Introduction
Predicting oncological behavior is important when
deciding between a surgical plan, aggressive surveillance and
aggressive adjuvant or neoadjuvant therapy (1). The 8th edition of the
tumor-node-metastasis (TNM) classification for non-small cell lung
cancer (NSCLC) is used worldwide (2). Computed tomography (CT) is used to
define the clinical T category of NSCLC (2). Numerous radiological observations
using CT have been reported to predict the prognosis of NSCLC,
including whole tumor size (WTS), consolidation size (CS),
consolidation-to-tumor ratio (CTR), tumor disappearance ratio
(TDR), tumor diameter in the mediastinal window (MD) and presence
of ground-glass opacity (GGO). Parameters were defined as follows.
WTS, whole tumor size on lung window setting; CS, consolidation
size on lung window setting, MD, diameter on mediastinal window
setting; CTR, CS/WTS; and TDR (%), 100 × (1-(MD/WTS)). In the 8th
edition of the TNM classification, clinical T category is assigned
based on CS assessed using high resolution CT (2). In 2019, Kim et al (3) reported that CTR and TDR are not
independently associated with long-term prognosis of NSCLC compared
with clinical T category using CS. The presence of GGO on CT has
been reported to indicate good prognosis in both clinical and
pathological T1N0-staged NSCLC (4–6).
However, the best prognostic radiological tools for solid nodules
without GGO in the early stage remain unknown.
A previous randomized clinical trial demonstrated
that positron emission tomography-CT (PET-CT) contributes to the
preoperative staging of NSCLC and decreases the number of futile
surgeries (7). The National
Comprehensive Cancer Network and Japanese Lung Cancer Society
Guideline recommend the use of 18F-fluorodeoxyglucose (FDG)-PET-CT
determine the presence of distant metastases requiring surveillance
(1,8). Previous studies have reported the
usefulness of maximal standardized uptake (SUVmax) value using
PET-CT (calculated based on the maximum activity of the volume of
the dose of FDG injected and patient weight), associated with
primary tumors for assessing the risk of occult lymph node
metastasis (LNM) using numerous cut-off values (9–11).
Despite previous studies on tumor morphology using
high-resolution CT (HRCT) and tumor metabolism using PET-CT have
been reported, the success of prediction of LNM based on the
combination of morphology and metabolism using these radiological
tools is not known to clinicians (4–6,10–12).
Therefore, in the present study, predictive radiological tools
(chest HRCT and PET-CT) for occult LNM in patients with clinical
stage I NSCLC were evaluated.
Materials and methods
Patients
The clinicopathological data of 420 patients who
underwent lobectomy for clinical stage I NSCLC at The Jikei
University School of Medicine (Tokyo, Japan) between July 2014 and
November 2021 were retrospectively reviewed. All enrolled patients
were evaluated using tumor markers, chest and abdominal CT, brain
magnetic resonance imaging or CT and PET-CT before surgery. The
present study was performed in accordance with The Declaration of
Helsinki. The data were retrospectively collected, registered in a
database and approved by the Review Board of The Jikei University
School of Medicine [approval number: 30-359(9380)].
Data collection
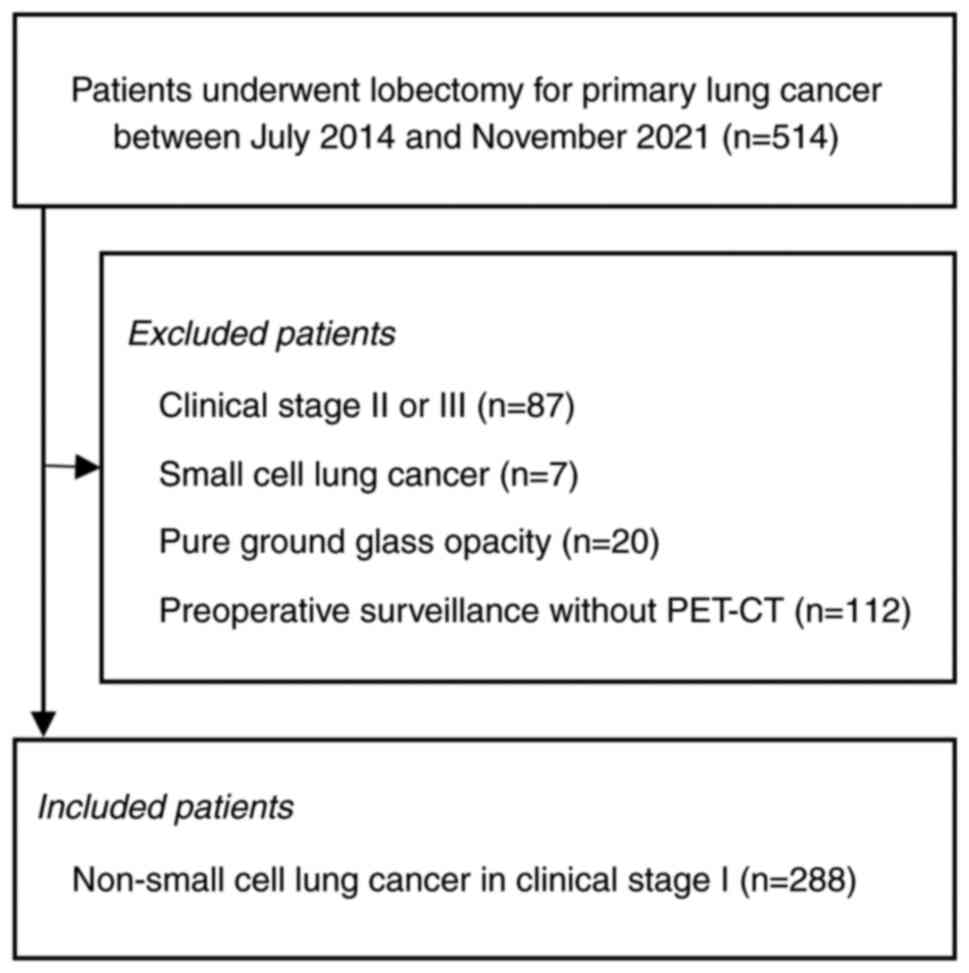
During the study period, 514 patients underwent
lobectomy at The Jikei University School of Medicine for primary
lung cancer, of whom 288 patients met the inclusion criteria
(Fig. 1). The median age of the
patients was 70 years (range, 31–87 years) and there were 189 males
and 99 females. The following patient characteristics were
collected: Age, sex, smoking index, body mass index, Charlson
Comorbidity Index score calculated based on comorbid conditions and
