|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global Cancer Statistics 2020:
GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36
Cancers in 185 Countries. CA Cancer J Clin. 71:209–249. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S,
Kim JS, Luo R, Feng J, Ye S, Yang TS, et al: Efficacy and safety of
sorafenib in patients in the Asia-Pacific region with advanced
hepatocellular carcinoma: A phase III randomised, double-blind,
placebo-controlled trial. Lancet Oncol. 10:25–34. 2009. View Article : Google Scholar
|
|
3
|
Llovet JM, Ricci S, Mazzaferro V, Hilgard
P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A,
et al: Sorafenib in advanced hepatocellular carcinoma. N Engl J
Med. 359:378–390. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cheng A, Qin S, Ikeda M, Galle PR, Ducreux
MP, Zhu AX, Kim T, Kudo M, Breder V, Merle P, et al: Imbrave150:
Efficacy and safety results from a ph III study evaluating
atezolizumab (atezo) + bevacizumab (bev) vs sorafenib (Sor) as
first treatment (tx) for patients (pts) with unresectable
hepatocellular carcinoma (HCC)'. Ann Oncol. 30 (Suppl
9):ix183–ix202. 2019. View Article : Google Scholar
|
|
5
|
Ghouri YA, Mian I and Rowe JH: Review of
hepatocellular carcinoma: Epidemiology, etiology, and
carcinogenesis. J Carcinog. 16:12017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Novikova MV, Khromova NV and Kopnin PB:
Components of the hepatocellular carcinoma microenvironment and
their role in tumor progression. Biochemistry (Mosc). 82:861–873.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jia W, Rajani C, Xu H and Zheng X: Gut
microbiota alterations are distinct for primary colorectal cancer
and hepatocellular carcinoma. Protein Cell. 12:374–393. 2021.
View Article : Google Scholar
|
|
8
|
Kumar V, Patel S, Tcyganov E and
Gabrilovich DI: The nature of myeloid-derived suppressor cells in
the tumor microenvironment. Trends Immunol. 37:208–220. 2016.
View Article : Google Scholar
|
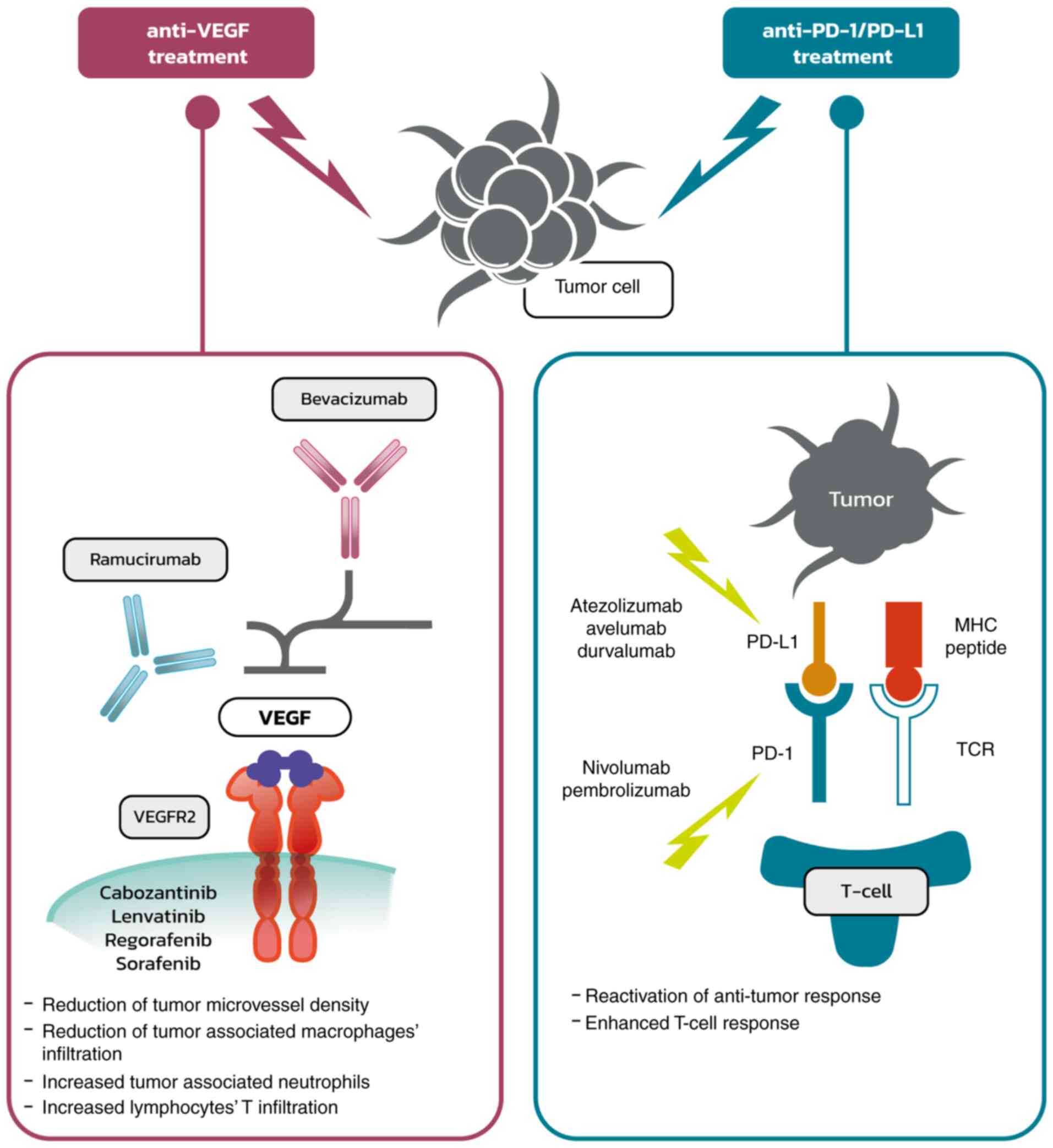
|
9
|
Chiu DK, Tse AP, Xu IM, Di Cui J, Lai RK,
Li LL, Koh HY, Tsang FH, Wei LL, Wong CM, et al: Hypoxia inducible
factor HIF-1 promotes myeloid-derived suppressor cells accumulation
through ENTPD2/CD39L1 in hepatocellular carcinoma. Nat Commun.
