Introduction
Oral cancer is a common malignancy worldwide, with
an estimated 53,260 new cases and 10,750 deaths in 2020 (1). Oral squamous cell carcinoma (OSCC),
which accounts for more than 90% of all malignant tumors of the
oral cavity, is mainly treated by surgery, radiotherapy, and
adjuvant chemotherapy. The prognosis in patients with early-stage
OSCC has substantially improved (2).
However, the overall survival rate in patients with advanced OSCC
has not improved significantly during the past four decades
(3). New approaches to early
detection, risk assessment, and early intervention are ongoing to
improve the survival in patients with OSCC. Therefore, studies
elucidating the oncological behavior of OSCC are needed.
The presence of pigmented melanocytes in
non-melanocytic neoplasms has been documented in various entities
in several sites, such as neuroendocrine carcinoma (4), breast carcinoma (5), and salivary gland tumor (6). Squamous cell carcinoma (SCC)
occasionally shows pleomorphic histological forms with several
subtypes. Among them, SCC with proliferating dendritic melanocytes
is a rare entity that has been reported in the skin (7), uterine cervix (8), conjunctiva (9), nasal cavity (10), scrotum (11), and external auditory canal (12). The clinical course of pigmented SCC
in these regions is nearly the same as that of nonpigmented SCCs,
and the prognosis is similar to that of the conventional SCC
(7,10–12).
Although pigmentation, commonly found in the oral
mucosa, represents various clinical patterns ranging from
physiological alterations to oral manifestations of systemic
diseases and malignancies, pigmented oral squamous cell carcinoma
(POSCC) is a rare and underrecognized pathological variant of OSCC.
To the best of our knowledge, only 18 cases have been reported in
the English literature (13–22). Owing to the lack of a large case
series, the clinical characteristics, treatment outcomes, and
prognosis of POSCC remain unclear.
Several types of biological markers have been used
to investigate the biological and clinical behavior of OSCC and
head and neck SCC. However, only a few reports on the use of these
biological markers for POSCC are available. p53 is a tumor
suppressor gene that regulates cell cycle control, apoptosis, and
preservation of genetic stability (23). In head and neck SCC, p53 mutations
acquire oncogenic functions to promote tumorigenesis and tumor
progression (24). Ki-67 is a
potential marker that reflects the total fraction of cell growth in
a neoplasm and serves as a molecular indicator of survival and
recurrence (25). High Ki-67
expression is a negative prognostic marker in patients with OSCC,
especially in Asian populations (25). E-cadherin and vimentin are useful
indicators of the epithelial-mesenchymal transition (EMT), a
critical biological event in which cohesive and polarized
epithelial cells switch to mesenchyme-like cells exhibiting no
polarization and high mobility (26). This acquired migratory phenotype is
essential for tumor growth, particularly during tumor invasion and
metastasis. A previous study showed that overexpression of EMT
factors was significantly associated with a poor prognosis and
could serve as a prognostic factor for head and neck SCC (26). Despite the great interest in the
potential malignancy and pathophysiology of POSCC, there have been
no studies on the biological properties of these molecules in POSCC
because of the rarity of disease occurence.
Therefore, this study aimed to evaluate the
clinicopathological characteristics, treatment outcomes, and
prognosis in patients with POSCC and to investigate the oncological
properties of POSCC via immunohistochemical analysis of p53, Ki-67,
E-cadherin, and vimentin expression.
Materials and methods
Patients and tissue specimens
We retrospectively evaluated all patients diagnosed
as having pathologically-confirmed SCC of the oral cavity, who were
treated at the Department of Oral and Maxillofacial Surgery, Tokyo
Medical and Dental University between January 2001 and December
2018. Pigmented lesions were observed in 26 out of the 1,512
patients. One patient with metal-derived pigmentation, which was
determined using the bleaching method, was excluded. Therefore, a
total of 25 patients (1.7% of all patients) were included in this
study. Clinical data on age, sex, primary location of the tumor,
TNM classification, stage, treatment, surgical margins,
pathological cervical lymph node metastases, locoregional
recurrence, and prognosis were obtained from their medical records.
Clinical staging was based on the TNM staging system of the Union
for International Cancer Control, 7th edition (27). The patterns of invasion in the
samples were analyzed according to the method used by Anneroth
et al (28) and subsequently
classified as either low-invasive OSCC (patterns of invasion grades
1, 2, or 3) or high-invasive OSCC (pattern of invasion grade 4)
(29). The patients were followed up
for a median of 1,789 days (interquartile range, 78–4372).
The specimens were fixed in 10% formalin, embedded
in paraffin, and cut into 4-µm sub-serial sections. All hematoxylin
and eosin-stained surgical slides were reviewed, and representative
blocks were selected for each patient. The sections were processed
with a bleaching method using potassium permanganate to ensure that
the pigments were melanin (30).
Furthermore, we assessed whether the melanocyte loading was
opposite to the submucosal inflammation. Submucosal inflammation
surrounding the pigmented and nonpigmented areas was evaluated via
hematoxylin and eosin staining based on inflammatory infiltration
rich in lymphocytes and neutrophils.
Immunohistochemistry
The paraffin blocks of the specimens were cut into
4-µm sections and examined immunohistochemically. The sections were
deparaffinized with xylene and rehydrated through a series of
graded alcohol concentrations, following which they were
transferred and rinsed with phosphate-buffered saline (PBS) (Dako
Denmark A/S). The epitopes were then retrieved by heating the
samples in 0.01 M citrate buffer (pH 6.0) for 30 min. After
cooling, endogenous peroxidase activity was blocked by 3% hydrogen
peroxide in methanol for 30 min. The slides were washed three times
with PBS and incubated overnight at 4°C with monoclonal mouse
antibody HMB45 (dilution 1:100; Dako), monoclonal mouse anti-human
Melan-A (dilution 1:50, clone A103; Dako), monoclonal mouse
anti-human p53 (dilution 1:100, clone DO-7; Dako), monoclonal mouse
anti-human Ki-67 (dilution 1:100, clone MIB-1; Dako), monoclonal
mouse anti-human E-cadherin (dilution 1:500, clone NCH-38; Dako),
or vimentin (RP21) rabbit monoclonal antibody (dilution 1:100, Cell
Marque). The reactive products were detected using a Histofine
SAB-PO Kit (Nichirei Biosciences), followed by the assessment of
color development using 3,3-diaminobenzidine as a chromogen and
Giemsa staining for HMB-45 and Melan-A slides, along with Mayer's
hematoxylin as a counterstain for the remaining groups. Appropriate
positive control sections were processed in parallel. The
specificity of staining was checked in negative control slides in
which a buffer solution substituted the primary specific
antibodies.
