Introduction
Lung cancer is the leading cause of cancer-related
death worldwide, with most patients presenting with metastases
during diagnosis (1). According to
the GLOBOCAN 2020 report by the World Health Organization's
International Agency for Research on Cancer, ~2.2 million new cases
of lung cancer occur worldwide each year, making it the world's
second most common but most fatal cancer type (2,3).
Patients with early-stage lung cancer are asymptomatic, whereas
those with advanced metastasis are frequently symptomatic due to
metastatic sites. Once distant metastasis occurs, there is almost
no opportunity for surgery and the prognosis is poor. Of note,
distant metastases occur most commonly in the brain, liver, adrenal
glands and bones. Furthermore, the gastrointestinal (GI) tract is
not a common site of primary lung cancer metastasis (4). According to clinical studies, the
incidence of gastrointestinal metastasis ranges from 0.2 to 1.7%,
whereas the rate from autopsy reports ranges from 4.7 to 14%. This
suggests that the process of GI metastasis of lung cancer is subtle
and lacks specific clinical symptoms. GI metastasis is frequently
found due to severe complications, such as intestinal obstruction
and bleeding (5,6). The present report describes an
uncommon case of small intestinal metastasis from lung cancer.
Furthermore, the literature relevant to the occurrence, diagnosis
and treatment of GI metastasis of lung cancer was reviewed.
Case report
A 57-year-old male patient had a paroxysmal cough
and produced 5 ml of spit and sputum mixed with blood daily without
any obvious underlying cause. The patient had a medical history of
diabetes for 1 year and tobacco smoking for 3 years. In March 2020,
2 months after initial symptom development, the patient underwent a
computed tomography (CT) scan, which revealed a mass 6.5×6.2×7.2 cm
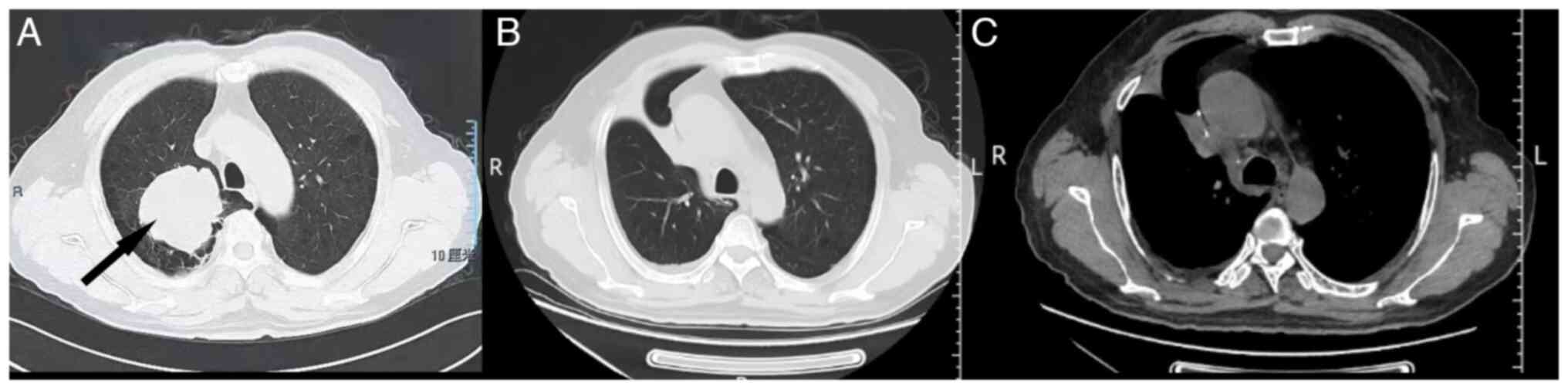
in size in the upper lobe of the right lung (Fig. 1A). The patient was subjected to
right upper lobe resection with lymph node dissection at the end of
March 2020 at a local hospital. Postoperative pathology indicated
infiltrating adenocarcinoma (right upper lobe mass) with poor
differentiation and lymph node metastasis. The protocol for
histopathology was performed according to standard procedures.
Immunohistochemistry (IHC) stains for pan-cytokeratin (cat. no.
ZM-0069), vimentin (cat. no. ZM-0260), cytokeratin 7 (CK7) (cat.
no. ZM-0071), thyroid transcription factor-1 (TTF-1) (cat. no.
