Introduction
Gynecological malignancies are the leading cause of
female mortality in the United States (1). Despite advancements in the
identification and treatment of gynecological malignancies, the
survival rate has remained constant for decades (2). Gynecological cancers predominately
comprise cervical, endometrial and ovarian cancers (3). Surgical care for these malignancies
has transformed during the past decade as a result of the
development of techniques that are less invasive such as
laparoscopic and robotic surgeries.
As a result of the US Federal Drug Administration's
approval of the da Vinci Surgical System for gynecological surgery
in 2005, the use of robot-assisted surgery in the treatment of
gynecological malignancies has become more common (4). There are several benefits to using
robotic technology, including 3D and high-definition optics,
endoscopic devices that may be used in numerous ways, the removal
of human tremors, and greater accuracy and autonomy for the surgeon
(5–7). The advantages of robot-assisted
surgery over conventional laparoscopic surgery are mainly due to
these aforementioned factors (8).
Women with gynecological malignancies who have
solitary pelvic lymph node or para-aortic lymph node metastases at
the time of their first diagnosis have a poor prognosis (9,10). It
is possible to compare the number of clear lymph nodes in
gynecological cancers treated with robotic surgery and traditional
laparoscopic surgery, to assess the relative benefits and drawbacks
of the two surgical methods in terms of prognosis. Lymph node
dissection is a controversial procedure, and the outcomes of the
two surgical approaches are still debated (11,12).
Robot-assisted surgery and laparoscopic surgery may not vary
significantly in the number of lymph node dissections, according to
certain previous reports (13,14).
However, numerous studies reported that robotic surgery has a
higher lymph node clearance rate than laparoscopic surgery
(15,16). Therefore, this meta-analysis used
evidence-based medicine to explore the difference in the number of
lymph nodes retrieved in gynecological cancer between robotic
surgery and laparoscopic surgery by pooling the results of relevant
previous studies.
Materials and methods
Protocol registration
The protocol used for the present study was
registered in the International Platform of Registered Systematic
Review and Meta-analysis Protocols (https://inplasy.com/), the registration number was
INPLASY2022120046 (DOI, 10.37766/inplasy2022.12.0046).
Literature inclusion and exclusion
criteria
The following inclusion criteria were used for
reports in the literature: The study was a cohort study or a
randomized controlled trial (RCT) study; the study was reported in
either English or Chinese; and studies where the observation group
was treated by robotic surgery for gynecological cancer (taken to
include cervical cancer, ovarian cancer and endometrial cancer) and
the control group was treated by laparoscopic surgery for
gynecological cancer.
The following exclusion criteria were used for
reports in the literature: Repeated publication of the same study;
studies without full text, incomplete information or for which data
extraction could not be performed; animal experiments; and reviews
and systematic reviews.
Search strategy
The Pubmed (https://pubmed.ncbi.nlm.nih.gov/), Embase (https://www.embase.com), Cochrane library (https://www.cochranelibrary.com/), China National
Knowledge Infrastructure (https://www.cnki.net/) and Wanfang (https://www.wanfangdata.com.cn/index.html) literature
databases were used in the present meta-analysis, and were searched
between their formation and January 1st 2021. The mesh terms used
were as follows: ‘robotic-assisted’, ‘robotic surgery’ and
‘laparoscopic’, ‘laparoscopy’ and ‘gynecological cancer’, ‘Uterine
Cervical Neoplasms’, ‘Endometrial Neoplasms’, ‘Ovarian Neoplasms’.
Detailed search strategies were presented in Data S1.
Literature screening and data
extraction
The literature search, screening and extraction of
relevant material was completed by two researchers, separately.
When there were questions or conflicts, a third person was
consulted before making a decision. Basic features (author, year,
research type, field of research on gynecological cancers, number
of patients, age of patients and place of diagnosis) and outcome
indicators (number of retrieved pelvic lymph nodes and para-aortic
lymph nodes, operative time, estimated blood loss, recurrence rate
and mortality rate) were included in the data extracted.
Literature quality assessment
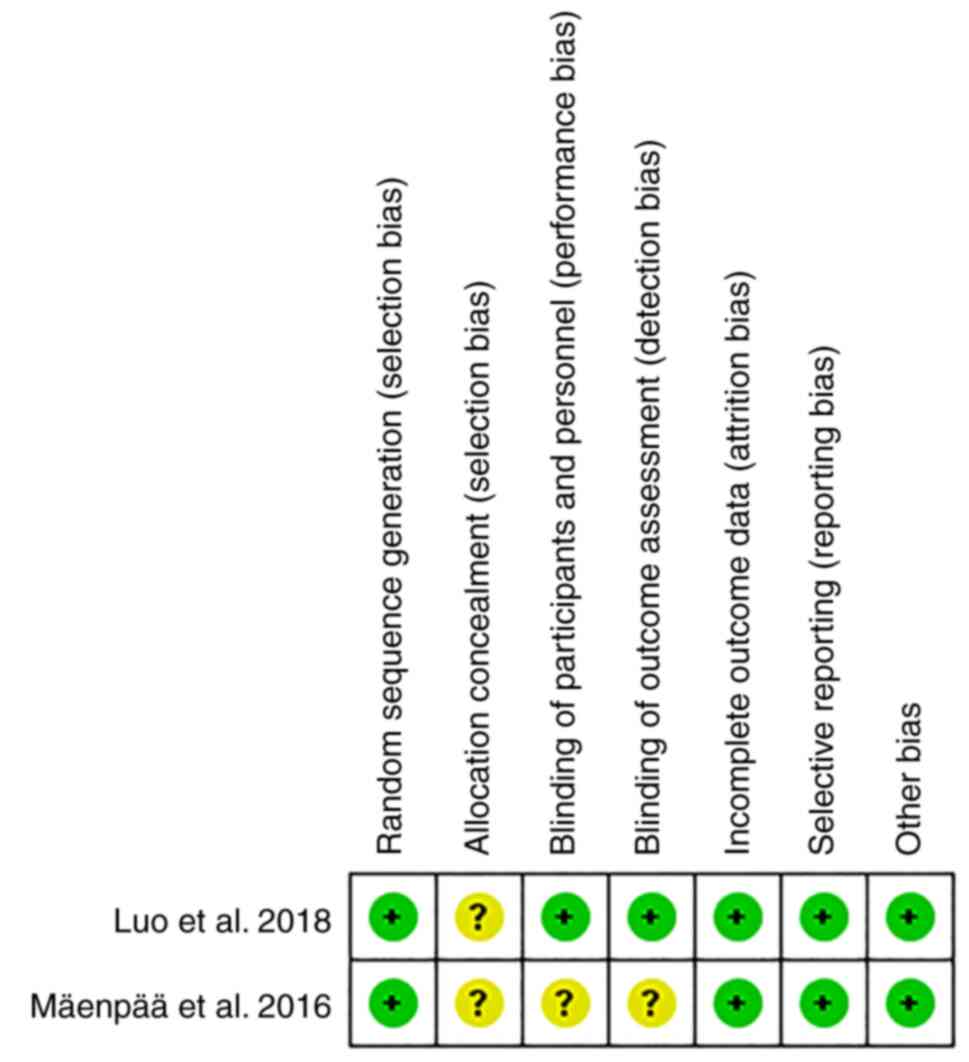
The Newcastle-Ottawa Scale (NOS) for evaluating the
quality of published literature was performed separately by two
academics (17)], in the present
study it was used to evaluate the quality of the 16 cohort studies.
