Introduction
Lung cancer is one of the most common malignant
tumors and is the leading cause of cancer-related deaths. In 2012,
lung cancer accounts for approximately 12.9% of all cancers
(1). The most common type of lung
cancer is non-small cell lung cancer (NSCLC). NSCLC accounts for
85–90% of lung cancer. NSCLC is mainly divided into adenocarcinoma
and squamous cell carcinoma subtypes, which are derived from
bronchial mucosa epithelium (2). At
present, surgical treatment is the most effective and important
method for early NSCLC (3). Although
the use of minimally invasive surgery in clinical practice has
increased in recent years, thoracotomy is still the most common
method of lobectomy (4). Studies
have shown that video-assisted thoracoscopic surgery (VATS) brings
more benefits to patients with early NSCLC compared with
conventional thoracotomy, including reduced hospital stay, relief
of recent postoperative pain, and less postoperative complications
(5). VATS lobectomy consists of
several incisions or ports, usually 3–4. With the development of
laparoscopic instrument technology, VATS is gradually reduced from
multiple incisions to double incision, namely single utility port
thoracoscopic surgery (6). Since
2010, single utility port VATS lobectomy has become a new area of
minimally invasive surgery (7).
Single utility port VATS is a less invasive surgical procedure.
With single utility port VATS, thoracic surgery can be performed
through a small incision of approximately 4 cm in diameter. This
technique has been increasingly accepted because of its remarkable
clinical effect (8). Compared with
conventional VATS, single utility port VATS not only have the
advantage of reducing surgical trauma, but also reduces
postoperative pain and prompts recovery (9). Clinical efficacy of single utility port
VATS has been extensively studied, but studies on the
post-operative stress response and the impact on quality of life
(physical, functional and social) in 3 months after surgery are
rare. In this study, single utility port VATS and three-port VATS
were performed in patients with NSCLC to compare the clinical
efficacy. Postoperative stress response and quality of life were
also compared.
Patients and methods
General information
One hundred and fifty-six patients with NSCLC who
underwent VATS in Taizhou Hospital of Zhejiang Province (Taizhou,
China) from July 2015 to January 2017 were selected as subjects.
Patients were randomly divided into group A (n=74) and group B
(n=82). Group A was treated with single utility port VATS and group
B was treated with three-port VATS. There were 43 males and 31
females in group A, aged 45–73 years, with a mean age of 62.67±9.16
years; tumor diameter was 1.4–4.8 cm, with mean diameter of
2.81±1.16 cm; TNM staging: 59 cases in stage I, 15 cases in stage
II; pathological types: 59 cases of adenocarcinoma, 10 cases of
squamous cell carcinoma, 5 cases of adenosquamous carcinoma. There
were 59 males and 23 females in group B, aged 41–72 years, with a
mean age of 61.83±8.26 years; tumor diameter was 1.3–4.5 cm, with a
mean diameter of 2.86±1.35 cm; TNM staging: 64 cases in stage I, 18
cases in stage II; pathological types: 61 cases of adenocarcinoma,
14 cases of squamous cell carcinoma, 7 cases of adenosquamous
carcinoma.
Inclusion and exclusion criteria
Inclusion criteria: Preoperative pathological
examination confirmed NSCLC (10);
No distant metastases under examination of CT, color Doppler
ultrasound, MRI and other imaging examinations, TNM stage was stage
I–II; no previous history of chemotherapy and radiation therapy;
first diagnosis; aged 18–75 years; Eastern Cancer Cooperative Group
(ECOG) (11) physical status was
0–1, expected survival time ≥12 months; no major organ
dysfunction.
Exclusion criteria: History of previous
thoracoscopic surgery; extensive pleural adhesions; difficulty in
maintaining single-lung ventilation during surgery; combined with
other tumors, severe liver and kidney dysfunction, connective
tissue disease, endocrine and metabolic diseases, hematopoietic
dysfunction, infectious diseases; mental illness or family history
of mental illness.
This study was approved by The Ethics Committee of
Taizhou Hospital of Zhejiang Province. Patients who participated in
this research had complete clinical data. The signed informed
consents were obtained from the patients or the guardians.
Treatment
Compound anesthesia was performed. After intubation
of the double lumen tube, single lung ventilation was performed
into the pleural cavity. Lateral position (90°) on the healthy side
was used. After disinfection, observation hole was made in the 7th
intercostal space of the midline of the iliac crest. A 2 cm
incision was made and thoracoscope was placed. For single utility
port VATS, an incision (4 cm) was made between the 4th and 5th ribs
of the iliac crest. For three-port VATS, 2 cm incision (main
operation hole) was made in the fifth intercostal space of the
iliac crest, and another 2 cm incision (sub-operation hole) was
made in the 7th intercostal space of the anterior subscapular line.
Mediastinal pleura was opened, and the lower ligament of the lower
lung was dissected. According to the condition of the resected lung
lobe, the venous, arterial, and bronchial organs were dissected by
a single-type lobectomy method. The (articular head) intra-cavity
linear cutting and closing device was used to close the detachment.
Lobes were removed, and mediastinal lymph nodes were also removed.
After that, the chest cavity was flushed, the blood was stopped,
the drainage tube was placed, and the chest was closed layer by
layer.