ZM-0262) and Ki-67 labeling index (35%) (cat. no. ZM-0166) were
positive (Fig. S1). IHC staining
was performed according to standard procedures. Ready-to-use
antibodies, which were not diluted, were purchased from Beijing
Zhongshan Golden Bridge Biological Technology Co., Ltd. Whole-body
CT examination revealed no distant metastases anywhere, including
the brain. The patient was diagnosed with lung adenocarcinoma
(pT4N2M0 stage IIIB) (7). Four
cycles of chemotherapy with docetaxel and nedaplatin stabilized the
patient's condition. After the chemotherapy, the patient received
no additional radiotherapy or other related treatments for personal
reasons.
Approximately 6 months after completing
chemotherapy, the patient presented with abdominal pain and melena.
He was transferred to Affiliated Hospital of Weifang Medical
University (Weifang, China) in January 2021. The abdominal CT
revealed multiple small intestinal tumors in the left lower
abdomen, whereas chest CT indicated no primary tumor in both lungs
or hilum (Fig. 1B). No obvious
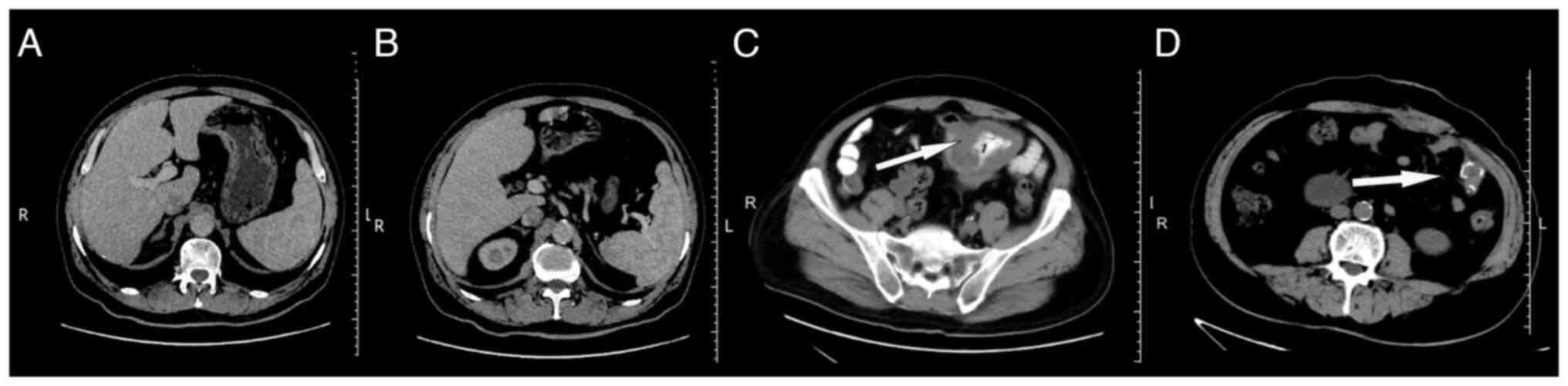
enlarged lymph nodes were found in the mediastinum (Fig. 1C). Simultaneously, the abdominal CT
displayed intrahepatic calcification without metastasis (Fig. 2A and B). Imaging examination
revealed a high possibility of small intestinal lymphoma (Fig. 2C). Upon hospital admission, the
patient underwent small bowel tumor resection and intestinal
adhesiolysis with tissue sampling to ascertain the nature of the
tumor. The patient tolerated the procedure well and the
postoperative course was uneventful. The postoperative CT indicated
that the surgical staples were present after resecting the small
bowel mass and the patient recovered well (Fig. 2D). Furthermore, the postoperative
pathology of the enteral mass indicated metastatic lesions from
poorly differentiated lung adenocarcinoma. Molecular analysis
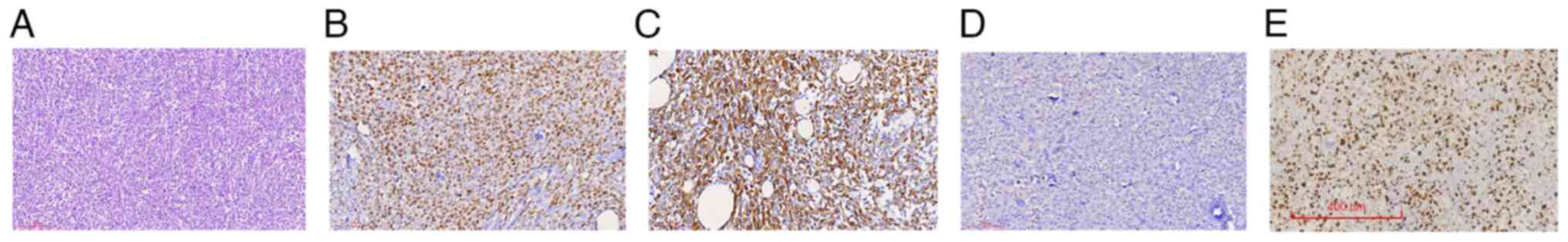
revealed no mutations in the proto-oncogene. Hematoxylin and eosin
staining showed that the tumor permeated the whole small intestinal
wall and regional lymph node carcinoma was positively identified
(Fig. 3A). IHC staining was
positive for CK7 (cat. no. Kit-0021) and TTF-1 (cat. no. MAB-0599),
with negative CK20 (cat. no. Kit-0025) (Fig. 3B-D). These antibodies were purchased
from Fuzhou Maixin Biotech, Co., Ltd. Furthermore, IHC stains for
CK7, TTF-1, epithelial membrane antigen and Ki-67 labeling index
(60%) were positive (Fig. 3E). None
of these antibodies were diluted. Immunohistochemistry (IHC)
staining was performed according to standard procedures. This IHC
staining profile supported metastatic adenocarcinoma from the
lungs, rather than primary intestinal adenocarcinoma. The
expression rate of programmed cell death-ligand 1 (PD-L1) (cat. no.
