Introduction
Gastric cancer (GC) is a common disease with
morbidity that ranks fifth worldwide. GC is the third cause of
human deaths worldwide. There are ~952,000 new cases of GC each
year, and there were ~783,000 deaths in 2018 (1,2). A study
has shown that diabetes is one of the independent predictive
factors of gastrectomy postoperative complications of patients with
GC (3). Studies have also reported
that the cancer risk of patients with diabetes is increased, and
the number of patients with type 2 diabetes mellitus (T2DM) and GC
is increasing (4,5). These results suggest that there is
relevance between T2DM and GC, probably due to their common risk
factors, such as obesity, insulin resistance, and smoking. The
underlying mechanism may be related to the imbalance of blood
glucose levels, oxidative stress, and adverse inflammatory
reactions (6). At present, the
treatment methods of complications of T2DM and GC are ineffective.
Surgery is still the first-line treatment method of GC; however,
the anesthesia in surgery has side effects and leads to systemic
dysfunction or even injury of important tissues (7,8).
Therefore, the study of the effects of anesthetics on patients with
T2DM and GC is important in order to improve the treatment methods
and reduce the complications of T2DM and GC.
The chemical structure of propofol is
2,6-diisopropylphenol. As an intravenous injectable anesthetic, it
is preferentially used for the induction and maintenance of general
anesthesia during surgery, even for the anesthesia and sedation of
children (9,10). A study has shown that propofol can
inhibit cell apoptosis and inflammation and has a neuroprotective
effect by regulating proteins associated with neuroprotection or
ion homeostasis (11). Propofol's
anesthetic effect is activated by γ-aminobutyric acid receptors to
regulate the excitatory amino acid neurotransmitter system and
protect the brain cells from oxidative stress (11). In the present study, in addition to
Propofol, an intravenous injectable anesthetic, an inhaled
anesthetic was investigated. Sevoflurane is an inhaled anesthetic
that is widely used in clinical practice. It takes effect in
different organs or systems and does not have great side effects.
Sevoflurane's anesthetic effect is safe (12). The minimum alveolar concentration
(MAC) value of sevoflurane decreases with the increase of age, and
the MAC value is negatively correlated with the effect of inhaled
anesthetics. This indicates that the anesthetic effect of
sevoflurane increases with the increase of age (13). In the study of Xu et al
(14), it was reported that propofol
and sevoflurane could protect the liver by regulating an
inflammatory reaction and reducing oxidative stress and apoptosis
of the liver cells. In the study of Zheng et al (15), patients with GC who had underwent
gastrectomy were studied. It was reported that the average survival
time of the patients in the propofol group was significantly longer
than that of the patients in sevoflurane group. This result
suggests that using propofol can significantly increase the
survival rate of patients who have GC and undergo gastrectomy.
The main purpose of this study was to compare the
effects of propofol and sevoflurane on blood glucose, hemodynamics,
and inflammatory factors of patients in perioperative period.
Mini-Mental State Examination (MMSE) cognitive function scores, the
anesthetic effect, and the incidence of adverse reactions were also
compared to provide clinical data on anesthesia for the
completeness of the comprehensive treatment of patients with T2DM
and GC.
Patients and methods
General data
One hundred and ten patients with T2DM and GC, who
were treated in The First Affiliated Hospital of Baotou Medical
College (Baotou, China) from January 2017 to December 2018, were
selected. There were 70 males and 40 females, 30–75 years of age,
with average age of 55.25±8.75 years, and weight 50–75 kg. Sixty
patients were included in the propofol group and 50 patients were
included in the sevoflurane group. The patients in the propofol
group were anesthetized by propofol, whereas the patients in the
sevoflurane group were anesthetized by sevoflurane. The study was
approved by the Ethics Committee of The First Affiliated Hospital
of Baotou Medical College. The patients and their family members
were informed and signed written informed consents.
Inclusion and exclusion criteria
Inclusion criteria: Patients with histological and
pathological examinations, and clinical symptoms conforming to T2DM
and GC (16,17); patients with American Society of
Anesthesiologists (ASA) grade I and II disease (18); patients with MMSE that was carried
out 10 h before the operation (19);
patients with score >24 points; patients with no surgical
contraindications and allergies to the medicines used in this
study; patients not using medicines that affect the level of blood
glucose, hemodynamic indicators, and the level of inflammatory
factors in the prior 15 days; patients that were informed and
cooperated voluntarily for this study. Exclusion criteria: Patients
with mental illness or taking a large dose of sedatives; patients
with vision, hearing, or language disorder; patients complicated
with other cancers; patients with severe heart, liver, lung, or
kidney dysfunction. The inclusion criteria were applicable for the
propofol and the sevoflurane groups.
Anesthesia methods
Before the patients in two groups were anesthetized,
they fasted for 6 h, and routine examinations were performed. The
fasting blood glucose level of the patients was maintained at ≤6.99
mmol/l by insulin injection. The anesthetic effect of the patients
in the propofol group was induced and maintained with propofol (4–8
mg/kg/min) (B33792-100 mg; Shanghai Yuanye Bio-Technology Co.,
Ltd.). The anesthetic effect of the patients in the sevoflurane
group was induced and maintained with 1–3% sevoflurane
(XY-EP-Y0001046; Shanghai Xiyuan Biotechnology Co., Ltd.), and the
patients were intubated to carry out mechanical ventilation.
Propofol or sevoflurane was supplemented according to the vital
signs of the patients in the two groups. After the patients were
anesthetized, the mechanical ventilation was replaced by assisted
breathing. When the patients regained consciousness, the tubes were
pulled out and the patients were transferred to Intensive Care
Unit. Venous blood (5 ml) was collected from the patients in two
groups before the anesthesia was carried out, 2 min after
intubation, 5 min after pneumoperitoneum, and 60 min after surgery.
