Introduction
Angiogenesis is a key factor associated with the
development of solid tumors, being required to provide adequate
nutrition and prompt waste disposal in the tumor microenvironment.
Angiogenesis may also serve a role in the shedding of neoplastic
cells in the initial stage of metastasis (1). The idea that anti-angiogenic therapies
may be used to repress the supply of nutrients and oxygen in order
to starve tumor cells and reduce metastasis was first reported by
Folkman (1), who proposed the novel
theory of inhibiting tumorigenesis via an anti-angiogenic approach.
However, attempts to de-vascularize tumors may result in the
exacerbation of hypoxia and acidosis within the tumor
microenvironment (1,2), an event which reportedly enhances
chemoresistance (3,4), reduces the efficacy of radiotherapy
(5,6), increases tumor cell malignancy and
promotes metastasis (2,7,8).
Considering these issues, Jain (9)
proposed that the tumor vasculature undergoes a transition from an
abnormal to normal state following anti-angiogenic therapy, which
may improve blood vessel structure and function. Therefore,
treatment with anti-angiogenic therapy may reduce the hypoxic
regions within tumors and increase tumor perfusion (9,11). This
may allow enhanced delivery of cytotoxic agents to the tumor via
improved blood vessel structure and function, improving the
efficacy of radiotherapy (3–7,10,11).
However, the period in which the tumor vasculature
becomes normalized is transient; this ‘time window’ may be
associated with the balance of anti-angiogenic and pro-angiogenic
factor activation, which affects drug resistance (9,11). Thus,
identifying the duration of tumor vasculature normalization is
crucial. In addition, patients can demonstrate varying
sensitivities to anti-angiogenic therapies, and some patients may
experience severe side effects, including hemorrhage and
thromboembolism (12). Therefore,
identifying biomarkers associated with vasculature normalization
may prove useful in the determination of which patients may benefit
from anti-angiogenic therapy, as well as in the optimization of
treatment with anti-tumor therapies (12).
Several studies have investigated the application of
the biomarkers associated with anti-angiogenic therapy: Schneider
et al (13) suggested that
vascular endothelial growth factor (VEGF)/VEGF receptor 2 (VEGFR2)
genotypes may be used to predict the therapeutic efficacy and
toxicity of bevacizumab in patients with advanced breast cancer. In
addition, findings have suggested that soluble VEGFR1 (also known
as sFlt1), which inhibits VEGF activity, may be a promising
biomarker of vascular normalization (14). However, these effects do not appear
to be associated with solid tumor vasculature normalization, which
is characterized by decreased regions of hypoxia and decreased
interstitial fluid pressure (IFP) (9,14). The
IFP of tumors can be monitored; however, a tissue puncture
examination cannot be performed, as this may promote the metastasis
of tumor cells. Recently, Lassau et al (15) used dynamic contrast enhanced
ultrasonography to observe tumor vascular normalization. This
method appeared to be suitable for clinical use for measuring the
degree of tumor blood perfusion over time.
Thrombospondin-1 (TSP-1) was the first characterized
endogenous angiogenesis inhibitor, which induces the apoptosis and
inhibits the migration of endothelial cells by binding to cluster
of differentiation (CD)36 and CD148 (16–18).
Metronomic chemotherapy can upregulate TSP-1 expression and
maintain the balance between pro- and anti-angiogenic factors; and
thus tumor vasculature normalization may be induced (19). Firlej et al (20) reported that high expression of TSP-1
in prostate cancer may inhibit angiogenesis; however, tumor
progression may be promoted. A major concern is that
anti-angiogenic therapies could excessively aggravate hypoxia and
stimulate the migration of cancer cells (2). It has been reported that hypoxia
modifies calcium homeostasis in prostate carcinoma C4-2 cells and
may also induce the expression of TSP-1 (20). Tumor vasculature normalization may
create a transient condition that alleviates hypoxia (9). Thus, TSP-1 expression levels in the
blood may be used to monitor the vascular normalization ‘time
window’. In the present study, recombinant human endostatin (rhES)
was employed as an anti-angiogenic agent to evaluate the
association between TSP-1 expression levels and tumor vascular
normalization.
Materials and methods
Cell isolation and culture
The colon carcinoma cell line SW620 was purchased
from the Cell Bank of Type Culture Collection of Chinese Academy of
Sciences (Shanghai, China) and was cultured in Dulbecco's modified
Eagle's medium at 37°C in 5% CO2. (Gibco; Thermo Fisher
Scientific, Inc., Waltham, MA, USA) supplemented with 10% fetal
bovine serum (Gibco; Thermo Fisher Scientific, Inc.) and 100 U/ml
penicillin-streptomycin.
Animal care and tumor
establishment
The present study was approved by the Laboratory
Animal Ethics Committee of Jinan University (Guangzhou, China).
Female BALB/c (nu/nu) mice (n=40; 4 weeks-old; mean body weight,
18.0±2.0 g) were obtained from Beijing HFK Bioscience Co., Ltd.
(Beijing, China), and were maintained under specific pathogen-free
conditions with food and water provided ad libitum. The
institutional laboratory housing temperature was maintained between
23 and 25°C and the relative humidity was maintained between 45 and
60% with a 12-h light/dark cycle. Prior to implantation of
tumorigenic cells, blood was obtained from the corner of the eye of
all mice, with 50–100 µl obtained each time to determine the basal
expression levels of TSP-1. Xenograft tumors were generated via
subcutaneous injection of SW620 cells (3×106
cells/mouse) into the right flank. Tumor size was measured daily
using Vernier calipers, and the volume (V) was calculated as
follows: V=(length × width2) ×0.523. Treatment with rhES
[5 mg/kg, diluted with normal saline (NS) to a final volume of 150
µl; n=20] was applied via an intraperitoneal injection when the
tumor size ranged between 100–150 mm3. The same volume
of NS was injected as a control (n=20). Reagents were administered
continuously for 4 days, and then every 2 days by single
injections. Tumor tissues were collected on days 0, 2, 4, 6 and 12
and the extent of tumor vascular normalization was determined.
Hypoxia inducible factor
(HIF)-1α/TSP-1 detection
Tumor samples (100 µg) were ground using a tissue
grinder, then centrifuged at 14,000 × g for 30 min at 4°C and the
expression levels of HIF-1α were detected by western blotting. The
levels of mouse TSP-1 in the serum were quantified using an ELISA
kit (Abcam, Cambridge, UK) according to the manufacturer's
protocol, plasma TSP-1 detection was performed 7 days before tumor
implantation, on the day of tumor implantation, and 2, 4, 6, 9 and
12 days after tumor implantation.
Immunohistochemical analysis
Tissues were fixed in 4% paraformaldehyde at room
temperature for 24 h and then paraffin-embedded, slices were
sectioned 6 µm thick, deparaffinized in xylene for 10 min, and
rehydrated via a graded alcohol gradient (100, 85 and 75%) and
ddH2O, each for 5 min. Samples were then subjected to
antigen retrieval at 95°C using citric acid buffer (pH 6.0).
