Introduction
Multiple myeloma (MM), although a relatively
uncommon disease, is the second most commonly diagnosed hematologic
malignancy after lymphoma (1,2). MM,
also known as plasma cell myeloma, begins with monoclonal
proliferation of plasma cells in the bone marrow and then spreads
throughout the body via the bloodstream, resulting in significant
bone destruction and displacement of normal hematopoietic cells
(3). Despite recent advances in
chemotherapeutic treatment, MM is still an incurable disease
characterized by remission and relapse in the majority of patients
(4). The molecular mechanisms of
many aspects of MM, including malignant transformation, progression
and dissemination, bone destruction, and chemotherapy resistance,
are not fully understood. Importantly, all these characteristics of
MM are seemingly associated with abnormal calcium homeostasis and
signaling (5). Intracellular
Ca2+ signaling, as an important second messenger,
regulates tumor cell behavior, and altered calcium signaling may
contribute to cancer progression, metastasis, and resistance to
chemotherapy (6). Calcium channels
that control Ca2+ influx and remodel cellular calcium
homeostasis regulate various cancer cell hallmarks such as
proliferation, migration, and invasion (7). Emerging evidence indicates that
calcium channels are involved in the development, progression, and
chemotherapy of MM (5).
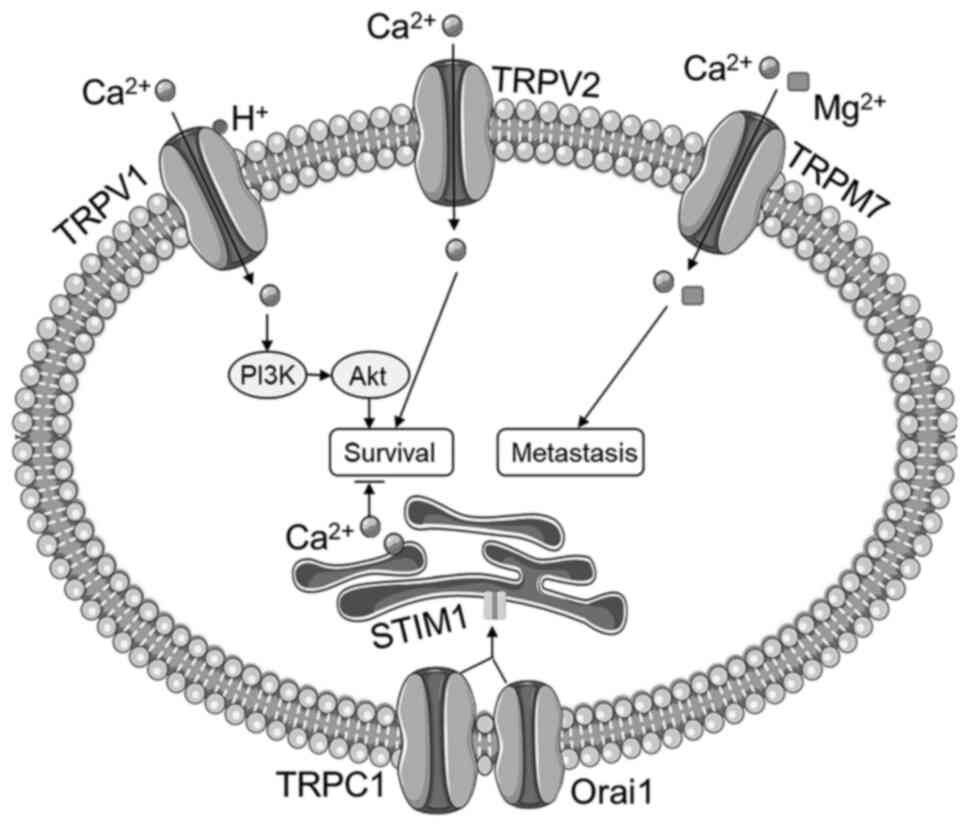
Transient receptor potential (TRP) cation channels
are a superfamily of non-selective Ca2+-permeable
channels consisting of six subfamilies: TRPV (vanilloid), TRPM
(melastatin), TRPA (ankyrin), TRPC (canonical), TRPP (polycystic),
and TRPML (mucolipin) in mammals (8). Most TRP channels are non-selective
Ca2+ permeable, while some of them are also permeable to
sodium and magnesium cations. Many members in the TRPV, TRPM, and
TRPA subfamilies are thermosensory channels, also known as
thermoTRPs, which are activated by changes in ambient temperature
ranging from noxious cold to unpleasant heat (9). Recent studies found that the S1-S4
domain in the protein structure of the TRPV1 channel significantly
contributes to thermosensing and temperature-dependent activation
(10). Although the thermoTRPs
such as TRPV1 and TRPV2 have similar function in mediating
Ca2+ entry, they have distinct functions in cellular
processes by changing their expression levels and responding to
different stimulants (11). We
realized that these thermosensory TRP channels can also detect
various endogenous stress stimuli and respond to tissue damage
(12). Members in the TRPC
subfamily are considered as calcium release activated channels that
contribute to store-operated calcium entry (SOCE) through
interacting with calcium release-activated calcium modulator 1
(Orai1) and stromal interaction molecule 1 (STIM1) (13). Although the primary roles of TRP
channels are perception of a variety of sensations such as pain,
temperature, tastes, pressure, and vision, accumulative evidence
demonstrates that TRP channels also participate in the regulation
of proliferation, differentiation, and apoptosis of malignant cells
through regulating intracellular Ca2+ signaling
(14–16). It has been demonstrated that
changes in the expression of TRP channels can regulate tumor cell
proliferation and their sensitivity to chemotherapy, suggesting
roles of TRP channels in malignancy-promoting effects and
resistance to antitumor chemotherapy (17). Moreover, TRP channels have been
reported to be linked to overall survival and progression of
various hematological malignancies, including leukemia and lymphoma
(18). During recent years, there
has been an increased interest in medical research into the
association between TRP channels and MM, leading to the discovery
of a variety of roles and functions of TRP channels in MM
tumorigenesis and progression, dissemination and metastasis,
MM-related osteolytic bone disease, and chemotherapy resistance
(5). In this review, we summarize
the evidence of the connections between TRP channels and MM
(Table I).