Observation indicators
i) Perioperative indicators such as operation time,
intraoperative blood loss, postoperative drainage, removal of
drainage tube, lymph node dissection, hospitalization time and
postoperative complications were observed.
ii) The degree of pain was assessed by visual analog
scale (VAS) (12) from 1 to 7 days
postoperatively (T1-T7). VAS score of 0 indicated no pain, and VAS
score of 10 indicated the most severe pain. The higher the VAS
score, the more severe the pain.
iii) Venous blood was taken from the study subjects
before and 1–7 days after surgery (T1-T7) under fasting conditions.
Blood was centrifuged at 670.8 × g at 20–25°C for 10 min to
separate serum. Expression of CRP and IL-6 in serum was detected by
enzyme-linked immunosorbent assay (ELISA) (13). Human CRP and IL-6 ELISA kits (Thermo
Fisher Scientific Co., Ltd., Shanghai, China) were used. All
operations were performed in strict accordance with manufacturer's
instructions. No reagent was added into the blank control well.
After adding samples, the plate was covered with film and incubated
at 37°C for 1 h. After that, the plate was washed and 80 µl
affinity chain enzyme was added into each well, followed by
incubation at 37°C for 30 min. After that, substrate A and B (50
µl) was added, followed by incubation at 37°C for 10 min. Then each
well was added with 50 µl stop solution. OD value of each well was
measured at 450 nm by using a fully automated enzyme label analyzer
(Miguel Molecular Instruments Co., Ltd., Shanghai, China), and the
expression levels of CRP and IL-6 were calculated.
iv) Functional assessment of cancer treatment - The
lung cancer questionnaire (FACT-L) (14) was used to assess the quality of life
of patients before and 3 months after surgery. FACT-L contains 27
items, including body, function, situation and social fields. Each
item has a 5-level scale (0–4 points, 0 = no, 4 = very much).
Statistical analysis
Statistical analysis was performed using SPSS 19.0
(IBM Corp, Armonk, NY, USA). Measurement data were expressed as
mean ± standard deviation, and the inter-group comparisons of
measurement data in accordance with the normal distribution were
compared by t-test. Comparison with a group before and after
treatment was performed by paired t-test. Count data were expressed
as number of cases/percentage [n (%)]. Chi-square test was used to
compare count data between groups. ANOVA was used for comparison
between multiple groups and the post hoc test was LSD test.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Baseline data of groups A and B
Groups A and B showed no significant difference in
sex, age, body mass index (BMI), smoking and drinking history,
lesion location, tumor diameter, TNM stage, pathological type,
pathological differentiation, alanine aminotransferase (ALT),
aspartate aminotransferase (AST) and blood sugar (Glu) (P<0.05)
(Table I).
 | Table I.Baseline data of groups A and B [n
(%)]/(mean ± SD). |
Table I.
Baseline data of groups A and B [n
(%)]/(mean ± SD).
| Items | Group A (n=74) | Group B (n=82) | t/χ2
value | P-value |
|---|
| Sex |
|
| 3.293 | 0.070 |
| Male | 43 (58.11) | 59 (71.95) |
|
|
|
Female | 31 (41.89) | 23 (28.05) |
|
|
| Age | 62.67±9.16 | 61.83±8.26 | 0.602 | 0.548 |
| BMI
(kg/m2) | 20.47±3.18 | 20.04±3.07 | 0.859 | 0.392 |
| History of
smoking |
|
| 2.212 | 0.137 |
| Yes | 30 (40.54) | 43 (52.44) |
|
|
| No | 44 (59.46) | 39 (47.56) |
|
|
| Drinking history |
|
| 0.562 | 0.454 |
| Yes | 22 (29.73) | 29 (35.37) |
|
|
| No | 52 (70.27) | 53 (64.63) |
|
|
| Lesion |
|
| 0.054 | 0.816 |
| Upper
left lobe | 16 (21.62) | 20 (24.39) |
|
|
| Left
lower lobe | 8
(10.81) | 9 (10.98) |
|
|
| Right
upper lobe | 17 (22.97) | 17 (20.73) |
|
|
| Right
middle lobe | 10 (13.51) | 10 (12.20) |
|
|
| Right
lower lobe | 23 (31.08) | 26 (31.71) |
|
|
| Tumor diameter
(cm) | 2.81±1.16 | 2.86±1.35 | 0.247 | 0.805 |
| TNM staging |
|
| 0.066 | 0.797 |
| Phase
I | 59 (79.73) | 64 (78.05) |
|
|
| Phase
II | 15 (20.27) | 18 (21.95) |
|
|
| Pathological
type |
|
| 0.537 | 0.464 |
|
Adenocarcinoma | 59 (79.73) | 61 (74.39) |
|
|
| Squamous
cell carcinoma | 10 (13.51) | 14 (17.07) |
|
|
|
Adenosquamous carcinoma | 5 (6.76) | 7 (8.54) |
|
|
| Degree of
pathological differentiation |
|
| 0.105 | 0.746 |
| Highly
differentiated | 17 (22.97) | 22 (26.83) |
|
|
| Medium
differentiation | 47 (63.51) | 43 (52.44) |
|
|
| Low
differentiation | 10 (13.51) | 17 (20.73) |
|
|
| ALT (U/l) | 27.47±5.18 | 26.91±6.33 | 0.600 | 0.549 |
| AST (U/l) | 17.18±4.27 | 17.69±4.82 | 0.696 | 0.487 |
| Glu (mmol/l |
5.97±0.38 | 6.06±0.47 | 1.306 | 0.193 |
Comparison of perioperative indicators
between groups A and B
There was no significant difference between the
groups in operation time, postoperative drainage volume, drainage
tube removal time and lymph node dissection (P>0.05). The blood
loss and hospitalization time in group A were significantly lower
than those in group B (P<0.001) (Table II).
 | Table II.Comparison of perioperative
indicators between groups A and B (mean ± SD). |
Table II.
