Introduction
Carcinosarcomas are relatively uncommon but highly
malignant tumors originated from female genital tract organs,
including the uterus (1–4). Recently, uterine carcinosarcomas
(UCs) were incorporated into the ‘high-risk’ endometrial cancer
(EC) group by the European Society of Gynecological
Oncology/European Society of Radiation Oncology/European Society
for Pathology Consortium (5). They
are composed of two different components, carcinomatous and
sarcomatous, and both of them are malignant. Although controversies
still exist over their origin, it is generally accepted that UCs
are monoclonal, in general (6–9).
Four theories of their histogenesis have been presented in numerous
studies up to now, although the composition theory (the stromal
component is not truly neoplastic, but acts as a reactive response
to the existence of a malignant epithelial component) has been
abandoned (8–10). A ‘milestone’
genetic/immunohistochemical (IHC) study by Wada et al
(11) argued that although most
UCs are combination tumors, some may develop as collision neoplasms
as well. Recently, somatic DNA mutational analysis was undertaken,
and gene expression and allelic imbalance of several genes were
separately analyzed in the sarcomatous and carcinomatous components
of 10 UC patients (12). The
researchers reported that both components of UCs exhibited similar
molecular profiling, suggesting that ‘the carcinomatous and
sarcomatous components may rise from a common precursor or perhaps
one of the components rises from the other at a late stage’
(12).
The 5-year overall survival of patients affected by
UCs is poor, and is significantly decreased when the clinical stage
of the disease increases (for example, the figures are nearly 50%
for stage I, whereas they are below 10% for stage IV) (13,14).
In general, patients affected by UCs are usually >50 years old,
with the median age being 62 years-old (2,8,15).
Risk factors for the development of UCs are similar to those of
ECs: Nulliparity, advanced age of patients, obesity, exposure to
estrogens and SERMs, as well as exposure to radiation therapy
(16–18).
In the scientific literature, a selected number of
reports have investigated the impact of proliferative activity on
the development and progression of UCs (19–29).
For example, Ki67 expression pattern was found to be higher in UCs,
as compared with uterine adenosarcomas (P=0.03) (19). Furthermore, Lee et al
(23) reported an elevated
expression of topoI and Ki67 in 20 UCs, although no correlation
between the two IHC proliferative markers existed (P=0.817). A
previous study from the authors also showed a significant
correlation of Ki67 immunoreactivity between two malignant
components of UCs (R=0.676, P<0.001) (26). However, there are no studies
investigating the relationship between proliferative markers
immunoreactivity independently in both components of UCs.
The aim of the present study was to ascertain IHC
proliferative markers [Ki67, proliferating cell nuclear antigen
(PCNA), minichromosome maintenance complex component 3 (MCM3), and
topoisomerase IIα (topoIIα)] expression in UCs, by analyzing
immunostaining reactivity independently in the two malignant
components. Moreover, the relationship of staining results to
clinicopathological variables of the neoplasm was examined, and the
correlation between proliferative markers was analyzed.
Materials and methods
Patients and tissue samples
A total of 30 paraffin-embedded slides of UCs were
collected from patients who underwent radical surgery at the Second
Department of Gynecology of Lublin Medical University (Lublin,
Poland) between January 1, 2006, and December 31, 2020. The
dilatation and curettage procedure was performed in all patients
pre-operatively, and the diagnosis of UC was conducted. Although
primarily 34 cases were included, there was not enough material to
perform all IHC experiments in three cases, and, in another, the
coexistence of two synchronous, independent neoplasms (UC and
cervical adenocarcinoma) was surprisingly discovered during the
reassessment of the slides for the experiments. Collectively, 26
endometrioid-type endometrial carcinomas and 4 non-endometrioid
carcinomas (2 clear-cell carcinomas, 1 papillary-serous carcinoma
and 1 undifferentiated carcinoma). Moreover, there were 21
homologous-type tumors (stromal sarcoma, n=14; leiomyosarcoma, n=4;
and not otherwise specified, n=3), and 9 heterologous-type
(rhabdomyosarcoma, n=5; chondrosarcoma, n=3; and osteosarcoma, 1)
tumors (Table I). The mean age of
patients was 67 years (from 42–84 years of age; median: 68 years).
No chemotherapy, radiotherapy or hormonotherapy were applied before
the surgery. Post-operative material was selected following
pathological review at the Department of Clinical Pathology, Lublin
Medical University, Lublin, Poland, by a highly-experienced
pathologist (DL). Histopathological assessment was performed based
on revised classification of World Health Organization (30), whereas clinical stage of the
disease was classified according to the revised the International
Federation of Gynecology and Obstetrics (FIGO) staging system for
ECs (31). The present study was
approved (approval no. 0254/144/2018) by the Independent Ethics
Committee of the Lublin Medical University (Lublin, Poland). Signed
informed consent was provided by all women prior to surgery, that
they agreed to use of paraffin-embedded slides in future scientific
research. Clinical and pathological characteristics of the study
group are presented in Table
I.
 | Table I.Clinicopathological features of 30
women affected by uterine carcinosarcomas. |
Table I.