22C3) was 40%. This antibody was purchased from Dako North America,
Inc. And PD-L1 staining was performed according to standard
procedures. The patient was diagnosed with small intestinal
metastasis from lung cancer. The patient demonstrated slow recovery
of intestinal function postoperatively, and due to being in a poor
personal economic situation, the patient refused systemic
treatment; therefore, no systemic therapy was administered.
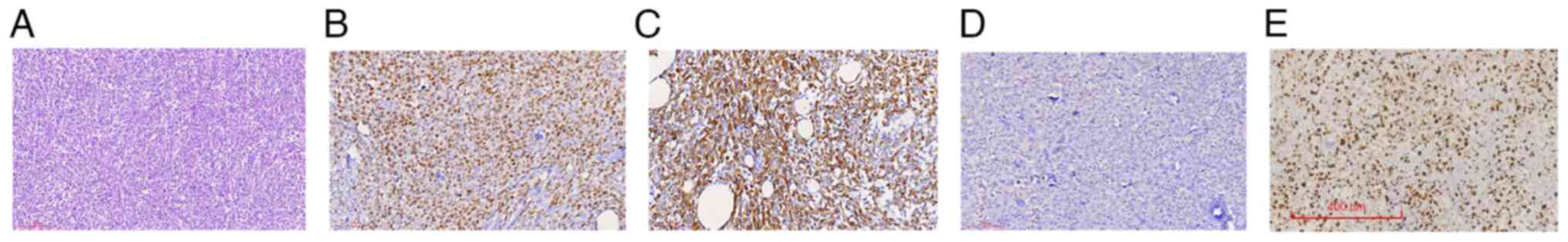 | Figure 3.Histological analyses of small bowel
tumors after resection (January 2021). (A) The tumor cells are
polygonal, with a cytoplasm, eosinophilic, nuclear polygonal and
without any obvious adenoid structure (hematoxylin and eosin
staining; magnification, ×100; scale bar, 200 µm). (B) Tumor cells
had positive staining for CK7 (IHC staining; magnification, ×200,
scale bar, 100 µm). (C) Tumor cells exhibited positive staining for
thyroid transcription factor-1 (IHC staining; magnification, ×200;
scale bar, 100 µm). (D) Tumor cells had negative staining for CK20
(IHC staining; magnification, ×200; scale bar, 100 µm). (E) The
tumor cells had a Ki-67 labeling index of 60% (IHC staining; scale
bar, 400 µm). CK, cytokeratin; IHC, immunohistochemical. |
After another two months, the patient was admitted
to the emergency department of our institution with persistent
abdominal pain. The patient reported the absence of gas and feces
with abdominal pain during the previous few days. Furthermore, a
physical examination revealed a distended abdomen with epigastric
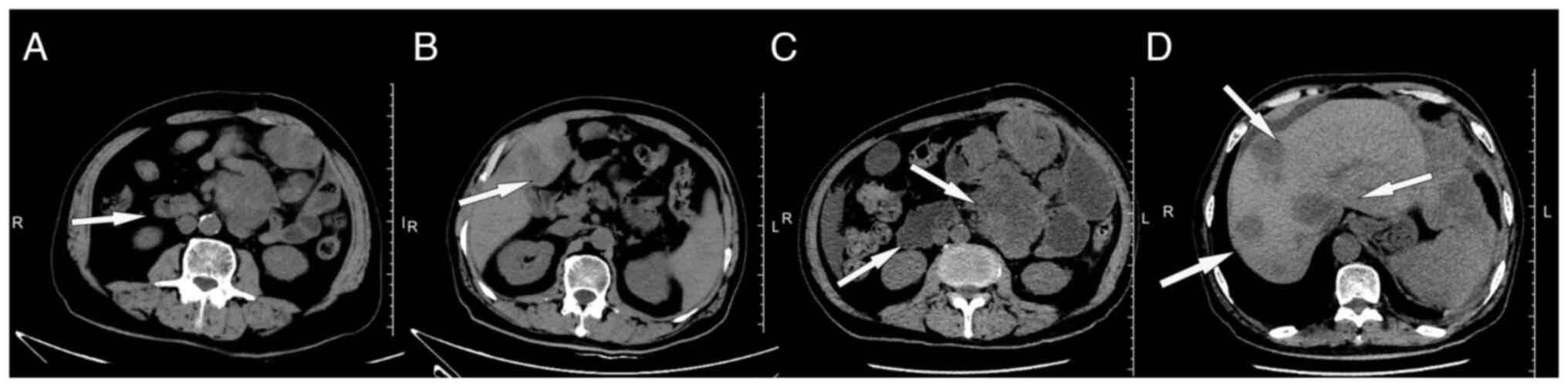
tenderness. An abdominal CT indicated multiple metastatic masses on
the small intestinal wall and multiple metastatic low-density
lesions in the liver (Fig. 4A and
B). The multiple intestinal metastases caused small bowel
obstruction. Tarry stools were observed after an enema, and GI
bleeding was suspected. Furthermore, laboratory evaluations
revealed a hemoglobin concentration of 71 g/l (reference range,
115–150 g/l) and a hematocrit (HCT) value of 23.8% (reference
range, 35–45%), both below the normal range. Based on these
observations, the patient was diagnosed with multiple small bowel
metastases from lung cancer accompanied by complete intestinal
obstruction and GI bleeding. The patient was too compromised for
surgery at this time to control disease progression, as the
performance status (PS) was >2. The PS score was developed by
