Introduction
Salivary gland carcinomas are rare tumors that
account for about 3 to 6% of head and neck cancers. The WHO
classified salivary gland tumors into over 20 different tissue
types in 2017 (1). Mucoepidermoid
carcinoma (MEC) is the most common malignant salivary tumor and
constitutes approximately 30% of all malignant tumors of the
salivary gland (2). Surgery is the
only definitive treatment for all salivary gland tumors, including
MEC. The types and scopes of surgery vary greatly depending on the
stage and grade of the tumor (3,4).
Preoperative diagnosis helps to guide operative strategy and
clinical management (5,6). A previous study reported that
high-grade MEC may have lymph node metastasis, and when high-grade
MEC is diagnosed before surgery, neck dissection is also considered
(7).
In addition to genetic changes, epigenetic changes
also play an important role in neoplastic transformation (8). The glycosylation of proteins also
changes with epigenetic alterations. Glycan alterations are common
features of tumor cells (9,10) and have been aggressively studied as
cancer biomarkers and functional molecules involved in malignant
behaviors, including metastasis and cancer cell proliferation.
Mucins are hyperglycosylated proteins in which the glycans attach
to Ser/Thr residues in the variable number of tandem repeat (VNTR)
region of the mucins. A serum tumor marker, CA19-9, is a glycan
antigen found on MUC1, and is involved in the promotion of
metastasis and the dissemination of cancer cells (11). MUC1, modified with certain glycans
(tumor-associated MUC1) such as sialyl Lewis a, sialyl Lewis X, and
sialyl Tn, is known as a marker of various tumors (12–15).
Tumor-associated MUC1 is widely distributed in both primary and
metastatic tumors, including cancer stem cells, and has been widely
considered a target for many diagnostic and immunological
therapeutic approaches. Based on certain criteria, such as
therapeutic function, immunogenicity, and cancer cell specificity,
MUC1 was listed by the National Cancer Institute pilot project to
prioritize cancer antigens as the second most promising target in
cancer research from a list of 75 tumor-associated antigens
(16). MUC1 expression has also been
reported to be associated with the histological grade of MEC
(17,18). In this study, mucins and their
glycans expressed in MEC were analyzed and compared with normal
salivary glands (NSGs). Mucins are extensively glycosylated
proteins with high molecular weights of over 1,000 kDa and are
difficult to analyzed using conventional proteomic techniques. In
the present study, mucins were analyzed using supported molecular
matrix electrophoresis (SMME), a membrane electrophoresis method,
that was previously developed to characterize mucins (19). The mucins were stained on the SMME
membranes using specific antibodies (20). Furthermore, we analyzed the glycans
attached to the mucins by mass spectrometry (MS) and revealed that
MEC specifically produced MUC1 with core 2 type glycans modified
with sialic acid.
Materials and methods
Case selection
All cases were diagnosed and classified by
experienced oral pathologists. The pathological classification was
described based on TNM Classification of Malignant Tumors (8th
edition) by the Union for International Cancer Control (UICC)
(21). Salivary glands were
surgically removed from patients with a diagnosis of MEC and other
salivary gland tumors. Surplus tissues that did not contain
malignant cells were used as samples of NSGs. In this study, MEC
samples and NSG samples were obtained from different patients,
respectively. The tissues were cut to a predetermined size (2×2 mm)
and then immediately stored in a freezer at −80°C until further
use. This research was approved by the Tokyo Dental College
Ichikawa General Hospital Ethics Review Committee (I16-74) and the
AIST Committee on Bioethics of Experiments Involving Human-derived
Materials (h-213). Written informed consent was obtained for
experimentation with human subjects.
Chemicals and materials
A polyvinylidene difluoride (PVDF) membrane
(Immobilon-P; pore size, 0.45 µm) was purchased from EMD Millipore.
Poly (vinyl alcohol) (PVA; MW, 22,000) was purchased from Wako Pure
Chemical Industries. Poly (ethylene glycol) (PEG; MW: 20,000) and
polyvinylpyrrolidone (PVP; MW: 20,000) were purchased from Nacalai
Tesque Inc. Porcine gastric mucin (PGM) (type III, partially
purified) and Alcian blue 8GX were purchased from Sigma-Aldrich;
Merck KGaA. Anti-sialyl MUC1 monoclonal antibody (MY.1E12) was
provided by Dr T. Irimura (Juntendo University, Japan) (22,23).
Hyaluronic acid binding protein (HABP) was obtained from Cosmo Bio
Co., Ltd. Other reagents and solvents were obtained from Wako Pure
Chemical Industries Ltd. and Nacalai Tesque Inc. All solvents used
were of analytical reagent grade.
Extraction of mucins
Mucin extraction was performed as reported in
previous studies (19,20). Briefly, pieces of MEC and NSG tissue
were homogenized in cold acetone. The homogenized mixtures were
centrifuged at 16,000 × g at 4°C for 10 min. After discarding the
supernatants, the resulting powders were homogenized in PBS (pH
7.4, 805 µl) containing 5 µl of protease inhibitor mix (GE
Healthcare Bio-Sciences). A saturated calcium acetate solution was
added to the supernatants at a ratio of 1:4, followed by the
addition of three volumes of ethanol. The mixtures were cooled at
−80°C, left to stand for 1 h, and centrifuged. The precipitates
were dissolved in 2 M urea in PBS (pH 7.4, 100 µl) and centrifuged
at 16,000 × g at 4°C for 10 min. The supernatants were transferred
into new tubes and precipitated with ethanol, as described above.
After centrifugation at 16,000 × g at 4°C for 10 min, the resulting
precipitates were dissolved in 8 M urea in PBS (pH 7.4, 20 µl). The
solutions were stored at 4°C until further use.
SMME
SMME membranes were prepared by immersion in a
hydrophilic polymer mixture of PVA:PVP=1:3 as previously described
(24). The SMME membranes
(separation length, 6 cm) were wetted in methanol and then
transferred into a running buffer (0.1 M pyridine-formic acid
buffer, pH 4.0). After equilibration for 30 min with gentle
shaking, the membranes were subjected to electrophoresis. The
solutions containing mucins extracted from clinical samples were
spotted at 1.5 cm from the edge of the membrane at the negative
node. Electrophoresis was performed using a membrane
electrophoresis chamber (EPC105AA; Advantec) in constant-current
mode at 1.0 mA/cm for 30 min. The membranes were then stained with
Alcian blue as previously described (19,20).
Immunostaining
Mucin immunostaining on the SMME membrane was
performed as previously reported (24,25).
Briefly, the electrophoresed membranes were immersed in acetone for
30 min, followed by heating at 150°C for 5 min (25,26). The
membranes were then rewetted by immersing in 5% BSA in PBS
containing 0.05% Tween-20 (PBS-T) for 1 h. Following washing with
PBS-T (5 min, 3 times), the membranes were incubated with PBS-T
containing a primary antibody (dilution of 1/1,000) at 4°C
overnight. After washing with PBS-T (5 min, 3 times), the membranes
were incubated with PBS-T containing secondary antibody labeled
with HRP (dilution of 1/2,000) for 1 h at room temperature. Binding
was visualized with ECL reagents (Western Lightning Plus-ECL;
PerkinElmer). Chemiluminescence images were obtained using ChemiDoc
XRS (Bio-Rad Laboratories, Inc.).
Release and permethylation of
O-glycans
O-glycans were released from mucins on the
SMME membranes by reductive β-elimination, followed by analysis
using mass spectrometry, as per previous studies (19,20).
Briefly, the stained mucin spots were excised from the SMME
membrane, transferred to a 500 µl microcentrifuge tube, and
incubated with 40 µl of 500 mM NaBH4 in 50 mM NaOH at
45°C for 16 h. The reaction mixtures were quenched by adding 4 µl
of glacial acetic acid until the hydrogen gas ceased. The mixtures
were desalted using a cation-exchange-solid-phase extraction
cartridge (3 ml) (Oasis MCX; Waters Corp.) and concentrated. The
obtained residues were dissolved in 100 µl of 1% (v/v) acetic acid
in methanol and dried again using a centrifugal evaporator. The
dissolving and drying procedures were repeated.