Clinicopathological features of 30
women affected by uterine carcinosarcomas.
| Parameters | n (%) |
|---|
| Age, years |
|
|
<50 | 2 (7) |
|
50-60 | 5 (17) |
|
>60 | 23 (76) |
| Carcinomatous
component |
|
|
Endometrioid | 26 (87) |
|
Non-endometrioid | 4 (13) |
| Sarcomatous
component |
|
|
Homologous | 21 (70) |
|
Heterologous | 9 (30) |
| Myometrial
invasion |
|
|
Yes | 16 (53) |
| No | 14 (47) |
| Lymphovascular
space invasion |
|
|
Yes | 18 (60) |
| No | 12 (40) |
| Stage (FIGO) |
|
| I | 11 (37) |
| II | 6 (20) |
|
III | 7 (23) |
| IV | 6 (20) |
| Presence of tumor
in the oviduct |
|
|
Yes | 7 (23) |
| No | 23 (77) |
| Grade |
|
| G1 | 5 (17) |
| G2 | 7 (23) |
| G3 | 18 (60) |
| Metastasis |
|
|
Yes | 12 (40) |
| No | 18 (60) |
| Omental
metastasis |
|
|
Yes | 4 (13) |
| No | 26 (87 |
Immunohistochemistry (IHC)
Tissue material collected at the operation theatre
was immediately fixed in 10% buffered formalin (pH 7.4) at room
temperature overnight, and the paraffin blocks were prepared
according to standard laboratory technique. Paraffin blocks were
cut on 3-µm slides, and put on silanized slides (Sigma-Aldrich;
Merck KGaA). The IHC technique was performed using the DAKO
REAL™EnVision™/HRT kit (Dako; Agilent
Technologies, Inc.) according to the manufacturer's protocol. DAB
(3,3′-di-aminobenzidine tetrahydrochloride) was exploited as a
chromogen. The following primary antibodies (Dako; Agilent
Technologies, Inc.) were applied: Monoclonal mouse anti-human
antibody against Ki67 (cat. no. M7240; clone MIB-1; 1:50);
monoclonal mouse anti-human antibody against PCNA (cat. no. M0879;
clone PC10; 1:1,000); monoclonal mouse anti-human antibody against
MCM3 (cat. no. M7263; clone 101; 1:25); and monoclonal mouse
anti-human antibody against topoIIα (cat. no. M7186; clone Ki-S1;
1:50). All antibodies were incubated for 30 min at room
temperature. Afterwards, the detection system was employed, and the
visualization was performed by 0.1% DAB solution for 5 min at room
temperature. The sections were finally counterstained with Mayer's
hematoxylin for 1 min at room temperature, dehydrated and
cover-slipped after being embedded in mounting medium. The slides
were stored at room temperature.
Immunohistochemical controls
Positive and negative controls were included in each
experiment. Positive control was an EC showing enhanced staining
for each antibody applied. Negative control was a section in which
the primary antibody was replaced by Tris-buffered saline.
Immunohistochemical assessment
The representative areas (500 cells) were selected
on a light microscope (Nikon Corporation) and counted by 2
independent researchers (DL and AS) who were aware of
clinicopathological variables. A full agreement of nearly 90% was
reported. However, when the consensus was not reached, both
researchers cooperatively analyzed region by region until the full
agreement was achieved. Nuclear Ki67 expression was considered
positive if >30% of the tumor cells showed positive
immunostaining as previously described (23). For nuclear PCNA, MCM3 and topoIIα
immunoreactivity, the scores >90, >25, and >5% were deemed
positive, respectively (32–34).
Statistical analyses
Statistical analyses were performed with
Kołmogorow-Smirnow, Shapiro-Wilk, χ2-Pearson's and
Fisher's exact tests. Spearman's rank correlation coefficient was
applied to determine correlations between proteins and patients'
age. Statistical analysis was carried out using Statistica 9.0
software (StatSoft, Inc.). P<0.05 was considered to indicate a
statistically significant difference.
