Introduction
Immune checkpoint inhibitors (ICIs) have shown to
improve overall survival in the recurrent/metastatic (R/M) setting
of squamous cell cancer of the head and neck (SCCHN). Nivolumab is
approved in second line after progression to platinum or in
first-line platinum-refractory disease (1). Pembrolizumab alone or combined with
chemotherapy is approved in the first-line platinum-sensitive
setting. However, objective response rates (ORR) with single-agent
PD(L)1 inhibitors in R/M SCCHN fall below 25% and are usually
slower than those observed with chemotherapy (2). In addition, chemotherapy aids in
promoting a more efficient neoantigen presentation and modifies the
tumor microenvironment (TME) reducing the immunosuppressive
component, thereby potentially synergizing with ICIs (3,4).
While pembrolizumab combined with three-weekly platinum and 5-FU
achieves ORR ranging from 36 to 42% depending on the combined
positive score (CPS) value, it is estimated, depending on the
population studied, that up to 40% R/M SCCHN patients are unfit for
high-dose cisplatin or for fluoropyrimidines (5,6).
Taxane-based chemo-immunotherapy (chemo-IO) combinations have been
tested in the locally-advanced neoadjuvant setting demonstrating
promising efficacy and safety profiles (7–10).
Recently, results of the Keynote-B10 trial with pembrolizumab and
three-weekly carboplatin and paclitaxel in first-line R/M SCCHN
were reported, demonstrating a notable ORR of 43%, a median
progression-free survival (PFS) of 5.6 months and a median overall
survival (OS) of 12.1 months (11). In addition, the same combination is
FDA- and EMA-approved in other squamous histologies such as CPS ≥1
first-line metastatic squamous cell non-small cell lung cancer
(sqNSCLC) (12). In addition,
taxane-based dose-adapted chemo-IO combinations are promising
alternatives for highly comorbid or ECOG ≥2 patients with R/M SCCHN
who need a high and deep response rate (NCT04282109) (11,13).
In the present series we aimed to retrospectively evaluate the
safety and preliminary activity of
pembrolizumab-carboplatin-paclitaxel (pembro + CP) in heavily
pretreated R/M SCCHN.
Materials and methods
Study design and patients
Retrospective study of R/M SCCHN patients that were
treated with pembrolizumab-carboplatin-paclitaxel as first- or
subsequent lines of therapy, via a compassionate use program for
cisplatin-unfit or fluoropyrimidine ineligible patients. Criteria
of cisplatin ineligibility were i) ECOG performance status (PS) of
2 and/or ii) creatinine-clearance (ClCr) <60 ml/min and/or iii)
CTCAE Gr ≥2 hearing loss and/or iv) CTCAE Gr ≥2 neuropathy and/or
v) history of ischemic heart disease and/or vi) history of heart
failure. Criteria of fluoropyrimidines ineligibility were i)
history of ischemic heart disease and/or ii) history of heart
failure and/or iii) complete dihydropyrimidine dehydrogenase (DPD)
deficiency and/or iv) severe hepatic insufficiency and/or v)
unavailable central venous catheter placement (6,14).
In addition, all patients treated with pembro + CP had to have a
CPS ≥1.
Other inclusion criteria were: i) ≥18 years of age;
ii) confirmed R/M SCCHN of the oropharynx, oral cavity, hypopharynx
or larynx progressing on or after a previous line of systemic
therapy and not eligible for a curative-intent therapy; iii)
Cisplatin-unfit and/or ineligible for fluoropyrimidines as per the
above definitions; iv) WHO/ECOG Performance status of 0, 1 or 2 at
the time of starting pembro + CP; v) Adequate organ function as
defined by: hemoglobin ≥9.0 g/dl, absolute neutrophil count
≥1,500/mm3, platelets ≥75,000/mm3, total
bilirubin ≤1.5× upper level of normal (ULN), AST and AST ≤2.5 ULN,
CrCl ≥30 ml/min as per the Cockcroft-Gault formula; vi) Body weight
>30 kg; vii) a minimum life expectancy of 12 weeks
Exclusion criteria were: i) a histologically
confirmed head and neck cancer of any other primary anatomic site,
an unknown primary site SCCHN or a non-squamous histology; ii) any
unresolved toxicity of CTCAE ≥ grade 2 except alopecia, vitiligo
and laboratory values defined in the inclusion criteria; iii) a
history or organ transplantation or active or previously documented
autoimmune disorders with the exception of vitiligo, alopecia,
stable and treated hypothyroidism; iv) active infection including
tuberculosis, hepatitis B, hepatitis C or human immunodeficiency
virus; v) an uncontrolled intercurrent illness such as ongoing or
active infection, congestive heart failure, uncontrolled
hypertension, unstable angina pectoris, uncontrolled cardiac
arrhythmia, chronic gastrointestinal conditions associated with
diarrhea or psychiatric illness or social conditions that would
limit the compliance with treatment.
A descriptive study of baseline characteristics was
performed. Three different geriatric and comorbidity scores were
used: the modified Charlson Comorbidity Index (mCCI) and the Adult
Comorbidity Evaluation-27 (ACE-27) with a mCCI ≥2 and ACE-27 ≥3
indicating moderate-to-severe comorbidity. The third scoring system
was the Generalized Competing Event Composite Omega Score (GCE-COS)
which encompasses different comorbidity scores to predict relative
cancer vs. noncancer risk and may be accessed through an online
tool, with a GCE-COS ≥0.6 indicating a higher overall survival with
oncological treatment (15).
Adverse events (AEs) were recorded using the
National Cancer Institute Common Terminology Criteria for Adverse
Events, version 4.0. ORR according to Response Evaluation Criteria
in Solid Tumors (RECIST) 1.1, disease control rate (DCR),
percentage of tumor change from baseline in target lesions (PCTL),
progression-free survival (PFS), duration of treatment (DOT), and
OS from the start of pembro + CP and from the start of first-line
therapy were studied (16). Dose
intensity for each agent and treatment compliance were also
recorded.
The primary endpoint was safety. Secondary endpoints
were, treatment compliance, ORR, DCR, PCTL, DOT, PFS and OS since
pembro + CP (defined as the time from the start of pembro + CP
until disease progression or death due to any cause, respectively),
and OS since the first line of treatment (defined as the time from
the start of first-line therapy until death from any cause).
Considering that this is a heterogenous series, with patients
receiving pembro + CP at different lines of therapy, efficacy
results are presented using a swimmers plot depicting the treatment
history from the start of pembro + CP and from the start of
first-line therapy following the Trial Reporting in Immuno-Oncology
(TRIO) guidelines (17).
Dosing of
pembrolimab-carboplatin-paclitaxel
Chemotherapy within the Pembro + CP regimen could be
administered as a weekly or a three-weekly schedule, as follows: a)
Pembrolizumab (200 mg/q3wk IV) plus three-weekly carboplatin (AUC
3–5) and paclitaxel (125–175 mg/m2); b) Pembrolizumab
(200 mg/q3wk IV) day 1 plus weekly carboplatin (AUC 1.5-2) and
paclitaxel (60–80 mg/m2) days 1, 8 and 15.
The final dosing of chemotherapy was allowed to be
modified (within the ranges detailed above) in the first or
subsequent cycles according to the ECOG performance status,
comorbidities, or previous toxicities, as per the investigator's
discretion.
Evaluation of response
RECIST 1.1 criteria were used for response
evaluation, with CT scans performed every 8 to 12 weeks, according
to the local protocol. Two expert radiologists in head and neck
cancer evaluated each case independently. A consensus was achieved
in case of discordant cases between the two.
A ≥30% decrease in the sum of the diameters of
target lesions (TL) and a ≥20% increase in the sum of diameters of
TL or the appearance of new metastatic lesions, defined a partial
response (PR) and progressive disease (PD), respectively. Stable
disease (SD) was defined as a change in the size of TL ranging
between a 30% decrease and a 20% increase in the sum of their
diameters (16).
DCR was defined as the percentage of patients
achieving CR, PR and SD. Confirmed responses or SD had to be
confirmed in at least two consecutive CT scans. Both confirmed and
unconfirmed responses, SD and DCR were reported.
PD-L1 expression
PD-L1 membrane expression was measured in tumor
cells using an immunohistochemistry assay. The PDL1 IHC 22C3
pharmDx (Dako North America, Carpinteria, CA) immunohistochemistry
assay, was used to measure PD-L1 expression in tumor and
mononuclear stromal cells. At least a partial membrane staining in
≥1% of cells had to be present to consider a positive expression.
The expression of PD-L1 in tumor cells only was used to calculate
the tumor proportion score (TPS), as previously described (1). The expression of PD-L1 in tumor cells
and mononuclear stromal cells were measured to calculate the CPS
value, as previously described (18).
Statistical analysis and sample size
justification
Dose-adapted pembro + CP was hypothesized to be less
toxic than the combination of pembrolizumab + three-weekly platinum
+ 5FU (PF) tested in the Keynote-048 trial (2). The combination of pembrolizumab plus
three-weekly platinum + 5FU is associated with a composite 94% of
grade ≥3 AEs (summatory of incidence of hematological,
gastrointestinal, and respiratory AEs). Dose-adjusted pembro + CP
was expected to account for a 45% composite rate of grade ≥3 AEs.
With an 80% power and a 95% CI (unilateral test), a total of 10
patients would have to be enrolled to demonstrate a 45% composite
rate of grade ≥3 AEs with pembro + CP.
A descriptive analysis of demographic and
clinicopathological data was performed. The Kaplan-Meier method was
used to estimate PFS and OS, and the Fisher's Exact Test and
Pearson's and Kendall's Correlations Tests were used to evaluate
any association or correlations, respectively. The software SPSS
Statistics for MacOS, version 23.0 (IBM SPSS Statistics for McOS,
Version 23.0, Armonk, NY) was used for all statistical
analyses.
