Early detection and systematic treatment can improve
the survival rate of patients with cancer. Nutritional supplements
and physical improvements, including timely supplementation of
protein and vitamins, and low intensity aerobic exercise, also play
a critical role in enhancing the clinical efficacy of the
treatments for HCC. Recently, physical parameters, such as muscle
strength and fat content, have been used as evaluation factors to
predict patient prognosis (6).
Sarcopenia is usually interpreted as a progressive
attenuation of muscle volume and a gradual decline in muscle
performance, which can cause adverse clinical events (7). Sarcopenia is caused by ageing as well
as diverse chronic illnesses, such as diabetes, heart failure and
cancer. It has been confirmed that sarcopenia is prevalent in
various tumors, including gastric cancer, lung cancer and
colorectal cancer, and has an adverse impact on patient prognosis
(8). To the best of our knowledge,
certain reviews have shown that sarcopenia is closely related to
lower survival rates and higher rates of postoperative syndrome in
patients with HCC (9,10). Therefore, unravelling the accurate
incidence rate of sarcopenia in HCC is important for early
screening, formulating adequate intervention measures and improving
patient prognosis.
To date, no meta-analysis has assessed the incidence
of sarcopenia among patients with HCC, to the best of our
knowledge. The evidence obtained from the present meta-analysis
will provide accurate and effective epidemiological information to
help prevent and treat sarcopenia. Therefore, the purpose of the
present study was to systematically dissect the published
literature on the morbidity of sarcopenia among patients with
HCC.
An extensive and systematic literature review was
conducted according to the PRISMA guidelines (11). Relevant literature published from
March 2001 to June 2022 in the English language was systematically
searched in PubMed (https://www.nih.gov/), Embase (https://www.embase.com/), Web of Science (https://www.webofscience.com) and the Cochrane Library
(http://www.cochranelibrary.com). The
detailed retrieval strategy is presented in Appendix S1. Two
authors independently retrieved the titles and abstracts to select
potentially suitable articles. Subsequently, the content of these
articles was assessed to determine which studies to include and
exclude. Reasons for inclusion and exclusion were recorded. All
discrepancies were resolved by discussion. All potential studies
were entered into EndNote X9 (Clarivate Plc) and duplicate studies
were removed. The Prospero registration no. of the present
systematic review is CRD42022328912 (https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022328912).
The inclusion criteria were as follows: i) Subject
population: Patients with HCC; ii) disease of concern: Sarcopenia
(at present, there is no unanimous standard for sarcopenia;
therefore, the original definition in each study was retained);
iii) the incidence or number of sarcopenia cases was reported; and
iv) research type: Prospective or retrospective cohort study. The
exclusion criteria were as follows: i) Lack of accurate diagnostic
standards for sarcopenia; ii) books, case reports, editorials,
letters to the editor and reviews; and iii) non-English
writing.
Two investigators separately extracted comprehensive
data from the eligible studies. The data filtered from every study
contained the following information: i) First author name; ii)
study type; iii) publication date; iv) sample size; v) number of
individuals with sarcopenia; vi) country where the study was
performed; vii) proportion of male patients; ix) average age and x)
diagnostic criteria for sarcopenia. Quality assessment was
performed separately by two investigators utilizing the
Newcastle-Ottawa Scale (NOS) (12).
Any disagreements were resolved by a third senior author.
In the present study, all statistical analyses were
performed using STATA software version 12.0 (StataCorp LP). The
incidence rates from the included studies were pooled using a
randomized effect meta-analysis (13). Heterogeneity was evaluated using the
I2 test. Values of 75, 50 and 25% from the I2
test indicated high, medium and low heterogeneity, respectively
(14). To clarify the possible
sources of heterogeneity, subgroup and meta-regression analyses
were performed on region, average age, proportion of male patients,
diagnostic criteria, sample size and year of publication.
Publication bias was tested using the Egger's test. The asymmetry
of the funnel plot was corrected using the trim-and-fill method
(15). P<0.05 was considered to
indicate a statistically significant difference.