preoperative spirometry test, including vital capacity and forced
vital capacity. Carcinoembryonic antigen and cytokeratin 19
fragment were evaluated as tumor markers in preoperative blood
tests within 2 months before surgery. WTS and CS in the lung window
setting were observed on CT. CTR was calculated as CS/WTS and
tumors were classified as a pure solid tumor (CTR=1), part solid
tumor (CTR<1) or pure GGO (CTR=0). For convenience in
classifying tumors according to CTR, the definition of pure solid
tumors included tumors with minor GGO components outside of the CTR
measurement site. All patients underwent PET-CT based on glycemic
control. SUVmax was evaluated using PET-CT. A surgical plan for
each patient was decided by preoperative conference. Mediastinal
lymph node (LN) dissection was evaluated in terms of surgical
parameters [nodal dissection (ND) level 1/2a-1/2a-2); level of
mediastinal LN dissection was determined at a preoperative
conference (13). Patients with
multiple comorbidities were omitted from mediastinal LN dissection.
Mediastinal LN sampling was included in LN dissection status ND1.
The total number of excised LNs was counted. Pathological
parameters included histological type (adenocarcinoma, squamous
cell carcinoma or other), pathological whole size, invasive size,
lympho-vascular and pleural invasion and LNM. Histological
assessment was performed according to the 8th edition of the TNM
classification (2). The
involvement of LN was assessed as a short diameter (>10 mm on
CT), focally increased FDG uptake compared with normal background
uptake or SUVmax >2.5 on PET. Endobronchial ultrasound-guided
transbronchial needle aspiration (EBUS-TBNA) was performed for
suspected LNM during preoperative surveillance.
The exclusion criteria were as follows: Patients
with clinical stage II or III, SCLC, benign tumors, pure GGO on CT,
preoperative surveillance without PET-CT and incomplete data.
Statistical analysis
Statistical analysis was performed using SPSS
version 21.0 software (IBM Corp.). P<0.05 was considered to
indicate a statistically significant difference. Data are presented
as median and interquartile range or mean ± standard deviation.
Quantitative continuous variables were compared using Student's
t-test for the mean and Mann-Whitney U test for the median.
Fisher's exact and χ2 test were used to compare
categorical variables. Parameters with P<0.05 in the univariate
analysis were selected for inclusion in multivariate logistic
regression analysis.
Multivariable parameters between LNM and non-LNM
groups in the whole cohort were compared. The optimal cut-off value
for predictive radiological tools for LNM was assessed according to
the area under the receiver operating characteristic (ROC)
curve.
Results
Patient characteristics
There were 175 patients (60.8%) with pure solid
tumors. In total, 39 (13.5%) patients were diagnosed with
pathological LNM, of which 38 (97.4%) were pure solid tumors.
EBUS-TBNA was performed on one patient with combined background
pulmonary fibrosis and emphysema. The lower paratracheal LN with
SUVmax of 5.7 was negative on EBUS and positive on postoperative
pathology with false negative.
Comparison of multivariable parameters
between LNM and non-LNM groups
Larger WTS (P<0.05) and CS (P<0.001), pure
solid tumor (P<0.05), higher SUVmax (P<0.001), histological
type (P<0.05), pathological whole (P<0.05) and invasive size
(P<0.001) and lympho-vascular (P<0.001) and pleural invasion
(P<0.001) were significantly associated with LNM (Table I). According to the respective
minimum values of CS and SUVmax, CS of 10 mm and SUVmax of 0.8 were
associated with LNM.
 | Table I.Comparison of pathological patients
with non-LNM and LNM clinical stage I non-small cell lung
cancer. |
Table I.
