|
1
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Herrero R, González P and Markowitz LE:
Present status of human papillomavirus vaccine development and
implementation. Lancet Oncol. 16:e206–e216. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Waggoner SE: Cervical cancer. Lancet.
361:2217–2225. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Golfetto L, Alves EV, Martins TR, Sincero
TCM, Castro JBS, Dannebrock C, Oliveira JG, Levi JE, Onofre ASC and
Bazzo ML: PCR-RFLP assay as an option for primary HPV test. Braz J
Med Biol Res. 51:e70982018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bruni L, Diaz M, Castellsagué X, Ferrer E,
Bosch FX and de Sanjosé S: Cervical human papillomavirus prevalence
in 5 continents: Meta-analysis of 1 million women with normal
cytological findings. J Infect Dis. 202:1789–1799. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kocjan BJ, Bzhalava D, Forslund O, Dillner
J and Poljak M: Molecular methods for identification and
characterization of novel papillomaviruses. Clin Microbiol Infect.
21:808–816. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ghebre RG, Grover S, Xu MJ, Chuang LT and
Simonds H: Cervical cancer control in HIV-infected women: Past,
present and future. Gynecol Oncol Rep. 21:101–108. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ferlay J, Soerjomataram I, Dikshit R, Eser
S, Mathers C, Rebelo M, Parkin DM, Forman D and Bray F: Cancer
incidence and mortality worldwide: Sources, methods and major
patterns in GLOBOCAN 2012. Int J Cancer. 136:E359–E386. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Idehen EE, Koponen P, Härkänen T,
Kangasniemi M, Pietilä AM and Korhonen T: Disparities in cervical
screening participation: A comparison of Russian, Somali and
Kurdish immigrants with the general Finnish population. Int J
Equity Health. 17:562018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Swanson M, Ueda S, Chen LM, Huchko MJ,
Nakisige C and Namugga J: Evidence-based improvisation: Facing the
challenges of cervical cancer care in Uganda. Gynecol Oncol Rep.
24:30–35. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Satterwhite CL, Torrone E, Meites E, Dunne
EF, Mahajan R, Ocfemia MC, Su J, Xu F and Weinstock H: Sexually
transmitted infections among US women and men: Prevalence and
incidence estimates, 2008. Sex Transm Dis. 40:187–193. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Say L, Chou D, Gemmill A, Tunçalp Ö,
Moller AB, Daniels J, Gülmezoglu AM, Temmerman M and Alkema L:
Global causes of maternal death: A WHO systematic analysis. Lancet
Glob Health. 2:e323–e333. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bray F, Ren JS, Masuyer E and Ferlay J:
Global estimates of cancer prevalence for 27 sites in the adult
population in 2008. Int J Cancer. 132:1133–1145. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Torre LA, Islami F, Siegel RL, Ward EM and
Jemal A: Global cancer in women: Burden and trends. Cancer Epidemol
Biomarkers Prev. 26:444–457. 2017. View Article : Google Scholar
|
|
15
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. 68:394–424. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
World Health Organization, . WHO
guidelines for screening and treatment of precancerous lesions for
cervical cancer prevention. World Health Organization.
2013.March
16–2019
|
|
17
|
Karsa LV, Anttila A, Ronco G, et al:
Cancer screening in the European Union. Report on the
implementation of the Council Recommendation on cancer screening.
In: Cancer screening in the European Union. Report on the
implementation of the Council Recommendation on cancer screening.
European Commission. (Luxembourg). 1602008.
|
|
18
|
Ginindza TG and Sartorius B: Projected
cervical cancer incidence in Swaziland using three methods and
local survey estimates. BMC Cancer. 18:6392018. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ferlay J, Colombet M, Soerjomataram I, et
al: Estimating the global cancer incidence and mortality in 2018:
GLOBOCAN sources and methods. Int J Cancer. 144:1941–1953. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sartorius K, Sartorius B, Aldous C,
Govender PS and Madiba TE: Global and country underestimation of
hepatocellular carcinoma (HCC) in 2012 and its implications. Cancer
Epidemiol. 39:284–290. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Nakisige C, Schwartz M and Ndira AO:
Cervical cancer screening and treatment in Uganda. Gynecol Oncol
Rep. 20:37–40. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ferlay J, Ervik M, Lam F, Colombet M, Mery
L, Piñeros M, Znaor A, Soerjomataram I and Bray F: 2018.Global
Cancer Observatory, . Cancer Today. (Lyon, France). International
Agency for Research on Cancer. March
18–2019
|
|
23
|
International Agency for Research on
Cancer, . GLOBOCAN 2012: Estimated cancer incidence, mortality and
prevalence worldwide in 2012. 2012.
|
|
24
|
Chibwesha CJ, Goeieman B, Levin S, Mulongo
M, Faesen M, Swarts A, Ramotshela S, Williams S, Rakhombe N, Bruce
S, et al: Estimating the burden of cervical disease among
HIV-infected women accessing screening services in South Africa: A
model-based analysis. S Afr Med J. 108:235–239. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Simonds HM, Wright JD, du Toit N, Neugut
AI and Jacobson JS: Completion of and early response to
chemoradiation among human immunodeficiency virus (HIV)-positive
and HIV-negative patients with locally advanced cervical carcinoma
in South Africa. Cancer. 118:2971–2979. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
UNAIDS, . UNAIDS Terminology Guidelines.
June
13–2019
|
|
27
|
UNAIDS, . Report on the global HIV/AIDS
epidemic. UNAIDS2002. http://data.unaids.org/pub/report/2002/brglobal_aids_report_en_pdf_red_en.pdfJune
13–2019
|
|
28
|
Jacobson G, Chuang L and Pankow M:
Improving quality of care and timely access to radiation therapy
for patients with invasive cervical cancer at the National Cancer
Institute Paraguay. Gynecol Oncol Rep. 25:82–86. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Bosch FX, Broker TR, Forman D, Moscicki
AB, Gillison ML, Doorbar J, Stern PL, Stanley M, Arbyn M, Poljak M,
et al: Comprehensive control of human papillomavirus infections and
related diseases. Vaccine. 31 (Suppl 7):H1–H31. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Forman D, de Martel C, Lacey CJ,
Soerjomataram I, Lortet-Tieulent J, Bruni L, Vignat J, Ferlay J,
Bray F, Plummer M, et al: Global burden of human papillomavirus and
related diseases. Vaccine. 30 (Suppl 5):F12–F23. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ginsburg O, Bray F, Coleman MP, Vanderpuye
V, Eniu A, Kotha SR, Sarker M, Huong TT, Allemani C, Dvaladze A, et
al: The global burden of women's cancers: A grand challenge in
global health. Lancet. 389:847–860. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Fields MM: New cervical cancer screening
guidelines: Was the annual pap too much of a good thing? J Adv
Pract Oncol. 4:59–64. 2013.PubMed/NCBI
|
|
33
|
Moyer VA; U.S. Preventive Services Task
Force, : Screening for cervical cancer: U.S. Preventive Services
Task Force recommendation statement. Ann Intern Med. 156:880–891,
W312. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Botha MH and Dochez C: Introducing human
papillomavirus vaccines into the health system in South Africa.