Sections were incubated with a solution of 3%
H2O2 in methanol for 30 min, and rinsed twice
with tris-buffered saline (TBS; 5 min per rinse). Subsequently,
sections were blocked in 5% normal goat serum (Beyotime Institute
of Biotechnology, Haimen, China) in TBS for 1 h at room
temperature. The sections were then incubated with mouse monoclonal
anti-pimonidazole antibody (1:50; HP1-200; Hypoxyprobe, Burlington,
MA, USA) in TBS at 4°C overnight. Sections were washed by TBS as
aforementioned, then incubated with biotin-conjugated anti-mouse
secondary antibody (1:200; A0286; Beyotime Institute of
Biotechnology, Haimen, China) in TBS for 1 h at room temperature.
Following rinsing, streptavidin-peroxidase was applied for 15 min
at room temperature; the sections were developed with the chromogen
3,3′-diaminobenzidine at room temperature. The sections were
dehydrated with graded alcohol (75, 85 and 100%) for 5 min,
transferred to xylene for 5 min and then air dried for 30 min prior
to mounting. Images were obtained using a Leica DM6000B microscope
(Leica Microsystems GmbH, Wetzlar, Germany).
Immunofluorescence analysis
Tissues were fixed, paraffin- embedded, sectioned,
dewaxed, rehydrated and subjected to antigen retrieval as
aforementioned. The sections were blocked in 2% normal goat serum
for 1 h and stained with the following primary antibodies:
Anti-CD31 (1:500; ab28364, Abcam) and anti-α-smooth muscle actin
(α-SMA; 1:100; 14395-1-AP, Proteintech Group Inc., Rosemont, IL,
USA), for labeling of the endothelium and pericytes, respectively.
The sections were then washed with TBS and incubated with
rhodamine-conjugated goat anti-rat immunoglobulin (Ig)G (H+L)
antibody (1:50; SA00007-7, Proteintech) or goat anti-rabbit
IgG-fluorescein isothiocyanate antibody (1:200; sc-2012, Santa Cruz
Biotechnology, Inc., Dallas, TX, USA) for 40 min at room
temperature. The degree of pericyte detection was presented as a
percentage of the length along CD31+ vessels.
Hematoxylin and eosin staining
The initial processing steps were the performed as
aforementioned. Slides were flamed and immersed in xylene for 15
min, which was then repeated prior to hydrating the tissue sections
via a decreasing series of graded alcohol (100, 90, 80 and 70%) and
water. The sections were stained in hematoxylin for 5 min at room
temperature, and then washed in running tap water for 5 min. The
slides were placed in 1% acid alcohol (1% HCl in 70% alcohol) for 3
min, and washed in running tap water. The slides were then stained
in 1% eosin Y for 5 min at room temperature and washed in tap water
for 1–5 min, then dehydrated in increasing concentrations of
alcohol (75, 85 and 100%) and cleared in xylene. Sections were cut
into 6 µm, and then examined under a light microscope (Leica
DM6000B) at ×20 magnification. Necrotic regions were determined
using ImageJ software (version 1.49; National Institutes of Health,
Bethesda, MA, USA).
Western blotting
For western blot analysis, cells or flesh tissues
were lysed on ice using PIPA buffer (P0013B; Beyotime Institute of
Biotechnology, Haimen, Chain) supplemented with PMSF (ST506,
Beyotime, Haimen, China). Concentrations were determined using a
BCA protein assay kit (P0010S; Beyotime Institute of Biotechnology,
Haimen, China). Proteins were loaded at a mass of 30 µg per lane
were separated via SDS-PAGE (10% gel) and transferred to
polyvinylidene difluoride membranes, which were blocked with a
blocking solution (5% bovine serum albumin and 0.1% Tween 20 in
TBS; Beyotime Institute Biotechnology) for 1 h at room temperature.
Subsequently, the membrane was incubated with anti-HIF-1α primary
antibodies (1:2,000; ab187524; Abcam) overnight at 4°C, followed by
incubation with horseradish peroxidase-conjugated secondary
antibodies (1:2,000; 31460; Thermo Fisher Scientific, Inc.). The
bands were visualized using an enhanced chemiluminescence detection
system (ChemiDoc XRS; Bio-Rad Laboratories, Inc., Hercules, CA,
USA) and were quantified using Quantity One software (version 4.6;
Bio-Rad Laboratories, Inc.).
Detection of hypoxia in tumors
For the detection of hypoxia, mice were divided into
two groups, the control mice (n=20) were treated with PBS, and the
treatment mice (n=20) were treated with Endostar. Following
treatment, each mouse was injected intraperitoneally with 60 mg/kg
pimonidazole (Hypoxyprobe). After 1 h, tumor samples were
collected, frozen in liquid nitrogen and cryosectioned into 10-µm
sections, and immunohistochemical analysis was performed as
above.
In vitro cell viability assays
The viability of SW620 cells was measured using a
Cell Counting Kit-8 (CCK-8; Dojindo Molecular Technologies, Inc.,
Kumamoto, Japan). Briefly, cells were seeded in 96-well plates
(104 cells per well) and treated with Endostar (0, 25 50
and 100 ug/ml) or PBS for 24 h at 37°C in 5% CO2. CCK-8
reagent (10 µl) was added to each well, and the plates were
incubated at 37°C in 5% CO2 for another 2 h. Absorbance
was measured at 450 nm using a microplate reader (BioTek
Instruments, Inc., Winooski, VT, USA).
Statistical analysis
Data were presented as the mean ± standard error of
the mean. Different groups were compared by one-way analysis of
variance with Bonferroni post-hoc test or unpaired Student's
t-tests. Statistical analyses were performed using GraphPad Prism
5.0 software (GraphPad Software, Inc., La Jolla, CA, USA). Each
experiment was conducted at least three times. P<0.05 was
considered to indicate a statistically significant difference.