A slurry of 50 µl (80 mg/ml) of NaOH in dimethyl
sulfoxide (DMSO) containing 1% (v/v) distilled water was added to
the dried samples, followed by 12.5 µl of methyl iodide. The
mixtures were then vigorously shaken for 30 min until the sodium
iodide precipitated. After adding 50 µl of 10% acetic acid, the
mixtures were diluted to 1 ml with distilled water. The diluted
solutions were subjected to a solid-phase extraction cartridge (50
mg) (Sep-Pak C18; Waters Corp.), washed with 1 ml of water three
times, and then dried. Finally, permethylated glycans were eluted
with 1 ml of 50% acetonitrile and concentrated using a centrifugal
evaporator.
MS
The MS spectra of the permethylated glycans were
acquired in reflectron positive ion mode using a matrix-assisted
laser desorption ionization (MALDI)-time-of-flight (TOF) mass
spectrometer (UltraFlex; Bruker-Daltonics) equipped with a 337 nm
pulsed nitrogen gas laser. 2,5-Dihydroxybenzoic acid (2,5-DHB) was
used as the matrix. For sample preparation, 0.5 µl of 2,5-DHB
solution (10 mg/ml in 30% ethanol) was deposited onto a MALDI
target plate and dried. Then 0.5 µl of the sample solution was
deposited over the dried spot of 2,5-DHB and dried. Tandem mass
spectrometry was performed using a MALDI-quadrupole ion trap
(QIT)-TOF mass spectrometer (AXIMA-QIT; Shimadzu Corp.) in a
positive ion mode. Argon gas was used as the collision gas for
collision-induced dissociation.
Statistical analysis
The relative intensities of the glycan signals in
the MS spectra were calculated as a percentage of the intensity in
the sum of the intensities of all observed 50 glycans. Unpaired
Student's t-tests for each glycan between MEC and NSGs were
performed using GraphPad Prism 8.4.2 (GraphPad Software). The MS/MS
spectra of the permethylated glycans were assigned using
GlycoWorkBench 2.1 (http://www.eurocarbdb.org/).
Glycan cartoon
The glycan structures were depicted using CFG
graphical notation for glycans (http://www.functionalglycomics.org/static/consortium/CFGnomenclature.pdf).
Results
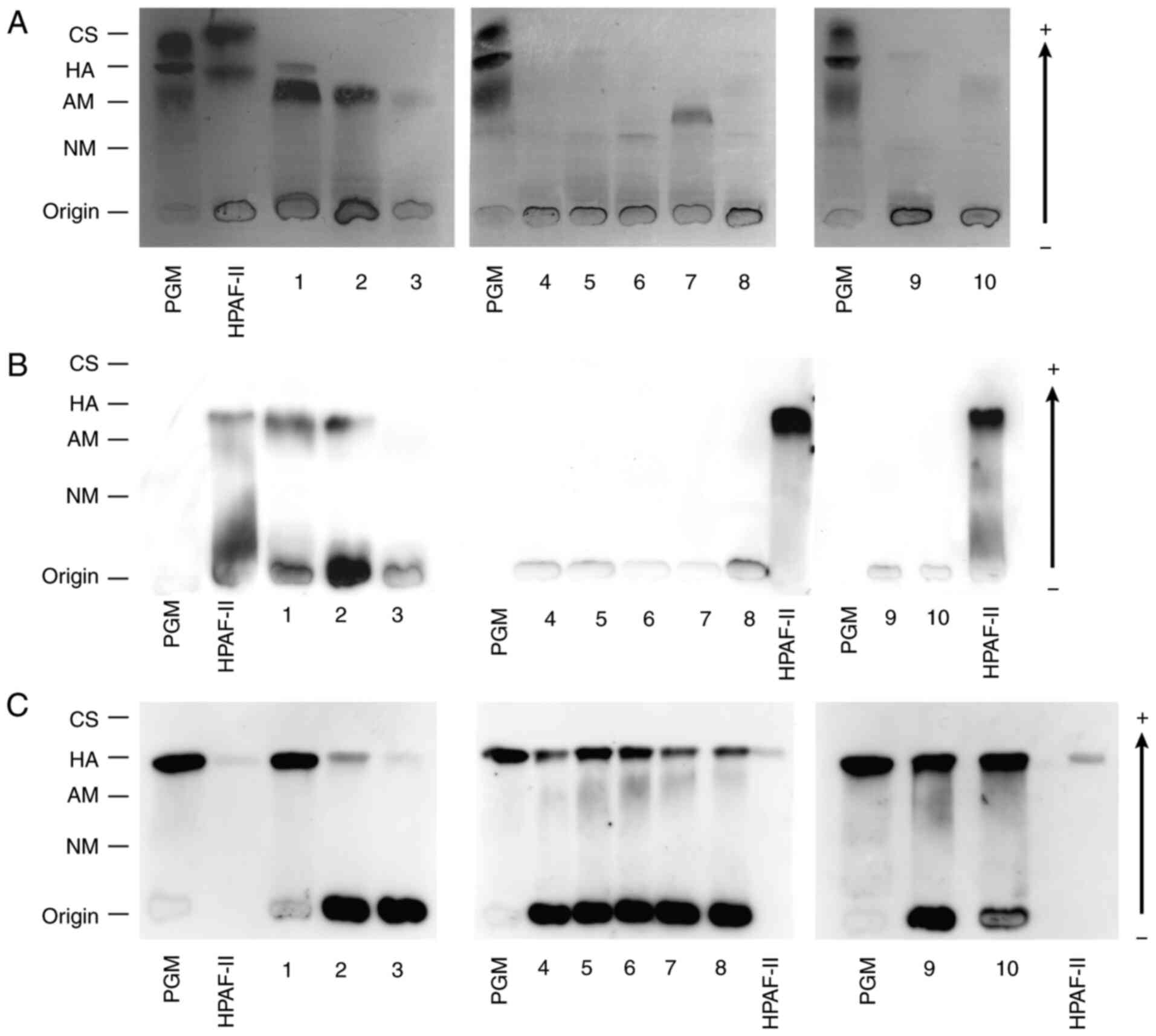
SMME analyses of MEC and NSGs
The clinical information of the salivary glands of
MEC and NSGs used in this study are summarized in Table I. The mucins extracted from the
salivary glands were separated by SMME and stained with Alcian blue
(Fig. 1A). A commercially obtained
PGM containing chondroitin sulfate, hyaluronic acid, acidic mucin,
and neutral mucin was used as the reference material in SMME. We
estimated the stained bands by comparing the migrating positions
with those of the corresponding constituents in the reference PGM.
Additionally, the mucin-enrichment fraction of cultured cells
(HPAF-II) was also used as a reference material containing MUC1
(25). All MEC samples 1–3 and NSGs
of the minor salivary gland 10 clearly showed bands at the
migrating position of the acidic mucin in the reference PGM.
Another dark band was observed at the position of neutral mucin
only from the NSG sample 7. Other samples showed a pale band at a
lower position of the neutral mucin and/or the same position of
hyaluronic acid in the reference PGM.
 | Table I.Summary of salivary glands used in
the present study. |
Table I.
Summary of salivary glands used in
the present study.
| Sample number | Age, years | Sex | Location | Tissue type | Histological grade
(TNM classification) |
|---|
| 1 | 38 | F | Minor salivary
gland | Mucoepidermoid
carcinoma | Low grade
(T1N0M0) |
| 2 | 39 | F | Minor salivary
gland | Mucoepidermoid
carcinoma | Low grade
(T1N0M0) |
| 3 | 52 | M | Minor salivary
gland | Mucoepidermoid
carcinoma | Low grade
(T2N0M0) |
| 4 | 90 | F | Submandibular
gland | Normal | Not
applicablea |
| 5 | 68 | F | Submandibular
gland | Normal | Not
applicablea |
| 6 | 57 | F | Submandibular
gland | Normal | Not
applicablea |
| 7 | 41 | M | Submandibular
gland | Normal | Not
applicablea |
| 8 | 55 | M | Submandibular
gland | Normal | Not
applicablea |
| 9 | 51 | M | Sublingual
gland | Normal | Not
applicablea |
| 10 | 87 | M | Minor salivary
gland | Normal | Not
applicablea |
We also stained the SMME membranes with specific
probes, such as a monoclonal antibody. Anti-MUC1 antibody (MY.1E12)
revealed that all three MEC samples contained MUC1 but not NSGs,
and the migrating positions of these MUC1 bands were just below
that of MUC1 in HPAF-II (Fig. 1B).