 | Table I.Role of TRP channels in MM. |
Table I.
Role of TRP channels in MM.
| TRP | Function and role
in MM | (Refs.) |
|---|
| TRPV1 | Promotes MM cell
survival via acid sensation | (34) |
|
| TRPV1 inhibition
synergizes with bortezomib in chemotherapy | (45) |
| TRPV2 | Upregulated in MM
and is associated with poor prognosis | (25–29) |
|
| Activates
osteoclasts and promotes lytic bone disease | (27) |
| TRPV4 | Triggers
osteoclastic activity | (46,47) |
| TRPM7 | Promotes MM
metastasis and dissemination | (38) |
| TRPM8 | Highly expressed in
MM | (42) |
| TRPA1 | TRPA1 inhibition
attenuates bortezomib-induced neuropathy | (66,67) |
| TRPC1 | Mediates the
anti-MM effects of MTI-101 | (59,61) |
TRP channels in the progression of multiple
myeloma (MM)
MM is a plasma cell malignancy characterized by
uncontrolled proliferation of plasma cell clones (19). It is broadly accepted that the
tumorigenesis of MM is primarily linked to multiple genetic
aberrations, including chromosome abnormalities, translocations,
copy number variations, and somatic mutations, which alter several
cellular processes and molecular pathways (19). These alterations that subsequently
lead to neoplastic transformation and progression involve abnormal
intracellular calcium signaling and altered expression of many
calcium channels, including TRP channels (5,18,20,21).
TRPV2 predicts the survival of
patients with MM
TRPV2 is a nonspecific cation channel which is a
member of the TRP vanilloid subfamily (22). TRPV2 can be activated by noxious
temperatures greater than 52°C and plays an important role in
cellular functions including cell proliferation and apoptosis
(23,24). Previous studies demonstrated that
TRPV2 was overexpressed in MM cell lines as well as in myeloma
samples from patients with MM and that TRPV2 was one of the two
most significantly upregulated genes in the 17p11.2-p12 region that
is an unstable chromosomal region and amplified in primary MM
tumors (25). The overexpression
of TRPV2 might be associated with the abnormal monoclonal
proliferation of MM tumor cells (26). Bai et al (27) confirmed that TRPV2 was highly
expressed in patients with MM and found that MM patients with
higher transcriptional levels of TRPV2 had shorter overall survival
rates than patients with lower TRPV2 expression levels, indicating
that TRPV2 overexpression is associated with poor prognosis in
patients with MM. These results suggest that TRPV2 may serve as a
marker of MM, and TRPV2 seemingly plays a detrimental role in MM
progression (Fig. 1). Then,
another research group found that tumor cells from patients with MM
could be divided into two subpopulations,
CD138+/TRPV2+ and
CD138+/TRPV2− tumor cells, with distinct
phenotypes, and that cannabidiol, a TRPV2 agonist, decreased
proliferation of CD138+/TRPV2+ cells
(28). Moreover, activation of
TRPV2 with its agonists significantly decreased MM cell viability
and inhibited MM cell proliferation without affecting apoptosis
likely though regulating intracellular free calcium levels
(27,29). These results seem to conflict with
previous findings. A reasonable explanation is that overexpression
of TRPV2 might serve as a compensatory response to the development
and progression of MM. Nevertheless, these findings suggest that
overexpression of TRPV2 may become a biomarker of MM and that TRPV2
may become a potential therapeutic target for the treatment of MM
(24).