Vaccine. 30 (Suppl 3):C28–C34. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
South African National Cancer Registry, .
Cancer in South Africa 2014. (Johannesburg). 2014.https://www.nicd.ac.za/wp-content/uploads/2019/12/2014-NCR-tables.pdfJanuary
7–2019
|
|
36
|
Denny L: Cervical cancer: The South
African perspective. FIGO 26th annual report on the results of
treatment in gynecological cancer. Int J Gynaecol Obstet. 95 (Suppl
1):S211–S214. 2006. View Article : Google Scholar
|
|
37
|
Bekker LG, Venter F, Cohen K, Goemare E,
Van Cutsem G, Boulle A and Wood R: Provision of antiretroviral
therapy in South Africa: The nuts and bolts. Antivir Ther. 19
(Suppl 3):S105–S116. 2014. View Article : Google Scholar
|
|
38
|
Dreyer G: Clinical implications of the
interaction between HPV and HIV infections. Best Pract Res Clin
Obstet Gynaecol. 47:95–106. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Mbulawa ZZA, Coetzee D and Williamson AL:
Human papillomavirus prevalence in South African women and men
according to age and human immunodeficiency virus status. BMC
Infect Dis. 15:459. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Tathiah N, Naidoo M and Moodley I: Human
papillomavirus (HPV) vaccination of adolescents in the South
African private health sector: Lessons from the HPV demonstration
project in KwaZulu-Natal. S Afr Med J. 105:9542015. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Lovgren K, Soliman AS, Ngoma T, Kahesa C
and Meza J: Characteristics and geographic distribution of
HIV-positive women diagnosed with cervical cancer in Dar es Salaam,
Tanzania. Int J STD AIDS. 27:1049–1056. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
McCree R, Giattas MR, Sahasrabuddhe VV,
Jolly PE, Martin MY, Usdan SL, Kohler C and Lisovicz N: Expanding
cervical cancer screening and treatment in Tanzania: Stakeholders'
perceptions of structural influences on scale-up. Oncologist.
20:621–626. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Ardahan M and Temel AB: Visual inspection
with acetic acid in cervical cancer screening. Cancer Nursing.
34:158–163. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Gross K, Armstrong Schellenberg J, Kessy
F, Pfeiffer C and Obrist B: Antenatal care in practice: An
exploratory study in antenatal care clinics in the Kilombero
Valley, south-eastern Tanzania. BMC Pregnancy Childbirth.
11:362011. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Runge AS, Bernstein ME, Lucas AN and
Tewari KS: Cervical cancer in Tanzania: A systematic review of
current challenges in six domains. Gynecol Oncol Rep. 29:40–47.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Mishra GA, Pimple SA and Shastri SS:
Prevention of cervix cancer in India. Oncology. 91 (Suppl 1):S1–S7.
2016. View Article : Google Scholar
|
|
47
|
Senapathy JG, Umadevi P and Kannika PS:
The present scenario of cervical cancer control and HPV
epidemiology in India: An outline. Asian Pac J Cancer Prev.
12:1107–1115. 2011.PubMed/NCBI
|
|
48
|
Gheit T, Vaccarella S, Schmitt M, Pawlita
M, Franceschi S, Sankaranarayanan R, Sylla BS, Tommasino M and
Gangane N: Prevalence of human papillomavirus types in cervical and
oral cancers in central India. Vaccine. 27:636–639. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Deodhar K, Gheit T, Vaccarella S, Romao
CC, Tenet V, Nene BM, Jayant K, Kelkar R, Malvi SG, Sylla BS, et
al: Prevalence of human papillomavirus types in cervical lesions
from women in rural Western India. J Med Virol. 84:1054–1060. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Chatterjee S, Chattopadhyay A, Samanta L
and Panigrahi P: HPV and cervical cancer epidemiology-current
status of HPV vaccination in India. Asian Pac J Cancer Prev.
17:3663–3673. 2016.PubMed/NCBI
|
|
51
|
Mattheij I, Pollock AM and Brhlikova P: Do
cervical cancer data justify HPV vaccination in India?
Epidemiological data sources and comprehensiveness. J R Soc Med.
105:250–262. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Lopez MS, Baker ES, Maza M, Fontes-Cintra
G, Lopez A, Carvajal JM, Nozar F, Fiol V and Schmeler KM: Cervical
cancer prevention and treatment in Latin America. J Surg Oncol.
115:615–618. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
HPV information centre, . Brazil human
papillomavirus and related cancers, fact sheet 2018 ICO/IARC
information centre on HPV and cancer, 2018. https://hpvcentre.net/statistics/reports/BRA_FS.pdfApril
17–2019
|
|
54
|
Napa LI: Cervical Cancer Screening:
Awareness and knowledge in Brazil. Clin Social Work Health
Intervention. 55–61. 2016. View Article : Google Scholar
|
|
55
|
Lorenzi AT, Syrjänen KJ and Longatto-Filho
A: Human papillomavirus (HPV) screening and cervical cancer burden.
A Brazilian perspective. Virol J. 12:112. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Cohen PA, Jhingran A, Oaknin A and Denny
L: Cervical cancer. Lancet. 393:169–182. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Castellsagué X and Muñoz N: Chapter 3:
Cofactors in human papillomavirus carcinogenesis-role of parity,
oral contraceptives, and tobacco smoking. J Natl Cancer Inst
Monogr. 20–28. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Chatzistamatiou K, Katsamagas T, Zafrakas
M, Zachou K, Orologa A, Fitsiou F, Theodoridis T, Konstantinidis T,
Konstantinidis TC and Agorastos T: Smoking and genital human
papilloma virus infection in women attending cervical cancer
screening in Greece. World J Obstet Gynecol. 2:53–61. 2013.
View Article : Google Scholar
|
|
59
|
Pista A, de Oliveira CF, Cunha MJ, Paixao
MT and Real O; CLEOPATRE Portugal Study Group, : Risk factors for
human papillomavirus infection among women in Portugal: The
CLEOPATRE Portugal Study. Int J Gynaecol Obstet. 118:112–116. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
International Collaboration of
Epidemiological Studies of Cervical Cancer, . Comparison of risk
factors for invasive squamous cell carcinoma and adenocarcinoma of
the cervix: Collaborative reanalysis of individual data on 8,097
women with squamous cell carcinoma and 1,374 women with
adenocarcinoma from 12 epidemiological studies. Int J Cancer.
