previously untreated squamous cell carcinoma (SCC) (as confirmed by
biopsy) in the hypopharynx invading the thyroid and/or cricoid
cartilage, who underwent either OPL or TL at E-DA Hospital
(Kaohsiung, Taiwan) and had a >6-month postoperative follow-up
were retrospectively enrolled. The mean follow-up was 45 months
(range, 12–89 months). The exclusion criteria were i) inoperability
(due to internal carotid artery encasement); ii) extensive thyroid
cartilage invasion; iii) refusal of adjuvant radiotherapy (RT)/CRT;
and iv) T4b (AJCC) disease. Patients with extensive cartilage
invasion and those with inoperable or T4b disease were treated
using TL or CRT. In addition, patients with invasion of the
post-cricoid area crossing the midline, bilateral vocal cords or
arytenoids, tracheal ring and the base of the tongue (>2 cm)
were excluded for OPL treatment (but were treated with TL). In
total, 44 patients were included and all of them were male. Tumor
invasion to thyroid and/or cricoid cartilage was determined by
computed tomography (CT) scans. Tumor staging was based on the
guidelines of the AJCC (2002) (27). The protocol of the present
study was approved by the Institutional Review Board of E-DA
Hospital (EMRP-102-077).
Surgical procedure
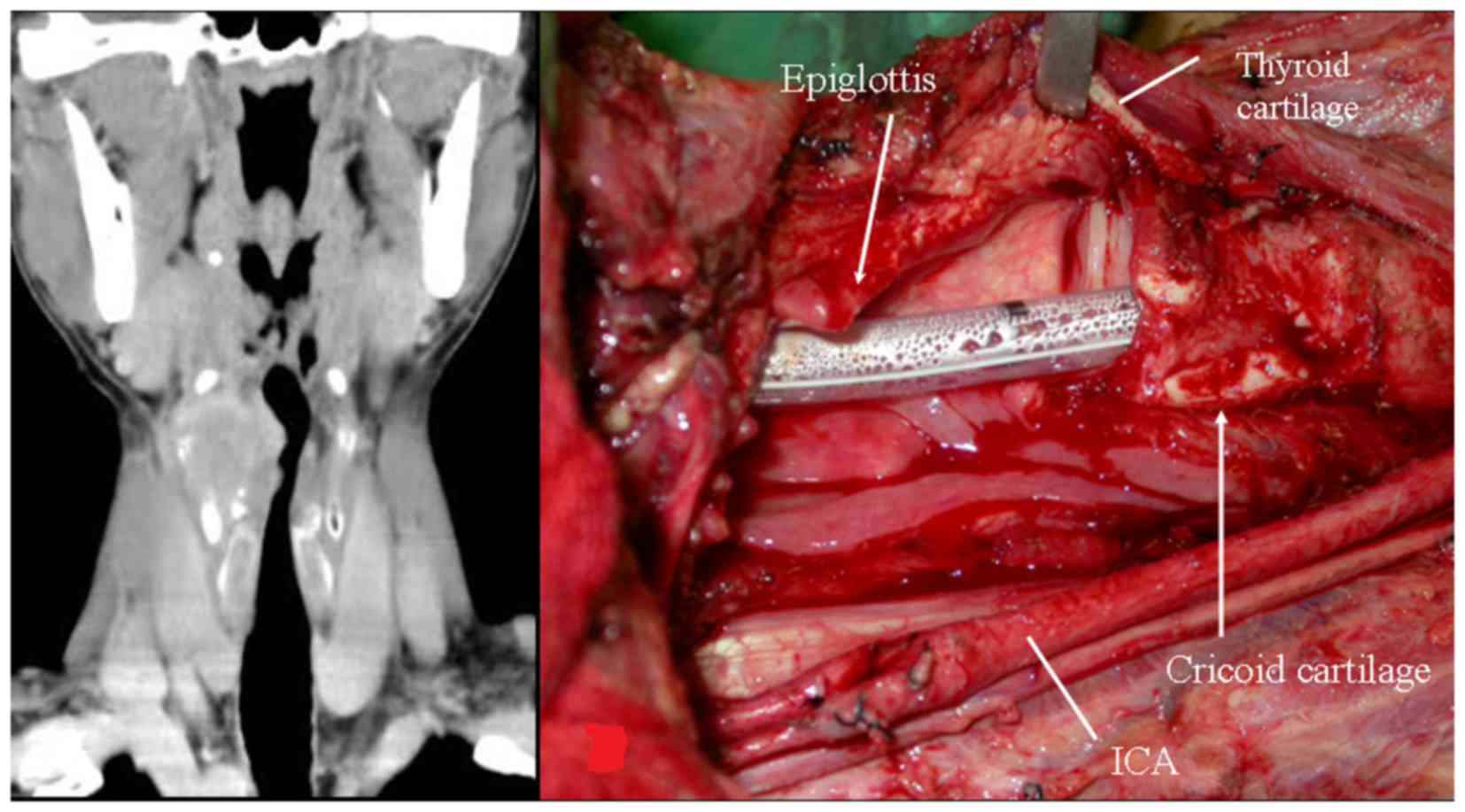
Surgical procedures were grouped into two types: i)
OPL with TFT and ii) TL with permanent tracheostomy, followed by
voice rehabilitation with an artificial larynx (pneumatic tube).