The sections were analyzed by two independent
observers who were blinded to the clinical data and outcomes.
Doubtful cases were reassessed, and discrepancies were settled by
consensus. Protein expression was semiquantitatively determined by
visual assessment under a light microscope in three representative
fields on each slide (Olympus System Microscope Model BX43). Image
acquisition was performed with a digital camera (AdvanCam-U3II;
Advan Vision Co.) coupled to the microscope.
For HMB-4 and Melan-A staining, a brown cytoplasmic
and membranous stain was counted as positive (31). For p53 and Ki-67 staining, the result
was considered positive when a brown color appeared in the cell
nuclei. The proportion of positively stained cells was expressed as
a percentage (0–100%) at the invasive tumor front. Low and high
levels of p53 expression were defined as immunostaining in <50%
and ≥50% of epithelial tumor cells, respectively (24). Subsequently, p53 expression was
classified as normal (low expression) and abnormal (no or high
expression). Meanwhile, Ki-67 expression was classified as low and
high if immunostaining occurred in <20% and ≥20% of epithelial
tumor cells, respectively (25).
Staining for E-cadherin (29) was
classified as preserved and reduced if membranous immunostaining
occurred in >50% and ≤50% of epithelial tumor cells,
respectively. The expression of vimentin (29) was classified as negative and positive
if cytoplasmic immunostaining occurred in <10% and ≥10% of
epithelial tumor cells, respectively.
Statistical analyses
Survival analyses were conducted using the
Kaplan-Meier method. Disease-specific survival was measured from
the date of surgery to the date of death from uncontrolled POSCC.
Disease-free survival was measured from the date of surgery to the
date of relapse. The association between p53 and Ki-67 expressions
was analyzed using the Fisher's exact test. The log-rank test was
used to compare differences in survival between the two groups. All
statistical analyses were performed using JMP14 (SAS Institute). A
P-value of <0.05 was considered statistically significant.
Results
Clinicopathological findings and
treatment outcomes
The median age of the patients was 62 (range, 26–85)
years, and there were 13 male and 12 female patients. Table I summarizes the clinicopathological
characteristics of patients. The most common location of POSCC was
the tongue (n=18, 72%), followed by the retromolar trigone (n=3,
12%), buccal mucosa (n=2, 8%), floor of the mouth (n=1, 4%), and
gingiva (n=1, 4%). All pathological T stages of the disease were
observed, and 23 (92%) tumors were diagnosed as T1-T2. The surface
configuration of tumors comprised exophytic (n=6, 24%), ulcerative
(n=5, 20%), indurated (n=7, 28%), and leukoplakic or erythroplakic
(n=7, 28%) types. With regard to differentiation, 20 (80%) tumors
were classified as well differentiated, 4 (16%) as moderately
differentiated, and 1 (4%) as poorly differentiated. Regarding the
pattern of invasion, 13 samples were initially classified as grade
1, 8 as grade 2, 2 as grade 3, and 2 as grade 4. Subsequently,
these scores were dichotomized as 23 (92%) low-invasive and 2 (8%)
high-invasive OSCCs. Three patients developed cervical lymph node
metastases and underwent neck dissection.
 | Table I.Clinicopathological characteristics
of patients (n=25). |
Table I.
Clinicopathological characteristics
of patients (n=25).
| Variables | Number |
|---|
| Age, years |
|
| Median
(range) | 62 (26–85) |
| Sex |
|
|
Male | 13 |
|
Female | 12 |
| Primary site |
|
|
Tongue | 18 |
|
Retromolar trigone | 3 |
| Buccal
mucosa | 2 |
| Floor
of the mouth | 1 |
|
Gingiva | 1 |
| Surface
configuration |
|
|
Exophytic | 6 |
|
Ulcerative | 5 |
|
Indurated | 7 |
|
Leukoplakic/Erythroplakic | 7 |
| pT stage |
|
|
T1-T2 | 23 |
|
T3-T4 | 2 |
|
Differentiation |
|
|
Well | 20 |
|
Moderate | 4 |
|
Poor | 1 |
| Pathological
cervical lymph node metastases |
|
|
Negative | 22 |
|
Positive | 3 |
| Pattern of
invasion |
|
|
Low | 23 |
|
High | 2 |
| Surgical
margin |
|
|
Negative | 22 |
|
Positive | 3 |
| PORT |
|
| No | 22 |
|
Yes | 3 |
| Locoregional
recurrence |
|
|
Negative | 22 |
|
Positive | 3 |
| Prognosis |
|
|
NED | 22 |
|
AWD | 1 |
|
DOD | 1 |
|
DOC | 1 |
All patients underwent surgery, and one patient was
administered preoperative chemotherapy (two courses of cisplatin
and 5-fluorouracil). One patient developed local recurrence of
POSCC. This patient underwent salvage surgery and was alive without
disease at the last follow-up. Two of the three patients with
pathological cervical lymph node metastases had regional
recurrences. One of these patients was alive with disease at the
last follow-up, however, and the other one had died of uncontrolled
regional recurrence. Overall, 3 of the 25 patients had locoregional
recurrence during the follow-up period. There were no distant
metastases observed.