Comparison of perioperative
indicators between groups A and B (mean ± SD).
| Items | Group A (n=74) | Group B (n=82) | t value | P-value |
|---|
| Operation time
(min) | 142.63±52.73 | 153.66±51.84 | 1.316 | 0.190 |
| Intraoperative
blood loss (ml) | 136.47±42.71 | 173.41±49.27 | 4.978 | <0.001 |
| Postoperative
drainage (ml) | 681.21±44.85 | 692.54±38.41 | 1.699 | 0.091 |
| Drainage tube
removal time (days) |
4.28±0.93 |
4.51±1.12 | 1.387 | 0.168 |
| Number of lymph
node dissections (a) | 14.17±4.18 | 13.87±4.41 | 0.435 | 0.664 |
| Hospital stay
(days) |
9.31±1.82 | 11.34±1.32 | 8.029 | <0.001 |
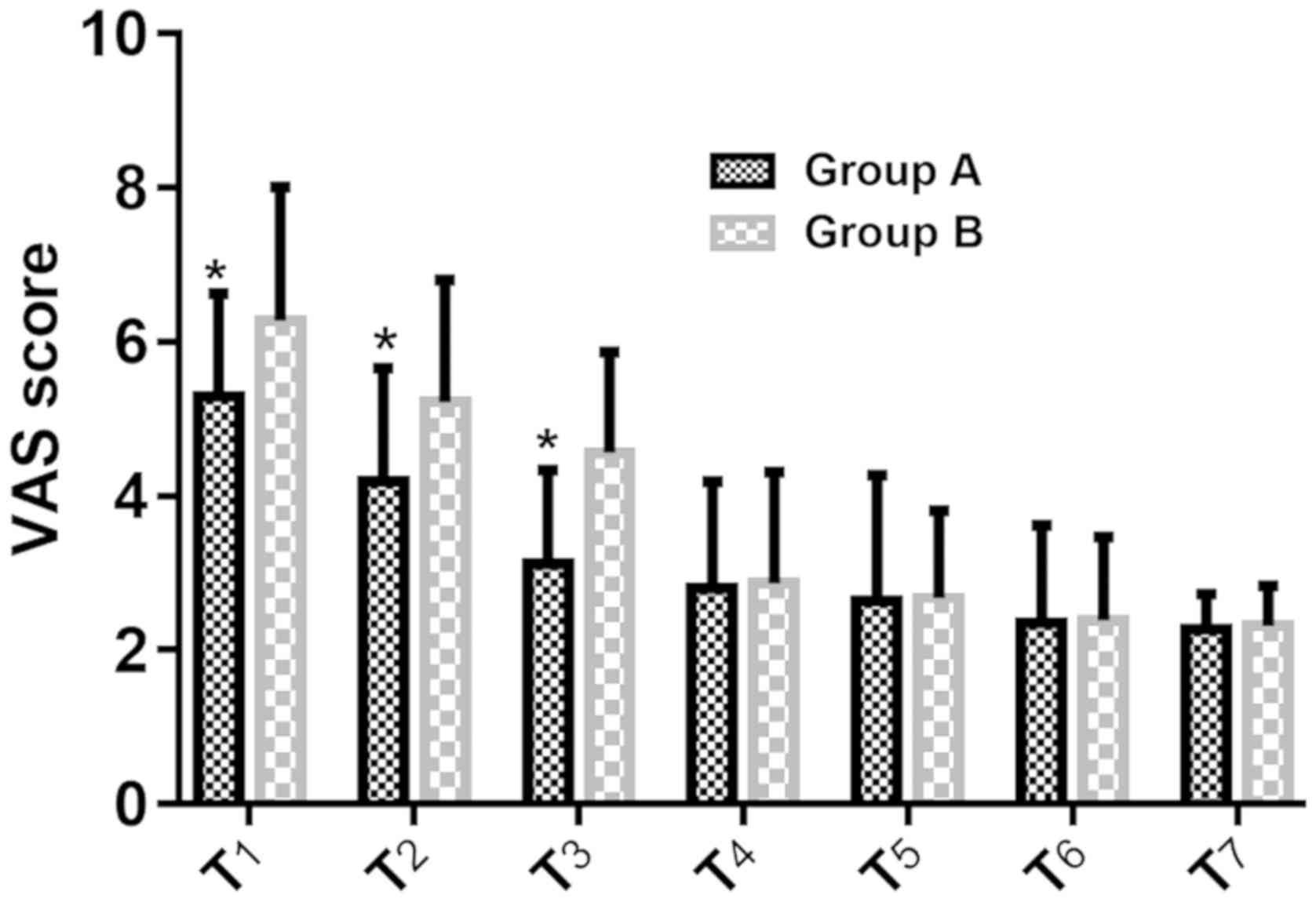
Comparison of VAS scores at 1 and 7
days after operation between groups A and B
VAS scores of group A were ssignificantly lower than
those of group B at 1–3 days after operation (P<0.001). There
was no significant difference between groups A and B at 4–7 days
after operation (P>0.05) (Table
III and Fig. 1).
 | Table III.Comparison of VAS scores at 1 and 7
days after operation between groups A and B (mean ± SD). |
Table III.