The NOS includes 4 items (4 points) for ‘Research Subject
Selection’, 1 item (2 points) for ‘Comparability between Groups’
and 3 items (3 points) for ‘Result Measurement’, for a maximum
score of 9 points. A score of ≥7 is classified as high-quality
literature, <7 is classified into lower-quality literature.
Following assessment using the NOS, the quality of the remaining
two RCT studies was assessed against the Cochrane Risk Assessment
Scale using the ReviewManager 5.3 (Cochrane) software risk
assessment tool.
Data synthesis and statistical
analysis
The data was analyzed using the STATA (version 15.1,
StataCorp LP) (18). The present
study used the combined effect size of standard mean difference
(SMD) (with a 95% confidence interval) as a continuous variable to
assess the number of retrieved pelvic lymph nodes and para-aortic
lymph nodes, as well as the amount of time spent operating and
estimated blood loss, and the odds ratio (OR; with a 95% confidence
interval) as a binary variable to measure the rates of recurrence
and mortality. The I2 statistic was used to determine
the degree of heterogeneity. If the results of the test for
heterogeneity were P≥0.1 and I2≤50%, this indicated that
the studies were homogeneous, and the fixed effects model (I–V) was
used for combined analysis; however, if the results were P<0.1
and I2>50%, this indicated that the studies were
heterogeneous. Since heterogeneity is always expected for the
intervention effects among multiple studies from different groups
and geographical locations, only the random effects model was used
to combine the results. Sensitivity analysis or subgroup analysis
was required to identify the source of heterogeneity. If the
heterogeneity was still large, the random effects model (D+L) was
used or the combination of results was stopped and descriptive
analysis was used. Egger's bias test was used to analyze the
publication prejudice.
Results
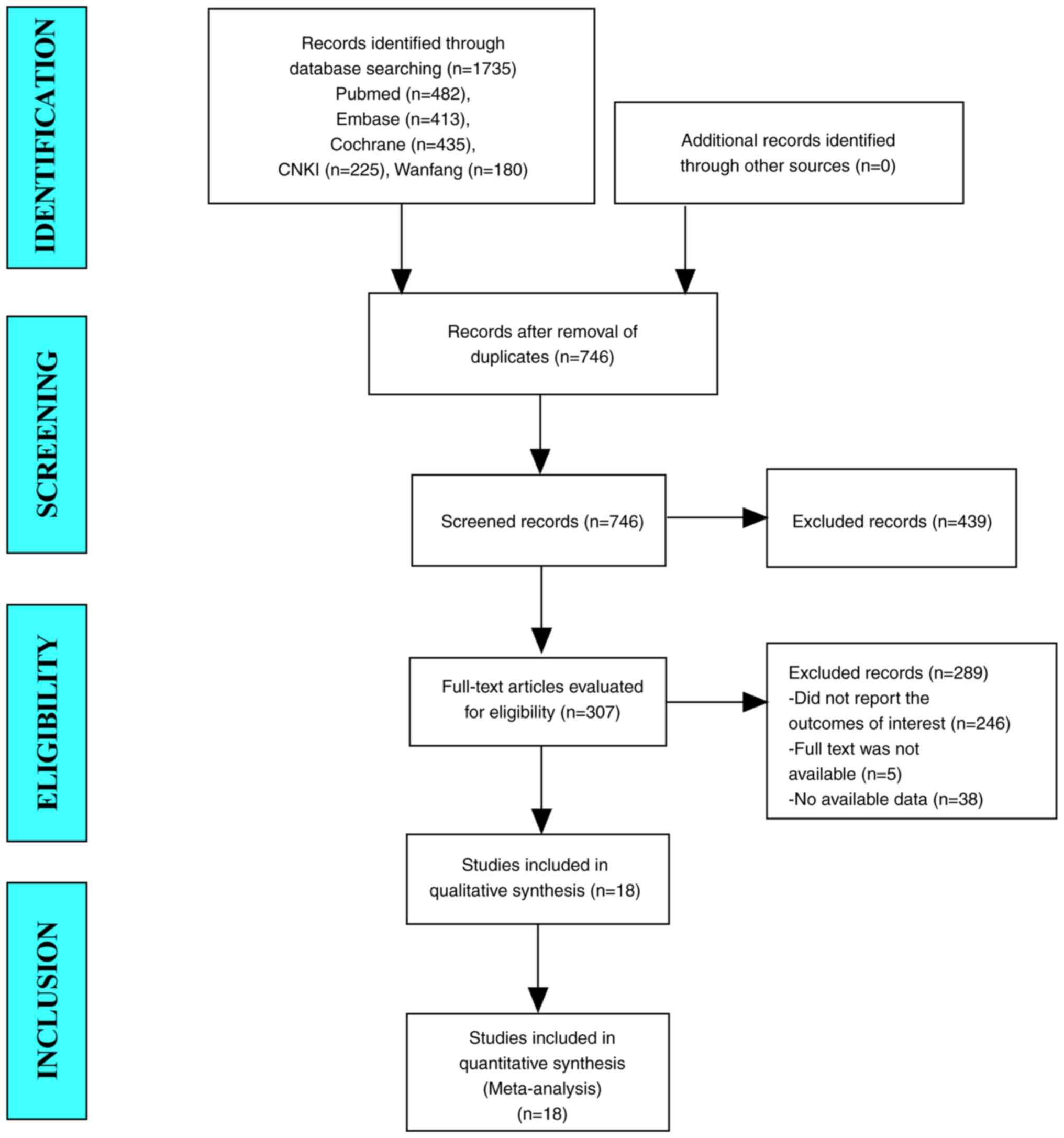
The results of literature search
In total, the database search yielded 1735 studies.
A total of 746 studies remained after duplicates were removed.
After browsing titles and abstracts, 307 studies were evaluated.
Finally, 18 papers were finally meta-analyzed after being read in
their entirety (Fig. 1).