Results
Expression of Ki67 in both components
of UC
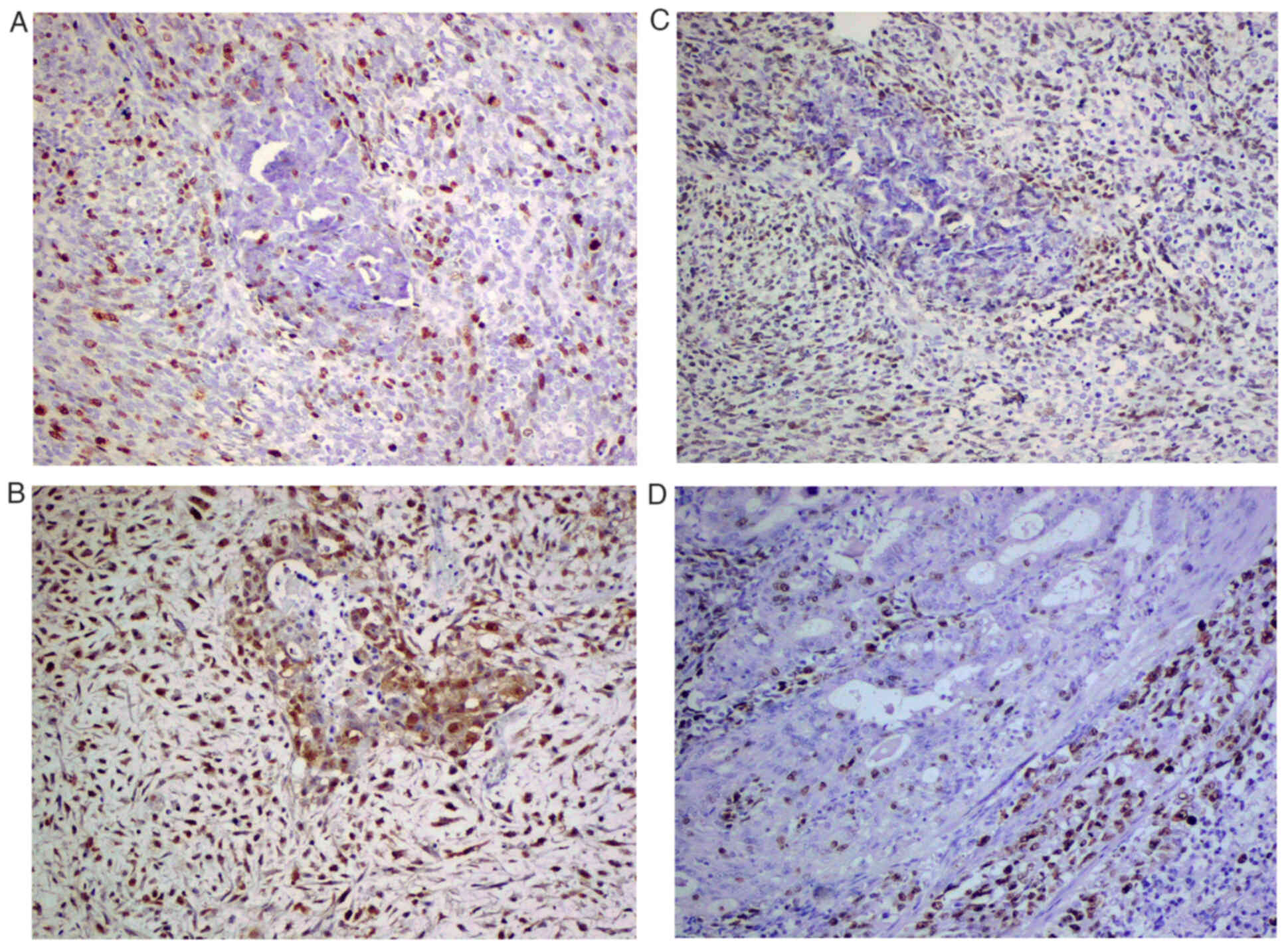
Ki67-positive nuclear staining was observed in 20
(67%) and 16 (53%) of the UC carcinomatous and sarcomatous
components, respectively (Fig.
1A). In the epithelial component, Ki67-positive reactivity was
related to FIGO stage (P=0.025), and histological grade (G1 vs.
G2/G3; P=0.031) (Table II).
However, only a trend was reported when histological grading was
analyzed separately (G1 vs. G2 vs. G3; P=0.057). In the sarcomatous
component, no significant relationship between Ki67 expression and
clinicopathological variables was identified.
 | Table II.Expression of Ki67 in relation to
clinicopathological features within the carcinomatous component of
uterine carcinosarcomas. |
Table II.
Expression of Ki67 in relation to
clinicopathological features within the carcinomatous component of
uterine carcinosarcomas.