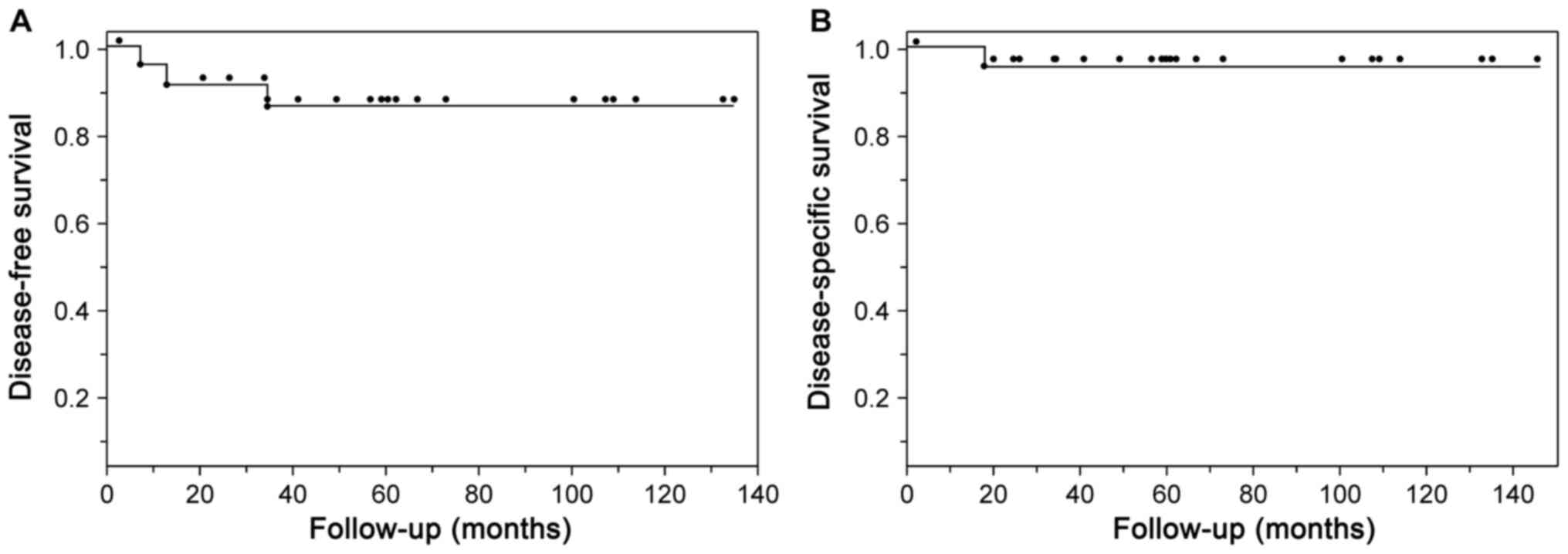
Fig. 1 shows the
Kaplan-Meier estimates of the 5-year disease-free survival (86.6%)
and disease-specific survival (95.8%) rates.
Characteristics of the pigmentations
of POSCC
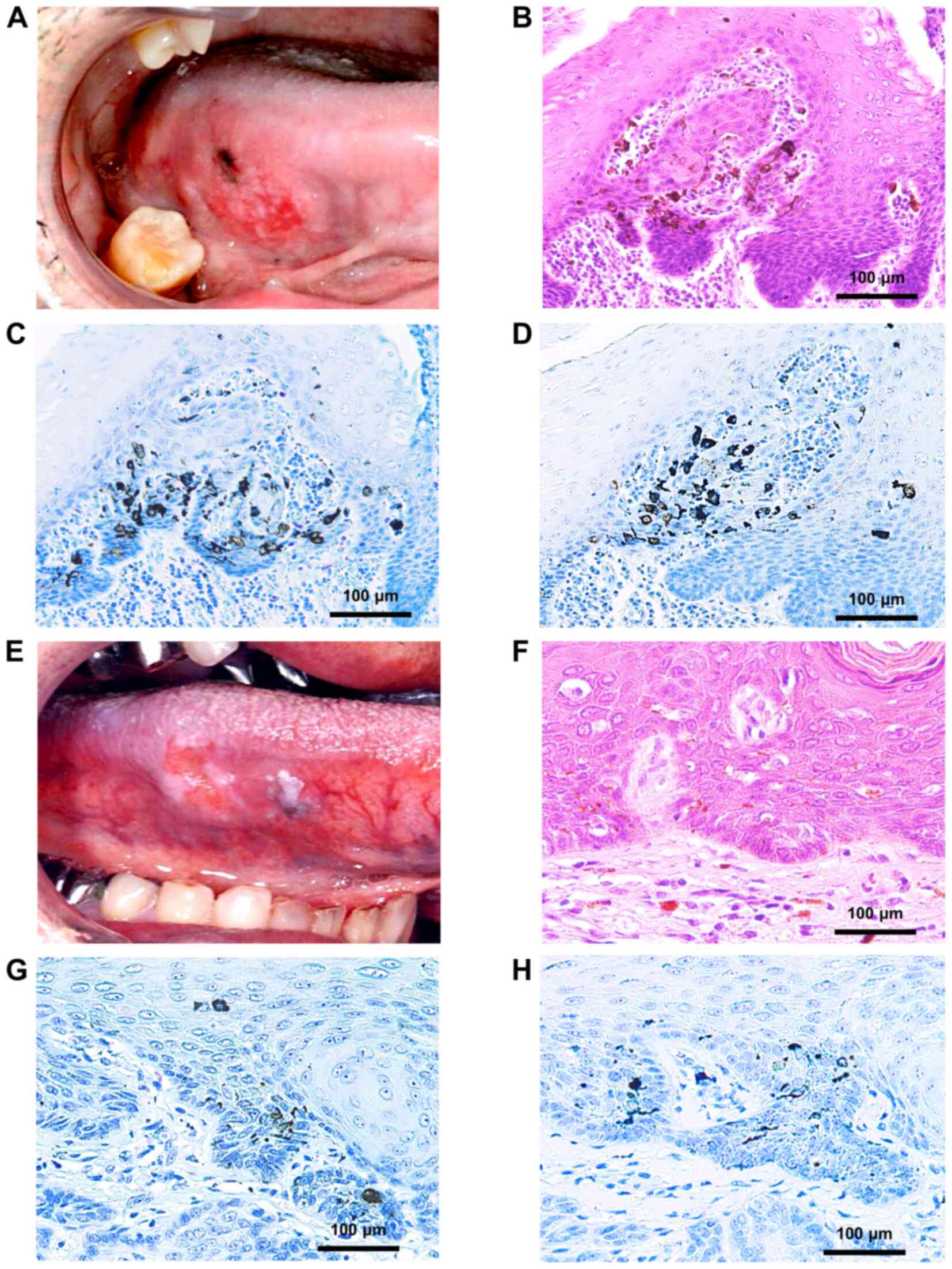
Pigmentation was observed macroscopically within the
tumor and surrounding the mucosal lesion. On histopathological
examination, 18 (72%) patients showed pigmentation within the OSCC,
while 7 (28%) patients showed pigmentation within the leukoplakia
associated with the tumor. The pigmentation showed wide-ranging
features, with asymmetrical and scattered distribution, uneven
color intensity, and ill-defined borders.
Microscopically, the histopathological features were
proliferation of atypical squamous cells, which was similar to that
in conventional SCC, with intermingled melanin without atypia.
Immunohistochemical staining of the tumor with HMB45 and Melan-A
showed strong positivity within the melanin pigments (Fig. 2). These melanin pigments were not
uniformly distributed and were dispersed in the cytoplasm of
neoplastic keratinocytes, the intercellular spaces from the surface
to the basal layer of the epithelium, or occasionally within the
superficial portion of the lamina propria. Morphologically, three
types of melanin were recognized: dendritic melanocytes, pigment
blockage melanocytes, and melanophages. Melanocyte colonies were
commonly formed by pigment blockade melanocytes, whereas dendritic
melanocytes were uniformly distributed without colonization.