All patients received either adjuvant RT or CRT. OPL in the present
study included ESGL, SCHLP and VHLP. In the present study, ESGL was
used for HPC with involvement of the supraglottis, extralaryngeal
space and the thyroid cartilage. SCHLP was used for HPC with
involvement of the preepiglottic, paraglottic and extralaryngeal
spaces, thyroid cartilage and unilateral vocal fold paralysis. In
addition, VHLP was used for hemilarynx fixation or when invasion of
the apex of the pyriform sinus and the cricoid cartilage was
present. Uninvolved tissues were preserved to the fullest extent
during ESGL, SCHLP and VHLP in order to aid repair and retain
function. These tailored surgical techniques were developed in
order to preserve postoperative function and may result in
different postoperative functional outcomes. The major surgical
procedures in the OPL group consisted of: i) Either ESGL, SCHLP or
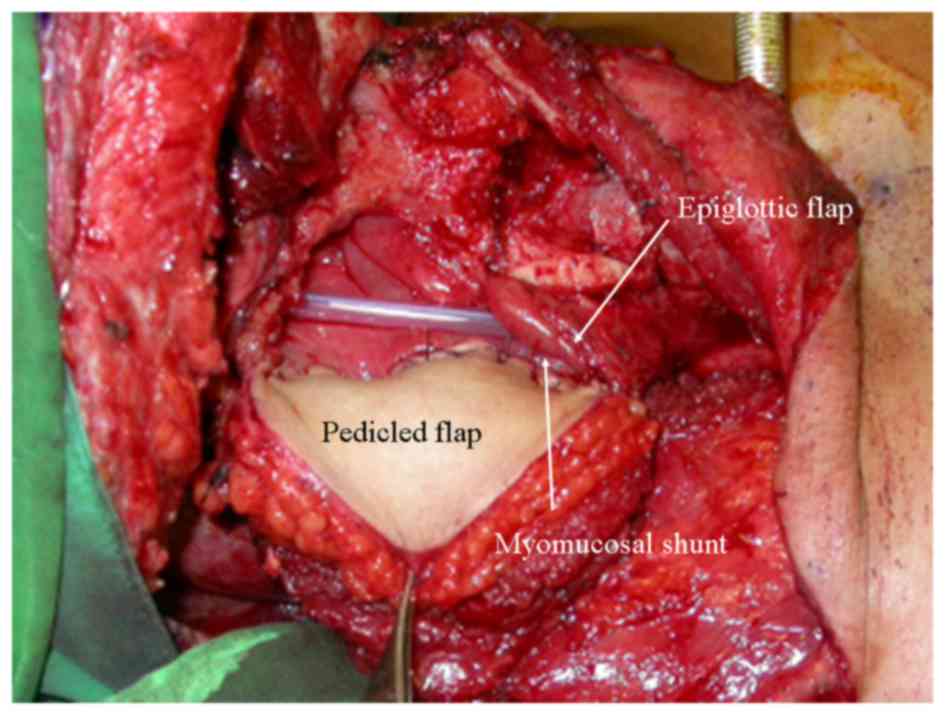
VHLP (Fig. 1), ii) reconstruction of
the epiglottis by suturing the residual epiglottis to the
preepiglottic tissue, tracheal mucosa or interarytenoid mucosa
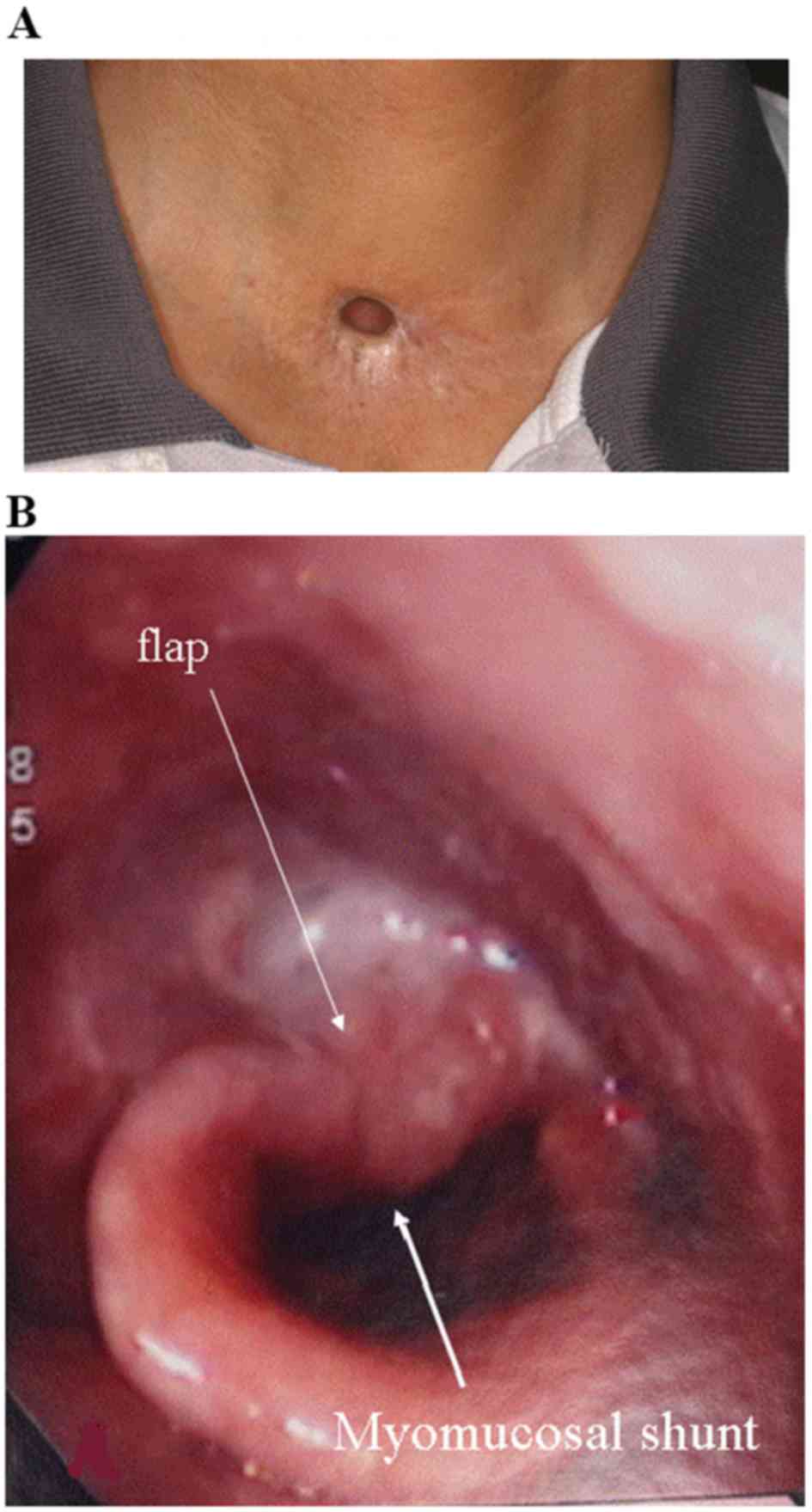
(Fig. 2); and iii) TFT (Fig. 3). A postoperative view of the flap and
the myomucosal shunt following tailored VHLP with resection
extending to a segment of the right cricoid cartilage is presented
in Fig. 3B. Lung-powered shunt speech
was produced by covering the tracheostoma with a finger.
Postoperative RT was administered to patients with
AJCC pathological stage N1-3 and T3-4 disease (27). Postoperative CRT was administered to
patients with extracapsular spread, involvement of the surgical
margins and N2-3 stage disease. Postoperative adjuvant RT (1.8–2.0
Gy/day, 5 days/week; 13–35 days/total) was administered to each
patient. The mean total dose was 60.1 Gy (range, 23.4–66.5 Gy).