Ethical considerations
All patients signed and informed consent form before
starting pembro + CP as part of a compassionate use program,
approved by the Compassionate Use Therapy Commission of Hospital
Clínico Universitario San Carlos. The present study was approved by
the Institutional Review Board of Hospital Clínico Universitario
San Carlos and was conducted in accordance with the principles of
the Declaration of Helsinki. The requirement of informed consent
was waived as the study was based on a retrospective analysis of
existing administrative and clinical data.
Results
Baseline characteristics
Between March 2020 and August 2021, ten patients
were included, that were followed until March 31st, 2022. Baseline
characteristics of the patients are summarized in Table I.
 | Table I.Patient (n=10) and tumor
characteristics. |
Table I.
Patient (n=10) and tumor
characteristics.
|
Characteristics | Value |
|---|
| Age at pembro + CP,
years |
|
| Median
(min-max) | 64 (36–89) |
| ≥70, n
(%) | 4 (40) |
| <70,
n (%) | 6 (60) |
| ECOG at pembro +
CP, n (%) |
|
| 0 | 0 (0) |
| 1 | 2 (20) |
| 2 | 8 (80) |
| Median mCCI (range,
min-max) | 9 (7–13) |
| Median ACE-27
(range, min-max) | 3 (3–3) |
| GCE-COS |
|
| Median
(range, min-max) | 0.812
(0.714-0.867) |
| COS
<0.6, n (%) | 0 (0) |
| COS
≥0.6, n (%) | 10 (100) |
| Smoking history, n
(%) | 10 (100) |
| Sex, n (%) |
|
|
Male | 4 (40) |
|
Female | 6 (60) |
| Anatomic subsite, n
(%) |
|
| Oral
cavity | 7 (70) |
|
Oropharynx | 3 (1 HPV+; 2 HPV-)
(30) |
| Stage, n (%) |
|
|
IVA | 7 (70) |
|
IVB | 2 (20) |
|
IVC | 1 (10) |
| Treatment at
initial diagnosis, n (%) |
|
|
Surgery | 6 (60) |
|
Adjuvant CRT | 6 (60) |
|
wkCDDP | 2 |
|
Cetuximab | 4 |
| Radical
CRT | 4 (40) |
|
3wkCDDP | 1 |
|
wkCDDP | 1 |
|
Cetuximab | 2 |
|
Induction CT | 4 (40) |
|
wkP-Cetuximab | 1 |
|
TPF | 3 |
| Upfront
TX for R/M | 1 (10) |
|
Pembro | 1 (10) |
| R/M disease at
pembro + CP |
|
|
Locoregional only, n (%) | 7 (70) |
| Distant
only, n (%) | 1 (10) |
|
Locoregional + distant, n
(%) | 2 (20) |
| Median
prior lines of TX (range, min-max) | 3 (1–5) |
| Prior
platinum-based TX, n (%) | 6 (60%) |
| Prior
ICIs, n (%) | 8 (80%) |
| Median no. of lines
for R/M disease (range, min-max) | 4 (2–7) |
The most common primary tumor location was the oral
cavity (70%). Seventy percent were stage IVA, 20% stage IVB and 10%
stage IVC at initial diagnosis. Seventy percent had been treated
with surgery, 80% with adjuvant radiotherapy (RT) or radical
chemoradiotherapy (CRT), and 40% had received induction
chemotherapy. In the R/M setting, 90% of the patients had received
at least one line of therapy prior to pembro + CP, with a median of
3 prior lines (range: 0–6), and up to 60 and 80% had received prior
platinum and prior ICIs in the R/M setting, respectively.
Sixty percent of patients were female, median age
was 64 years old, and 40% were ≥70 years old. At the start of
pembro + CP 20% of patients had ECOG 1 and 80% had ECOG 2. All
patients were cisplatin-unfit, and, in addition, 2 patients were
not eligible for fluoropyrimidines. Median mCCI score was 9 (range:
7–13), ACE-27 was 3 (range: 3–3) and GCE-COS was 0.812 (range:
0.714-0.867).
Pembro + CP regimens used were as follows: a)
Pembrolizumab (200 mg/q3wk IV) plus three-weekly carboplatin (AUC5)
and paclitaxel (150 mg/m2): n=1; b) Pembrolizumab (200
mg/q3wk IV) plus three-weekly carboplatin (AUC4) and paclitaxel
(150 mg/m2): n=2; c) Pembrolizumab (200 mg/q3wk IV) plus
three-weekly carboplatin (AUC3) and paclitaxel (150
mg/m2): n=5; d) Pembrolizumab (200 mg/q3wk IV) plus
weekly carboplatin (AUC2) and paclitaxel (80 mg/m2) days
1, 8 and 15: n=2.
Toxicity during pembro + CP
In the whole series of 10 patients, grade 1 or 2 AEs
occurred in 100% all of them during the combination phase of pembro
+ CP. Grade 3–5 AEs developed in 30% of patients (Tables II and SI), being grade 3 in all of them and all
of them occurring during the combination phase of pembro + CP as
well. There were no treatment-related deaths.
 | Table II.Summary of toxicity during treatment
with pembrolizumab + carboplatin-paclitaxel in 10 patients. |
Table II.
Summary of toxicity during treatment
with pembrolizumab + carboplatin-paclitaxel in 10 patients.
|
| Event grade (CTCAE
v4.0) |
|---|
|
|
|
|---|
| Toxicity | G1-2, n (%) | G1, n (%) | G2, n (%) | G3-5, n (%) | G3, n (%) | G4, n (%) | G5, n (%) |
|---|
| General |
|
|
|
|
|
|
|
|
Asthenia | 10/10 (100) | 1/10 (10) | 9/10 (90) | - | - | - | - |
| Nutrition and
metabolic disorders |
|
|
|
|
|
|
|
|
Decreased appetite | 8/10 (80) | - | 8/10 (80) | - | - | - | - |
|
Hypomagnesemia | 2/10 (20) | 2/10 (20) | - | 1/10 (10) | 1/10 (10) | - | - |
|
Gastrointestinal |
|
|
|
|
|
|
|
|
Nausea | 1/10 (10) | - | 1/10 (10) | - | - | - | - |
| Skin |
|
|
|
|
|
|
|
|
Alopecia | 8/10 (80) | - | 8/10 (80) | - | - | - | - |
| Infections |
|
|
|
|
|
|
|
|
URT | 4/10 (40) | - | 4/10 (40) | - | - | - | - |
|
Otitis | 1/10 (10) | 1/10 (10) | - | - | - | - | - |
| Soft
tissue | 1/10 (10) | 1/10 (10) | - | - | - | - | - |
| Blood and lymphatic
system disorders |
|
|
|
|
|
|
|
|
Anemia | 6/10 (60) | 1/10 (10) | 5/10 (50) | - | - | - | - |
|
Neutropenia | 1/10 (10) | - | 1/10 (10) | 2/10 (20) | 2/10 (20) | - | - |
|
Thrombopenia | 5/10 (50) | 1/10 (10) | 4/10 (40) | 1/10 (10) | 1/10 (10) | - | - |
| Nervous system
disorders |
|
|
|
|
|
|
|
|
Peripheral neuropathy | 8/10 (80) | 7/10 (70) | 1/10 (10) | - | - | - | - |
| Vascular system
disorders |
|
|
|
|
|
|
|
|
Hypertension | - |
| - | 1/10 (10) | 1/10 (10) | - | - |
Among patients treated with three-weekly pembro + CP
(n=8), AEs of grades 1 or 2 occurred in 100% of the patients, the
most common being asthenia, decreased appetite, anemia, peripheral
neuropathy, hypomagnesemia, and alopecia. Grade 3–5 AEs occurred in
3 patients (37.5%), with 2 patients suffering grade 3 neutropenia,
1 grade 3 thrombopenia, 1 grade 3 hypomagnesemia, and 1 patient
with grade 3 hypertension, the latter considered unrelated to
pembro + CP (Tables II and
SI).
Among patients treated with pembrolizumab combined
with weekly CP (n=2) both patients suffered from AEs of grades 1 or
2 while no grade 3–5 AEs occurred. Tables II and SI summarize adverse events during pembro
+ CP in the whole population and in each individual patient,
respectively.
Among the 8 patients treated with anti-PD(L)1 agents
in previous lines in the R/M setting, three patients had suffered
from irAEs: Patient 5 suffered from hyperprogressive disease after
3 doses of first-line nivolumab that was successfully rescued with
cetuximab-based chemotherapy, Patient 6 suffered from grade 3
pneumonitis after 5 doses of fifth-line nivolumab, and Patient 9
developed grade 2 hypothirodism after 6 doses of first-line
nivolumab. None of them, suffered from these or any other irAEs
during treatment with pembro + CP.
Treatment compliance during pembro +
CP
Median DOT with pembro + CP was 4.5 months (Min-Max:
0.5-24). Median number of combination pembro + CP cycles was 3
(range: 1–11). Five patients also received maintenance
pembrolizumab [median 1 cycle (range: 1–25)].
Among patients who received pembro + 3wkCP (n=8)
median number of pembrolizumab, carboplatin and paclitaxel cycles 6
(range-1-11). Only three patients suffered delayed administration
of pembro + 3wkCP due to toxicity, with a median of 1 cycle delayed
(range: 1–2) and a median delay of 7 days (range: 7–14).
Among patients who received pembro + wkCP (n=2) one
patient received 3 cycles of three-weekly pembrolizumab and the
other patient received 2 cycles. Number of weekly carboplatin and
paclitaxel doses were 2 in one patient and 3 the other patient,
respectively. None of the patients suffered delays in treatment
administration.
All patients discontinued pembro + CP due to
radiological and/or clinical progression.
Detailed dosages of each agent received by each
patient are summarized in Tables
III and SII.
 | Table III.Summary of treatment compliance
during treatment with pembrolizumab + carboplatin-paclitaxel. |
Table III.