Baseline characteristics and quality assessment
of the included studies
Baseline characteristics
The present meta-analysis included 18 publications,
16 of which were cohort studies and two of which were RCTs. The
sample sizes ranged from 42 to 933, and the present meta-analysis
included a total of 2,381 patients (all women; age, >44.1
years). Among the included studies, 11 reported cervical cancer,
three reported ovarian cancer, three reported endometrial cancer
and one reported gynecological cancers, including cervical cancer,
ovarian cancer and endometrial cancer. A total of 16 cohort studies
had NOS ratings of at ≥7 and satisfied all other conditions
(Table I). The quality evaluation
of the randomized controlled trials was presented in Fig. 2.
 | Table I.The baseline characteristics and
quality assessment of the cohort studies. |
Table I.
The baseline characteristics and
quality assessment of the cohort studies.
|
|
|
| No. patients | Age, years (mean ±
SD or median with range) |
|
|
|
|---|
|
|
|
|
|
|
|
|
|
|---|
| First author/s,
year | Study type | Study area | Robotic
surgery | Laparoscopic
surgery | Robotic
surgery | Laparoscopic
surgery | Site of
gynecological cancer | NOS score | (Refs.) |
|---|
| Magrina et
al, 2011 | Cohort | USA | 25 | 27 | 62.0±15.0 | 61.0±16.0 | Ovarian cancer | 7 | (27) |
| Sert and
Abeler, 2011 | Cohort | Norway | 35 | 7 | 44.1±10.5 | 45.0±12.9 | Cervical
Cancer | 8 | (28) |
| Chong et al,
2013 | Cohort | South Korea | 50 | 50 | 48.0±9.9 | 47.1±11.0 | Cervical
Cancer | 7 | (29) |
| Chen et al,
2014 [14] | Cohort | China | 24 | 32 | 53.7±15.3 | 51.2±11.9 | Cervical
Cancer | 7 | (14) |
| Coronado et
al, 2014 | Cohort | Spain | 32 | 30 | 57.5
(47.5–66.7) | 59.0
(38.6–66.3) | Gynecological
cancer | 8 | (30) |
| Díaz-Feijoo et
al, 2014 | Cohort | Spain | 83 | 17 | 51.0
(24.0–74.0) | 49.0
(29.0–66.0) | Cervical
Cancer | 7 | (31) |
| Yim et al,
2014 [11] | Cohort | South Korea | 60 | 42 | 46.3±9.9 | 49.8±11.4 | Cervical
Cancer | 7 | (11) |
| Chen et al,
2016 | Cohort | China | 44 | 21 | 44.3±12.3 | 43.8±10.3 | Ovarian cancer | 7 | (32) |
| Manchana et
al, 2015 | Cohort | Thailand | 28 | 47 | 55.5
(48.2–61.5) | 54.0
(49.0–62.0) | Endometrial
cancer | 7 | (33) |
| Gallotta et
al, 2017 | Cohort | Italy | 32 | 64 | 49.0
(32.0–76.0) | 49.0
(27.0–73.0) | Ovarian cancer | 8 | (15) |
| Mäenpää et
al, 2016 | RCT | Finland | 50 | 49 | 67.0
(43.0–84.0) | 70.0
(48.0–83.0) | Endometrial
cancer | / | (34) |
| Mendivil et
al, 2016 | Cohort | USA | 58 | 49 | 47.3±11.2 | 47.8±12.0 | Cervical
Cancer | 7 | (35) |
| Lee et al,
2018 | Cohort | South Korea | 26 | 16 | 56.7±6.9 | 51.1±7.8 | Endometrial
cancer | 8 | (4) |
| Pellegrino et
al, 2017 | Cohort | Italy | 34 | 18 | 46.9±9.5 | 48.2±13.1 | Cervical
Cancer | 8 | (36) |
| Nie et al,
2017 | Cohort | China | 100 | 833 | 47.1±9.5 | 45.9±8.9 | Cervical
Cancer | 7 | (37) |
| Luo et al,
2018 | RCT | China | 30 | 30 | 65.0
(62.0–67.0) | 64.0
(62.0–66.0) | Cervical
Cancer | / | (38) |
| Oyama et al,