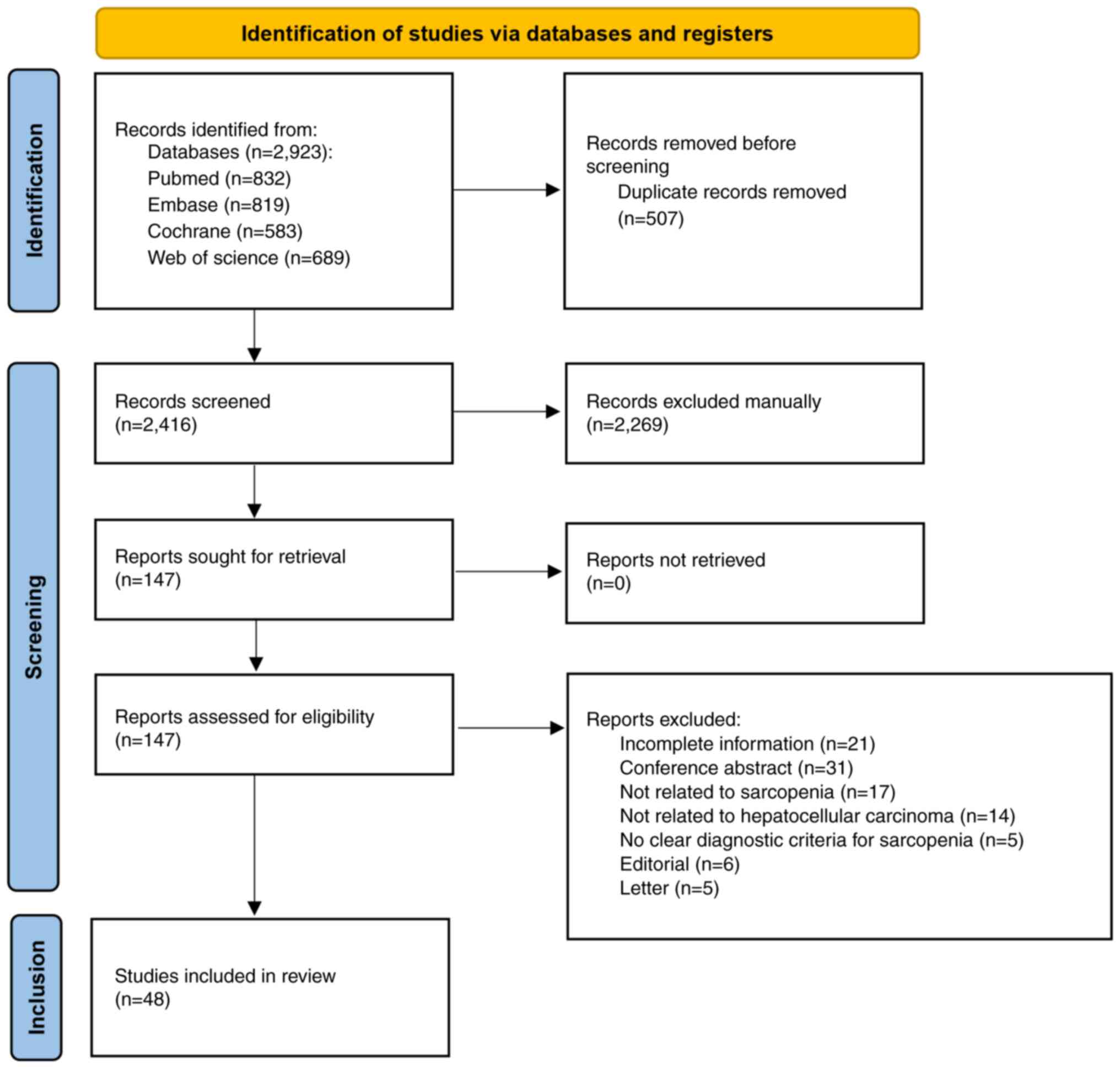
In total, 2,923 relevant studies were retrieved,
including 832 from PubMed, 819 from Embase, 583 from Cochrane and
689 from Web of Science. After removing duplicates and reading the
titles and abstracts, a total of 2,776 studies were excluded. After
screening the full texts, 48 studies that met the inclusion
criteria were included. A flowchart of the document retrieval
process is presented in Fig. 1.