The change of blood glucose levels of the patients was measured by
a blood glucose monitoring device in different periods (Beijing
Anteng Medical Devices Co., Ltd.). The levels of serum inflammatory
factors, IL-1β, IL-6, IL-10 and TNF-α, were measured by an
enzyme-linked immunosorbent assay (ELISA) according to the
manufacturer's instructions of human IL-1β ELISA kit, human IL-6
ELISA kit, human IL-10 ELISA kit, and human TNF-α ELISA kit
(FK-R0180, FK-R0049, FK-R0066, FK-0122; Shanghai Fanke
Biotechnology Co., Ltd.).
MMSE score rules
Each question was 1 point and the full score was 30
points. There were 10 questions on orientation, such as time,
location, and site; 3 questions on memory; 5 questions on attention
and arithmetic; 3 questions on recall; 9 questions on language
ability, including name, retelling, three-step command, reading,
writing and structure. The higher the MMSE score was, the better
the cognitive ability was.
Observation indicators
The level of blood glucose, the hemodynamic
indicators, including heart rate (HR), oxygen saturation
(SpO2), systolic blood pressure (SBP), and mean blood
pressure (MBP), and the levels of the serum inflammatory factors
IL-1β, IL-6, IL-10 and TNF-α, were observed and compared at
T0 (before anesthesia), T1 (2 min after
intubation), T2 (5 min after pneumoperitoneum), and
T3 (60 min after surgery). In addition, MMSE scores were
observed and compared at T0 (before anesthesia),
T4 (6 h after surgery), and T5 (72 h after
surgery). The anesthetic effect after surgery (time of spontaneous
breath, eye opening, extubation, and verbal response), and the
incidence of adverse reactions (nausea, emesis, cough, bradycardia,
dysphoria, breath holding, laryngospasm, and bronchospasm) were
also compared between the two groups.
Statistical analysis
SPSS 19.0 (IBM Corp.) was used to carry out
statistical analysis. GraphPad Prism 6 (GraphPad Software, Inc.,)
was used for data visualization. The measurement data were
expressed as mean ± standard deviation (mean ± SD), and the
independent samples t-test was used to compare the measurement data
between groups. The count data were expressed as the number of
cases and percentage [n (%)], and χ2 test was used to