Comparison of pathological patients
with non-LNM and LNM clinical stage I non-small cell lung
cancer.
| Clinicopathological
characteristic | Non-LNM (n=249) | LNM (n=39) | P-value |
|---|
| Age, years, median
(IQR) | 70.0 (63.0-75.0) | 67.0 (62.0-74.0) | 0.440a |
| Male, n (%) | 164.0 (65.9) | 25 (64.1) | 0.727b |
| Smoking index, mean ±
SD (range) | 653.8±732.9
(0–6000) | 509.2±536.0
(0–1760) | 0.238c |
| BMI, median
(IQR) | 22.4 (19.8-24.3) | 22.6 (19.5-24.4) | 0.624a |
| CCI, mean ± SD
(range) | 1.1±1.2
(0.0-7.0) | 0.8±1.2
(0.0-4.0) | 0.167c |
| Spirometry |
|
|
|
| VC, ml,
median (IQR) | 3210.0
(2740.0-3820.0) | 3220.0
(2629.0-3770.0) | 0.766a |
| FVC,
ml, median (IQR) | 3230.0
(2695.0-3770.0) | 3475.0
(3060.0-4105.0) | 0.121a |
| Findings on CT |
|
|
|
| Whole
tumor size, mm, median (IQR) | 22.0
(15.0-28.0) | 25.0
(19.0-35.0) | 0.045a |
|
Consolidation size, mm, median
(IQR) | 15.0
(11.0-23.0) | 25.0
(19.0-35.0) | <0.001a |
| Pure solid tumor, n
(%) | 137.0 (55.0) | 38 (97.4) | <0.001b |
| SUVmax, mean ± SD
(range) | 5.5±5.0
(0.6-42.1) | 9.4±6.5
(0.8-25.0) | <0.001c |
| CEA, mean ± SD
(range) | 6.4±13.9
(0.9-208.0) | 7.5±6.9
(0.8-40.5) | 0.647c |
| CYFRA, mean ± SD
(range) | 2.7±3.2
(0.7-39.4) | 2.2±1.6
(0.9-8.4) | 0.444c |
| Lymph node