2019 | Cohort | Japan | 64 | 57 | 43.4±12.2 | 44.9±12.3 | Cervical
Cancer | 7 | (16) |
| Loverix et
al, 2020 | Cohort | Belgium | 55 | 162 | 49.0
(22.0–79.0) | 48.0
(22.0–78.0) | Cervical
Cancer | 8 | (12) |
Results of the meta-analysis
Number of retrieved lymph nodes
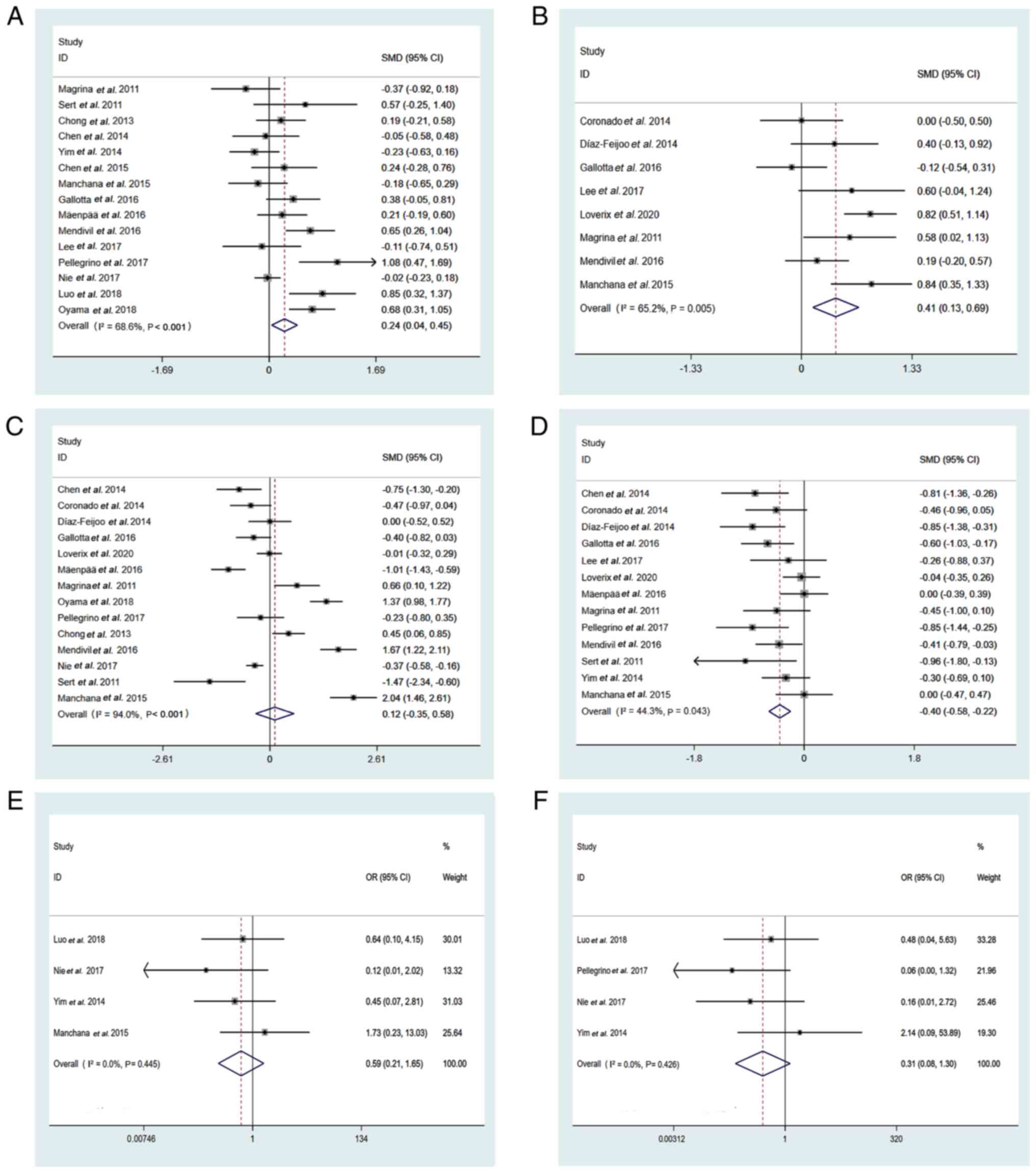
i) Number of retrieved pelvic lymph nodes. A total
of >2,000 patients participated in 15 studies, which reported on
the number of pelvic lymph nodes that were retrieved. The
meta-analysis was performed using a random-effects model because of
the large amount of variation in the data (I2=68.6%,
P<0.001). The pooled results demonstrated that the number of
pelvic lymph nodes retrieved by robotic surgery was significantly
higher than that of laparoscopic surgery (SMD=0.24; 95% CI,
0.04-0.45; P=0.007; Fig. 3A).
ii) Number of retrieved para-aortic lymph nodes. A
total of eight studies including 751 patients reported on the
number of para-aortic lymph nodes that were removed. Meta-analysis
was performed using a random-effects model due to significant
heterogeneity (I2=65.2%, P=0.004). The combined data
demonstrated that the number of para-aortic lymph nodes recovered
by robotic surgery was significantly greater than the number
retrieved by laparoscopic surgery, which was a considerable
improvement (SMD=0.41; 95% CI, 0.13-0.69; P=0.004; Fig. 3B).
Operation time
Operation time was recorded in 14 studies, which
included 2112 patients. To account for the substantial variability
in the data, a random effects model was used (I2=94.0%,
P<0.001). The data indicated that, robotic surgery and
laparoscopic surgery took the same amount of time to perform
(SMD=0.12; 95% CI, −0.35-0.58; P=0.616; Fig. 3C).
Estimated blood loss
A total of 13 studies including 1102 patients,
estimated blood loss. Because of the substantial heterogeneity,
meta-analysis was performed using a random-effects model
(I2=44.3%, P=0.043). There was a significant difference
in blood loss between robotic and laparoscopic surgery,
demonstrated by the pooled findings [SMD=−0.40; 95% CI,
−0.58-(−0.22); P<0.001; Fig.
3D].
Disease prognosis
i) Recurrence rate. A total of four studies,
including 1170 patients, reported recurrence rate. Meta-analysis
was performed using a random-effects model. Recurrence rates were
not significantly different between robotic and laparoscopic
surgery, according to the pooled statistics (OR=0.59; 95% CI,
0.21-1.65; P=0.318; Fig. 3E).
ii) Mortality rate. The death rate was recorded in 4
studies, which included 1147 patients. Meta-analysis was performed
using a random-effects model. Mortality rate was not significantly
different between robotic and laparoscopic surgery, according to
the pooled statistics (OR=0.31; 95% CI, 0.08-1.30; P=0.109;
Fig. 3F)
Subgroup analysis
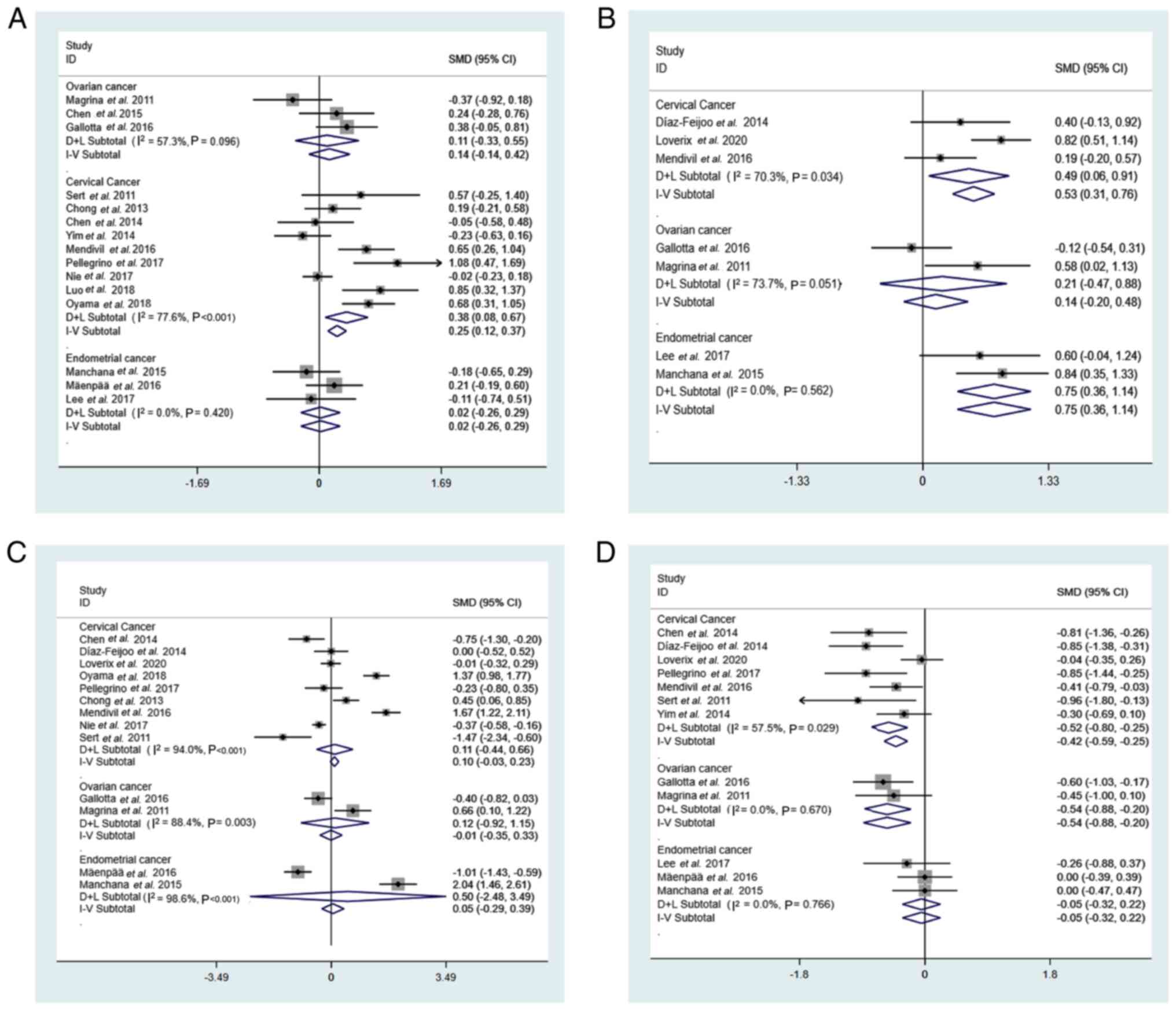
Subgroup analysis of the number of retrieved lymph
nodes, operation time and estimated blood loss according to
different gynecological cancers was performed.