The important features of the studies included in
the present meta-analysis are presented in Table I. A total of 8,959 participants were
enrolled in the eligible studies (16–63). A
large number of the studies included in the current review were
performed in Asia, especially in Japan, and 15 documented studies
were performed outside Asia, such as Africa (n=4), North America
(n=4) and Europe (n=7). The studies included in the present
meta-analysis were published between 2013 and 2022. The sample size
of patient cohorts in the analyzed studies ranged from 40 to 1,257
patients. Of these, two were observational studies, three were
prospective studies and the rest were retrospective studies.
In 43 articles, to define sarcopenia, the skeletal
muscle near the third lumbar vertebra was detected by computed
tomography (CT), while three of the 43 studies also used grip
strength measured using a hand grip dynamometer. In four studies,
CT was used to detect the psoas muscle near the third lumbar spine.
In addition, one study used magnetic resonance imaging to detect
the fat-free muscle area (FFMA) near the superior mesenteric
artery.
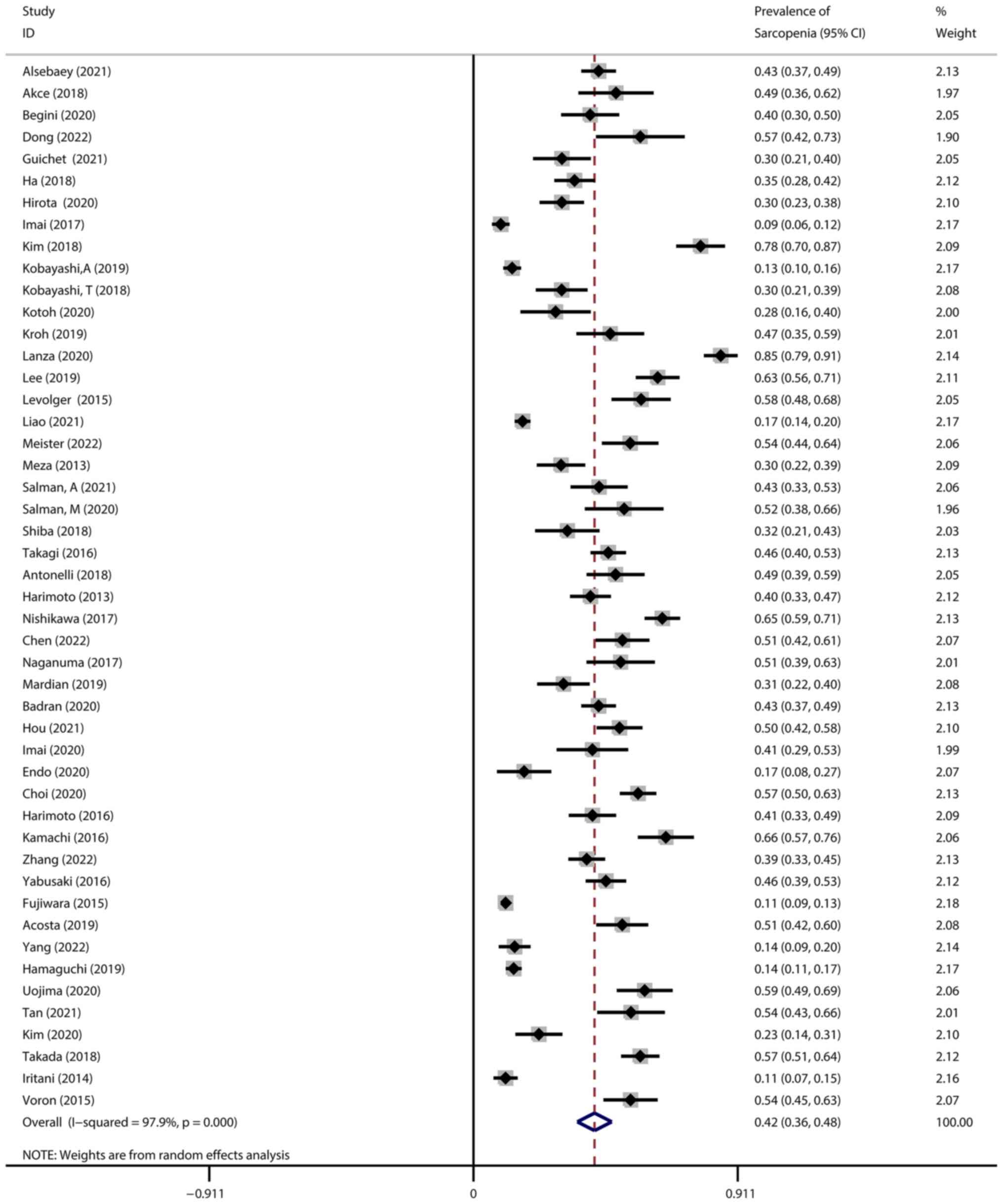
The pooled incidence rate of sarcopenia among
patients with HCC was 42% (95% CI, 0.36-0.48). Remarkable
heterogeneity was observed among the 48 studies
(I2=97.9%, P<0.001) (Fig.