compare the count data between groups. ANOVA with Dunnett's post
hoc test was used for comparison between multiple groups. P<0.05
was considered to indicate a statistically significant
difference.
Results
General data
The general data of the patients in two groups were
compared, including sex, age, body mass index (BMI), smoking
history, drinking history, hypertension, marital status, TNM stage,
pathological differentiation degree and ASA grade. No significant
difference was found in these data (P>0.05) (Table I).
 | Table I.Comparison of the general data of
patients in the two groups [n (%), mean ± SD]. |
Table I.
Comparison of the general data of
patients in the two groups [n (%), mean ± SD].
| Category | n | Propofol group
(n=60) | Sevoflurane group
(n=50) |
χ2/t-test | P-value |
|---|
| Sex |
|
|
| 0.469 | 0.524 |
| Male | 70 | 40 (66.67) | 30 (60.00) |
|
|
|
Female | 40 | 20 (33.33) | 20 (40.00) |
|
|
| Age (years) |
|
|
| 0.764 | 0.382 |
| ≤60 | 60 | 35 (58.33) | 25 (50.00) |
|
|
|
>60 | 50 | 25 (41.67) | 25 (50.00) |
|
|
| BMI
(kg/m2) | 110 | 22.50±4.50 | 22.40±4.60 | 0.115 | 0.909 |
| Smoking
history |
|
|
| 0.177 | 0.860 |
| No | 45 | 25 (41.67) | 20 (40.00) |
|
|
|
Yes | 65 | 35 (58.33) | 30 (60.00) |
|
|
| Drinking
history |
|
|
| 2.700 | 0.100 |
| No | 51 | 23 (38.33) | 28 (56.00) |
|
|
|
Yes | 59 | 37 (61.67) | 22 (44.00) |
|
|
| Hypertension |
|
|
| 0.046 | 0.831 |
| No | 43 | 24 (40.00) | 19 (38.00) |
|
|
|
Yes | 67 | 36 (60.00) | 31 (62.00) |
|
|
| Marital status |
|
|
| 2.829 | 0.093 |
|
Unmarried | 35 | 15 (25.00) | 20 (40.00) |
|
|
|
Married | 75 | 45 (75.00) | 30 (60.00) |
|
|
| TNM stage |
|
|
| 0.031 | 0.860 |
|
I/II | 65 | 35 (58.33) | 30 (60.00) |
|
|
|
III/IV | 45 | 25 (41.67) | 20 (40.00) |
|
|
| Pathological
differentiation degree |
|
|
| 1.604 | 0.205 |
|
Middle/high
differentiation | 70 | 35 (58.33) | 35 (70.00) |
|
|
| Low
differentiation | 40 | 25 (41.67) | 15 (30.00) |
|
|
| ASA grade |
|
|
| 1.243 | 0.265 |
| Grade
I | 53 | 26 (43.33) | 27 (54.00) |
|
|
| Grade
II | 57 | 34 (56.67) | 23 (46.00) |
|
|
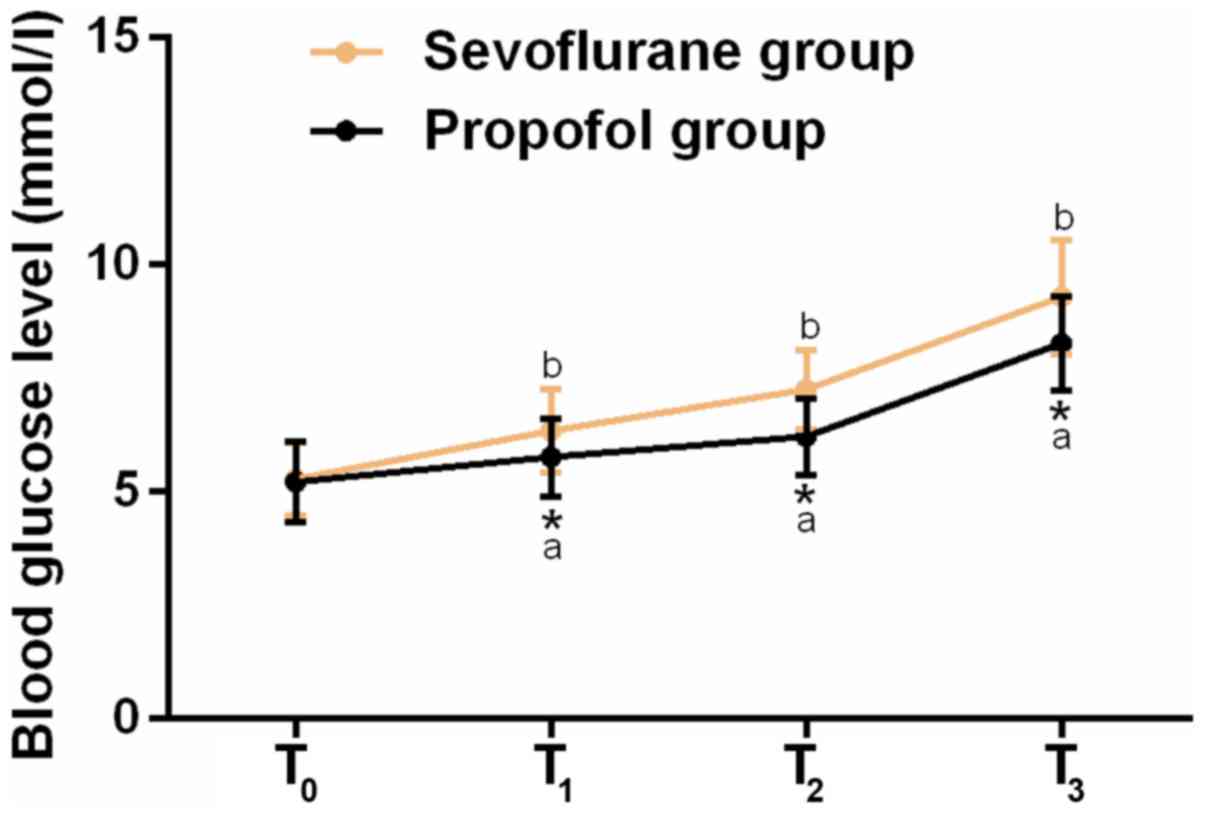
Comparison of blood glucose
levels
In order to investigate the effects of propofol and