On the other hand, the mucins of the minor salivary gland 10 were
not stained even by increasing the exposure time of
chemiluminescence reaction (Fig.
S1A). MUC1 and hyaluronic acid appeared close in the SMME. To
confirm hyaluronic acid, we also stained the SMME membrane with
HABP (Fig. 1C). Hyaluronic acid was
detected in all samples at the same migration position as the
reference hyaluronic acid in PGM.
Comparison of O-glycans on mucins
between MEC and NSGs
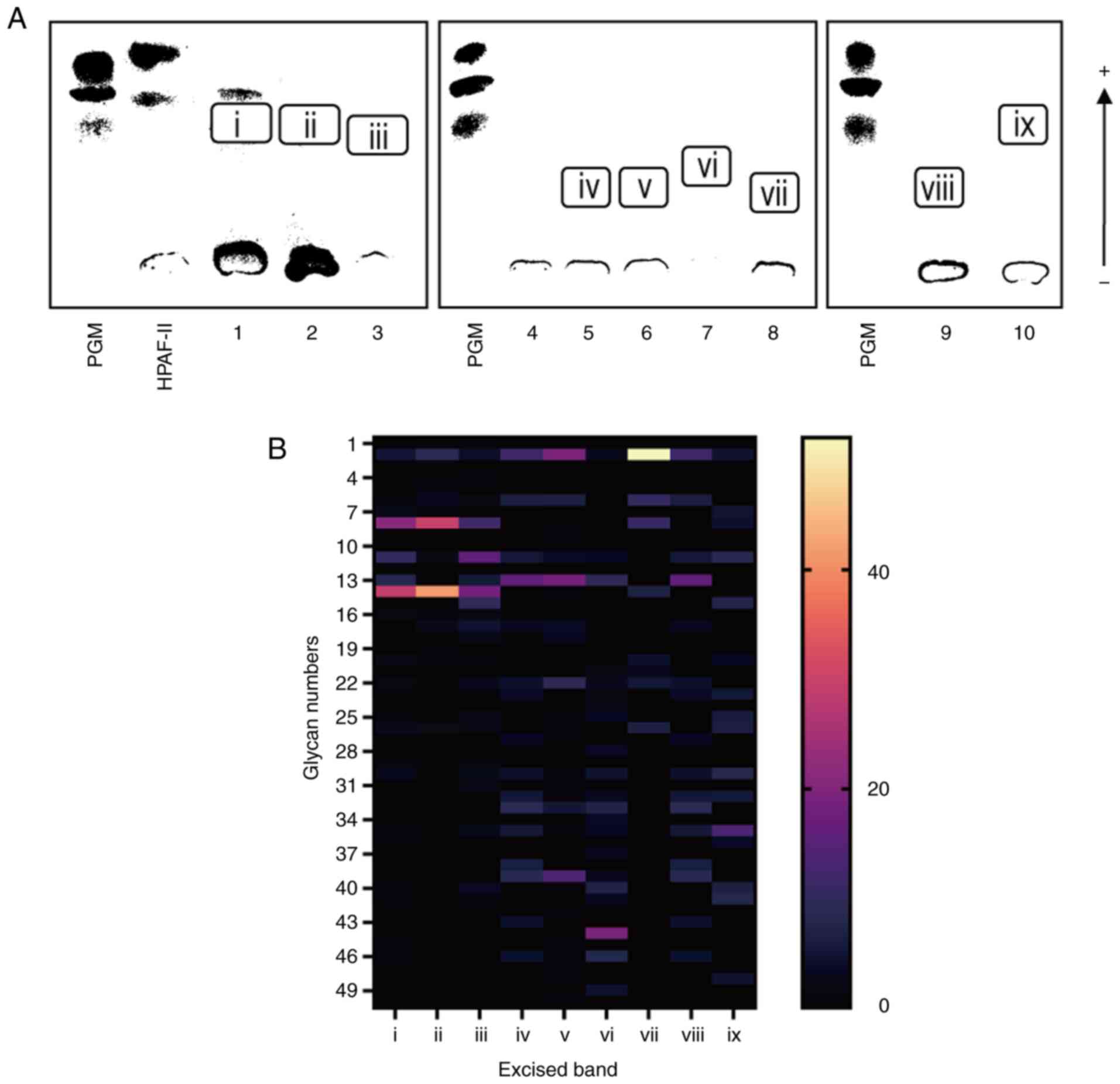
Each band of mucin stained with Alcian blue was
excised and subjected to reductive β-elimination, in which the
O-glycans attached to mucins were released and reduced to
the corresponding alditols (Fig.
2A). The obtained glycan alditols were permethylated and
analyzed using MALDI-TOF MS. All of the observed glycan signals
were categorized into two groups: Sialoglycans and neutral glycans,
as summarized in Table II. The
relative intensities of the glycan signals observed from each band
are depicted in heatmap (Fig. 2B).
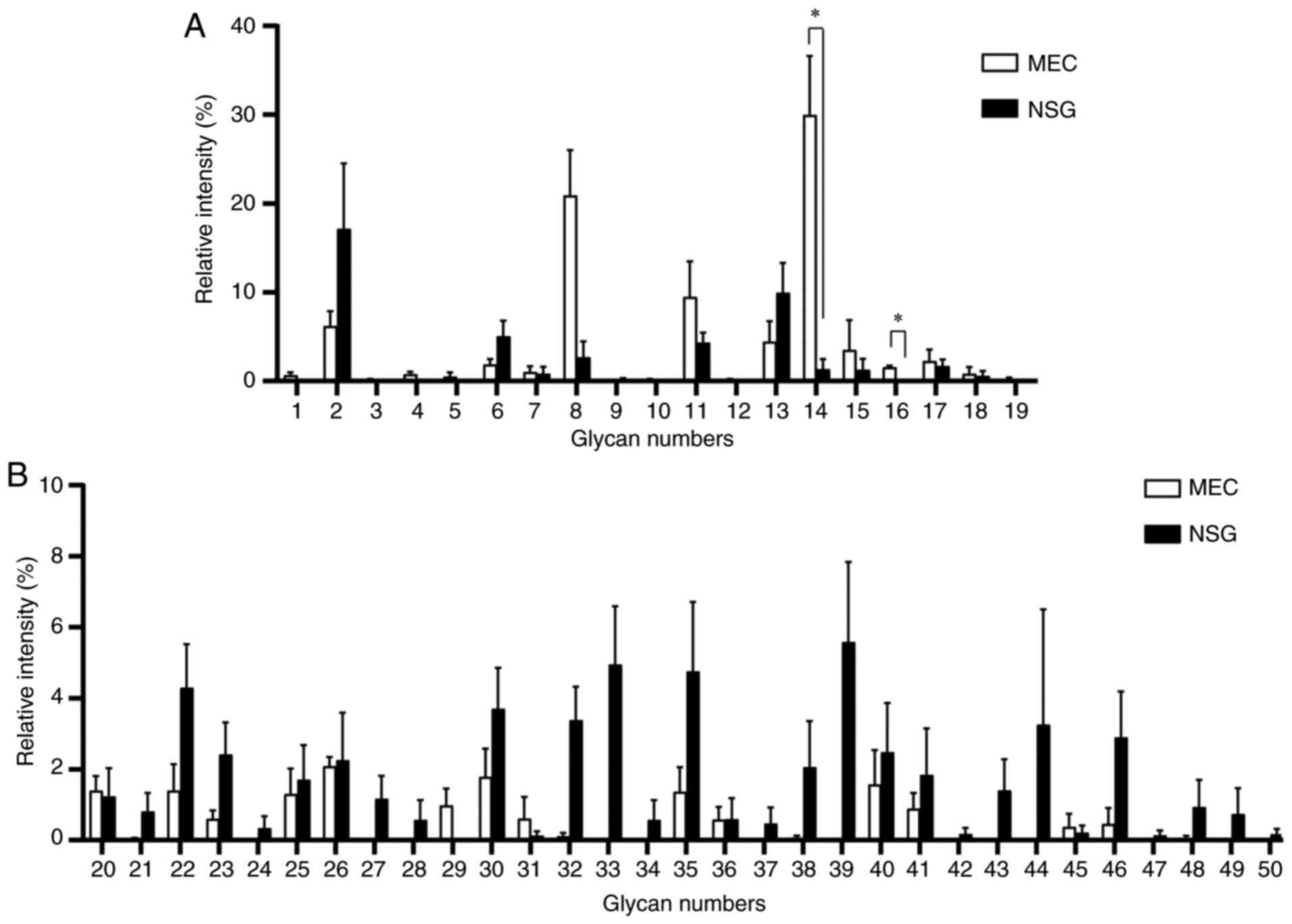
The O-glycans from MEC (i-iii) mostly consisted of
sialoglycans 8 and 14 (orange cells), while the O-glycans
from NSGs (iv-ix) contained substantial neutral glycans (navy blue
cells). This is a distinctive difference in the glycan profiles of
MEC and NSGs. In all of the observed glycan signals, the mean
relative intensities in the two groups MEC (i-iii) and NSG (iv-ix)
were compared (Fig. 3). Notably,
glycan 8 and 14 showed high intensities in MEC compared with NSGs.