Weekly cisplatin (20–40 mg/m2) and cisplatin (100
mg/m2) for 4 to 8 courses were administered as
postoperative chemotherapy.
Questionnaires and voice
evaluation
All participants provided written informed consent
and answered various questionnaires, which were evaluated >6
months after surgery. Dysphagia score (DS) was evaluated based on
symptoms during food deglutition (28). Performance Status Scale for Head and
Neck Cancer (PSSHN) was used to evaluate the understandability of
speech, the normalcy of diet and the ability to eat in public, and
was rated on a scale from 0 to 100, with 100 representing normal
function (29). The Voice Handicap
Index (VHI) was designed for all voice disorders (30). A VHI score of 0–30 represented a
minimal/mild voice impediment, 31–60 a moderate degree and 61–120 a
significant degree of impediment. The European Organization for the
Research and Treatment of Cancer Core Quality of Life Questionnaire
(EORTC QLQ-C30) is a widely used questionnaire for various types of
malignancies, including head and neck squamous cell carcinoma
(HNSCC) (31). The EORTC Head and
Neck Quality of Life Questionnaire (QLQ-H&N35) was a specific
questionnaire used for patients with HNSCC (32). The scores of the QLQ-C30 and of the
QLQ-H&N35 were transformed to a scale of 0–100, with higher
scores on the symptom or single item scales indicating poorer
functioning, and higher scores on the functioning and global
Quality of Life (QOL) scales indicating improved functioning.
Statistical analysis
Baseline characteristics between the two study
groups were compared with Pearson's χ2 test and
independent Student's t-test for categorical and continuous
variables, respectively. The survival curves were constructed using
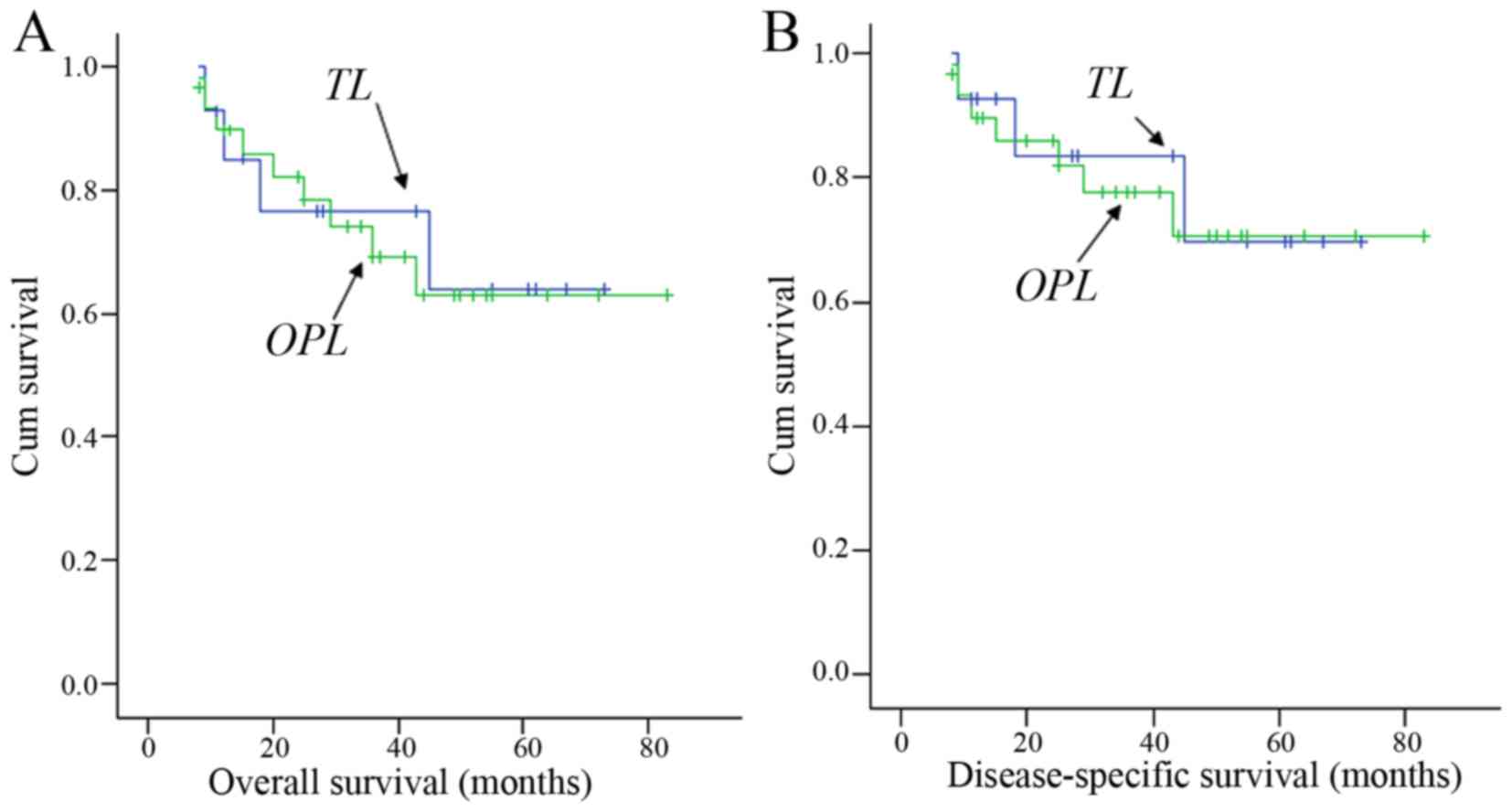
the Kaplan-Meier method. OS analysis was based on mortality from
any cause. For the calculation of disease-specific survival (DSS),
the patients were censored if the cause of mortality was not
directly associated with HPC. Mann-Whitney U test was used to
compare nonparametric variables. All statistical analyses were
performed using the Stata statistical software (version 12.1;
StataCorp LP, College Station, TX, USA).
Results
Associations between
clinicopathological characteristics and type of surgery and
survival rates
In the study groups, a majority of the patients were
pT4a (all cT4a) and stage IV. There was a significantly increased
number of patients with lymphovascular invasion observed in the OPL
group compared with the TL group (P=0.003). All the cases in the
two groups exhibited clinical invasion of the thyroid cartilage,
but there was a significantly higher number of cases with
simultaneous invasion of thyroid and cricoid cartilages in the TL
group compared with the OPL group (P=0.005; Table I). With a mean follow-up of 45 months
(range, 12–89 months), the 5-year OS was 65.8 and 72.6% in the OPL
and TL groups, respectively (P=0.533), while the 5-year DSS was
72.0 and 84.7% (P=0.330). The OS and DSS rates between groups were
not significantly different (Fig. 4).
