Laryngeal squamous cell carcinoma (LSCC) is one of
the most commonly diagnosed malignancies in the head and neck, with
an increased incidence rate in middle-aged and elderly males
worldwide in the last few decades (1–3). LSCC
originates from laryngeal epithelial tissue and may spread directly
to adjacent structures, or through lymphatic and blood vessels to
lymph nodes and more distant sites (4). Despite considerable improvements in
laryngeal carcinoma treatment, which have improved patient quality
of life, the global survival rates have remained unchanged
throughout the last 3 decades (5–7).
Circulating tumor cells (CTCs) are rare cells that
derive from both primitive cancer and metastases, pass through the
blood vessels and circulate together with the red and white blood
cells. CTCs are absent in healthy patients (8). Several studies have investigated the
presence of CTCs associated with solid types of cancer, including
head and neck squamous cell carcinoma (9,10), and
proposed the use of liquid biopsy in clinical assessment of
patients with cancer (11–19). The presence of CTCs has been
validated as a prognostic factor in metastatic breast, colorectal
and prostate cancers (15,17), and confirmed in previous
meta-analyses (20,21); however, only a few studies have
examined CTCs in patients with head and neck and laryngeal cancer
(9–11,14,18).
Several techniques for the detection and enumeration
of CTCs have been developed during the last decade. For example,
epithelial antigenic properties of cancer cells are used to detect
and isolate cancer cells from blood using immunomagnetic or
microfluidic-based enrichment methods (22). The current techniques allow the
isolation of CTCs as: epithelial cells (cytokeratin positive),
cells in the epithelial to mesenchymal transition (EMT) phase
(cytokeratin negative), stem cells and clusters (two or more CTCs
together) (23). However, a number
of these detection systems are not commercially available and/or
economically accessible (23).
Previously, it has been demonstrated that the epithelial
antigen-based detection of CTCs may underestimate the real number
of CTC (24). This may be due to
EMT, which represents an integral component of the metastatic
process in which cancer cells downregulate the expression of
epithelial markers in favor of mesenchymal markers, inducing the
increased stemness of cancer cells and facilitating the development
of chemoresistance (25–28). The ScreenCell system, a
filtration-based size and antigen-independent technology, has been
developed to identify CTCs (29,30), and
the rationale of this device is based on the larger size of CTCs
compared with hematological cells (31).
The present pilot study aimed to detect CTCs in the
blood of patients with laryngeal squamous carcinoma pre- and
post-operatively using the ScreenCell system, and to evaluate the
association between CTC presence and patient prognosis.
The Ethics Committee of the Sapienza University of
Rome approved the present pilot study (approval no. 32/2017). The
experimental protocol met the guidelines and the precepts
established by the Declaration of Helsinki; experiments were
undertaken with the understanding and written consent of each
subject and according to the aforementioned principles.
A total of 8/32 patients diagnosed with laryngeal
cancer were included in the present study, according to the
following sequential inclusion criteria: i) Biopsy specimen
positive squamous cell carcinoma (n=32); ii) absence of synchronous
and metachronous cancer (n=26); iii) Tumor-Node-Metastasis
(TNM)-stage III/IV (n=13); iv) candidates for total or subtotal
laryngectomy with neck dissection (n=12); v) no candidates for
neoadjuvant therapy (n=10); and vi) patients that provided written
informed consent (n=8). In order to increase the uniformity of the
population, only patients with homogeneous characteristics for
clinical and histopathological parameters were included. All
participants were males, smokers, non-alcoholics, age >65 years
(age range=61-83; mean age=69 years) with a diagnosis of LSCC. The
included patients were waiting for primary laryngeal surgery and
were classified, according to the TNM classification (32), as T3N+M0. In the total
cohort, 1 patient underwent total laryngectomy and 7 underwent
subtotal laryngectomy, according to cancer staging. All patients
underwent radical bilateral neck lymph node dissection.
The stages of the study were: i) biopsy by
microlaryngoscopy and staging by computed tomography (CT) scan,
fibro- and micro-laryngoscopy; ii) preoperative blood sampling;
iii) surgery; iv) postoperative short- and medium-term follow-up at
3, 6 and 12 months with clinical evaluation and blood sampling for
CTC detection; and v) data analysis. The association between CTC
detection and prognosis was studied via the comparison between CTC
presence with recurrence/lymph node metastasis/death and adjuvant
therapy/secondary surgery.
Leukocyte depletion was performed using Dynabeads
CD45 (Invitrogen; Thermo Fisher Scientific, Inc.) in order to
enrich CTCs from whole blood, following the manufacturer's
instructions, as previously described (33). Each blood sample was incubated with
Dynabeads (Invitrogen; Thermo Fisher Scientific, Inc.) for 30 min
at 2°C with gentle tilting rotation. The tube was then removed from
the mixer and placed on a magnet for 10 min at 20–25°C. The
supernatant was transferred into a new tube and immediately
processed for downstream analysis using the ScreenCell device
(ScreenCell Ltd.).
