|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kroeger PT Jr and Drapkin R: Pathogenesis
and heterogeneity of ovarian cancer. Curr Opin Obstet Gynecol.
29:26–34. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
De Leo A, Santini D, Ceccarelli C,
Santandrea G, Palicelli A, Acquaviva G, Chiarucci F, Rosini F,
Ravegnini G, Pession A, et al: What is new on ovarian carcinoma:
Integrated morphologic and molecular analysis following the new
2020 World Health Organization classification of female genital
tumors. Diagnostics (Basel). 11:6972021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kenda Suster N and Virant-Klun I: Presence
and role of stem cells in ovarian cancer. World J Stem Cells.
11:383–397. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nebgen DR, Lu KH and Bast RC Jr: Novel
approaches to ovarian cancer screening. Curr Oncol Rep. 21:752019.
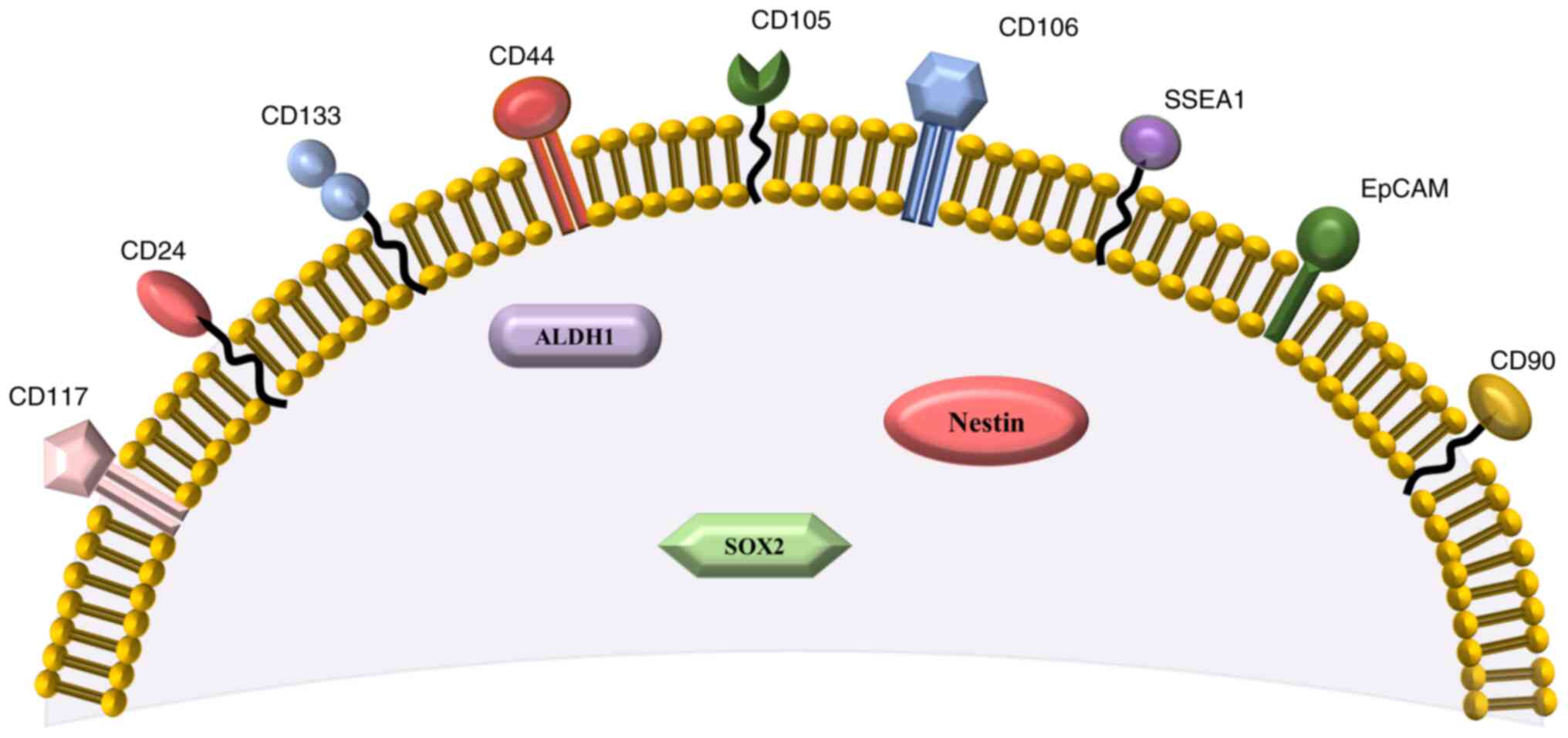
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kujawa KA and Lisowska KM: Ovarian
cancer-from biology to clinic. Postepy Hig Med. Dosw (online).