Comparison of VAS scores at 1 and 7
days after operation between groups A and B (mean ± SD).
| Time points | Group A (n=74) | Group B (n=82) | t value | P-value |
|---|
| T1 | 5.29±1.34 | 6.28±1.73 | 3.685 | <0.001 |
| T2 | 4.19±1.47 | 5.22±1.58 | 4.170 | <0.001 |
| T3 | 3.13±1.21 | 4.56±1.31 | 6.303 | <0.001 |
| T4 | 2.81±1.38 | 2.87±1.44 | 0.374 | 0.708 |
| T5 | 2.64±1.63 | 2.68±1.13 | 0.689 | 0.492 |
| T6 | 2.35±1.27 | 2.39±1.08 | 0.546 | 0.604 |
| T7 | 2.27±0.46 | 2.31±0.53 | 0.938 | 0.350 |
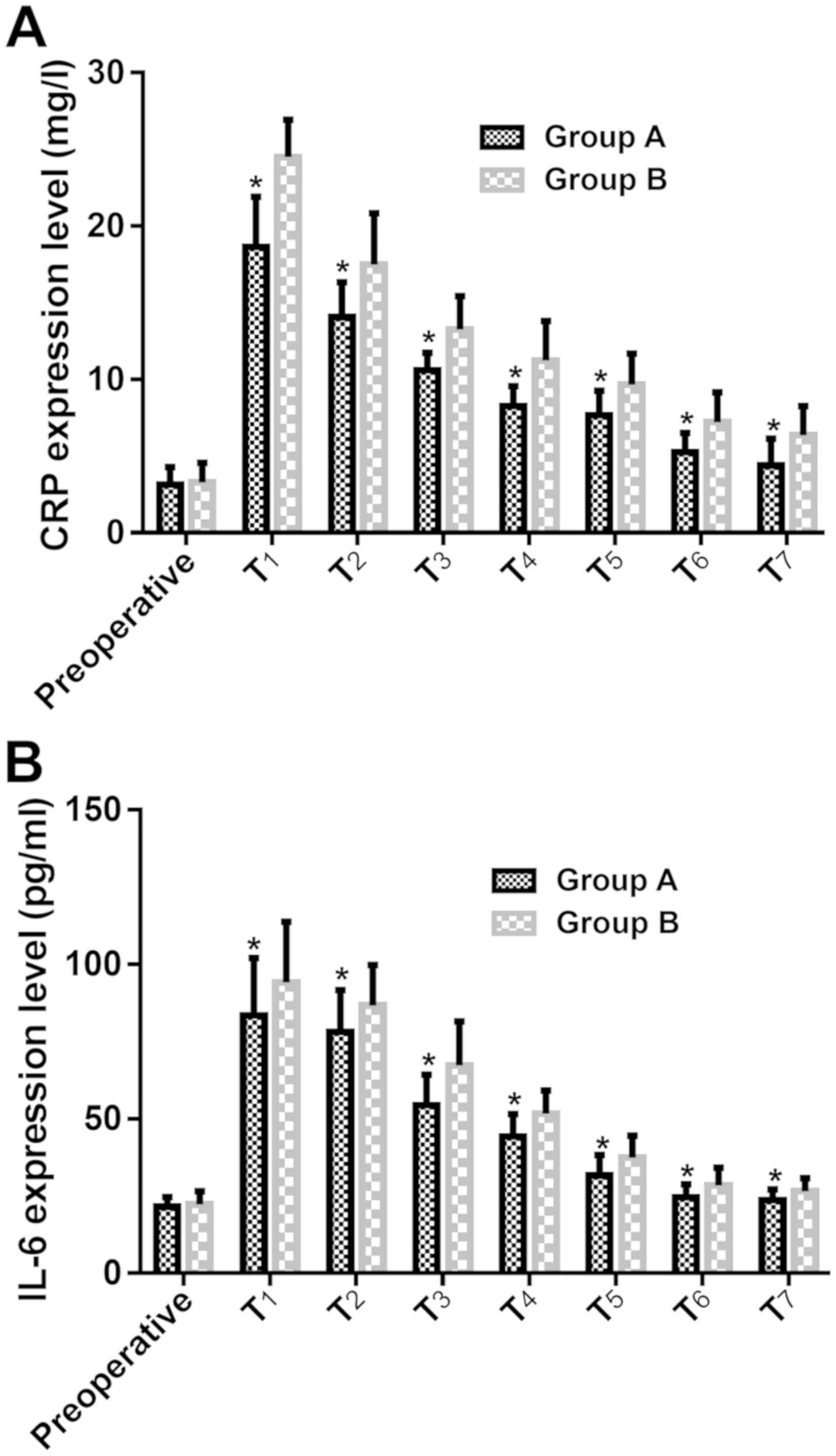
Comparison of serum CRP and IL-6
expression levels between groups A and B before and 1 to 7 days
after operation
There was no significant difference in serum CRP and
IL-6 expression levels between groups A and B before operation
(P>0.05). Levels of serum CRP and IL-6 in group A were
significantly lower than those in group B at 1–7 days after
operation (P<0.001) (Tables IV
and V; Fig. 2).
 | Table IV.Comparison of serum CRP expression
levels between groups A and B before and 1–7 days after surgery
(mean ± SD, mg/l). |
Table IV.