The most common second primary cancer in this cohort was oral
cancer (4/44, 9.1%), followed by esophageal cancer (3/44, 6.8%),
renal cancer (2/44, 4.5%), liver cancer (1/44, 2.3%) and thyroid
cancer (1/44, 2.3%).
 | Table I.Baseline characteristics of patients
with hypopharyngeal cancer in OPL and TL treated groups. |
Table I.
Baseline characteristics of patients
with hypopharyngeal cancer in OPL and TL treated groups.
|
| Surgery (n=
44) |
|---|
|
|
|
|---|
|
Characteristics | OPL (n=27) | TL (n=17) | P-value |
|---|
| Age, years (mean ±
SD) | 54.9±11.1 | 54.6±11.4 | 0.945 |
| pT classification
(T3/T4a), n | 4/23 | 1/16 | 0.634 |
| pTNM stage
(III/IV), n | 2/25 | 1/16 | >0.99 |
| Thyroid and cricoid
cartilagea, n (%) | 6 (22.2) | 11 (64.7) | 0.005 |
| OPL
(ESGL/SCHLP/VHLP), n | 6/3/18 | – |
|
| Cricoidectomy, n
(%) | 18 (67) | – |
|
| Adjuvant RT/CRT,
n | 13/14 | 10/7 | 0.477 |
Complications and life quality between
groups treated with TL and OPL
The questionnaires (DS and QLQ H&N 35) were
completed in 19 cases in the OPL group and in 11 cases in the TL
group. In the OPL group, one patient had fed using percutaneous
gastrostomy prior to OPL due to ischemic bowel following operation,
so he could not be evaluated for DS and swallowing. In the TL
group, one patient could not be evaluated for DS due to
neopharyngeal stenosis, and thus had fed with percutaneous
gastrostomy. An additional two other patients could not be
evaluated for VHI, including one with stomal stenosis requiring
Teflon as a stent and the other with a stomal skin allergy to the
prosthesis. The complications (Table
II) and the results from DS and QLQ H&N 35 questionnaires
(Table III) were revealed to be
comparable between the two groups. However, results of VHI
(P=0.032), understandability of speech (P<0.001) and normalcy of
diet (P=0.041) from PSSHN, and senses (P=0.006), speech
(P<0.001), social contact (P=0.004) and smell (P=0.005) from QLQ
H&N 35 were all significantly improved in the OPL group
compared with the TL group (Table
III).
 | Table II.Oncologic and functional outcomes and
complications. |
Table II.
Oncologic and functional outcomes and
complications.
|
| Surgery |
|---|
|
|
|
|---|
| Outcomes | OPL | TL | P-value |
|---|
| Hospitalization,
days (mean ± SD) | 27±6 | 31±10 | 0.114 |
| Tumor recurrence, n
(%) |
|
|
|
|
Local/regional | 1/1 (3.7) | 0/0 | NA |
| Distant
metastasis | 6 (22.2) | 1 (5.9) | 0.220 |
| 5-year survival,
% |
|
|
|
| OS | 65.8 | 72.6 | 0.533 |
|
DSS | 72.0 | 84.7 | 0.330 |
| Prognosis, n |
|
|
|
| Alive
without hypopharyngeal cancer | 16 | 13 |
|
|
Succumbed to hypopharyngeal
cancer | 6 | 1 |
|
|
Succumbed to other causes | 2 | 3 |
|
| Removal of NG |
|
|
|
| Failure
to remove NG, n (%) | 3 (11.1) | 5 (29.4) | 0.227 |
| Time to
remove NG, days (mean ± SD) | 58±51 | 35±33 | 0.181 |
| Complications, n
(%) |
|
|
|
|
Pneumoniaa | 1 (3.7) | 0 (0.0) | >0.99 |
| Flap
failure | 1 (3.7) | 4 (23.5) | 0.065 |
| Stomal
stenosis | 4 (14.8) | 3 (17.6) | >0.99 |
|
Postoperative hemorrhage | 1 (3.7) | 2 (11.8) | 0.549 |
 | Table III.Comparison of quality of life between
OPL and TL. |
Table III.
Comparison of quality of life between
OPL and TL.
|
| Surgery |
|
|---|
|
|
|
|
|---|
| Questionnaires | OPL (n=19) | TL (n=11) | P-value |
|---|
| Dysphagia
score | 1.8±0.6 | 1.4±0.5 | 0.133 |
| VHI | 20.1±15.3 | 35.9±22.8 | 0.032 |
| PSSHN |
|
|
|
|
EIP | 80.3±21.4 | 68.2±35.5 | 0.475 |
|
UOS | 86.8±12.8 | 25.0±35.4 | <0.001 |
|
NOD | 76.8±27.9 | 57.3±26.1 | 0.041 |
| QLQ H&N 35
assessment |
|
|
|
|
Swallowing | 14.8±12.3 | 22.0±28.0 | 0.747 |
|
Senses | 15.8±18.8 | 39.4±20.2 | 0.006 |
|
Speech | 26.2±24.1 | 65.2±17.6 | <0.001 |
| Social
contact | 2.9±4.1 | 12.3±10.3 | 0.004 |
|
Smell | 21.0±25.4 | 57.5±33.8 | 0.005 |
Discussion
The results of the present study revealed that 23
(85%) of the 27 patients in the OPL group and 16 (94%) of the 17
patients in the TL group with clinical invasion of thyroid and/or
cricoid cartilage presented with pathologically confirmed cortical
bone invasion. HPC has a more complex anatomic structure (lesions
over the pyriform sinus and postcricoid mucosa frequently cannot be
readily investigated by mere visual inspection) and less specific
symptoms, which may cause delayed diagnoses and high rates of
thyroid and/or cicoid cartilage invasion when compared with LC
(15). These features also make
treatment strategies for HPC different from those for LC. This
accounts for why cricoidectomy is probably more frequently
performed for HPC compared with LC. Advanced HPC with extensive
invasion of the cartilage is difficult to treat with conventional
OPL (16–19), and therefore, either TL or CRT is
preferred. When TL and permanent tracheostomy are employed,
laryngeal function and sensory function may be severely compromised
(33). However, treatment with CRT
may result in high rates of local recurrence (9,10,12), feeding tube dependence (34) and salvage laryngectomy (2,11).
In the present study, the partial resection of the
cricoid cartilage was performed in 18 of 27 (67%) cases in the OPL
group. In severe cases with total unilateral cordectomy, a
tracheopharyngeal myomucosal shunt was created between the
contralateral normal cord and a flap by tailoring the flap to
precisely match the dimensions of the defect. To produce adequate
lung-powered shunt speech, a narrow myomucosal shunt was required.