69:1275–1290. 2015.(In Polish). View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Stewart C, Ralyea C and Lockwood S:
Ovarian cancer: An integrated review. Semin Oncol Nurs. 35:151–156.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ottevanger PB: Ovarian cancer stem cells
more questions than answers. Semin Cancer Biol. 44:67–71. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cortez AJ, Tudrej P, Kujawa KA and
Lisowska KM: Advances in ovarian cancer therapy. Cancer Chemother
Pharmacol. 81:17–38. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Valabrega G, Scotto G, Tuninetti V, Pani A
and Scaglione F: Differences in PARP inhibitors for the treatment
of ovarian cancer: Mechanisms of action, pharmacology, safety, and
efficacy. Int J Mol Sci. 22:42032021. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liu L, Cai S, Han C, Banerjee A, Wu D, Cui
T, Xie G, Zhang J, Zhang X, McLaughlin E, et al: ALDH1A1
contributes to PARP inhibitor resistance via enhancing DNA repair
in BRCA2−/− ovarian cancer cells. Mol Cancer Ther.
19:199–210. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pan Y, Ma S, Cao K, Zhou S, Zhao A, Li M,
Qian F and Zhu C: Therapeutic approaches targeting cancer stem
cells. J Cancer Res Ther. 14:1469–1475. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Rich JN: Cancer stem cells: Understanding
tumour hierarchy and heterogeneity. Medicine (Baltimore). 95 (Suppl
1):S2–S7. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Plaks V, Kong N and Werb Z: The cancer
stem cell niche: How essential is the niche in regulating stemness
of tumor cells? Cell Stem Cell. 16:225–238. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Afify SM and Seno M: Conversion of stem
cells to cancer stem cells: Undercurrent of cancer initiation.
Cancers (Basel). 11:3452019. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Szaryńska M and Kmieć Z: The role of
cancer stem cells in pathogenesis and therapy of cancer. Forum Med
Rodz. 5:47–56. 2011.
|
|
17
|
Melzer C, von der Ohe J, Lehnert H,
Ungefroren H and Hass R: Cancer stem cell niche models and
contribution by mesenchymal stroma/stem cells. Mol Cancer.
16:282017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wang T, Shigdar S, Gantier MP, Hou Y, Wang
L, Li Y, Shamaileh HA, Yin W, Zhou SF, Zhao X and Duan W: Cancer
stem cell targeted therapy: Progress amid controversies.
Oncotarget. 6:44191–44206. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Markowska J, Kojs Z and Twardawa D: Cancer
stem cells in targeted therapy. Curr Gynecol Oncol. 16:96–100.