8:5172017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hoechst B, Ormandy LA, Ballmaier M, Lehner
F, Krüger C, Manns MP, Greten TF and Korangy F: A new population of
myeloid-derived suppressor cells in hepatocellular carcinoma
patients induces CD4(+)CD25(+)Foxp3(+) T cells. Gastroenterology.
135:234–243. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yang L, DeBusk LM, Fukuda K, Fingleton B,
Green-Jarvis B, Shyr Y, Matrisian LM, Carbone DP and Lin PC:
Expansion of myeloid immune suppressor Gr+CD11b+ cells in
tumor-bearing host directly promotes tumor angiogenesis. Cancer
Cell. 6:409–421. 2004. View Article : Google Scholar
|
|
12
|
Li H, Han Y, Guo Q, Zhang M and Cao X:
Cancer-expanded myeloid-derived suppressor cells induce anergy of
NK cells through membrane-bound TGF-beta 1. J Immunol. 182:240–249.
2009. View Article : Google Scholar
|
|
13
|
Yan W, Liu X, Ma H, Zhang H, Song X, Gao
L, Liang X and Ma C: Tim-3 fosters HCC development by enhancing
TGF-β-mediated alternative activation of macrophages. Gut.
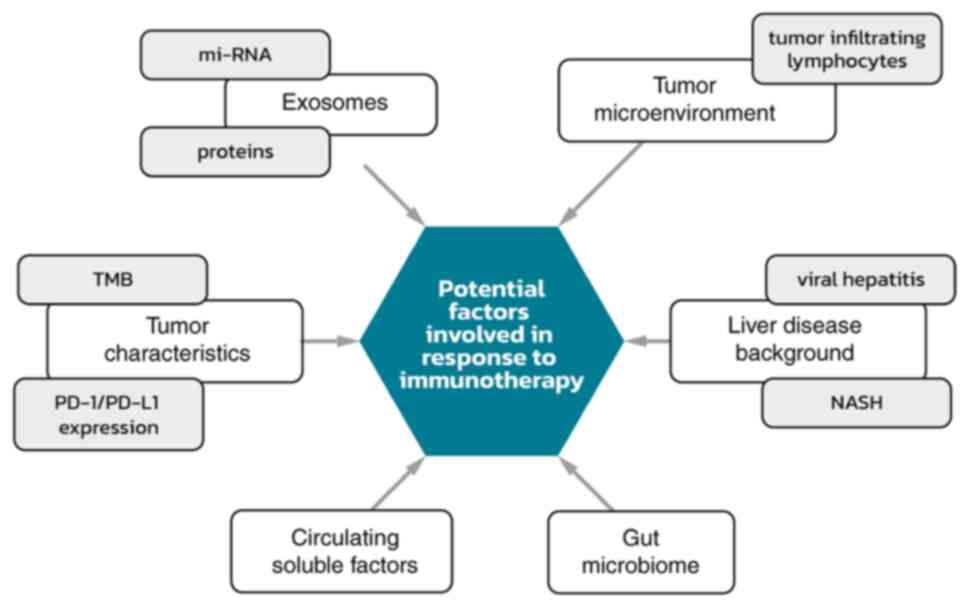
64:1593–1604. 2015. View Article : Google Scholar
|
|
14
|
Chang CJ, Yang YH, Chiu CJ, Lu LC, Liao
CC, Liang CW, Hsu CH and Cheng AL: Targeting tumor-infiltrating
Ly6G+ myeloid cells improves sorafenib efficacy in mouse
orthotopic hepatocellular carcinoma. Int J Cancer. 142:1878–1889.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mantovani A, Bottazzi B, Colotta F,
Sozzani S and Ruco L: The origin and function of tumor-associated
macrophages. Immunol Today. 13:265–270. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gordon S and Taylor PR: Monocyte and
macrophage heterogeneity. Nat Rev Immunol. 5:953–964. 2005.
View Article : Google Scholar
|
|
17
|
Martinez FO and Gordon S: The M1 and M2
paradigm of macrophage activation: Time for reassessment.
F1000Prime Rep. 6:132014. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhou D, Huang C, Lin Z, Zhan S, Kong L,
Fang C and Li J: Macrophage polarization and function with emphasis
on the evolving roles of coordinated regulation of cellular
signaling pathways. Cell Signal. 26:192–197. 2014. View Article : Google Scholar
|
|
19
|
Solinas G, Germano G, Mantovani A and
Allavena P: Tumor-associated macrophages (TAM) as major players of
the cancer-related inflammation. J Leukoc Biol. 86:1065–1073. 2009.
View Article : Google Scholar
|
|
20
|
Yao Y, Xu XH and Jin L: Macrophage
polarization in physiological and pathological pregnancy. Front
Immunol. 10:7922019. View Article : Google Scholar
|
|
21
|
Wan S, Kuo N, Kryczek I, Zou W and Welling
TH: Myeloid cells in hepatocellular carcinoma. Hepatology.