the Eastern Cooperative Oncology Group (ECOG), also known as the
ECOG-PS score, which refers to the general health status and
treatment tolerance of patients from their physical strength
(8). Instead, the patient was
placed on systemic therapy with pemetrexed, carboplatin and
camrelizumab [a programmed cell death 1 (PD-1) inhibitor].
Subsequently, the patient developed severe anemia (HCT 19.6%) from
GI bleeding and received blood transfusion and fluid rehydration
therapy. Severe abdominal pain and reduced HCT during systemic
treatment significantly reduced the patient's physical condition.
The final abdominal CT revealed multiple metastases in the liver,
small intestine and abdominal cavity, which had increased in number
and size (Fig. 4C and D). The
patient was no longer able to tolerate anti-tumor therapy;
therefore, only symptomatic treatment was continued. The patient
experienced excessive GI bleeding and died the next day.
Discussion
Lung cancer is one of the most common malignant
tumors in humans (1). The following
are the two main histological types of lung cancer: small cell lung
cancer and non-small cell lung cancer (NSCLC). NSCLC is the most
common histological type of lung cancer, which includes squamous
cell carcinoma, adenocarcinoma, large cell carcinoma, adenosquamous
carcinoma and sarcomatoid carcinoma (9,10). As
demonstrated in autopsy studies, lung cancer metastases may
infiltrate every systemic tissue (11). Squamous cell carcinoma (28.5%),
adenocarcinoma (27.6%) and large cell carcinoma (20.9%) are the
three most common histological types of NSCLC to develop distant
metastasis (5). Small intestinal
metastasis from NSCLC is unusual (11–14).
Recently, the incidence of GI metastasis from lung cancer has been
reported to be <2% (14). The
small intestine has a low incidence of metastasis, which may be
attributed to abundant lymphoid tissue in the intestinal wall,
which includes numerous T lymphocytes, and provides the wall with a
high level of protection. Of note, the jejunum and ileum are the
most common metastatic sites of the digestive tract, followed by
the duodenum (15,16). As indicated in the abdominal CT of
the patient, the intestinal wall of the ileum in the left lower
abdomen was thickened and multiple lymph node shadows were
observed. The reason for the difference in small intestinal
metastasis site may be the abundant lymphoid tissue and blood
supply around the empty ileum.