2018. View Article : Google Scholar
|
|
20
|
Islam F, Qiao B, Smith RA, Gopalan V and
Lam AK: Cancer stem cell: fundamental experimental pathological
concepts and updates. Exp Mol Pathol. 98:184–191. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Atashzar MR, Baharlou R, Karami J,
Abdollahi H, Rezaei R, Pourramezan F and Zoljalali Moghaddam SH:
Cancer stem cells: A review from origin to therapeutic
implications. J Cell Physiol. 235:790–803. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nimmakayala RK, Batra SK and Ponnusamy MP:
Unraveling the journey of cancer stem cells from origin to
metastasis. Biochim Biophys Acta Rev Cancer. 1871:50–63. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wang H and Unternaehrer JJ:
Epithelial-mesenchymal transition and cancer stem cells: At the
crossroads of differentiation and dedifferentiation. Dev Dyn.
248:10–20. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bar JK, Grelewski P, Lis-Nawara A and
Drobnikowska K: The role of cancer stem cells in progressive growth
and resistance of ovarian cancer: True or fiction? Postepy Hig Med
Dosw (Online). 69:1077–1086. 2015.(In Polish). PubMed/NCBI
|
|
25
|
Huang R and Rofstad EK: Cancer stem cells
(CSCs), cervical CSCs and targeted therapies. Oncotarget.
8:35351–35367. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Al-Alem LF, Pandya UM, Baker AT, Bellio C,
Zarrella BD, Clark J, DiGloria CM and Rueda BR: Ovarian cancer stem
cells: What progress have we made? Int J Biochem Cell Biol.
107:92–103. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Lathia JD and Liu H: Overview of cancer
stem cells and stemness for community oncologists. Target Oncol.
12:387–399. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wan Kamarul Zaman WS, Nurul AA and Nordin
F: Stem cells and cancer stem cells: The Jekyll and Hyde scenario
and their implications in stem cell therapy. Biomedicines.
9:12452021. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Prieto-Vila M, Takahashi RU, Usuba W,
Kohama I and Ochiya T: Drug resistance driven by cancer stem cells
and their niche. Int J Mol Sci. 18:25742017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Bighetti-Trevisan RL, Sousa LO, Castilho
RM and Almeida LO: Cancer stem cells: Powerful targets to improve
current anticancer therapeutics. Stem Cells Int. 2019:96180652019.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Helbrecht I, Szymanski Ł, Fiedorowicz M,
Matak D, Bartnik E, Golik P, Szczylik C and Czarnecka AM: Isolation
of renal cancer stem cells. Postępy Biologii Komórki. 45:115–134.
2018.
|
|
32
|
Bandhavkar S: Cancer stem cells: A
metastasizing menace! Cancer Med. 5:649–655. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Codd AS, Kanaseki T, Torigo T and Tabi Z:
Cancer stem cells as targets for immunotherapy. Immunology.
153:304–314. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Bapat SA, Mali AM, Koppikar CB and Kurrey
NK: Stem and progenitor-like cells contribute to the aggressive
behavior of human epithelial ovarian cancer. Cancer Res.
65:3025–3029. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Lupia M and Cavallaro U: Ovarian cancer
stem cells: Still an elusive entity? Mol Cancer. 16:642017.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Bregenzer ME, Horst EN, Mehta P, Novak CM,
Repetto T and Mehta G: The role of cancer stem cells and mechanical
forces in ovarian cancer metastasis. Cancers (Basel). 11:10082019.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Li SS, Ma J and Wong AST: Chemoresistance
in ovarian cancer: Exploiting cancer stem cell metabolism. J
Gynecol Oncol. 29:e322018. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Klemba A, Purzycka-Olewiecka JK, Wcisło G,
Czarnecka AM, Lewicki S, Lesyng B, Szczylik C and Kieda C: Surface
markers of cancer stem-like cells of ovarian cancer and their
clinical relevance. Contemp Oncol (Pozn). 22:48–55. 2018.PubMed/NCBI
|
|
39
|
Walcher L, Kistenmacher AK, Suo H, Kitte
R, Dluczek S, Strauß A, Blaudszun AR, Yevsa T, Fricke S and
Kossatz-Boehlert U: Cancer stem cells-origins and biomarkers:
Perspectives for targeted personalized therapies. Front Immunol.