Results
Short-term rhES treatment induces a
‘time window’ of tumor vascular normalization
The ‘time window’ of tumor vascular normalization
has been suggested to occur on days 4 to 6 following
anti-angiogenic treatment; in most cases, maximum tumor vascular
normalization occurred on day 7 (15,21). To
examine the association between TSP-1 expression and vascular
normalization, the vascular appearance, including the density and
coverage of pericytes, in a SW620 ×enograft tumor model was
dynamically monitored. CD31 was used as a biomarker of vascular
endothelial cells to detect alterations in vascular morphology and
vessel density. The results of immunofluorescence staining
demonstrated that vessel density significantly increased by day 12
compared with day 0 in the control group (P<0.05). In
rhES-treated mice, the vessel density was significantly decreased
at day 4 (P<0.05) and low vessel density persisted until day 6
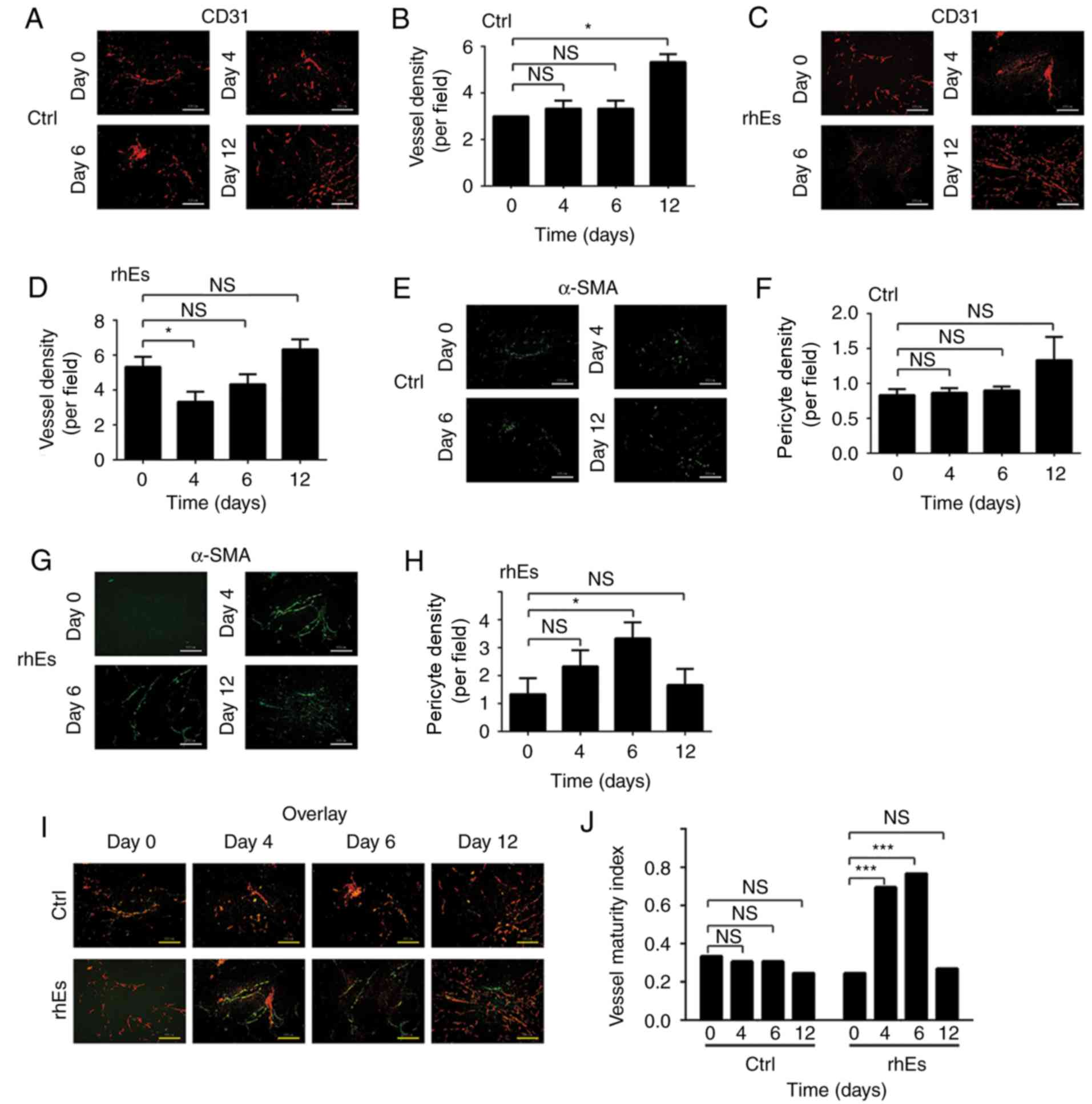
(Fig. 1A-D).
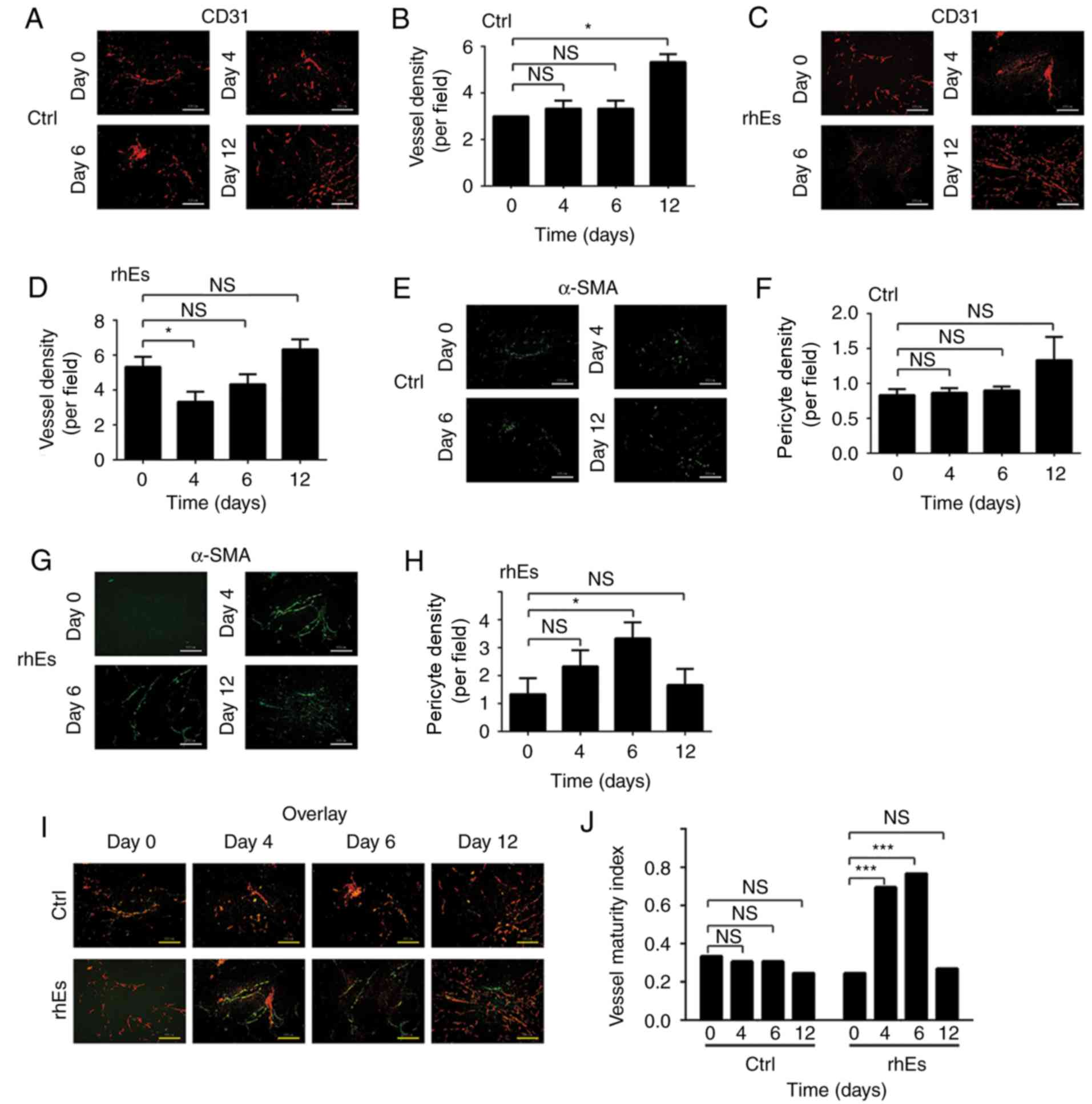 | Figure 1.(A-J) rhES-induced tumor vasculature
normalization in SW620-bearing mice. (A and C) Immunofluorescence
for CD31 (red). Scale bar, 100 µm. Representative images of SW620
tumor sections from (A) control and (C) rhES-treated groups (after
0, 4, 6 and 12 days, n=20. (B and D) Quantification of vessel
density. (B) A significant increase in vessel density was observed
on day 12 in the control group. (D) A significant decrease at day 4
was observed in the rhES-treated group. (E and G)
Immunofluorescence for α-SMA (green) in tumors of the (E) control
and (G) rhES-treated groups (after 0, 4, 6 and 12 days, n=20. Scale
bar, 100 µm. (F and H) Quantification of pericytes of vessels
marked by α-SMA. (F) No differences in pericyte coverage was
observed in the control group. (H) A significant increase at day 6
was observed in the rhES-treated group. (I) Overlay of (A and E)
and (C and G). Vessel maturity index was determined as the ratio of
α-SMA-positive to CD31-positive areas. (J) There were no
differences in the vessel maturity index among days 0–12 in the
control group. A significant increase in the vessel maturity index
of rhES-treated tumors was observed at days 4 and 6, but was
restored by day 12. All quantitative data are presented as the mean
± standard error of the mean. *P<0.05; ***P<0.001. CD,
cluster of differentiation; rhES, recombinant human endostatin;
α-SMA, α-smooth muscle actin; Ctrl, control; NS, not
significant. |
Pericytes surround the vascular endothelium and are