An analysis of 366 cases revealed that of those
patients with lung cancer diagnosed with small bowel metastasis,
>50% die within 3 months (5) and
<10% of lung cancer patients with small bowel metastasis have
been reported to survive for >1 year. In the present case, the
patient died within <3 months of the diagnosis due to small
intestinal metastasis. The reasons for the short survival may be as
follows: First, previous studies have indicated that lung cancer
metastasis in the small intestine is frequently accompanied by
metastasis from other sites, such as the kidney and liver. In this
scenario, multiple metastases in the liver and abdominal cavity
also occurred in the late stage of small intestinal metastasis,
which implies that the prognosis of patients with tumors is poor,
and the median survival time was <3 months (17). Furthermore, because small intestinal
metastasis from lung cancer is uncommon and has no obvious clinical
symptoms in its early stage, it may lead to life-threatening
abdominal symptoms, such as hemorrhage (24.6%), obstruction (20.4%)
and perforation (20%) (5,18). In the present case, intestinal
obstruction and bleeding symptoms occurred during the late stage of
small intestinal metastasis of the patient. Due to the patient's
poor physical condition, instead of surgery to relieve the
obstruction, conservative treatment such as enema was performed,
which may have exacerbated the possibility of intestinal bleeding
and further aggravated the condition. Third, due to the patient's
limited economic situation, no effective radiotherapy was provided
in the early stage and no systemic treatment was administered to
the small intestine tumor postoperatively. Therefore, as this
treatment opportunity was missed, the tumor was not effectively
controlled, resulting in a poor prognosis for the patient. Finally,
although this patient was eligible for the first-line treatment of
advanced or metastatic lung cancer and PD-L1 expression was 40%,
the patient had a poor constitution and an ECOG PS >2. For
treating small intestinal metastasis of lung cancer, particularly
for patients who have undergone small intestinal surgery,
first-line treatment for lung cancer is still the main treatment,
including chemotherapy, radiotherapy, immunotherapy, targeted
therapy and various combination therapies (19). By contrast, National Comprehensive
Cancer Network guidelines recommend that systemic treatment may be
applied to advanced or metastatic first-line treatment when the PS
is 0–2. This disease progresses rapidly, and to control the
disease, the combination of immunotherapy with chemotherapy may be
the reason for the poor prognosis, which the patient may not
tolerate.
Based on the patient's symptoms, imaging
examinations help detect extrapulmonary lesions. Kim et al
(20) evaluated the CT scanning
results of 28 patients with GI metastasis from lung cancer and
found that 5/26 and 21/26 had two and one lesion, respectively. The
shapes of the GI lesions varied on CT scans, including wall
thickening in 14 cases, an intraluminal polypoid mass in 14 and an
exophytic mass in the other 3 (20). Lardinois et al (21) reported that solitary extrapulmonary
lesions were observed in 21% of patients with NSCLC using positron
emission tomography (PET)-CT imaging. Compared with conventional CT
and other imaging methods, PET-CT may detect solitary
extrapulmonary malignant lesions, such as GI tumors (18,20–22).
However, PET-CT is not yet routinely performed, as it is expensive.
For instance, in the case of the present study, PET-CT was not
performed due to the economic limitations of this patient.
Furthermore, imaging studies cannot determine the intestinal
tumor's source or histopathological type. Pathological diagnosis
using IHC, in contrast to imaging methods, remains the gold
standard for differentiating primary and metastatic lesions of
small intestinal malignancies. IHC staining for TTF-1, caudal type
homeobox transcription factor 2, CK7 and CK20 helps distinguish a
primary small bowel tumor from lung cancer metastasis (23,24).
Primary lung carcinomas usually exhibit a
CK7+/CK20− immunophenotype, as opposed to the
common CK7−/CK20+ pattern of intestinal
adenocarcinomas (23). However,
primary small bowel adenocarcinomas may also be
CK7+/CK20− (6). Therefore, TTF-1 and Napsin A
positivity is critical in establishing a primary lung cancer
origin. TTF-1 is highly specific for lung adenocarcinomas,
exhibiting a positive predictive value of >90% (23,25).
Based on the histological characteristics, an
effective treatment plan for patients may be formulated. Liu et
al (26) reported that
postoperative adjuvant chemotherapy, radiotherapy, immunotherapy,
targeted therapy or various combination therapies improved the
survival rate of patients with intestinal metastasis of lung cancer
presenting with GI obstruction, perforation or other acute
abdominal issues. In addition, Nitipir et al (27) reported a case of GI metastasis in a
patient with lung carcinoma with poor physical fitness who received
chemotherapy, and the disease was controlled for 22 weeks. AlSaeed
et al (28) reported a case
of GI metastasis in patients with lung carcinoma who received
radiotherapy, and the symptoms were relieved. Furthermore,
Letaief-Ksontini et al (29)
reported that the prognosis was prolonged in the case of GI
metastasis of patients with lung carcinoma who underwent surgery
and postoperative adjuvant chemotherapy. In addition, clinical
studies indicated that PD-1/PD-L1 inhibitors successfully
progressed in treating advanced NSCLC (30–32).