However, oxygen supply was usually insufficient once a narrow
myomucosal shunt had been created, so an additional oxygen supply
provided by TFT or tracheostomy was necessary.
In the present study, TFT was performed by creating
a superiorly based U-shaped and an inferiorly based inverted
U-shaped flap on the anterior tracheal wall for the formation of a
mucocutaneous junction between the trachea and the skin surface,
which was a modification of the Bjork's tracheostomy flap (35). Several advantages of TFT compared with
a standard tracheostomy include no irritation to the surrounding
tissue by the device, no risk of tube dislodgement, no monthly
change of the tube, improved hygiene and speech without a tracheal
tube (23,36). Therefore, the narrow myomucosal shunt
was considered for better phonation, but the TFT was employed for
providing a sufficient oxygen supply and for increasing QOL. In a
number of patients with a sufficient oxygen supply, the
tracheostoma may be closed completely. Extended and tailored
radical surgery may impair many processes for swallowing, including
tongue base retraction, neoglottic closure and hyolaryngeal
anterior and vertical movement, which would easily result in
aspiration (37). An epiglottis was
constructed to prevent aspiration from the tracheopharyngeal
myomucosal shunt.
In E-DA Hospital, adjuvant chemotherapy is
administered at a lower dosage [weekly cisplatin (20–40
mg/m2) and cisplatin (100 mg/m2) for 4 to 8
courses] compared with that suggested by National Comprehensive
Cancer Network (NCCN) guidelines, as morbidities and/or mortalities
have been frequently encountered when following NCCN guidelines.
Attempts have been made to administer adjuvant RT to patients
according to NCCN guidelines, but due to complications and a lack
of compliance, a complete course of adjuvant RT was not achieved in
many patients. A positive margin was revealed in only one patient
(pT4aN1M0) in the OPL group. The patient experienced distant
metastasis 5 months following surgery and succumbed to mortality 4
months following distant metastasis. Adjuvant CRT was administered
to the patient prior to surgery due to the presence of the positive
extracapsular spread and a positive margin. In patients with a
positive surgical margin, adjuvant CRT rather than adjuvant RT, was
administered in E-DA Hospital, which is recommended by suggested by
NCCN guidelines.
Locoregional recurrence rate (3.7%) in the present
study was lower compared with those of the treatment results for
CRT (12.5–28.0%) for advanced LC and HPC with or without cartilage
invasion (6,7,9,12,13,34).
However, the rate of distant metastasis (22.2%) in the OPL group
was higher compared with that (5.9%) in the TL group and higher
compared with those treated with CRT for LC or HPC with cartilage
invasion in previously published studies (12,13), so
more frequent follow-up for lung metastasis is suggested for
patients receiving OPL, and aggressive treatment for lung
metastasis is also recommended. During the follow-up, 2 patients
with early lung metastasis were identified in the OPL group and
immediate lung wedge resection for metastatic lung nodules were
performed. These 2 patients were then followed up for 16 and 47
months following lung wedge resection and remain alive at present.
A total of 6 patients with distant metastasis were identified in
the OPL group. However, only 1 patient experienced local recurrence
6 months after surgery and distant metastasis occurred 3 months
after local recurrence. Locoregional control was improved by a
surgical treatment strategy with adjuvant RT/CRT. In addition,
regional recurrence was reduced by bilateral neck dissections in
patients with suspected neck metastasis.
At E-DA Hospital, the regular annual follow-up
images included chest x-rays, head and neck CT/magnetic resonance
imaging (MRI) with contrast, abdominal ultrasound, bone scans and
panendoscopy with NBI. If any abnormal finding was identified by
chest x-ray, abdominal ultrasound or bone scans, then an abdominal
CT, chest CT or bronchoscopy would be arranged. If recurrence or
distant metastasis cannot be distinguished by these methods,
positron emission tomography-CT would be arranged for further
confirmation. Regular follow-ups at the outpatient department would
be performed every 1–3 months in the first year, every 2–4 months
in the second year, every 4–6 months in the third to fifth year and
every 6–12 months after the fifth year. If recurrence or distant
metastasis was suspected, abdominal ultrasound, chest x-ray,
fiberscope, panendoscopy, abdominal CT, chest CT or head and neck
CT/MRI would be arranged to rule out the disease.
The 5-year OS was 65.8 and 72.6% in the OPL and TL
groups, respectively (P=0.533), while the 5-year DSS was 72.0 and
84.7% (P=0.330). The 5-year survival of the patients in the present
study was higher compared with those reported in the literature
(6,7,9,13,34). The
survival outcomes do not indicate that patients treated with OPL
have an improved prognosis compared with TL, or that patients
treated with TL have a better prognosis compared with CRT, as
patients with T4b stage disease and extensive cartilage invasion
often receive either TL or CRT as primary treatment. The high
survival rates in the OPL group were presumably due to the
following reasons: i) Relatively non-extensive invasion of the base
of the tongue and cartilage; ii) exclusion of patients with T4b and
inoperable diseases; iii) surgical treatment strategy with adjuvant
RT/CRT for raising local control; iv) treatment with bilateral neck
dissections for reducing regional recurrence; v) inclusion of
patients with early second primary tumor (1 case of early
esophageal cancer and 1 case of esophageal high grade dysplasia
with endoscopic submucosal dissection); vi) inclusion of patients
with early lung metastasis (2 patients received lung wedge
resection) and vii) shorter follow-up periods. Despite a low larynx
preservation rate in the present cohort of patients due to the
presence of tracheostoma, the treatment strategies with OPL and TFT
may still achieve high rates of local control, survival and
lung-powered shunt speech.
Of the 44 patients in the present study, only 1
patient presented with a positive margin in the OPL group. Distant
metastasis was identified 5 months following surgery and the
patient succumbed to HPC 9 months after surgery. It appears that
the presence of a positive surgical margin may result in poorer
survival rates. However, a cohort study with a large number of
cases will be required in order to confirm the results.
In the OPL group, 1 patient with esophageal cancer
(T1N0M0) received endoscopic submucosal dissection. In the TL
group, 1 patient with esophageal cancer (T2N1M0) received CCRT, and
the other patient with esophageal cancer (T1bN0M0) received an
esophagectomy. The patient in the OPL group experienced distant
metastasis 15 months following surgery and succumbed to HPC 16
months following surgery. In the TL group, 1 patient succumbed to
HPC 45 months following surgery, and the other patient succumbed to
mortality due to esophageal cancer-associated complications
(gastric invasion with massive bleeding and pneumonia). As only 3
patients with HPC with second esophageal cancer were identified in
the present cohort and only 1 of the 3 cases succumbed to
esophageal cancer-associated complications, it was difficult to
derive the survival impact from the 3 cases.