Comparison of serum CRP expression
levels between groups A and B before and 1–7 days after surgery
(mean ± SD, mg/l).
| Time points | Group A (n=74) | Group B (n=82) | t value | P-value |
|---|
| Before
operation | 3.15±1.13 | 3.29±1.27 | 0.724 | 0.470 |
| T1 | 18.64±3.27 | 24.52±2.41 | 12.870 | <0.001 |
| T2 | 14.05±2.29 | 17.49±3.36 |
7.392 | <0.001 |
| T3 | 10.59±1.15 | 13.25±2.18 |
9.382 | <0.001 |
| T4 |
8.25±1.32 | 11.23±2.57 |
8.963 | <0.001 |
| T5 |
7.67±1.59 |
9.67±2.03 |
6.799 | <0.001 |
| T6 |
5.27±1.24 |
7.22±1.94 |
7.390 | <0.001 |
| T7 |
4.38±1.76 |
6.37±1.89 |
6.784 | <0.001 |
 | Table V.Comparison of serum IL-6 expression
levels between groups A and B before and 1 to 7 days after surgery
(mean ± SD, pg/l). |
Table V.
Comparison of serum IL-6 expression
levels between groups A and B before and 1 to 7 days after surgery
(mean ± SD, pg/l).
| Time points | Group A (n=74) | Group B (n=82) | t value | P-value |
|---|
| Before
operation | 21.53±3.18 | 22.37±4.18 | 1.401 | 0.163 |
| T1 |
83.47±18.63 |
94.18±19.67 | 3.482 | <0.001 |
| T2 |
78.20±13.47 |
86.74±13.08 | 4.005 | <0.001 |
| T3 | 54.43±9.85 |
67.36±14.22 | 6.533 | <0.001 |
| T4 | 44.27±7.31 | 51.64±7.58 | 6.167 | <0.001 |
| T5 | 31.74±6.52 | 37.41±7.15 | 5.156 | <0.001 |
| T6 | 24.58±4.28 | 28.47±5.74 | 4.757 | <0.001 |
| T7 | 23.69±3.51 | 26.51±4.28 | 4.471 | <0.001 |
Comparison of postoperative
complications between groups A and B
In group A, 1 case (1.35%) had lung leak, 2 cases
(2.70%) had atelectasis, 6 cases (8.11%) had arrhythmia, and the
complication rate was 12.16%. In group B, 2 cases (2.44%) had
pulmonary infection, 1 case (1.22%) had lung leak, 3 cases (3.66%)
had atelectasis, 8 cases (9.76%) had arrhythmia, and the
complication rate was 17.07%. There was no significant difference
in the incidence of complications between groups A and B
(P>0.05) (Table VI).
 | Table VI.Comparison of postoperative
complications between groups A and B [n (%)]. |
Table VI.
Comparison of postoperative
complications between groups A and B [n (%)].
| Groups | n | Pulmonary
infection | Lung leak | Atelectasis | Arrhythmia | Incidence rate
(%) |
|---|
| A | 74 | 0 (0.00) | 1 (1.35) | 2 (2.70) | 6 (8.11) | 12.16 |
| B | 82 | 2 (2.44) | 1 (1.22) | 3 (3.66) | 8 (9.76) | 17.07 |
| χ2
value | – | – | – | – | – | 0.746 |
| P-value | – | – | – | – | – | 0.388 |
Comparison of quality of life between
groups A and B before and after operation
There was no significant difference in physical,
functional, emotional, social and additional status scores between
groups A and B before and after operation (P>0.05). The overall
status score of groups A and B after operation was significantly
lower than that before operation (P<0.001), and the overall
status score of group A after operation was significantly higher
than that of group B (P<0.001) (Table VII).
 | Table VII.Comparison of quality of life between
groups A and B before and after operation (mean ± SD). |
Table VII.
Comparison of quality of life between
groups A and B before and after operation (mean ± SD).