TRPV1 promotes MM cell survival via
acid sensation
It is well known that an acidic tumor
microenvironment is a driving force promoting cancer development
and progression by activating tumor cell proliferation and survival
signals (30). TRPV1, a member of
the TRP vanilloid subfamily, is a non-selective cation channel that
serves as a sensor of noxious heat with temperature greater than
43°C (31). TRPV1 can also be
activated by a wide variety of endogenous physical and chemical
stimuli, including acidic conditions with pH values lower than 5.9
(31). Myeloma cells stimulate and
activate osteoclasts to produce numerous protons to form an acidic
tumor microenvironment, in which the pH values are usually below
5.5 (32,33). It has been reported that the TRPV1
channel on MM cells is activated in the MM acidic microenvironment,
which subsequently activates PI3K/Akt survival signaling and
further increases the expression of TRPV1 in MM cells to enhance
acid sensation (34). The PI3K/Akt
pathway was found to be aberrantly activated in myeloma cells from
patients with MM and to play a crucial role in survival and
chemotherapy resistance of myeloma cells (34,35).
This positive feedback loop between upregulation of TRPV1 as an
acid sensor and activation of the PI3K/Akt pathway forms a vicious
cycle that could contribute to myeloma progression (Fig. 1).
TRPM7 promotes MM metastasis
MM arises from the bone marrow and then continuously
spreads or disseminates to multiple sites throughout the body
(36). Although the molecular
mechanisms of the metastasis process are not fully understood,
intracellular Ca2+ signaling is believed to play an
important role in tumor cell motility and migration (37). It has been shown that TRPM7 is
significantly upregulated in myeloma cells compared with normal
plasma cells and that knockout or inhibition of TRPM7 inhibits MM
cell migration and dissemination (38). These findings suggest that TRPM7 is
a critical regulator of MM cell motility and dissemination and
could become a therapeutic target for the prevention and/or
treatment of metastatic MM (Fig.
1).
TRPM8 may become a marker of MM
TRPM8 serves as a receptor of cool temperature below
27°C and menthol and is the primary molecular transducer of
non-noxious cool somatosensation in humans (39). TRPM8 is upregulated in a variety of
malignant tumors such as prostate cancer (40,41).
Hirai et al (42) reported
that TRPM8 is highly expressed in myeloma cells compared with
normal plasma cells. It has also been reported that TRPM8
contributes to proliferation, survival, and invasion of cancer
cells and that overexpression of TRPM8 is associated with tumor
progression. However, the role of TRPM8 in the progression of MM
warrants further investigation (40).
TRP channels in the bone destruction of
MM
Osteolytic bone disease is a hallmark and a frequent
complication of MM. Up to 80% of patients with MM have osteolytic
bone lesions, leading to a significant cause of morbidity and
mortality (43). Under
physiological conditions, there is a balance between bone formation
and resorption, which are mediated by osteoblastic and osteoclastic
activity, respectively. Enhanced osteoclastic activity is
considered as the culprit in the development of osteolytic bone
lesions in patients with MM (44).
Intracellular Ca2+ is an important second messenger that
regulates the activity of both osteoblasts and osteoclasts.
TRPV4 triggers osteoclastic
activity
Members of the TRP vanilloid subfamily, especially
TRPV1, TRPV2, TRPV4, and TRPV5, have been identified to contribute
to intracellular Ca2+ signaling in bone cells and bone
homeostasis (45). For example,
TRPV4-mediated Ca2+ influx is required for osteoclast
differentiation by triggering nuclear factor of activated T-cells
cytoplasmic 1 (NFATC1)-dependent gene expression (46). Moreover, knockout of TRPV4 or TRPV1
increased bone mass in a mouse model (47). Therefore, antagonizing TRPV4 may
become a novel strategy to prevent or treat MM-associated bone
destruction.
TRPV2 activates osteoclasts
Activation of the receptor activator of nuclear
factor-κB ligand (RANKL)/RANK signaling pathway plays a crucial
role in osteoclast differentiation and activation, leading to
accelerated bone resorption and lytic bone lesions (48). It has been reported that
TRPV2-mediated Ca2+ influx promotes osteoclastic
differentiation and activation by modulating calcineurin-NFAT
activity and the release of RANKL and that blocking Ca2+
entry attenuates MM-induced osteoclast formation (27). These findings suggest that blocking
the TRPV2 channel may provide a promising therapeutic strategy for
osteolytic bone disease in patients with MM.
TRP channels in the chemotherapy of MM
Chemotherapy for MM is performed utilizing
medications with different mechanisms of action, including
alkylating agents, proteasome inhibitors, histone deacetylase
inhibitors, and monoclonal antibodies (49–51).