2).
The prevalence of sarcopenia was 44% in Africa, 40%
in North America, 56% in Europe and 39% in Asia, although the
I2 statistic showed significant heterogeneity among the
studies included in each subgroup, except for Africa (Table II; Fig. S1A).
Considering the proportion of male patients included
in the present study, 75% was used as the analysis cut-off. The
prevalence of sarcopenia in the subgroup with a high proportion of
male patients was higher compared with the prevalence in the
subgroup with a low proportion of males (45 vs. 37%, respectively;
Table II; Fig. S1B).
In the subgroup analysis, the incidence rate of
sarcopenia based on average age was found to be higher in young
patients (<60 years old; 46%) compared with the incidence in
elderly patients (≥60 years old; 39%; Table II; Fig. S1C).
Furthermore, in the subgroup analysis with different
diagnostic criteria, the male skeletal muscle index (SMI) of 42
cm2/m2 and female SMI of 38
cm2/m2 was used as the cut-off. The morbidity
of sarcopenia was higher in the studies with SMI > cut-off
(50%), followed by SMI selectively > cut-off (44%), equal to the
cut-off (41%) and < cut-off (23%) (Fig. S1D). In addition, the studies using
SMI combined with body mass index as the diagnostic standard had a
higher incidence rate of sarcopenia (43%) compared with the studies
using SMI combined with hand grip strength (24%). Interestingly,
when using other diagnostic methods, such as the psoas muscle index
(PMI) or FFMA, the incidence rate of sarcopenia was the highest
(54%) among all diagnostic criteria used. All aforementioned
subgroup analyses are depicted in Fig.
S1.
The year of publication of the data collected for
the current review did not affect the incidence rate of sarcopenia
in the meta-regression analysis (regression coefficient, 0.004; 95%
CI, 0.171-0.262; P=0.68; Table
III). However, the total sample size could explain ~40% of the
heterogeneity among these studies in the meta-regression analysis
(regression coefficient, −0.0003; 95% CI, 0.0006 to −0.0001;
P<0.001; Table III).