|
| Group A (n=74) |
|
| Group B (n=82) |
|
|
|---|
| Status scores | Before
operation | After
operation | t value | P-value | Before
operation | After
operation | t value | P-value |
|---|
| Physical
status |
19.35±2.81 | 19.25±1.83 | 0.257 | 0.798 |
19.36±2.68 | 19.07±2.13 | 0.743 | 0.459 |
| Functional
status |
21.03±2.37 | 20.62±2.13 | 1.107 | 0.270 |
20.71±2.16 | 19.85±2.38 | 1.513 | 0.132 |
| Emotional
status |
19.82±2.47 | 19.32±1.94 | 1.369 | 0.173 |
19.44±2.02 | 18.86±1.92 | 1.833 | 0.069 |
| Social status |
18.36±4.28 | 17.33±3.25 | 1.649 | 0.101 |
18.49±4.17 | 17.52±2.86 | 1.737 | 0.084 |
| Additional
status |
24.05±5.36 | 23.16±4.03 | 1.142 | 0.256 |
23.51±4.13 | 22.72±3.11 | 1.384 | 0.168 |
| Overall status | 102.15±7.35 | 98.31±5.23 | 3.662 |
<0.001a | 101.36±8.52 | 95.13±5.68 | 5.509 |
<0.001a |
Discussion
The number of lung cancer patients has increased in
recent years and lung cancer has become the leading cause of human
death. For the early treatment of lung cancer, surgical resection
is still the main method. Traditional thoracotomy causes severe
incision and trauma, and postoperative pain is serious, which makes
the quality of life of lung cancer patients greatly reduced
(15). With the continuous
development of endoscopic techniques, minimally invasive treatment
has become a hot research topic that could reduce postoperative
complications and improve the quality of life of patients with
NSCLC (16). Single utility port
VATS is operated with only one incision. With single utility port
VATS, thoracoscope and instruments are operated in one hole during
the operation, and the trauma is small, and blood vessels and
intercostal nerve damage are avoided, and postoperative pain is
also lighter (17). Thus, single
utility port VATS therapy is receiving increasing attention in
clinical treatment of NSCLC.
Previous studies have shown that the surgical
incision of single utility port VATS is mostly between 4.0 and 7.0
cm (18). The length of the incision
in this study is about 4.0 to 5.0 cm, which is similar to previous
studies. Three-port VATS usually requires three incisions. The
first incision is generally used as an observation hole between the
7th and 8th intercostals, and second incision is used as the main
operation hole in the 5th or 6th intercostal space of the ankle
line, and the 3rd incision is a sub-operation hole (19) made between the rear line and the
shoulder line.
Single utility port VATS is a modified 2-incision
technique in which the operating hole is located at the 4th
intercostal space of the incision, and the incision is large enough
for the operator to accurately position the endoscopic stapler on
the fragile pulmonary vessel; and with less incision on the chest
wall, the intercostal nerve injury and intercostal traction could
be minimized during surgery (18).
Results of this study showed that blood loss in group A was
significantly lower than that in group B. The VAS score was
significantly lower in group A than that in group B at 1–3 days
after operation, suggesting that single utility port VATS performed
for patients with NSCLC can reduce intraoperative blood loss,
reduce trauma during surgery and reduce postoperative pain, this
result is similar with the study of Zhu et al (20). Single utility hole VATS is a
single-hole operation and ribs are not pulled, so thoracic damage
and pain are relatively light. This may be because single utility
port VATS is without rib traction, which causes less pain to the
patient's thorax, while 3 holes from the posterior tibial incision
as a secondary operation hole. There are many layers of muscles in
the thoracic back, abundant blood supply and nerve distribution,
narrow rib space, and thus easy to bleed during the incision. An
important indicator of successful operation in radical surgery for
lung cancer is the hilar mediastinal lymphadenectomy. Effective
removal of the hilar and mediastinal lymph nodes during surgery can
not only provide reference for postoperative pathological staging,
but also affect the prognosis of patients (21,22). The
results of Chang et al (23)
showed that the total number of single utility port or double-port
VATS lymph node dissection was similar. Results of this study
showed that there was no significant difference in the number of
lymph node dissections between groups A and B. Therefore, single
utility port VATS can also achieve the purpose of treating
NSCLC.
IL-6 is an acute phase mediator involved in B cell
stimulation. Peak value of IL-6 is usually reached 2 h after
surgery, and then rapidly decreases in patients without
complications. CRP is one of the representatives of acute phase
proteins and provides a reliable screening test for acute phase
reactants. CRP level reaches peaks between 24 and 72 h after
surgery, and its level may continue to rise for approximately 2
weeks (24,25). Therefore, IL-6 and CRP can be used as
objective biochemical markers reflecting surgical tissue trauma.
Results of this study showed that levels of serum CRP and IL-6 in
group A were significantly lower than those in group B at 1 to 7
days after surgery, indicating that single utility port VATS can
reduce the surgical trauma and reduce stress response in patients
with NSCLC. In addition, results of this study showed that
incidence of complication in group A was not significantly
different from that in group B, but the length of hospital stay was
significantly shorter than that in group B, indicating that single
utility port VATS can shorten hospital stay. Dai et al
(26) showed that single-pore VATS
have the advantages of reducing blood loss and reducing
postoperative pain compared with dual-pore VATS. Surgery-induced
intercostal nerve injury is an important cause of pain in patients
(27). Overall incision length of
single utility port VATS is significantly reduced compared with
three-port VATS, and intercostal nerve damage is reduced, and the
amount of intraoperative blood loss is also reduced. Therefore,
complications such as lung infections are inhibited, and hospital
stay is shortened.
Quality of life of cancer patients has become an
important criterion for the evaluation of tumor treatment efficacy
(28). Our 3-month follow-up study
showed that there was no significant difference in physical,
functional, emotional, social, and additional status scores between
the preoperative and postoperative levels in groups A and B.