sevoflurane on the blood glucose levels, a glucometer was used to
measure the blood glucose levels of the patients in the propofol
and sevoflurane group at T0, T1,
T2, and T3. The results revealed that there
was no significant difference between the blood glucose levels of
the patients in the propofol group and those of the patients in the
sevoflurane group at T0 (P>0.05). As the operation
time went on, blood glucose levels of the patients at
T1, T2, and T3 increased and were
significantly higher than those at T0 (P<0.05). The
blood glucose levels of the patients in the propofol group were
significantly lower than those of the patients in the sevoflurane
group at T1, T2 and T3 (P<0.05)
(Fig. 1).
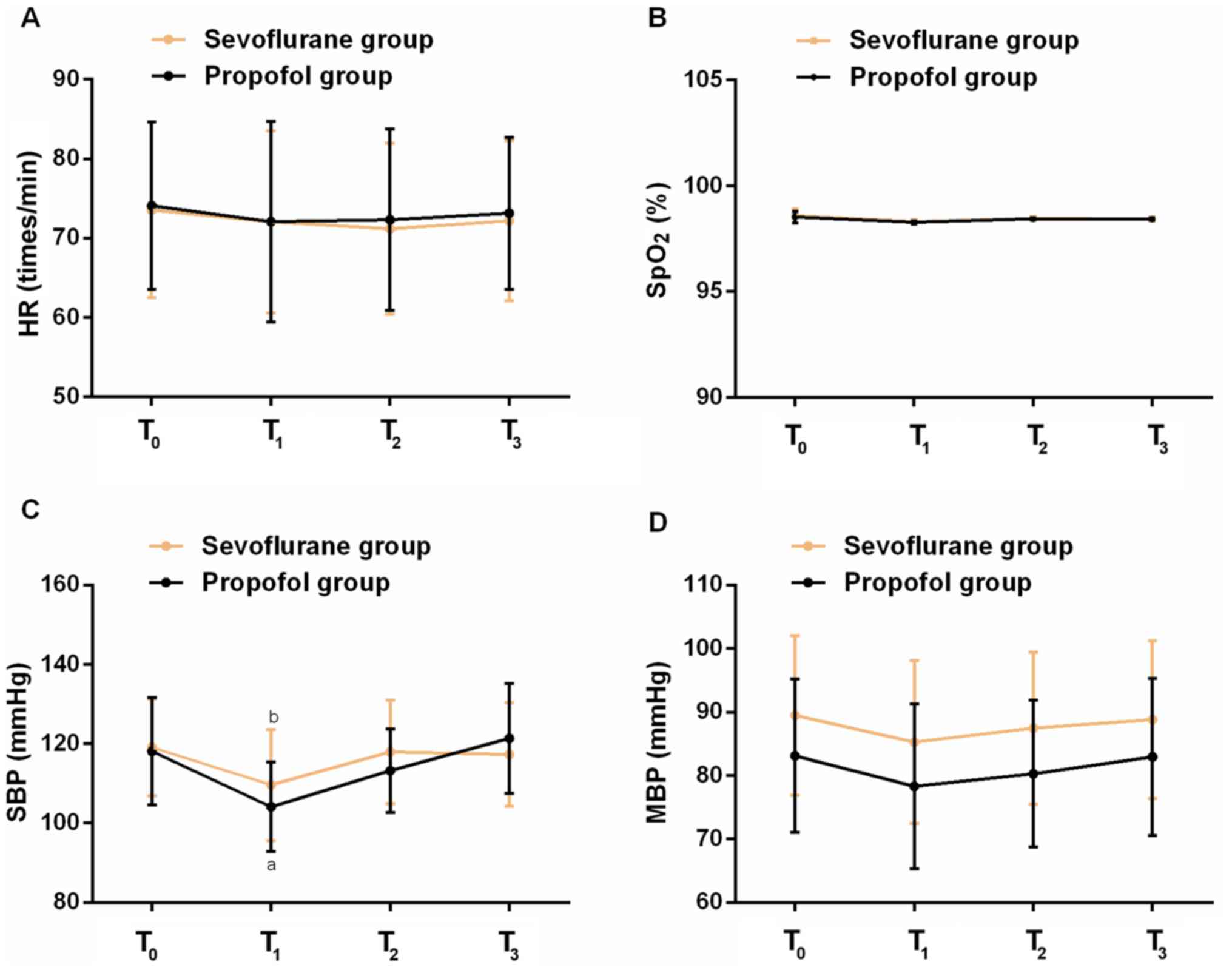
Comparison of hemodynamic
indicators
In order to investigate the effects of propofol and
sevoflurane on the hemodynamic indicators, the hemodynamic
indicators HR, SpO2, SBP and MBP were observed and
compared in the propofol and the sevoflurane group at
T0, T1, T2, and T3. The
results showed that there was no significant difference in HR,
SpO2, SBP and MBP of the patients in two groups at
T0, T1, T2 and T3
(P>0.05). Compared with the hemodynamic indicators at
T0, the hemodynamic indicators of the patients in the
propofol and sevoflurane group decreased at approximately
T1, whereas they increased at T2. There was
no significant difference between the hemodynamic indicators of the
patients in the propofol and sevoflurane group at T3 or
T0 (P>0.05) (Fig.
2).
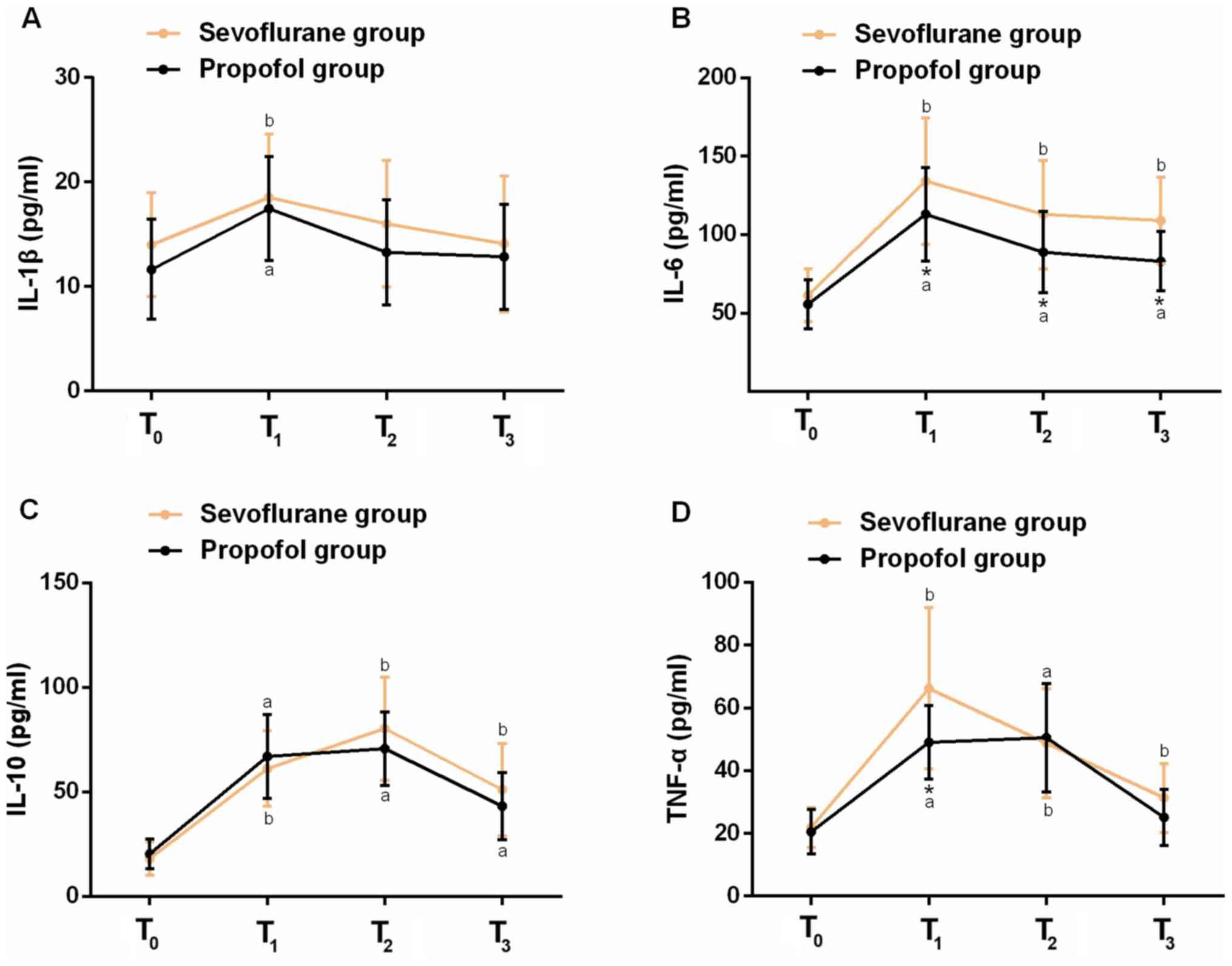
Comparison of the levels of
inflammatory factors
In order to investigate the effects of propofol and
sevoflurane on inflammatory factors, the levels of serum
inflammatory factors IL-1β, IL-6, IL-10 and TNF-α were measured in
the propofol and sevoflurane group at T0, T1,
T2 and T3 using ELISA. The results revealed
that the levels of IL-1β, IL-6, IL-10 and TNF-α in the propofol and
sevoflurane group were first increased, and then decreased to the
level at T0. There was no significant difference between
the levels of IL-1β, IL-6, IL-10 and TNF-α in the propofol group
and those in the sevoflurane group at T0 (P>0.05).