These glycans were mono-sialylated and di-sialylated of a common
core structure (Hex)2(HexNAc)2, respectively.
Glycan 1 is sialyl Tn antigen, a well-known glycan biomarker for
various malignant tumors (27,28), and
was detected in two out of three MEC samples, but not in the NSG
samples. On the other hand, many highly fucosylated neutral glycans
(glycan 33, 35, 39, and 44) were abundantly observed in NSGs.
 | Table II.Summary of MS signals of
O-glycans detected from the excised band (Fig. 2A). |
Table II.
Summary of MS signals of
O-glycans detected from the excised band (Fig. 2A).
| A, Acidic
glycans |
|---|
|
|---|
| Glycan no. | Composition | Calcd,
m/za | Obsd,
m/zb |
|---|
| 1 |
(HexNAc)1(NeuAc)1 | 691.36 | 691.37 |
| 2 |
(Hex)1(HexNAc)1(NeuAc)1 | 895.46 | 895.49 |
| 3 |
(HexNAc)2(NeuAc)1 | 936.49 | 936.54 |
| 4 |
(Hex)1(HexNAc)1(Deoxyhexose)1(NeuAc)1 | 1,069.55 | 1,069.58 |
| 5 |
(Hex)1(HexNAc)2(NeuAc)1 | 1,140.59 | 1,140.64 |
| 6 |
(Hex)1(HexNAc)1(NeuAc)2 | 1,256.64 | 1,256.67 |
| 7 |
(Hex)1(HexNAc)2(Deoxyhexose)1(NeuAc)1 | 1,314.68 | 1,314.71 |
| 8 |
(Hex)2(HexNAc)2(NeuAc)1 | 1,344.69 | 1,344.74 |
| 9 |
(Hex)2(HexNAc)1(Deoxyhexose)2(NeuAc)1 | 1,447.74 | 1,447.79 |
| 10 |
(Hex)1(HexNAc)2(NeuAc)2 | 1,501.76 | 1,501.81 |
| 11 |
(Hex)2(HexNAc)2(Deoxyhexose)1(NeuAc)1 | 1,518.78 | 1,518.82 |
| 12 |
(Hex)2(HexNAc)3(NeuAc)1 | 1,589.82 | 1,589.86 |
| 13 |
(Hex)2(HexNAc)2(Deoxyhexose)2(NeuAc)1 | 1,692.87 | 1,692.89 |
| 14 |
(Hex)2(HexNAc)2(NeuAc)2 | 1,705.86 | 1,705.88 |
| 15 |
(Hex)2(HexNAc)3(Deoxyhexose)1(NeuAc)1 | 1,763.90 | 1,763.94 |
| 16 |
(Hex)3(HexNAc)3(NeuAc)1 | 1,793.92 | 1,793.90 |
| 17 |
(Hex)2(HexNAc)2(Deoxyhexose)1(NeuAc)2 | 1,879.95 | 1,880.01 |
| 18 |
(Hex)2(HexNAc)3(Deoxyhexose)2(NeuAc)1 | 1,937.99 | 1,938.03 |
| 19 |
(Hex)2(HexNAc)3(NeuAc)2 | 1,950.99 | 1,951.06 |
|
| B, Neutral
glycans |
|
| Glycan
no. |
Composition | Calcd,
m/za | Obsd,
m/zb |
|
| 20 |
(Hex)1(HexNAc)1 | 534.29 | 534.28 |
| 21 |
(HexNAc)2 | 575.32 | 575.18 |
| 22 |
(Hex)1(HexNAc)1(Deoxyhexose)1 | 708.38 | 708.40 |
| 23 |
(Hex)1(HexNAc)2 | 779.41 | 779.44 |
| 24 |
(Hex)2(HexNAc)1(Deoxyhexose)1 | 912.48 | 912.46 |
| 25 |
(Hex)1(HexNAc)2(Deoxyhexose)1 | 953.50 | 953.54 |
| 26 |
(Hex)2(HexNAc)2 | 983.52 | 983.57 |
| 27 |
(Hex)1(HexNAc)3 | 1,024.54 | 1,024.59 |
| 28 |
(Hex)2(HexNAc)1(Deoxyhexose)2 | 1,086.57 | 1,086.53 |
| 29 |
(Hex)1(HexNAc)2(Deoxyhexose)2 | 1,127.59 | 1,127.63 |
| 30 |
(Hex)2(HexNAc)2(Deoxyhexose)1 | 1,157.60 | 1,157.64 |
| 31 |
(Hex)1(HexNAc)3(Deoxyhexose)1 | 1,198.63 | 1,198.69 |
| 32 |
(Hex)2(HexNAc)3 | 1,228.64 | 1,228.68 |
| 33 |
(Hex)2(HexNAc)2(Deoxyhexose)2 | 1,331.69 | 1,331.75 |
| 34 |
(Hex)3(HexNAc)2(Deoxyhexose)1 | 1,361.70 | 1,361.66 |
| 35 |
(Hex)2(HexNAc)3(Deoxyhexose)1 | 1,402.73 | 1,402.78 |
| 36 |
(Hex)3(HexNAc)3 | 1,432.74 | 1,432.75 |
| 37 |
(Hex)3(HexNAc)1(Deoxyhexose)3 | 1,464.76 | 1,464.69 |
| 38 |
(Hex)2(HexNAc)4 | 1,473.77 | 1,473.83 |
| 39 |
(Hex)2(HexNAc)2(Deoxyhexose)3 | 1,505.78 | 1,505.81 |
| 40 |
(Hex)2(HexNAc)3(Deoxyhexose)2 | 1,576.82 | 1,576.85 |
| 41 |
(Hex)3(HexNAc)3(Deoxyhexose)1 | 1,606.83 | 1,606.82 |
| 42 |
(Hex)4(HexNAc)3 | 1,636.84 | 1,636.94 |
| 43 |
(Hex)2(HexNAc)4(Deoxyhexose)1 | 1,647.86 | 1,647.88 |
| 44 |
(Hex)3(HexNAc)2(Deoxyhexose)3 | 1,709.88 | 1,709.81 |
| 45 |
(Hex)2(HexNAc)3(Deoxyhexose)3 | 1,750.91 | 1,750.96 |
| 46 |
(Hex)3(HexNAc)3(Deoxyhexose)2 | 1,780.92 | 1,780.95 |
| 47 |
(Hex)2(HexNAc)4(Deoxyhexose)2 | 1,821.95 | 1,822.05 |
| 48 |
(Hex)3(HexNAc)4(Deoxyhexose)1 | 1,851.96 | 1,852.00 |
| 49 |
(Hex)3(HexNAc)3(Deoxyhexose)3 | 1,955.01 | 1,954.90 |
| 50 |
(Hex)2(HexNAc)4(Deoxyhexose)3 | 1,996.04 | 1,996.10 |
Structural analysis of the glycans
from MEC
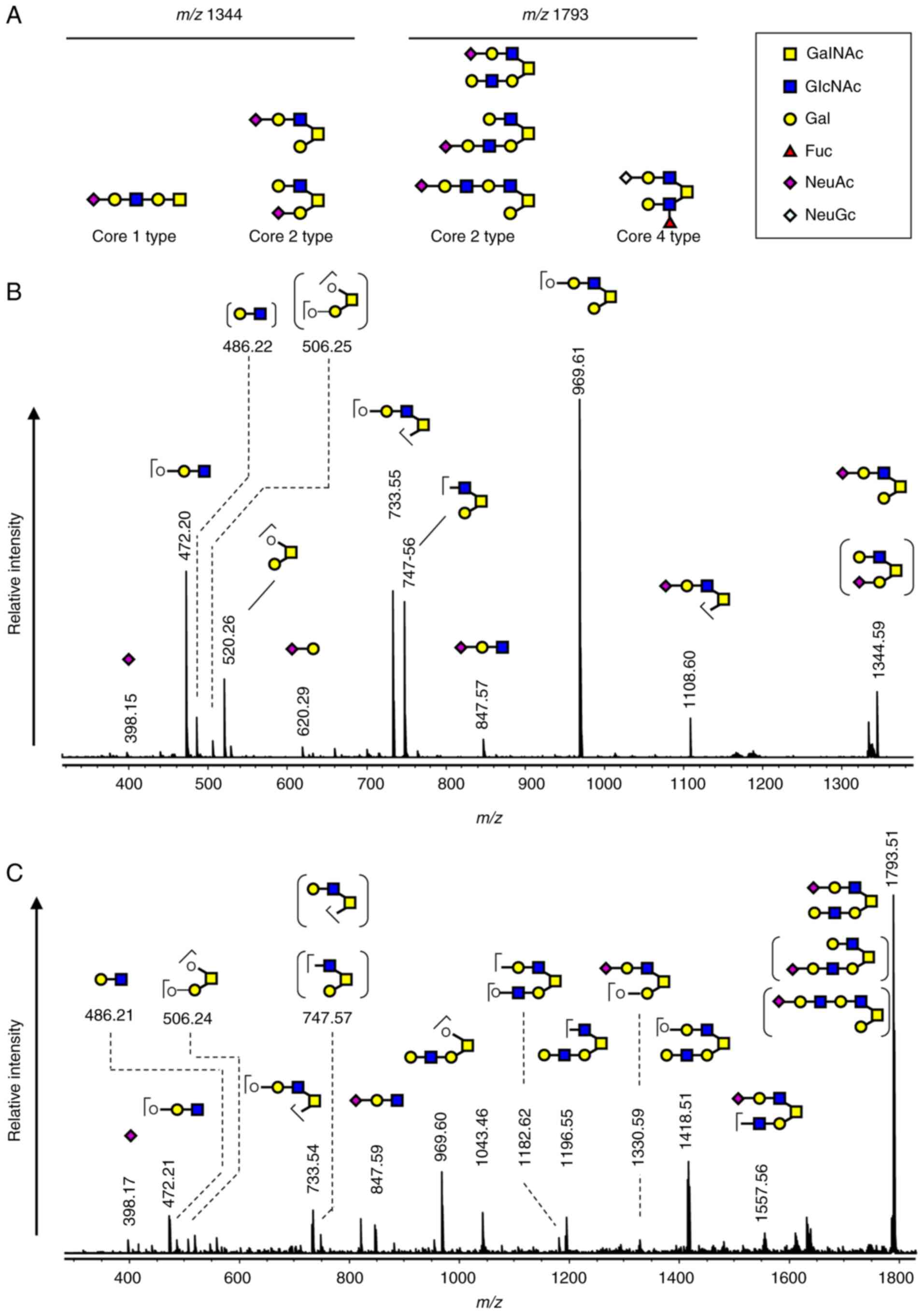
The significant glycan 8 and 14 were mono- and
di-sialylated structures of the same core structure
(Hex)2(HexNAc)2, respectively. Another
significant glycan, glycan 16, is the mono-sialylated structure of
(Hex)3(HexNAc)3. To elucidate the core
structures of the significant glycans in MEC, we acquired the MS/MS