|
|
| Expression level of
Ki67 |
|
|---|
|
|
|
|
|
|---|
| Parameter | n | Yes, n (%) | No, n (%) | P-value |
|---|
| Age, years |
|
|
| 0.385a |
|
<50 | 2 | 2 (100) | 0 |
|
|
50-60 | 5 | 3 (60) | 2 (40) |
|
|
>60 | 23 | 14 (61) | 9 (39) |
|
| Carcinomatous
component |
|
|
| 1.00b |
|
Endometrioid | 26 | 9 (35) | 17 (65) |
|
|
Non-endometrioid | 4 | 1 (25) | 3 (75) |
|
| Myometrial
invasion |
|
|
| 0.122b |
|
Yes | 16 | 3 (19) | 13 (81) |
|
| No | 14 | 7 (50) | 7 (50) |
|
| Lymphovascular
space invasion |
|
|
| 0.139b |
|
Yes | 18 | 4 (22) | 14 (78) |
|
| No | 12 | 6 (50) | 6 (50) |
|
| Stage (FIGO) |
|
|
| 0.025a |
| I | 11 | 6 (55) | 5 (45) |
|
| II | 6 | 1(17) | 5 (83) |
|
|
III | 7 | 0 | 7 (100) |
|
| IV | 6 | 3 (50) | 3 (50) |
|
| Presence of tumor
in the oviduct |
|
|
| 0.657b |
|
Yes | 7 | 3 (43) | 4 (57) |
|
| No | 23 | 7 (30) | 16 (70) |
|
| Grade |
|
|
| 0.057a |
| G1 | 5 | 4 (80) | 1 (20) |
|
| G2 | 7 | 2 (29) | 5 (71) |
|
| G3 | 18 | 4 (22) | 14 (78) |
|
| Metastasis |
|
|
| 0.694b |
|
Yes | 12 | 3 (25) | 9 (75) |
|
| No | 18 | 7 (39) | 11 (61) |
|
| Omental
metastasis |
|
|
| 0.095b |
|
Yes | 4 | 3 (75) | 1 (25) |
|
| No | 26 | 7 (27) | 19 (73) |
|
Expression of PCNA in both components
of UC
Nuclear PCNA reactivity was detected in 18 (60%) and
16 (53%) of the UC carcinomatous and sarcomatous components,
respectively (Fig. 1B). Notably,
all four cases with omental metastases were PCNA-positive, and a
relationship between staining pattern and the existence of
metastases was of significant value (P=0.018; Table SI). None of the
clinicopathological variables in the mesenchymal component were
related to PCNA staining.
Expression of MCM3 in both components
of UC
MCM3 expression was found nearly twice as high in
the carcinomatous (n=19, 63%), as the sarcomatous (n=11, 37%) UC
component, respectively. Only nuclear MCM3 reactivity was
considered positive (Fig. 1C).
MCM3 staining in the epithelial component was related to clinical
stage (P=0.03), and to the existence of omental metastasis
(P=0.012) (Table SII). None of
the clinicopathologic features showed significant relationship with
MCM3 staining in the sarcomatous UC component.
Expression of topoIIα in both
components of UC
Out of the 30 cases, 17 (57%) and 13 (43%) showed
nuclear positivity in the carcinomatous and sarcomatous component,
respectively (Fig. 1D). A
significant relationship between protein immunoreactivity with
clinical stage (P=0.049), and omental metastasis (P=0.026) was
found to exist (Table SIII).
Moreover, there was a trend towards increasing topoIIα expression
pattern with the advancement of myometrial invasion (P=0.063). No
significant differences between topoIIα expression and
clinicopathological features in the sarcomatous UC component were
indicated.
Correlation between protein expression
patterns in different components of UC
Statistical analyses of the correlation between
selected IHC markers in different UC components are presented in
Tables III and IV. For example, in the cancerous UC
component, Ki67 staining was correlated with expression of MCM3 and
topoIIα, and PCNA with MCM3 and topoIIα (Table III). Finally, it is worth
pointing out that proliferative markers revealed a significant
correlation with each other in the sarcomatous component of UC
(Table IV). There was no
correlation between protein reactivity and patient age (P>0.05;
Spearman rank correlation test; data not shown).
 | Table III.Correlational analysis of different
proliferative markers in the carcinomatous component of uterine
carcinosarcomas (Spearman rank correlation test). |
Table III.
Correlational analysis of different
proliferative markers in the carcinomatous component of uterine
carcinosarcomas (Spearman rank correlation test).
|
| Ki67 | PCNA | MCM3 | topoIIα |
|---|
| Ki67 |
| R=0.2886 | R=0.3423 | R=0.6659 |
|
|
| P=0.1218 | P=0.064 | P=0.000059 |
| PCNA | R=0.2886 |
| R=0.3671 | R=0.3844 |
|
| P=0.1218 |
| P=0.04597 | P=0.0359 |
| MCM3 | R=0.3423 | R=0.3671 |
| R=0.3403 |
|
| P=0.064 | P=0.04597 |
| P=0.06577 |
| topoIIα | R=0.6659 | R=0.3844 | R=0.3403 |
|
|
| P=0.000059 | P=0.0359 | P=0.06577 |
|
 | Table IV.Correlational analysis of different
proliferative markers in the sarcomatous component of uterine
carcinosarcomas (Spearman rank correlation test). |
Table IV.