The PD-1 inhibitor camrelizumab (SHR-1210) (33) is a novel and popular anti-tumor
immunotherapy. Camrelizumab combination chemotherapy with
pemetrexed and carboplatin is the first-line treatment for advanced
non-squamous NSCLC without genetic mutations (34). Improvement of overall survival was
reported in patients with NSCLC regardless of PD-L1 expression;
however, patients with high levels of PD-L1 benefited the most
(35). Although the outcome of the
patient of the present study was poor, it does not discredit the
efficacy and safety of immunotherapy combined with chemotherapy
(35). Based on the latest National
Comprehensive Cancer Network guidelines, the combination of
pembrolizumab, pemetrexed and carboplatin may be given as a
first-line treatment for patients with advanced or metastatic
disease (36). This supports the
viability of combined immunotherapy and chemotherapy. Clinical
studies have demonstrated that camrelizumab combined with
pemetrexed and carboplatin has long-term survival benefits and
controllable toxicity (34,37). Depending on the type of lung
carcinoma, metastases in multiple sites, heavy tumor load and
postoperative complications may result in poor prognosis. GI
cancers with perforation, obstruction or hemorrhage have been
associated with less favorable outcomes. Effective treatment may
increase the duration of patient survival; however, the prognosis
significantly depends on the predominant symptoms at the initial
presentation and the subsequent massive bleeding 2 months after the
diagnosis of small intestinal metastasis. The patient of the
present study was intolerant to treatment and ultimately died the
day after the obstruction was discovered. If this patient had been
able to receive timely and effective treatment, his survival may
have been prolonged. Furthermore, early detection and therapeutic
intervention may have improved survival (24).
In conclusion, the occurrence of small intestinal
metastasis from lung cancer is rare and may be life-threatening.
Therefore, GI metastases should be considered when patients with a
history of primary lung cancer have abdominal symptoms. When a
patient is diagnosed with lung cancer, abdominal CT or MRI should
be performed regularly, regardless of whether the cancer is in its
early or late stage. If conditions permit, a PET-CT examination may
be performed. Furthermore, when abnormalities occur, a pathological
diagnosis should be performed immediately to determine the nature
and source of the tumor, and patients with lung cancer with small
intestinal metastasis should be thoroughly evaluated. Those who
meet the indications of surgery should undergo surgery immediately,
while for those who cannot tolerate surgery, their physical
condition should be strictly assessed and individualized treatment
should be administered in strict accordance with oncology
guidelines to effectively prevent complications, improve quality of
life and prolong overall survival.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TZL, YG, ZCW, JL, XTP and YH contributed to the
study conception and design. Material preparation, and data
collection and analysis were performed by ZCW, JL, XTP and YH. The
original draft of the manuscript was written by TZL and YG. And all
authors commented on previous versions of the manuscript. TZL, YG
and YH confirm the authenticity of all the raw data. All authors
have read and agreed to the published version of the
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent has been obtained from
family members of the patient to publish this case report with the
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
CK7
|
cytokeratin 7
|
|
CT
|
computed tomography
|
|
GI
|
gastrointestinal
|
|
HCT
|
hematocrit
|
|
IHC
|
immunohistochemistry
|
|
NSCLC
|
non-small cell lung cancer
|
|
PET
|
positron emission tomography
|
|
PD-L1
|
programmed cell death-ligand 1
|
|
PD-1
|
programmed cell death 1
|
|
TTF-1
|
thyroid transcription factor-1
|
References
|
1
|
Balata H, Fong KM, Hendriks LE, Lam S,
Ostroff JS, Peled N, Wu N and Aggarwal C: Prevention and early
detection for NSCLC: Advances in thoracic oncology 2018. J Thorac
Oncol. 14:1513–1527. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Xia C, Dong X, Li H, Cao M, Sun D, He S,
Yang F, Yan X, Zhang S, Li N and Chen W: Cancer statistics in China
and United States, 2022: profiles, trends, and determinants. Chin
Med J (Engl). 135:584–590. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Siegel RL, Miller KD, Fuchs HE and Jemal
A: Cancer statistics, 2022. CA Cancer J Clin. 72:7–33. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Niu FY, Zhou Q, Yang JJ, Zhong WZ, Chen
ZH, Deng W, He YY, Chen HJ, Zeng Z, Ke EE, et al: Distribution and
prognosis of uncommon metastases from non-small cell lung cancer.