To isolate fixed cells for cytological studies, a
ScreenCell Cytokit was used according to the manufacturer's
protocol (Caltag Medsystems, Ltd.). A 3 ml leukocyte-depleted blood
sample was diluted using 4 ml filtration buffer ScreenCell fixed
cells (FC2) dilution buffer (ScreenCell) to fix cells and lyse red
blood cells (RBCs). Before use, 30% NaOH was added to the FC buffer
until a pH ~7 was reached. After 8 min of incubation at room
temperature, 7 ml diluted sample was added into the device tank and
filtered under a pressure gradient (determined between the
atmosphere pressure and vacuum tube) using a vacutainer tube.
Filtration was completed within 3 min. After washing with PBS to
remove RBC debris, the filter was left on absorbing paper to dry at
room temperature and then stored at −20°C until Giemsa and
immunofluorescence staining were performed. For each patient, the
filtration was carried out in duplicate.
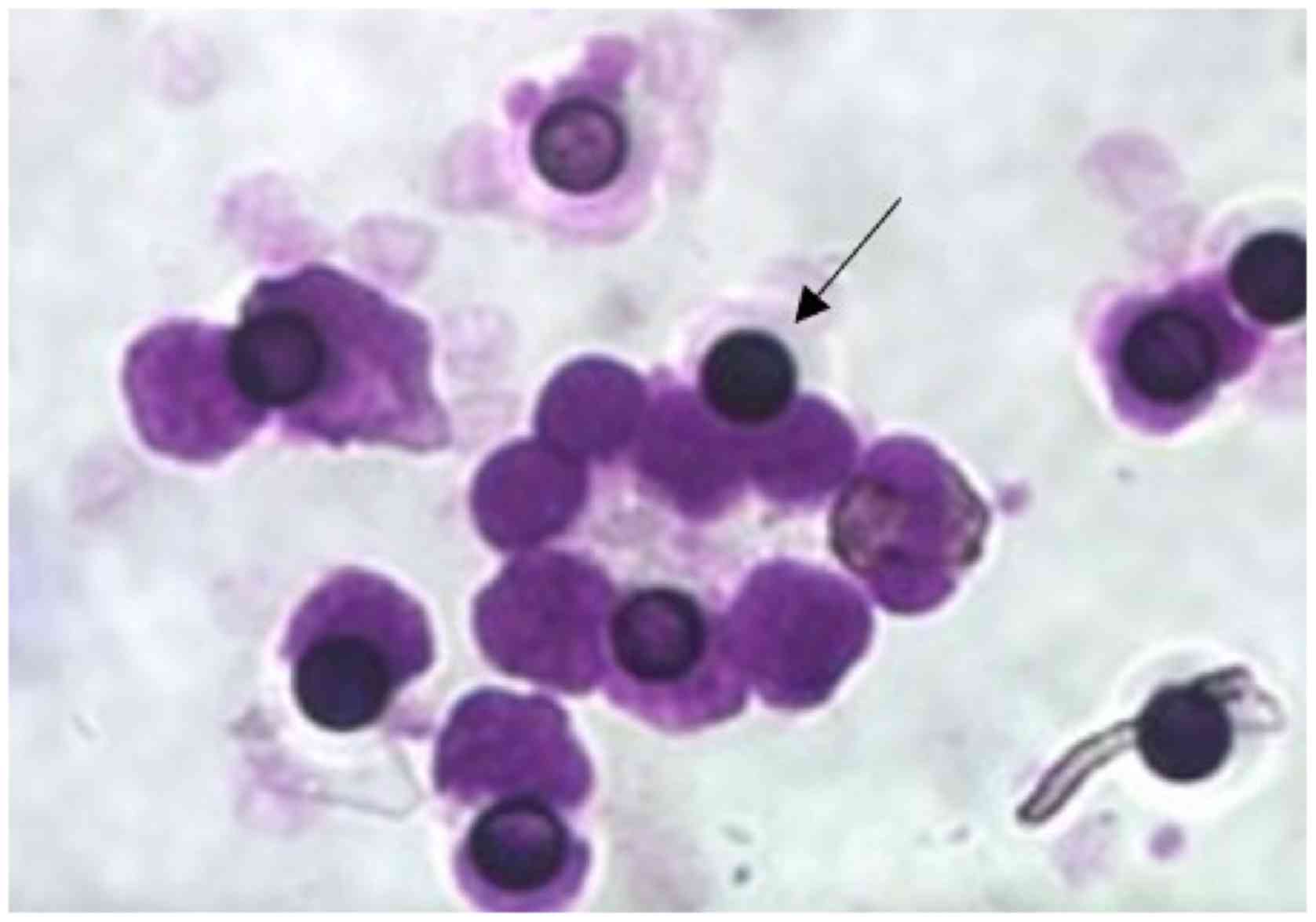
The filters were stained for 30 min at room
temperature with Giemsa stain (1:10; cat. no. 453616; Carlo Erba)
and examined using a light microscope (magnification, ×400) (Leitz
DMRB Camera; Leica Microsystems Inc.) to evaluate the presence of
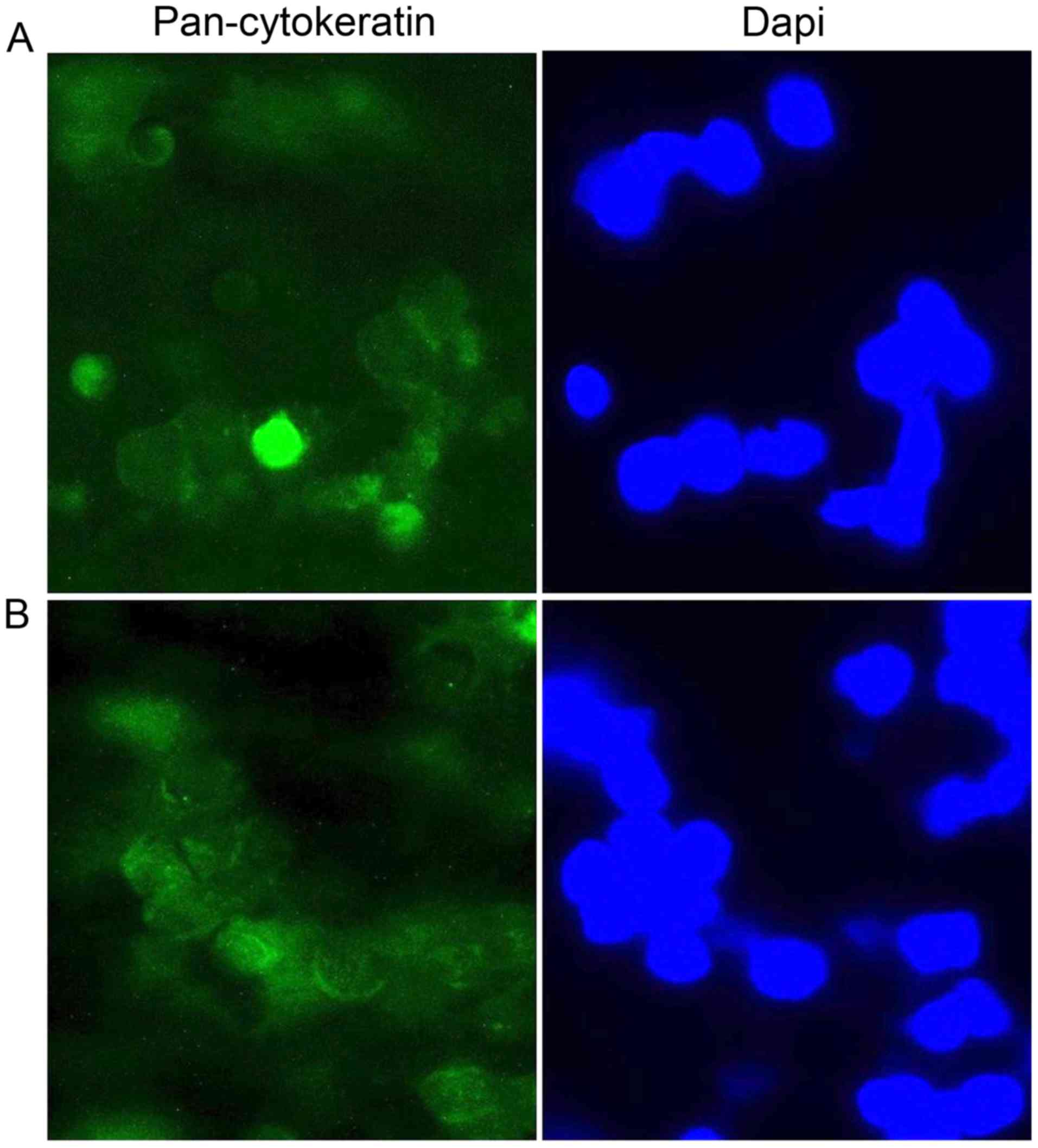
cells adhered to the filter membrane. The double immunofluorescence
analysis, using anti-Pan-Cytokeratin (CK) and anti-epithelial cell
adhesion molecule (EpCAM) antibodies, was used to identify the