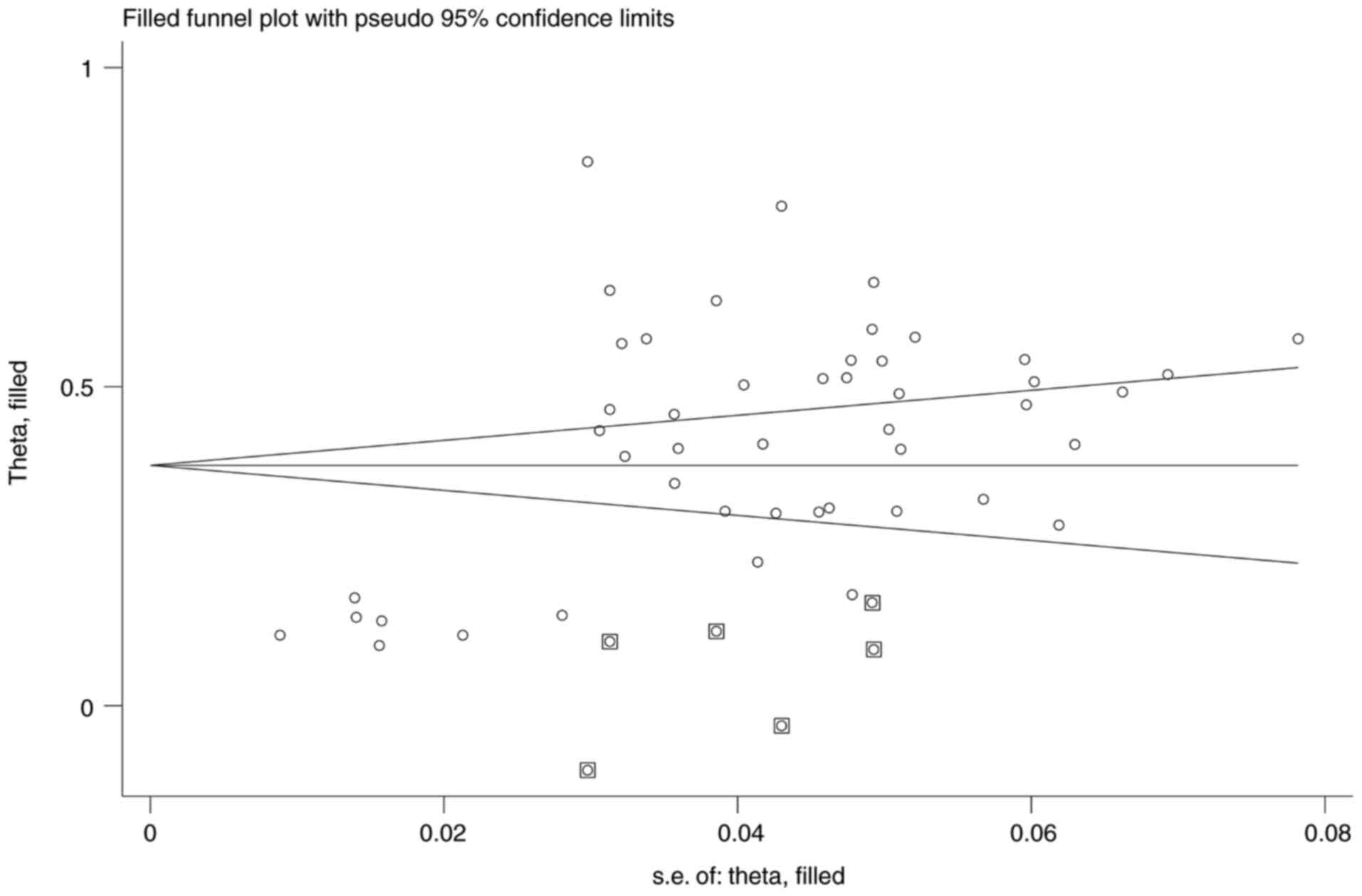
In the current meta-analysis, potential publication
bias was found according to the asymmetry of the funnel plot
(Fig. S2) and Egger's test
(P<0.001; 95% CI, 6.93-12.09). Subsequently, the trim-and-fill
method was used to correct the asymmetry of the funnel plots. The
processed data showed that the results were not reversed after the
addition of six studies (P<0.0001; 95% CI, 0.32-0.43), which
further indicated that despite publication bias, the original
results were relatively stable (Fig.
3).
To the best of our knowledge, the present study
performed the first systematic review and meta-analysis on the
morbidity assessment of sarcopenia among patients with HCC. The
current meta-analysis included 48 studies that evaluated the
morbidity of sarcopenia among patients with HCC and were performed
across nine countries. The outcomes of the present comprehensive
analysis demonstrated that current evidence on the morbidity of
sarcopenia among patients with HCC varied considerably depending on
the region, average age, proportion of male patients and diagnostic
criteria used.