Although the survival outcomes of patients with MM have improved
substantially due to advances in chemotherapy, myelomas frequently
relapse or become refractory to chemotherapy mostly due to drug
resistance, which serves as a major hurdle towards improving the
long-term outcomes of patients with MM (52). Chemotherapy-induced tumor cell
apoptosis and necrosis are closely regulated by cytoplasmic and
mitochondrial calcium signaling (53). Evidence shows that aberrant calcium
circularity and abnormal expression of calcium channels are
involved in the drug resistance of MM (54).
TRPV1 inhibition synergizes with
bortezomib
The proteasome which degrades ubiquitylated abnormal
or misfolded proteins contributes to maintenance of the immortal
phenotype of myeloma cells (55).
Bortezomib, a proteasome inhibitor, is used to treat MM by inducing
accumulation of misfolded proteins and pro-apoptotic factors, which
triggers apoptosis of myeloma cells (56). However, bortezomib-induced unfolded
protein response can increase expression of chaperons such as
HSP70, which restores the folding capacity, promotes cellular
survival, and subsequently reduces the responsiveness and induces
resistance to bortezomib (57).
TRPV1 is a calcium-permeable channel expressed in the cytoplasmic
and mitochondrial membrane, and activation of TRPV1 with capsaicin
upregulates HSP70 (58). Beider
et al (45) found that
inhibition of TRPV1 with AMG9810 disturbed mitochondrial calcium
signaling, abolished bortezomib-induced mitochondrial HSP70
accumulation and synergistically induced myeloma cell apoptosis
with bortezomib. They also found that bortezomib plus the TRPV1
antagonist AMG9810 effectively reduced MM tumor burden in a mouse
model (45). Thus, TRPV1
inhibition could be used to increase the sensitivity of bortezomib
in treating MM.
TRPV2 activation synergizes with
bortezomib
Similar to TRPV1, targeting TRPV2 also shows
synergism with bortezomib in treating MM. Morelli et al
demonstrated that activation of TRPV2 with cannabidiol
synergistically inhibited myeloma cell growth and induced myeloma
cell death in combination with bortezomib through suppressing
extracellular-regulated kinase, serine/threonine protein kinase B,
and nuclear factor κB (28). In
addition, the therapeutic effects of cannabidiol were only present
in TRPV2+/+ myeloma cells but not in TRPV2−/−
tumor cells (28). These findings
suggest that TRPV2 agonists could be used to enhance the
responsiveness of MM patients to bortezomib treatment.
TRPC1 determines the responsiveness to
MTI-101
MTI-101, a cyclic beta-hairpin peptide, has been
developed to treat patients with MM through binding to a
CD44/integrin α4β1-containing complex and provoking myeloma cell
necrosis. The mechanisms underlying the therapeutic effects of
MTI-101 include inducing robust calcium influx, increasing levels
of reactive oxygen species, and depolarizing the mitochondrial
membrane potential, all of which are hallmarks of necrotic cell
death. It has been reported that MTI-101-induced cell death is
largely due to mitochondrial calcium overload through components of
store-operated calcium channels (SOCs) such as TRPC1, as knockdown
of TRPC1 was found to abolish MTI-101-induced necrosis (59). TRPC1 is the first identified
mammalian TRP channel and is considered as a component of SOCs
along with Orai1 and STIM1 (60).
Treatment with MTI-101 remodels calcium homeostasis and circuitry,
and resistance to MTI-101 is associated with downregulation of
TRPC1 and TRPM7 and upregulation of TRPM6 and TRPM8 in MM cells
(59). Further studies have
demonstrated that MTI-101 induced TRPC1 translocating to the
cytoplasmic membrane and forming a complex with STIM1 and that
TRPC1, TRPC4, and TRPC5 were required for MTI-101-induced calcium
influx and cell death (61).
Importantly, the expression levels of SOC components other than
TRPC channels in myelomas were identified as poor prognostic
indicators in patients with MM (61). These findings suggest that the
expression profile of TRPC1 may be a determinant of responsiveness
to MTI-101 in MM (Fig. 1).
TRPA1 serves as a therapeutic target
for bortezomib-induced peripheral neuropathy
As mentioned above, bortezomib is broadly used to
treat patients with MM. In addition to drug resistance,
bortezomib-induced painful peripheral neuropathy significantly
limits its clinical use (62).
Although the underlying mechanisms of bortezomib-induced peripheral
neuropathy are not fully understood, neurophysiological
abnormalities in dorsal root ganglia (DRG) and nociceptive Aδ/C
peripheral nerve fibers are believed to contribute to mechanical
allodynia caused by bortezomib treatment (63). TRPA1, the only member in the TRPA
subfamily, contains 14 N-terminal ankyrin repeats and is expressed
primarily in DRG and Aδ and C fibers (64). Activated by cold temperature and
other chemical and physical stimuli, TRPA1 functions as a
mechanical and chemical stress sensor that conveys pain sensation
to the brain (65). It was
demonstrated that the expression level of TRPA1 was significantly
increased in DRG of rats treated with bortezomib, suggesting that
this upregulation might contribute to bortezomib-induced peripheral
neuropathy and neuropathic pain (66). Moreover, blocking TRPA1 ameliorated
bortezomib-elicited mechanical pain and cold sensitivity in rats
(66). Further study demonstrated
that interleukin-6 (IL-6) was responsible for bortezomib-induced
TRPA1 upregulation and that blocking the IL-6 signaling reduced
TRPA1 expression and attenuated mechanical hyperalgesia and cold
hypersensitivity in rats treated with bortezomib (67). These findings suggest that TRPA1
may become a therapeutic target for bortezomib-induced painful
peripheral neuropathy in patients with MM.