adherent cells as CTCs. For this scope, the filters were fixed
using 4% paraformaldehyde solution for 5 min at 4°C and
subsequently permeabilized using PBS and 0.01% Tween-20 (Merck
KGaA) for 20 min at room temperature. Then, both the filters were
incubated with monoclonal mouse anti-Pan-Cytokeratin antibody 2A4
(1:100; cat. no. ab118855; Abcam) for 1 h at room temperature. The
filters were incubated with secondary antibody Alexa Fluor 488 goat
anti-mouse IgG (H + L) (1:300; cat. no. A11001; Thermo Fisher
Scientific, Inc.; green staining). Successively, the filters were
incubated with monoclonal mouse anti-EpCAM antibody (clone C-10;
1:50; cat. no. sc-25308, Santa Cruz Biotechnology) for 1 h at room
temperature followed by incubation with secondary antibody Alexa
Fluor 594 goat anti-mouse IgG (H + L) (1:300; cat. no. A11005;
Thermo Fisher Scientific, Inc.; red staining). . The nuclei were
counterstained for 10 min at room temperature using DAPI (1:1,000;
cat. no. D1306; Thermo Fisher Scientific, Inc.). Immunostaining was
examined under a fluorescence microscope (Olympus Corporation) at
magnification, ×400. For each sample, five randomly selected
microscopic fields were evaluated and cells positive for
anti-Pan-Cytokeratin (cytoplasmatic green stain) and anti-EpCAM
(cytoplasmatic red stain) immunostaining, were counted. The cells
positive for anti-Pan-Cytokeratin and anti-EpCAM were considered to
be CTCs.