62:1304–1312. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wang J, Li D, Cang H and Guo B: Crosstalk
between cancer and immune cells: Role of tumor-associated
macrophages in the tumor microenvironment. Cancer Med. 8:4709–4721.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Guo B, Li L, Guo J, Liu A, Wu J, Wang H,
Shi J, Pang D and Cao Q: M2 tumor-associated macrophages produce
interleukin-17 to suppress oxaliplatin-induced apoptosis in
hepatocellular carcinoma. Oncotarget. 8:44465–44476. 2017.
View Article : Google Scholar
|
|
24
|
Fu XT, Song K, Zhou J, Shi YH, Liu WR, Shi
GM, Gao Q, Wang XY, Ding ZB and Fan J: Tumor-associated macrophages
modulate resistance to oxaliplatin via inducing autophagy in
hepatocellular carcinoma. Cancer Cell Int. 19:712019. View Article : Google Scholar
|
|
25
|
Zhang J, Chang L, Zhang X, Zhou Z and Gao
Y: Meta-analysis of the prognostic and clinical value of
tumor-associated macrophages in hepatocellular carcinoma. J Invest
Surg. 34:297–306. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zong Z, Zou J, Mao R, Ma C, Li N, Wang J,
Wang X, Zhou H, Zhang L and Shi Y: M1 macrophages induce PD-L1
expression in hepatocellular carcinoma cells through IL-1β
signaling. Front Immunol. 10:16432019. View Article : Google Scholar
|
|
27
|
Ding W, Tan Y, Qian Y, Xue W, Wang Y,
Jiang P and Xu X: Clinicopathologic and prognostic significance of
tumor-associated macrophages in patients with hepatocellular
carcinoma: A meta-analysis. PLoS One. 14:e02239712019. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lau J, Cheung J, Navarro A, Lianoglou S,
Haley B, Totpal K, Sanders L, Koeppen H, Caplazi P, McBride J, et
al: Tumour and host cell PD-L1 is required to mediate suppression
of anti-tumour immunity in mice. Nat Commun. 8:145722017.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Umezu D, Okada N, Sakoda Y, Adachi K,
Ojima T, Yamaue H, Eto M and Tamada K: Inhibitory functions of
PD-L1 and PD-L2 in the regulation of anti-tumor immunity in murine
tumor microenvironment. Cancer Immunol Immunother. 68:201–211.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Dong N, Shi X, Wang S, Gao Y, Kuang Z, Xie
Q, Li Y, Deng H, Wu Y, Li M and Li JL: M2 macrophages mediate
sorafenib resistance by secreting HGF in a feed-forward manner in
hepatocellular carcinoma. Br J Cancer. 121:22–33. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zhou DY, Qin J, Huang J, Wang F, Xu GP, Lv
YT, Zhang JB and Shen LM: Zoledronic acid inhibits infiltration of
tumor-associated macrophages and angiogenesis following
transcatheter arterial chemoembolization in rat hepatocellular
carcinoma models. Oncol Lett. 14:4078–4084. 2017. View Article : Google Scholar
|
|
32
|
Ao JY, Zhu XD, Chai ZT, Cai H, Zhang YY,
Zhang KZ, Kong LQ, Zhang N, Ye BG, Ma DN and Sun HC:
Colony-stimulating factor 1 receptor blockade inhibits tumour
growth by altering the polarization of tumour-associated
macrophages in hepatocellular carcinoma. Mol Cancer Ther.
16:1544–1554. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Sun S, Cui Y, Ren K, Quan M, Song Z, Zou
H, Li D, Zheng Y and Cao J: 8-bromo-7-methoxychrysin reversed M2
polarization of tumour-associated macrophages induced by liver
cancer stem-like cells. Anticancer Agents Med Chem. 17:286–293.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Wan S, Zhao E, Kryczek I, Vatan L,
Sadovskaya A, Ludema G, Simeone DM, Zou W and Welling TH:
Tumor-associated macrophages produce interleukin 6 and signal via
STAT3 to promote expansion of human hepatocellular carcinoma stem
cells. Gastroenterology. 147:1393–1404. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Li X, Yao W, Yuan Y, Chen P, Li B, Li J,
Chu R, Song H, Xie D, Jiang X and Wang H: Targeting of
tumour-infiltrating macrophages via CCL2/CCR2 signalling as a
therapeutic strategy against hepatocellular carcinoma. Gut.
66:157–167. 2017. View Article : Google Scholar
|
|
36
|
Yao W, Ba Q, Li X, Li H, Zhang S, Yuan Y,
Wang F, Duan X, Li J, Zhang W and Wang H: A natural CCR93
antagonist relieves tumour-associated macrophage-mediated
immunosuppression to produce a therapeutic effect for liver cancer.
EBioMedicine. 22:58–67. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Zhang JP, Yan J, Xu J, Pang XH, Chen MS,
Li L, Wu C, Li SP and Zheng L: Increased intratumoral
IL-17-producing cells correlate with poor survival in
hepatocellular carcinoma patients. J Hepatol. 50:980–989. 2009.
View Article : Google Scholar
|
|
38
|
Flecken T, Schmidt N, Hild S, Gostick E,
Drognitz O, Zeiser R, Schemmer P, Bruns H, Eiermann T, Price DA, et
al: Immunodominance and functional alterations of tumor-associated
antigen-specific CD8+ T-cell responses in hepatocellular carcinoma.