120:885–891. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
International Collaboration of
Epidemiological Studies of Cervical Cancer, . Appleby P, Beral V,
Berrington de González A, Colin D, Franceschi S, Goodhill A, Green
J, Peto J, Plummer M and Sweetland S: Cervical cancer and hormonal
contraceptives: Collaborative reanalysis of individual data for
16,573 women with cervical cancer and 35,509 women without cervical
cancer from 24 epidemiological studies. Lancet. 370:1609–1621.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Haverkos HW: Multifactorial etiology of
cervical cancer: A hypothesis. MedGenMed. 7:572005.PubMed/NCBI
|
|
63
|
Haverkos HW, Haverkos GP and O'Mara M:
Co-carcinogenesis: Human papillomaviruses, coal tar derivatives,
and squamous cell cervical cancer. Front Microbiol. 8:22532017.
View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Muñoz N, Castellsagué X, de González AB
and Gissmann L: HPV in the etiology of human cancer. Vaccine. 24
(Suppl 3):S1–S10. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Goodson WH III, Lowe L, Carpenter DO,
Gilbertson M, Manaf Ali A, Lopez de Cerain Salsamendi A, Lasfar A,
Carnero A, Azqueta A, Amedei A, et al: Assessing the carcinogenic
potential of low-dose exposures to chemical mixtures in the
environment: The challenge ahead. Carcinogenesis. 36 (Suppl
1):S254–S296. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Velema JP, Ferrera A, Figueroa M, Bulnes
R, Toro LA, de Barahona O, Claros JM and Melchers WJ: Burning wood
in the kitchen increases the risk of cervical neoplasia in
HPV-infected women in Honduras. Int J Cancer. 97:536–541. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Bennett C, Kuhn AE and Haverkos HW: Human
papillomavirus and tar hypothesis for squamous cell cervical
cancer. J Biosci. 35:331–337. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Fujiki H: Gist of Dr. Katsusaburo
Yamagiwa's papers entitled ‘Experimental study on the pathogenesis
of epithelial tumors’ (I to VI reports). Cancer Sci. 105:143–149.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Rotkin ID: Epidemiology of cancer of the
cervix. 3. Sexual characteristics of a cervical cancer population.
Am J Public Health Nations Health. 57:815–829. 1967. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Karki R, Pandya D, Elston RC and Ferlini
C: Defining ‘mutation’ and ‘polymorphism’ in the era of personal
genomics. BMC Med Genomics. 8:37. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Mehta AM, Mooij M, Brankovic I, Ouburg S,
Morre SA and Jordanova ES: Cervical carcinogenesis and immune
response gene polymorphisms: A review. J Immunol Res.
2017:89138602017. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
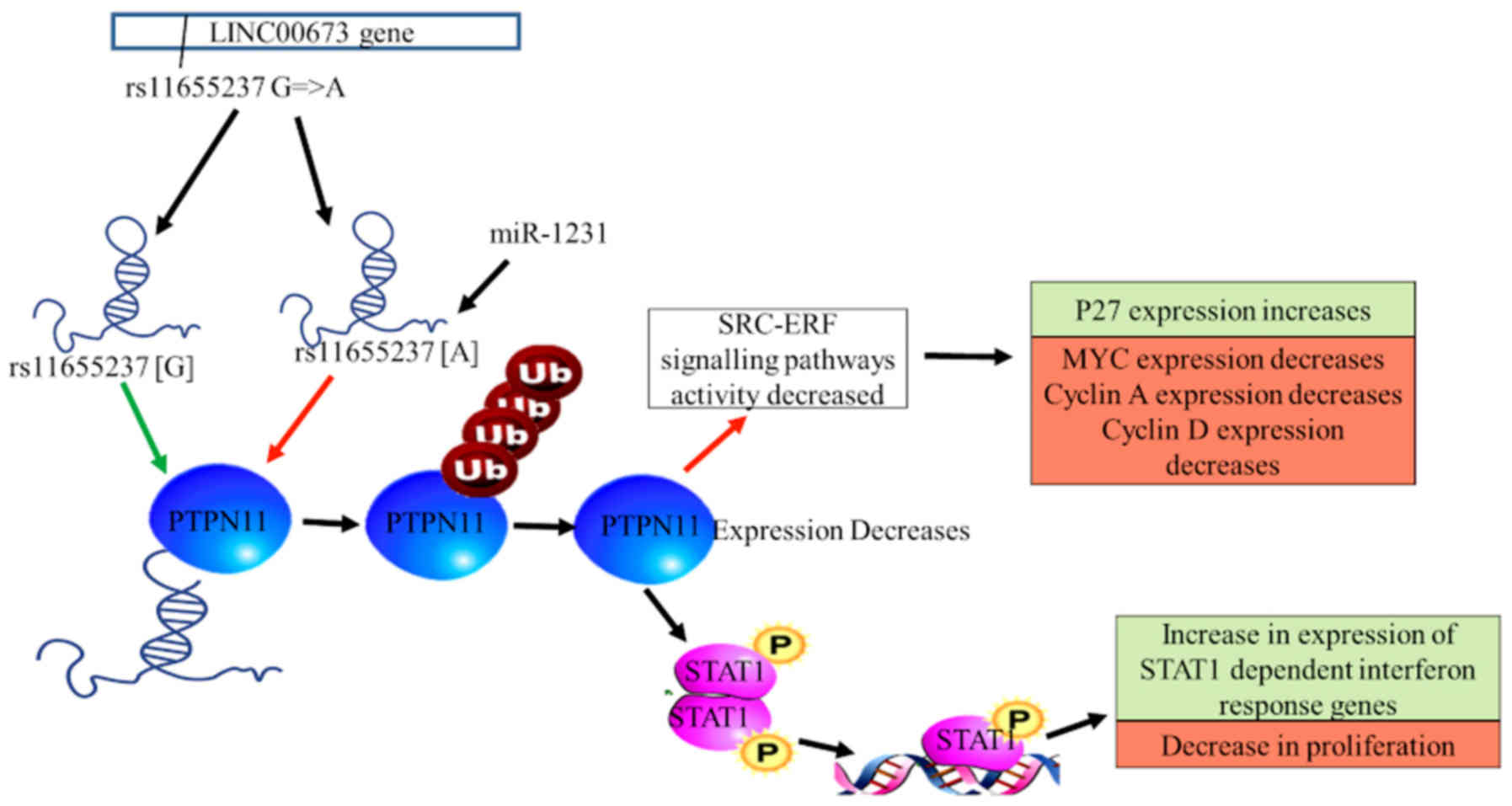
Wang Y and Luo T: LINC00673 rs11655237
polymorphism is associated with increased risk of cervical cancer
in a Chinese population. Cancer Control. 25:10732748188039422018.