spectra of glycan 8 and 16. Based on the biosynthetic pathway of
the O-glycans, we proposed potential structures for glycans
8 (m/z 1,344) and 16 (m/z 1,793), respectively
(Fig. 4A). The MS/MS spectrum of
glycan 8 (m/z 1,344) revealed that glycan 8 was a mixture of
the positional isomers of sialylation of the same structure that
was galactosylated at the GlcNAc of core 2 (Fig. 4B). The MS/MS spectrum of glycan 16
(m/z 1,973) was in agreement with the calculated fragments
of the N-acetyl lactosamine (LacNAc) elongated core 2
(Fig. 4C).
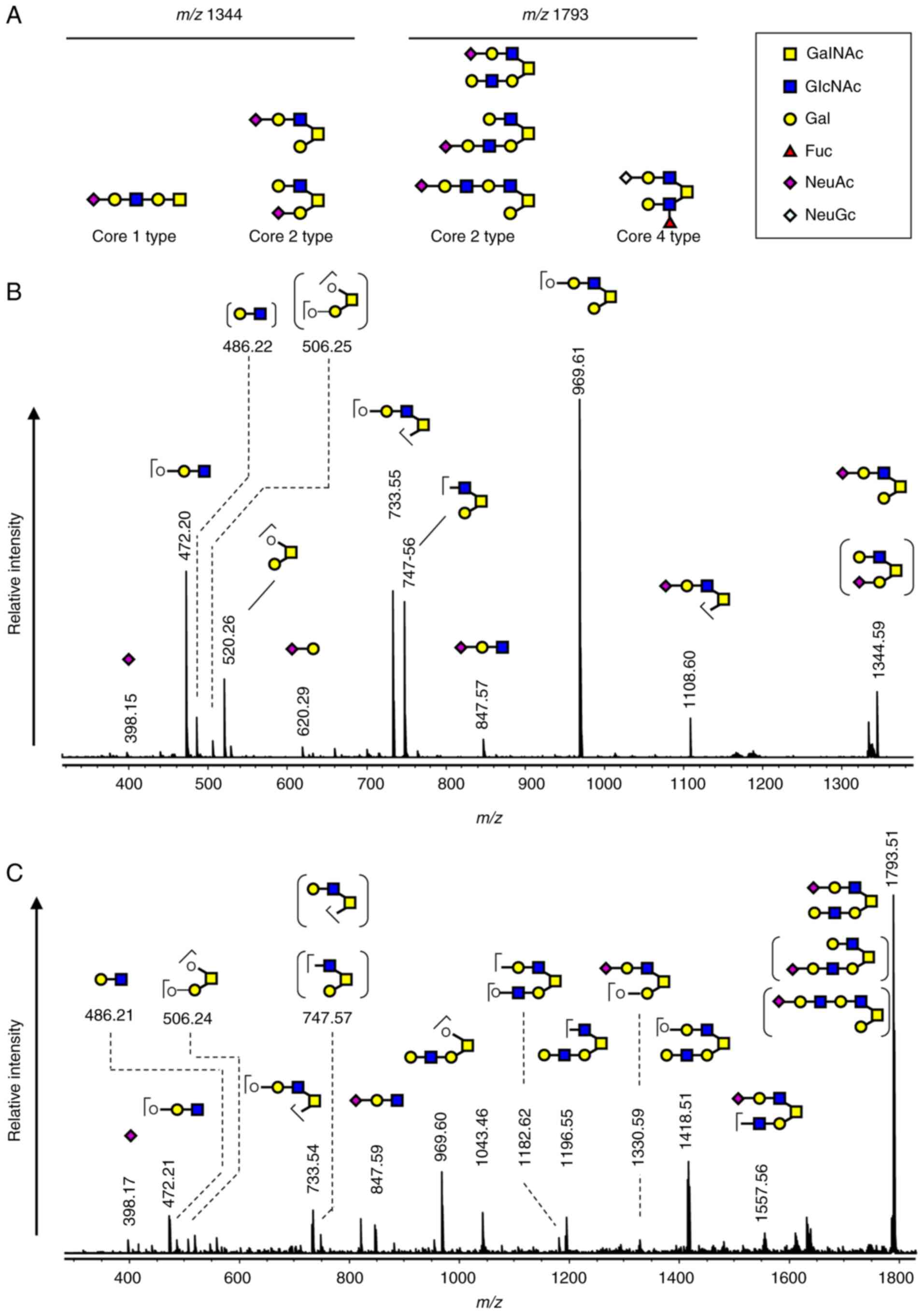 | Figure 4.Proposed structures for the two
significant glycans, glycan 8 (m/z, 1,344) and 16
(m/z, 1,793). (A) Possible structures for glycans 8
(m/z, 1,344) and 16 (m/z, 1,793) based on the
biosynthetic pathway. (B) MS/MS spectrum of glycan 8 (m/z,
1,344). (C) MS/MS spectrum of glycan 16 (m/z, 1,793). The
proposed structure and assignment of the fragment ions are
indicated in the spectra. The structures in parentheses are
considered to be minor components. MS/MS, tandem mass
spectrometry. |
Discussion
In this study, MEC was found to abundantly produce
MUC1, which was characteristically modified with core 2 type
sialoglycans. The secretion of mucins in the oral cavity and the
number of sialic acids on the mucins have been reported to decrease
with aging (29). MEC samples 1 and
2 and NSG sample 7 were obtained from middle-aged patients (38–41
years old) and showed dark bands in Alcian blue staining during
SMME analysis, while other samples from patients over 50 years of
age showed pale bands. This is consistent with the previous report
described above. MUC1 is involved in cell proliferation and signal
transduction (11,30) and has been known to be overexpressed
in malignant tumors (31).
Immunohistochemistry using the MUC1 antibody showed that higher
levels of MUC1 expression were positively correlated with the
malignancy and prognosis of MEC (17,18). In
our experiments, MUC1 was only detected in MEC. Although MEC sample
3 appeared to be MUC1-negative, all three MEC samples became
MUC1-positive by increasing the exposure time of chemiluminescence
imaging (Fig. S1A). On the other
hand, all NSGs in our experiment were found to be MUC1-negative.
The incidence of MEC is high in relatively young patients (average
age: 48.8 years old) (32). Notably,
MUC1 was not detected even in the NSGs of relatively young patients
(6, 7, 8, 9: 41–57 years old). MUC1 is expressed as a
membrane-bound mucin in the ducts of all normal salivary gland
tissues (33,34). In the present study, only the
water-soluble fraction was analyzed, suggesting that the expression
of water-soluble MUC1 was closely related to the development of
MEC. The MUC1 antibody, MY.1E12, recognizes MUC1 with a sialyl T
(Neu5Acα2-3Galβ1-3GalNAc) structure (23). We could not deny that NSGs produce
MUC1 without this sialyl T structure. To clarify this point, the
SMME membranes were stained using another anti-MUC1 antibody, VU4H5
which recognizes a tandem repeat domain of MUC1. The results
supported the finding that MEC but not the NSGs expressed MUC1
(Fig. S1B). The origin spots of the
MEC samples were strongly stained, which suggested that MUC1 exists
in its insoluble form in the sample solution (Fig. S1A and B). MUC1, one of the
membrane-bound mucins, has a cleavage site in the extracellular
domain (35,36). The cleaved MUC1 is able to migrate to
the upper part during SMME, while the membrane-bound form remains
in the origin. On the Alcian blue stained membrane, NSG sample 10
showed a mucin band at almost the same position as MUC1 from the
MEC samples. However, the band could not be stained with either of
the MUC1 antibodies, MY.1E12 and VU4H5 (Fig. S1).
All of the MEC samples in this study were obtained
from minor salivary glands. For NSG, samples 4–8 were obtained from
submandibular glands, while samples 9 and 10 were obtained from the
sublingual gland and the minor salivary gland, respectively. The
difference in the types of salivary glands may affect mucin