Hepatology. 59:1415–1426. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Ringelhan M, Pfister D, O'Connor T,
Pikarsky E and Heikenwalder M: The immunology of hepatocellular
carcinoma. Nat Immunol. 19:222–232. 2018. View Article : Google Scholar
|
|
40
|
Khan O, Giles JR, McDonald S, Manne S,
Ngiow SF, Patel KP, Werner MT, Huang AC, Alexander KA, Wu JE, et
al: TOX transcriptionally and epigenetically programs
CD8+ T cell exhaustion. Nature. 571:211–218. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Blackburn SD, Shin H, Haining WN, Zou T,
Workman CJ, Polley A, Betts MR, Freeman GJ, Vignali DA and Wherry
EJ: Coregulation of CD8+ T cell exhaustion by multiple inhibitory
receptors during chronic viral infection. Nat Immunol. 10:29–37.
2009. View Article : Google Scholar
|
|
42
|
Wherry EJ and Kurachi M: Molecular and
cellular insights into T cell exhaustion. Nat Rev Immunol.
15:486–499. 2015. View Article : Google Scholar
|
|
43
|
Kim HD, Song GW, Park S, Jung MK, Kim MH,
Kang HJ, Yoo C, Yi K, Kim KH, Eo S, et al: Association between
expression level of PD1 by tumor-infiltrating CD8(+) T cells and
features of hepatocellular carcinoma. Gastroenterology.
155:1936–1950.e17. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Gao Q, Qiu SJ, Fan J, Zhou J, Wang XY,
Xiao YS, Xu Y, Li YW and Tang ZY: Intratumoral balance of
regulatory and cytotoxic T cells is associated with prognosis of
hepatocellular carcinoma after resection. J Clin Oncol.
25:2586–2593. 2007. View Article : Google Scholar
|
|
45
|
Fu J, Xu D, Liu Z, Shi M, Zhao P, Fu B,
Zhang Z, Yang H, Zhang H, Zhou C, et al: Increased regulatory T
cells correlate with CD8 T-cell impairment and poor survival in
hepatocellular carcinoma patients. Gastroenterology. 132:2328–2339.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Sideras K, Biermann K, Verheij J,
Takkenberg BR, Mancham S, Hansen BE, Schutz HM, de Man RA,
Sprengers D, Buschow SI, et al: PD-L1, Galectin-9 and
CD8+ tumor-infiltrating lymphocytes are associated with
survival in hepatocellular carcinoma. OncoImmunology.
6:e12733092017. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Kang HJ, Oh JH, Chun SM, Kim D, Ryu YM,
Hwang HS, Kim SY, An J, Cho EJ, Lee H, et al: Immunogenomic
landscape of hepatocellular carcinoma with immune cell stroma and
EBV-positive tumor-infiltrating lymphocytes. J Hepatol. 71:91–103.
2019. View Article : Google Scholar
|
|
48
|
Cariani E and Missale G: Immune landscape
of hepatocellular carcinoma microenvironment: Implications for
prognosis and therapeutic applications. Liver Int. 39:1608–1621.
2019. View Article : Google Scholar
|
|
49
|
Zhou SL, Zhou ZJ, Hu ZQ, Huang XW, Wang Z,
Chen EB, Fan J, Cao Y, Dai Z and Zhou J: Tumor-Associated
Neutrophils Recruit Macrophages and T-Regulatory Cells to Promote
Progression of Hepatocellular Carcinoma and Resistance to
Sorafenib. Gastroenterology. 150:1646–1658.e17. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Zhou SL, Yin D, Hu ZQ, Luo CB, Zhou ZJ,
Xin HY, Yang XR, Shi YH, Wang Z, Huang XW, et al: A positive
feedback loop between cancer stem-like cells and tumor-associated
neutrophils controls hepatocellular carcinoma progression.
Hepatology. 70:1214–1230. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Zhang W, Zhu XD, Sun HC, Xiong YQ, Zhuang
PY, Xu HX, Kong LQ, Wang L, Wu WZ and Tang ZY: Depletion of
tumor-associated macrophages enhances the effect of sorafenib in
metastatic liver cancer models by antimetastatic and antiangiogenic
effects. Clin Cancer Res. 16:3420–3430. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Tian XP, Wang CY, Jin XH, Li M, Wang FW,
Huang WJ, Yun JP, Xu RH, Cai QQ and Xie D: Acidic microenvironment
up-regulates exosomal miR-21 and miR-10b in early-stage
hepatocellular carcinoma to promote cancer cell proliferation and
metastasis. Theranostics. 9:1965–1979. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Gao X, Huang H, Wang Y, Pan C, Yin S, Zhou
L and Zheng S: Tumor immune microenvironment characterization in
hepatocellular carcinoma identifies four prognostic and
immunotherapeutically relevant subclasses. Front Oncol.