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Lu W, Zhang H, Niu Y, Wu Y, Sun W, Li H,
Kong J, Ding K, Shen HM, Wu H, et al: Long non-coding RNA linc00673
regulated non-small cell lung cancer proliferation, migration,
invasion and epithelial mesenchymal transition by sponging
miR-150-5p. Mol Cancer. 16:1182017. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Zheng J, Huang X, Tan W, Yu D, Du Z, Chang
J, Wei L, Han Y, Wang C, Che X, et al: Pancreatic cancer risk
variant in LINC00673 creates a miR-1231 binding site and interferes
with PTPN11 degradation. Nat Genet. 48:747–757. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Weng SL, Wu WJ, Hsiao YH, Yang SF, Hsu CF
and Wang PH: Significant association of long non-coding RNAs HOTAIR
genetic polymorphisms with cancer recurrence and patient survival
in patients with uterine cervical cancer. Int J Med Sci.
15:1312–1319. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Pan W, Liu L, Wei J, Ge Y, Zhang J, Chen
H, Zhou L, Yuan Q, Zhou C and Yang M: A functional lncRNA HOTAIR
genetic variant contributes to gastric cancer susceptibility. Mol
Carcinog. 55:90–96. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Chu H, Chen Y, Yuan Q, Hua Q, Zhang X,
Wang M, Tong N, Zhang W, Chen J and Zhang Z: The HOTAIR, PRNCR1 and
POLR2E polymorphisms are associated with cancer risk: A
meta-analysis. Oncotarget. 8:43271–43283. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Yang Y, Liu Y, Li G, Li L, Geng P and Song
H: microRNA-214 suppresses the growth of cervical cancer cells by
targeting EZH2. Oncol Lett. 16:5679–5686. 2018.PubMed/NCBI
|
|
79
|
Pandey NO, Chauhan AV, Raithatha NS, Patel
PK, Khandelwal R, Desai AN, Choxi Y, Kapadia RS and Jain ND:
Association of TLR4 and TLR9 polymorphisms and haplotypes with
cervical cancer susceptibility. Sci Rep. 9:9729. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Fehri E, Ennaifer E, Ardhaoui M, Ouerhani
K, Laassili T, Bel Haj Rhouma R, Guizani I and Boubaker S:
Expression of Toll-like receptor 9 increases with progression of
cervical neoplasia in Tunisian women-a comparative analysis of
condyloma, cervical intraepithelial neoplasia and invasive
carcinoma. Asian Pac J Cancer Prev. 15:6145–6150. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
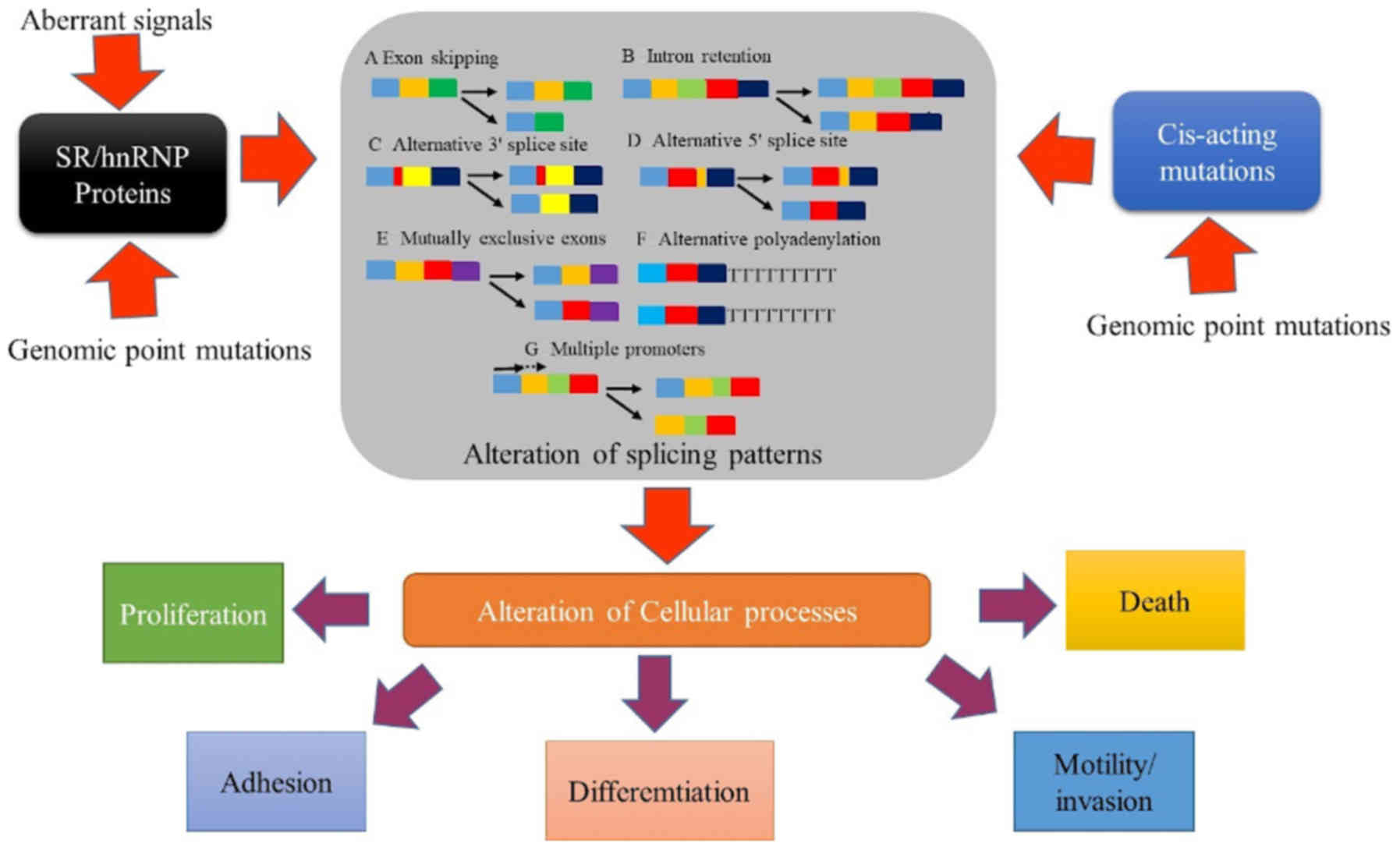
Stamm S, Ben-Ari S, Rafalska I, Tang Y,
Zhang Z, Toiber D, Thanaraj TA and Soreq H: Function of alternative
splicing. Gene. 344:1–20. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Chen M and Manley JL: Mechanisms of
alternative splicing regulation: Insights from molecular and
genomics approaches. Nat Rev Mol Cell Biol. 10:741–754. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Tazi J, Bakkour N and Stamm S: Alternative
splicing and disease. Biochim Biophys Acta. 1792:14–26. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Gonçalves V, Pereira JFS and Jordan P:
Signaling pathways driving aberrant splicing in cancer cells. Genes
(Basel). 9:E92017. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Irimia M and Roy SW: Origin of
spliceosomal introns and alternative splicing. Cold Spring Harb
Perspect Biol. 6:a0160712014. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Skotheim RI and Nees M: Alternative
splicing in cancer: Noise, functional, or systematic? Int J Biochem
Cell Biol. 39:1432–1449. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Faustino NA and Cooper TA: Pre-mRNA
splicing and human disease. Genes Dev. 17:419–437. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Bisognin A, Pizzini S, Perilli L, Esposito
G, Mocellin S, Nitti D, Zanovello P, Bortoluzzi S and Mandruzzato
S: An integrative framework identifies alternative splicing events
in colorectal cancer development. Mol Oncol. 8:129–141. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Pal S, Gupta R and Davuluri RV:
Alternative transcription and alternative splicing in cancer.