Conclusion
TRP channels connect tumor microenvironment stimuli
to intracellular calcium signaling and play crucial roles in
various behaviors of cancer cells. In this review, we summarize the
currently available evidence showing the roles of TRP channels in
many aspects of MM, including tumor progression, dissemination,
bone destruction, and drug resistance. This is an emerging field,
and there are still a lot of unknown questions regarding the role
of TRP channels in the development and progression of MM. It is
challenging to treat MM by targeting TRP channels. As discussed,
activation of TRPV2 was found to improve the sensitivity of myeloma
cells to chemotherapy but may exacerbate MM-related bone disease by
stimulating osteoclasts. Therefore, selectively targeting TRP
channels in myeloma cells or osteoclasts may be required to
delivery optimal treatment. Many previous studies in this topic
were performed in cultured cells and animal models; therefore, the
clinical significance of the role of TRP channels in MM is not well
documented. Especially, the role of TRPV1, TRPV2, TRPV4, TRPC1, and
TRPM7 in MM should be evaluated in the clinical setting. Future
studies may identify certain TRP channels as markers or therapeutic
targets for predicting prognosis, preventing disease progression,
and improving drug responsiveness of MM. Further understanding of
the role of TRP channels in MM may benefit the survival and
long-term outcome of patients with MM.
Acknowledgements
Not applicable.
Funding
This work was supported by grants from the National Key R&D
Program of China (2018YFC0116901 and 2018YFC1315604), the Science
and Technology Development Project of Jilin Province
(20180101124JC), the Special Project for Health Research of Jilin
Province (2018SCZ031 and 2019SCZ055), and the Health Technology
Innovation Project of Jilin Province (3D517ED43430).
Availability of data and materials
Data sharing is not applicable to this article, as
no datasets were generated or analyzed during the current
study.
Authors' contributions
Conceptualization of the review concept and
manuscript drafting were conducted by LM. Literature review and
manuscript revision were carried out by GG. Conceptualization of
the review concept, supervision, and manuscript revision were
conducted by LB. Data authentication is not applicable. All authors
read and approved the final version of the manuscript for
publication.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
MM
|
multiple myeloma
|
|
TRP
|
transient receptor potential
|
|
SOCE
|
store-operated calcium entry
|
|
Orai1
|
calcium release-activated calcium
modulator 1
|
|
STIM1
|
stromal interaction molecule 1
|
|
NFATC1
|
nuclear factor of activated T-cells
cytoplasmic 1
|
|
RANKL
|
receptor activator of nuclear
factor-κB ligand
|
|
SOCs
|
store-operated calcium channels
|
|
DRG
|
dorsal root ganglia
|
References
|
1
|
van de Donk N, Pawlyn C and Yong KL:
Multiple myeloma. Lancet. 397:410–427. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ghandili S, Weisel KC, Bokemeyer C and
Leypoldt LB: Current treatment approaches to newly diagnosed
multiple myeloma. Oncol Res Treat. 44:690–699. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kazandjian D: Multiple myeloma
epidemiology and survival: A unique malignancy. Semin Oncol.
43:676–681. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Costa LJ and Usmani SZ: Defining and
managing high-risk multiple myeloma: Current concepts. J Natl Compr
Canc Netw. 18:1730–1737. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Li T, Chen J and Zeng Z:
Pathophysiological role of calcium channels and transporters in the
multiple myeloma. Cell Commun Signal. 19:992021. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Stewart TA, Yapa KT and Monteith GR:
Altered calcium signaling in cancer cells. Biochim Biophys Acta.
1848:2502–2511. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Deliot N and Constantin B: Plasma membrane
calcium channels in cancer: Alterations and consequences for cell
proliferation and migration. Biochim Biophys Acta. 1848:2512–2522.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nilius B, Owsianik G, Voets T and Peters
JA: Transient receptor potential cation channels in disease.