Number of retrieved lymph nodes
i) Number of retrieved pelvic lymph nodes. The
pooled results showed that the number of pelvic lymph nodes
retrieved by robotic surgery was significantly larger than that
obtained by laparoscopic surgery in cervical cancer (SMD=0.38; 95%
CI, 0.08-0.67; P=0.012; I2=77.6%; P<0.001) (Fig. 4A). However, in ovarian cancer
(SMD=0.11; 95% CI, −0.33-0.55; P=0.634; I2=57.3%;
P=0.096) and endometrial cancer (SMD=0.02; 95% CI, −0.26-0.29;
P=0.904; I2=0.0%; P=0.420), the difference between
robotic surgery and laparoscopic surgery in the number of retrieved
pelvic lymph nodes was not statistically significant (Fig. 4A).
ii) Number of retrieved para-aortic lymph nodes. The
pooled results demonstrated that in cervical cancer (SMD=0.49; 95%
CI, 0.06-0.91; P=0.024; I2=70.3%, P=0.034) and
endometrial cancer (SMD=0.75; 95% CI, 0.36-1.14; P<0.001;
I2=0.0%; P=0.562), the number of para-aortic lymph nodes
retrieved by robotic surgery were significantly increased compared
with laparoscopic surgery (Fig.
4B). For ovarian cancer therapy, the number of para-aortic
lymph nodes removed by robotic surgery and laparoscopic surgery did
not differ significantly between the two techniques, according to
the results of the present meta-analysis (SMD=0.21; 95% CI,
−0.47-0.88; P=0.554; I2=73.7%; P=0.051; Fig. 4B).
Operation time
The pooled results demonstrated that in cervical
cancer (SMD=0.11; 95% CI, −0.44-0.66; P=0.701; I2=94.0%;
P<0.001), ovarian cancer (SMD=0.121; 95% CI, −0.92-1.15;
P=0.827; I2=88.4%; P=0.003) and endometrial cancer
(SMD=0.50; 95% CI, −2.48-3.49; P=0.616; I2=98.6%;
P<0.001), the difference in operation time between robotic
surgery and laparoscopic surgery was not statistically significant
(Fig. 4C).
Estimated blood loss
The pooled results demonstrated that in cervical
cancer [SMD=−0.52; 95% CI, −0.80-(−0.25); P<0.001;
I2=57.5%; P=0.029] and ovarian cancer [SMD=−0.54; 95%
CI, −0.88-(−0.20); P=0.002; I2=0.0%; P=0.670], the
estimated blood loss of robotic surgery was significantly lower
than that of laparoscopic surgery (Fig.
4D). There was no statistically significant difference in
estimated blood loss when compared between robotic surgery and
laparoscopic surgery for endometrial cancer (SMD=−0.05; 95% CI,
−0.32-0.22; P=0.725; I2=0.0%; P=0.766; Fig. 4D).
Sensitivity analysis
The remaining investigations were subjected to a
pooled analysis to assess whether any of the included studies had a
disproportionate influence on the meta-analysis's overall results,
which was accomplished using sensitivity analyses that eliminated
each included publication one at a time. The results of this
meta-analysis indicated that no research had a disproportionate
influence on its results, which suggested that the findings were
steady and credible (Fig. S1,
Fig. S2, Fig. S3, Fig.
S4, Fig. S5, Fig. S6).