10:6105132021. View Article : Google Scholar
|
|
54
|
Budimir N, Thomas GD, Dolina JS and
Salek-Ardakani S: Reversing T-cell exhaustion in cancer: Lessons
learned from PD-1/PD-L1 immune checkpoint blockade. Cancer Immunol
Res. 10:146–153. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Kato Y, Tabata K, Kimura T,
Yachie-Kinoshita A, Ozawa Y, Yamada K, Ito J, Tachino S, Hori Y,
Matsuki M, et al: Lenvatinib plus anti-PD-1 antibody combination
treatment activates CD8+ T cells through reduction of
tumor-associated macrophage and activation of the interferon
pathway. PLoS One. 14:e02125132019. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Lu M, Zhang X, Gao X, Sun S, Wei X, Hu X,
Huang C, Xu H, Wang B, Zhang W, et al: Lenvatinib enhances T cell
immunity and the efficacy of adoptive chimeric antigen
receptor-modified T cells by decreasing myeloid-derived suppressor
cells in cancer. Pharmacol Res. 174:1058292021. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Huang X, Xu L, Ma T, Yin X, Huang Z, Ran
Y, Ni Y, Bi X and Che X: Lenvatinib plus immune checkpoint
inhibitors improve survival in advanced hepatocellular carcinoma: A
Retrospective Study. Front Oncol. 11:7511592021. View Article : Google Scholar
|
|
58
|
Wang BJ, Bao JJ, Wang JZ, Wang Y, Jiang M,
Xing MY, Zhang WG, Qi JY, Roggendorf M, Lu MJ and Yang DL:
Immunostaining of PD-1/PD-Ls in liver tissues of patients with
hepatitis and hepatocellular carcinoma. World J Gastroenterol.
17:3322–3329. 2011. View Article : Google Scholar
|
|
59
|
Garon EB, Rizvi NA, Hui R, Leighl N,
Balmanoukian AS, Eder JP, Patnaik A, Aggarwal C, Gubens M, Horn L,
et al: Pembrolizumab for the treatment of non-small-cell lung
cancer. N Engl J Med. 372:2018–2028. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Lin H, Wei S, Hurt EM, Green MD, Zhao L,
Vatan L, Szeliga W, Herbst R, Harms PW, Fecher LA, et al: Host
expression of PD-L1 determines efficacy of PD-L1 pathway
blockade-mediated tumor regression. J Clin Invest. 128:805–815.
2018. View Article : Google Scholar
|
|
61
|
Calderaro J, Rousseau B, Amaddeo G, Mercey
M, Charpy C, Costentin C, Luciani A, Zafrani ES, Laurent A, Azoulay
D, et al: Programmed death ligand 1 expression in hepatocellular
carcinoma: Relationship With clinical and pathological features.
Hepatology. 64:2038–2046. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Teng MW, Ngiow SF, Ribas A and Smyth MJ:
Classifying cancers based on T-cell infiltration and PD-L1. Cancer
Res. 75:2139–2145. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Woo SR, Turnis ME, Goldberg MV, Bankoti J,
Selby M, Nirschl CJ, Bettini ML, Gravano DM, Vogel P, Liu CL, et
al: Immune inhibitory molecules LAG-3 and PD-1 synergistically
regulate T-cell function to promote tumoral immune escape. Cancer
Res. 72:917–927. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Kurebayashi Y, Ojima H, Tsujikawa H,
Kubota N, Maehara J, Abe Y, Kitago M, Shinoda M, Kitagawa Y and
Sakamoto M: Landscape of immune microenvironment in hepatocellular
carcinoma and its additional impact on histological and molecular
classification. Hepatology. 68:1025–1041. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Abdou Y, Pandey M, Sarma M, Shah S, Baron
J and Ernstoff MS: Mechanism-based treatment of cancer with immune
checkpoint inhibitor therapies. Br J Clin Pharmacol. 86:1690–1702.
2020. View Article : Google Scholar
|
|
66
|
European Medicine Agency, . Bevacizumab,
Avastin Summary of Product Characteristics. https://www.ema.europa.eu/en/documents/product-information/avastin-epar-product-information_en.pdfJune
12–2022
|
|
67
|
European Medicine Agency, . Atezolizumab
Summary of Product Characteristics. June 12–2022
|
|
68
|
Roland CL, Dineen SP, Lynn KD, Sullivan
LA, Dellinger MT, Sadegh L, Sullivan JP, Shames DS and Brekken RA:
Inhibition of vascular endothelial growth factor reduces
angiogenesis and modulates immune cell infiltration of orthotopic
breast cancer xenografts. Mol Cancer Ther. 8:1761–1771. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Voron T, Colussi O, Marcheteau E, Pernot
S, Nizard M, Pointet AL, Latreche S, Bergaya S, Benhamouda N,
Tanchot C, et al: VEGF-A modulates expression of inhibitory
checkpoints on CD8+ T cells in tumors. J Exp Med. 212:139–148.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Finn RS, Qin S, Ikeda M, Galle PR, Ducreux
M, Kim TY, Kudo M, Breder V, Merle P, Kaseb AO, et al: Atezolizumab
plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J
Med. 382:1894–1905. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Yau T, Park JW, Finn RS, Cheng AL,
Mathurin P, Edeline J, Kudo M, Harding JJ, Merle P, Rosmorduc O, et
al: Nivolumab versus sorafenib in advanced hepatocellular carcinoma
(CheckMate 459): a randomised, multicentre, open-label, phase 3
trial. Lancet Oncol. 23:77–90. 2022. View Article : Google Scholar
|
|
72
|
Yau T, Kang YK, Kim TY, El-Khoueiry AB,
Santoro A, Sangro B, Melero I, Kudo M, Hou MM, Matilla A, et al:
Efficacy and safety of nivolumab plus ipilimumab in patients with
advanced hepatocellular carcinoma previously treated with
sorafenib: The checkmate 040 randomized clinical trial. JAMA Oncol.