expression. The staining of the SMME membranes with Alcian blue
showed clear differences between the minor salivary glands (1–3,
and 10) and submandibular glands (4–8).
Moreover, the sublingual gland (9)
was different from the other two types. Although the number of
cases will need to be increased to confirm differences depending on
the type of salivary gland, the fact that MUC1 was only detected in
MEC (1–3), and not NSGs (10), obtained from minor salivary glands is
a key result. In the present study, only three MEC samples were
compared with the NSGs. It would have been better if we could have
compared MEC lesions and normal areas in the same patients, but all
of the MEC in this study were minor salivary glands, and we could
not clearly distinguish between normal areas and lesions.
Therefore, we cannot deny that individual differences may have
affected the present results. In the future, we plan to conduct
similar experiments involving the analyses of MECs in the major
salivary glands and other mucus-producing salivary gland tumors,
such as acinic cell carcinoma, low-grade salivary duct carcinoma,
mammary analog secretory carcinoma, and mucinous variant of
myoepithelioma, all of which are MUC1 positive (37–40). We
thereby aim to clarify whether the origin and types of salivary
gland tumors affect the glycan structure of tumor-associated
MUC1.
The glycan profiles of mucin were also clearly
different between MEC (i-iii) and NSG (iv-ix) The glycans from the
MEC mucins largely consisted of sialoglycans, while those from NSG
mucins contained many neutral glycans. Although sialic acids have
been reported to decrease with aging (29), NSG mucin (vi) from the submandibular
gland of a 41-year-old patient had fewer sialoglycans and NSG mucin
(vii) compared to the submandibular gland of a 55-year-old patient,
whose glycan profile showed a high ratio of sialoglycans. It was
also unclear whether the types of salivary glands had an effect on
the glycan profiles of the mucins in our experiment. In the two
group comparisons between MEC and NSG, the intensities of glycan 8
and 14 were found to be significantly high in MEC. The two glycans
were sialylated core 2 glycans. The mRNA expression of core
2-β-1,6-N-acetylglucosaminyltransferase-1 (GCNT1), one of
the key enzymes responsible for the core 2 branched structure, is
associated with the progression of several cancers, including
colorectal cancer, pulmonary adenocarcinoma, and prostate cancer
(41–43). It has also been suggested that MUC1
carrying core 2 glycans contribute to the ability of cancer cells
to evade attack by natural killer cells (44). Thus, MUC 1 carrying core 2 glycans
expressed in MEC may play an important role in malignant cellular
behavior. The sialyl Tn (STn) antigen has been widely reported as a
tumor-associated glycan antigen. In the present study, STn (glycan
1) was only detected in MEC samples, but with a very small
intensity. The STn antigen in MUC1 has potential as a specific
biomarker for MEC, however, the sialylated core 2 glycans described
above are more likely to be used as biomarkers because of their
prominent intensities. It has also been reported that the sialic
acid levels are increased in malignant tumors (45), which is in good agreement with our
results. The abnormal sialylation of cancer cells is a
characteristic alteration associated with malignant properties,
including invasiveness and metastatic potential (46). Although it has been reported that
high MUC1 expression is positively correlated with malignancy, it
is still unclear whether the glycan structures of the
tumor-associated MUC1 are correlated to the MEC grade because our
experiments used only low-grade MEC samples. Using
immunohistochemistry, a previous study revealed that the positivity
rate of Tn and Lewis a is decreased in high-grade MEC (28). We intend to obtain experimental data
on the correlation between the grades and glycan structures of
tumor-associated MUC1 in the water-soluble fractions of MEC samples
in the future.