11:12802020. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Liou GY: CD133 as a regulator of cancer
metastasis through the cancer stem cells. Int J Biochem Cell Biol.
106:1–7. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Zhou Q, Chen A, Song H, Tao J, Yang H and
Zuo M: Prognostic value of cancer stem cell marker CD133 in ovarian
cancer: A meta-analysis. Int J Clin Exp Med. 8:3080–3088.
2015.PubMed/NCBI
|
|
42
|
Tao Y, Li H, Huang R, Mo D, Zeng T, Fang M
and Li M: Clinicopathological and prognostic significance of cancer
stem cell markers in ovarian cancer patients: Evidence from 52
studies. Cell Physiol Biochem. 46:1716–1726. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Onisim A, Iancu M, Vlad C, Kubelac P,
Fetica B, Fulop A, Achimas-Cadariu A and Achimas-Cadariu P:
Expression of Nestin and CD133 in serous ovarian carcinoma. J BUON.
21:1168–1175. 2016.PubMed/NCBI
|
|
44
|
Ruscito I, Cacsire Castillo-Tong D,
Vergote I, Ignat I, Stanske M, Vanderstichele A, Ganapathi RN,
Glajzer J, Kulbe H, Trillsch F, et al: Exploring the clonal
evolution of CD133/aldehyde-dehydrogenase-1 (ALDH1)-positive cancer
stem-like cells from primary to recurrent high-grade serous ovarian
cancer (HGSOC). A study of the ovarian cancer therapy-innovative
models prolong survival (OCTIPS) consortium. Eur J Cancer.
79:214–225. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Steg AD, Bevis KS, Katre AA, Ziebarth A,
Dobbin ZC, Alvarez RD, Zhang K, Conner M and Landen CN: Stem cell
pathways contribute to clinical chemoresistance in ovarian cancer.
Clin Cancer Res. 18:869–881. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Liu BL, Liu SJ, Baskys A, Cheng H, Han Y,
Xie C, Song H, Li J and Xin XY: Platinum sensitivity and CD133
expression as risk and prognostic predictors of central nervous
system metastases in patients with epithelial ovarian cancer. BMC
Cancer. 14:8292014. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Liu CL, Chen YJ, Fan MH, Liao YJ and Mao
TL: Characteristics of CD133-sustained chemoresistant cancer
stem-like cells in human ovarian carcinoma. Int J Mol Sci.
21:64672020. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Ween MP, Oehler MK and Ricciardelli C:
Role of versican, hyaluronan and CD44 in ovarian cancer metastasis.
Int J Mol Sci. 12:1009–1029. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Sacks JD and Barbolina MV: Expression and
function of CD44 in epithelial ovarian carcinoma. Biomolecules.
5:3051–3066. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Lin J and Ding D: The prognostic role of
the cancer stem cell marker CD44 in ovarian cancer: A
meta-analysis. Cancer Cell Int. 17:82017. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Zhou J, Du Y, Lu Y, Luan B, Xu C, Yu Y and
Zhao H: CD44 expression predicts prognosis of ovarian cancer
patients through promoting epithelial-mesenchymal transition (EMT)
by regulating snail, ZEB1, and caveolin-1. Front Oncol. 9:8022019.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Zhang J, Yuan B, Zhang H and Li H: Human
epithelial ovarian cancer cells expressing CD105, CD44 and CD106
surface markers exhibit increased invasive capacity and drug
resistance. Oncol Lett. 17:5351–5360. 2019.PubMed/NCBI
|
|
53
|
Zhu Y, Zhang H, Zhang G, Shi Y and Huang
J: Co-expression of CD44/MyD88 is a poor prognostic factor in
advanced epithelial ovarian cancer. Ann Transl Med. 7:912019.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Zhang HF, Hu P and Fang SQ: Understanding
the role of CD44V6 in ovarian cancer. Oncol Lett. 14:1989–1992.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Tjhay F, Motohara T, Tayama S, Narantuya
D, Fujimoto K, Guo J, Sakaguchi I, Honda R, Tashiro H and Katabuchi
H: CD44 variant 6 is correlated with peritoneal dissemination and
poor prognosis in patients with advanced epithelial ovarian cancer.