dissection ND1/ND2a-1/ND2a-2 (%) | 67.0/181.0/1
(26.9/72.7/0.4) | 11.0/28.0/0.0
(28.2/71.8/0.0) | 0.868d |
| Total number of
excised lymph nodes, mean ± SD (range) | 13.4±7.3
(1.0-41.0) | 14.4±8.9
(3.0-36.0) | 0.427c |
| AD/SQ/other, n
(%) | 182/55/12
(73.1/22.1/4.8) | 28/4/7
(71.8/10.3/17.9) | 0.003b |
| Pathological whole
size, mm, median (IQR) | 22.0
(15.0-30.0) | 25.0
(20.0-37.0) | 0.046a |
| Pathological
invasive size, mm, median (IQR) | 14.0
(7.0-22.0) | 24.0
(17.0-37.0) | <0.001a |
| Lympho-vascular
invasion, n (%) | 73.0 (29.3) | 34.0 (87.2) | <0.001b |
| Pleural invasion, n
(%) | 52.0 (20.9) | 18.0 (46.2) | <0.001b |
Cut-off values of SUVmax and CS
associated with LNM
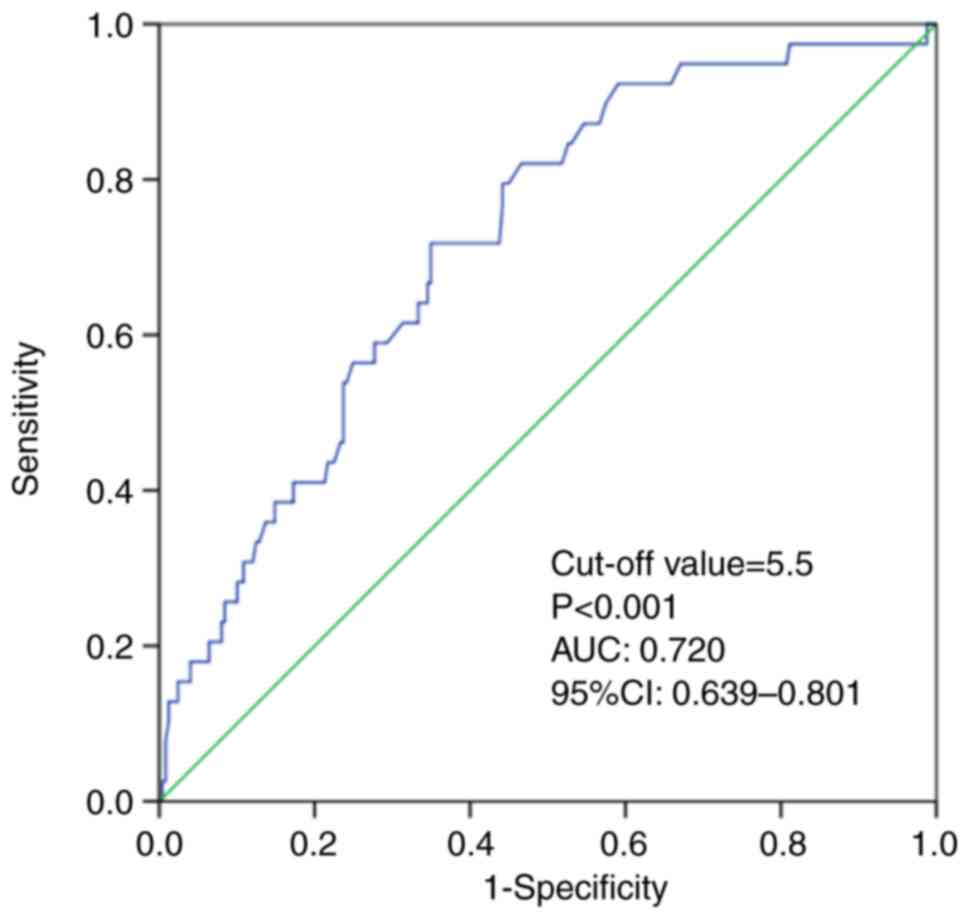
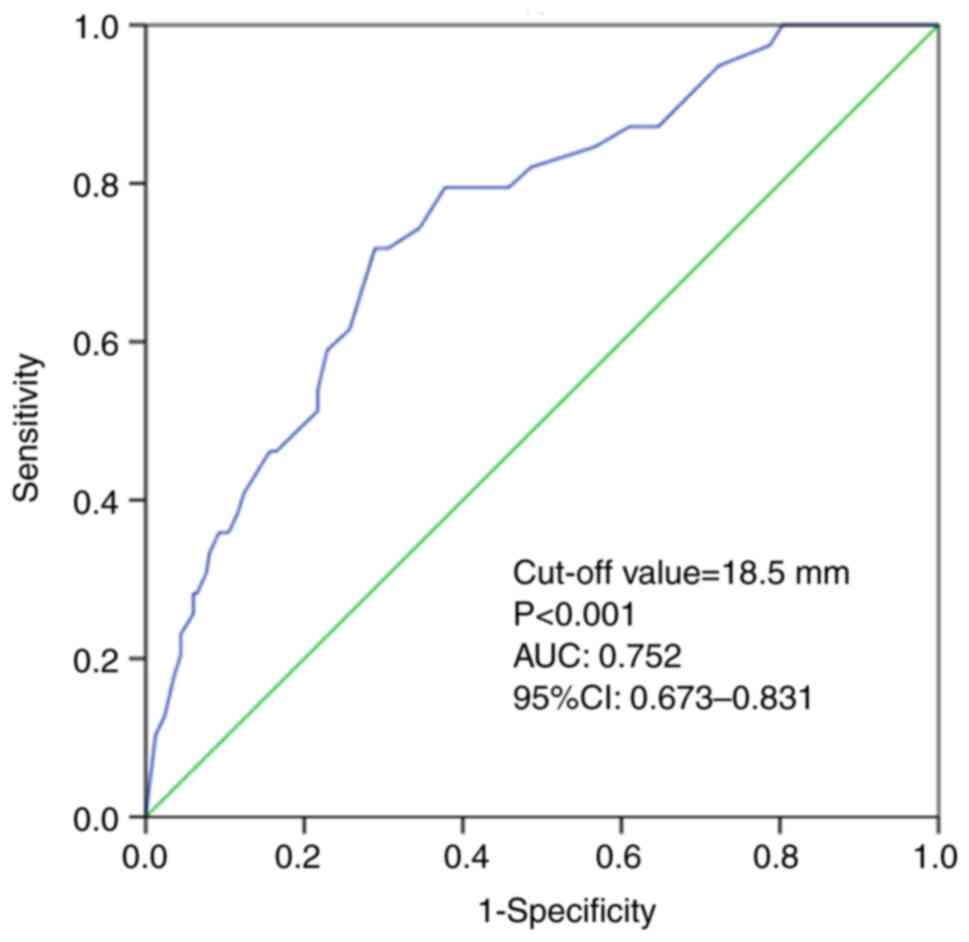
Analysis of the area under the ROC curve
demonstrated that the optimal cutoff value of SUVmax for predicting
LNM was 5.5 [area under the curve (AUC), 0.720; sensitivity, 71.8%;
specificity, 62.2%; 95% confidence interval (CI), 0.639-0.801;
P<0.001; Fig. 2]. The optimal
cut-off value of CS for predicting LNM was 18.5 mm (AUC, 0.752;
sensitivity, 79.5%; specificity, 62.2%; 95% CI, 0.673-0.831;
P<0.001; Fig. 3). These results
indicated that SUVmax and CS were useful predictive radiological
tools for LNM.