Physiol Rev. 87:165–217. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ferrandiz-Huertas C, Mathivanan S, Wolf
CJ, Devesa I and Ferrer-Montiel A: Trafficking of ThermoTRP
channels. Membranes (Basel). 4:525–564. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kim M, Sisco NJ, Hilton JK, Montano CM,
Castro MA, Cherry BR, Levitus M and Horn WD: Evidence that the
TRPV1 S1-S4 membrane domain contributes to thermosensing. Nat
Commun. 11:41692020. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gorbunov AS, Maslov LN, Jaggi AS, Singh N,
Petrocellis LD, Boshchenko AA, Roohbakhsh A, Bezuglov VV and
Oeltgen PR: Physiological and pathological role of TRPV1, TRPV2 and
TRPV4 channels in heart. Curr Cardiol Rev. 15:244–251. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Vay L, Gu C and McNaughton PA: The
thermo-TRP ion channel family: Properties and therapeutic
implications. Br J Pharmacol. 165:787–801. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ambudkar IS, de Souza LB and Ong HL:
TRPC1, orai1, and STIM1 in SOCE: Friends in tight spaces. Cell
Calcium. 63:33–39. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Santoni G and Farfariello V: TRP channels
and cancer: new targets for diagnosis and chemotherapy. Endocr
Metab Immune Disord Drug Targets. 11:54–67. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Canales J, Morales D, Blanco C, Rivas J,
Díaz N, Angelopoulos I and Cerda O: A TR(i)P to cell migration: New
roles of TRP channels in mechanotransduction and cancer. Front
Physiol. 10:7572019. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Prevarskaya N, Zhang L and Barritt G: TRP
channels in cancer. Biochim Biophys Acta. 1772:937–946. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Santoni G, Maggi F, Morelli MB, Santoni M
and Marinelli O: Transient receptor potential cation channels in
cancer therapy. Med Sci (Basel). 7:1082019.PubMed/NCBI
|
|
18
|
Maggi F, Morelli MB, Nabissi M, Marinelli
O, Zeppa L, Aguzzi C, Santoni G and Amantini C: Transient receptor
potential (TRP) channels in haematological malignancies: An update.
Biomolecules. 11:7652021. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Heider M, Nickel K, Hogner M and
Bassermann F: Multiple myeloma: Molecular pathogenesis and disease
evolution. Oncol Res Treat. 44:672–681. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hodeify R, Yu F, Courjaret R, Nader N, Dib
M, Sun L, Adap E, Hubrack S and Machaca K: Regulation and Role of
Store-Operated Ca(2+) Entry in Cellular Proliferation. In: Calcium
Entry Channels in Non-Excitable Cells. Kozak JA and Putney JW Jr:
CRC Press/Taylor & Francis; Boca Raton, FL: pp. 215–240. 2018,
PubMed/NCBI
|
|
21
|
Karki T and Tojkander S: TRPV protein
family-from mechanosensing to cancer invasion. Biomolecules.
11:10192021. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kojima I and Nagasawa M: Trpv2. Handb Exp
Pharmacol. 222:247–272. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Liberati S, Morelli MB, Amantini C,
Santoni M, Nabissi M, Cardinali C and Santoni G: Advances in
transient receptor potential vanilloid-2 channel expression and
function in tumor growth and progression. Curr Protein Pept Sci.
15:732–737. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Siveen KS, Nizamuddin PB, Uddin S,
Al-Thani M, Frenneaux MP, Janahi IA, Steinhoff M and Azizi F:
TRPV2: A cancer biomarker and potential therapeutic target. Dis
Markers. 2020:88923122020. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Fabris S, Todoerti K, Mosca L, Agnelli L,
Intini D, Lionetti M, Guerneri S, Lambertenghi-Deliliers G, Bertoni
F and Neri A: Molecular and transcriptional characterization of the
novel 17p11.2-p12 amplicon in multiple myeloma. Genes Chromosomes
Cancer. 46:1109–1118. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Liberati S, Morelli MB, Amantini C,
Farfariello V, Santoni M, Conti A, Nabissi M, Cascinu S and Santoni
G: Loss of TRPV2 homeostatic control of cell proliferation drives
tumor progression. Cells. 3:112–128. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Bai H, Zhu H, Yan Q, Shen X, Lu X, Wang J,
Li J and Chen L: TRPV2-induced Ca(2+)-calcineurin-NFAT signaling
regulates differentiation of osteoclast in multiple myeloma. Cell
Commun Signal. 16:682018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Morelli MB, Offidani M, Alesiani F,
Discepoli G, Liberati S, Olivieri A, Santoni M, Santoni G, Leoni P
and Nabissi M: The effects of cannabidiol and its synergism with
bortezomib in multiple myeloma cell lines. A role for transient
receptor potential vanilloid type-2. Int J Cancer. 134:2534–2546.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Nabissi M, Offidani M, Morelli MB,
Pettinari M, Caraffa P, Gentili S, Corvatta L, Santoni G, Alesiani
F and Leoni P: TRPV2 expression and its role in proliferation of
human multiple myeloma cell lines. Blood. 118:50032011. View Article : Google Scholar
|
|
30
|
Boedtkjer E and Pedersen SF: The acidic
tumor microenvironment as a driver of cancer. Annu Rev Physiol.