In this study, we analyzed the soluble fractions
obtained from the homogenates of salivary glands and identified a
characteristic mucin, namely MUC1 with sialylated core 2 glycans.
Unlike MUC7, which is secreted by goblet cells via exocytosis from
the salivary glands into the saliva, MUC1 is usually not secreted,
even in the case of soluble MUC1, which is cleaved at the
extracellular domain. Soluble MUC1 may enter the blood circulation
from lesion areas and has potential for use as a serum biomarker
for several tumors that produce MUC1 with characteristic glycans,
such as STn and sialyl Lewis a (47). A previous study reported that the
serum levels of CA153, a MUC1 antigen recognized by the two
anti-MUC1 antibodies DF3 and 115D8, are elevated in some diseases,
including various cancers, type 2 diabetes, and coronary heart
disease (48). The authors proposed
that pathological leakage of CA153 from the epithelium, in addition
to the decreased CA153 clearance rate may cause the MUC1 antigen to
appear in the blood of patients with the aforementioned diseases.
When MUC1 with sialylated core 2 glycans can be used as a serum
biomarker for MEC, CA153 in the serum of patients with these
diseases may be a confounding variable for tumor-associated MUC1
from MEC. To avoid such confusion, it may be important to
distinguish the differences in the glycans of MUC1. KL6 for lung
disease and WFA-positive MUC1 for intrahepatic cholangiocarcinoma
are known examples in which the glycans of MUC1 differ among
primary tumor tissues (49,50). Regrettably, there is no information
on the glycans of MUC1 in salivary glands. To clarify these issues
in the future, it is necessary to analyze the expression of MUC1,
including its glycans, in other oral tumors, and investigate its
leakage into the bloodstream.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
The present study was partially supported by the
Japan Society for the Promotion of Science KAKENHI (grant nos.
JP17H03808 and JP17K19627) and the Mizutani Foundation for
Glycoscience (grant no. 200049).
Availability of data and materials
The datasets generated and/or analyzed during the
current study are available in the MassIVE repository (https://massive.ucsd.edu/ProteoSAFe/dataset.jsp?task=441d55f0338f4e09a75d00be9f0acbc0;
accession no. MSV000087578).
Authors' contributions
EI, TN, KK, UA and AK designed the study. KH
performed pathological evaluation of the salivary glands. EI, TS
and AK performed SMME and glycan analysis. EI, TS and AK confirmed
the authenticity of all the raw data. EI and AK interpreted the
acquired data and prepared the manuscript. TN, KK and UA
contributed to critical revision of the manuscript for important
intellectual content. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
This research was approved by the Tokyo Dental
College Ichikawa General Hospital Ethics Review Committee (approval
no. I16-74; Ichikawa, Japan) and the AIST Committee on Bioethics of
Experiments Involving Human-derived Materials (approval no. h-213;
Tokyo, Japan). Written informed consent was obtained for
experimentation with human subjects.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
2,5-DHB
|
2,5-dihydroxybezoic acid
|
|
FNAC
|
fine-needle aspiration cytology
|
|
HABP
|
hyaluronic acid binding protein
|
|
MEC
|
mucoepidermoid carcinoma
|
|
MS
|
mass spectrometry
|
|
NSG
|
normal salivary gland
|
|
PGM
|
porcine gastric mucin
|
|
PVA
|
poly (vinyl alcohol)
|
|
PVP
|
polyvinylpyrrolidone
|
|
QIT
|
quadrupole ion trap
|
|
SMME
|
supported molecular matrix
electrophoresis
|
|
STn
|
sialyl Tn
|
|
TOF
|
time-of-flight
|
|
VNTR
|
variable number of tandem repeat
|
References
|
1
|
EI-Naggar AK, Chan JKC, Grandis JR, Takata
T and Slootweg PJ: WHO classification of head and neck tumors. 4th
edition. IARC Press; Lyon: 2017
|
|
2
|
Diwakar JK, Agarwal A, Garg C, Giri KY,
Dandriyal R and Kumar G: A rare case of mucoepidermoid carcinoma of
parotid with mandibular metastasis. Ann Maxillofac Surg. 9:205–207.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Janet-Ofelia GC, Rafael MV, Guillermo GA,
Carlos-Enrique CV, José-Martín RM, Henry GM and Jaime-Enrique MG:
Mucoepidermoid carcinoma of the salivary glands: Survival and
prognostic factors. J Maxillofac Oral Surg. 16:431–437. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liu S, Ow A, Ruan M, Yang W and Zhang C,
Wang L and Zhang C: Prognostic factors in primary salivary gland
mucoepidermoid carcinoma: An analysis of 376 cases in an Eastern
Chinese population. Int J Oral Maxillofac Surg. 43:667–673. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pusztaszeri MP and Faquin WC: Update in
salivary gland cytopathology: Recent molecular advances and
diagnostic applications. Semin Diagn Pathol. 32:264–274. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lombardi D, McGurk M, Vander Poorten V,
Guzzo M, Accorona R, Rampinelli V and Nicolai P: Surgical treatment
of salivary malignant tumors. Oral Oncol. 65:102–113. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Brandwein MS, Ferlito A, Bradley PJ, Hille
JJ and Rinaldo A: Diagnosis and classification of salivary
neoplasms: Pathologic challenges and relevance to clinical
outcomes. Acta Otolaryngol. 122:758–764. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Stowell SR, Ju T and Cummings RD: Protein
glycosylation in cancer. Annu Rev Pathol. 10:473–510. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Varki A: Biological roles of
oligosaccharides: All of the theories are correct. Glycobiology.
3:97–130. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Adamczyk B, Tharmalingam T and Rudd PM:
Glycans as cancer biomarkers. Biochim Biophys Acta. 1820:1347–1353.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gendler SJ: MUC1, the renaissance
molecule. J Mammary Gland Biol Neoplasia. 6:339–353. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pinto R, Carvalho AS, Conze T, Magalhães
A, Picco G, Burchell JM, Taylor-Papadimitriou J, Reis CA, Almeida
R, Mandel U, et al: Identification of new cancer biomarkers based
on aberrant mucin glycoforms by in situ proximity ligation. J Cell
Mol Med. 16:1474–1484. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Julien S, Videira PA and Delannoy P:
Sialyl-tn in cancer: (How) Did we miss the target? Biomolecules.
2:435–466. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kudelka MR, Ju T, Heimburg-Molinaro J and
Cummings RD: Simple sugars to complex disease-mucin-type O-glycans
in cancer. Adv Cancer Res. 126:53–135. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cazet A, Julien S, Bobowski M, Burchell J
and Delannoy P: Tumour-associated carbohydrate antigens in breast
cancer. Breast Cancer Res. 12:2042010. View
Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cheever MA, Allison JP, Ferris AS, Finn
OJ, Hastings BM, Hecht TT, Mellman I, Prindiville SA, Viner JL,
Weiner LM and Matrisian LM: The prioritization of cancer antigens:
A national cancer institute pilot project for the acceleration of
translational research. Clin Cancer Res. 15:5323–5337. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Alos L, Lujan B, Castillo M, Nadal A,
Carreras M, Caballero M, de Bolos C and Cardesa A: Expression of
membrane-bound mucins (MUC1 and MUC4) and secreted mucins (MUC2,
MUC5AC, MUC5B, MUC6 and MUC7) in mucoepidermoid carcinomas of
salivary glands. Am J Surg Pathol. 29:806–813. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Handra-Luca A, Lamas G, Bertrand JC and
Fouret P: MUC1, MUC2, MUC4, and MUC5AC expression in salivary gland
mucoepidermoid carcinoma: Diagnostic and prognostic implications.
Am J Surg Pathol. 29:881–889. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Matsuno YK, Saito T, Gotoh M, Narimatsu H
and Kameyama A: Supported molecular matrix electrophoresis: A new
tool for characterization of glycoproteins. Anal Chem.