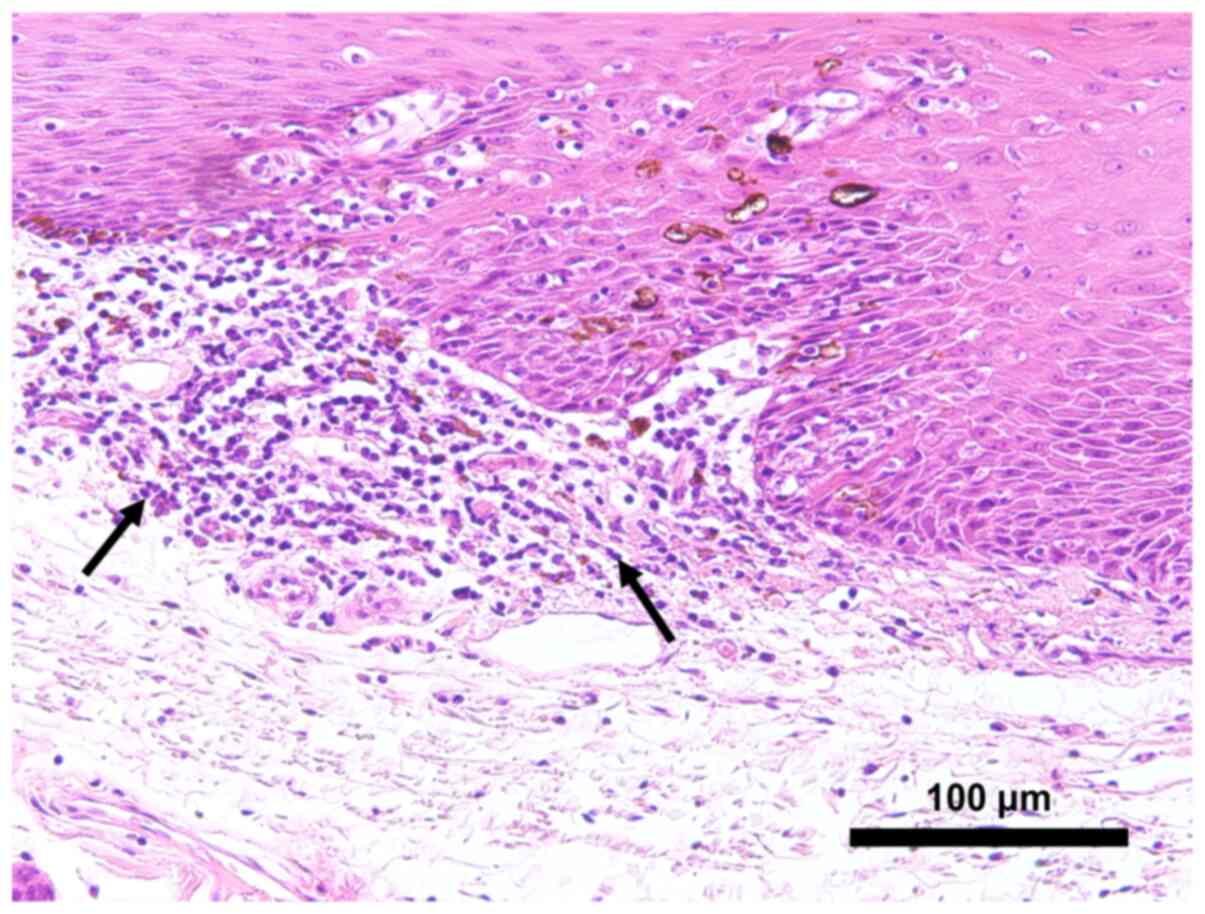
Notably, 7 (28%) tumors showed early invasion
patterns, with architectural disturbance of the stratified squamous
epithelium. Increased mitotic figures and drop-shaped rete ridges
with no invasive growth toward subepithelial tissues were also
noted in these tumors.
All patients had intense (n=21, 84%) or vague (n=4,
16%) inflammatory infiltration rich in lymphocytes and neutrophils
in the submucosa facing the pigmented area with localization of
melanocytes in POSCC. In contrast, in the nonpigmented area of
POSCC, there was intense inflammatory infiltration in 11 (44%),
vague inflammatory infiltration in 1 (4%), and minimal inflammatory
infiltration in 13 (48%) patients (Fig.
3).
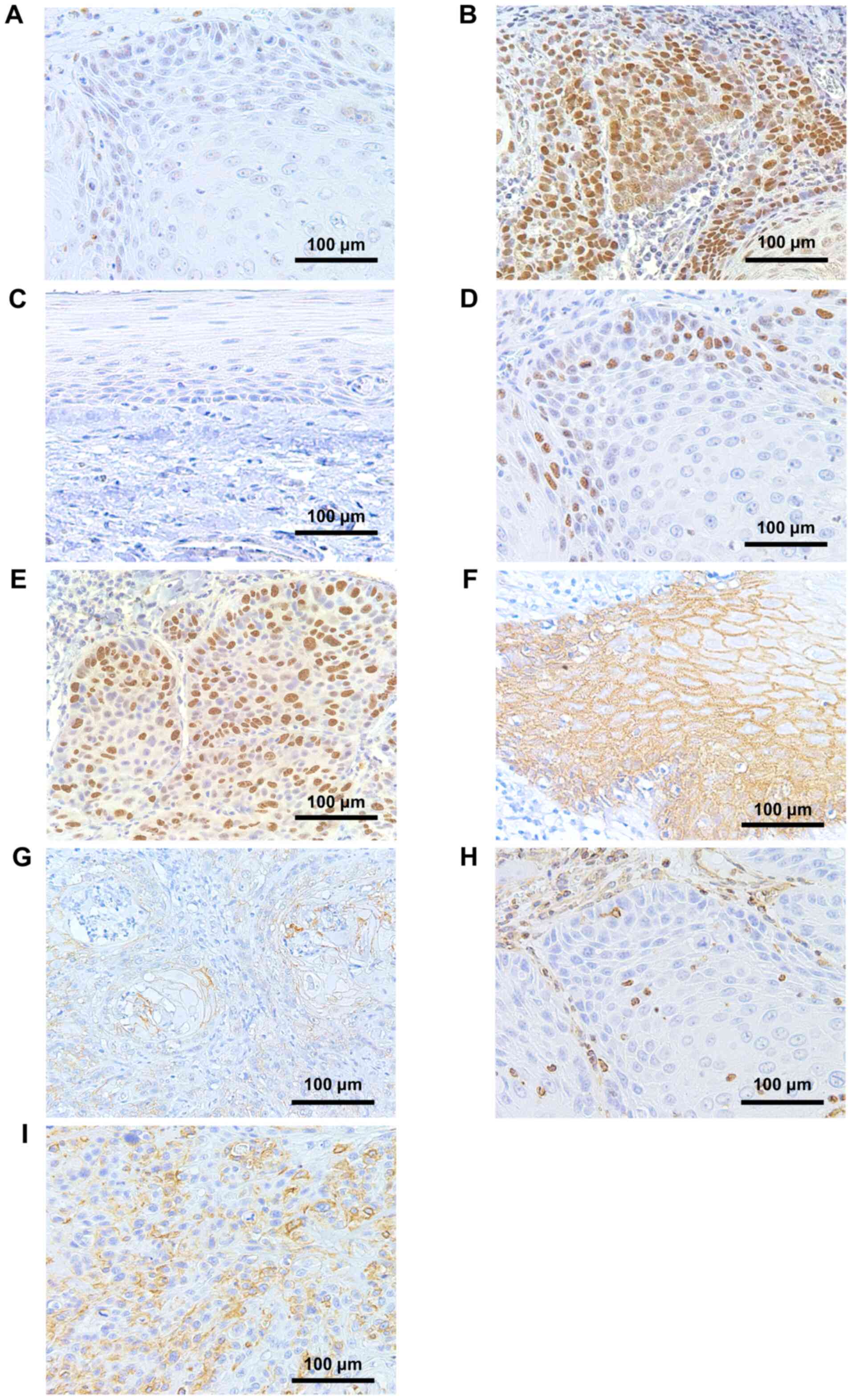
Immunohistochemical studies of p53,
Ki-67, and EMT-associated molecules
Table II and
Fig. 4 show the immunohistochemical
expression of p53, Ki-67, and EMT-associated molecules and their
representative staining. Overall, a high percentage of POSCC cases
exhibited low expression of p53 and Ki-67, preserved expression of