The levels of IL-1β, IL-6 and IL-10 in the propofol group were
lower than those in the sevoflurane group at T3, and the
level of IL-6 in the propofol group was significantly lower than
that in the sevoflurane group at T1, T2 and
T3 (P<0.05) (Fig.
3).
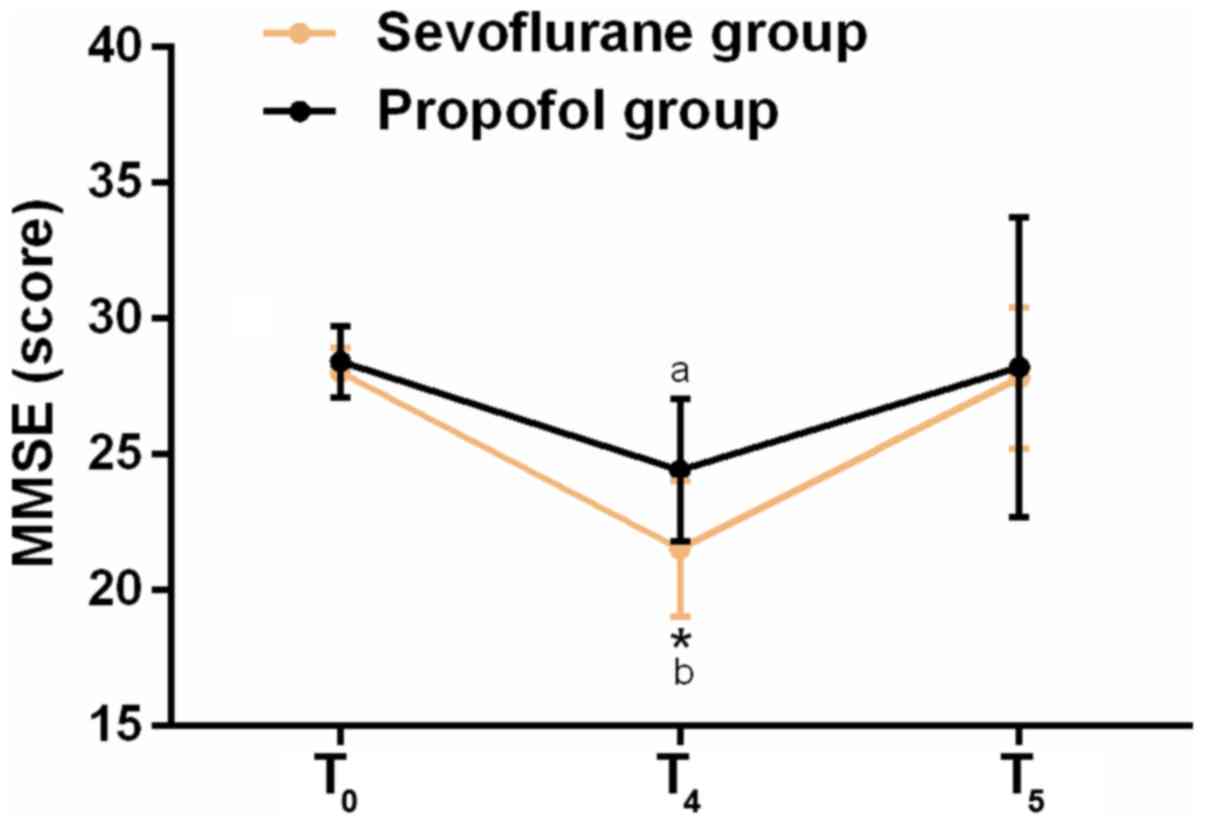
Comparison of MMSE cognitive function
scores
In order to investigate the effects of propofol and
sevoflurane on the cognitive function, MMSE cognitive function
scores in the propofol group and sevoflurane group were counted at
T0, T4, and T5. The results showed
that there was no significant difference between the MMSE cognitive
function scores in the propofol and the sevoflurane group at
T0 (P>0.05). MMSE cognitive function scores in the
propofol group were significantly higher than those in the
sevoflurane group at T4 (P<0.05), and MMSE cognitive
function scores in the propofol group and the sevoflurane group at
T4 were significantly lower than those at T0
(P<0.05). There was no significant difference between MMSE
cognitive function scores in the propofol and the sevoflurane group
at T5 and those at T0 (P>0.05) (Fig. 4).