Summary of treatment compliance
during treatment with pembrolizumab + carboplatin-paclitaxel.
|
|
| Pembro + CP | Maintenance
pembrolizumab |
|---|
|
|
|
|
|
|---|
| Regimen | Agent | Mean/median no. of
cyclesa | Mean dose per
cyclea | Mean/median no. of
cyclesa | Mean dose per
cycle, mga |
|---|
| Pembro + wkCP | Pembrolizumab | 2.5 (mean) | 200
mg | 2 (n=1) | 200 |
| (n=2) | Carboplatin | 2.5 (mean) | 142
mg/m2 | - | - |
|
| Paclitaxel | 2.5 (mean) |
70
mg/m2 | - | - |
| Pembro + 3wkCP | Pembrolizumab |
6
(median) | 200
mg | 1 (1–25)
(n=4) | 200 |
| (n=8) | Carboplatin |
6
(median) | 203
mg/m2 | - | - |
|
| Paclitaxel |
6
(median) | 103
mg/m2 | - | - |
Response during pembro + CP
Among 7 evaluable patients, ORR was 14% (1/7), with
1 complete response (CR) in a patient that received pembro + 3wkCP
as second line therapy. Three patients showed stable disease (SD)
and 3 progressive disease (PD) as best responses during pembro +
CP. DCR after the first CT scan evaluation was 43%. Confirmed DCR
(after at least 2 consecutive CT scan evaluations) was 14%. The
patient achieving a CR to pembro + CP was the only one where ORR
was confirmed with at least two consecutive CT scans. Therefore,
the confirmed ORR was 14%. Median PCTL was 10% (range: −100% to
+80%) (Tables IV and V).
 | Table IV.Response rate, best percentage change
from baseline in target lesions and Kaplan-Meier estimates of PFS
and OS. |
Table IV.
Response rate, best percentage change
from baseline in target lesions and Kaplan-Meier estimates of PFS
and OS.
| Variable | Value |
|---|
| Tumor response
(n=7) |
|
|
ORRa, % (fraction) | 14 (1/7) |
| Type of
responsea, %
(fraction) |
|
| CR | 14 (1/7) |
| PR | 0 (0/7) |
| SD | 29 (2/7) |
| PD | 57 (4/7) |
| Best
PCTL among objective responders, | +10 (range, |
| %
(range) | −100 to +80) |
|
DCRa, % (fraction) | 43 (3/7) |
| Median survival
(range) (n=10)b,c |
|
|
Follow-upb since pembro + CP, months | 6.5 (0.5-24.0) |
| PFS
since pembro + CP, months | 5 (1.0-9.0) |
| OS
since pembro + CP, months | 6 (0.5-14.0) |
| PFS
since pembro + 3wkCP, months (n=8) | 3 (1.1-4.8) |
| OS
since pembro + 3wkCP, months (n=8) | 11 (1.4-20.6) |
|
Follow-upb since 1st line, months | 25.5
(7.0-63.0) |
| OS
since 1st line, months | 30 (18.0-42.0) |
 | Table V.Clinical history and lines of
treatment received before, during and after salvage pembrolizumab +
carboplatin-paclitaxel for each individual patient. |
Table V.
Clinical history and lines of
treatment received before, during and after salvage pembrolizumab +
carboplatin-paclitaxel for each individual patient.
| Patient order