Correlational analysis of different
proliferative markers in the sarcomatous component of uterine
carcinosarcomas (Spearman rank correlation test).
|
| Ki67 | PCNA | MCM3 | topoIIα |
|---|
| Ki67 |
| R=0.7321 | R=0.4193 | R=0.5483 |
|
|
| P=0.000004 | P=0.02108 | P=0.0017 |
| PCNA | R=0.7321 |
| R=0.4193 | R=0.5483 |
|
| P=0.000004 |
| P=0.0211 | P=0.0017 |
| MCM3 | R=0.4193 | R=0.4193 |
| R=0.3429 |
|
| P=0.02108 | P=0.0211 |
| P=0.0635 |
| topoIIα | R=0.5483 | R=0.5483 | R=0.3429 |
|
|
| P=0.0017 | P=0.0017 | P=0.0635 |
|
Discussion
Assessment of cell proliferation activity by antigen
retrieval techniques, using formalin-fixed and paraffin-embedded
slides, has been extensively applied as prognosticator in various
gynecologic malignancies (35–37).
In certain circumstances, IHC cell proliferation assessment has
also been incorporated into routine clinical practice (35,38).
For example, Mittal et al (35) recommended the application of a
panel of antibodies, including cytokeratin, desmin, S100 and myoD1,
for distinguishing between undifferentiated EC, undifferentiated
uterine sarcoma and UC. However, quantification of epithelial cell
proliferation in biphasic female genital tract neoplasms is a
scientific challenge due to the lack of reported investigations.
Based on the fact that their histogenesis remains a matter of
controversy, the assessment of cell proliferation is an innovative
and interesting task.
The present study is an extension of our broad
scientific interest in investigating the impact of various
IHC/genetic alterations on the development and progression of UCs
and their corresponding metastases (26,39–43).
In the present study, an enhanced proliferative expression pattern
of all markers was demonstrated in the carcinomatous component of
UC, as compared with the sarcomatous one. Moreover, IHC markers
immunostaining (Ki67, MCM3 and topoIIα) were found to be related to
clinical stage [the most important prognostic factor of patients
with UC (8)], and to the
development of omental metastasis, but only in the carcinomatous
component. By contrast, no proliferative markers expression pattern
was demonstrated to be related to clinico-prognostical features in
the sarcomatous component. Based on the present observations, there
are two possible explanations of this phenomenon.
Firstly, the carcinomatous UC component may be more
important in the malignant transformation of UCs, as previously
described (21,44,45).
The present data is also in line with that of Ikeda et al
(22), who reported significantly
higher Ki67 in the carcinomatous, compared with the sarcomatous
component (P=0.0173). Similar observations have been presented
previously by Nicotina et al (20), who suggested that mitotic index and
MIB-1 labeling index may be used as complementary indices to assess
the outcome of UCs. It is thus of interest to cite the study by
Yoshida et al (21), who
reported that carcinomatous component ‘may play an important role
in aggressive biologic behavior in UCs’.
Upon investigating molecular markers and
clinicopathological features of UCs, de Jong et al (45) also put forward that the
carcinomatous component is ‘truly’ a major factor determining the
prognostic impact of UC patients, causing the majority of
metastases, as well as vascular infiltration. By contrast, however,
there are also data reporting no significant difference of Ki67
immunostaining between carcinomatous and sarcomatous UC components
(46).
Secondly, the present observations indicated via
indirect evidence that the carcinomatous component may be a
‘driving force’ in potential tumor spread, being responsible for
the development of distant (omental) metastases. The most common
sites of UC metastasis are the lung (49%), peritoneum (44%),
pelvic/paraoartic lymph nodes (35%), adrenal gland or bone (19%),
heart or pericardium (9%) and/or brain (7%) (8). Notably, most of these metastases are
clinically asymptomatic and generally spread throughout the
lymphatic system. Although only ten cases were investigated by
Yoshida et al (21),
regional lymph node metastases (3 out of 10) were found to be only
fold ups of the carcinomatous component. These data are in line
with the ‘core’ study by Sreenan and Hart (47), which demonstrated that most
metastatic UCs consist primarily of a pure carcinomatous component,
although carcinomatous/sarcomatous, and a pure sarcomatous
component were also incidentally detected.
In the present study, although only four UC (all
poorly-differentiated disseminated neoplasms) cases showed omental
metastasis, all of them revealed proliferative markers (PCNA, MCM3
and topoIIα) positive immunostaining in the carcinomatous
component. It is worth to mention that investigations of UC omental
metastasis are of utmost uncommon based on pertinent literature
review. However, to make a final conclusion, a cohort of primary UC
tumors corresponding with metastases should be simultaneously
assessed using IHC in an international cooperative research
study.
In the literature, there is only one study reporting
the simultaneous correlational analysis of different proliferative
markers in both UC components. While no significant difference
between Ki67 expression pattern and elevated topoI (not topoIIα)
staining was presented in 20 UCs by Korean researchers (23), on the contrary, however,
significant correlation between each different proliferative marker
in UCs has been currently documented, particularly in the
sarcomatous component. It was assumed that certain of the
proliferative markers (Ki67 and PCNA) may be potentially applied to
assess the proliferative potential in selected histological
subtypes of uterine sarcomas. According to the opinion of the
authors, positive correlation between proliferative markers may be
explain by the enhanced antigen activity in selected phases of the
cell-cycle (48). Limited number
of cases investigated (although one of the largest series reported
so far) may be also responsible for the lack of correlation in
different IHC UC components, particularly in the carcinomatous one.