often used as an indicator of blood vessel function and integrity,
and can be detected via α-SMA expression (22). The present study observed that the
pericyte coverage of tumor vessels was increased in the
rhES-treated group, particularly at day 6 (P<0.05), while there
were no significant differences in control mice (Fig. 1E-H). Collectively, these data
indicated that anti-angiogenic treatment using rhES may facilitate
a transient vascular normalization ‘time window’ that occurs
approximately between day 4 and 6 following treatment. The ratio of
α-SMA-positive to CD31-positive areas has often been used to
identify the vessel maturity index (11,22).
Analysis of vascular maturity (an important indicator of tumor
vessel integrity) in the present study revealed that maturity
significantly increased at days 4 and 6 in rhES-treated mice,
compared with day 0 (P<0.001), while control mice exhibited no
significant difference. These results suggested that rhES may
transiently normalize tumor vessels; however, the maturity appeared
to reverse to baseline at day 12. This may potentially be due to
the continuous use of rhES resulting in abnormal vessel development
by subsequent over-pruning (Fig. 1I and
J).
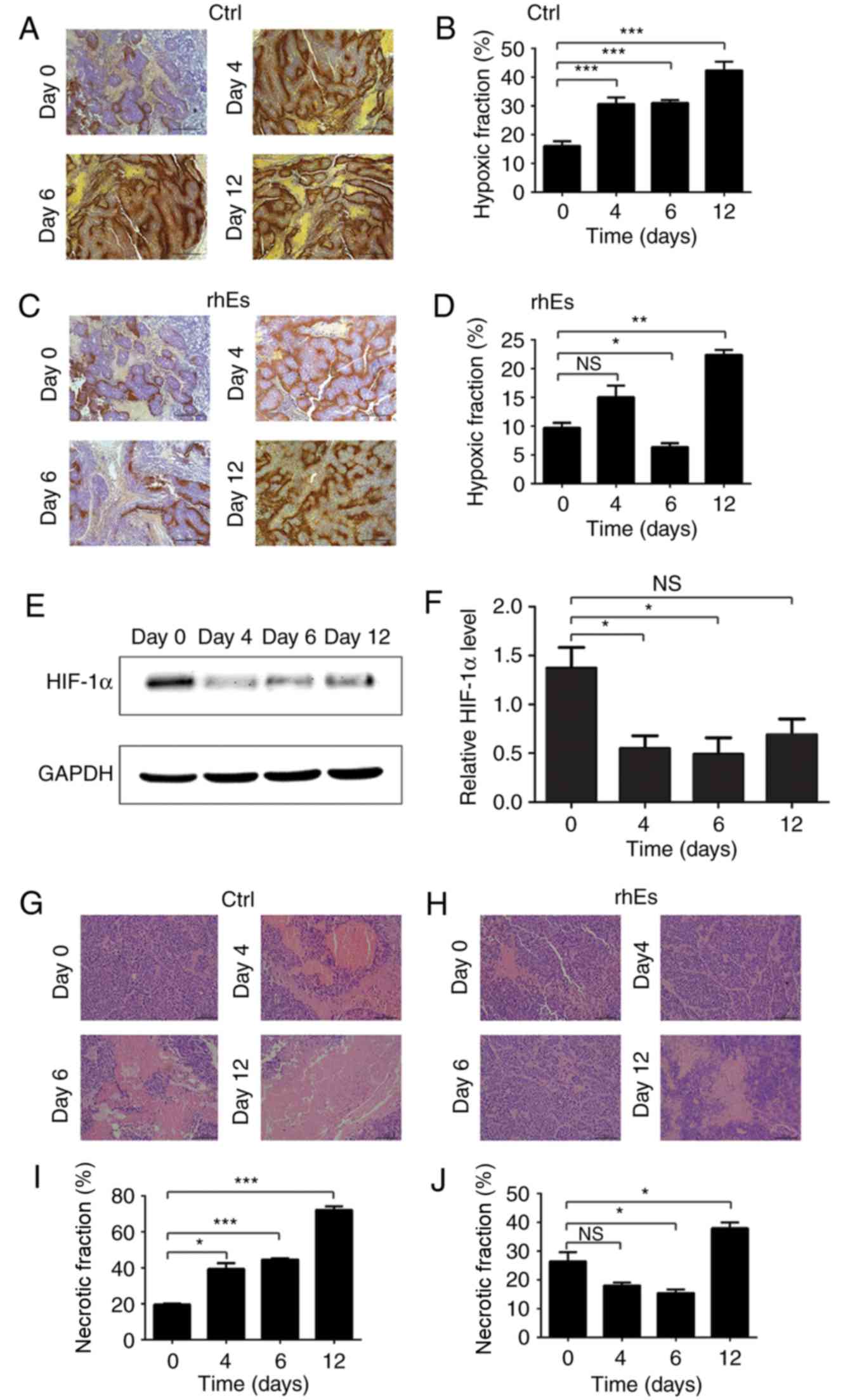
Tumor tissue exhibits reduced hypoxia
during the ‘time window’ of tumor vascular normalization
Rapid growth of solid tumors is often accompanied by
hypoxia, which increases the degree of malignancy and reduces the
efficacy of therapy (9). The
remission of hypoxia is an additional feature of tumor vascular
normalization (9,21), and therefore reductions in hypoxia
may be applied in the prediction of the ‘time window’ associated
with tumor vascular normalization. To evaluate the oxygen supply,
the present study analyzed the pimonidazole staining patterns in
tumors. The results revealed that the extent of hypoxia was
significantly decreased at 6 days after treatment with rhES
(P<0.05); however, it was observed that hypoxia was increased
again after 12 days. (P<0.01; Fig. 2A
and B). This indicated that the tumor vessels were no longer
normalized at day 12. To further detect the recovery of oxygen in
tumors, HIF-1α levels in tumor sections were analyzed by western
blot analysis. Compared with the expression levels at day 0,
significant downregulation of HIF-1α was observed on days 4 and 6
(P<0.05), while no difference was observed on day 12 (Fig. 2E and F). In addition, the necrotic
areas of tumor sections were analyzed, since this is established to
be associated with hypoxia (Fig.