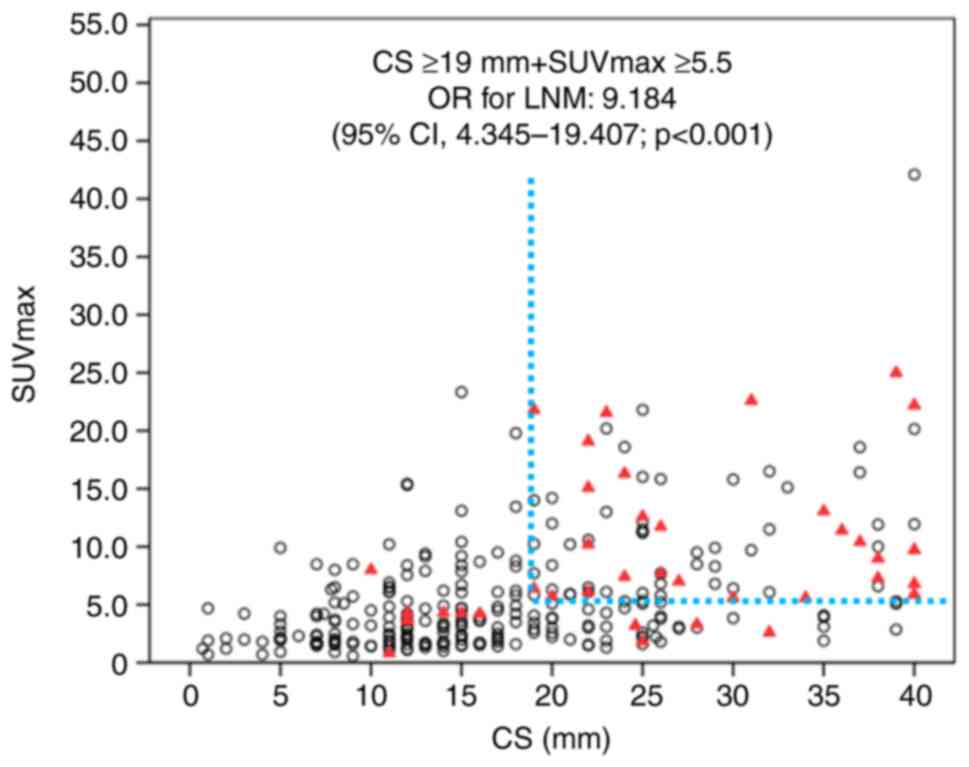
Odds ratios (ORs) for LNM according to
radiological parameters
ORs for LMN according to radiological parameters,
including CS ≥19 mm, SUVmax ≥5.5, CS ≥19 mm + SUVmax ≥5.5 and pure
solid tumor were calculated. CS and SUVmax are similar in terms of
quantitative radiation scale. These tools were evaluated for their
ORs for LNM when used alone and in combination, respectively. OR of
CS ≥19 mm was 6.390 (95% CI,2.819-14.484; P<0.001). OR of SUVmax
≥5.5 was 4.740 (95% CI, 2.251-9.979; P<0.001). CS ≥19 mm +
SUVmax ≥5.5 demonstrated an OR of 9.184 (95% CI, 4.345-19.407;
P<0.001). The pure solid tumor OR was 31.066 (95% CI,
4.199-229.87; P<0.001; Table
II). Scatter diagrams of LNM for both CS and SUVmax (Fig. 4) demonstrated that CS ≥19 mm +
SUVmax ≥5.5 indicated high risk for LNM.
 | Table II.Odds ratios for lymph node metastasis
according to radiological parameters. |
Table II.
Odds ratios for lymph node metastasis
according to radiological parameters.
| Parameter | Odds ratio | 95% confidence
interval | P-value |
|---|
| CS ≥19 mm | 6.390 | 2.819-14.484 | <0.001 |
| SUVmax ≥5.5 | 4.740 | 2.251-9.979 | <0.001 |
| CS ≥19 mm + SUVmax
≥5.5 | 9.184 | 4.345-19.407 | <0.001 |
| Pure solid
tumor | 31.066 | 4.199-229.870 | <0.001 |
Discussion
In NSCLC, primary tumor with a GGO component has a
better prognosis than a solitary tumor (4–6).
Hattori et al (14)
reported that the presence or absence of GGO should be considered
an essential parameter in clinical T classification. Suzuki et
al (15) demonstrated that
sufficient local control and recurrence-free survival (RFS) can be
achieved by sub-lobar resection with adequate surgical margin for
lung cancer with a maximum tumor diameter ≤2.0 cm and CTR ≤0.25
based on thin-section CT that has been clinically determined as N0.