E-cadherin, and negative expression of vimentin. Specifically, p53
and Ki-67 were identified in 18 (72%) and 19 (76%) cases,
respectively, with a low expression index. There was no case with
no expression of p53 in tumor cells of POSCC. There was no
statistically significant association between p53 and Ki-67
staining (Fisher's exact test, two-tailed P-value>0.99)
(Table III). Furthermore, there
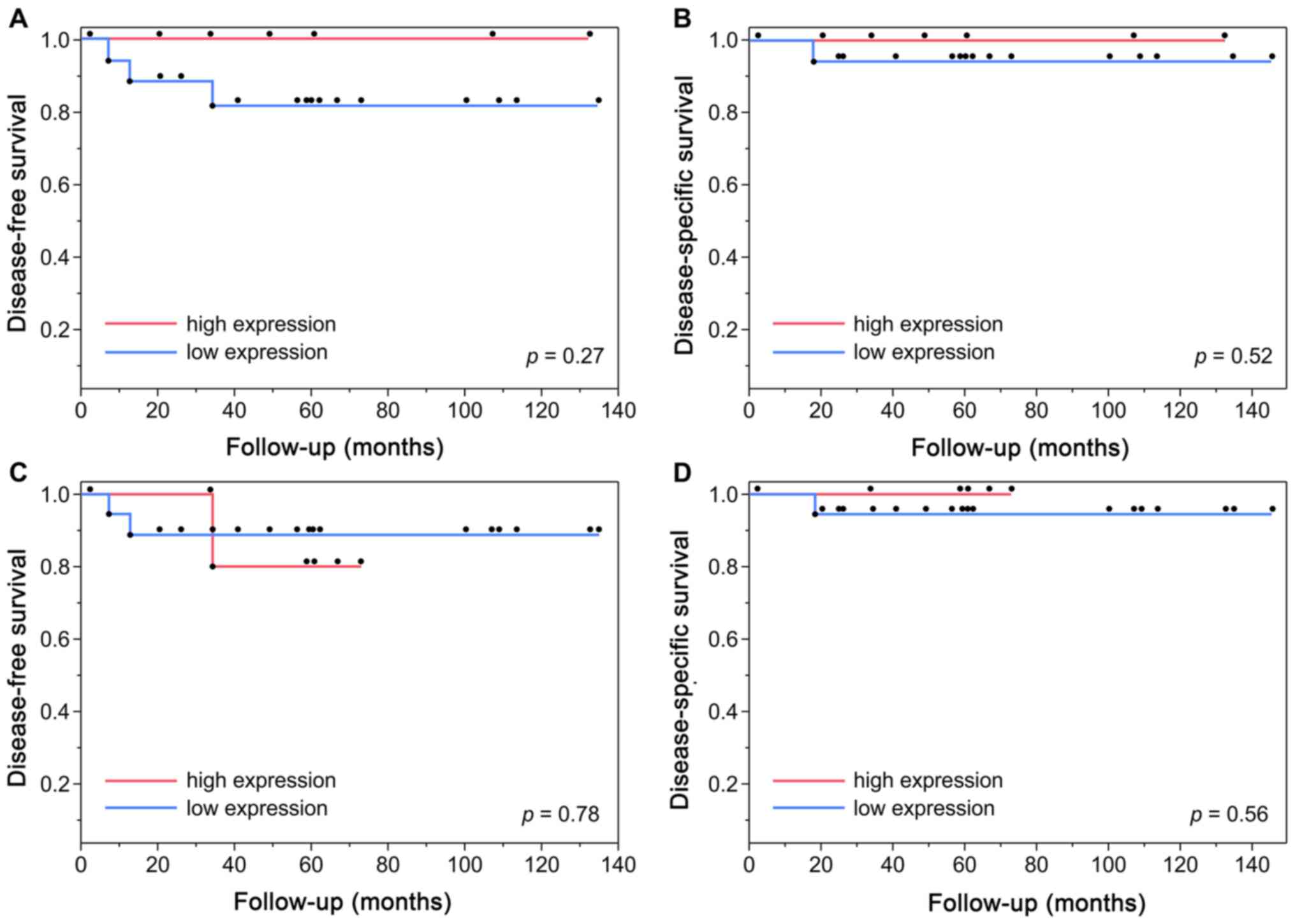
were no statistical differences in the DFS (log-rank test, P=0.27
or P=0.78) and DSS (log-rank test, P=0.52 or P=0.56) between low-
and high- p53 or Ki-67 expression groups, respectively (Fig. 5). Preserved E-cadherin expression was
detected in 24 (96%) tumors, and positive expression of vimentin
was observed in 1 (4%) tumor. EMT status was assessed based on the
expression of both proteins. Accordingly, 24 (96%) tumors exhibited
preserved E-cadherin and negative vimentin expressions, and 1 (4%)
showed reduced E-cadherin and positive vimentin expressions.
 | Table II.Immunohistochemical expression
(n=25). |
Table II.