Pharmacol Ther. 136:283–294. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Chen X, Du H, Liu B, Zou L, Chen W, Yang
Y, Zhu Y, Gong Y, Tian J, Li F and Zhong S: The associations
between RNA splicing complex gene SF3A1 polymorphisms and
colorectal cancer risk in a Chinese population. PLoS One.
10:e01303772015. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Tian J, Liu Y, Zhu B, Tian Y, Zhong R,
Chen W, Lu X, Zou L, Shen N, Qian J, et al: SF3A1 and pancreatic
cancer: New evidence for the association of the spliceosome and
cancer. Oncotarget. 6:37750–37757. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Yoshida K, Sanada M, Shiraishi Y, Nowak D,
Nagata Y, Yamamoto R, Sato Y, Sato-Otsubo A, Kon A, Nagasaki M, et
al: Frequent pathway mutations of splicing machinery in
myelodysplasia. Nature. 478:64–69. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Liu F, Dai M, Xu Q, Zhu X, Zhou Y, Jiang
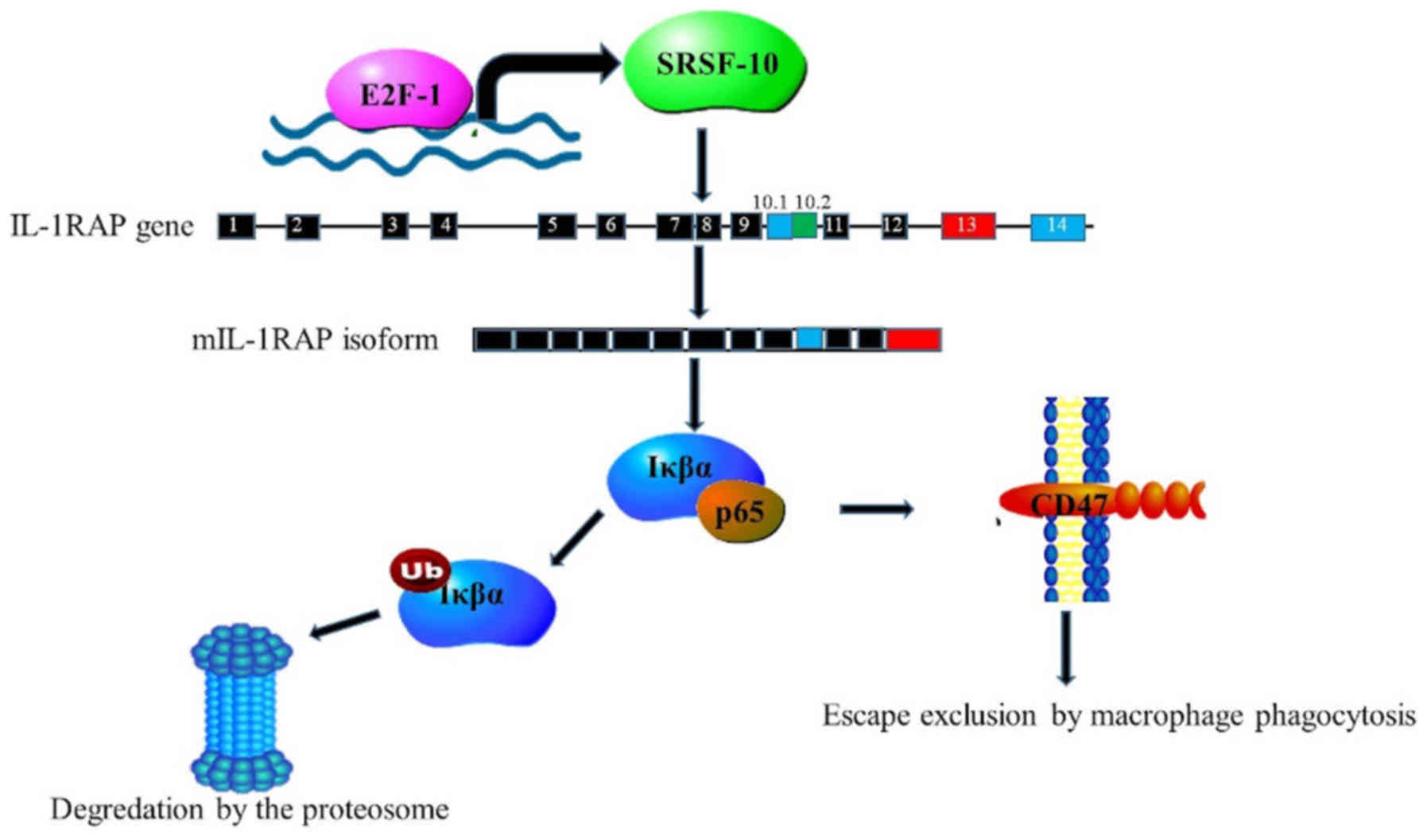
S, Wang Y, Ai Z, Ma L, Zhang Y, et al: SRSF10-mediated IL1RAP
alternative splicing regulates cervical cancer oncogenesis via
mIL1RAP-NF-κB-CD47 axis. Oncogene. 37:2394–2409. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Liu B, Tian Y, Li F, Zhao Z, Jiang X, Zhai
C, Han X and Zhang L: Tumor-suppressing roles of miR-214 and
miR-218 in breast cancer. Oncol Rep. 35:3178–3184. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Korneev KV, Atretkhany KN, Drutskaya MS,
Grivennikov SI, Kuprash DV and Nedospasov SA: TLR-signaling and
proinflammatory cytokines as drivers of tumorigenesis. Cytokine.
89:127–135. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Zidi S, Sghaier I, Gazouani E, Mezlini A
and Yacoubi-Loueslati B: Evaluation of Toll-Like receptors 2/3/4/9
gene polymorphisms in cervical cancer evolution. Pathol Oncol Res.