Preoperatively, 6 patients had evidence of CTCs and
2 patients were negative. The data revealed that the presence of
CTC before the surgery may be associated with a less favorable
prognosis, whereas a negative result for CTCs preoperatively was
associated with a favorable prognosis. The majority of patients who
were CTC+ (83.3%) exhibited a poor prognosis (4 died and
1 underwent secondary surgery), while all patients who were
CTC− preoperatively were disease-free at all follow-up
visits (Table I).
The analysis of the data at medium-term (6 months
after surgery) revealed that: i) Negative matching of CTC in the
pre- and post-operative at 6 months may be a positive prognostic
factor (25% of patients CTC− in the pre- and
post-6-months were disease-free at all follow-ups); ii) patients
who underwent chemotherapy were negative for CTCs; and iii) 50% of
patients with detectable CTC both in pre- and post-6-months follow
up experienced a progression of disease (Table I).
Data collected 12 months after surgery indicated
that: i) CTC negativity preoperatively and at the 12-month follow
up were associated with a more favorable prognosis; and ii) CTC
positivity preoperatively and at the 12-month follow up was
associated with a less favorable prognosis. In fact, all patients
that were CTC+ both pre- and post-operative died, except
the patient that exhibited a decrease in CTC levels in the
long-term (Table I).
In the last two decades, comprehensive treatment
measures, such as surgery, radiotherapy, chemotherapy and gene
therapy, have resulted in a higher 5-year survival rate globally
for patients with laryngeal cancer; however, 30–40% of patients
still succumbed to the disease due to tumor recurrence or
metastasis (34). An improved
understanding of the metastatic processes underlying LSCC is needed
to identify novel prognostic factors and treatment methods.
The present pilot study evaluated whether the
presence of CTCs in patients with laryngeal cancer may represent a
novel independent prognostic factor and may be quantified in a
liquid biopsy to aid clinical evaluation. The techniques used for
CTC detection in the present study were immunological and
morphological; CTCs were isolated from the blood of patients with
LSCC using the ScreenCell system, a technology based on
polycarbonate filter with 8 µm diameter pores able to isolate CTCs
from other blood cells. An advantage of this technology is the
possibility to detect CTCs using Giemsa histochemical staining and
to identify the presence of CTC markers by immunofluorescence
staining (29). Leukocyte depletion
was performed prior to the CTC isolation in order to improve the
CTC detection (35).
To the best of our knowledge, the present study is
the first to focus exclusively on CTCs in laryngeal cancer using
the ScreenCell system. No other studies have been published on the
use of ScreenCell in laryngeal cancer and these preliminary results
may present an incentive for further studies on this topic. The
ScreenCell system differs from other systems such as the
CellCollector system, used by Zhang et al (36) in which CTCs from laryngeal cancer
were evaluated as it is a filtration-based size and
antigen-independent technology (29). CTC isolation using the ScreenCell
system is promising due to its simplicity, speed and the benefit
that it eliminates any antibody bias that may be introduced by
other techniques (37,38). Although no complex instruments or
training are needed to use this system, the costs are high.
The development of semiautomatic technologies, such
as the CellSearch system, has allowed evaluation of the prognostic
role of CTC status in patients with other types of cancer, such as
lung and breast cancer, with promising results (37–49). A
recent study from Chudasama et al (38) evaluated the efficacy of the
ScreenCell filtration system, to capture, isolate and propagate
CTCs from patients with primary lung cancer. The results suggested
that the ScreenCell system had the potential to be used as a CTC
isolation tool following further work, adaptations and improvements
to the technology and validation of results. Another study from
Hashimoto et al (48)
concluded that there was an increase in the CTC count of pulmonary
vein blood following surgical manipulation of a tumor. Hou et
al (49) identified an
association between an increased CTC count and less favorable
patient survival in small cell lung cancer.
The preliminary results of the present study
indicate that, in laryngeal cancer, the absence of CTCs may predict
a more favorable prognosis, while high levels of CTCs in the
peripheral blood may be associated with a less favorable prognosis.
A decrease of CTCs in postoperative sampling may suggest an
improved response to surgical treatment, and the early detection of
CTCs may predict recurrence or metastasis.