Finally, the primary size UC assessment was not performed due to
the retrospective nature of the present study.
In conclusion, the assessment of proliferative
activity may be associated with tumor aggressiveness during the
process of development and widespread of UCs. A combined analysis
of Ki67, PCNA, MCM3 and topoIIα may, therefore, provide detailed
data of cell-cycle regulation mechanisms determining the
inter-component heterogeneity of UCs. Finally, pertinent literature
review, being in preparation from the authors, may support the role
of selected proliferative markers assessment in differential
diagnosis of uterine carcinoma, uterine sarcoma and UC.
Supplementary Material
Supporting Data
Acknowledgements
The authors would like to acknowledge Professor
Michal Bogusiewicz and Professor Marek Gogacz (Second Department of
Gynecology, Lublin Medical University, Lublin, Poland) for
providing valuable suggestions and meaningful discussions during
the preparation of the manuscript.
Funding
The present study was supported by the Lublin Medical
University, Lublin, Poland (grant no. 326/21).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AP, DL, BB and MC conceived and designed the study.
AAG, ASS and AS analyzed the data and wrote the manuscript. AS
supervized the final preparation and submission of the manuscript.
All authors read and approved the final version of the manuscript.
AP and AS confirm the authenticity of all the raw data.
Ethics approval and consent to
participate
The present study was approved (approval no.
0254/144/2018) by the Independent Ethics Committee of the Lublin
Medical University (Lublin, Poland). Signed informed consent was
provided by all patients prior to surgery, who agreed to the use of
paraffin-embedded slides in future scientific research.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kernochan LE and Garcia RL:
Carcinosarcomas (malignant mixed Müllerian tumor) of the uterus:
Advances in elucidation of biologic and clinical characteristics. J
Natl Compr Canc Netw. 7:550–557. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lopez-Garcia MA and Palacios J: Pathologic
and molecular features of uterine carcinosarcomas. Semin Diagn
Pathol. 27:274–286. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Singh R: Review literature on uterine
carcinosarcoma. J Cancer Res Ther. 10:461–468. 2014.PubMed/NCBI
|
|
4
|
Liao CI, Caesar MA, Lee D, Chan A, Darcy
KM, Tian C, Kapp DS and Chan JK: Increasing incidence of uterine
carcinosarcoma: A United States cancer statistics study. Gynecol
Oncol Rep. 40:1009362022. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Concin N, Matias-Guiu X, Vergote I, Cibula
D, Mirza MR, Marnitz S, Ledermann J, Bosse T, Chargari C, Fagotti
A, et al: ESGO/ESTRO/ESP guidelines for the management of patients
with endometrial carcinoma. Int J Gynecol Cancer. 31:12–39. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kounelis S, Jones MW, Papadaki H, Bakker
A, Swalsky P and Finkelstein SD: Carcinosarcomas (malignant mixed
mullerian tumors) of the female genital tract: Comparative
molecular analysis of epithelial and mesenchymal components. Hum
Pathol. 29:82–87. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
McCluggage WG: Malignant biphasic uterine
tumours: Carcinosarcomas or metaplastic carcinomas? J Clin Pathol.
55:321–325. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kanthan R and Senger JL: Uterine
carcinosarcomas (malignant mixed Müllerian tumours): A review with
special emphasis on the controversies in management. Obstet Gynecol
Int. 2011:4707952011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Matsuzaki S, Klar M, Matsuzaki S, Roman
LD, Sood AK and Matsuo K: Uterine carcinosarcoma: Contemporary
clinical summary, molecular updates, and future research
opportunity. Gynecol Oncol. 160:586–601. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kadota K, Haba R, Ishikawa M, Kushida Y,
Katsuki N, Hayashi T, Miyai Y, Bando K, Shiota A and Hata T:
Uterine cervical carcinosarcoma with heterologous mesenchymal
component: A case report and review of the literature. Arch Gynecol
Obstet. 280:839–843. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wada H, Enomoto T, Fujita M, Yoshino K,
Nakashima R, Kurachi H, Haba T, Wakasa K, Shroyer KR, Tsujimoto M,
et al: Molecular evidence that most but not all carcinosarcomas of
the uterus are combination tumors. Cancer Res. 57:5379–5385.