Cancer Sci. 106:1421–1428. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Motohara T, Fujimoto K, Tayama S,
Narantuya D, Sakaguchi I, Tashiro H and Katabuchi H: CD44 variant 6
as a predictive biomarker for distant metastasis in patients with
epithelial ovarian cancer. Obstet Gynecol. 127:1003–1011. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Deng S, Yang X, Lassus H, Liang S, Kaur S,
Ye Q, Li C, Wang LP, Roby KF, Orsulic S, et al: Distinct expression
levels and patterns of stem cell marker, aldehyde dehydrogenase
isoform 1 (ALDH1), in human epithelial cancers. PLoS One.
5:e102772010. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Kuroda T, Hirohashi Y, Torigoe T, Yasuda
K, Takahashi A, Asanuma H, Morita R, Mariya T, Asano T, Mizuuchi M,
et al: ALDH1-high ovarian cancer stem-like cells can be isolated
from serous and clear cell adenocarcinoma cells, and ALDH1 high
expression is associated with poor prognosis. PLoS One.
8:e651582013. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Wang YC, Yo YT, Lee HY, Liao YP, Chao TK,
Su PH and Lai HC: ALDH1-bright epithelial ovarian cancer cells are
associated with CD44 expression, drug resistance, and poor clinical
outcome. Am J Pathol. 180:1159–1169. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Chang B, Liu G, Xue F, Rosen DG, Xiao L,
Wang X and Liu J: ALDH1 expression correlates with favorable
prognosis in ovarian cancers. Mod Pathol. 22:817–823. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Huang R, Li X, Holm R, Trope CG, Nesland
JM and Suo Z: The expression of aldehyde dehydrogenase 1 (ALDH1) in
ovarian carcinomas and its clinicopathological associations: A
retrospective study. BMC Cancer. 15:5022015. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Zhao W, Zang C, Zhang T, Li J, Liu R, Feng
F, Lv Q, Zheng L, Tian J and Sun C: Clinicopathological
characteristics and prognostic value of the cancer stem cell marker
ALDH1 in ovarian cancer: A meta-analysis. Onco Targets Ther.
11:1821–1831. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Ayub TH, Keyver-Paik MD, Debald M,
Rostamzadeh B, Thiesler T, Schröder L, Barchet W, Abramian A,
Kaiser C, Kristiansen G, et al: Accumulation of ALDH1-positive
cells after neoadjuvant chemotherapy predicts treatment resistance
and prognosticates poor outcome in ovarian cancer. Oncotarget.
6:16437–16448. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Roy M, Connor J, Al-Niaimi A, Rose SL and
Mahajan A: Aldehyde dehydrogenase 1A1 (ALDH1A1) expression by
immunohistochemistry is associated with chemo-refractoriness in
patients with high-grade ovarian serous carcinoma. Hum Pathol.
73:1–6. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Ricci F, Bernasconi S, Porcu L, Erba E,
Panini N, Fruscio R, Sina F, Torri V, Broggini M and Damia G: ALDH
enzymatic activity and CD133 positivity and response to
chemotherapy in ovarian cancer patients. Am J Cancer Res.
3:221–229. 2013.PubMed/NCBI
|
|
66
|
Silva IA, Bai S, McLean K, Yang K,
Griffith K, Thomas D, Ginestier C, Johnston C, Kueck A, Reynolds
RK, et al: Aldehyde dehydrogenase in combination with CD133 defines
angiogenic ovarian cancer stem cells that portend poor patient
survival. Cancer Res. 71:3991–4001. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Tarhriz V, Bandehpour M, Dastmalchi S,
Ouladsahebmadarek E, Zarredar H and Eyvazi S: Overview of CD24 as a
new molecular marker in ovarian cancer. J Cell Physiol.