2G-J). The necrotic area increased continuously in control mice
over the 12 day observation period; meanwhile, in the rhES
treatment group, a significant decrease at day 6, but an increase
at day 12 was observed (both P<0.05), which appeared associated
with the levels of hypoxia induction. Collectively, these results
demonstrated that the reduction in hypoxia may be temporary, and
the duration of reduced hypoxia may coincide with the suggested
‘time window’.
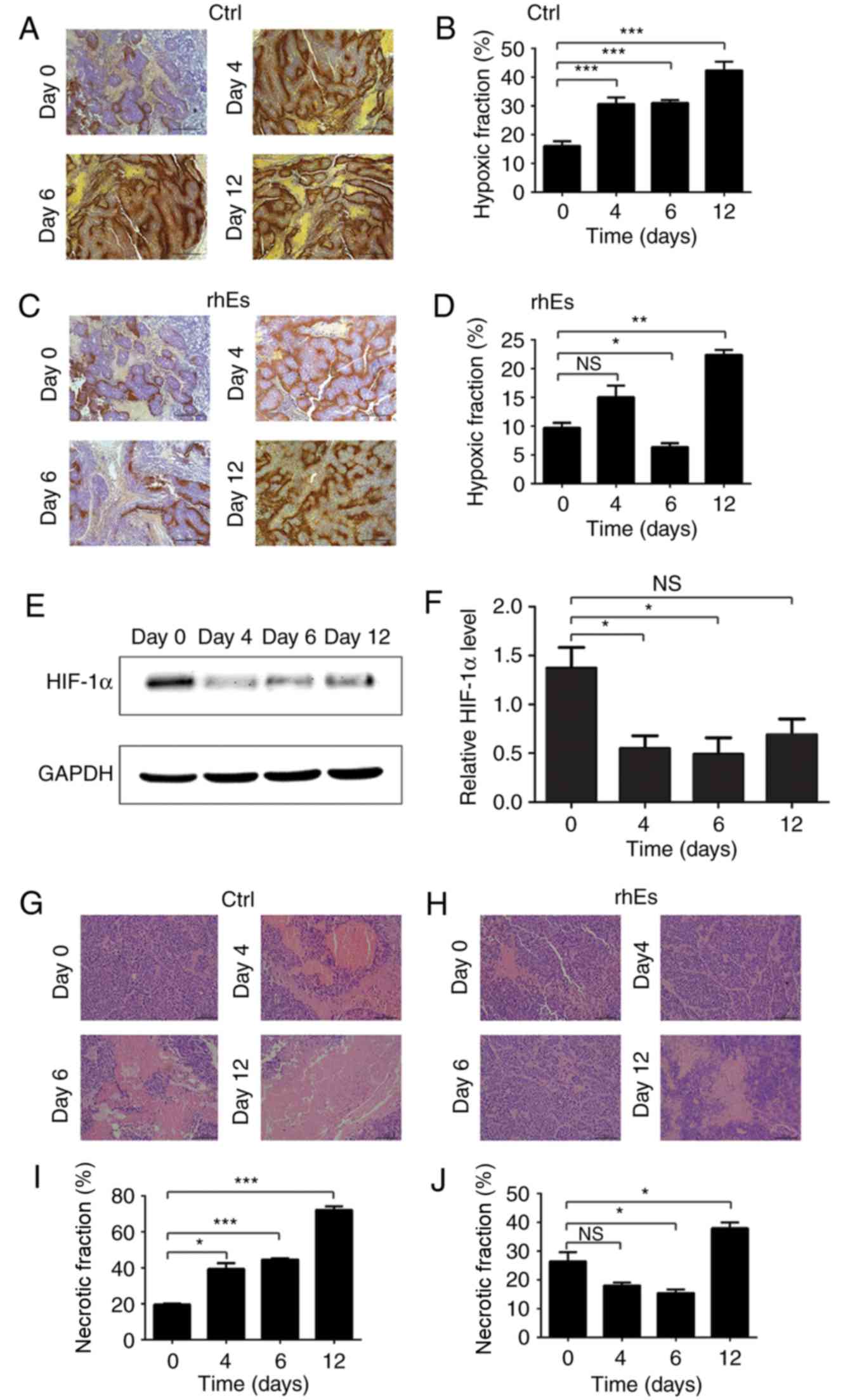 | Figure 2.Decrease in tumor hypoxia during
tumor vasculature normalization. Tumor tissue from mice bearing
primary xenograft tumors were collected, and pimonidazole staining
of the tumor tissue was conducted to indicate the hypoxic tissue.
(A and C) Hypoxia marker staining by pimonidazole (brown) in
sections from (A) control mice (after 0, 4, 6 and 12 days; n=20 and
(C) rhES-treated mice (after 0, 4, 6 and 12 days; n=20). Scale bar,
500 µm. (B and D) Quantification of pimonidazole-positive areas as
a percentage of the whole tumor area. (B) Within the control mice,
the hypoxic areas increased significantly at days 4, 6 and 12. (D)
Hypoxia was significantly decreased at day 6, but increased at day
12 in the rhES-treated mice. (E) HIF-1α expression in the tumor
sections of rhES-treated mice was significantly decreased at days 4
and 6, indicating reductions in tumor hypoxia; (F) no significant
change in HIF-1α expression was detected at day 12. (G and H)
Necrotic areas in tumors of the (G) control and (H) rhES-treated
mice (after 0, 4, 6 and 12 days; hematoxylin and eosin staining).