6:e2045642020. View Article : Google Scholar
|
|
73
|
European Medicine Agency, . Pembrolizumab
Summary of Product Characteristics. https://www.ema.europa.eu/en/documents/product-information/keytruda-epar-product-information_en.pdfJune
12–2022
|
|
74
|
Zhu AX, Finn RS, Edeline J, Cattan S,
Ogasawara S, Palmer D, Verslype C, Zagonel V, Fartoux L, Vogel A,
et al: Pembrolizumab in patients with advanced hepatocellular
carcinoma previously treated with sorafenib (KEYNOTE-224): A
non-randomised, open-label phase 2 trial. Lancet Oncol. 19:940–952.
2018. View Article : Google Scholar
|
|
75
|
Finn RS, Ryoo BY, Merle P, Kudo M,
Bouattour M, Lim HY, Breder V, Edeline J, Chao Y, Ogasawara S, et
al: Pembrolizumab as second-line therapy in patients with advanced
hepatocellular carcinoma in KEYNOTE-240: A randomized,
double-blind, phase III trial. J Clin Oncol. 38:193–202. 2020.
View Article : Google Scholar
|
|
76
|
Kelley RK, Sangro B, Harris W, Ikeda M,
Okusaka T, Kang YK, Qin S, Tai DW, Lim HY, Yau T, et al: Safety,
efficacy, and pharmacodynamics of tremelimumab plus durvalumab for
patients with unresectable hepatocellular carcinoma: Randomized
expansion of a phase I/II study. J Clin Oncol. 39:2991–3001. 2021.
View Article : Google Scholar
|
|
77
|
U.S. National Library of Medicine (NIH), .
Study of Durvalumab and Tremelimumab as First-line Treatment in
Patients With Advanced Hepatocellular Carcinoma (HIMALAYA).
ClinicalTrials.gov Identifier: NCT03298451. NIH; Bethesda, MD:
2017, https://clinicaltrials.gov/ct2/show/NCT03298451April
19–2021
|
|
78
|
U.S. National Library of Medicine (NIH), .
Combination Therapy of Microwave Ablation and Cellular
Immunotherapy for Hepatocellular Carcinoma. ClinicalTrials.gov
Identifier: NCT02851784. NIH; Bethesda, MD: 2016, https://clinicaltrials.gov/ct2/show/NCT02851784November
20–2021
|
|
79
|
U.S. National Library of Medicine (NIH), .
Hepatocellular Carcinoma Study Comparing Vaccinia Virus Based
Immunotherapy Plus Sorafenib vs Sorafenib Alone (PHOCUS).
ClinicalTrials.gov Identifier: NCT02562755. NIH; Bethesda, MD:
2015, https://clinicaltrials.gov/ct2/show/NCT02562755November
20–2021
|
|
80
|
U.S. National Library of Medicine (NIH), .
FImmunotherapy for Advanced Liver Cancer (ALIVE).
ClinicalTrials.gov Identifier: NCT05033522. NIH; Bethesda, MD:
2021, https://clinicaltrials.gov/ct2/show/NCT05033522November
20–2021
|
|
81
|
U.S. National Library of Medicine (NIH), .
An Investigational Immuno-therapy Study of Nivolumab Compared to
Sorafenib as a First Treatment in Patients With Advanced
Hepatocellular Carcinoma. ClinicalTrials.gov Identifier:
NCT02576509. NIH; Bethesda, MD: 2015, https://clinicaltrials.gov/ct2/show/NCT02576509November
20–2021
|
|
82
|
U.S. National Library of Medicine (NIH), .
RRFA+Highly-purified CTL vs. RFA Alone for Recurrent HCC.
ClinicalTrials.gov Identifier: NCT02678013. NIH; Bethesda, MD:
2016, https://clinicaltrials.gov/ct2/show/NCT02678013November
20–2021
|
|
83
|
U.S. National Library of Medicine (NIH), .
Combination of Sintilimab and Stereotactic Body Radiotherapy in
Hepatocellular Carcinoma (ISBRT01) (ISBRT01). ClinicalTrials.gov
Identifier: NCT04167293. NIH; Bethesda, MD: 2019, https://clinicaltrials.gov/ct2/show/NCT04167293November
20–2021
|
|
84
|
U.S. National Library of Medicine (NIH), .
Infusion of PD1/PDL1 Inhibitor Via Hepatic Arterial Versus Vein for
Immunotherapy of Advanced Hepatocellular Carcinoma.
ClinicalTrials.gov Identifier: NCT03949231. NIH; Bethesda, MD:
2019, https://clinicaltrials.gov/ct2/show/NCT03949231November
20–2021
|
|
85
|
U.S. National Library of Medicine (NIH), .
DEB-TACE Plus Lenvatinib or Sorafenib or PD-1 Inhibitor for
Unresectable Hepatocellular Carcinoma. ClinicalTrials.gov
Identifier: NCT04229355. NIH; Bethesda, MD: 2020, https://clinicaltrials.gov/ct2/show/NCT04229355November
20–2021
|
|
86
|
U.S. National Library of Medicine (NIH), .
Efficacy and Safety of Immuncell-LC Group and Non-treatment Group
in Hepatocelluar Carcinoma Patients. ClinicalTrials.gov Identifier:
NCT00699816. NIH; Bethesda, MD: 2008, https://clinicaltrials.gov/ct2/show/NCT00699816November
20–2021
|
|
87
|
U.S. National Library of Medicine (NIH), .
Resection+Highly Purified CTL Versus Resection Alone for HCC.
ClinicalTrials.gov Identifier: NCT02709070. NIH; Bethesda, MD:
2016, https://clinicaltrials.gov/ct2/show/NCT02709070November
20–2021
|
|
88
|
U.S. National Library of Medicine (NIH), .