Removal of the NG tube failed in 3 (3/17; 11.1%)
patients in the OPL group and 5 (5/17; 29.4%) patients in the TL
group. In the OPL group, failure to remove the NG tube was
presumably the result of esophageal cancer (T1N0M0) post-endoscopic
submucosal dissection in 1 patient, old age (72 years) with partial
resection of the base of the tongue and cricoid cartilage in 1
patient, and oncological failure (weakness following surgery and
adjuvant CRT, distant metastasis 5 months after surgery and
succumbed to mortality 4 months after distant metastasis) in 1
patient. In the TL group, failure to remove the NG tube was
presumably caused by a failure in the reconstruction of pharyngeal
defects (including 2 cases of upper esophageal defects) in 4
patients (2 cases with anterolateral thigh flap tubing, 1 case with
radical ablative surgery and radial forearm free flap, 1 case with
jejunal flap; followed by salvage deltopectoral flap or pectoralis
major myocutaneous flap) and esophageal high grade dysplasia (over
middle third of the esophagus) post-endoscopic submucosal
dissection in 1 patient. Esophageal diseases, including HPC with
upper esophageal involvement or esophageal tumor, were identified
in 1 of the 3 patients in the OPL group and in 3 of 5 patients in
the TL group, in whom the removal of the NG tube failed, indicating
an association of esophageal diseases with a failure to remove the
NG tubes. The DS was 1.8 and 1.4 in the OPL and TL groups,
respectively (P=0.133). This indicated that coughing rarely
occurred during liquid food deglutition in the two groups.
Generally, following the healing of the primary
(pharyngolaryngeal) and cervical wounds and the completion of
adjuvant therapy, swallowing evaluation and rehabilitation would be
arranged to assess the postoperative swallowing function and to
assist with improving oral intake (using methods including position
change and food selection). Azevedo et al (38) reported that the mean total scores of
VHI following the treatment of advanced SCC of the larynx and
hypopharynx were 24.0, 28.2 and 34.2 in patients who underwent PL,
TL and total pharyngolaryngectomy, respectively. In addition, in
another previous study where VHI was assessed in patients treated
with CRT for advanced HPC, a majority of patients were observed to
reveal mild or mild to moderate problems with speech rehabilitation
(39).
In the present study, the mean VHI score for
patients treated with OPL was 20.1, which was improved when
compared with that obtained from the patients treated with TL (and
not worse when compared with those treated with CRT) (39). According to the PSSHN results,
patients who underwent OPL obtained higher mean scores compared
with those who underwent TL for the categories, the
understandability of speech (86.8 vs. 25.0; P<0.001) and
normalcy of diet (76.8 vs. 57.3; P=0.041). This is consistent with
previously published results (29).
In the present study, patients treated with TL had increased
sensory problems (P=0.006) and greater impairment with speech
(P<0.001) compared with those treated with OPL, which was also
consistent with previously published data (40). On the contrary, from a systemic review
assessing the functional outcomes following pharyngolaryngectomy,
successful speech outcomes are more likely to be achieved with
surgical (namely, tracheoesophageal voice prosthesis) procedures
compared with non-surgical techniques (41). The tracheoesophageal voice prosthesis
is a good option, however there are a number of disadvantages,
including the requirement for frequent replacements for a new
tracheoesophageal voice prosthesis by surgical intervention under
general anesthesia and complications, including wound infection,
valve incompetence, formation of granulation tissue, aspiration of
the prosthesis into airway and aspiration pneumonia (42,43).
Speech rehabilitation with tracheoesophageal voice
prosthesis was not widely accepted in Taiwan in previous decades.
Despite unsatisfactory intelligibility and speech quality, speech
rehabilitation with an artificial larynx (pneumatic tube) was still
more commonly used compared with tracheoesophageal voice prosthesis
(44). In the present study, better
social contact was also identified in the OPL group (P=0.004),
which is consistent with previously published findings by Lee et
al (40). Compared with the
results on the subscales of swallowing, senses (smell, taste) and
speech (with mean scores of 34, 34 and 31, respectively) as
reported by Keereweer et alw39) in a study on the treatment
of patients with CRT for advanced HPC, a markedly improved QOL with
regards to swallowing and senses and a similar improvement in
speech were identified in patients in the OPL group of the present
study. Furthermore, an improved QOL with regards to swallowing was
observed for patients receiving OPL and TL. The swallowing
dysfunction may be attributed to the post-radiation
pharyngolaryngeal edema, decreased tongue movement, decreased
laryngeal elevation and epiglottic inversion. A number of surgical
treatment modalities have been successfully applied to LC, but a
limited number of procedures have been reported for advanced HPC
with cartilage invasion. With regards to the modification of
surgical interventions for preservation of more normal mucosa,
tissue and cartilage (tailor made for each patient) for further
repair, a combination of OPL and TFT may be an alternative
procedure that can be successfully applied to treat selected cases
of HPC with non-extensive cartilage invasion, which offers
favorable functional outcomes and QOL without compromising
survival. From clinical experiences, it was revealed that to
survive and return to a normal life, numerous patients require
pulmonary-driven speech and numerous patients require a working
sense of smell and taste. The ability to detect gas leaks and toxic
chemicals, and to differentiate fresh from spoiled food is also
required by the majority of patients. To fulfill these
requirements, OPL with TFT is a feasible treatment modality for the
treatment of patients with HPC with non-extensive invasion of the
thyroid and/or cricoid cartilage.
In the present study, patients in the TL group have
a more severe invasion of thyroid and cricoid cartilages compared
with those in the OPL group, thus it is not reasonable to compare
the survival outcomes between the two treatment modalities.
However, the result may reflect that the acceptable oncologic
outcome is achievable by treatment with OPL and TFT. Furthermore,
despite of the difference in patient selection, the comparative
results may partially reflect that markedly improved functional
outcomes of speech and senses of smell and taste may be achieved by
treatment with OPL and TFT.
The QLQ H&N 35 questionnaires were completed by
30 of the 32 (93.8%) living patients in the present study. Due to
the retrospective nature of the present study, 12 of the 44 (27.3%)
patients had succumbed to mortality prior to completion of the
study. Overall, response rates to the QLQ H&N 35 questionnaires
were 19 out of 27 (70.4%) cases in the OPL group and 11 out of 17
(64.7%) cases in the TL group. Although the compliance rates were
high, the response rates of the questionnaires were not.