Scale bar, 100 µm. (I and J) Percentage of necrosis of the whole
tumor area. (I) Necrosis was significantly increased at days 4, 6
and 12 in control mice. (J) Necrosis was significantly decreased at
day 6, but significantly increased at day 12 in rhES-treated mice
(J). All quantitative data are presented as the mean ± standard
error of the mean. *P<0.05; **P<0.01; ***P<0.001. HIF-1α,
hypoxia inducible factor-1α; rhES, rhES, recombinant human
endostatin; Ctrl, control; NS, not significant. |
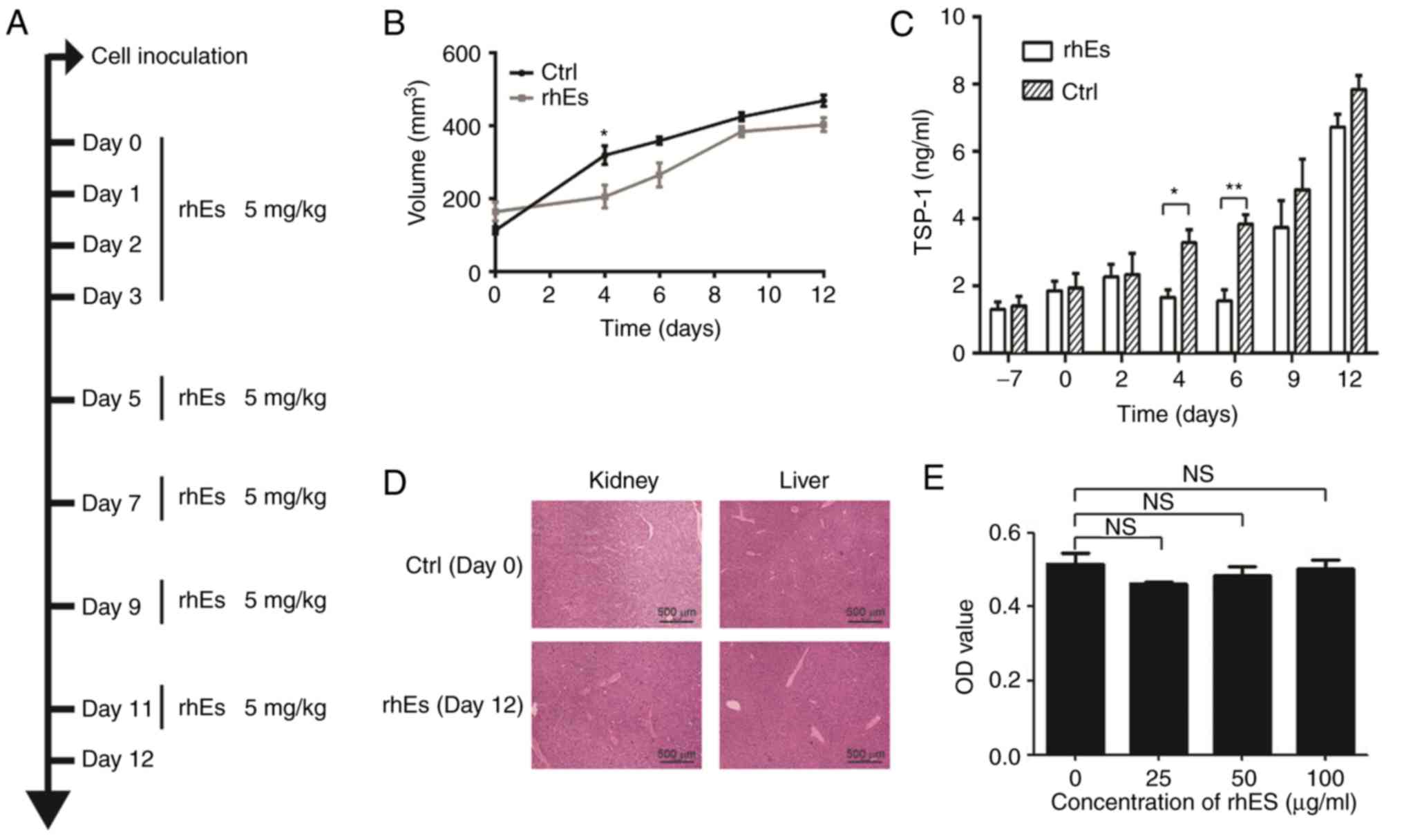
Consistent with the
‘abnormal-normal-abnormal’ transformation of tumor vasculature,
plasma TSP-1 expression levels fluctuate dynamically
The present study hypothesized that the oxygen
content available to tumors is associated with the tumor vascular
normalization ‘time window’, the analysis of hypoxia may
theoretically indicate alterations in the duration of the window.
However, current methods to detect tumor hypoxia are not readily
applicable in the clinic. Therefore, the present study aimed to
identify an effective biomarker of the tumor vascular normalization
‘time window’ based on secreted factors in the blood plasma.
TSP-1 is an endogenous anti-angiogenic factor
associated with hypoxia. Therefore, the present study investigated
whether tumor vascular normalization may induce corresponding
alterations in the levels of TSP-1 in the plasma. First, rhES was
applied to induce tumor vasculature normalization. To eliminate the
effect of rhES itself on plasma TSP-1, the drug was used
continuously (Fig. 3A), which may
generate abnormal tumor vasculature due to over-pruning. The tumor
volumes did not differ significantly between the control and
rhES-treated mice, except on day 4, which suggested that
angiogenesis may have been controlled (Fig. 3B).
Following treatment with rhES, the levels of TSP-1
in the plasma gradually decreased from day 2 to 6, after which
TSP-1 level exhibited a gradual increasing trend (Fig. 3C). This trend was consistent with the
amelioration of the morphological characteristics of blood vessels;
pericytes of vessels were increased, vessel density was decreased,
and the improvements in tumor hypoxia observed in our previous
experiments, the most direct effect of hypoxia improvement was that
the area of hypoxia necrosis in tumor tissue was decreased
(8,9). Conversely, TSP-1 levels in the control
samples increased during the observation period. In addition,
structural alterations in the morphology of the liver and kidney
were not observed during treatment with rhES, indicating that rhES
may not affect the expression of TSP-1 in other organs (Fig. 3D). Meanwhile, the in vitro
cell viability assays demonstrated that rhES only minimally
affected SW620 cell proliferation, which suggested that rhES may
not notably affect the secretion of TSP-1 by SW620 cells (Fig. 3E). Therefore, alterations in TSP-1
levels may indicate the duration of tumor vasculature
normalization, which may be associated with alleviations in
hypoxia.
Discussion
Solid tumors receive nutrients and oxygen via
pervasive abnormal blood vessels, which leads to hypoxia and
increased interstitial fluid pressure (IFP) in the tumor stroma
(1,23,24).
These events increase the degree of malignancy, and the risk of
invasion and metastasis (25); the
efficacy of radiotherapy and chemotherapy is also reduced.
Normalization of the tumor vasculature via anti-angiogenic therapy
can reduce hypoxia and decrease the degree of IFP (26), which may enhance the effects of
traditional anti-cancer therapies (27–30).
Unfortunately, the tumor vascular normalization ‘time window’ is
transient, and patients with various types of tumors may exhibit
variations in their respective window (31). Therefore, identifying a readily
detected and representative biomarker to analyze the ‘time window’
may be critical in the application of anti-cancer treatment. The
findings of the present study suggested that plasma TSP-1 levels
following anti-angiogenic treatment may be used as an indicator of
the progression of tumor vasculature normalization.