Overall, the present meta-analysis confirmed that a
high proportion of patients with HCC suffered from sarcopenia
(42%). The morbidity of sarcopenia in Europe (56%) was higher
compared with that in other continents, especially Asia (39%). In
addition, the incidence rate of sarcopenia in studies with a high
proportion of male patients (45%) was higher than that in studies
with a low proportion of male patients (37%). It was also revealed
that the studies with PMI or FFMA as the diagnostic standard had
the highest incidence of sarcopenia (54%) among all diagnostic
criteria used. When SMI was greater than the cut-off value of the
diagnostic criteria for both male and female patients, the
incidence rate was also high (50%). Surprisingly, the morbidity
rate of sarcopenia in the young age group (46%) was higher than
that in the old age group (39%). All the epidemiological data were
significantly higher than those of healthy individuals, indicating
that sarcopenia is an urgent problem occurring in patients with
HCC, and further research into its prevention and treatment is
required to improve patient prognosis (64).
The present systematic review and meta-analysis had
several limitations that need to be addressed. Firstly, most of the
included studies were conducted in Asia, especially Japan;
therefore, the incidence rate of sarcopenia in patients with HCC
reported in the present study did not fully represent the global
trend. Secondly, only studies published in English were included;
therefore, the results of studies published in other languages were
omitted.
In the present study, nearly half of the patients
with HCC exhibited sarcopenia. Numerous studies have also reported
that sarcopenia significantly negatively affects the survival
outcomes of patients with HCC. Several important factors contribute
to the high morbidity associated with sarcopenia in patients with
HCC. First, cancer leads to changes in the patients' lifestyle,
such as decreased physical activity and reduced food intake, which
can lead to the loss of muscle volume and insufficient protein
intake, thus aggravating the degree of sarcopenia (65,66).
Second, in HCC proinflammatory cytokines(including IL-6 and TNF-a)
are released, thereby interfering with related molecular pathways
(such as the PI3K/Akt and Akt-mTOR pathways), which consequently
causes muscle recession (67).
Third, HCC disrupts the normal metabolic mechanisms in the human
body, such as reducing the content of testosterone, thereby slowing
down muscle growth (68). In
addition, HCC can affect cellular processes, leading to cell
autophagy, oxidative stress and mitochondrial dysfunction, which
ultimately leads to muscle cell atrophy (69). In summary, multiple factors may
jointly contribute to the high incidence rate of sarcopenia in
patients with HCC.
The current analysis showed that studies with a high
proportion of male patients had a higher morbidity of sarcopenia
compared with studies with a lower proportion of males patients,
which was consistent with the prevalence of sarcopenia reported in
the general population (70). The
possible reasons for the difference in the incidence rate of
sarcopenia between sexes include different hormone profiles and
distinct muscle sensitivities when hormone levels decrease
(71). Therefore, biological and
genetic differences may be the most important factors affecting the
changes observed. It may be hypothesized that sarcopenia can have a
higher incidence rate in the older age group compared with younger
individuals; however, the opposite conclusion was reached by the
present study. A potential reason for this may be the higher
malignancy of HCC in the younger population (72).
The current meta-analysis showed considerable
heterogeneity; therefore, a cautious interpretation of the pooled
data is necessary. This heterogeneity may be owing to the features
of the patients and methodological differences in the included
studies. Therefore, a subgroup analysis was performed by region,
male proportion, average age and diagnostic criteria, to resolve
the potential sources of heterogeneity. Subsequently, by conducting
a meta-regression analysis, it was found that the total sample size
could explain nearly half of the heterogeneity.
The present systematic review confirmed that the
morbidity of sarcopenia is high in patients with HCC, indicating
the benefits of early screening and prevention of sarcopenia in
this population. However, in the near future, more in-depth
research is needed on the causes of sarcopenia in patients with
HCC. Additionally, efforts should be made to study the precautions
and treatment of sarcopenia in patients with HCC.
The authors would like to thank Dr Minglin Li (China
Medical University, Shenyang, China) for support with study
retrieval.
This work was supported by the 345 Talent Project of Shengjing
Hospital of China Medical University.
The datasets used and/or analysed during the current
study are available from the corresponding author on reasonable
request.