Immunohistochemical expression
(n=25).
| Marker | N (%) |
|---|
| p53 |
|
|
Low | 18 (72) |
|
High | 7 (28) |
| Ki-67 |
|
|
Low | 19 (76) |
|
High | 6 (24) |
| E-cadherin |
|
|
Preserved | 24 (96) |
|
Reduced | 1 (4) |
| Vimentin |
|
|
Negative | 24 (96) |
|
Positive | 1 (4) |
 | Table III.p53 and Ki-67 expression. |
Table III.
p53 and Ki-67 expression.
|
| p53 expression |
|---|
|
|
|
|---|
| Ki-67
expression | Low | High |
|---|
|
Low | 14 | 5 |
|
High | 4 | 2 |
Discussion
POSCC is a rare variant of SCC that is
histologically similar to typical SCC but with the presence of
non-neoplastic melanocytes within the lesion (20,22).
Pigmentation in POSCC is not always macroscopically visible and may
be detected only microscopically (18,19). Our
study examined only the cases in which the pigmentation could be
macroscopically observed in the primary sites. There was no data in
the literature on the prevalence of POSCC. In this study, POSCC was
prevalent in 1.7% of the total OSCC cases. To the best of our
knowledge, this is the first study to evaluate the
clinicopathological and biological features of POSCC.
The most common location of POSCC in this study was
the tongue (72%), which is consistent with previous findings
(13–22) and in line with conventional OSCC.
Similar to 18 reported cases (13–22), 23
tumors (92%) were diagnosed as pathological T1-T2 stage. In total,
23 of 25 cases (92%) were low-invasive type POSCC. There were 3 of
25 patients (12%) who had pathological lymph node metastases,
compared with 1 in the previously 18 reported cases (5.6%)
(20). Cervical lymph node
metastases generally develop in 30% of conventional OSCC cases
(32). Although the number of cases
in our study were insufficient to draw any conclusions, these
results suggest that POSCC has an early tumor stage with a low
tendency of metastasis to the cervical lymph nodes. There was 1
POSCC case (4%) with local recurrence in our study, compared with
that of 1 among 18 previously reported cases (5.6%) (20). Further, we found a 5-year
disease-free and disease-specific survival rates of 86.6 and 95.8%,
respectively, in the POSCC patients. These results suggest that the
patients with POSCC exhibit good local control and good
prognosis.
Our study found that pigments were interspersed in
neoplastic cells from the epithelial surface to the basal layer.
Histological analysis revealed that 28% of cases, showing early
invasion patterns, shared some similarities with the
characteristics of pigmented carcinoma in situ (22). In previous studies, there have been
four cases of OSCC in situ with the symbiosis of melanocytes
(13,15,21,22), two
of which showed white discoloration on the lesion (15,21). Our
study found pigmentation in leukoplakia associated with the tumor
in 7 cases (28%). Leukoplakia is one of the most common potentially
malignant disorders of the oral cavity (33). Matsumoto et al (21) stated that the presence of a pigment
in a white mucosal lesion might be a sign of a pigmented
pre-cancerous lesion or pigmented SCC. The appearance of
pigmentation may not be an incidental physiological finding but is
probably reactive and stimulated by local microenvironmental
triggers from SCC tumors. It has been reported that the enhanced
expression of various growth factors and cytokines in carcinoma
cells may result in melanocyte proliferation and melanin production
(22,34). However, these mechanisms were not
evaluated in this study.
To gain more insight into the biological
characteristics of these tumors, we performed immunohistochemical
studies with p53, Ki-67, E-cadherin, and vimentin. The analyzed
region was the invasive tumor front, which is the area of greatest
tumor progression where the deepest and most aggressive cells
reside (35). The inactivation and
mutation of p53, which play an essential role in tumorigenesis and
progression of head and neck carcinoma, are among the most frequent
genetic alterations in oral squamous cell carcinoma (36). In oral malignancy, epithelial
dysplastic lesion, and leukoplakia, p53 overexpression was
identified via immunohistochemical studies (37–40).
Similar to this finding, in all patients (n=25), the proportion and
staining intensity of positive p53 expression in the tumor was
higher than that in the healthy epithelium. Current evidence
regarding the prognostic value of p53 and Ki-67 in patients with
head and neck SCC is still controversial and inconclusive because
of the heterogeneous and conflicting results (25,41).
Some studies found that p53 overexpression by more than 50%
indicated a poor prognosis in advanced tumors, whereas a weak or
negative expression indicated a good prognosis and longer survival
(24). Some studies showed a
significant relationship between Ki-67 expression and overall
survival, whereby, high Ki-67 expression was a marker of poor
prognosis in OSCC patients (25).
Motta et al (42) reported
that co-expression of p53 and Ki-67 markers in SCCs of the oral
cavity and tongue suggested a worse prognosis. Despite the lack of
significant differences between p53 and Ki-67 expression and
clinicopathological parameters (data not shown), our study revealed
that most POSCCs exhibited low expression of p53 and Ki-67. We
found low expression of E-cadherin and positive expression of
vimentin in only one tumor. Low expression of E-cadherin in OSCC
has been previously reported to be associated with lower
disease-free rates, higher rates of lymph node metastases, lower
survival rates, and a more invasive histological pattern (29). Meanwhile, positive vimentin
expression has been associated with a higher prevalence of
recurrence and shorter survival time in OSCC and has been
considered a reliable predictive EMT marker for poor prognosis in
OSCC (43). Collectively, our
immunohistochemical results suggest low malignancy of POSCC.
However, most of our understanding of oral
melanocytes is derived from insights into the regulation and
biology of epidermal melanocytes, which act not only to absorb
ultraviolet radiation, but also as antioxidant and radical
scavenging agents (44). Increasing
evidence has shown that melanocytes are also active factors in the
skin immune system and have immunomodulatory properties (45). In the oral cavity, melanocytes
produced by the gingival epithelium can neutralize reactive oxygen
species generated by dentogingival plaque-induced inflammation in
the periodontal microenvironment (46). Moreover, treatment with antioxidants
has the potential to prevent, inhibit, and reverse the multiple
steps involved in oral carcinogenesis (47). Therefore, increased production of
melanin with its antioxidant properties may be involved in the
protective immune response and may inhibit the process of
carcinogenesis in POSCC. In our study, intense inflammatory
infiltration was observed near the pigmented area with localization
of melanocytes in 21 (84%) and at the nonpigmented area in 11 (44%)
patients. Hence, the localization of melanocytes is associated with
inflammatory infiltration in POSCC. However, a firm conclusion
about the association between melanocyte loading and immune
response and their immunological significance in POSCC cannot be
obtained due to the limited number of cases and evaluations. Thus,
elucidation of the precise mechanism of this effect requires
further studies with more specific molecular investigations.