In patients with sub-centimeter NSCLC with high SUVmax, Hattori
et al (16) reported that
lobectomy is associated with better 3-year RFS than sub-lobar
resection (88.3 vs. 50.0%, P=0.0453); for patients with pure-solid
sub-centimeter NSCLC and high SUVmax, major lung resection with LN
dissection is required for radical locoregional management to
prevent recurrence. In the present study, the predictive
radiological tools chest CT and PET-CT for occult LNM
classification for clinical stage I NSCLC were evaluated. Various
radiological findings using CT have been reported as predicting
prognosis of NSCLC, including WTS, CS, CTR, TDR, MD and presence of
GGO (12). Our previous review
reported that numerous studies have demonstrated that CS is the
most useful CT morphology method for predicting malignant behavior
regarding NSCLC (12,17–23).
Therefore, in the present study, CS was used for morphological
assessment using CT.
In the present study, larger CS, pure solid tumor
and higher SUVmax demonstrated significant association with LNM
(all P<0.05). In total, 39 (13.5%) patients were diagnosed with
pathological LNM. Lesions were pure solid type for 38 (97.4%) of
these patients. For convenience, the definition of pure solid
tumors in the present study included tumors with minor GGO
components outside of the CTR measurement site. Numerous authors
have suggested that part-solid tumors should be considered a
clinical subtype with better prognosis for both clinical and
pathological T1N0-staged lung adenocarcinomas (4–6). In
both clinical and pathological T1N0-staged NSCLC, solid tumors with
no GGO and larger CS are associated with longer disease-free
survival (21–23). In the present study, SUVmax and CS
were shown to be useful in predicting occult LNM. Optimal cut-off
values of SUVmax and CS for predicting LNM were 5.5 and 18.5 mm,
respectively. CS ≥19 mm + SUVmax ≥5.5 demonstrated a markedly
higher OR than these parameters separately (OR, 9.184; 95% CI,
4.345-19.407). The scatter diagrams of SUVmax and CS demonstrated
that CS ≥19 mm + SUVmax ≥5.5 indicated high risk for LNM; this may
assist in surgical planning. Pure solid type was a marked risk
factor for LNM (OR, 31.066; 95% CI, 4.199-229.87). Considering all
the results, it was determined that pure solid type and CS as
morphological factors and SUVmax as a metabolic factor were useful
tools that complemented each other in predicting LNM. The combined
method of evaluating SUVmax and CS may support determination of
eligibility for LN dissection.
Minimally invasive adenocarcinoma (MIA) has good
prognosis owing to the absence of lymphatic, vascular or pleural
invasion or necrosis (24).
Several radiological tools have been reported for the
identification of lympho-vascular invasion and LNM using CT
(12,25,26).
Hayashi et al (25)
reported that solid component size (tumor diameter in the MD >5
mm or CS >8 mm) predicts LNM and local invasiveness in T1 lung
adenocarcinoma. In the present study, CS of 10 mm was the minimum
value for LNM. Sakakura et al (26) reported that MD ≤2 mm predicts MIA
with a specificity of 94.5%. Previously, CS ≤5 mm was defined as
cT1mi category in the 8th TNM classification (2).
PET-CT is an imaging method that predicts tumor
activity by measuring tumor metabolism. However clinicians cannot
overlook differences in SUVmax when using PET-CT because SUVmax
varies due to different types of PET-CT scanners in each facility
(27). SUVmax of the primary tumor
is useful for predicting occult LNM in patients with lung cancer
(11,28,29).
Park et al (28) suggested
that SUVmax >7.3 in primary tumor independently predicts LNM in
clinical stage IA NSCLC. Furthermore, Kaseda et al (11) reported that the optimal cut-off
value for tumor SUVmax to predict LNM using the ROC curve is 3.0 in
clinical stage I NSCLC. Nambu et al (29) reported that the minimum SUVmax for
tumors in an LNM group is 2.5. Compared with these effective values
of SUVmax, our study showed that SUVmax ≥5.5 was the cutoff value
for occult LNM, which was within the range of previously reported
values (11,28,29).
However, in the present study, the minimum values of CS and SUVmax
associated with LNM were 10 mm and 0.8 respectively. Therefore, the
results of the present study do not confirm omission of LN
dissection for patients who do not meet the cut-off values for CS
and SUVmax. By eliminating the differences in SUV measurement
between centers, it may be possible to develop surgical strategies
based on PET and CT findings for use in clinical practice
worldwide.
The present study had certain limitations. This
retrospective observational study was performed in only a single
facility. Furthermore, other CT parameters, including pleural
indentation, lobule and notch are important in predicting behavior
of malignancy; however, these radiological tools were not
considered. Depending on patient comorbidities, mediastinal LN
dissection was omitted or limited to mediastinal LN sampling; this
lack of uniformity in level of mediastinal LN dissection may have
resulted in missed occult LNM and affected the analysis. Further
studies are needed to evaluate LNM with more accurate pathological
study.
Pure solid formation and CS morphology and SUVmax as
a metabolic aspect are useful tools that complement each other in
predicting LNM. The combined method of evaluating SUVmax and CS
identifies eligibility for LN dissection. However, considering the
minimum values of CS and SUVmax in LNM, it cannot affirm the
omission of LN dissection for cases that do not meet the combined
criteria using HRCT and PET-CT.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TN conceived the study, designed and performed the
experiments, analyzed data and wrote the manuscript. MY designed
and performed the experiments and edited the manuscript. TO
performed the experiments, supervised the study and edited the
manuscript. TN and MY confirm the authenticity of all the raw data.