Nivolumab in Combination With TACE/TAE for Patients With
Intermediate Stage HCC (TACE-3). ClinicalTrials.gov Identifier:
NCT04268888. NIH; Bethesda, MD: 2020, https://clinicaltrials.gov/ct2/show/NCT04268888November
20–2021
|
|
89
|
U.S. National Library of Medicine (NIH), .
Safety and Efficacy of Pembrolizumab (MK-3475) Versus Placebo as
Adjuvant Therapy in Participants With Hepatocellular Carcinoma
(HCC) and Complete Radiological Response After Surgical Resection
or Local Ablation (MK-3475-937 / KEYNOTE-937). ClinicalTrials.gov
Identifier: NCT03867084. NIH; Bethesda, MD: 2019, https://clinicaltrials.gov/ct2/show/NCT03867084November
20–2021
|
|
90
|
U.S. National Library of Medicine (NIH), .
Sintilimab Plus Bevacizumab as Adjuvant Therapy in HCC Patients at
High Risk of Recurrence After Curative Resection (DaDaLi).
ClinicalTrials.gov Identifier: NCT04682210. NIH; Bethesda, MD:
2020, https://www.clinicaltrials.gov/ct2/show/NCT04682210November
20–2021
|
|
91
|
U.S. National Library of Medicine
(NIH):CIK Treatment for HCC Patient Underwent Radical Resection, .
ClinicalTrials.gov Identifier NCT01749865. NIH; Bethesda, MD: 2012,
https://clinicaltrials.gov/ct2/show/NCT01749865November
20–2021
|
|
92
|
Schwacha-Eipper B, Minciuna I, Banz V and
Dufour JF: Immunotherapy as a downstaging therapy for liver
transplantation. Hepatology. 72:1488–1490. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Tabrizian P, Florman SS and Schwartz ME:
PD-1 inhibitor as bridge therapy to liver transplantation? Am J
Transplant. 21:1979–1980. 2021. View Article : Google Scholar
|
|
94
|
Tanimine N, Tanaka Y, Ishiyama K, Ohira M,
Shimizu S, Yano T and Ohdan H: Adoptive Immunotherapy with Liver
allograft-derived NK Cells Improves Recurrence-free Survival after
Living-donor Liver Transplantation in Patients with Hepatocellular
Carcinoma. Am J Transplant. 15 (Suppl 3):3172015.
|
|
95
|
Pandey A and Cohen DJ: Ipilumumab for
hepatocellular cancer in a liver transplant recipient, with durable
response, tolerance and without allograft rejection. Immunotherapy.
12:287–292. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Luo Y, Teng F, Fu H and Ding GS:
Immunotherapy in liver transplantation for hepatocellular
carcinoma: Pros and cons. World J Gastrointest Oncol. 14:163–180.
2022. View Article : Google Scholar
|
|
97
|
Burtness B, Harrington KJ, Greil R,
Soulières D, Tahara M, de Castro G Jr, Psyrri A, Basté N, Neupane
P, Bratland Å, et al: Pembrolizumab alone or with chemotherapy
versus cetuximab with chemotherapy for recurrent or metastatic
squamous cell carcinoma of the head and neck (KEYNOTE-048): A
randomised, open-label, phase 3 study. Lancet. 394:1915–1928. 2019.
View Article : Google Scholar
|
|
98
|
Daud AI, Wolchok JD, Robert C, Hwu WJ,
Weber JS, Ribas A, Hodi FS, Joshua AM, Kefford R, Hersey P, et al:
Programmed Death-Ligand 1 expression and response to the
anti-programmed death 1 antibody pembrolizumab in melanoma. J Clin
Oncol. 34:4102–4109. 2016. View Article : Google Scholar
|
|
99
|
Tian P, He B, Mu W, Liu K, Liu L, Zeng H,
Liu Y, Jiang L, Zhou P, Huang Z, et al: Assessing PD-L1 expression
in non-small cell lung cancer and predicting responses to immune
checkpoint inhibitors using deep learning on computed tomography
images. Theranostics. 11:2098–2107. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Feun LG, Li YY, Wu C, Wangpaichitr M,
Jones PD, Richman SP, Madrazo B, Kwon D, Garcia-Buitrago M, Martin
P, et al: Phase 2 study of pembrolizumab and circulating biomarkers
to predict anticancer response in advanced, unresectable
hepatocellular carcinoma. Cancer. 125:3603–3614. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Zhang H, Li XX, Yang Y, Zhang Y, Wang HY
and Zheng XFS: Significance and mechanism of androgen receptor
overexpression and androgen receptor/mechanistic target of
rapamycin cross-talk in hepatocellular carcinoma. Hepatology.
67:2271–2286. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Azuma K, Ota K, Kawahara A, Hattori S,
Iwama E, Harada T, Matsumoto K, Takayama K, Takamori S, Kage M, et
al: Association of PD-L1 overexpression with activating EGFR
mutations in surgically resected nonsmall-cell lung cancer. Ann
Oncol. 25:1935–1940. 2014. View Article : Google Scholar
|
|
103
|
Taube JM, Klein A, Brahmer JR, Xu H, Pan
X, Kim JH, Chen L, Pardoll DM, Topalian SL and Anders RA:
Association of PD-1, PD-1 ligands, and other features of the tumour
immune microenvironment with response to anti-PD-1 therapy. Clin
Cancer Res. 20:5064–5074. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Macek Jilkova Z, Aspord C, Kurma K, Granon
A, Sengel C, Sturm N, Marche PN and Decaens T: Immunologic features
of patients with advanced hepatocellular carcinoma before and
during sorafenib or anti-programmed death-1/programmed death-L1
treatment. Clin Transl Gastroenterol. 10:e000582019. View Article : Google Scholar
|
|
105
|
Kleinovink JW, van Hall T, Ossendorp F and
Fransen MF: PD-L1 immune suppression in cancer: Tumor cells or host
cells? OncoImmunology. 6:e13259822017. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Vilain RE, Menzies AM, Wilmott JS,
Kakavand H, Madore J, Guminski A, Liniker E, Kong BY, Cooper AJ,
Howle JR, et al: Dynamic changes in PD-L1 expression and immune
infiltrates early during treatment predict response to PD-1
blockade in melanoma. Clin Cancer Res. 23:5024–5033. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Sia D, Jiao Y, Martinez-Quetglas I, Kuchuk
O, Villacorta-Martin C, Castro de Moura M, Putra J, Camprecios G,
Bassaganyas L, Akers N, et al: Identification of an immune-specific
class of hepatocellular carcinoma, based on molecular features.