Publication bias
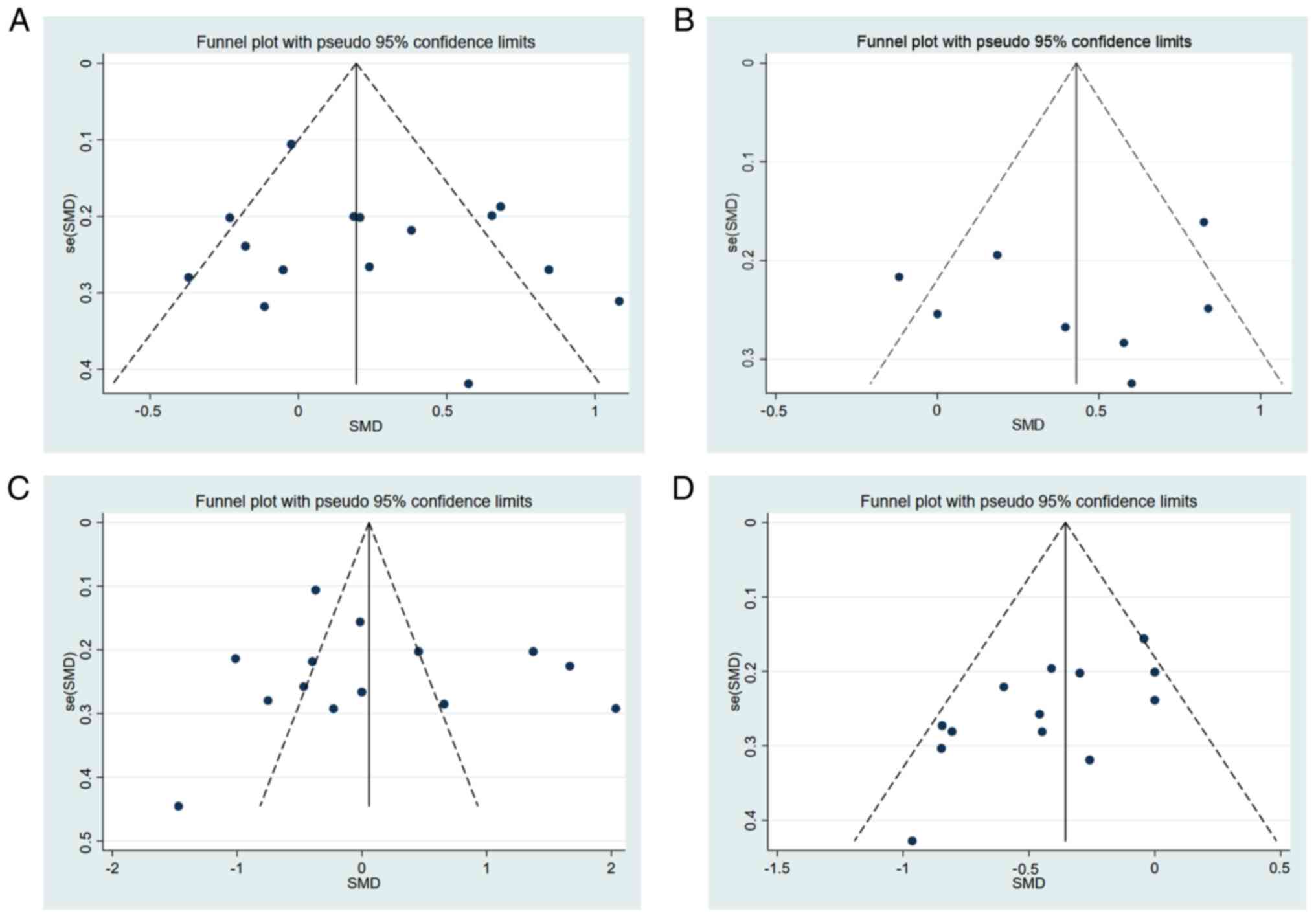
Egger's test (P=0.305; P=0.684; P=0.547; and
P=0.366) was used to assess the four funnel plots created in the
present study and found no significant publication bias was
demonstrated (Fig. 5).
Discussion
The development of minimally invasive technologies
is important in surgical systems. Minimally invasive surgery can
result in better treatment outcomes, faster recovery times, shorter
hospital stays, and reduced physical and psychological trauma
(19). Recently, a growing number
of studies have reported the efficiency and safety of da Vinci
robots for the treatment of benign and malignant gynecological
tumors (20–22). Due to subjective factors such as the
patient's subjective choice of surgical method, difficultly in
ensuring the informed consent of patients and their families with
randomized surgical methods and difficulty in achieving
double-blinding of the wound type after surgery, it is difficult to
randomize surgical methods. Therefore, clinical randomized
controlled trials exploring different surgical techniques are
currently lacking. Since lymph node metastasis has an impact on the
prognosis of tumors, including recurrence rate and mortality, it is
very important to evaluate the number of lymph nodes removed. This
meta-analysis included 18 articles with a total of 2,381 patients
who underwent either robotic surgery or conventional laparoscopic
surgery for gynecological cancers. The clinical outcomes of da
Vinci robot-assisted laparoscopic surgery for gynecological cancers
were compared with those of conventional laparoscopic surgery. The
number of lymph nodes removed (pelvic and abdominal aortic lymph
nodes), length of surgery, expected blood loss, recurrence rate and
mortality rate were analyzed.
The number of lymph nodes removed was the first
factor assessed. In 15 of the studies, a total of 2002 patients
underwent pelvic lymph node removal. The pooled results in the
present study demonstrated that the number of pelvic lymph nodes
retrieved by robotic surgery was significantly higher than that of
laparoscopic surgery (SMD=0.24; 95% CI, 0.04-0.45; P=0.007).
Furthermore, 751 patients in eight studies had their para-aortic
lymph nodes removed. The pooled results demonstrated that
significantly more para-aortic lymph nodes were removed using
robotic surgery compared with laparoscopic surgery (SMD=0.41; 95%
CI, 0.13-0.69; P=0.004). This result may be due to the ability of
the da Vinci robot's simulated wrist endoscopy operating instrument
to complete a 7-direction degrees of freedom operation, which means
it can reach positions that cannot be reached by human hands
(23). Consequently, the robotic
system can operate more precisely, allowing for the removal of more
lymph nodes. For gynecological cancers, lymph node metastases are
an essential channel of spread, and the positive identification
rate of lymph nodes is directly linked to postoperative therapy and
prognosis (24). The present study
performed subgroup analyses for different forms of gynecological
cancer. In cervical cancer, the number of pelvic lymph nodes
retrieved via robotic surgery was significantly greater than that
retrieved via laparoscopic surgery (SMD=0.38; 95% CI, 0.08-0.67;
P=0.012). The results of the present study also demonstrated that
only in cervical (SMD=0.49; 95% CI, 0.06-0.91; P=0.024) and
endometrial (SMD=0.75; 95% CI, 0.36-1.14; P<0.001) cancers were
the number of para-aortic lymph nodes retrieved by robotic surgery
significantly increased compared with laparoscopic surgery. This
may have been due to the differences in the anatomical morphology
of gynecological cancer at different locations, which suggested
that the combination of the number of lymph nodes removed with the
location of the gynecological cancer should be used to choose the
most appropriate surgical method for each patient.
A total of 14 publications, which included 2,112
patients, were pooled to examine the difference in operating time
between laparoscopic and robotic surgery. All available data
demonstrated that there was no significant difference in the
operating time between the two types of surgery (SMD=0.12; 95% CI,
−0.35-0.58; P=0.616). This result may be due to the da Vinci
robot-assisted laparoscopic system being an emerging technology and
surgical operators in different countries and regions have
different proficiencies in robotic and laparoscopic surgery. As the
proficiency of laparoscopic operators is improved, the operation
time will be reduced in the future. The difference in estimated
blood loss between robotic and laparoscopic surgery was also
assessed in the present study. Compared with laparoscopy, the
robot-assisted technique has been previously reported to minimize
blood loss in gynecological malignancies (25). The pooled results of the present
study also demonstrated that the estimated blood loss in robotic
surgery was significantly lower compared with that in laparoscopic
surgery [SMD=−0.40; 95% CI, −0.58-(−0.22), P<0.001]. This has
been reported to be because the robotic surgical system can provide
a high-definition, 10–15× magnification view of the surgical field
of view, which has a magnifying effect on blood vessels and can
avoid the problem of missing small blood vessels in the surgical
area (26). When the subsets of
patients were assessed, there was no statistically significant
difference in estimated blood loss between robotic and laparoscopic
surgery for endometrial cancer (SMD=−0.05; 95% CI, −0.32-0.22;
P=0.725), which indicated that the blood loss in certain sections
of the malignancy may vary.