1997.PubMed/NCBI
|
|
12
|
Liu Y, Weber Z, San Lucas FA, Deshpande A,
Jakubek YA, Sulaiman R, Fagerness M, Flier N, Sulaiman J, Davis CM,
et al: Assessing inter-component heterogeneity of biphasic uterine
carcinosarcomas. Gynecol Oncol. 151:243–249. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jonson AL, Bliss RL, Trusnikovsky A,
Judson P, Argenta P, Carson L, Dusenbery K and Downs LS Jr:
Clinical features and outcomes of uterine and ovarian
carcinosarcoma. Gynecol Oncol. 100:561–564. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rauh-Hain JA, Shoni M, Schorge JO, Goodman
A, Horowitz NS and del Carmen MG: Prognostic determinants in
patients with uterine and ovarian carcinosarcoma. J Reprod Med.
58:297–304. 2013.PubMed/NCBI
|
|
15
|
Adachi Y, Nonogaki H, Minamiguchu S, Li M
and Ikehara S: Carcinosarcoma of the uterus: A case report. Mol
Clin Oncol. 4:571–573. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Callister M, Ramondetta LM, Jhingran A,
Burke TW and Eifel PJ: Malignant mixed Müllerian tumors of the
uterus: Analysis of patterns of failure, prognostic factors, and
treatment outcome. Int J Radiat Oncol Biol Phys. 58:786–796. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Villena-Heinsen C, Diesing D, Griesinger
G, Maas N, Diedrich K and Friedrich M: Carcinosarcomas-a
retrospective analysis of 21 patients. Anticancer Res.
26:4817–4823. 2006.PubMed/NCBI
|
|
18
|
Chen X, Arend R, Hamele-Bena D, Tergas AI,
Hawver M, Tong GX, Wright TC and Wright JD: Uterine
carcinosarcomas: Clinical, histopathologic and immunohistochemical
characteristics. Int J Gynecol Pathol. 36:412–419. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Swisher EM, Gown AM, Skelly M, Ek M,
Tamimi HK, Cain JM, Greer BE, Muntz HG and Goff BA: The expression
of epidermal growth factor receptor, HER-2/Neu, p53, and Ki-67
antigen in uterine malignant mixed mesodermal tumors and
adenosarcoma. Gynecol Oncol. 60:81–88. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nicotina PA, Ferlazzo G and Vincelli AM:
Proliferation indices and p53-immunocytochemistry in uterine mixed
mullerian tumors. Histol Histopathol. 12:967–972. 1997.PubMed/NCBI
|
|
21
|
Yoshida Y, Kurokawa T, Fukuno N,
Nishiokawa Y, Kamitani N and Kotsuji F: Markers of apoptosis and
angiogenesis indicate that carcinomatous components play an
important role in the malignant behavior of uterine carcinosarcoma.
Hum Pathol. 31:1448–1454. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ikeda K, Tate G, Suzuki T and Mitsuya T:
Effusion cytodiagnosis of carcinosarcoma derived from the female
genital tract: Immunohistochemical features of MMP-7 and Ki-67 and
immunofluorescence double staining analyses of eight cases. Gynecol
Oncol. 97:323–329. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lee SJ, Kim HS, Kim HS, Chun YK, Hong YR
and Lee JH: Immunohistochemical study of DNA topoisomerase I, p53,
and Ki-67 in uterine carcinosarcomas. Hum Pathol. 38:1226–1231.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kanthan R, Senger JL and Diudea D:
Malignant mixed mullerian tumors of the uterus: Histopathological
evaluation of cell cycle and apoptotic regulatory proteins. World J
Surg Oncol. 8:602010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Koivisto-Korander R, Butzow R, Koivistro
AM and Leminen A: Immunohistochemical studies on uterine
carcinosarcoma, leiomyosarcoma, and endometrial stromal sarcoma:
Expression and prognostic importance of ten different markers.
Tumor Biol. 32:451–459. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bałon B, Kaznowska E, Ignatov A, Steć A,
Semczuk-Sikora A, Schneider-Stock R, Jóźwik M, Sulkowski S,
Cybulski M, Szumiło J and Semczuk A: p53 is not related to Ki-67
immunostaining in the epithelial and mesenchymal components of
female genital tract carcinosarcomas. Oncol Rep. 30:1661–1668.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yue X, Utsunomita H, Akahira JI, Suzuki F,
Ito K, Nagase S, Sasano H and Yaegashi N: Expression of steroid and
xenobiotic receptor in uterine carcinosarcoma, leiomyosarcoma and
endometrial stromal sarcoma. Oncol Lett. 5:835–839. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhou Y, Huang H, Yuan LJ, Xiong Y, Huang
X, Lin JX and Zheng M: CD146 as an adverse prognostic factor in
uterine sarcoma. Eur J Med Res. 20:672015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Tochimoto M, Oguri Y, Hashimura M, Konno
R, Matsumoto T, Yokoi A, Kodera Y and Saegusa M: S100A4/non-muscle
myosin II signaling regulates epithelial-mesenchymal transition and
stemness in uterine carcinosarcoma. Lab Invest. 100:682–695. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Female Genital Tumors, . WHO
classification of tumors. 5th edition. Vol. 4. WHO Classification
of Tumours Editorial Board; 2020
|
|
31
|
Koksas M, Amant F, Mirza MR and Creutzberg
CL: Cancer of the corpus uteri: 2021 update. Int J Gynecol Obstet.