82:103–126. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Caterina MJ, Schumacher MA, Tominaga M,
Rosen TA, Levine JD and Julius D: The capsaicin receptor: A
heat-activated ion channel in the pain pathway. Nature.
389:816–824. 1997. View
Article : Google Scholar : PubMed/NCBI
|
|
32
|
Swietach P, Vaughan-Jones RD, Harris AL
and Hulikova A: The chemistry, physiology and pathology of pH in
cancer. Philos Trans R Soc Lond B Biol Sci. 369:201300992014.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Gastelum G, Veena M, Lyons K, Lamb C,
Jacobs N, Yamada A, Baibussinov A, Sarafyan M, Shamis R, Kraut J
and Frost P: Can targeting hypoxia-mediated acidification of the
bone marrow microenvironment kill myeloma tumor cells? Front Oncol.
11:7038782021. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Amachi R, Hiasa M, Teramachi J, Harada T,
Oda A, Nakamura S, Hanson D, Watanabe K, Fujii S, Miki H, et al: A
vicious cycle between acid sensing and survival signaling in
myeloma cells: acid-induced epigenetic alteration. Oncotarget.
7:70447–70461. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Ramakrishnan V and Kumar S: PI3K/AKT/mTOR
pathway in multiple myeloma: From basic biology to clinical
promise. Leuk Lymphoma. 59:2524–2534. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Ghobrial IM: Myeloma as a model for the
process of metastasis: Implications for therapy. Blood. 120:20–30.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
White C: The regulation of tumor cell
invasion and metastasis by endoplasmic reticulum-to-mitochondrial
Ca(2+) transfer. Front Oncol. 7:1712017. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Samart P, Luanpitpong S, Rojanasakul Y and
Issaragrisil S: O-GlcNAcylation homeostasis controlled by calcium
influx channels regulates multiple myeloma dissemination. J Exp
Clin Cancer Res. 40:1002021. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Pina R, Ugarte G, Campos M,
Íñigo-Portugués A, Olivares E, Orio P, Belmonte C, Bacigalupo J and
Madrid R: Role of TRPM8 channels in altered cold sensitivity of
corneal primary sensory neurons induced by axonal damage. J
Neurosci. 39:8177–8192. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Yee NS: Roles of TRPM8 ion channels in
cancer: Proliferation, survival, and invasion. Cancers (Basel).
7:2134–2146. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Bidaux G, Flourakis M, Thebault S, Zholos
A, Beck B, Gkika D, Roudbaraki M, Bonnal JL, Mauroy B, Shuba Y, et
al: Prostate cell differentiation status determines transient
receptor potential melastatin member 8 channel subcellular
localization and function. J Clin Invest. 117:1647–1657. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Hirai A, Aung NY, Ohe R, Nishida A, Kato
T, Meng H, Ishizawa K, Fujii J and Yamakawa M: Expression of TRPM8
in human reactive lymphoid tissues and mature B-cell neoplasms.
Oncol Lett. 16:5930–5938. 2018.PubMed/NCBI
|
|
43
|
Terpos E, Morgan G, Dimopoulos MA, Drake
MT, Lentzsch S, Raje N, Sezer O, García-Sanz R, Shimizu K, Turesson
I, et al: International myeloma working group recommendations for
the treatment of multiple myeloma-related bone disease. J Clin
Oncol. 31:2347–2357. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Terpos E, Ntanasis-Stathopoulos I,
Gavriatopoulou M and Dimopoulos MA: Pathogenesis of bone disease in
multiple myeloma: From bench to bedside. Blood Cancer J. 8:72018.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Beider K, Rosenberg E, Dimenshtein-Voevoda
V, Sirovsky Y, Vladimirsky J, Magen H, Ostrovsky O, Shimoni A,
Bromberg Z, Weiss L, et al: Blocking of transient receptor
potential vanilloid 1 (TRPV1) promotes terminal mitophagy in
multiple myeloma, disturbing calcium homeostasis and targeting
ubiquitin pathway and bortezomib-induced unfolded protein response.
J Hematol Oncol. 13:1582020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Masuyama R, Vriens J, Voets T, Karashima
Y, Owsianik G, Vennekens R, Lieben L, Torrekens S, Moermans K,
Bosch AV, et al: TRPV4-mediated calcium influx regulates terminal
differentiation of osteoclasts. Cell Metab. 8:257–265. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Nishimura H, Kawasaki M, Tsukamoto M,
Menuki K, Suzuki H, Matsuura T, Baba K, Motojima Y, Fujitani T,
Ohnishi H, et al: Transient receptor potential vanilloid 1 and 4
double knockout leads to increased bone mass in mice. Bone Rep.
12:1002682020. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Raje NS, Bhatta S and Terpos E: Role of
the RANK/RANKL pathway in multiple myeloma. Clin Cancer Res.