The results of the present study are in accordance
with other studies investigating CTCs in solid cancers, including
the head and neck, which revealed that the presence of CTCs may
influence prognosis (11–17,44–57).
Zhang et al (36) and He
et al (58) revealed that
CTCs have a role in the progression and metastasis of head and neck
squamous cell carcinoma. Nichols et al (59) isolated CTCs in 6/15 patients with
advanced head and neck carcinoma using CellSearch and demonstrated
an association with lung nodules >1 cm. Winter et al
(60) tested 16 patients with
advanced head and neck squamous cell carcinoma and demonstrated
that almost all (15/17) patients had circulating cells at the time
of surgery, similar to what was observed in the patients in the
present study (6/8 were positive to CTC preoperatively). A recent
meta-analysis comprised of 17 studies confirmed the significant
prognostic value of CTCs in patients with head and neck cancer,
wherein positive CTCs were significantly associated with poor
overall, disease-free and progression-free survival (61). Patients who were CTC+
tended to have higher recurrence and regional lymph node metastasis
rate and a more advanced tumor stage. The authors concluded that
the presence of CTCs may be used as a monitoring tool for tumor
status of head and neck cancer, especially for the early detection
of tumor recurrence and progression, advanced disease and node
metastasis.
The primary limitation of the present study is the
small number of patients included. Such small sample did not allow
reliable statistical analyses to be performed. Further studies
aimed at investigating CTCs in laryngeal cancer using the
ScreenCell system in a larger cohort of patients are necessary to
improve the definition of the sensitivity and specificity of the
ScreenCell filtration system and to confirm the preliminary
results.
In conclusion, the results of the present study
revealed a possible association between the presence of CTCs and a
less favorable prognosis in patients with LSCC. The current
preliminary findings may encourage more research into the
incorporation of a liquid biopsy test in the management of LSCC, as
it may help identify patients with occult metastatic disease
earlier and in a non-invasive manner. This may also represent an
independent prognostic factor which may help in clinical
evaluation. Further studies aimed at investigating the role of CTC
using the ScreenCell system in a larger number of patients with
laryngeal cancer are necessary to confirm these preliminary
results.
The authors wish to thank Mr Jay Joseph Abedin for
his thoughtful revision of the English language and grammar of this
manuscript.
No funding was received.
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
MIR and MR conceived and designed the study. CN and
AGra collected and analyzed the samples and interpreted the data.
CN, CDG and RC prepared the first draft of the manuscript. CDG,
AGre and RC made substantial contributions to acquisition and
analysis and interpretation of data. MR and MDV performed the
clinical evaluations and surgical procedures. AGre and CDG reviewed
and revised the manuscript critically for important intellectual
content. All authors have read and approved the final
manuscript.
The Ethics Committee of the Sapienza University of
Rome approved this pilot study (approval no. 32/2017). All patients
provided informed written consent.
Signed informed consent for publication has been
obtained from the patients.
The authors declare that they have no competing
interests.
|
1
|
Greco A, Rizzo MI, De Virgilio A, Gallo A,
Fusconi M, Pagliuca G, Martellucci S, Turchetta R and De Vincentiis
M: Cancer stem cells in laryngeal cancer: What we know. Eur Arch
Otorhinolaryngol. 273:3487–3495. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Yu D, Liu Y, Yang J, Jin C, Zhao X, Cheng
J, Liu X and Qi X: Clinical implications of BMI-1 in cancer stem
cells of laryngeal carcinoma. Cell Biochem Biophys. 71:261–269.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jemal A, Siegel R, Xu J and Ward E: Cancer
statistics, 2010. CA Cancer J Clin. 60:277–300. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mäkitie AA and Monni O: Molecular
profiling of laryngeal cancer. Expert Rev Anticancer Ther.
9:1251–1260. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wan G, Zhou L, Xie M, Chen H and Tian J:
Characterization of side population cells from laryngeal cancer
cell lines. Head Neck. 32:1302–1309. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
De Virgilio A, Ralli M, Longo L, Mancini
P, Attanasio G, Atturo F, De Vincentiis M and Greco A:
Electrochemotherapy in head and neck cancer: A review of an
emerging cancer treatment. Oncol Lett. 16:3415–3423.
2018.PubMed/NCBI
|
|
7
|
Bussu F, Paludetti G, Almadori G, De
Virgilio A, Galli J, Miccichè F, Tombolini M, Rizzo D, Gallo A,
Giglia V, et al: Comparison of total laryngectomy with surgical
(cricohyoidopexy) and nonsurgical organ-preservation modalities in
advanced laryngeal squamous cell carcinomas: A multicenter
retrospective analysis. Head Neck. 35:554–561. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
García SA, Weitz J and Schölch S:
Circulating tumor cells. Methods Mol Biol. 1692:213–219. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wu XL, Tu Q, Faure G, Gallet P, Kohler C
and Bittencourt MC: Diagnostic and prognostic value of circulating
tumor cells in head and neck squamous cell carcinoma: A systematic
review and meta-analysis. Sci Rep. 6:202102016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wang Z, Cui K, Xue Y, Tong F and Li S:
Prognostic value of circulating tumor cells in patients with
squamous cell carcinoma of the head and neck: A systematic review
and meta-analysis. Med Oncol. 32:1642015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Grisanti S, Almici C, Consoli F, Buglione
M, Verardi R, Bolzoni-Villaret A, Bianchetti A, Ciccarese C,
Mangoni M, Ferrari L, et al: Circulating tumor cells in patients
with recurrent or metastatic head and neck carcinoma: Prognostic
and predictive significance. PLoS One. 9:e1039182014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Alix-Panabieres C and Pantel K: The
circulating tumor cells: Liquid biopsy of cancer. Klin Lab Diagn.