No. | Age, years/primary
tumor/AJCC 8th Ed stage/HPV/CPS/ treatment at initial DX | Age, years/CU or
FI/CrCl/PR/ECOG/mCCI/ACE-27/GCE-COS/at pembro + CP | Location of disease
at 1st SCAI | 1st line (DOT) | 2nd line (DOT) | 3rd line (DOT) | 4th line (DOT) | 5th line (DOT) | 6th line (DOT) | 7th line (DOT) | OS Pembro + CP (m);
OS 1st line (m); Status |
|---|
| 1 |
75/OC/pT2N2bM0/ | 78/CU/66
ml/min/ | M (Pleuro- | wkP-Cetux | Nivo | wkCDDP- | Nivo | wkCDDP- | Pembro + | - | OS PCT, 2 m; |
|
|
IVA/HPV(−)/CPS= | Non-PRf/ECOG
2/ | pulmonary) | (5 m) | (12 m) | Cetux (3 m) | (6 m) | Cetux (2 m) | wkCP (2 m, |
| OS 1st L, 30
m; |
|
| 80 TPS=80%/SX | mCCI=9/ACE-27= |
|
|
|
|
|
| PD; +30%) |
| DOD |
|
| followed by Adj
BRT |
3/GCE-COS=0.778 |
|
|
|
|
|
|
|
|
|
| 2 |
82/OC/pT4aN2bM0/ | 83/CU + FI/95
ml/ | LR | wkP-Cetux | Nivo | wkP-Cetux | Nivo | wkPC- | Pembro + | - | OS PCT, 4 m; |
|
|
IVA/HPV(−)/CPS= | min/Non-PRf/ |
| (2.5 m) | (4 m) | (2.5 m) | (2 m) | Cetux | 3wkCP |
| OS 1st L, 18
m; |
|
| 70 TPS=50%/SX | ECOG
2/mCCI=13/ |
|
|
|
|
| (1.5 m) | (2 m) |
| DOD |
|
| followed by Adj
BRT | ACE-27=3/GCE- |
|
|
|
|
|
|
|
|
|
|
|
| COS=0.714 |
|
|
|
|
|
|
|
|
|
| 3 |
50/OPC/pT4N2cM0/ | 53/CU/104
ml/min/ | L + R | Nivo | wkP-Cetux | Pembro | Pembro + | (−) | (−) | (−) | OS PCT, 12 m; |
|
|
III/HPV(+)/CPS= | PRf/ECOG 2/ |
| (5 m) | (14 m) | (6 m) | 3wkCP (9 m, |
|
| OS 1st L, 41
m; |
|
|
| 10 TPS=2%/TPF
×3 | mCCI=7/ACE-27= |
|
|
|
| PD; −13%) |
|
|
| DOD |
|
| followed by
Radical |
3/GCE-COS=0.812 |
|
|
|
|
|
|
|
|
|
|
| RT + 3wkCDDP |
|
|
|
|
|
|
|
|
|
|
| 4 |
52/OC/pT4bN2cM0/ | 55/CU/100
ml/min/ | L | wkP-Cetux | Pembro + | (−) | (−) | (−) | (−) | (−) | OS PCT, 24 m; |
|
|
IVB/HPV(−)/CPS= | Non-PRf/ECOG
2/ |
| (3 m) | 3wkCP |
|
|
|
|
| OS 1st L, |
|
| 100 TPS=100%/ | mCCI=7/ACE-27= |
|
| (24 m); CR; |
|
|
|
| AWOD |
|
|
| TPF × 3
followed |
3/GCE-COS=0.867 |
|
|
| −100%) |
|
|
|
|
|
|
| by Radical RT
+ |
|
|
|
|
|
|
|
|
|
|
|
| 3wkCDDP |
|
|
|
|
|
|
|
|
|
|
| 5 |
62/OPC/pT4aN0M0/ | 64/CU + FI/114
ml/ | L + R | Nivo | wkP-Cetux | wkCDDP- | Nivo | wkP-Cetux | Pembro + | (−) | OS PCT, 2.5 m; |
|
|
IVA/HPV(−)/CPS= | min/Non-PRf/ | (1 m) | (3 m) | Cetux | (4 m) | (6 m) | wkCP (2 m) |
| OS 1st L, 30
m; |
|
|
| 60 TPS=60%/SX | ECOG 2/mCCI=9/ |
|
|
| followed |
|
|
|
| DOD |
|
| followed by Adj
BRT | ACE-27=3/GCE- |
|
|
| by Cetux |
|
|
|
|
|
|
|
| COS=0.844 |
|
|
| (13 m) |
|
|
|
|
|
| 6 |
64/OPC/pT2N2bM0/ | 71/CU/97
ml/min/ | L | Anti-PDL1 | wkP-Cetux | Nivo | wkCDDP- | Pembro + | wkP-Cetux | Pembro- | OS PCT, 9.5 m; |
|
|
IVA/HPV(−)/CPS=20 | Non-PRf/ECOG
2/ |