BMC Cancer. 16:1492016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hu Y, Feit N, Huang Y, Xu W, Zheng S and
Li X: Gastrointestinal metastasis of primary lung cancer: An
analysis of 366 cases. Oncol Lett. 15:9766–9776. 2018.PubMed/NCBI
|
|
6
|
Yoshimoto A, Kasahara K and Kawashima A:
Gastrointestinal metastases from primary lung cancer. Eur J Cancer.
42:3157–3160. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Goldstraw P, Chansky K, Crowley J,
Rami-Porta R, Asamura H, Eberhardt WE, Nicholson AG, Groome P,
Mitchell A, Bolejack V, et al: The IASLC lung cancer staging
project: Proposals for revision of the TNM stage groupings in the
forthcoming (Eighth) edition of the TNM classification for lung
cancer. J Thorac Oncol. 11:39–51. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Neeman E, Gresham G, Ovasapians N,
Hendifar A, Tuli R, Figlin R and Shinde A: Comparing physician and
nurse eastern cooperative oncology group performance status
(ECOG-PS) ratings as predictors of clinical outcomes in patients
with cancer. Oncologist. 24:e1460–e1466. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Herbst RS, Morgensztern D and Boshoff C:
The biology and management of non-small cell lung cancer. Nature.
553:446–454. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Barta JA, Powell CA and Wisnivesky JP:
Global epidemiology of lung cancer. Ann Glob Health. 85:82019.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hoffman PC, Mauer AM and Vokes EE: Lung
cancer. Lancet. 355:479–485. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
McNeill PM, Wagman LD and Neifeld JP:
Small bowel metastases from primary carcinoma of the lung. Cancer.
59:1486–1489. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hung TI, Chu KE, Chou YH and Yang KC:
Gastric metastasis of lung cancer mimicking an adrenal tumor. Case
Rep Gastroenterol. 8:77–81. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jevremovic V: Is gastrointestinal
metastasis of primary lung malignancy as rare as reported in the
literature? A comparison between clinical cases and post-mortem
studies. Stud Oncol Hematol Rev. 12:51–57. 2016.
|
|
15
|
Yamada H, Akahane T, Horiuchi A, Shimada
R, Shibuya H, Hayama T, Nozawa K, Ishihara S, Matsuda K and
Watanabe T: A case of lung squamous cell carcinoma with metastases
to the duodenum and small intestine. Int Surg. 96:176–181. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Janež J: Acute intestinal obstruction due
to metastatic lung cancer-case report. J Surg Case Rep.
2017:rjx0312017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Di JZ, Peng JY and Wang ZG: Prevalence,
clinicopathological characteristics, treatment, and rognosis of
intestinal metastasis of primary lung cancer: A comprehensive
review. Surg Oncol. 23:72–80. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yang CJ, Hwang JJ, Kang WY, Chong IW, Wang
TH, Sheu CC, Tsai JR and Huang MS: Gastro-intestinal metastasis of
primary lung carcinoma: Clinical presentations and outcome. Lung
Cancer. 54:319–323. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Xue C, Hu Z, Jiang W, Zhao Y, Xu F, Huang
Y, Zhao H, Wu J, Zhang Y, Zhao L, et al: National survey of the
medical treatment status for non-small cell lung cancer (NSCLC) in
China. Lung Cancer. 77:371–375. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kim SY, Ha HK, Park SW, Kang J, Kim KW,
Lee SS, Park SH and Kim AY: Gastrointestinal metastasis from
primary lung cancer: CT findings and clinicopathologic features.
AJR Am J Roentgenol. 193:W197–W201. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lardinois D, Weder W, Roudas M, von
Schulthess GK, Tutic M, Moch H, Stahel RA and Steinert HC: Etiology
of solitary extrapulmonary positron emission tomography and
computed tomography findings in patients with lung cancer. J Clin
Oncol. 23:6846–6853. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Stinchcombe TE, Socinski MA, Gangarosa LM
and Khandani AH: Lung cancer presenting with a solitary colon
metastasis detected on positron emission tomography scan. J Clin
Oncol. 24:4939–4940. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Rossi G, Marchioni A, Romagnani E,
Bertolini F, Longo L, Cavazza A and Barbieri F: Primary lung cancer
presenting with gastrointestinal tract involvement:
Clinicopathologic and immunohistochemical features in a series of
18 consecutive cases. J Thorac Oncol. 2:115–120. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Sakai H, Egi H, Hinoi T, Tokunaga M,
Kawaguchi Y, Shinomura M, Adachi T, Arihiro K and Ohda H: Primary
lung cancer presenting with metastasis to the colon: A case report.