4:60–64. 2014.(In Russian).
|
|
13
|
Heitzer E, Auer M, Ulz P, Geigl JB and
Speicher MR: Circulating tumor cells and DNA as liquid biopsies.
Genome Med. 5:732013. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hristozova T, Konschak R, Stromberger C,
Fusi A, Liu Z, Weichert W, Stenzinger A, Budach V, Keilholz U and
Tinhofer I: The presence of circulating tumor cells (CTCs)
correlates with lymph node metastasis in nonresectable squamous
cell carcinoma of the head and neck region (SCCHN). Ann Oncol.
22:1878–1885. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cohen SJ, Punt CJ, Iannotti N, Saidman BH,
Sabbath KD, Gabrail NY, Picus J, Morse M, Mitchell E, Miller MC, et
al: Relationship of circulating tumor cells to tumor response,
progression-free survival, and overall survival in patients with
metastatic colorectal cancer. J Clin Oncol. 26:3213–3221. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Danila DC, Heller G, Gignac GA,
Gonzalez-Espinoza R, Anand A, Tanaka E, Lilja H, Schwartz L, Larson
S, Fleisher M, et al: Circulating tumor cell number and prognosis
in progressive castration-resistant prostate cancer. Clin Cancer
Res. 13:7053–7058. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cristofanilli M, Hayes DF, Budd GT, Ellis
MJ, Stopeck A, Reuben JM, Doyle GV, Matera J, Allard WJ, Miller MC,
et al: Circulating tumor cells: A novel prognostic factor for newly
diagnosed metastatic breast cancer. J Clin Oncol. 23:1420–1430.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Nonaka T and Wong DT: Liquid biopsy in
head and neck cancer: Promises and Challenges. J Dent Res.
97:701–708. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Economopoulou P, Kotsantis I, Kyrodimos E,
Lianidou ES and Psyrri A: Liquid biopsy: An emerging prognostic and
predictive tool in Head and Neck Squamous Cell Carcinoma (HNSCC).
Focus on Circulating Tumor Cells (CTCs). Oral Oncol. 74:83–89.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhao S, Liu Y, Zhang Q, Li H, Zhang M, Ma
W, Zhao W, Wang J and Yang M: The prognostic role of circulating
tumor cells (CTCs) detected by RT-PCR in breast cancer: A
meta-analysis of published literature. Breast Cancer Res Treat.
130:809–816. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rahbari NN, Aigner M, Thorlund K, Mollberg
N, Motschall E, Jensen K, Diener MK, Büchler MW, Koch M and Weitz
J: Meta-analysis shows that detection of circulating tumor cells
indicates poor prognosis in patients with colorectal cancer.
Gastroenterology. 138:1714–1726. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Parkinson DR, Dracopoli N, Petty BG,
Compton C, Cristofanilli M, Deisseroth A, Hayes DF, Kapke G, Kumar
P, Lee JS, et al: Considerations in the development of circulating
tumor cell technology for clinical use. J Transl Med. 10:1382012.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ferreira MM, Ramani VC and Jeffrey SS:
Circulating tumor cell technologies. Mol Oncol. 10:374–394. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
El-Heliebi A, Kroneis T, Zöhrer E,
Haybaeck J, Fischereder K, Kampel-Kettner K, Zigeuner R, Pock H,
Riedl R, Stauber R, et al: Are morphological criteria sufficient
for the identification of circulating tumor cells in renal cancer?
J Transl Med. 11:2142013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Papadaki MA, Stoupis G, Theodoropoulos PA,
Mavroudis D, Georgoulias V and Agelaki S: Circulating tumor cells
with stemness and epithelial-to-mesenchymal transition features are
chemoresistant and predictive of poor outcome in metastatic breast
cancer. Mol Cancer Ther. 18:437–447. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Joosse SA and Pantel K: Biologic
challenges in the detection of circulating tumor cells. Cancer Res.
73:8–11. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Krebs MG, Hou JM, Sloane R, Lancashire L,
Priest L, Nonaka D, Ward TH, Backen A, Clack G, Hughes A, et al:
Analysis of circulating tumor cells in patients with non-small cell
lung cancer using epithelial marker-dependent and -independent
approaches. J Thorac Oncol. 7:306–315. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Christiansen JJ and Rajasekaran AK:
Reassessing epithelial to mesenchymal transition as a prerequisite
for carcinoma invasion and metastasis. Cancer Res. 66:8319–8326.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Desitter I, Guerrouahen BS, Benali-Furet
N, Wechsler J, Jänne PA, Kuang Y, Yanagita M, Wang L, Berkowitz JA,
Distel RJ, et al: A new device for rapid isolation by size and
characterization of rare circulating tumor cells. Anticancer Res.