| (CT) | (14 m) | (15 m) | Cetux (4 m) | 3wkCP | (1 m) | Cetux (3 m) | OS 1st L, 64
m; |
|
| TPS=10%/TPF ×3 | mCCI=9/ACE-27= |
|
|
|
|
| (4.5 m; |
|
| DOD |
|
| followed by
Radical |
3/GCE-COS=0.757 |
|
|
|
|
| SD; +10%) |
|
|
|
|
| RT + wkCDDP |
|
|
|
|
|
|
|
|
|
|
| 7 |
70/OC/pT3N2bM0/ | 72/CU/89
ml/min/ | L + R | Anti-PDL1 | wkP-Cetux | Pembro + | Pembro- | (−) | (−) | (−) | OS PCT, 6.5 m; |
|
|
IVA/HPV(−)/CPS=1 | Non-PRf/ECOG
2/ |
| (CT) | (9 m) | 3wkCP (2 m; | Cetux (4 m) |
|
|
| OS 1st L, 19
m; |
|
| TPS=0/SX
followed | mCCI=9/ACE-27= |
|
|
| PD; +80%) |
|
|
|
| DOD |
|
| by Adj BRT |
3/GCE-COS=0.748 |
|
|
|
|
|
|
|
|
|
|
8a |
59/OC/pT4aN0M1/ | 59/CU/102
ml/min/ | L + M | Pembro | wkPC-Cetux | Nivo-Cetux | Pembro + | (−) | (−) | (−) | OS PCT, 0.5 m; |
|
|
IVC/HPV(−)/CPS= | Non-PRf/ECOG
2/ | (lung, | (1 m) | (6 m) | (1 m) | 3wkCP |
|
|
| OS 1st L, 11
m; |
|
| 60 TPS=50% | mCCI=9/ACE-27= | bone) |
|
| (0.5
m)a |
|
|
|
| DWDa |
|
|
|
3/GCE-COS=0.841 |
|
|
|
|
|
|
|
|
|
| 9 |
59/OC/cT4bN0M0/ | 59/CU/111
ml/min/ | R | Nivo | TPEx | Pembro + | wkP-Cetux | (−) | (−) | (−) | OS PCT, 11 m; |
|
|
IVB/HPV(−)/CPS= | Non-PRf/ECOG
2/ |
| (5 m) | (8 m) | 3wkCP (6.5 m; | (5 m) |
|
| OS 1st L, 25
m; |
|
|
| 60 TPS=60%/TPF
×3 | mCCI=7/ACE-27= |
|
|
| SD; +10%) |
|
|
|
| AWD |
|
| followed by
Radical |
3/GCE-COS=0.855 |
|
|
|
|
|
|
|
|
|
|
| BRT |
|
|
|
|
|
|
|
|
|
|
| 10 |
64/OC/pT4aN0M0/ | 64/CU/71
ml/min/ | L + M | Pembro + | Cetux + | (−) | (−) | (−) | (−) | (−) | OS PCT, 8 m; |
|
|
IVA/HPV(−)/CPS= | PRf/ECOG 1/ | (lung) | 3wkCP (5 m, | Mona/Pbo |
|
|
|
| OS 1st L, 8 m; |
|
|
| 60 TPS=40%/SX | mCCI=9/ACE-27= |
| PD; −20%) | (CT) |
|
|
|
|
| AWD |
|
| followed by
Adj |
3/GCE-COS=0.820 |
|
|
|
|
|
|
|
|
|
|
| RT + wkCDDP |
|
|
|
|
|
|
|
|
|
|
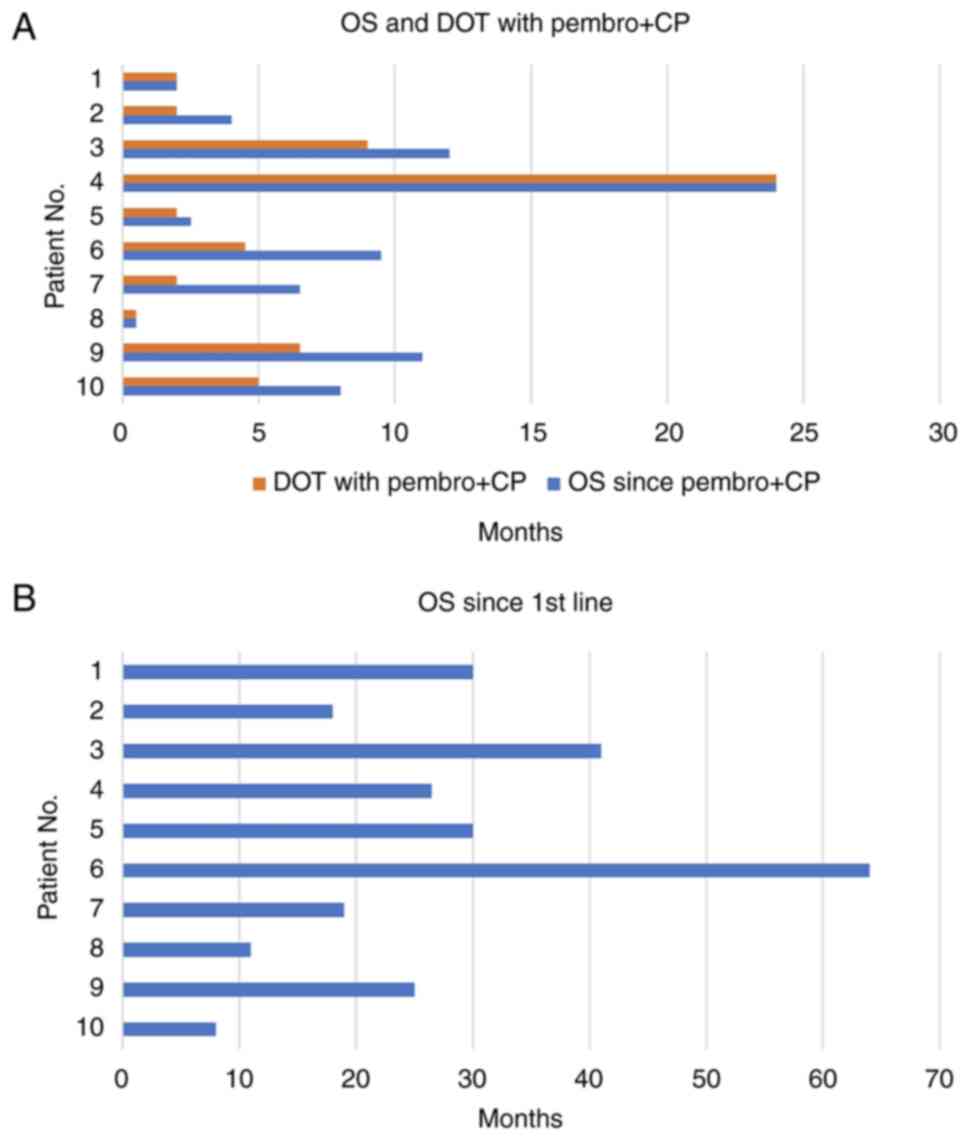
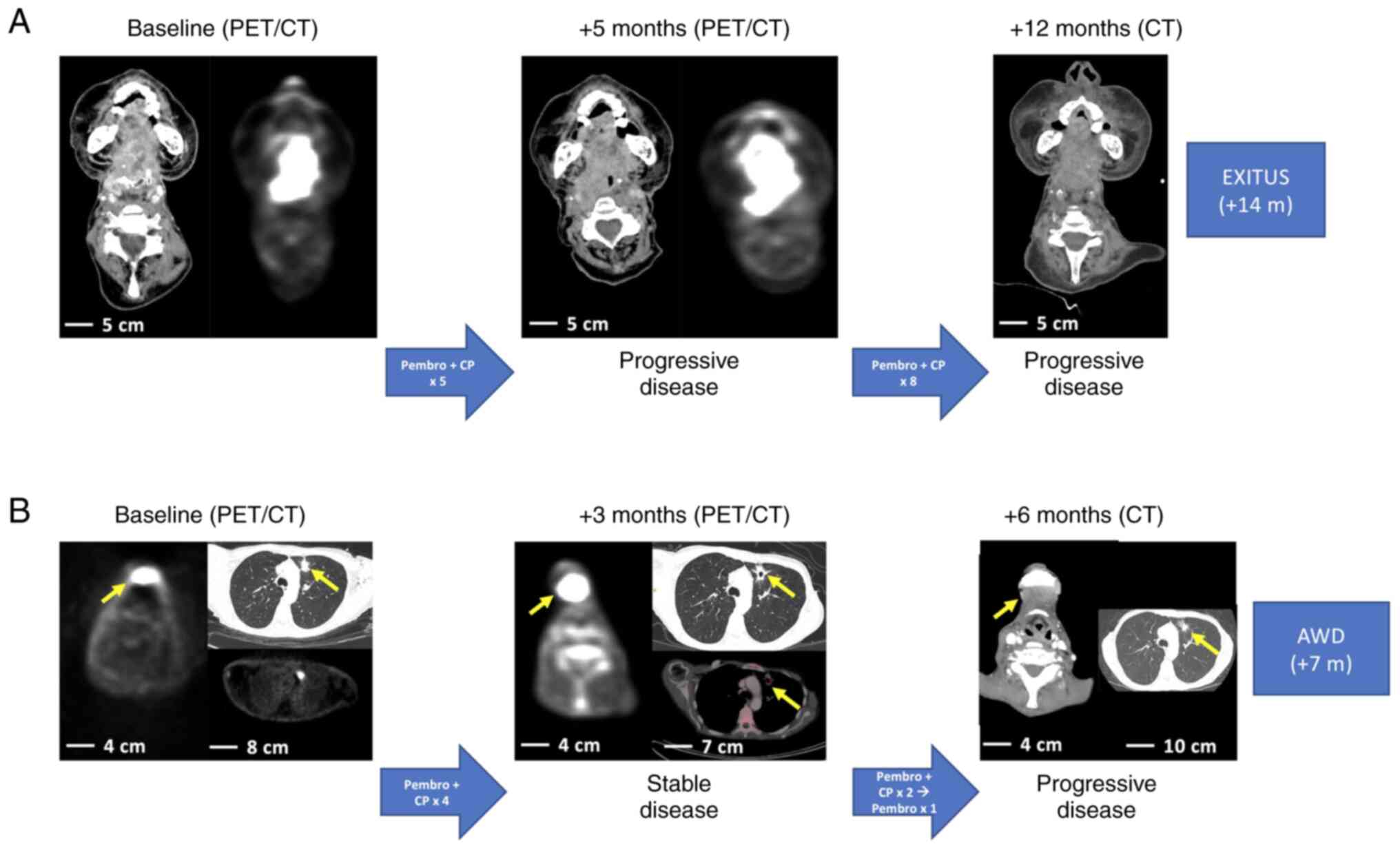
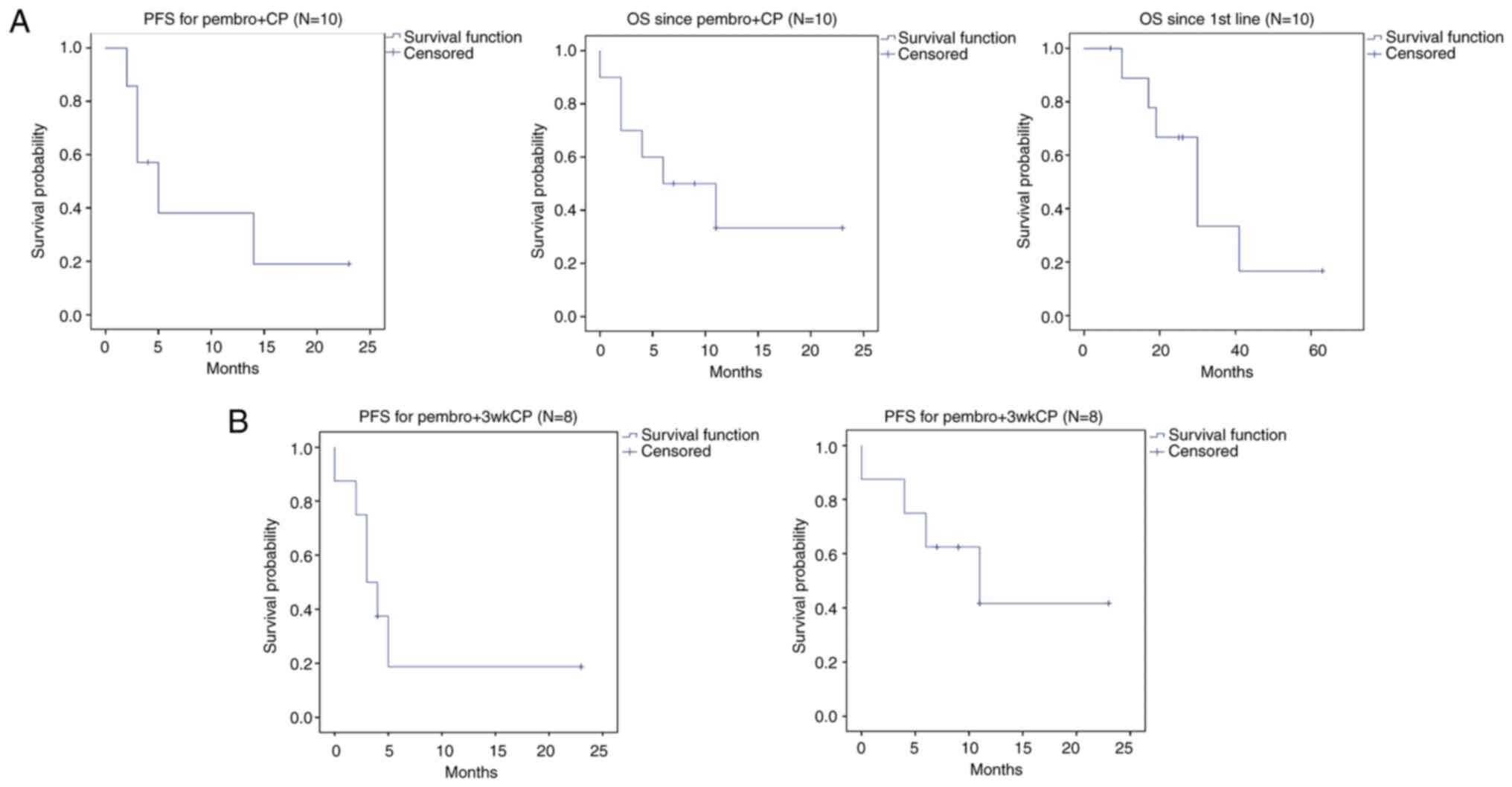
Progression-free survival and overall
survival
In the whole population, after a median follow-up of
6.5 months (range: 0.5-24), median OS since pembro + CP was 6
months (95% CI 0.5-14) and PFS was 5 months (95% CI 1–9). After a
median follow-up of 25.5 m (range: 7–63), median OS since first
line was 30 months (95% CI 18–42). Median PFS and OS in the 8
patients treated with pembro + 3wkCP were and 3 months (95% CI
1.1-4.8) and 11 months (95% CI 1.4-20.6), respectively (Tables IV and V, and Fig.
1, Fig. 2, Fig. 3, Fig.
4).
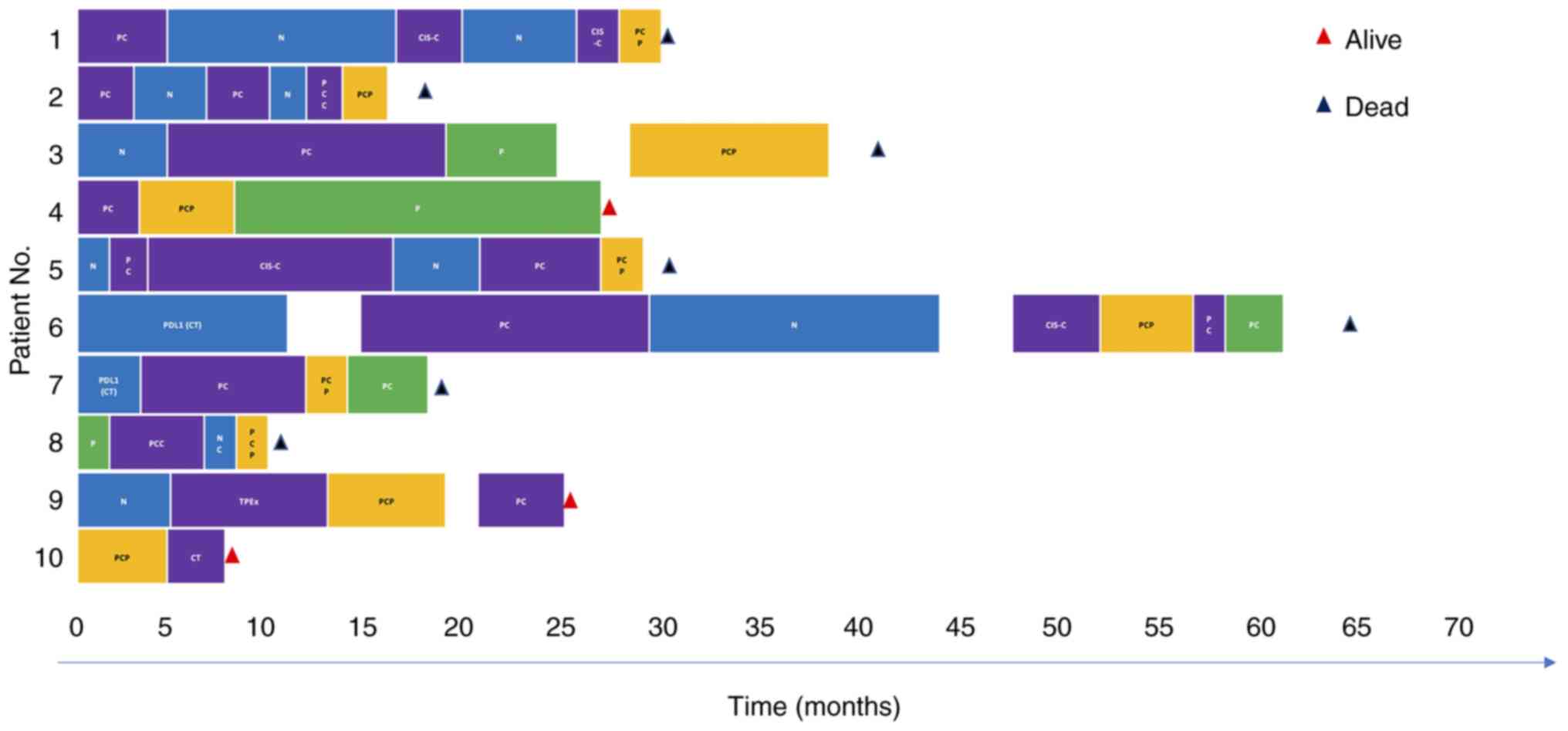
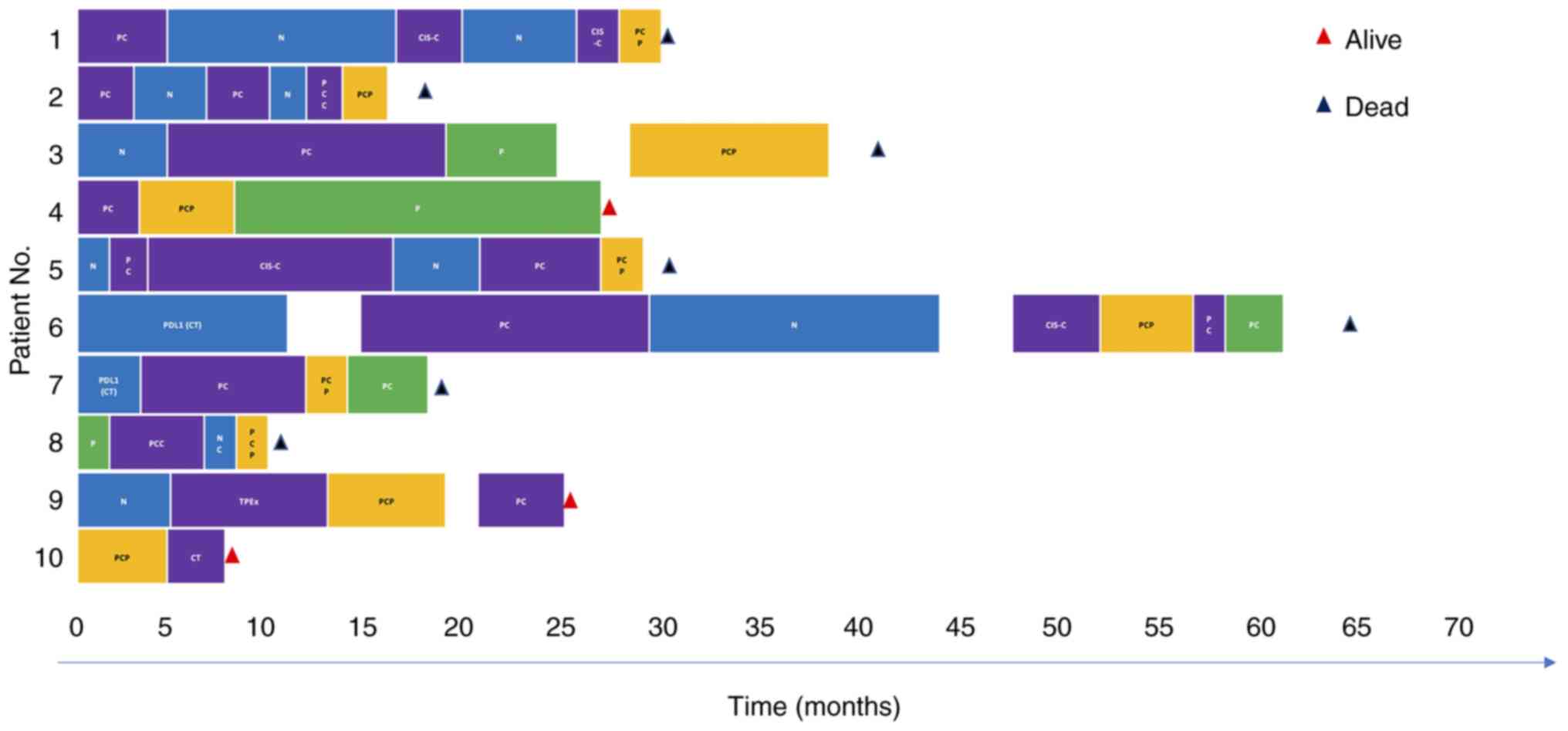 | Figure 4.Treatment history since the start of
first-line therapy in the 10 patients treated with pembro + CP.