The cancer recurrence and death rates were further
evaluated. Robotic surgery demonstrated a significantly lower death
rate compared with laparoscopic surgery (OR=0.2; 95% CI, 0.08-0.95;
P=0.041); however, there was no significant difference in
recurrence rate and mortality rate between the two procedures.
However, few studies have reported recurrence and mortality rates,
and other reasons, such as failure to complete postoperative
adjuvant treatment during the follow-up period, may affect the
postoperative recurrence rate and mortality rate for certain
patients. Therefore, to evaluate the long-term efficacy of robotic
surgery the sample size should expanded in further research.
This meta-analysis has several limitations. Firstly,
the majority of the studies included in this research were
retrospective cohort studies, with only two randomized controlled
studies; therefore, the quality of the literature was uneven, which
could lead to selection bias. Secondly, the literature included in
this study did not describe the surgeon's proficiency in the use of
the da Vinci Robotic Surgery System, laparoscopic surgery or open
surgery, and differences between surgeons' skills may also be a
reason for the heterogeneity in this study. Therefore, it will be
necessary to include additional studies in the future and expand
the sample size to further verify the findings of the present
study. Thirdly, as the patients included in each study were not all
at a specific cancer stage, it was not possible to perform further
subgroup analyses by cancer stage. Fourth, as the complication
rates analyzed in the included studies were all robotic surgery and
conventional laparoscopic surgery for gynecological cancers, it was
not possible to analyze complications after lymph node dissection.
If a relevant study is performed, a correlation analysis should be
performed.
The results of the present study have demonstrated
that lymph nodes from the pelvic and para-aortic areas may be
retrieved more effectively using robotic surgery than with
laparoscopy. The difference in operation time between the two
surgical methods w not statistically significant; however, the
estimated blood loss of robotic surgery is significantly lower than
that of traditional laparoscopic surgery. Furthermore, robotic
surgery has a significantly lower death rate than laparoscopic
surgery; however, the recurrence rates were not statistically
different.
Supplementary Material
Supporting Data
Supporting Data
Acknowledgements
Not applicable.
Funding
The present study was supported by the Guigang Self-funded
Scientific Research Project (grant no. 2100031).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YLu conceived the study and wrote the manuscript;
WL, YS, LL, RW and MW performed the acquisition of the data. YLi,
YC and YLu performed the data analyses; JC helped to perform the
analysis. YLu and YC confirm the authenticity of all the raw data.
All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Keyvani V, Kheradmand N, Navaei ZN,
Mollazadeh S and Esmaeili SA: Epidemiological trends and risk
factors of gynecological cancers: An update. Med Oncol. 40:932023.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wu Z, Tang H, Xiong Q, Liu D, Xia T, Liang
H and Ye Q: Prognostic role of microRNA-205 in human gynecological
cancer: A meta-analysis of fourteen studies. DNA Cell Biol.
39:875–889. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lu J, Gu Y, Li Q, Zhong H, Wang X, Zheng
Z, Hu W and Wen L: Wilms' tumor 1 (WT1) as a prognosis factor in
gynecological cancers: A meta-analysis. Medicine (Baltimore).
97:e114852018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lee HJ, Lee YH, Chong GO, Hong DG and Lee
YS: Comparison of robotic-assisted versus laparoscopy for
transperitoneal infrarenal para-aortic lymphadenectomy in patients
with endometrial cancer. J Obstet Gynaecol Res. 44:547–555. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Seamon LG, Cohn DE, Richardson DL,
Valmadre S, Carlson MJ, Phillips GS and Fowler JM: Robotic
hysterectomy and pelvic-aortic lymphadenectomy for endometrial
cancer. Obstet Gynecol. 112:1207–1213. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lowe MP, Johnson PR, Kamelle SA, Kumar S,
Chamberlain DH and Tillmanns TD: A multiinstitutional experience
with robotic-assisted hysterectomy with staging for endometrial
cancer. Obstet Gynecol. 114:236–243. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lim PC, Kang E and Park DH: A comparative
detail analysis of the learning curve and surgical outcome for
robotic hysterectomy with lymphadenectomy versus laparoscopic
hysterectomy with lymphadenectomy in treatment of endometrial
cancer: A case-matched controlled study of the first one hundred
twenty two patients. Gynecol Oncol. 120:413–418. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Holloway RW, Ahmad S, DeNardis SA,
Peterson LB, Sultana N, Bigsby GE IV, Pikaart DP and Finkler NJ:
Robotic-assisted laparoscopic hysterectomy and lymphadenectomy for
endometrial cancer: Analysis of surgical performance. Gynecol
Oncol. 115:447–452. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Diaz-Feijoo B, Luna-Guibourg R, Cabrera S,
Manrique S and Gil-Moreno A: Laparoscopic extraperitoneal pelvic
lymph node debulking in locally advanced cervical cancer. J Minim
Invasive Gynecol. 26:3662019. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Fastrez M, Goffin F, Vergote I, Vandromme
J, Petit P, Leunen K and Degueldre M: Multi-center experience of
robot-assisted laparoscopic para-aortic lymphadenectomy for staging
of locally advanced cervical carcinoma. Acta Obstet Gynecol Scand.
92:895–901. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yim GW, Kim SW, Nam EJ, Kim S, Kim HJ and
Kim YT: Surgical outcomes of robotic radical hysterectomy using
three robotic arms versus conventional multiport laparoscopy in
patients with cervical cancer. Yonsei Med J. 55:1222–1230. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Loverix L, Salihi RR, Van Nieuwenhuysen E,
Concin N, Han S, van Gorp T and Vergote I: Para-aortic lymph node
surgical staging in locally-advanced cervical cancer: Comparison
between robotic versus conventional laparoscopy. Int J Gynecol
Cancer. 30:466–472. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Magrina JF, Cetta RL, Chang YH, Guevara G
and Magtibay PM: Analysis of secondary cytoreduction for recurrent
ovarian cancer by robotics, laparoscopy and laparotomy. Gynecol
Oncol. 129:336–340. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chen CH, Chiu LH, Chang CW, Yen YK, Huang
YH and Liu WM: Comparing robotic surgery with conventional
laparoscopy and laparotomy for cervical cancer management. Int J
Gynecol Cancer. 24:1105–1111. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gallotta V, Cicero C, Conte C, Vizzielli
G, Petrillo M, Fagotti A, Chiantera V, Costantini B, Scambia G and
Ferrandina G: Robotic versus laparoscopic staging for early ovarian
cancer: A case-matched control study. J Minim Invasive Gynecol.