25:12–20. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Pinto V, Bergantim R, Caires HR, Seca H,
Guimarães JE and Vasconcelos MH: Multiple myeloma: Available
therapies and causes of drug resistance. Cancers (Basel).
12:4072020. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Painuly U, Ramakrishnan V, Kimlinger T,
Wellik L, Haug J, Gonsalves W, Bi L, Huang Z, Rajkumar SV and Kumar
S: Aurora kinase and FGFR3 inhibition results in significant
apoptosis in molecular subgroups of multiple myeloma. Oncotarget.
9:34582–34594. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Ramakrishnan V, Gomez M, Prasad V,
Kimlinger T, Painuly U, Mukhopadhyay B, Haug J, Bi L, Rajkumar SV
and Kumar S: Smac mimetic LCL161 overcomes protective ER stress
induced by obatoclax, synergistically causing cell death in
multiple myeloma. Oncotarget. 7:56253–56265. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Robak P, Drozdz I, Szemraj J and Robak T:
Drug resistance in multiple myeloma. Cancer Treat Rev. 70:199–208.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Kerkhofs M, Bittremieux M, Morciano G,
Giorgi C, Pinton P, Parys JB and Bultynck G: Emerging molecular
mechanisms in chemotherapy: Ca(2+) signaling at the
mitochondria-associated endoplasmic reticulum membranes. Cell Death
Dis. 9:3342018. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Liu M, Wang Y, Miettinen JJ, Kumari R,
Majumder MM, Tierney C, Bazou D, Parsons A, Suvela M, Lievonen J,
et al: S100 calcium binding protein family members associate with
poor patient outcome and response to proteasome inhibition in
multiple myeloma. Front Cell Dev Biol. 9:7230162021. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Ito S: Proteasome inhibitors for the
treatment of multiple myeloma. Cancers (Basel). 12:2652020.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Robak P, Szemraj J, Mikulski D, Drozdz I,
Juszczak K, Jarych D, Misiewicz M, Kościelny K, Fendler W and Robak
T: Prognostic value of resistance proteins in plasma cells from
multiple myeloma patients treated with bortezomib-based regimens. J
Clin Med. 10:50282021. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Zaal EA, Wu W, Jansen G, Zweegman S, Cloos
J and Berkers CR: Bortezomib resistance in multiple myeloma is
associated with increased serine synthesis. Cancer Metab. 5:72017.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Bromberg Z, Goloubinoff P, Saidi Y and
Weiss YG: The membrane-associated transient receptor potential
vanilloid channel is the central heat shock receptor controlling
the cellular heat shock response in epithelial cells. PLoS One.
8:e571492013. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Emmons MF, Anreddy N, Cuevas J,
Steinberger K, Yang S, McLaughlin M, Silva A and Hazlehurst LA:
MTI-101 treatment inducing activation of Stim1 and TRPC1 expression
is a determinant of response in multiple myeloma. Sci Rep.
7:26852017. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Xu SZ and Beech DJ: TrpC1 is a
membrane-spanning subunit of store-operated Ca(2+) channels in
native vascular smooth muscle cells. Circ Res. 88:84–87. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Elzamzamy OM, Johnson BE, Chen WC, Hu G,
Penner R and Hazlehurst LA: Transient receptor potential C 1/4/5 is
a determinant of MTI-101 induced calcium influx and cell death in
multiple myeloma. Cells. 10:14902021. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Carozzi VA, Renn CL, Bardini M, Fazio G,
Chiorazzi A, Meregalli C, Oggioni N, Shanks K, Quartu M, Serra MP,
et al: Bortezomib-induced painful peripheral neuropathy: An
electrophysiological, behavioral, morphological and mechanistic
study in the mouse. PLoS One. 8:e729952013. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Argyriou AA, Iconomou G and Kalofonos HP:
Bortezomib-induced peripheral neuropathy in multiple myeloma: A
comprehensive review of the literature. Blood. 112:1593–1599. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Hu F, Song X and Long D: Transient
receptor potential ankyrin 1 and calcium: Interactions and
association with disease (Review). Exp Ther Med. 22:14622021.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Nilius B, Appendino G and Owsianik G: The
transient receptor potential channel TRPA1: From gene to
pathophysiology. Pflugers Arch. 464:425–458. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Wang Q, Wang J, Gao D and Li J: Inhibition
of PAR2 and TRPA1 signals alleviates neuropathic pain evoked by
chemotherapeutic bortezomib. J Biol Regul Homeost Agents.
31:977–983. 2017.PubMed/NCBI
|
|
67
|
Liu D, Sun M, Xu D, Ma X, Gao D and Yu H:
Inhibition of TRPA1 and IL-6 signal alleviates neuropathic pain
following chemotherapeutic bortezomib. Physiol Res. 68:845–855.
2019. View Article : Google Scholar : PubMed/NCBI
|