This study has some limitations that might have
influenced the results. Information regarding lifestyle habits was
limited owing to the retrospective study design. In addition, we
could not undermine the potential effects of previous mucosal
diseases with post-inflammatory pigmentation. Our results need to
be interpreted with caution from a non-comparative study. Future
prospective investigations with a large cohort of patients and
involving more specific molecular mechanisms are warranted to
further extend our understanding of POSCC.
In conclusion, the clinical findings and
immunohistochemical analyses presented here indicated that POSCC
has a tendency towards nonaggressive oncological behavior and a
good prognosis. These findings enhance our current understanding of
the clinicopathological and biological characteristics of POSCC and
further elucidate the oncological behavior of this rare
pathological variant of OSCC.
Acknowledgements
The authors would like to thank Ms. Kiyoko Nagumo
(Clinical Laboratory, Tokyo Medical and Dental University, Dental
Hospital) for her technical support.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HH and YM conceived the current study. TK and KK
conceived and designed the experiments. HH and TK confirmed the
authenticity of all the raw data. YO analyzed statistical data. TK
interpreted the data and revised the manuscript. CMT was involved
in all the stages of the study, performed the immunohistochemical
staining and was a major contributor in writing the manuscript. All
authors read and approved the final version of the manuscript.
Ethics approval and consent to
participate
The study complied with the standards of the
Declaration of Helsinki and was approved by the Institutional
Review Board of Tokyo Medical and Dental University (approval no.
D2020-600). The need for informed consent was waived owing to the
retrospective nature of the study.
Patient consent for publication
Written informed consent for the publication of the
oral photographs in Fig. 2 was
obtained from the patients.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
SCC
|
squamous cell carcinoma
|
|
OSCC
|
oral squamous cell carcinoma
|
|
POSCC
|
pigmented oral squamous cell
carcinoma
|
|
EMT
|
epithelial-mesenchymal transition
|
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2020. CA Cancer J Clin. 70:7–30. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pulte D and Brenner H: Changes in survival
in head and neck cancers in the late 20th and early 21st century: A
period analysis. Oncologist. 15:994–1001. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sim YC, Hwang JH and Ahn KM: Overall and
disease-specific survival outcomes following primary surgery for
oral squamous cell carcinoma: Analysis of consecutive 67 patients.
J Korean Assoc Oral Maxillofac Surg. 45:83–90. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Iihara K, Yamaguchi K, Fujioka Y and Uno
S: Pigmented neuroendocrine tumor of the lung, showing
neuromelanin. Pathol Int. 52:734–739. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhang X, Liang Y and Wang HY: Invasive
ductal carcinoma of the breast associated with extensive melanin
melanosis: A case report and review of the literature. Int J Clin
Exp Pathol. 7:1218–1223. 2014.PubMed/NCBI
|
|
6
|
Takeda Y and Kurose A: Pigmented
mucoepidermoid carcinoma, a case report and review of the
literature on melanin-pigmented salivary gland tumors. J Oral Sci.
48:253–256. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Satter EK: Pigmented squamous cell
carcinoma. Am J Dermatopathol. 29:486–489. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Masuzawa N, Kishimoto M and Takahashi Y:
Pigmented squamous cell carcinoma of the uterine cervix. Int J
Gynecol Pathol. 22:285–288. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shields JA, Shields CL, Eagle RC Jr, Singh
AD, Demirci H and Wolf MA: Pigmented conjunctival squamous cell
carcinoma simulating a conjunctival melanoma. Am J Ophthalmol.
132:104–106. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mathews A, Abraham EK, Amman S and Nair
MK: Pigmented squamous cell carcinoma of nasal cavity.
Histopathology. 33:184–185. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Matsumoto M, Sonobe H, Takeuchi T,
Furihata M, Iwata J, Ikeda M and Ohtsuki Y: Pigmented squamous cell
carcinoma of the scrotum associated with a lentigo. Br J Dermatol.
141:132–136. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kamiya M, Maehara R, Iizuka S, Yoshida T,
Yamanouchi H, Yokoo H, Sasaki A, Hirato J and Nakazato Y: Pigmented
squamous cell carcinoma with dendritic melanocyte colonization in
the external auditory canal. Pathol Int. 49:909–912. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Patakas B, Hecker R and Kramer HS: Report
on an oral, pigmented, squamous cell carcinoma. Int J Oral Surg.
3:445–448. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ide F, Kusuhara S, Ohnuma H, Miyake T,
Nakajima T and Kimura T: Pigmented squamous cell carcinoma of the
oral mucosa - with special reference to the role of
non-keratinocytes in tumors and tumorous conditions. J Nihon Univ
Sch Dent. 23:1–9. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Dunlap CL and Tomich CE: Melanocyte
colonization of oral squamous cell carcinoma. Oral Surg Oral Med
Oral Pathol. 52:524–530. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Modica LA, Youngberg GA and Avila FO:
Melanocyte colonization of an oral carcinoma. Histopathology.
17:477–478. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kuwabara H, Uda H, Miyaguchi M, Nagai M,
Saito K and Shibanushi T: Pigmented squamous cell carcinoma of the
alveolar ridge in the oral mucosa. Oral Surg Oral Med Oral Pathol.
77:61–65. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Satomura K, Tokuyama R, Yamasaki Y, Yuasa
T, Tatehara S, Ishimaru N, Hayashi Y and Nagayama M: Possible
involvement of stem cell factor and endothelin-1 in the emergence
of pigmented squamous cell carcinoma in oral mucosa. J Oral Pathol
Med. 36:621–624. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lisboa Castro J, Cazal C, Gomes Henriques
AC, Carneiro Leão J, de Vasconcelos Carvalho M, de Carvalho Dourado
HT and Carvalho AA: Pigmented oral squamous cell carcinoma: A case
report and brief review of the literature. Int J Surg Pathol.
17:153–157. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mikami T, Furuya I, Kumagai A, Furuuchi H,
Hoshi H, Iijima S, Sugiyama Y and Takeda Y: Pigmented squamous cell
carcinoma of oral mucosa: Clinicopathologic study of 3 cases. J
Oral Maxillofac Surg. 70:1232–1239. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Matsumoto N, Kitano T, Oki H, Omagari D,
Matsue Y, Okudera M, Yamamura T, Nishikawa Y, Nishimura S, Asano M,
et al: Pigmented oral carcinoma in situ: A case report and
literature review. Oral Surg Oral Med Oral Pathol Oral Radiol.