TSP-1 is a glycoprotein secreted from platelets and
was the first identified endogenous protein inhibitor of
angiogenesis (16,23). TSP-1 has an in vivo half-life
of ~9 h (24), which is beneficial
for an endogenous marker. Hypoxia has been reported to increase the
secretion of TSP-1 (25) and promote
angiogenesis in tumors (32,33). The present study suggested that as
tumor hypoxia decreases, the expression levels of TSP-1 in the
plasma may change accordingly. Notably, it was demonstrated that
plasma TSP-1 expression levels decreased from day 4 to day 6
following treatment with rhES; these levels returned to those of
the control group from day 9. Alterations in the levels of TSP-1
were accompanied by changes in vascular morphology, which exhibited
features of normalization. In accordance with these changes, HIF-1α
expression in the tumor tissue reflected a decrease in hypoxia.
Additionally, the control and rhES-treated groups exhibited gradual
increases in the expression of TSP-1, which was accompanied with
increases in tumor volume under hypoxia. However, plasma levels of
TSP-1 fluctuated in the rhES-treated group but not in the control
mice. RhES, a vascular angiogenesis-disrupting agent, has been
reported to exhibit anti-tumor effects following treatment for 3
weeks (34). However, in the present
study, tumor volumes overall lacked significant differences between
the control- and rhES-treated mice. This may be due to the short
duration of the <1 week of induction of tumor vasculature
normalization by rhES.
To further investigate the inhibitory effects of
rhES on TSP-1 expression in vivo, continuous administration
of treatment was conducted in the present study. This method of
treatment may have produced effective decreases in hypoxia during
the ‘time window’ and increased hypoxia in areas where tumor
vessels were excessively depleted. Under these circumstances,
dynamic alterations in TSP-1 expression levels were observed.
Furthermore, it was observed that rhES did not notably affect the
proliferation of SW620 cells and did not alter the structure of
other organs. This suggested that the reduction in TSP-1 expression
levels may be due to a negative feedback mechanism following
increased oxygen content, which improved during vascular
normalization, rather than inhibiting cell proliferation or via
other underlying mechanisms.
Tissue puncture examinations can measure changes in
IFP for analysis of the ‘time window’; however, tissue puncture can
cause damage to the body, restricting the use of this method.
Furthermore, advanced ‘vasculature’ MRI techniques may be used to
evaluate the structural and functional parameters of blood vessels
over time, a possibility that has been researched previously
(35). Once identified, the
anti-angiogenic ‘time window’, the time from the initiation of
tumor vasculature normalization to the end, may be applied in the
design of concomitant chemotherapy or radiotherapy regimens to
enhance therapeutic effects, avoid unnecessary drug toxicities, and
possibly reduce costs. Furthermore, this information may provide an
opportunity to identify patients who may be sensitive to
anti-angiogenic drugs, but not to mass medication. In the present
study, tumor vasculature normalization was investigated via the
analysis of TSP-1 levels, a readily detected factor that circulates
in the blood.
In conclusion, TSP-1 expression increased in
response to hypoxia, but decreased when hypoxia was alleviated in
the ‘time window’ of tumor vasculature normalization, induced by
rhES treatment in SW620-xenograft mice. However, whether the ‘time
window’ induced by other anti-angiogenic drugs, including
bevacizumab and cediranib, may be associated with TSP-1 levels
requires further investigation. In addition, the efficacy of TSP-1
expression as a biomarker of the ‘time window’ for a variety of
anti-angiogenic drugs in the clinic should be validated in the
future.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant no. 81472849), the
Guangdong Natural Science Research (grant no. 2014A030313383) and
the Guangdong High-level University Construction Fund for Jinan
University (grant no. 88016013034).
Availability of data and materials
The datasets used and analyzed during the present
study are available from the corresponding author upon reasonable
request.
Authors' contributions
WY and YP conceived the study and wrote the
manuscript. WY, FP and WL collected and analyzed the primary data.
XY, XZ and LQ provided technical support with the experiments,
revised the manuscript and gave final approval of the version to be
published. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The research was approved by the Laboratory Animal
Ethics Committee of Jinan University (Guangzhou, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Folkman J: Tumor angiogenesis: Therapeutic
implications. N Engl J Med. 285:1182–1186. 1971. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rupaimoole R, Ivan C, Yang D, Gharpure KM,
Wu SY, Pecot CV, Previs RA, Nagaraja AS, Armaiz-Pena GN, McGuire M,
et al: Hypoxia-upregulated microRNA-630 targets Dicer, leading to
increased tumor progression. Oncogene. 35:4312–4320. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Adapala RK, Thoppil RJ, Ghosh K, Cappelli
HC, Dudley AC, Paruchuri S, Keshamouni V, Klagsbrun M, Meszaros JG,
Chilian WM, et al: Activation of mechanosensitive ion channel TRPV4
normalizes tumor vasculature and improves cancer therapy. Oncogene.
35:314–322. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Shin DH, Choi YJ and Park JW: SIRT1 and
AMPK mediate hypoxia-induced resistance of non-small cell lung
cancers to cisplatin and doxorubicin. Cancer Res. 74:298–308. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sen A, Capitano ML, Spernyak JA,
Schueckler JT, Thomas S, Singh AK, Evans SS, Hylander BL and
Repasky EA: Mild elevation of body temperature reduces tumor
interstitial fluid pressure and hypoxia and enhances efficacy of
radiotherapy in murine tumor models. Cancer Res. 71:3872–3880.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ashton TM, Fokas E, Kunz-Schughart LA,
Folkes LK, Anbalagan S, Huether M, Kelly CJ, Pirovano G, Buffa FM,
Hammond EM, et al: The anti-malarial atovaquone increases
radiosensitivity by alleviating tumour hypoxia. Nat Commun.
7:123082016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Meijer TW, Kaanders JH, Span PN and
Bussink J: Targeting hypoxia, HIF-1, and tumor glucose metabolism
to improve radiotherapy efficacy. Clin Cancer Res. 18:5585–5594.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhang HM, Ren Y, Tang XJ, Wang K, Liu Y,
Zhang L, Li X, Liu P, Zhao C and He J: Vascular normalization
induced by sinomenine hydrochloride results in suppressed mammary
tumor growth and metastasis. Sci Rep. 5:88882015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jain RK: Normalizing tumor vasculature
with anti-angiogenic therapy: A new paradigm for combination
therapy. Nat Med. 7:987–989. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chatterjee S, Wieczorek C, Schöttle J,
Siobal M, Hinze Y, Franz T, Florin A, Adamczak J, Heukamp LC,
Neumaier B and Ullrich RT: Transient antiangiogenic treatment
improves delivery of cytotoxic compounds and therapeutic outcome in
lung cancer. Cancer Res. 74:2816–2824. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ader I, Gstalder C, Bouquerel P, Golzio M,
Andrieu G, Zalvidea S, Richard S, Sabbadini RA, Malavaud B and
Cuvillier O: Neutralizing S1P inhibits intratumoral hypoxia,
induces vascular remodelling and sensitizes to chemotherapy in
prostate cancer. Oncotarget. 6:13803–13821. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Goel S, Duda DG, Xu L, Munn LL, Boucher Y,
Fukumura D and Jain RK: Normalization of the vasculature for
treatment of cancer and other diseases. Physiol Rev. 91:1071–1121.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Schneider BP, Wang M, Radovich M, Sledge
GW, Badve S, Thor A, Flockhart DA, Hancock B, Davidson N, Gralow J,
et al: Association of vascular endothelial growth factor and
vascular endothelial growth factor receptor-2 genetic polymorphisms
with outcome in a trial of paclitaxel compared with paclitaxel plus
bevacizumab in advanced breast cancer: ECOG 2100. J Clin Oncol.