There were a number of limitations to the present
study, including differences in patient selection between TL and
OPL groups, where patients in the TL group presented with a more
severe invasion of thyroid and cricoid cartilages. Additionally,
the response rates of the QLQ H&N 35 questionnaires were low,
which makes it prone to selection bias and overoptimistic results.
The study also involved a small number of cases and it was a
non-randomized study. Furthermore, there was a lack of
pre-treatment QOL scores. The follow-up periods were also
relatively short, where the shortest follow-up was 12 months.
Therefore a longer follow up period would provide a more accurate
assessment of survival time, complications and QOL.
In conclusion, the main advantage of OPL with TFT
includes good postoperative oncologic and functional outcomes, and
QOL on the subscales of swallowing, speech, senses (smell) and
social contact. Therefore, OPL with TFT is a feasible option to
treat selected HPC cases with non-extensive invasion of the thyroid
and/or cricoid cartilage.
Acknowledgements
The authors would like to thank Dr Shyh-An Yeh
(Department of Radiation Oncology, E-DA Hospital/I-Shou University)
for providing detailed data on adjuvant radiotherapy.
Funding
The present study was supported by the E-DA Hospital
of I-Shou University (grant no. EDAHP103009).
Availability of data and materials
The datasets used and analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
CFL and TZH conceived the study, analyzed the data,
drafted the manuscript and revised the intellectual content. CCW
performed data acquisition and interpretation, and drafted the
manuscript. HHW performed data analysis and interpretation, and
revised the manuscript for intellectual content. CFL designed and
interpreted the data, and drafted the manuscript. BSL performed
data interpretation and revised the manuscript. CYL performed data
acquisition and interpretation, and drafted the manuscript. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
All patients provided written informed consent. The
protocol of the present study was approved by the Institutional
Review Board of E-DA Hospital (EMRP-102-077).
Patient consent for publication
In the present study, no identifiable information
was contained. The patient granted permission to publish
unidentifiable images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lefebvre JL, Chevalier D, Luboinski B,
Kirkpatrick A, Collette L and Sahmoud T: Larynx preservation in
pyriform sinus cancer: Preliminary results of a european
organizationfor research and treatment of cancer phase iii trial.
EORTC head and neck cancer cooperative group. J Natl Cancer Inst.
88:890–899. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wolf GT, Fisher SG, Hong WK, Hillman R,
Spaulding M, Laramore GE, Endicott JW, McClatchey K and Henderson
WG; The Department of Veterans Affairs Laryngeal Cancer Study
Group, : Induction chemotherapy plus radiation compared with
surgery plus radiation in patients with advanced laryngeal cancer.
N Engl J Med. 324:1685–1690. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Forastiere AA, Goepfert H, Maor M, Pajak
TF, Weber R, Morrison W, Glisson B, Trotti A, Ridge JA, Chao C, et
al: Concurrent chemotherapy and radiotherapy for organ preservation
in advanced laryngeal cancer. N Engl J Med. 349:2091–2098. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Beauvillain C, Mahé M, Bourdin S, Peuvrel
P, Bergerot P, Rivière A, Vignoud J, Deraucourt D and Wesoluch M:
Final results of a randomized trial comparing chemotherapy plus
radiotherapy with chemotherapy plus surgery plus radiotherapy in
locally advanced resectable hypopharyngeal carcinomas.
Laryngoscope. 107:648–653. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tsou YA, Lin MH, Hua CH, Tseng HC, Chen
SW, Yang SN, Liang JA and Tsai MH: Survival outcome by early
chemoradiation therapy salvage or early surgical salvage for the
treatment of hypopharyngeal cancer. Otolaryngol Head Neck Surg.
137:711–716. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Krstevska V, Stojkovski I and Lukarski D:
Concurrent radiochemotherapy in advanced hypopharyngeal cancer.
Radiat Oncol. 5:392010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Prades JM, Schmitt TM, Timoshenko AP,
Simon PG, de Cornulier J, Durand M, Guillot A and Martin C:
Concomitant chemoradiotherapy in pyriform sinus carcinoma. Arch
Otolaryngol Head Neck Surg. 128:384–388. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ganly I, Patel S, Matsuo J, Singh B, Kraus
D, Boyle J, Wong R, Lee N, Pfister DG, Shaha A and Shah J:
Postoperative complications of salvage total laryngectomy. Cancer.
103:2073–2081. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Patel UA and Howell LK: Local response to
chemoradiation in T4 larynx cancer with cartilage invasion.
Laryngoscope. 121:106–110. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Francis E, Matar N, Khoueir N, Nassif C,
Farah C and Haddad A: T4a laryngeal cancer survival: Retrospective
institutional analysis and systematic review. Laryngoscope.
124:1618–1623. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lefebvre JL and Ang KK; Larynx
Preservation Consensus Panel, : Larynx preservation clinical trial
design: Key issues and recommendations-a consensus panel summary.
Int J Radiat Oncol Biol Phys. 73:1293–1303. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wagner MM, Curé JK, Caudell JJ, Spencer
SA, Nabell LM, Carroll WR and Bonner JA: Prognostic significance of
thyroid or cricoid cartilage invasion in laryngeal or
hypopharyngeal cancer treated with organ preserving strategies.
Radiat Oncol. 7:2192012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Worden FP, Moyer J, Lee JS, Taylor JM,
Urba SG, Eisbruch A, Teknos TN, Chepeha DB, Prince ME, Hogikyan N,
et al: Chemoselection as a strategy for organ preservation in
patients with T4 laryngeal squamous cell carcinoma with cartilage
invasion. Laryngoscope. 119:1510–1517. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Joshi P, Nair S, Chaturvedi P, Nair D,
Shivakumar T and D'Cruz AK: Thyroid gland involvement in carcinoma
of the hypopharynx. J Laryngol Otol. 128:64–67. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Guizard AN, Dejardin OJ, Launay LC, Bara
S, Lapôtre-Ledoux BM and Ligier KA: Diagnosis and management of
head and neck cancers in a high incidence area in France: A
population-based study. Medicine (Baltimore). 96:e72852017.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Urken ML, Blackwell K and Biller HF:
Reconstruction of the laryngopharynx after hemicricoid/hemithyroid
cartilage resection. Preliminary functional results. Arch
Otolaryngol Head Neck Surg. 123:1213–1222. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kim MS, Joo YH, Cho KJ, Park JO and Sun
DI: A classification system for the reconstruction of vertical
hemipharyngolaryngectomy for hypopharyngeal squamous cell
carcinoma. Arch Otolaryngol Head Neck Surg. 137:88–94. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hamoir M, Fievez J, Schmitz S, Velasco D
and Lengele B: Extended voice-sparing surgery in selected pyriform
sinus carcinoma: Techniques and outcomes. Head Neck. 35:1482–1489.