Segmented bars show different colors that correspond to the
different therapeutic regimens used during the treatment journey of
each patient. The colors are as follows: Violet, cetuximab-based
chemotherapy; blue, nivolumab-based treatment; yellow,
pembrolizumab + CP; and green, pembrolizumab alone. Time is shown
in months. Patient 4 received 6 cycles of pembro + 3-weekly
carboplatin-paclitaxel (appears in yellow) followed by maintenance
therapy with pembrolizumab (appears in green; still ongoing), which
has been described in a previous publication (19). Patient 8 died from COVID19
pneumonia 2 weeks after starting pembro + CP. CIS-C, weekly
cisplatin + weekly cetuximab; CT, clinical trial; N, nivolumab; NC,
nivolumab + weekly cetuximab; P (green), pembrolizumab; PC
(violet), weekly paclitaxel and cetuximab; PC (green),
pembrolizumab + weekly cetuximab; PCC (violet), weekly carboplatin,
paclitaxel and cetuximab; PCP, pembro + CP; PDL1, anti-PDL1 agent;
pembro + CP, pembrolizumab-carboplatin-paclitaxel; TPEx, 3-weekly
docetaxel + 3-weekly platinum + weekly cetuximab. |
Fig. 4 summarizes
the treatment journey since the first line of therapy in each of
the 10 patients included in the study.
Association of PDL1 expression with
response and survival
All patients had a CPS 31, and 8 patients
harbored a CPS ≥20. Patient 3 (CPS=10) and patient 7 (CPS=1) had a
CPS <20. In all patients CPS was performed in an archived tumor
sample obtained at initial diagnosis, and therefore in all cases
other therapies-either in the early or R/M settings-had been
administered between the time of biopsy collection and the start of
pembro + CP. No statistically significant associations nor
correlations were found between PDL1 expression measured through
the TPS or CPS and ORR, PFS and OS in the whole series as well as
in the 8 patients treated with pembro + 3wkCP (Table SIII).
Discussion
In this hypothesis-generating retrospective study of
10 patients with R/M SCCHN treated with pembro + CP, the regimen
was well tolerated with no new safety signals attributable to any
of the three systemic agents. Among the 8 patients treated with
three-weekly pembro + CP, there were 37.5% grade 3 AEs and there
were no grade 4 or 5 AEs. Among the 2 patients treated with
three-weekly pembrolizumab combined with weekly CP, there were no
grade 3–5 AEs. While our patients had a lower toxicity with pembro
+ CP than previously reported with a similar combination in the
Keynote-B10 trial in first-line R/M SCCHN patients-71% suffered
grade ≥3 AEs- and in patients with sqNSCLC in the first-line
setting-69.8% suffered grade ≥3 AEs-, it must be noted that dosing
of carboplatin and paclitaxel in our series was considerably lower
due to the heavily pre-treated status of the patients and their
poor ECOG (11,12). Probably for the same reasons,
toxicity in our series was lower than taxane-and-cisplatin-based
chemo-IO combinations previously used in the neoadjuvant setting in
patients with LA SCCHN (7–12). Of note, the three patients who
suffered from grade ≥3 AEs, all received pembro + 3wkCP and
treatment lasted for a minimum of 5 months. In addition, these
three patients, received pembro + 3wkCP in the first-, second- and
fourth-line settings, and thus were less pre-treated than most of
the other patients in the current study. Therefore, higher doses of
pembro + 3wkCP and longer treatment periods possibly explain the
higher rates of toxicity in these three patients compared to the
rest of the patients in the study.
Interestingly, none of the patients in our series
suffered from immune-related AEs other than grade 1–2 asthenia,
which could also be attributable to chemotherapy. Interestingly,
none of the three patients who suffered irAEs under a prior
ICI-therapy, developed irAEs during or after treatment with pembro
+ CP. Although probably explained by the small sample size of our
series, this is in contrast with results from Keynote-B10 in
patients treated with first-line pembro + CP in R/M SCCHN where
irAEs occurred in 26.1%, of which 4.3% where grade ≥3, as well as
in contrast with data from patients with sqNSCLC treated with
pembro + CP where a 28.8% rate of irAEs was reported, of which
10.8% where grade ≥3 (11,12).
In addition, treatment compliance was high for
patients treated with pembro + CP in our series. Only three
patients suffered delayed administration of pembro + CP due to
toxicity, with a median of 1 cycle delayed and a median delay of 7
days.
In the present series, only 1 complete response to
pembro + CP was achieved in an ICI-naïve and platinum-naïve patient
after suffering a bulky progression to weekly cetuximab +
paclitaxel - which can be found in a previous publication (19) - thereby reaching an ORR of 14%
among 7 patients evaluable for response. However, the unconfirmed
DCR (i.e. at first CT evaluation) was 43% and median DOT reached
4.5 months, which is notable considering that our patients were
fragile and heavily pretreated, which may indicate a potential
synergy of the combination of pembro + CP. Among 7 evaluable
patients, median PFS for pembro + CP was 5 months (95% CI 1–9) and
median OS was 6 months (95% CI 0.5-14). In the Keynote-B10 trial,
patients received pembrolizumab (200 mg/21d) + three-weekly
carboplatin (AUC5) and paclitaxel (175 mg/m2 d1 or 100
mg/m2 d1,8) in the first-line setting of R/M SCCHN.
Among 92 enrolled patients, ORR reached 43%, median PFS was 5.6
months and median OS achieved 12.1 months (12). In Checkmate-141, in an ICI-naïve
population, nivolumab compared to second-line standard-of-care
(SOC) chemotherapy achieved a median PFS of 2.0 months (vs. 2.3
months) and a median OS of 7.7 months (vs. 5.1 months) (20). Likewise, in Keynote-040,
pembrolizumab compared to second-line SOC chemotherapy in patients
with a TPS ≥50%, achieved a median OS of 11.6 months vs. 6.6
months, respectively (21).
However, it should be noted that in our series, patients had
received a median of three prior lines before pembro + CP and that
80% of the patients received pembro + CP as a third or further line
of therapy. Indeed, only two patients received pembro + CP as
first- or second line, respectively. In addition, 80% of the
patients had received treatment with anti-PD(L)1 agents before
pembro + CP. Although all the patients were also PDL1 positive with
80% harboring a CPS ≥20, and this may explain the notable PFS and
OS achieved, the low ORR compared to other chemo-IO combinations
such as pembro + PF in the Keynote-048 where ORR ranged from 35 to
42%, may be explained by the heavily pre-treated nature and reduced
chemotherapy dosing in our series (2).
Median OS since the first line achieved 30 months
(95% CI 18–42) in our series. In Keynote-048, pembrolizumab
combined with platinum-5FU administered for 6 cycles and then
followed by maintenance pembrolizumab up to a maximum of 35 cycles,
achieved a median OS of 14.7 months in patients with a CPS ≥20
(2). Although our results cannot
be compared to those from a large phase III trial, the fact that
only half of the patients in Keynote-048 received second-line
therapy after IO, while in the current study the median number of
treatment lines before pembro + CP was 3, with up to 80% of our
patients receiving prior therapy with anti-PD(L)1 agents, may
explain the prolonged survival times achieved (2). Indeed, prospective, and retrospective
evidence suggests sequential treatment with ICIs followed by
salvage chemotherapy associates with longer survival (22–27).
In addition, the use of ICI rechallenge may also allow to improve
outcomes in patients with R/M SCCHN and in other entities such as
NSCLC (25,28–30).
In a recently published series of 23 patients treated with ICIs
followed by cetuximab-based salvage chemotherapy, our group
reported a median OS of 28 months since the start of first-line
therapy. Up to 14 patients in that series had received rechallenge
with ICIs probably explaining this survival times (25). Wakasugi et al (30), in a recently published
retrospective series of 29 patients, reported that OS was
significantly longer in patients treated with ICI rechallenge
compared to those not receiving ICI rechallenge (17.5 vs. 5.8
months, P=0.034).