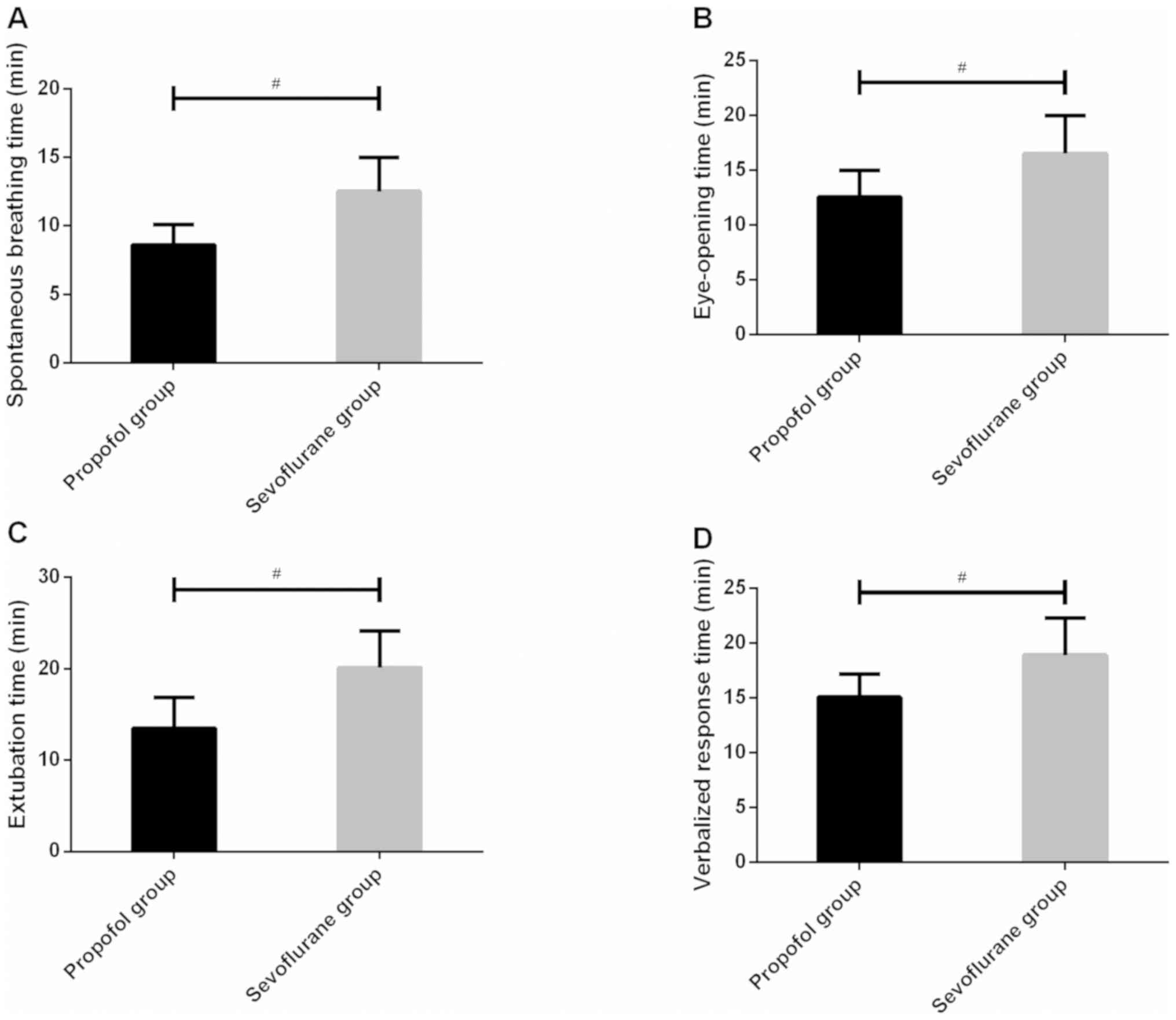
Comparison of the anesthetic
effect
In order to compare the anesthetic effects of
propofol and sevoflurane, the time of spontaneous breath, eye
opening, extubation and verbal response were observed and recorded
for both groups. The results showed that the time of spontaneous
breath, eye opening, extubation and verbal response in the propofol
group were significantly shorter than those in the sevoflurane
group (P<0.05) (Fig. 5).
Comparison of adverse reactions
In order to investigate the incidence of adverse
reactions of propofol and sevoflurane, the number of patients who
had nausea, vomiting, cough, bradycardia, restlessness, breath
holding, laryngospasm, and bronchospasm in the propofol and the
sevoflurane group was recorded. The results showed that there was
no patient with breath holding, laryngospasm, or bronchospasm in
the propofol or the sevoflurane group. There was 1 patient with
nausea and vomiting, 1 patient with cough, and 1 patient with
restlessness in the propofol group. The incidence of adverse
reactions was 5% in the propofol group (3/60). There were 6
patients with nausea and vomiting, 2 patients with cough, 1 patient
with bradycardia, 2 patients with restlessness in the sevoflurane
group. The incidence of adverse reactions was 22% in the
sevoflurane group (11/50). The results revealed that the incidence
of adverse reactions in the propofol group was lower than that in
the sevoflurane group (Table
II).
 | Table II.Comparison of adverse reactions of
the patients in two groups [n (%)]. |
Table II.
Comparison of adverse reactions of
the patients in two groups [n (%)].