118:e79–e83. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Martins F, Mistro FZ, Kignel S, Palmieri
M, do Canto AM and Braz-Silva PH: Pigmented squamous cell carcinoma
in situ: Report of a new case and review of the literature. J Clin
Exp Dent. 9:e1362–e1365. 2017.PubMed/NCBI
|
|
23
|
Zhou G, Liu Z and Myers JN: TP53 Mutations
in head and neck squamous cell carcinoma and their impact on
disease progression and treatment response. J Cell Biochem.
117:2682–2692. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cutilli T, Leocata P, Dolo V and Altobelli
E: p53 as a prognostic marker associated with the risk of mortality
for oral squamous cell carcinoma. Oncol Lett. 12:1046–1050. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Xie S, Liu Y, Qiao X, Hua RX, Wang K, Shan
XF and Cai ZG: What is the prognostic significance of Ki-67
positivity in oral squamous cell carcinoma? J Cancer. 7:758–767.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wan Y, Liu H, Zhang M, Huang Z, Zhou H,
Zhu Y, Tao Y, Xie N, Liu X, Hou J, et al: Prognostic value of
epithelial-mesenchymal transition-inducing transcription factors in
head and neck squamous cell carcinoma: A meta-analysis. Head Neck.
42:1067–1076. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sobin LH, Gospodarowicz MK and Wittekind
C: TNM Classification of Malignant Tumours. John Wiley & Sons
Ltd; West Sussex: pp. 3322010
|
|
28
|
Anneroth G, Batsakis J and Luna M: Review
of the literature and a recommended system of malignancy grading in
oral squamous cell carcinomas. Scand J Dent Res. 95:229–249.
1987.PubMed/NCBI
|
|
29
|
Costa LC, Leite CF, Cardoso SV, Loyola AM,
Faria PR, Souza PE and Horta MC: Expression of
epithelial-mesenchymal transition markers at the invasive front of
oral squamous cell carcinoma. J Appl Oral Sci. 23:169–178. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Shen H and Wu W: Study of melanin
bleaching after immunohistochemistry of melanin-containing tissues.
Appl Immunohistochem Mol Morphol. 23:303–307. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yu CH, Chen HH, Liu CM, Jeng YM, Wang JT,
Wang YP, Liu BY, Sun A and Chiang CP: HMB-45 may be a more
sensitive maker than S-100 or Melan-A for immunohistochemical
diagnosis of primary oral and nasal mucosal melanomas. J Oral
Pathol Med. 34:540–545. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
De Silva RK, Siriwardena BSMS,
Samaranayaka A, Abeyasinghe WAMUL and Tilakaratne WM: A model to
predict nodal metastasis in patients with oral squamous cell
carcinoma. PLoS One. 13:e02017552018. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Abidullah M, Kiran G, Gaddikeri K, Raghoji
S and Ravishankar TS: Leuloplakia - review of a potentially
malignant disorder. J Clin Diagn Res. 8:ZE01–ZE04. 2014.PubMed/NCBI
|
|
34
|
Hirobe T: Role of keratinocyte-derived
factors involved in regulating the proliferation and
differentiation of mammalian epidermal melanocytes. Pigment Cell
Res. 18:2–12. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Sharma M, Sah P, Sharma SS and
Radhakrishnan R: Molecular changes in invasive front of oral
cancer. J Oral Maxillofac Pathol. 17:240–247. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Li Y, Li B, Xu B, Han B, Xia H, Chen QM
and Li LJ: Expression of p53, p21(CIP1/WAF1) and eIF4E in the
adjacent tissues of oral squamous cell carcinoma: Establishing the
molecular boundary and a cancer progression model. Int J Oral Sci.
7:161–168. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Varun BR, Ranganathan K, Rao UK and Joshua
E: Immunohistochemical detection of p53 and p63 in oral squamous
cell carcinoma, oral leukoplakia, and oral submucous fibrosis. J
Investig Clin Dent. 5:214–219. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Swaminathan U, Joshua E, Rao UK and
Ranganathan K: Expression of p53 and Cyclin D1 in oral squamous
cell carcinoma and normal mucosa: An Immunohistochemical study. J
Oral Maxillofac Pathol. 16:172–177. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Lavieille JP, Brambilla E, Riva-Lavieille
C, Reyt E, Charachon R and Brambilla C: Immunohistochemical
detection of p53 protein in preneoplastic lesions and squamous cell
carcinoma of the head and neck. Acta Otolaryngol. 115:334–339.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Nadal A, Campo E, Pinto J, Mallofré C,
Palacín A, Arias C, Traserra J and Cardesa A: p53 expression in
normal, dysplastic, and neoplastic laryngeal epithelium. Absence of
a correlation with prognostic factors. J Pathol. 175:181–188. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Tandon S, Tudur-Smith C, Riley RD, Boyd MT
and Jones TM: A systematic review of p53 as a prognostic factor of
survival in squamous cell carcinoma of the four main anatomical
subsites of the head and neck. Cancer Epidemiol Biomarkers Prev.
19:574–587. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Motta RR, Zettler CG, Cambruzzi E, Jotz GP
and Berni RB: Ki-67 and p53 correlation prognostic value in
squamous cell carcinomas of the oral cavity and tongue. Rev Bras
Otorrinolaringol (Engl Ed). 75:544–549. 2009.
|
|
43
|
Liu S, Liu L, Ye W, Ye D, Wang T, Guo W,
Liao Y, Xu D, Song H, Zhang L, et al: High vimentin expression
associated with lymph node metastasis and predicated a poor
prognosis in oral squamous cell carcinoma. Sci Rep. 6:388342016.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Feller L, Masilana A, Khammissa RA, Altini
M, Jadwat Y and Lemmer J: Melanin: The biophysiology of oral
melanocytes and physiological oral pigmentation. Head Face Med.
10:82014. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Plonka PM, Passeron T, Brenner M, Tobin
DJ, Shibahara S, Thomas A, Slominski A, Kadekaro AL, Hershkovitz D,
Peters E, et al: What are melanocytes really doing all day long…?
Exp Dermatol. 18:799–819. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Nilima S and Vandana KL: Melanin: A
scavenger in gingival inflammation. Indian J Dent Res. 22:38–43.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Choudhari SK, Chaudhary M, Gadbail AR,
Sharma A and Tekade S: Oxidative and antioxidative mechanisms in
oral cancer and precancer: A review. Oral Oncol. 50:10–18. 2014.
View Article : Google Scholar : PubMed/NCBI
|