22:323–330. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
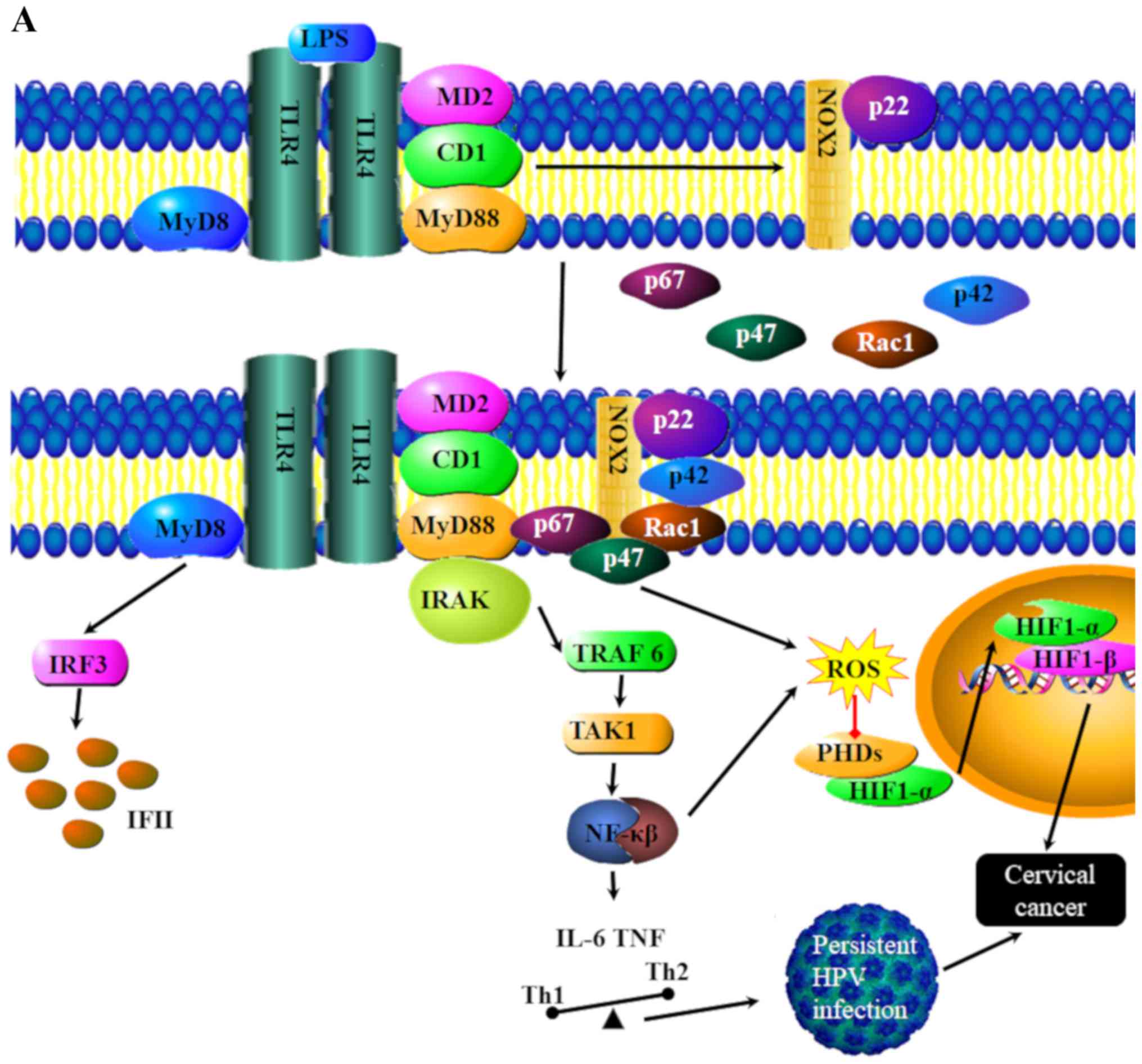
Yang X, Cheng Y and Li C: The role of TLRs
in cervical cancer with HPV infection: A review. Signal Transduct
Target Ther. 2:170552017. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Urban-Wojciuk Z, Khan MM, Oyler BL,
Fåhraeus R, Marek-Trzonkowska N, Nita-Lazar A, Hupp TR and Goodlett
DR: The role of TLRs in anti-cancer immunity and tumor rejection.
Front Immunol. 10:23882019. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Zhou Q, Zhu K and Cheng H: Toll-like
receptors in human papillomavirus infection. Arch Immunol Ther Exp
(Warsz). 61:203–215. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Hasimu A, Ge L, Li QZ, Zhang RP and Guo X:
Expressions of Toll-like receptors 3, 4, 7, and 9 in cervical
lesions and their correlation with HPV16 infection in Uighur women.
Chin J Cancer. 30:344–350. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
DeCarlo CA, Rosa B, Jackson R, Niccoli S,
Escott NG and Zehbe I: Toll-like receptor transcriptome in the
HPV-positive cervical cancer microenvironment. Clin Dev Immunol.
2012:7858252012. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Daud II, Scott ME, Ma Y, Shiboski S,
Farhat S and Moscicki AB: Association between toll-like receptor
expression and human papillomavirus type 16 persistence. Int J
Cancer. 128:879–886. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Hasan UA, Bates E, Takeshita F, Biliato A,
Accardi R, Bouvard V, Mansour M, Vincent I, Gissmann L, Iftner T,
et al: TLR9 expression and function is abolished by the cervical
cancer-associated human papillomavirus type 16. J Immunol.
178:3186–3197. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Hasan UA, Zannetti C, Parroche P, Goutagny
N, Malfroy M, Roblot G, Carreira C, Hussain I, Müller M,
Taylor-Papadimitriou J, et al: The human papillomavirus type 16 E7
oncoprotein induces a transcriptional repressor complex on the
Toll-like receptor 9 promoter. J Exp Med. 210:1369–1387. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Zolini GP, Lima GK, Lucinda N, Silva MA,
Dias MF, Pessoa NL, Coura BP, Cartelle CT, Arantes RM, Kroon EG and
Campos MA: Defense against HSV-1 in a murine model is mediated by
iNOS and orchestrated by the activation of TLR2 and TLR9 in
trigeminal ganglia. J Neuroinflammation. 11:202014. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Parroche P, Roblot G, Le Calvez-Kelm F,
Tout I, Marotel M, Malfroy M, Durand G, McKay J, Ainouze M,
Carreira C, et al: TLR9 re-expression in cancer cells extends the
S-phase and stabilizes p16(INK4a) protein expression. Oncogenesis.
5:e2442016. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Kaur G and Sethi RS: Multiple exposures to
poultry barn air and lipopolysaccharide synergistically increase
the pulmonary expression of TLR-4 and IL-1β. J Occup Health. Oct
27–2019.(Epub ahead of print). doi: 10.1002/1348-9585.12094.
PubMed/NCBI
|
|
108
|
Felekkis K, Touvana E, Stefanou C and
Deltas C: microRNAs: A newly described class of encoded molecules
that play a role in health and disease. Hippokratia. 14:236–240.