World J Surg Oncol. 10:1–5. 2012. View Article : Google Scholar
|
|
25
|
Goh BK, Yeo AW, Koong HN, Ooi LL and Wong
WK: Laparotomy for acute complications of gastrointestinal
metastases from lung cancer: Is it a worthwhile or futile effort?
Surg Today. 37:370–374. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Liu W, Zhou W, Qi WL, Ma YD and Xu YY:
Gastrointestinal hemorrhage due to ileal metastasis from primary
lung cancer. World J Gastroenterol. 21:3435–3440. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Nitipir C, Ginghina O, Popa L, Andrei F,
Tudor N, Radu I, Iaciu C, Orlov C, Vasilescu F, Balalau C, et al: A
rare case of advanced lung cancer presenting as a symptomatic
gastric tumor. Mol Clin Oncol. 8:595–599. 2018.PubMed/NCBI
|
|
28
|
AlSaeed EF, Tunio MA, AlSayari K, AlDandan
S and Riaz K: Duodenal metastasis from lung adenocarcinoma: A rare
cause of melena. Int J Surg Case Rep. 13:91–94. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Letaief-Ksontini F, Boujnah R, Yahiaoui Y,
Zaimi Y, Ksentini M, Aloui R, Meddeb K and Mezlini A: An acute
jejunojejunal intussusception revealing a metastatic combined lung
cancer. Case Rep Surg. 2021:99996052021.PubMed/NCBI
|
|
30
|
Rittmeyer A, Barlesi F, Waterkamp D, Park
K, Ciardiello F, von Pawel J, Gadgeel SM, Hida T, Kowalski DM, Dols
MC, et al: Atezolizumab versus docetaxel in patients with
previously treated non-small-cell lung cancer (OAK): A phase 3,
open-label, multicentre randomised controlled trial. Lancet.
389:255–265. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Vokes EE, Ready N, Felip E, Horn L, Burgio
MA, Antonia SJ, Aren Frontera O, Gettinger S, Holgado E, Spigel D,
et al: Nivolumab versus docetaxel in previously treated advanced
non-small-cell lung cancer (CheckMate 017 and CheckMate 057):
3-year update and outcomes in patients with liver metastases. Ann
Oncol. 29:959–965. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Socinski MA, Jotte RM, Cappuzzo F, Orlandi
F, Stroyakovskiy D, Nogami N, Rodriguez-Abreu D, Moro-Sibilot D,
Thomas CA, Barlesi F, et al: Atezolizumab for First-Line Treatment
of Metastatic Nonsquamous NSCLC. N Engl J Med. 378:2288–2301. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Mo H, Huang J, Xu J, Chen X, Wu D, Qu D,
Wang X, Lan B, Wang X, Xu J, et al: Safety, anti-tumour activity,
and pharmacokinetics of fixed-dose SHR-1210, an anti-PD-1 antibody
in advanced solid tumours: A dose-escalation, phase 1 study. Br J
Cancer. 119:538–545. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Zhou C, Chen G, Huang Y, Zhou J, Lin L,
Feng J, Wang Z, Shu Y, Shi J, Hu Y, et al: Camrelizumab plus
carboplatin and pemetrexed versus chemotherapy alone in
chemotherapy-naive patients with advanced non-squamous
non-small-cell lung cancer (CameL): A randomised, open-label,
multicentre, phase 3 trial. Lancet Respir Med. 9:305–314. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Hou X, Zhou C, Wu G, Lin W, Xie Z, Zhang
H, Yi J, Peng Z, Yin L, Ma C and Chen L: Efficacy, safety, and
health-related quality of life with camrelizumab plus pemetrexed
and carboplatin as first-line treatment for advanced nonsquamous
NSCLC with brain metastases (CAP-BRAIN): A multicenter, open-label,
single-arm, phase 2 study. J Thorac Oncol.
2:S1556–S0864(23)00092-8. 2023.
|
|
36
|
Ettinger DS, Wood DE, Aisner DL, Akerley
W, Bauman JR, Bharat A, Bruno DS, Chang JY, Chirieac LR, D'Amico
TA, et al: Non-small cell lung cancer, version 3.2022, NCCN
clinical practice guidelines in oncology. J Natl Compr Canc Netw.
20:497–530. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Zhou C, Chen G, Huang Y, Zhou J, Lin L,
Feng J, Wang Z, Shu Y, Shi J, Hu Y, et al: Camrelizumab plus
carboplatin and pemetrexed as first-line treatment for advanced
nonsquamous NSCLC: Extended follow-up of camel phase 3 trial. J
Thorac Oncol. 13:S1556S0864(22)01993-1. 2023.
|