234:2134–2142. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Kristiansen G, Denkert C, Schlüns K, Dahl
E, Pilarsky C and Hauptmann S: CD24 is expressed in ovarian cancer
and is a new independent prognostic marker of patient survival. Am
J Pathol. 161:1215–1221. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Nakamura K, Terai Y, Tanabe A, Ono YJ,
Hayashi M, Maeda K, Fujiwara S, Ashihara K, Nakamura M, Tanaka Y,
et al: CD24 expression is a marker for predicting clinical outcome
and regulates the epithelial-mesenchymal transition in ovarian
cancer via both the Akt and ERK pathways. Oncol Rep. 37:3189–3200.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Soltész B, Lukács J, Szilágyi E, Márton É,
Szilágyi Bónizs M, Penyige A, Póka R and Nagy B: Expression of CD24
in plasma, exosome and ovarian tissue samples of serous ovarian
cancer patients. J Biotechnol. 298:16–20. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Yang B, Yan X, Liu L, Jiang C and Hou S:
Overexpression of the cancer stem cell marker CD117 predicts poor
prognosis in epithelial ovarian cancer patients: Evidence from
meta-analysis. Onco Targets Ther. 10:2951–2961. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Luo L, Zeng J, Liang B, Zhao Z, Sun L, Cao
D, Yang J and Shen K: Ovarian cancer cells with the CD117 phenotype
are highly tumorigenic and are related to chemotherapy outcome. Exp
Mol Pathol. 91:596–602. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Taskiran C, Erdem O, Onan A, Arisoy O,
Acar A, Vural C, Erdem M, Ataoglu O and Guner H: The prognostic
value of endoglin (CD105) expression in ovarian carcinoma. Int J
Gynecol Cancer. 16:1789–1793. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Bai S, Zhu W, Coffman L, Vlad A, Schwartz
LE, Elishaev E, Drapkin R and Buckanovich RJ: CD105 is expressed in
ovarian cancer precursor lesions and is required for metastasis to
the ovary. Cancers (Basel). 11:17102019. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Ziebarth AJ, Nowsheen S, Steg AD, Shah MM,
Katre AA, Dobbin ZC, Han HD, Lopez-Berestein G, Sood AK, Conner M,
et al: Endoglin (CD105) contributes to platinum resistance and is a
target for tumor-specific therapy in epithelial ovarian cancer.
Clin Cancer Res. 19:170–182. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Huang J, Zhang J, Li H, Lu Z, Shan W,
Mercado-Uribe I and Liu J: VCAM1 expression correlated with
tumorigenesis and poor prognosis in high grade serous ovarian
cancer. Am J Transl Res. 5:336–346. 2013.PubMed/NCBI
|
|
77
|
Scalici JM, Arapovic S, Saks EJ, Atkins
KA, Petroni G, Duska LR and Slack-Davis JK: Mesothelium expression
of vascular cell adhesion molecule-1 (VCAM-1) is associated with an
unfavorable prognosis in epithelial ovarian cancer (EOC). Cancer.
123:977–984. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Tayama S, Motohara T, Narantuya D, Li C,
Fujimoto K, Sakaguchi I, Tashiro H, Saya H, Nagano O and Katabuchi
H: The impact of EpCAM expression on response to chemotherapy and
clinical outcomes in patients with epithelial ovarian cancer.