81:3816–3823. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kameyama A, Yamakoshi K and Watanabe A: A
rapid separation and characterization of mucins from mouse
submandibular glands by supported molecular matrix electrophoresis.
Biochim Biophys Acta Proteins Proteom. 1867:76–81. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Brierley JD, Gospodarowicz MK and
Wittekind C: TNM Classification of Malignant Tumours. 8th edition.
Wiley-Blackwell; Oxford: pp. p2722016
|
|
22
|
Yamamoto M, Bhavanandan VP, Nakamori S and
Irimura T: A novel monoclonal antibody specific for sialylated MUC1
mucin. Jpn J Cancer Res. 87:488–496. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Takeuchi H, Kato K, Denda-Nagai K, Hanisch
FG, Clausen H and Irimura T: The epitope recognized by the unique
anti-MUC1 monoclonal antibody MY.1E12 involves sialyl alpha
2-3galactosyl beta 1-3N-acetylgalactosaminide linked to a distinct
threonine residue in the MUC1 tandem repeat. J Immunol Methods.
270:199–209. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Matsuno YK, Dong W, Yokoyama S, Yonezawa
S, Saito T, Gotoh M, Narimatsu H and Kameyama A: Improved method
for immunostaining of mucin separated by supported molecular matrix
electrophoresis by optimizing the matrix composition and fixation
procedure. Electrophoresis. 32:1829–1836. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Matsuno YK, Dong W, Yokoyama S, Yonezawa
S, Narimatsu H and Kameyama A: Identification of mucins by using a
method involving a combination of on-membrane chemical
deglycosylation and immunostaining. J Immunol Methods. 394:125–130.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Xu J, Sun H, Huang G, Liu G, Li Z, Yang H,
Jin L, Cui X, Shi L, Ma T, et al: A fixation method for the
optimisation of western blotting. Sci Rep. 9:66492019. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ju T, Lanneau GS, Gautam T, Wang Y, Xia B,
Stowell SR, Willard MT, Wang W, Xia JY, Zuna RE, et al: Human tumor
antigens Tn and sialyl Tn arise from mutations in Cosmc. Cancer
Res. 68:1636–1646. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Matse JH, Bharos WK, Veerman ECI, Bloemena
E and Bolscher JGM: Mucoepidermoid carcinoma-associated expression
of MUC5AC, MUC5B and mucin-type carbohydrate antigen sialyl-Tn in
the parotid gland. Arch Oral Biol. 82:121–126. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Pushpass RG, Pellicciotta N, Kelly C,
Proctor G and Carpenter GH: Reduced salivary mucin binding and
glycosylation in older adults influences taste in an in vitro cell
model. Nutrients. 11:22802019. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Bafna S, Kaur S and Batra SK:
Membrane-bound mucins: The mechanistic basis for alterations in the
growth and survival of cancer cells. Oncogene. 29:2893–2904. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Xu F, Liu F, Zhao H, An G and Feng G:
Prognostic significance of mucin antigen MUC1 in various human
epithelial cancers: A meta-analysis. Medicine (Baltimore).
94:e22862015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Peraza A, Gómez R, Beltran J and Amarista
FJ: Mucoepidermoid carcinoma. An update and review of the
literature. J Stomatol Oral Maxillofac Surg. 121:713–720. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Sengupta A, Valdramidou D, Huntley S,
Hicks SJ, Carrington SD and Corfield AP: Distribution of MUC1 in
the normal human oral cavity is localized to the ducts of minor
salivary glands. Arch Oral Biol. 46:529–538. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ponce-Bravo S, Ledesma-Montes C and
Morales-Sánchez I: MUC-1 mucin in normal human salivary glands
detected by HMFG-1 and HMFG-2 monoclonal antibodies. APMIS.
116:93–98. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Levitin F, Stern O, Weiss M, Gil-Henn C,
Ziv R, Prokocimer Z, Smorodinsky NI, Rubinstein DB and Wreschner
DH: The MUC1 SEA module is a self-cleaving domain. J Biol Chem.
280:33374–33386. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Duraisamy S, Kufe T, Ramasamy S and Kufe
D: Evolution of the human MUC1 oncoprotein. Int J Oncol.
31:671–677. 2007.PubMed/NCBI
|
|
37
|
Ma S, An F, Li LH, Lin YY and Wang J:
Expression of Mucin 1 in salivary gland tumors and its correlation
with clinicopathological factors. J Biol Regul Homeost Agents.
33:563–569. 2019.PubMed/NCBI
|
|
38
|
Kusafuka K, Itoh H, Sugiyama C and
Nakajima T: Low-grade salivary duct carcinoma of the parotid gland:
Report of a case with immunohistochemical analysis. Med Mol
Morphol. 43:178–184. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Cros J, Sbidian E, Hans S, Roussel H,
Scotte F, Tartour E, Brasnu D, Laurent-Puig P, Bruneval P, Blons H
and Badoual C: Expression and mutational status of
treatment-relevant targets and key oncogenes in 123 malignant
salivary gland tumours. Ann Oncol. 24:2624–2629. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Khurram SA, Sultan-Khan J, Atkey N and
Speight PM: Cytogenetic and immunohistochemical characterization of
mammary analogue secretory carcinoma of salivary glands. Oral Surg
Oral Med Oral Pathol Oral Radiol. 122:731–742. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
St Hill CA, Farooqui M, Mitcheltree G,
Gulbahce HE, Jessurun J, Cao Q and Walcheck B: The high affinity
selectin glycan ligand C2-O-sLex and mRNA transcripts of the core 2
beta-1,6-N-acetylglucosaminyltransferase (C2GnT1) gene are highly
expressed in human colorectal adenocarcinomas. BMC Cancer.
9:792009. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Machida E, Nakayama J, Amano J and Fukuda
M: Clinicopathological significance of core 2
beta1,6-N-acetylglucosaminyltransferase messenger RNA expressed in
the pulmonary adenocarcinoma determined by in situ hybridization.
Cancer Res. 61:2226–2231. 2001.PubMed/NCBI
|
|
43
|
Chen Z, Gulzar ZG, St Hill CA, Walcheck B
and Brooks JD: Increased expression of GCNT1 is associated with
altered O-glycosylation of PSA, PAP, and MUC1 in human prostate
cancers. Prostate. 74:1059–1067. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Tsuboi S, Sutoh M, Hatakeyama S, Hiraoka
N, Habuchi T, Horikawa Y, Hashimoto Y, Yoneyama T, Mori K, Koie T,
et al: A novel strategy for evasion of NK cell immunity by tumours
expressing core2 O-glycans. EMBO J. 30:3173–3185. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Basu S, Basu M and Basu SS: Biological
specificity of sialyltransferases. Biology of the sialic acids.
Rosenberg A: Plenum Press; New York: pp. 69–94. 1995, View Article : Google Scholar
|
|
46
|
Vajaria BN, Patel KR, Begum R and Patel
PS: Sialylation: An avenue to target cancer cells. Pathol Oncol
Res. 22:443–447. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Kirwan A, Utratna M, O'Dwyer ME, Joshi L
and Kilcoyne M: Glycosylation-based serum biomarkers for cancer
diagnostics and prognostics. Biomed Res Int. 2015:4905312015.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Li X, Xu Y and Zhang L: Serum CA153 as
biomarker for cancer and noncancer diseases. Prog Mol Biol Transl
Sci. 162:265–276. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Ishikawa N, Hattori N, Yokoyama A and
Kohno N: Utility of KL-6/MUC1 in the clinical management of
interstitial lung diseases. Respir Investig. 50:3–13. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Silsirivanit A, Matsuda A, Kuno A, Tsuruno
C, Uenoyama Y, Seubwai W, Angata K, Teeravirote K, Wongkham C,
Araki N, et al: Multi-serum glycobiomarkers improves the diagnosis
and prognostic prediction of cholangiocarcinoma. Clin Chim Acta.
510:142–149. 2020. View Article : Google Scholar : PubMed/NCBI
|