| Category | Propofol group
(n=60) | Sevoflurane group
(n=50) | χ2
test | P-value |
|---|
| Nausea and
vomiting |
|
| 4.887 | <0.05 |
|
Yes | 1
(1.67) | 6
(12.00) |
|
|
| No | 59 (98.33) | 44 (88.00) |
|
|
| Cough |
|
| 0.560 | >0.05 |
|
Yes | 1
(1.67) | 2
(4.00) |
|
|
| No | 59 (98.33) | 48 (96.00) |
|
|
| Bradycardia |
|
| 1.211 | >0.05 |
|
Yes | 0
(0.00) | 1
(2.00) |
|
|
| No | 60 (100.00) | 49 (98.00) |
|
|
| Restlessness |
|
| 0.560 | >0.05 |
|
Yes | 1
(1.67) | 2
(4.00) |
|
|
| No | 59 (98.33) | 48 (96.00) |
|
|
| Breath holding |
|
| – | – |
|
Yes | 0
(0.00) | 0
(0.00) |
|
|
| No | 60 (100.00) | 50 (100.00) |
|
|
| Laryngospasm |
|
| – | – |
|
Yes | 0
(0.00) | 0
(0.00) |
|
|
| No | 60 (100.00) | 50 (100.00) |
|
|
| Bronchospasm |
|
| – | – |
|
Yes | 0
(0.00) | 0
(0.00) |
|
|
| No | 60 (100.00) | 50 (100.00) |
|
|
Discussion
The results on blood glucose levels showed that
there was no significant difference between blood glucose levels of
the patients in the propofol group and those in the sevoflurane
group before they were anesthetized (T0). After surgery,
the blood glucose levels of the patients gradually increased and
were significantly higher than those before the patients were
anesthetized. In addition, the blood glucose levels of the patients
in the propofol group were significantly lower than those in the
sevoflurane group. This result indicates that the effect of
propofol was less than that of sevoflurane on glucose metabolism
and the stress response of propofol was less than that of
sevoflurane to surgical stimulation. A report on anesthetic
management by Kitamura et al (20) demonstrated that the blood glucose
levels of the patients in the propofol group were significantly
higher than those in the sevoflurane group within 4 h after the
patients were anesthetized, similarly to the results of the present
study. Our results on hemodynamic indicators showed that there was
no significant difference in HR, SpO2, SBP and MBP of
the patients in the two groups. Compared with the hemodynamic
indicators before the patients were anesthetized (T0),
the hemodynamic indicators decreased slightly and then increased
after the surgery was started. There was no significant difference
between the hemodynamic indicators of the patients in two groups
after surgery was finished and those before surgery. This result
indicates that the hemodynamic indicators of the patients in two
groups were stable. Khare et al (21) studied the anesthesia of laparoscopic
cholecystectomy, and found that SBP, DBP and MBP of the patients in
the propofol group decreased in different periods compared with
those in the sevoflurane group; however, there was no significant
difference between the two groups. The hemodynamic indicators of
the patients in two groups were stable. This result was similar to
the results of our study. In this study, the results on
inflammatory factors showed that there was no significant
difference between baseline inflammatory factor indicators in the
propofol group and those in the sevoflurane group. The levels of
serum inflammatory factors IL-1β, IL-6, IL-10 and TNF-α were first
increased, then decreased, and gradually returned to the
preoperative level after the surgery was finished. The levels of
IL-1β, IL-6 and IL-10 in the propofol group were lower than those
in the sevoflurane group after pneumoperitoneum was carried out for
5 min. This result indicates that the effect of propofol is better
than that of sevoflurane on reducing serum inflammatory factors. A
study on propofol or sevoflurane combined with remifentanil was
carried out by Shen et al (22) showing that the levels of serum IL-1β,
IL-6 and TNF-α in the propofol and the sevoflurane group after
surgery were significantly higher than those before surgery, and
the levels of serum IL-1β, IL-6 and TNF-α in the propofol group
were significantly lower than those in the sevoflurane group. These
results suggested that remifentanil combined with propofol could
reduce the concentration of serum inflammatory factors effectively
in accordance to the results of the present study. The MMSE
cognitive function scores showed that there was no significant
difference between MMSE cognitive function scores in the propofol
group and those in the sevoflurane group before the patients were
anesthetized. MMSE cognitive function scores in the propofol and
the sevoflurane group at 6 h after the beginning of surgery were
significantly lower than those before the anesthetization of
patients. MMSE cognitive function scores in the propofol group were
significantly higher than those in the sevoflurane group at 6 h
after the surgery was started. There was no significant difference
between MMSE cognitive function scores in the propofol and the
sevoflurane group at T5 and those before the
anesthetization of patients. This result indicates that the effect
of propofol is less than that of sevoflurane on the cognitive
function of patients with T2DM and GC. A study on effects of
propofol and sevoflurane on the cognitive function of elderly
patients (23), showed that propofol
and sevoflurane had similar effects; however, the effect of
propofol was less than that of sevoflurane on the cognitive
function. This result is similar to the results of the present
study. The results on the anesthetic effect showed that the time of
spontaneous breath, eye opening, extubation, and verbal response in
the propofol group were significantly shorter than those in the
sevoflurane group, indicating that the anesthetic effect and
analepsia quality of propofol are better than those of sevoflurane
for patients with T2DM and GC. A study has shown that compared with
general anesthesia, propofol or sevoflurane combined with epidural
block is conducive in improving the analepsia quality of elderly
patients with GC after undergoing anesthesia of radical surgeries,
increases the stability of the patients' hemodynamics and shortens
their awakening time (24). In the
present study, the results on adverse reactions showed that the
patients had adverse reactions, such as nausea, vomiting, cough and
restlessness in the propofol and the sevoflurane group. The number
of patients with nausea and vomiting in the propofol group was
significantly less than that in the sevoflurane group, and the
incidence of adverse reactions in the propofol group was
significantly lower than that in the sevoflurane group. This result
suggests that side effects of propofol might be less than those of
sevoflurane, and adverse impacts of propofol are less than those of
sevoflurane. A study on anesthetic postoperative pain was carried
out by Peng et al (25),
showing that the patients who were anesthetized with propofol
needed less postoperative rescue analgesics than that of patients
anesthetized with sevoflurane, and the execution time of
postoperative analgesia was later. This result forcefully proved
that the incidence of adverse reactions of propofol is lower than
that of sevoflurane.
This study confirmed that the effect of propofol is
less than that of sevoflurane on blood glucose, hemodynamics, and
inflammatory factors of patients with T2DM and GC and that patients
with high MMSE cognitive function scores have a good anesthetic
effect and a low incidence of adverse reactions.
In conclusion, propofol is worthy of promotion in
clinical practice for patients with T2DM and GC, and sevoflurane
can be used as a second option.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
JL and LY conceived and designed the study,
collected, analyzed and interpreted the experiment data, drafted
the manuscript, and revised it critically for important
intellectual content. Both authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
The First Affiliated Hospital of Baotou Medical College (Baotou,
China). Signed written informed consents were obtained from the
patients and/or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Venerito M, Link A, Rokkas T and
Malfertheiner P: Gastric cancer-clinical aspects (Review).