2013.PubMed/NCBI
|
|
19
|
Laccourreye O, Ishoo E, de Mones E, Garcia
D, Kania R and Hans S: Supracricoid hemilaryngopharyngectomy in
patients with invasive squamous cell carcinoma of the pyriform
sinus. Part I: Technique, complications, and long-term functional
outcome. Ann Otol Rhinol Laryngol. 114:25–34. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Balatoni Z and Elö J: Indication and
surgical technique for extended hemilaryngectomy. Eur Arch
Otorhinolaryngol. 256:400–402. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hamoir M, Lengelé B, Rombaux P, El-Din AB
and El Fouly P: Stretched radial forearm flap for reconstruction of
the laryngopharynx: An alternative conservation procedure for
radiation-failure carcinoma of the pyriform sinus. Laryngoscope.
109:1339–1343. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Shenoy AM, Sridharan S, Srihariprasad AV,
Reddy BK, Anand VT and Premalatha BS: Nanjundappa: Near-total
laryngectomy in advanced cancers of the larynx and pyriform sinus:
A comparative study of morbidity and functional and oncological
outcomes. Ann Otol Rhinol Laryngol. 111:50–56. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Eliachar I: Unaided speech in long-term
tube-free tracheostomy. Laryngoscope. 110:749–760. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Miller FR, Eliachar I and Tucker HM:
Technique, management, and complications of the long-term flap
tracheostomy. Laryngoscope. 105:543–547. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sahni R, Blakley B and Maisel RH: Flap
tracheostomy in sleep apnea patients. Laryngoscope. 95:221–223.
1985.PubMed/NCBI
|
|
26
|
Eliachar I, Zohar S, Golz A, Joachims HZ
and Goldsher M: Permanent tracheostomy. Head Neck Surg. 7:99–103.
1984. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Greene FL, Page DL, Fleming ID, Fritz AG,
Balch CM, Haller DG and Morrow M: AJCC Cancer Staging Manual. 6th.
American Joint Committee on Cancer; Chicago, IL: 2002, View Article : Google Scholar
|
|
28
|
Bergamini G, Alicandri-Ciufelli M, Molteni
G, De Siati DR, Luppi MP, Marchioni D and Presutti L:
Rehabilitation of swallowing with polydimethylsiloxane injections
in patients who underwentpartial laryngectomy. Head Neck.
31:1022–1030. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
List MA, Ritter Sterr C and Lansky SB: A
performance status scale for head and neck cancer patients. Cancer.
66:564–569. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Jacobson BH, Johnson A, Grywalski C,
Silbergleit A, Jacobson G, Benninger MS and Newman CW: The voice
handicap index (VHI): Development and validation. Am J Speech
Lang-Pathol. 6:66–70. 1997. View Article : Google Scholar
|
|
31
|
Bjordal K and Kaasa S: Psychometric
validation of the EORTC core quality of life questionnaire, 30-item
version and a diagnosis-specific module for head and neck cancer
patients. Acta Oncol. 31:311–321. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Bjordal K, Hammerlid E, Ahlner-Elmqvist M,
de Graeff A, Boysen M, Evensen JF, Biörklund A, de Leeuw JR, Fayers
PM, Jannert M, et al: Quality of life in head and neck cancer
patients: Validation of the european organization for research and
treatment of cancer quality of life questionnaire-H&N35. J Clin
Oncol. 17:1008–1019. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
van Dam FS, Hilgers FJ, Emsbroek G, Touw
FI, van As CJ and de Jong N: Deterioration of olfaction and
gustation as a consequence of total laryngectomy. Laryngoscope.
109:1150–1155. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Lee NY, O'Meara W, Chan K, Della-Bianca C,
Mechalakos JG, Zhung J, Wolden SL, Narayana A, Kraus D, Shah JP and
Pfister DG: Concurrent chemotherapy and intensity-modulated
radiotherapy for locoregionally advanced laryngeal and
hypopharyngeal cancers. Int J Radiat Oncol Biol Phys. 69:459–468.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kinley CE: A technique of tracheostomy.
Can Med Assoc J. 92:79–81. 1965.PubMed/NCBI
|
|
36
|
Akst LM and Eliachar I: Long-term,
tube-free (permanent) tracheostomy in morbidly obese patients.
Laryngoscope. 114:1511–1512. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Pauloski BR: Rehabilitation of dysphagia
following head and neck cancer. Phys Med Rehabil Clin N Am.
19:889–928. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Azevedo EH, Montoni N, Goncalves Filho J,
Kowalski LP and Carrara-de Angelis E: Vocal handicap and quality of
life after treatment of advanced squamous carcinoma of the larynx
and/or hypopharynx. J Voice. 26:e63–e71. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Keereweer S, Kerrebijn JDF, Al-Mamgani A,
Sewnaik A, de Jong RJ and van Meerten E: Chemoradiation for
advanced hypopharyngeal carcinoma: A retrospective study on
efficacy, morbidity and quality of life. Eur Arch Otorhinolaryngol.
269:939–946. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Lee TL, Wang LW, Mu-Hsin Chang P and Chu
PY: Quality of life for patients with hypopharyngeal cancer after
different therapeutic modalities. Head Neck. 35:280–285. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Mahalingam S, Srinivasan R and Spielmann
P: Quality-of-life and functional outcomes following
pharyngolaryngectomy: A systematic review of literature. Clin
Otolaryngol. 41:25–43. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Bozec A, Poissonnet G, Chamorey E, Demard
F, Santini J, Peyrade F, Ortholan C, Benezery K, Thariat J, Sudaka
A, et al: Results of vocal rehabilitation using tracheoesophageal
voice prosthesis after total laryngectomy and their predictive
factors. Eur Arch Otorhinolaryngol. 267:751–758. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Gitomer SA, Hutcheson KA, Christianson BL,
Samuelson MB, Barringer DA, Roberts DB, Hessel AC, Weber RS, Lewin
JS and Zafereo ME: Influence of timing, radiation, and
reconstruction on complications and speech outcomes with
tracheoesophageal puncture. Head Neck. 38:1765–1771. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Tsai TL, Chang SY, Guo YC and Chu PY:
Voice rehabilitation in laryngectomees: Comparison of daily-life
performance of 4 types of alaryngeal speech. J Chin Med Assoc.
66:360–363. 2003.PubMed/NCBI
|