2010.PubMed/NCBI
|
|
109
|
Calin GA, Dumitru CD, Shimizu M, Bichi R,
Zupo S, Noch E, Aldler H, Rattan S, Keating M, Rai K, et al:
Frequent deletions and down-regulation of micro- RNA genes miR15
and miR16 at 13q14 in chronic lymphocytic leukemia. Proc Natl Acad
Sci USA. 99:15524–15529. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Deng Y, Xiong Y and Liu Y: miR-376c
inhibits cervical cancer cell proliferation and invasion by
targeting BMI1. Int J Exp Pathol. 97:257–265. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Zhang B, Pan X, Cobb GP and Anderson TA:
microRNAs as oncogenes and tumor suppressors. Dev Biol. 302:1–12.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Fan Z, Cui H, Yu H, Ji Q, Kang L, Han B,
Wang J, Dong Q, Li Y, Yan Z, et al: MiR-125a promotes paclitaxel
sensitivity in cervical cancer through altering STAT3 expression.
Oncogenesis. 5:e2232016. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Fang W, Shu S, Yongmei L, Endong Z, Lirong
Y and Bei S: miR-224-3p inhibits autophagy in cervical cancer cells
by targeting FIP200. Sci Rep. 6:332292016. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Huang P, Xi J and Liu S: MiR-139-3p
induces cell apoptosis and inhibits metastasis of cervical cancer
by targeting NOB1. Biomed Pharmacother. 83:850–856. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Cheng X, Chen J and Huang Z: miR-372
promotes breast cancer cell proliferation by directly targeting
LATS2. Exp Ther Med. 15:2812–2817. 2018.PubMed/NCBI
|
|
116
|
Liao J, Lin J, Lin D, Zou C, Kurata J, Lin
R, He Z and Su Y: Down-regulation of miR-214 reverses erlotinib
resistance in non-small-cell lung cancer through up-regulating LHX6
expression. Sci Rep. 7:7812017. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Lu Q, Xu L, Li C, Yuan Y, Huang S and Chen
H: miR-214 inhibits invasion and migration via downregulating
GALNT7 in esophageal squamous cell cancer. Tumour Biol.
37:14605–14614. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Xia D, Li X, Niu Q, Liu X, Xu W, Ma C, Gu
H, Liu Z, Shi L, Tian X, et al: MicroRNA-185 suppresses pancreatic
cell proliferation by targeting transcriptional coactivator with
PDZ-binding motif in pancreatic cancer. Exp Ther Med. 15:657–666.
2018.PubMed/NCBI
|
|
119
|
Yu G, Wang J, Xu K and Dong J: Dynamic
regulation of uncoupling protein 2 expression by microRNA-214 in
hepatocellular carcinoma. Biosci Rep. 36:e003352016. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Zhu X, Ju S, Yuan F, Chen G, Shu Y, Li C,
Xu Y, Luo J and Xia L: microRNA-664 enhances proliferation,
migration and invasion of lung cancer cells. Exp Ther Med.
13:3555–3562. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Chen Z, Wang M, He Q, Li Z, Zhao Y, Wang
W, Ma J, Li Y and Chang G: MicroRNA-98 rescues proliferation and
alleviates ox-LDL-induced apoptosis in HUVECs by targeting LOX-1.
Exp Ther Med. 13:1702–1710. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Zhu Y, Wu G, Yan W, Zhan H and Sun P:
miR-146b-5p regulates cell growth, invasion, and metabolism by
targeting PDHB in colorectal cancer. Am J Cancer Res. 7:1136–1150.
2017.PubMed/NCBI
|
|
123
|
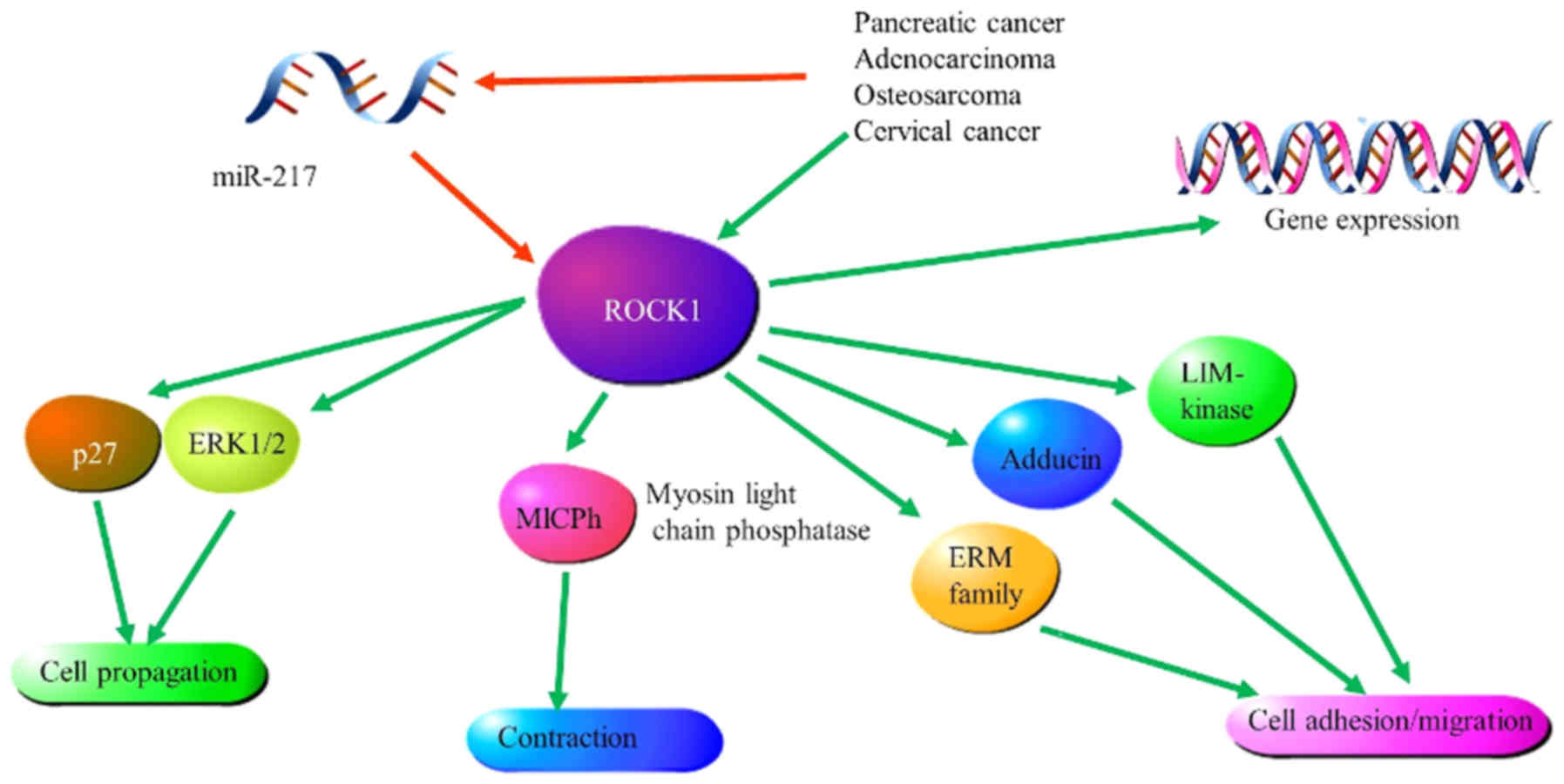
Dong J, Wang M, Ni D, Zhang L, Wang W, Cui
X, Fu S and Yao S: MicroRNA-217 functions as a tumor suppressor in
cervical cancer cells through targeting Rho-associated protein
kinase 1. Oncoly Lett. 16:5535–5542. 2018.