24:293–298. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Oyama K, Kanno K, Kojima R, Shirane A,
Yanai S, Ota Y and Andou M: Short-term outcomes of robotic-assisted
versus conventional laparoscopic radical hysterectomy for
early-stage cervical cancer: A single-center study. J Obstet
Gynaecol Res. 45:405–411. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cook DA and Reed DA: Appraising the
quality of medical education research methods: The medical
education research study quality instrument and the
Newcastle-Ottawa scale-education. Acad Med. 90:1067–1076. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Holzman SA, Grant C, Zee RS, Rana MS,
Sprague B, Blum E and Rushton HG: High incidence of abnormal
imaging findings in circumcised boys diagnosed with urinary tract
infections. J Pediatr Urol. 16:560–565. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nezhat FR, Datta MS, Liu C, Chuang L and
Zakashansky K: Robotic radical hysterectomy versus total
laparoscopic radical hysterectomy with pelvic lymphadenectomy for
treatment of early cervical cancer. JSLS. 12:227–237.
2008.PubMed/NCBI
|
|
20
|
Shi C, Gao Y, Yang Y, Zhang L, Yu J and
Zhang T: Comparison of efficacy of robotic surgery, laparoscopy,
and laparotomy in the treatment of ovarian cancer: A meta-analysis.
World J Surg Oncol. 17:1622019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Su MC, Zheng Y, Yang F and Liu YY:
Placement of robotic single-site surgery using the da Vinci Xi
platform and the tumor-free technique for early cervical cancer.
Asian J Surg. S1015-9584(22)01307-0. 2022.(Epub ahead of
print).
|
|
22
|
Yotsumoto F, Sanui A, Ito T, Miyahara D,
Yoshikawa K, Shigekawa K, Noguchi Y, Yasunaga S and Miyamoto S:
Cumulative summation analysis of learning curve for
robotic-assisted hysterectomy in patients with gynecologic tumors.
Anticancer Res. 42:4111–4117. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lanfranco AR, Castellanos AE, Desai JP and
Meyers WC: Robotic surgery: A current perspective. Ann Surg.
239:14–21. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ji Y and Wang H: Prognostic prediction of
systemic immune-inflammation index for patients with gynecological
and breast cancers: A meta-analysis. World J Surg Oncol.
18:1972020. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Reza M, Maeso S, Blasco JA and Andradas E:
Meta-analysis of observational studies on the safety and
effectiveness of robotic gynaecological surgery. Br J Surg.
97:1772–1783. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
26
|
Camarillo DB, Krummel TM and Salisbury JK
Jr: Robotic technology in surgery: Past, present, and future. Am J
Surg. 188((4A Suppl)): 2S–15S. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Magrina JF, Zanagnolo V, Noble BN, Kho RM
and Magtibay P: Robotic approach for ovarian cancer: Perioperative
and survival results and comparison with laparoscopy and
laparotomy. Gynecol Oncol. 121:100–105. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Sert MB and Abeler V: Robot-assisted
laparoscopic radical hysterectomy: Comparison with total
laparoscopic hysterectomy and abdominal radical hysterectomy; one
surgeon's experience at the Norwegian Radium Hospital. Gynecol
Oncol. 121:600–604. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chong GO, Lee YH, Hong DG, Cho YL, Park IS
and Lee YS: Robot versus laparoscopic nerve-sparing radical
hysterectomy for cervical cancer: A comparison of the
intraoperative and perioperative results of a single surgeon's
initial experience. Int J Gynecol Cancer. 23:1145–1149. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Coronado PJ, Fasero M, Magrina JF, Herraiz
MA and Vidart JA: Comparison of perioperative outcomes and cost
between robotic-assisted and conventional laparoscopy for
transperitoneal infrarenal para-aortic lymphadenectomy (TIPAL). J
Minim Invasive Gynecol. 21:674–681. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Díaz-Feijoo B, Gil-Ibáñez B,
Pérez-Benavente A, Martínez-Gómez X, Colás E, Sánchez-Iglesias JL,
Cabrera-Díaz S, Puig-Puig O, Magrina JF and Gil-Moreno A:
Comparison of robotic-assisted vs conventional laparoscopy for
extraperitoneal paraaortic lymphadenectomy. Gynecol Oncol.
132:98–101. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chen CH, Chiu LH, Chen HH, Chan C and Liu
WM: Comparison of robotic approach, laparoscopic approach and
laparotomy in treating epithelial ovarian cancer. Int J Med Robot.
12:268–275. 2016. View
Article : Google Scholar : PubMed/NCBI
|
|
33
|
Manchana T, Puangsricharoen P, Sirisabya
N, Worasethsin P, Vasuratna A, Termrungruanglert W and Tresukosol
D: Comparison of perioperative and oncologic outcomes with
laparotomy, and laparoscopic or robotic surgery for women with
endometrial cancer. Asian Pac J Cancer Prev. 16:5483–5488. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Mäenpää MM, Nieminen K, Tomás EI, Laurila
M, Luukkaala TH and Mäenpää JU: Robotic-assisted vs traditional
laparoscopic surgery for endometrial cancer: A randomized
controlled trial. Am J Obstet Gynecol. 215:588.e1–588.e7. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Mendivil AA, Rettenmaier MA, Abaid LN,
Brown JV III, Micha JP, Lopez KL and Goldstein BH: Survival rate
comparisons amongst cervical cancer patients treated with an open,
robotic-assisted or laparoscopic radical hysterectomy: A five year
experience. Surg Oncol. 25:66–71. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Pellegrino A, Damiani GR, Loverro M,
Pirovano C, Fachechi G, Corso S and Trojano G: Comparison of
robotic and laparoscopic radical type-B and C hysterectomy for
cervical cancer: Long term-outcomes. Acta Biomed. 88:289–296.
2017.PubMed/NCBI
|
|
37
|
Nie JC, Yan AQ and Liu XS:
Robotic-assisted radical hysterectomy results in better surgical
outcomes compared with the traditional laparoscopic radical
hysterectomy for the treatment of cervical cancer. Int J Gynecol
Cancer. 27:1990–1999. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Luo C, Liu M and Li X: Efficacy and safety
outcomes of robotic radical hysterectomy in Chinese older women
with cervical cancer compared with laparoscopic radical
hysterectomy. BMC Womens Health. 18:612018. View Article : Google Scholar : PubMed/NCBI
|