Gastroenterology. 153:812–826. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Chang B, Shen L, Wang K, Jin J, Huang T,
Chen Q, Li W and Wu P: High number of PD-1 positive intratumoural
lymphocytes predicts survival benefit of cytokine-induced killer
cells for hepatocellular carcinoma patients. Liver Int.
38:1449–1458. 2018. View Article : Google Scholar
|
|
109
|
Ding Z, Dong Z, Chen Z, Hong J, Yan L, Li
H, Yao S, Yan Y, Yang Y, Yang C and Li T: Viral status and efficacy
of immunotherapy in hepatocellular carcinoma: A systematic review
with meta-analysis. Front Immunol. 12:7335302021. View Article : Google Scholar
|
|
110
|
Pfister D, Núñez NG, Pinyol R, Govaere O,
Pinter M, Szydlowska M, Gupta R, Qiu M, Deczkowska A, Weiner A, et
al: NASH limits anti-tumour surveillance in immunotherapy-treated
HCC. Nature. 592:450–456. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Zheng Y, Wang T, Tu X, Huang Y, Zhang H,
Tan D, Jiang W, Cai S, Zhao P, Song R, et al: Gut microbiome
affects the response to anti-PD-1 immunotherapy in patients with
hepatocellular carcinoma. J Immunother Cancer. 7:1932019.
View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Sasaki R, Kanda T, Yokosuka O, Kato N,
Matsuoka S and Moriyama M: Exosomes and hepatocellular carcinoma:
From bench to bedside. Int J Mol Sci. 20:14062019. View Article : Google Scholar
|
|
113
|
Hao J, Liang C and Jiao B: Eukaryotic
translation initiation factor 3, subunit C is overexpressed and
promotes cell proliferation in human glioma U-87 MG cells. Oncol
Lett. 9:2525–2533. 2015. View Article : Google Scholar
|
|
114
|
Lin XJ, Fang JH, Yang XJ, Zhang C, Yuan Y,
Zheng L and Zhuang SM: Hepatocellular carcinoma cell-secreted
exosomal MicroRNA-210 promotes angiogenesis in vitro and in vivo.
Mol Ther Nucleic Acids. 11:243–252. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Tai YL, Chen KC, Hsieh JT and Shen TL:
Exosomes in cancer development and clinical applications. Cancer
Sci. 109:2364–2374. 2018. View Article : Google Scholar
|
|
116
|
Wang G, Liu W, Zou Y, Wang G, Deng Y, Luo
J, Zhang Y, Li H, Zhang Q, Yang Y and Chen G: Three isoforms of
exosomal circPTGR1 promote hepatocellular carcinoma metastasis via
the miR449a-MET pathway. EBioMedicine. 40:432–445. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Ang C, Klempner SJ, Ali SM, Madison R,
Ross JS, Severson EA, Fabrizio D, Goodman A, Kurzrock R, Suh J and
Millis SZ: Prevalence of established and emerging biomarkers of
immune checkpoint inhibitor response in advanced hepatocellular
carcinoma. Oncotarget. 10:4018–4025. 2019. View Article : Google Scholar
|
|
118
|
Chen F, Wang J, Wu Y, Gao Q and Zhang S:
Potential biomarkers for liver cancer diagnosis based on
multi-omics strategy. Front Oncol. 12:8224492022. View Article : Google Scholar
|
|
119
|
Dominguez DA and Wang XW: Impact of
next-generation sequencing on outcomes in hepatocellular carcinoma:
How precise are we really? J Hepatocell Carcinoma. 7:33–37. 2020.
View Article : Google Scholar
|
|
120
|
Harding JJ, Nandakumar S, Armenia J,
Khalil DN, Albano M, Ly M, Shia J, Hechtman JF, Kundra R, El Dika
I, et al: Prospective genotyping of hepatocellular carcinoma:
Clinical Implications of next-generation sequencing for matching
patients to targeted and immune therapies. Clin Cancer Res.
25:2116–2126. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Lee PC, Chao Y, Chen MH, Lan KH, Lee CJ,
Lee IC, Chen SC, Hou MC and Huang YH: Predictors of response and
survival in immune checkpoint inhibitor-treated unresectable
hepatocellular carcinoma. Cancers (Basel). 12:1822020. View Article : Google Scholar
|
|
122
|
Kim JY, Kronbichler A, Eisenhut M, Hong
SH, van der Vliet HJ, Kang J, Shin JI and Gamerith G: Tumour
mutational burden and efficacy of immune checkpoint inhibitors: A
systematic review and meta-analysis. Cancers (Basel). 11:17982019.
View Article : Google Scholar
|