All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was performed according to the
guidelines of the Declaration of Helsinki and approved by the
Review Board of Jikei University School of Medicine [approval no.
30-359(9380)].
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
AUC
|
area under the curve
|
|
CS
|
consolidation size
|
|
CT
|
computed tomography
|
|
CTR
|
consolidation-to-tumor ratio
|
|
EBUS-TBNA
|
endobronchial ultrasound-guided
transbronchial needle aspiration
|
|
FDG
|
18F-fluorodeoxyglucose
|
|
GGO
|
ground-glass opacity
|
|
LNM
|
lymph node metastasis
|
|
MIA
|
minimally invasive adenocarcinoma
|
|
NSCLC
|
non-small cell lung cancer
|
|
OR
|
odds ratio
|
|
PET
|
positron emission tomography
|
|
ROC
|
receiver operating characteristic
|
|
TDR
|
tumor disappearance ratio
|
|
TNM
|
tumor-node-metastasis
|
|
WTS
|
whole tumor size
|
References
|
1
|
National Comprehensive Cancer Network®, .
NCCN Clinical Practice Guideline in Oncology (NCCN
Guideline®) Non-small cell lung cancer. https://www2.tri-kobe.org/nccn/guideline/lung/englishJune
10–2019
|
|
2
|
Goldstraw P, Chansky K, Crowley J,
Rami-Porta R, Asamura H, Eberhardt WE, Nicholson AG, Groome P,
Mitchell A, Bolejack V, et al: The IASLC lung cancer staging
project: Proposals for revision of the TNM stage groupings in the
forthcoming (Eighth) edition of the TNM classification for lung
cancer. J Thorac Oncol. 11:39–51. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kim H, Goo JM, Kim YT and Park CM:
Consolidation-to-tumor ratio and tumor disappearance ratio are not
independent prognostic factors for the patients with resected lung
adenocarcinomas. Lung Cancer. 137:123–128. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hattori A, Hirayama S, Matsunaga T,
Hayashi T, Takamochi K, Oh S and Suzuki K: Distinct
clinicopathologic characteristics and prognosis based on the
presence of ground glass opacity component in clinical stage IA
lung adenocarcinoma. J Thorac Oncol. 14:265–275. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ye T, Deng L, Wang S, Xiang J, Zhang Y, Hu
H, Sun Y, Li Y, Shen L, Xie L, et al: Lung adenocarcinomas
manifesting as radiological part-solid nodules define a special
clinical subtype. J Thorac Oncol. 14:617–627. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Miyoshi T, Aokage K, Katsumata S, Tane K,
Ishii G and Tsuboi M: Ground-glass opacity is a strong
prognosticator for pathologic stage IA lung adenocarcinoma. Ann
Thorac Surg. 108:249–255. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fischer B, Lassen U, Mortensen J, Larsen
S, Loft A, Bertelsen A, Ravn J, Clementsen P, Høgholm A, Larsen K,
et al: Preoperative staging of lung cancer with combined PET-CT. N
Engl J Med. 361:32–39. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
The Japan Lung Cancer Society, . Japanese
guideline for lung cancer treatment. https://www.haigan.gr.jp/guideline/2018/1/1/180101050100.htmlJune
10–2019
|
|
9
|
Shirai K, Abe T, Saitoh JI, Mizukami T,
Irie D, Takakusagi Y, Shiba S, Okano N, Ebara T, Ohno T and Nakano
T: Maximum standardized uptake value on FDG-PET predicts survival
in stage I non-small cell lung cancer following carbon ion
radiotherapy. Oncol Lett. 13:4420–4426. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li L, Ren S, Zhang Y, Guan Y, Zhao J, Liu
J, Wang Q, Chen G, Chen H, Xiang J and Fu X: Risk factors for
predicting the occult nodal metastasis in T1-2N0M0 NSCLC patients
staged by PET/CT: Potential value in the clinic. Lung Cancer.
81:213–217. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kaseda K, Asakura K, Kazama A and Ozawa Y:
Risk factors for predicting occult lymph node metastasis in
patients with clinical stage I non-small cell lung cancer staged by
integrated fluorodeoxyglucose positron emission tomography/computed
tomography. World J Surg. 40:2976–2983. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nakada T and Kuroda H: Narrative review of
optimal prognostic radiological tools using computed tomography for
T1N0-staged non-small cell lung cancer. J Thorac Dis. 13:3171–3181.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hishida T, Miyaoka E, Yokoi K, Tsuboi M,
Asamura H, Kiura K, Takahashi K, Dosaka-Akita H, Kobayashi H, Date
H, et al: Lobe-specific nodal dissection for clinical stage I and
II NSCLC: Japanese multi-institutional retrospective study using a
propensity score analysis. J Thorac Oncol. 11:1529–1537. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hattori A, Suzuki K, Takamochi K,
Wakabayashi M, Aokage K, Saji H and Watanabe SI; Japan Clinical
Oncology Group Lung Cancer Surgical Study Group, : Prognostic
impact of a ground-glass opacity component in clinical stage IA
non-small cell lung cancer. J Thorac Cardiovasc Surg.