Oncotarget. 8:44312–44325. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Spizzo G, Went P, Dirnhofer S, Obrist P,
Moch H, Baeuerle PA, Mueller-Holzner E, Marth C, Gastl G and Zeimet
AG: Overexpression of epithelial cell adhesion molecule (Ep-CAM) is
an independent prognostic marker for reduced survival of patients
with epithelial ovarian cancer. Gynecol Oncol. 103:483–488. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Woopen H, Pietzner K, Richter R,
Fotopoulou C, Joens T, Braicu EI, Mellstedt H, Mahner S, Lindhofer
H, Darb-Esfahani S, et al: Overexpression of the epithelial cell
adhesion molecule is associated with a more favorable prognosis and
response to platinum-based chemotherapy in ovarian cancer. J
Gynecol Oncol. 25:221–228. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Zhang J, Chang DY, Mercado-Uribe I and Liu
J: Sex-determining region Y-box 2 expression predicts poor
prognosis in human ovarian carcinoma. Hum Pathol. 43:1405–1412.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Bååth M, Westbom-Fremer S, Martin de la
Fuente L, Ebbesson A, Davis J, Malander S, Måsbäck A, Kannisto P
and Hedenfalk I: SOX2 is a promising predictor of relapse and death
in advanced stage high-grade serous ovarian cancer patients with
residual disease after debulking surgery. Mol Cell Oncol.
7:18050942020. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Li Y, Chen K, Li L, Li R, Zhang J and Ren
W: Overexpression of SOX2 is involved in paclitaxel resistance of
ovarian cancer via the PI3K/Akt pathway. Tumour Biol. 36:9823–9828.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Czekierdowski A, Stachowicz N,
Czekierdowska S, Łoziński T, Gurynowicz G and Kluz T: Prognostic
significance of TEM7 and nestin expression in women with advanced
high grade serous ovarian cancer. Ginekol Pol. 89:135–141. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Qin Q, Sun Y, Fei M, Zhang J, Jia Y, Gu M,
Xia R, Chen S and Deng A: Expression of putative stem marker nestin
and CD133 in advanced serous ovarian cancer. Neoplasma. 59:310–315.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Davidson B, Holth A and Dong HP:
Expression of the cancer stem cell marker SSEA1 is associated with
poor survival in metastatic high-grade serous carcinoma. Virchows
Arch. 477:677–685. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Chen WC, Hsu HP, Li CY, Yang YJ, Hung YH,
Cho CY, Wang CY, Weng TY and Lai MD: Cancer stem cell marker CD90
inhibits ovarian cancer formation via β3 integrin. Int J Oncol.
49:1881–1889. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Connor EV, Saygin C, Braley C, Wiechert
AC, Karunanithi S, Crean-Tate K, Abdul-Karim FW, Michener CM, Rose
PG, Lathia JD and Reizes O: Thy-1 predicts poor prognosis and is
associated with self-renewal in ovarian cancer. J Ovarian Res.
12:1122019. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Kim WT and Ryu CJ: Cancer stem cell
surface markers on normal stem cells. BMB Rep. 50:285–298. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Yang W, Kim D, Kim DK, Choi KU, Suh DS and
Kim JH: Therapeutic strategies for targeting ovarian cancer stem
cells. Int J Mol Sci. 22:50592021. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Barzegar Behrooz A, Syahir A and Ahmad S:
CD133: Beyond a cancer stem cell biomarker. J Drug Target.
27:257–269. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Yang L, Shi P, Zhao G, Xu J, Peng W, Zhang
J, Zhang G, Wang X, Dong Z, Chen F and Cui H: Targeting cancer stem
cell pathways for cancer therapy. Signal Transduct Target Ther.
5:82020. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Masoumi J, Jafarzadeh A, Abdolalizadeh J,
Khan H, Philippe J, Mirzaei H and Mirzaei HR: Cancer stem
cell-targeted chimeric antigen receptor (CAR)-T cell therapy:
Challenges and prospects. Acta Pharm Sin B. 11:1721–1739. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Huang B, Miao L, Liu J, Zhang J and Li Y:
A promising antitumor method: Targeting CSC with immune cells
modified with CAR. Front Immunol. 13:9373272022. View Article : Google Scholar : PubMed/NCBI
|