In our study 80% of the patients received pembro +
three-weekly CP and only 2 patients were treated with pembro +
wkCP, with the latter suffering from only grade 1–2 AEs although
treatment duration was only 2 months in both patients due to
progressive disease. While the limited sample does not allow to
make useful comparisons between the two regimens, dosing of
chemotherapy may be relevant in R/M SCCHN as has been shown in
other entities such as ovarian cancer, where taxane-based
dose-dense weekly regimens achieve longer PFS and OS than
three-weekly regimens with a better toxicity profile (31). In R/M SCCHN the combination of
weekly cetuximab + paclitaxel (wkPCx) has been shown to achieve
notable response and survival rates both in the first- and
second-line settings. Hitt et al (32), in a phase II non-randomized trial
demonstrated an ORR of 54% and a median PFS and OS of 4.2 months
and 8.1 months, respectively, in patients treated with first-line
wkPCx. In the second-line setting, Chevalier et al (33), reported an ORR of 16.4% and a
5.5-month median OS with wkPCx. In the Keynote-B10 study mentioned
before, there were no differences between using three-weekly
paclitaxel (175 mg/m2 d1) and weekly paclitaxel (100
mg/m2 d1,8), suggesting that weekly paclitaxel may be
similar in terms of efficacy with a potentially more favourable
toxicity profile (11).
Interestingly, taxane-based weekly chemotherapy combined with
cetuximab after progression to ICIs has been reported to achieve
higher responses with a favorable impact in survival compared to
historical data from the pre-ICI era (22–27).
For all these reasons, weekly taxane-based chemotherapy should be
further evaluated -and compared with three-weekly taxane-based
regimens (either in combination or sequentially with anti-PD(L)1
agents in R/M SCCHN).
The main limitations of the present study are its
small sample size, and that it is a heterogenous sample where
patients received pembro + CP at different dose-intensities and in
different lines of therapy being, therefore, variably pre-treated.
As initially planned, only 10 patients were enrolled since it was a
single-center study of a novel chemoimmunotherapy combination in
R/M SCCHN. Therefore, these results can only be considered
hypothesis-generating. Although 8 of the 10 patients enrolled had
received prior therapy with ICIs, it was considered ethical to
offer pembro + CP to ICI-pretreated patients since they had no
other treatment options, the combination had been evaluated in a
phase III trial of patients with sqNSCLC and the study allowed to
use weekly instead of three-weekly doses of chemotherapy to reduce
toxicity and favor treatment compliance (12). Besides our own experience with ICI
rechallenge-reported in a previous publication (25), other authors have reported on the
feasibility, favorable toxicity profile and potential positive
impact in survival of ICI rechallenge in R/M SCCHN (25,28–30).
In summary, although our series is limited by its reduced sample
size and its heterogeneity and therefore the main conclusions that
can be drawn are related to safety, the preliminary activity
results are relevant considering that the median duration of
treatment reached 4.5 months and median OS since the start of
Pembro + CP achieved 6 months as a median 4th line of therapy. To
our knowledge this is the second reported evidence of a
taxane-based chemo-IO combination in the R/M setting. Finally, it
would have been of interest to have biopsies for biomarker and
immune-related studies prior to the start of pembro + CP that could
aid in understanding the role of this chemo-IO combination.
Currently ongoing trials combining anti-PD(L)1 agents with a
taxane-based chemotherapy backbone (NCT04282109, NCT04858269,
NCT04857164, NCT04943445, NCT03944915, NCT03829722, NCT03723967,
NCT03174275, NCT02658214) will provide more data on the safety and
potential benefit of such combinations for patients with head and
neck cancer (Table VI).
 | Table VI.Currently ongoing studies evaluating
the role of taxane-based chemo-immunotherapy combinations in head
and neck cancer. |
Table VI.
Currently ongoing studies evaluating
the role of taxane-based chemo-immunotherapy combinations in head
and neck cancer.
| ClinicalTrials.gov (other study IDs) | Study design | No. | Design details | Primary
endpoint | Secondary
endpoints | Status |
|---|
| NCT04282109
(NIVOTAX) | Randomized phase II
(1st line) | 141 | Exp. Arm, Nivo +
wkPaclitaxel; Control arm: Cetux + wkPaclitaxel | 2-year OS | PFS, ORR, DCR, DoR,
safety | Active. Recruitment
completed |
| NCT04858269 | Non-randomized
phase II (1st line) | 35 | Pembro + CBDCA
(AUC1.5) d1,8,15 + Paclitaxel (45 mg/m2 d1,8,15) | ORR | PFS, OS,
safety | Recruiting |
| NCT04857164 | Non-randomized
phase II (1st line) | 20 | Pembro + Platinum
+Nab-paclitaxel | ORRPFS, OS,
safety | DCR, DoR, | Recruiting |
| NCT04943445 (SMART
KEY) | Non-randomized
phase II (LA) | 42 | Pembro +
CBDCA(AUC6) + Paclitaxel (175 mg/m2) followed by RT +
Pembro | 2-year LFS | 2-year LDFS | Recruiting |
| NCT03944915
(DEPEND) | Non-randomized
phase II (LA HPV-) | 36 | Arm 1, Nivo +
3wkCBDCA + wkPaclitaxel; Arm 2, Radical CRT | DRR | PFS, OS, LRFS,
DMFS | Recruiting |
| NCT03829722 | Non-randomized
phase II (LA HPV+) | 40 | Nivo + CBDCA +
Paclitaxel + RT followed by Adj Nivo | 2-year PFS | 2-year OS,
safety | Recruiting |
| NCT03723967 (GORTEC
2018-03/FRAIL-IMMUNE) | Non-randomized
phase II (1st line) | 102 | Durva + CBDCA +
Paclitaxel | 1-year OS | PFS, TTF, ORR, BOR,
DoR, QoL | Recruiting |
| NCT03174275 | Non-randomized
phase II (LA) | 39 | Low-risk, Durva +
followed by SX wkNab-paclitaxel followed by SX followed by Adj
Durva; Medium risk, Durva + wkCBDCA + wkNab-paclitaxel followed by
SX followed by wkCDDP + RT followed by Adj Durva; High risk, Durva
+ wkCBDCA + wkNab-paclitaxel followed by SX followed by wkCDDP + RT
followed by Adj Durva | pCR after
iCT-IO | cCRR, CRL, PFS, OS,
safety | Active. Not
recruiting |
| NCT02658214 | Non-randomized
phase Ib (1st line) | 32 (various solid
tumors) | Durva + Treme +
CBDCA + Paclitaxel | Safety and
tolerability | - | Recruitment
completed |
In conclusion, in this small retrospective series of
heavily pretreated and/or fragile patients with R/M SCCHN, the
combination of pembrolizumab plus carboplatin and paclitaxel
associated with a manageable toxicity profile and preliminary signs
of activity in terms of progression-free and overall-survival. Data
from ongoing and future studies using platinum-and-taxane-based
chemoimmunotherapy combinations are eagerly awaited to better
understand their role in head and neck cancer.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SCC conceptualized, supervised and administered the
study and designed the methodology, performed the investigations,
obtained the resources and conducted the formal analysis and
curation of the data, and prepared the original draft of the
manuscript and was responsible for the writing of the manuscript as
well as its review and editing. SMM, MNCM, MJS, JCPH, FF and MCIM
performed the investigations, obtained the resources and conducted
the formal analysis and curation of the data. PPS supervised the
study and performed the investigations, obtained the resources and
conducted the formal analysis and curation of the data. SCC and MJS
confirm the authenticity of all the raw data. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Institutional
Review Board of Hospital Clínico Universitario San Carlos (IRB code
19/157-E; Madrid, Spain) and was conducted in accordance with the
principles of the Declaration of Helsinki. All patients signed an
informed consent form before starting pembro + CP as part of a
compassionate use program, approved by the Compassionate Use
Therapy Commission of Hospital Clínico Universitario San Carlos
(Madrid, Spain). The requirement of informed consent for conducting
this research was waived as the study was based on a retrospective
analysis of existing administrative and clinical data.
Patient consent for publication
Not applicable.
Competing interests
SCC has worked as a consultant and as a Speaker's
Bureau representative for Bristol-Myers Squibb, Merck and MSD, and
has received grant/research support from clinical trials with
AstraZeneca, MSD and Merck. PPS has also worked as a consultant and
as a Speaker's Bureau representative for Bristol-Myers Squibb,
Merck and MSD, and received grant/research support from clinical
trials with Bristol-Myers Squibb, AstraZeneca and MSD. The
remainder of the authors declare that they have no competing
interests.
References
|
1
|
Ferris RL, Blumenschein G Jr, Fayette J,
Guigay J, Colevas AD, Licitra L, Harrington K, Kasper S, Vokes EE,
Even C, et al: Nivolumab for recurrent squamous-cell carcinoma of
the head and neck. N Engl J Med. 375:1856–1867. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Burtness B, Harrington KJ, Greil R,
Soulières D, Tahara M, de Castro G Jr, Psyrri A, Basté N, Neupane
P, Bratland Å, et al: Pembrolizumab alone or with chemotherapy
versus cetuximab with chemotherapy for recurrent or metastatic
squamous cell carcinoma of the head and neck (KENOTE-048): A
randomised, open-label, phase 3 study. Lancet. 394:1915–1928. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Galluzzi L, Senovilla L, Zitvogel L and
Kroemer G: The secret ally: Immunostimulation by anticancer drugs.
Nat Rev Drug Discov. 11:215–233. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
4
|
Allen CT, Clavijo PE, Van Waes C and Chen
Z: Anti-tumor immunity in head and neck cancer: Understanding the
evidence, how tumors escape and immunotherapeutic approaches.
Cancers (Basel). 7:2397–2414. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Szturz P, Cristina V, Gómez RGH, Bourhis
J, Simon C and Vermorken JB: Cisplatin eligibility issues and
alternative regimens in locoregionally advanced head and neck
cancer: Recommendations for clinical practice. Front Oncol.