31:427–441. 2011.PubMed/NCBI
|
|
30
|
Zheng S, Lin HK, Lu B, Williams A, Datar
R, Cote RJ and Tai YC: 3D microfilter device for viable circulating
tumor cell (CTC) enrichment from blood. Biomed Microdevices.
13:203–213. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Vona G, Sabile A, Louha M, Sitruk V,
Romana S, Schütze K, Capron F, Franco D, Pazzagli M, Vekemans M, et
al: Isolation by size of epithelial tumor cells : A new method for
the immunomorphological and molecular characterization of
circulating tumor cells. Am J Pathol. 156:57–63. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Huang SH and O'Sullivan B: Overview of the
8th edition TNM classification for head and neck cancer. Curr Treat
Options Oncol. 18:402017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Nicolazzo C, Raimondi C, Francescangeli F,
Ceccarelli S, Trenta P, Magri V, Marchese C, Zeuner A, Gradilone A
and Gazzaniga P: EpCAM-expressing circulating tumor cells in
colorectal cancer. Int J Biol Markers. 32:e415–e420. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Yu D, Jin C, Liu Y, Yang J, Zhao Y, Wang
H, Zhao X, Cheng J, Liu X and Liu C: Clinical implications of
cancer stem cell-like side population cells in human laryngeal
cancer. Tumour Biol. 34:3603–3610. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Yang L, Lang JC, Balasubramanian P, Jatana
KR, Schuller D, Agrawal A, Zborowski M and Chalmers JJ:
Optimization of an enrichment process for circulating tumor cells
from the blood of head and neck cancer patients through depletion
of normal cells. Biotechnol Bioeng. 102:521–534. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhang HD, Gong SC, Liu YQ, Liang LJ, He
SB, Zhang QX, Si MY and Yu ZK: The significance of circulating
tumor cells in head and neck squamous cell carcinoma: A preliminary
study. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 53:39–44.
2018.PubMed/NCBI
|
|
37
|
Chudasama D, Katopodis P, Stone N, Haskell
J, Sheridan H, Gardner B, Urnovitz H, Schuetz E, Beck J, Hall M, et
al: Liquid biopsies in lung cancer: Four emerging technologies and
potential clinical applications. Cancers (Basel). 11:E3312019.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Chudasama D, Burnside N, Beeson J,
Karteris E, Rice A and Anikin V: Perioperative detection of
circulating tumour cells in patients with lung cancer. Oncol Lett.
14:1281–1286. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Amantini C, Morelli MB, Nabissi M, Piva F,
Marinelli O, Maggi F, Bianchi F, Bittoni A, Berardi R, Giampieri R,
et al: Expression profiling of circulating tumor cells in
pancreatic ductal adenocarcinoma patients: Biomarkers predicting
overall survival. Front Oncol. 9:8742019. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Nicolazzo C, Raimondi C, Gradilone A,
Emiliani A, Zeuner A, Francescangeli F, Belardinilli F, Seminara P,
Loreni F and Magri V: Circulating tumor cells in right- and
left-sided colorectal cancer. Cancers (Basel). 11:E10422019.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Kuvendjiska J, Bronsert P, Martini V, Lang
S, Pitman MB, Hoeppner J, Kulemann B, et al: Non-metastatic
esophageal adenocarcinoma: Circulating tumor cells in the course of
multimodal tumor treatment. Cancers (Basel). 11:E3972019.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Nicolazzo C, Colangelo L, Corsi A, Carpino
G, Gradilone A, Sonato C, Raimondi C, Gaudio E, Gazzaniga P and
Gianni W: Liquid Biopsy in Rare Cancers: Lessons from
Hemangiopericytoma. Anal Cell Pathol (Amst).
2018:97185852018.PubMed/NCBI
|
|
43
|
Mascalchi M, Maddau C, Sali L, Bertelli E,
Salvianti F, Zuccherelli S, Matucci M, Borgheresi A, Raspanti C,
Lanzetta M, et al: Circulating tumor cells and microemboli can
differentiate malignant and benign pulmonary lesions. J Cancer.
8:2223–2230. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Fina E, Necchi A, Bottelli S, Reduzzi C,
Pizzamiglio S, Iacona C, Daidone MG, Verderio P and Cappelletti V:
Detection of circulating tumour cells in urothelial cancers and
clinical correlations: Comparison of two methods. Dis Markers.