Helicobacter. 24 (Suppl 1):e126432019. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sah BR, Owczarczyk K, Siddique M, Cook GJR
and Goh V: Radiomics in esophageal and gastric cancer. Abdom Radiol
(NY). 44:2048–2058. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wang SL, Zhuang CL, Huang DD, Pang WY, Lou
N, Chen FF, Zhou CJ, Shen X and Yu Z: Sarcopenia adversely impacts
postoperative clinical outcomes following gastrectomy in patients
with gastric cancer: A prospective study. Ann Surg Oncol.
23:556–564. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Baglia ML, Cui Y, Zheng T, Yang G, Li H,
You M, Xu L, Murff H, Gao YT, Zheng W, et al: Diabetes medication
use in association with survival among patients of breast,
colorectal, lung, or gastric cancer. Cancer Res Treat. 51:538–546.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kim JH, Huh YJ, Park S, Park YS, Park DJ,
Kwon JW, Lee JH, Heo Y and Choi SH: Multicenter results of
long-limb bypass reconstruction after gastrectomy in patients with
gastric cancer and type II diabetes. Asian J Surg. May
3–2019.(E-pub ahead of print).
doi.org/10.1016/j.asjsur.2019.03.018. View Article : Google Scholar
|
|
6
|
Tseng CH and Tseng FH: Diabetes and
gastric cancer: The potential links. World J Gastroenterol.
20:1701–1711. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Charalampakis N, Economopoulou P,
Kotsantis I, Tolia M, Schizas D, Liakakos T, Elimova E, Ajani JA
and Psyrri A: Medical management of gastric cancer: A 2017 update.
Cancer Med. 7:123–133. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tuttnauer A and Levin PD: Diabetes
mellitus and anesthesia. Anesthesiol Clin. 24:579–597. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Qiu Q, Choi SW, Wong SS, Irwin MG and
Cheung CW: Effects of intra-operative maintenance of general
anaesthesia with propofol on postoperative pain outcomes - a
systematic review and meta-analysis. Anaesthesia. 71:1222–1233.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chidambaran V, Costandi A and D'Mello A:
Propofol: A review of its role in pediatric anesthesia and
sedation. CNS Drugs. 29:543–563. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fan W, Zhu X, Wu L, Wu Z, Li D, Huang F
and He H: Propofol: An anesthetic possessing neuroprotective
effects. Eur Rev Med Pharmacol Sci. 19:1520–1529. 2015.PubMed/NCBI
|
|
12
|
De Hert S and Moerman A: Sevoflurane.
F1000 Res. 4:(F1000 Faculty Rev). 6262015. View Article : Google Scholar
|
|
13
|
Kanazawa S, Oda Y, Maeda C and Okutani R:
Electroencephalo-graphic effect of age-adjusted 1 MAC desflurane
and sevoflurane in young, middle-aged, and elderly patients. J
Anesth. 31:744–750. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Xu Z, Yu J, Wu J, Qi F, Wang H and Wang Z
and Wang Z: The effects of two anesthetics, propofol and
sevoflurane, on liver ischemia/reperfusion injury. Cell Physiol
Biochem. 38:1631–1642. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zheng X, Wang Y, Dong L, Zhao S, Wang L,
Chen H, Xu Y and Wang G: Effects of propofol-based total
intravenous anesthesia on gastric cancer: A retrospective study.
OncoTargets Ther. 11:1141–1148. 2018. View Article : Google Scholar
|
|
16
|
Baynes HW: Classification,
pathophysiology, diagnosis and management of diabetes mellitus. J
Diabetes Metab. 6:1–9. 2015.
|
|
17
|
Smyth EC, Verheij M, Allum W, Cunningham
D, Cervantes A and Arnold D; ESMO Guidelines Committee, : Gastric
cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment
and follow-up. Ann Oncol. 27 (Suppl 5):V38–V49. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Doyle DJ and Garmon EH: American Society
of Anesthesiologists Classification (ASA Class) [Updated 2019 May
13]. StatPearls [Internet] Treasure Island (FL): StatPearls
Publishing; 2019
|
|
19
|
Mitchell AJ: The Mini-Mental State
Examination (MMSE): Update on its diagnostic accuracy and clinical
utility for cognitive disorders. Cognitive Screening Instruments.
Larner AJ: 2nd. Springer International Publishing; Switzerland: pp.
37–48. 2017, View Article : Google Scholar
|
|
20
|
Kitamura T, Kawamura G and Ogawa Mand
Yamada Y: Comparison of the changes in blood glucose levels during
anesthetic management using sevoflurane and propofol. Masui.
58:81–84. 2009.(In Japanese). PubMed/NCBI
|
|
21
|
Khare A, Mathur V, Jain K, Sethi S, Garg D
and Vishnoi R: A prospective randomized study for comparison of
haemodynamic changes and recovery characteristics with propofol and
sevoflurane anaesthesia during laparoscopic cholecystectomies. Int
J Res Med Sci. 4:5241–5247. 2016. View Article : Google Scholar
|
|
22
|
Shen Q, Peng J, Shi Y and Yang LL: Effects
of remifentanil combined with propofol anesthesia on IL-1β, IL-6,
TNF-α and hemodynamics in patients with brain surgery. J Hain Med
Univ. 23:61–64. 2017.
|
|
23
|
Yu W: Anesthesia with propofol and
sevoflurane on postoperative cognitive function of elderly patients
undergoing general thoracic surgery. Pak J Pharm Sci.
30:(3(Special)). 1107–1110. 2017.PubMed/NCBI
|
|
24
|
Zhang L, Chen C, Wang L, Cheng G, Wu WW
and Li YH: Awakening from anesthesia using propofol or sevoflurane
with epidural block in radical surgery for senile gastric cancer.
Int J Clin Exp Med. 8:19412–19417. 2015.PubMed/NCBI
|
|
25
|
Peng K, Liu HY, Wu SR, Liu H, Zhang ZC and
Ji FH: Does propofol anesthesia lead to less postoperative pain
compared with inhalational anesthesia?: A systematic review and
meta-analysis. Anesth Analg. 123:846–858. 2016. View Article : Google Scholar : PubMed/NCBI
|