9:4642019. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ahn MJ, D'Cruz A, Vermorken JB, Chen JP,
Chitapanarux I, Dang HQT, Guminski A, Kannarunimit D, Lin TY, Ng
WT, et al: Clinical recommendations for defining platinum
unsuitable head and neck cancer patient populations on
chemoradiotherapy: A literature review. Oral Oncol. 53:10–16. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rosenberg AJ, Agrawal N, Pearson A, Gooi
Z, Blair E, Cursio J, Juloori A, Ginat D, Howard A, Chin J, et al:
Risk and response adapted de-intensified treatment for
HPV-associated oropharyngeal cancer: Optima paradigm expanded
experience. Oral Oncol. 122:1055662021. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hecht M, Gostian AO, Eckstein M, Rutzner
S, Von Der Grün J, Illmer T, Hautmann MG, Klautke G, Laban S,
Brunner T, et al: Safety and efficacy of single cycle induction
treatment with cisplatin/docetaxel/durvalumab/tremelimumab in
locally advanced HNSCC: First results of CheckRad-CD8. J Immunother
Cancer. 8:e0013782020. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Semrau S, Gostian AO, Traxdorf M, Eckstein
M, Rutzner S, von der Grün J, Illmer T, Hautmann M, Klautke G,
Laban S, et al: Implementation of double immune checkpoint blockade
increases response rate to induction chemotherapy in head and neck
cancer. Cancers (Basel). 13:19592021. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hecht M, Eckstein M, Rutzner S, Von Der
Grün J, Illmer T, Klautke G, Laban S, Hautmann MG, Brunner TB,
Tamaskovics B, et al: Induction chemoimmunotherapy followed by CD8+
immune cell-based patient selection for chemotherapy-free
radioimmunotherapy in locally advanced head and neck cancer. J
Immunother Cancer. 10:e0037472022. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dzienis MR, Cundom JE, Fuentes CS, Hansen
AR, Nordlinger MJ, Pastor AV, Oppelt P, Neki A, Gregg RW, Lima PF,
et al: 651O-Pembrolizumab (pembro) + carboplatin (carbo) +
paclitaxel (pacli) as first-line (1L) therapy in
recurrent/metastatic (R/M) head and neck squamous cell carcinoma
(HNSCC): Phase VI KEYNOTE-B10 study. Ann Oncol. 33 (Suppl
7):S295–S322. 2022. View Article : Google Scholar
|
|
12
|
Paz-Ares L, Luft A, Vicente D, Tafreshi A,
Gümüş M, Mazières J, Hermes B, Çay Şenler F, Csőszi T, Fülöp A, et
al: Pembrolizumab plus chemotherapy for squamous non-small-cell
lung cancer. N Engl J Med. 379:2040–2051. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cabezas-Camarero S, Alonso-Ovies A,
Merino-Menéndez S, Cabrera-Martín MN, Plaza-Hernández JC and
Pérez-Segura P: Major pathological response and durable
locoregional control after neoadjuvant
pembrolizumab-carboplatin-paclitaxel in head and neck cancer. Oral
Oncol. 123:1055892021. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Guigay J, Aupérin A, Fayette J,
Saada-Bouzid E, Lafond C, Taberna M, Geoffrois L, Martin L,
Capitain O, Cupissol D, et al: Cetuximab, docetaxel, and cisplatin
versus platinum, fluorouracil, and cetuximab as first-line
treatment in patients with recurrent or metastatic head and neck
squamous-cell carcinoma (GORTEC 2014-01 TPExtreme): A multicentre,
open-label, randomised, phase 2 trial. Lancet Oncol. 22:463–475.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Vitzthum LK, Feng CH, Noticewala S, Hines
PJ, Nguyen C, Zakeri K, Sojourner EJ, Shen H and Mell LK:
Comparison of comorbidity and frailty indices in patients with head
and neck cancer using an online tool. JCO Clin Cancer Inform.
2:1–9. 2018. View Article : Google Scholar
|
|
16
|
Eisenhauer EA, Therasse P, Bogaerts J,
Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S,
Mooney M, et al: New response evaluation criteria in solid tumours:
Revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tsimberidou AM, Levit LA, Schilsky RL,
Averbuch SD, Chen D, Kirkwood JM, McShane LM, Sharon E, Mileham KF
and Postow MA: Trial reporting in immuno-oncology (TRIO): An
American society of clinical oncology-society for immunotherapy of
cancer statement. J Clin Oncol. 37:72–80. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
de Ruiter EJ, Mulder FJ, Koomen BM, Speel
EJ, van den Hout MFCM, de Roest RH, Bloemena E, Devriese LA and
Willems SM: Comparison of three PD-L1 immunohistochemical assays in
head and neck squamous cell carcinoma (HNSCC). Mod Pathol.
34:1125–1132. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cabezas-Camarero S, Cabrera-Martin MN,
Saiz-Pardo Sanz M and Perez-Segura P: Major and durable response to
second-line pembrolizumab-carboplatin-paclitaxel in an oral cavity
cancer patient. Anticancer Drugs. 32:580–584. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ferris RL, Blumenschein G Jr, Fayette J,
Guigay J, Colevas AD, Licitra L, Harrington KJ, Kasper S, Vokes EE,
Even C, et al: Nivolumab vs investigator's choice in recurrent or
metastatic squamous cell carcinoma of the head and neck: 2-Year
long-term survival update of CheckMate 141 with analyses by tumor
PD-L1 expression. Oral Oncol. 81:45–51. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Cohen EEW, Soulières D, Le Tourneau C,
Dinis J, Licitra L, Ahn MJ, Soria A, Machiels JP, Mach N, Mehra R,
et al: Pembrolizumab versus methotrexate, docetaxel, or cetuximab
for recurrent or metastatic head-and-neck squamous cell carcinoma
(KEYNOTE-040): A randomised, open-label, phase 3 study. Lancet.
393:156–167. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Harrington KJ, Burtness B, Greil R,
Soulières D, Tahara M, de Castro G Jr, Psyrri A, Brana I, Basté N,
Neupane P, et al: Pembrolizumab with or without chemotherapy in
recurrent or metastatic head and neck squamous cell carcinoma:
Updated results of the phase III KEYNOTE-048 study. J Clin Oncol.
Oct 11–2022.(Epub ahead of print). View Article : Google Scholar
|
|
23
|
Saleh K, Daste A, Martin N, Pons-Tostivint
E, Auperin A, Herrera-Gomez RG, Baste-Rotllan N, Bidault F, Guigay
J, Le Tourneau C, et al: Response to salvage chemotherapy after
progression on immune checkpoint inhibitors in patients with
recurrent and/or metastatic squamous cell carcinoma of the head and
neck. Eur J Cancer. 121:123–129. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Pestana RC, Becnel M, Rubin ML, Torman DK,
Crespo J, Phan J, Hanna E, Bell D, Glisson BS, Johnson JM, et al:
Response rates and survival to systemic therapy after immune
checkpoint inhibitor failure in recurrent/metastatic head and neck
squamous cell carcinoma. Oral Oncol. 101:1045232020. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Cabezas-Camarero S, Cabrera-Martín MN,
Merino-Menéndez S, Paz-Cabezas M, García-Barberán V, Sáiz-Pardo
Sanz M, Iglesias-Moreno M, Alonso-Ovies A and Pérez-Segura P:
Safety and efficacy of cetuximab-based salvage chemotherapy after
checkpoint inhibitors in head and neck cancer. Oncologist.
26:e1018–e1035. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Suzuki S, Toyoma S, Kawasaki Y, Koizumi K,
Iikawa N, Shiina K, Endo T, Abe T, Kouga T and Yamada T: Clinical
outcomes of cetuximab and paclitaxel after progression on immune
checkpoint inhibitors in recurrent or metastatic head and neck
squamous cell carcinoma. Medicina (Kaunas). 57:11512021. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Fushimi C, Okamoto I, Matsuki T, Masubuchi
T, Okada T, Sato H, Tsukahara K, Kondo T, Yamashita T, Hanyu K, et
al: Salvage chemotherapy after nivolumab for recurrent or
metastatic head and neck carcinoma. Anticancer Res. 40:5277–5283.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Katayama Y, Shimamoto T, Yamada T, Takeda
T, Yamada T, Shiotsu S, Chihara Y, Hiranuma O, Iwasaku M, Kaneko Y,
et al: Retrospective efficacy analysis of immune checkpoint
inhibitor rechallenge in patients with non-small cell lung cancer.
J Clin Med. 9:1022019. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Gobbini E, Toffart AC, Pérol M, Assié JB,
Duruisseaux M, Coupez D, Dubos C, Westeel V, Delaunay M, Guisier F,
et al: Immune checkpoint inhibitors rechallenge efficacy in
non-small-cell lung cancer patients. Clin Lung Cancer.
21:e3497–e510. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wakasugi T, Takeuchi S, Ohkubo JI and
Suzuki H: Retreatment with nivolumab for patients with recurrent
and/or metastatic head and neck cancer. Acta Otolaryngol.
142:206–212. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Katsumata N, Yasuda M, Isonishi S,
Takahashi F, Michimae H, Kimura E, Aoki D, Jobo T, Kodama S,
Terauchi F, et al: Long-term results of dose-dense paclitaxel and
carboplatin versus conventional paclitaxel and carboplatin for
treatment of advanced epithelial ovarian, fallopian tube, or
primary peritoneal cancer (JCOG 3016): A randomised, controlled,
open-label trial. Lancet Oncol. 14:1020–1026. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Hitt R, Irigoyen A, Cortes-Funes H, Grau
JJ, García-Sáenz JA and Cruz-Hernández JJ; Spanish Head and Neck
Cancer Cooperative Group (TTCC), : Phase II study of the
combination of cetuximab and weekly paclitaxel in the first-line
treatment of patients with recurrent and/or metastatic squamous
cell carcinoma of the head and neck. Ann Oncol. 23:1016–1022. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Chevalier T, Daste A, Saada-Bouzid E,
Loundou A, Peyraud F, Lambert T, Le Tourneau C, Peyrade F, Dupuis
C, Alfonsi M, et al: Cetuximab combined with paclitaxel or
paclitaxel alone for patients with recurrent or metastatic head and
neck squamous cell carcinoma progressing after EXTREME. Cancer Med.
10:3952–3963. 2021. View Article : Google Scholar : PubMed/NCBI
|