155 (Suppl 1):S45–S60. 2021. View Article : Google Scholar
|
|
32
|
Hassab El-Naby NED, Muhammad EMS,
El-Nashar AT, Sotouhy SMM and Mahmoude SM: P0173 use of PTEN, PCNA,
and β-cathenin to differentiate between endometrial hyperplasia and
endometrial adenocarcinoma. Eur J Cancer. 50 (Suppl 4):E592014.
View Article : Google Scholar
|
|
33
|
Lameira AG, Pontes FS, Guimarães DM, Alves
AC, de Jesus AS, Pontes HA and Pinto Ddos S Jr: MCM3 could be a
better marker than Ki-67 for evaluation of dysplastic oral lesions:
An immunohistochemical study. J Oral Pathol Med. 43:427–434. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kreisholt JM, Sorensen M, Jensen PB,
Nielsen BS, Andersen CB and Sehested M: Immunohistochemical
detection of DNA topoisomerase IIalpha, P-glycoprotein and
multidrug resistance protein (MRP) in small-cell and non-small-cell
lung cancer. Br J Cancer. 77:1469–1473. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Mittal K, Soslow R and McCluggage WG:
Application of immunohistochemistry to gynecologic pathology. Arch
Pathol Lab Med. 132:402–423. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Kaspar HG and Crum CP: The utility of
immunohistochemistry in the differential diagnosis of gynecologic
disorders. Arch Pathol Lab Med. 139:39–54. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Hirsch MS and Watkins J: A comprehensive
review of biomarker use in the gynecologic tract including
differential diagnoses and diagnostic pitfalls. Adv Anat Pathol.
27:164–192. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
McCluggage WG: Immunohistochemical and
functional biomarkers of value in female genital tract lesions. Int
J Gynecol Pathol. 25:101–120. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Semczuk A, Skomra D, Chyzynska M, Szewczuk
W, Olcha P and Korobowicz E: Immunohistochemical analysis of
carcinomatous and sarcomatous components in the uterine
carcinosarcoma: A case report. Pathol Res Pract. 204:203–207. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Semczuk A, Zakrzewski PK, Forma E,
Cygankiewicz AI, Semczuk-Sikora A, Bryś M, Rechberger T and
Krajewska WM: TGFβ-pathway is down-regulated in a uterine
carcinosarcoma: A case study. Pathol Res Pract. 209:740–744. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Semczuk A, Colas E, Walczyna B, Joźwik M,
Pyra A, Semczuk-Sikora A and Rechberger T: Coexistence of
homologous-type cervical carcinosarcoma with endometrioid-type G1
endometrial cancer: A case report with an immunohistochemical
study. Int J Clin Exp Pathol. 7:7191–7195. 2014.PubMed/NCBI
|
|
42
|
Semczuk A, Ignatov A, Obrzut B, Reventos J
and Rechberger T: Role of p53 pathway alterations in uterine
carcinosarcomas (malignant mixed Müllerian tumors). Oncology.
87:193–204. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Semczuk A, Lewkowicz D, Jóźwik M, Mrozek
A, Gogacz M, Semczuk-Sikora A and Rechberger T: Bilateral lymph
node metastases from primary uterine carcinosarcoma: An
immunohistochemical case study. Int J Clin Exp Pathol. 9:8754–8758.
2016.
|
|
44
|
Watanabe M, Shimizu K, Kato H, Imai H,
Nakano H, Sugawa M and Shiraishi T: Carcinosarcoma of the uterus:
Immunohistochemical and genetic analysis of clonality of one case.
Gynecol Oncol. 82:563–567. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
de Jong RA, Nijman HW, Wijbrandi TF,
Reyners AK, Boezen HM and Hollema H: Molecular markers and clinical
behavior of uterine carcinosarcomas: Focus on the epithelial tumor
component. Mod Pathol. 24:1368–1379. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Iwasa Y, Haga H, Konishi I, Kobashi Y,
Higuchi K, Katsuyama E, Minamiguchi S and Yamabe H: Prognostic
factors in uterine carcinosarcoma: A clinicopathologic study of 25
patients. Cancer. 82:512–519. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Sreenan JJ and Hart WR: Carcinosarcomas of
the female genital tract. A pathologic study of 29 metastatic
tumors: Further evidence for the dominant role of the epithelial
component and the conversion theory of histogenesis. Am J Surg
Pathol. 19:666–674. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Bologna-Molina R, Beyoda-Borella AM,
Soria-Moreira L and Soría-Suárez S: Molecular biomarkers of cell
proliferation in amenoblastomas. World J Stomatol. 2:79–85. 2013.
View Article : Google Scholar
|