2017:34149102017. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Awe JA, Saranchuk J, Drachenberg D and Mai
S: Filtration-based enrichment of circulating tumor cells from all
prostate cancer risk groups. Urol Oncol. 35:300–309. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Mu Z, Benali-Furet N, Uzan G, Znaty A, Ye
Z, Paolillo C, Wang C, Austin L, Rossi G, Fortina P, Yang H, et al:
Detection and characterization of circulating tumor associated
cells in metastatic Breast Cancer. Int J Mol Sci. 17:E16652016.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Kulasinghe A, Kenny L, Perry C, Thiery JP,
Jovanovic L, Vela I, Nelson C and Punyadeera C: Impact of
label-free technologies in head and neck cancer circulating tumour
cells. Oncotarget. 7:71223–71234. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Hashimoto M, Tanaka F, Yoneda K, Takuwa T,
Matsumoto S, Okumura Y, Kondo N, Tsubota N, Tsujimura T, Tabata C,
et al: Significant increase in circulating tumour cells in
pulmonary venous blood during surgical manipulation in patients
with primary lung cancer. Interact Cardiovasc Thorac Surg.
18:775–783. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Hou JM, Greystoke A, Lancashire L,
Cummings J, Ward T, Board R, Amir E, Hughes S, Krebs M, Hughes A,
et al: Evaluation of circulating tumor cells and serological cell
death biomarkers in small cell lung cancer patients undergoing
chemotherapy. Am J Pathol. 175:808–816. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Wang HM, Wu MH, Chang PH, Lin HC, Liao CD,
Wu SM, Hung TM, Lin CY, Chang TC, Tzu-Tsen Y, et al: The change in
circulating tumor cells before and during concurrent
chemoradiotherapy is associated with survival in patients with
locally advanced head and neck cancer. Head Neck. 41:2676–2687.
2019.PubMed/NCBI
|
|
51
|
Chikamatsu K, Tada H, Takahashi H,
Kuwabara-Yokobori Y, Ishii H, Ida S and Shino M: Expression of
immune-regulatory molecules in circulating tumor cells derived from
patients with head and neck squamous cell carcinoma. Oral Oncol.
89:34–39. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Kulasinghe A, Kapeleris J, Kimberley R,
Mattarollo SR, Thompson EW, Thiery JP, Kenny L, O'Byrne K and
Punyadeera C: The prognostic significance of circulating tumor
cells in head and neck and non-small-cell lung cancer. Cancer Med.
7:5910–5919. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Ng SP, Bahig H, Wang J, Cardenas CE, Lucci
A, Hall CS, Meas S, Sarli VN, Yuan Y, Urbauer DL, et al: Predicting
treatment Response based on Dual assessment of magnetic resonance
Imaging kinetics and Circulating Tumor cells in patients with Head
and Neck cancer (PREDICT-HN): Matching ‘liquid biopsy’ and
quantitative tumor modeling. BMC Cancer. 18:9032018. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Morgan TM, Wang X, Qian X, Switchenko JM,
Nie S, Patel KR, Cassidy RJ, Shin DM and Beitler JJ: Measurement of
circulating tumor cells in squamous cell carcinoma of the head and
neck and patient outcomes. Clin Transl Oncol. 21:342–347. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Lou JL, Guo L, Zheng WH, Zhao JZ, Zhao JQ,
Liang Z, Wang SY and Fang MY: Peripheral blood circulating tumor
cells in local advanced head and neck squamous cell carcinoma.
Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 52:824–829. 2017.(In
Chinese). PubMed/NCBI
|
|
56
|
Kawada T, Takahashi H, Sakakura K, Ida S,
Mito I, Toyoda M and Chikamatsu K: Circulating tumor cells in
patients with head and neck squamous cell carcinoma: Feasibility of
detection and quantitation. Head Neck. 39:2180–2186. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Fanelli MF, Oliveira TB, Braun AC, Corassa
M, Abdallah EA, Nicolau UR, da Silva Alves V, Garcia D, Calsavara
VF, Kowalski LP, et al: Evaluation of incidence, significance, and
prognostic role of circulating tumor microemboli and transforming
growth factor-β receptor I in head and neck cancer. Head Neck.
39:2283–2292. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
He S, Li P, He S, Long T, Zhang N, Fang J
and Yu Z: Detection of circulating tumour cells with the CellSearch
system in patients with advanced-stage head and neck cancer:
Preliminary results. J Laryngol Otol. 127:788–793. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Nichols AC, Lowes LE, Szeto CC, Basmaji J,
Dhaliwal S, Chapeskie C, Todorovic B, Read N, Venkatesan V, Hammond
A, et al: Detection of circulating tumor cells in advanced head and
neck cancer using the CellSearch system. Head Neck. 34:1440–1444.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Winter SC, Stephenson SA, Subramaniam SK,
Paleri V, Ha K, Marnane C, Krishnan S and Rees G: Long term
survival following the detection of circulating tumour cells in
head and neck squamous cell carcinoma. BMC Cancer. 9:4242009.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Sun T, Zou K, Yuan Z, Yang C, Lin X and
Xiong B: Clinicopathological and prognostic significance of
circulating tumor cells in patients with head and neck cancer: A
meta-analysis. OncoTargets Ther. 10:3907–3916. 2017. View Article : Google Scholar
|