Overall status of group A and B was significantly worse than that
of preoperative conditions. Overall status of group A was
significantly higher than that of group B, suggesting that VATS
will affect the quality of life of patients with NSCLC, but the
effect of single utility port VATS on short-term quality of life is
better than that of three-port VATS, possibly due to the smaller
trauma caused by single utility port VATS. Möller et al
(29) followed up patients
undergoing lung cancer surgery and found that the SF-36 quality of
life score decreased 6 months after surgery, which confirmed that
thoracic surgery would affect the quality of life of patients,
however, the report also showed Age, extent of resection, and
subsequent adjuvant therapy were closely associated with a decline
in quality of life associated with physical condition at 6 months
postoperatively. Although the differences between the single
utility port and three-port VATS perioperative indexes were
observed in this study, long-term follow-up results are lacking.
The recurrence of cancer was not investigated. Thus, studies with
longer follow-up are still required.
In conclusion, clinical efficacies of single utility
port VATS and three-port VATS were similar. Single utility port
VATS can reduce trauma during surgery, reduce stress response,
relieve postoperative pain, and facilitate the recovery of
postoperative quality of life.
Acknowledgements
Not applicable.
Funding
This study was supported by Taizhou Science and
Technology Bureau (no. 14sf03).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZY and BZ conceived and designed the study. YC
collected the patient data. ZY and JL analyzed and interpreted the
patient data regarding the non-small cell lung cancer. ZY and BZ
performed the experiment of single utility port VATS and three-port
VATS. ZY was a major contributor in writing the manuscript. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by The Ethics Committee of
Taizhou Hospital of Zhejiang Province (Taizhou, China). Patients
who participated in this research had complete clinical data. The
signed informed consents were obtained from the patients or the
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Chen W, Zheng R, Zeng H and Zhang S:
Epidemiology of lung cancer in China. Thorac Cancer. 6:209–215.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bhaumik S, Ahmad F and Das BR: Molecular
binary classification of NSCLC: miR-375 is a potential biomarker to
differentiate SQCC from ADCC in Indian NSCLC patients. Appl Cancer
Res. 37:282017. View Article : Google Scholar
|
|
3
|
Higuchi M, Yaginuma H, Yonechi A, Kanno R,
Ohishi A, Suzuki H and Gotoh M: Long-term outcomes after
video-assisted thoracic surgery (VATS) lobectomy versus lobectomy
via open thoracotomy for clinical stage IA non-small cell lung
cancer. J Cardiothorac Surg. 9:882014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Paul S, Sedrakyan A, Chiu YL, Nasar A,
Port JL, Lee PC, Stiles BM and Altorki NK: Outcomes after lobectomy
using thoracoscopy vs thoracotomy: A comparative effectiveness
analysis utilizing the Nationwide Inpatient Sample database. Eur J
Cardiothorac Surg. 43:813–817. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yang HX, Woo KM, Sima CS, Bains MS,
Adusumilli PS, Huang J, Finley DJ, Rizk NP, Rusch VW, Jones DR, et
al: Long-term survival based on the surgical approach to lobectomy
for clinical stage I nonsmall cell lung cancer: Comparison of
robotic, video-assisted thoracic surgery, and thoracotomy
lobectomy. Ann Surg. 265:431–437. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ng CSH, Gonzalez-Rivas D, D'Amico TA and
Rocco G: Uniportal VATS - a new era in lung cancer surgery. J
Thorac Dis. 7:1489–1491. 2015.PubMed/NCBI
|
|
7
|
Gonzalez-Rivas D, de la Torre M, Fernandez
R and Mosquera VX: Single-port video-assisted thoracoscopic left
upper lobectomy. Interact Cardiovasc Thorac Surg. 13:539–541. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Anile M, Diso D, De Giacomo T, Rendina EA
and Venuta F: Uniportal thoracoscopic lobectomy. Ann Thorac Surg.
96:7452013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Abouarab AA, Rahouma M, Kamel M, Ghaly G
and Mohamed A: Single versus multi-incisional video-assisted
thoracic surgery: A systematic review and meta-analysis. J
Laparoendosc Adv Surg Tech A. 28:174–185. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Reck M, Popat S, Reinmuth N, De Ruysscher
D, Kerr KM and Peters S; ESMO Guidelines Working Group, :
Metastatic non-small-cell lung cancer (NSCLC): ESMO Clinical
Practice Guidelines for diagnosis, treatment and follow-up. Ann
Oncol. 25 (Suppl 3):iii27–iii39. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hanna NH, Dahlberg SE, Kolesar JM,
Aggarwal C, Hirsch FR, Ramalingam SS and Schiller JH: Three-arm,
randomized, phase 2 study of carboplatin and paclitaxel in
combination with cetuximab, cixutumumab, or both for advanced
non-small cell lung cancer (NSCLC) patients who will not receive
bevacizumab-based therapy: An Eastern Cooperative Oncology Group
(ECOG) study (E4508). Cancer. 121:2253–2261. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sato J, Ohtori S, Orita S, Yamauchi K,
Eguchi Y, Ochiai N, Kuniyoshi K, Aoki Y, Nakamura J, Miyagi M, et
al: Radiographic evaluation of indirect decompression of mini-open
anterior retroperitoneal lumbar interbody fusion: Oblique lateral
interbody fusion for degenerated lumbar spondylolisthesis. Eur
Spine J. 26:671–678. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sapan HB, Paturusi I, Jusuf I, Patellongi
I, Massi MN, Pusponegoro AD, Arief SK, Labeda I, Islam AA, Rendy L,
et al: Pattern of cytokine (IL-6 and IL-10) level as inflammation
and anti-inflammation mediator of multiple organ dysfunction
syndrome (MODS) in polytrauma. Int J Burns Trauma. 6:37–43.