161:1469–1480. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Suzuki K, Watanabe SI, Wakabayashi M, Saji
H, Aokage K, Moriya Y, Yoshino I, Tsuboi M, Nakamura S, Nakamura K,
et al: A single-arm study of sublobar resection for ground-glass
opacity dominant peripheral lung cancer. J Thorac Cardiovasc Surg.
163:289–301.e2. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hattori A, Matsunaga T, Takamochi K, Oh S
and Suzuki K: Clinical significance of positron emission tomography
in subcentimeter non-small cell lung cancer. Ann Thorac Surg.
103:1614–1620. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kuroda H, Nakada T, Oya Y, Takahashi Y,
Matsusita H and Sakakura N: Clinical adjustability of radiological
tools in patients with surgically resected cT1N0-staged
non-small-cell lung cancer from the long-term survival evaluation.
J Thorac Dis. 12:6655–6662. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kim H, Goo JM, Kim YT and Park CM:
Validation of the eighth edition clinical T categorization system
for clinical stage IA, resected lung adenocarcinomas: Prognostic
implications of the ground-glass opacity component. J Thorac Oncol.
15:580–588. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chiang XH, Hsu HH, Hsieh MS, Chang CH,
Tsai TM, Liao HC, Tsou KC, Lin MW and Chen JS: Propensity-matched
analysis comparing survival after sublobar resection and lobectomy
for cT1N0 LUNG ADENOCARCINoma. Ann Surg Oncol. 27:703–715. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Su H, Dai C, She Y, Ren Y, Zhang L, Xie H,
Xie D, Jiang G and Chen C: Which T descriptor is more predictive of
recurrence after sublobar resection: Whole tumour size versus solid
component size? Eur J Cardiothorac Surg. 54:1028–1036. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hattori A, Matsunaga T, Takamochi K, Oh S
and Suzuki K: Importance of ground glass opacity component in
clinical stage IA radiologic invasive lung cancer. Ann Thorac Surg.
104:313–320. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Takenaka T, Yamazaki K, Miura N, Mori R
and Takeo S: The prognostic impact of tumor volume in patients with
clinical stage IA non-small cell lung cancer. J Thorac Oncol.
11:1074–1080. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Fu F, Zhang Y, Wen Z, Zheng D, Gao Z, Han
H, Deng L, Wang S, Liu Q, Li Y, et al: Distinct prognostic factors
in patients with stage I non-small cell lung cancer with radiologic
part-solid or solid lesions. J Thorac Oncol. 14:2133–2142. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Travis WD, Brambilla E, Noguchi M,
Nicholson AG, Geisinger KR, Yatabe Y, Beer DG, Powell CA, Riely GJ,
Van Schil PE, et al: International association for the study of
lung cancer/american thoracic society/european respiratory society
international multidisciplinary classification of lung
adenocarcinoma. J Thorac Oncol. 6:44–285. 2011. View Article : Google Scholar
|
|
25
|
Hayashi H, Ashizawa K, Ogihara Y, Nishida
A, Matsumoto K, Yamasaki N, Nagayasu T, Fukuda M, Honda S and
Uetani M: Comparison between solid component size on thin-section
CT and pathologic lymph node metastasis and local invasion in T1
lung adenocarcinoma. Jpn J Radiol. 35:109–115. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sakakura N, Inaba Y, Yatabe Y, Mizuno T,
Kuroda H, Yoshimura K and Sakao Y: Estimation of the pathological
invasive size of pulmonary adenocarcinoma using high-resolution
computed tomography of the chest: A consideration based on lung and
mediastinal window settings. Lung Cancer. 95:51–56. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Taira N, Atsumi E, Nakachi S, Takamatsu R,
Yohena T, Kawasaki H, Kawabata T and Yoshimi N: Comparison of
GLUT-1, SGLT-1, and SGLT-2 expression in false-negative and
true-positive lymph nodes during the 18F-FDG PET/CT
mediastinal nodal staging of non-small cell lung cancer. Lung
Cancer. 123:30–35. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Park HK, Jeon K, Koh WJ, Suh GY, Kim H,
Kwon OJ, Chung MP, Lee KS, Shim YM, Han J and Um SW: Occult nodal
metastasis in patients with non-small cell lung cancer at clinical
stage IA by PET/CT. Respirology. 15:1179–1184. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Nambu A, Kato S, Sato Y, Okuwaki H,
Nishikawa K, Saito A, Matsumoto K, Ichikawa T and Araki T:
Relationship between maximum standardized uptake value (SUVmax) of
lung cancer and lymph node metastasis on FDG-PET. Ann Nucl Med.
23:269–275. 2009. View Article : Google Scholar : PubMed/NCBI
|