26:4672–4678. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Schneider Duda DG, Willett CG, Ancukiewicz
M, di Tomaso E, Shah M, Czito BG, Bentley R, Poleski M, Lauwers GY,
Carroll M, et al: Plasma soluble VEGFR-1 is a potential dual
biomarker of response and toxicity for bevacizumab with
chemoradiation in locally advanced rectal cancer. Oncologist.
15:577–583. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lassau N, Coiffier B, Kind M, Vilgrain V,
Lacroix J, Cuinet M, Taieb S, Aziza R, Sarran A, Labbe-Devilliers
C, et al: Selection of an early biomarker for vascular
normalization using dynamic contrast-enhanced ultrasonography to
predict outcomes of metastatic patients treated with bevacizumab.
Ann Oncol. 27:1922–1928. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Good DJ, Polverini PJ, Rastinejad F, Le
Beau MM, Lemons RS, Frazier WA and Bouck NP: A tumor
suppressor-dependent inhibitor of angiogenesis is immunologically
and functionally indistinguishable from a fragment of
thrombospondin. Proc Natl Acad Sci USA. 87:6624–6628. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Takahashi K, Sumarriva K, Kim R, Jiang R,
Brantley-Sieders DM, Chen J, Mernaugh RL and Takahashi T:
Determination of the CD148-interacting region in thrombospondin-1.
PLoS One. 11:e01549162016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hamano Y, Sugimoto H, Soubasakos MA,
Kieran M, Olsen BR, Lawler J, Sudhakar A and Kalluri R:
Thrombospondin-1 associated with tumor microenvironment contributes
to low-dose cyclophosphamide-mediated endothelial cell apoptosis
and tumor growth suppression. Cancer Res. 64:1570–1574. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bocci G, Francia G, Man S, Lawler J and
Kerbel RS: Thrombospondin 1, a mediator of the antiangiogenic
effects of low-dose metronomic chemotherapy. Proc Natl Acad Sci
USA. 100:12917–12922. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Firlej V, Mathieu JR, Gilbert C, Lemonnier
L, Nakhlé J, Gallou-Kabani C, Guarmit B, Morin A, Prevarskaya N,
Delongchamps NB and Cabon F: Thrombospondin-1 triggers cell
migration and development of advanced prostate tumors. Cancer Res.
71:7649–7658. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ohta M, Kawabata T, Yamamoto M, Tanaka T,
Kikuchi H, Hiramatsu Y, Kamiya K, Baba M and Konno H: TSU68, an
antiangiogenic receptor tyrosine kinase inhibitor, induces tumor
vascular normalization in a human cancer xenograft nude mouse
model. Surg Today. 39:1046–1053. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Meng MB, Zaorsky NG, Deng L, Wang HH, Chao
J, Zhao LJ, Yuan ZY and Ping W: Pericytes: Adouble-edged sword in
cancer therapy. Future Oncol. 11:169–179. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gaustad JV, Simonsen TG, Andersen LM and
Rofstad EK: Thrombospondin-1 domain-containing peptide
properdistatin improves vascular function in human melanoma
xenografts. Microvasc Res. 98:159–165. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Dawes J, Clemetson KJ, Gogstad GO,
McGregor J, Clezardin P, Prowse CV and Pepper DS: A
radioimmunoassay for thrombospondin, used in a comparative study of
thrombospondin, beta-thromboglobulin and platelet factor 4 in
healthy volunteers. Thromb Res. 29:569–581. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Phelan MW, Forman LW, Perrine SP and
Faller DV: Hypoxia increases thrombospondin-1 transcript and
protein in cultured endothelial cells. J Lab Clin Med. 132:519–529.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Jain RK: Normalization of tumor
vasculature: An emerging concept in antiangiogenic therapy.
Science. 307:58–62. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Giantonio BJ, Catalano PJ, Meropol NJ,
O'Dwyer PJ, Mitchell EP, Alberts SR, Schwartz MA and Benson AB III;
Eastern Cooperative Oncology Group Study E3200, : Bevacizumab in
combination with oxaliplatin, fluorouracil, and leucovorin
(FOLFOX4) for previously treated metastatic colorectal cancer:
Results from the Eastern cooperative oncology group study E3200. J
Clin Oncol. 25:1539–1544. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Browder T, Butterfield CE, Kräling BM, Shi
B, Marshall B, O'Reilly MS and Folkman J: Antiangiogenic scheduling
of chemotherapy improves efficacy against experimental
drug-resistant cancer. Cancer Res. 60:1878–1886. 2000.PubMed/NCBI
|
|
29
|
Segers J, Di Fazio V, Ansiaux R, Martinive
P, Feron O, Wallemacq P and Gallez B: Potentiation of
cyclophosphamide chemotherapy using the anti-angiogenic drug
thalidomide: Importance of optimal scheduling to exploit the
‘normalization’ window of the tumor vasculature. Cancer Lett.
244:129–135. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Dickson PV, Hamner JB, Sims TL, Fraga CH,
Ng CY, Rajasekeran S, Hagedorn NL, McCarville MB, Stewart CF and
Davidoff AM: Bevacizumab-induced transient remodeling of the
vasculature in neuroblastoma xenografts results in improved
delivery and efficacy of systemically administered chemotherapy.
Clin Cancer Res. 13:3942–3950. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Jain RK, Duda DG, Willett CG, Sahani DV,
Zhu AX, Loeffler JS, Batchelor TT and Sorensen AG: Biomarkers of
response and resistance to antiangiogenic therapy. Nat Rev Clin
Oncol. 6:327–338. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Facciabene A, Peng XH, Hagemann IS, Balint
K, Barchetti A, Wang LP, Gimotty PA, Gilks CB, Lal P, Zhang L and
Coukos G: Tumour hypoxia promotes tolerance and angiogenesis via
CCL28 and T-(reg) cells. Nature. 475:226–230. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Chouaib S, Messai Y, Couve S, Escudier B,
Hasmim M and Noman MZ: Hypoxia promotes tumor growth in linking
angiogenesis to immune escape. Front Immunol. 3:212012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Jia Y, Liu M, Huang W, Wang Z, He Y, Wu J,
Ren S, Ju Y, Geng R and Li Z: Recombinant human endostatin endostar
inhibits tumor growth and metastasis in a mouse xenograft model of
colon cancer. Pathol Oncol Res. 18:315–323. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Sorensen AG, Batchelor TT, Zhang WT, Chen
PJ, Yeo P, Wang MY, Jennings D, Wen PY, Lahdenranta J, Ancukiewicz
M, et al: A ‘Vascular Normalization Index’ as potential mechanistic
biomarker to predict survival after a single dose of cediranib in
recurrent glioblastoma patients. Cancer Res. 69:5296–5300. 2009.
View Article : Google Scholar : PubMed/NCBI
|