2016.PubMed/NCBI
|
|
14
|
Ferrell B, Sun V, Hurria A, Cristea M, Raz
DJ, Kim JY, Reckamp K, Williams AC, Borneman T, Uman G, et al:
Interdisciplinary palliative care for patients with lung cancer. J
Pain Symptom Manag. 50:758–767. 2015. View Article : Google Scholar
|
|
15
|
Bendixen M, Jørgensen OD, Kronborg C,
Andersen C and Licht PB: Postoperative pain and quality of life
after lobectomy via video-assisted thoracoscopic surgery or
anterolateral thoracotomy for early stage lung cancer: A randomised
controlled trial. Lancet Oncol. 17:836–844. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hao Z, Cai Y, Fu S, Zhang N and Fu X:
Comparison study of post-operative pain and short-term quality of
life between uniportal and three portal video-assisted thoracic
surgery for radical lung cancer resection. Zhongguo Fei Ai Za Zhi.
19:122–128. 2016.(In Chinese). PubMed/NCBI
|
|
17
|
Hirai K, Takeuchi S and Usuda J:
Single-incision thoracoscopic surgery and conventional
video-assisted thoracoscopic surgery: a retrospective comparative
study of perioperative clinical outcomes. Eur J Cardiothorac Surg.
49 (Suppl 1):i37–i41. 2016.PubMed/NCBI
|
|
18
|
Wang BY, Liu CY, Hsu PK, Shih CS and Liu
CC: Single-incision versus multiple-incision thoracoscopic
lobectomy and segmentectomy: A propensity-matched analysis. Ann
Surg. 261:793–799. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Shen Y, Wang H, Feng M, Xi Y, Tan L and
Wang Q: Single-versus multiple-port thoracoscopic lobectomy for
lung cancer: a propensity-matched study. Eur J Cardiothorac Surg.
49 (Suppl 1):i48–i53. 2016.PubMed/NCBI
|
|
20
|
Zhu Y, Liang M, Wu W, Zheng J, Zheng W,
Guo Z, Zheng B, Xu G and Chen C: Preliminary results of single-port
versus triple-port complete thoracoscopic lobectomy for non-small
cell lung cancer. Ann Transl Med. 3:922015.PubMed/NCBI
|
|
21
|
Wang W, Yin W, Shao W, Jiang G, Wang Q,
Liu L, Liu D, Wang Z, Zhu Z, Chen H, et al: Comparative study of
systematic thoracoscopic lymphadenectomy and conventional
thoracotomy in resectable non-small cell lung cancer. J Thorac Dis.
6:45–51. 2014.PubMed/NCBI
|
|
22
|
Finley R, Mayo J, Donagh C, Leo J, Grant
K, Lam S and English J: P1. 16–34 The impact of pathology, staging
and operative resection on survival and CT evidence of recurrence
of early NSCLC. J Thorac Oncol. 13:S640–S641. 2018. View Article : Google Scholar
|
|
23
|
Chang JM, Kam KH, Yen YT, Huang WL, Chen
W, Tseng YL, Wu MH, Lai WW and Gonzalez-Rivas D: From biportal to
uniportal video-assisted thoracoscopic anatomical lung resection: A
single-institute experience. Medicine (Baltimore). 95:e50972016.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Leung KL, Lai PBS, Ho RLK, Meng WC, Yiu
RY, Lee JF and Lau WY: Systemic cytokine response after
laparoscopic-assisted resection of rectosigmoid carcinoma: A
prospective randomized trial. Ann Surg. 231:506–511. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Fretland AA, Sokolov A, Postriganova N,
Kazaryan AM, Pischke SE, Nilsson PH, Rognes IN, Bjornbeth BA,
Fagerland MW, Mollnes TE, et al: Inflammatory response after
laparoscopic versus open resection of colorectal liver metastases:
Data from the Oslo-CoMet Trial. Medicine (Baltimore). 94:e17862015.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Dai F, Meng S, Mei L, Guan C and Ma Z:
Single-port video-assisted thoracic surgery in the treatment of
non-small cell lung cancer: A propensity-matched comparative
analysis. J Thorac Dis. 8:2872–2878. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Mier JM, Chavarin A, Izquierdo-Vidal C,
Fibla JJ and Molins L: A prospective study comparing three-port
video-assisted thoracoscopy with the single-incision laparoscopic
surgery (SILS) port and instruments for the video thoracoscopic
approach: A pilot study. Surg Endosc. 27:2557–2560. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Quinten C, Martinelli F, Coens C,
Sprangers MA, Ringash J, Gotay C, Bjordal K, Greimel E, Reeve BB,
Maringwa J, et al Patient Reported Outcomes and Behavioral Evidence
(PROBE) the European Organization for Research and Treatment of
Cancer (EORTC) Clinical Groups, : A global analysis of multitrial
data investigating quality of life and symptoms as prognostic
factors for survival in different tumor sites. Cancer. 120:302–311.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Möller A and Sartipy U: Predictors of
postoperative quality of life after surgery for lung cancer. J
Thorac Oncol. 7:406–411. 2012. View Article : Google Scholar : PubMed/NCBI
|