|
|
124
|
Scarinci IC, Garcia FAR, Kobetz E,
Partridge EE, Brandt HM, Bell MC, Dignan M, Ma GX, Daye JL and
Castle PE: Cervical cancer prevention: New tools and old barriers.
Cancer. 116:2531–2542. 2010.PubMed/NCBI
|
|
125
|
Adesina A, Chumba D, Nelson AM, Orem J,
Roberts DJ, Wabinga H, Wilson M and Rebbeck TR: Improvement of
pathology in sub-Saharan Africa. Lancet Oncol. 14:e152–e157. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Gelband H, Sankaranarayanan R, Gauvreau
CL, Horton S, Anderson BO, Bray F, Cleary J, Dare AJ, Denny L,
Gospodarowicz MK, et al: Costs, affordability, and feasibility of
an essential package of cancer control interventions in low-income
and middle-income countries: Key messages from Disease Control
Priorities, 3rd edition. Lancet. 387:2133–2144. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Goss PE, Lee BL, Badovinac-Crnjevic T,
Strasser-Weippl K, Chavarri-Guerra Y, St Louis J, Villarreal-Garza
C, Unger-Saldaña K, Ferreyra M, Debiasi M, et al: Planning cancer
control in Latin America and the Caribbean. Lancet Oncol.
14:391–436. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Jit M, Brisson M, Portnoy A and Hutubessy
R: Cost-effectiveness of female human papillomavirus vaccination in
179 countries: A PRIME modelling study. Lancet Glob Health.
2:e406–e414. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Schiller JT, Castellsagué X and Garland
SM: A review of clinical trials of human papillomavirus
prophylactic vaccines. Vaccine. 30:F123–F138. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
FUTURE II Study Group, : Quadrivalent
vaccine against human papillomavirus to prevent high-grade cervical
lesions. N Engl J Med. 356:1915–1927. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Joura EA, Giuliano AR, Iversen OE,
Bouchard C, Mao C, Mehlsen J, Moreira ED Jr, Ngan Y, Petersen LK,
Lazcano-Ponce E, et al: A 9-valent HPV vaccine against infection
and intraepithelial neoplasia in women. N Engl J Med. 372:711–723.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Levin A, Wang SA, Levin C, Tsu V and
Hutubessy R: Costs of introducing and delivering HPV vaccines in
low and lower middle income countries: Inputs for GAVI policy on
introduction grant support to countries. PLoS One. 9:e1011142014.
View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Goldie SJ, Gaffikin L, Goldhaber-Fiebert
JD, Gordillo-Tobar A, Levin C, Mahé C and Wright TC; Alliance for
Cervical Cancer Prevention Cost Working Group, : Cost-effectiveness
of cervical-cancer screening in five developing countries. N Engl J
Med. 353:2158–2168. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Cronjé HS and Beyer E: Screening for
cervical cancer in an African setting. Int J Gynaecol Obstet.
98:168–171. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Gakidou E, Nordhagen S and Obermeyer Z:
Coverage of cervical cancer screening in 57 countries: Low average
levels and large inequalities. PLoS Med. 5:e1322008. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Wake RM, Rebe K and Burch VC: Patient
perception of cervical screening among women living with human
immuno-deficiency virus infection attending an antiretroviral
therapy clinic in urban South Africa. J Obstet Gynaecol. 29:44–48.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Gopal S, Achenbach CJ, Yanik EL, Dittmer
DP, Eron JJ and Engels EA: Moving forward in HIV-associated cancer.
J Clin Oncol. 32:876–880. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Bruggmann D, Kayser L, Jaque J, Bundschuh
M, Klingelhöfer D and Groneberg DA: Human papilloma virus: Global
research architecture assessed by density-equalizing mapping.
Oncotarget. 9:21965–21977. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Ndejjo R, Mukama T, Musabyimana A and
Musoke D: Uptake of cervical cancer screening and associated
factors among women in Rural Uganda: A cross sectional study. PLoS
One. 11:e01496962016. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Idehen EE, Korhonen T, Castaneda A,
Juntunen T, Kangasniemi M, Pietilä AM and Koponen P: Factors
associated with cervical cancer screening participation among
immigrants of Russian, Somali and Kurdish origin: A
population-based study in Finland. BMC Women Health. 17:192017.
View Article : Google Scholar
|
|
141
|
Marlow LA, Wardle J and Waller J:
Understanding cervical screening non-attendance among ethnic
minority women in England. Br J Cancer. 113:833–839. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Olsson E, Lau M, Lifvergren S and
Chakhunashvili A: Community collaboration to increase foreign-born
women's participation in a cervical cancer screening program in
Sweden: A quality improvement project. Int J Equity Health.
13:622014. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Raine R, Fitzpatrick R, Barratt H, Bevan
G, Black N, Boaden R, Bower P, Campbell M, Denis JL, Devers K, et
al: Challenges, solutions and future directions in the evaluation
of service innovations in health care and public health. Health
Services and Delivery Researc. 4:162016.
|
|
144
|
Karl-Trummer U and Sardadvar S: The
interplay of health, migrant status and socioeconomic status in
eight EU countries. Health inequalities and risk factors among
migrants and ethnic minorities. COST Series Health Div. 1:79–92.
2012.
|
|
145
|
Simon J, Kiss N, Łaszewska A and Mayer S:
Public health aspects of migrant health: a review of the evidence
on health status for labour migrants in the European Region. World
Health Organisation Regional Office for Europe. 2015.
|
|
146
|
Kunckler M, Schumacher F, Kenfack B,
Catarino R, Viviano M, Tincho E, Tebeu PM, Temogne L, Vassilakos P
and Petignat P: Cervical cancer screening in a low-resource
setting: A pilot study on an HPV-based screen-and-treat approach.
Cancer Med. 6:1752–1761. 2017. View Article : Google Scholar : PubMed/NCBI
|