JW was responsible for study design. LH was in
charge of analyzing the data. JL and HL wrote the manuscript and
conducted the acquisition and interpretation of data. JL and LH
confirm the authenticity of all the raw data. All authors have read
and approved the final manuscript.
Not applicable.
Not applicable.
The authors declare that they have no competing
interests.
|
1
|
Hartke J, Johnson M and Ghabril M: The
diagnosis and treatment of hepatocellular carcinoma. Semin Diagn
Pathol. 34:153–159. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rumgay H, Arnold M, Ferlay J, Lesi O,
Cabasag CJ, Vignat J, Laversanne M, McGlynn KA and Soerjomataram I:
Global burden of primary liver cancer in 2020 and predictions to
2040. J Hepatol. 77:1598–1606. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Li C and He WQ: Comparison of primary
liver cancer mortality estimates from World Health Organization,
global burden disease and global cancer observatory. Liver Int.
42:2299–2316. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Clark T, Maximin S, Meier J, Pokharel S
and Bhargava P: Hepatocellular carcinoma: Review of epidemiology,
screening, imaging diagnosis, response assessment, and treatment.
Curr Probl Diagn Radiol. 44:479–486. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Villanueva A: Hepatocellular carcinoma. N
Engl J Med. 380:1450–1462. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chang KV, Chen JD, Wu WT, Huang KC, Hsu CT
and Han DS: Association between loss of skeletal muscle mass and
mortality and tumor recurrence in hepatocellular carcinoma: A
systematic review and meta-analysis. Liver Cancer. 7:90–103. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Papadopoulou SK: Sarcopenia: A
contemporary health problem among older adult populations.
Nutrients. 12:12932020. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rier HN, Jager A, Sleijfer S, Maier AB and
Levin MD: The prevalence and prognostic value of low muscle mass in
cancer patients: A review of the literature. Oncologist.
21:1396–1409. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gibson DJ, Burden ST, Strauss BJ, Todd C
and Lal S: The role of computed tomography in evaluating body
composition and the influence of reduced muscle mass on clinical
outcome in abdominal malignancy: A systematic review. Eur J Clin
Nutr. 69:1079–1086. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shachar SS, Williams GR, Muss HB and
Nishijima TF: Prognostic value of sarcopenia in adults with solid
tumours: A meta-analysis and systematic review. Eur J Cancer.
57:58–67. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Moher D, Shamseer L, Clarke M, Ghersi D,
Liberati A, Petticrew M, Shekelle P and Stewart LA; PRISMA-P Group,
: Preferred reporting items for systematic review and meta-analysis
protocols (PRISMA-P) 2015 statement. Syst Rev. 4:12015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lo CK, Mertz D and Loeb M:
Newcastle-Ottawa Scale: Comparing reviewers' to authors'
assessments. BMC Med Res Methodol. 14:452014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Borenstein M, Hedges LV, Higgins JP and
Rothstein HR: A basic introduction to fixed-effect and
random-effects models for meta-analysis. Res Synth Methods.
1:97–111. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Higgins JP, Thompson SG, Deeks JJ and
Altman DG: Measuring inconsistency in meta-analyses. BMJ.
327:557–560. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Duval S and Tweedie R: Trim and fill: A
simple funnel-plot-based method of testing and adjusting for
publication bias in meta-analysis. Biometrics. 56:455–463. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Alsebaey A, Sabry A, Rashed HS, Elsabaawy
MM, Ragab A, Aly RA and Badran H: MELD-sarcopenia is better than
ALBI and MELD score in patients with hepatocellular carcinoma
awaiting liver transplantation. Asian Pac J Cancer Prev.
22:2005–2009. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Akce M, Liu Y, Zakka KM, Martini DJ,
Draper A, Alese OB, Shaib WL, Wu C, Wedd J, Sellers MT, et al: The
impact of inflammatory biomarkers, BMI, and sarcopenia on survival
in advanced hepatocellular carcinoma treated with immunotherapy. J
Clin Oncol. 38 (4 Suppl):S5532020. View Article : Google Scholar
|
|
18
|
Begini P, Gigante E, Antonelli G,
Carbonetti F, Iannicelli E, Anania G, Imperatrice B, Pellicelli AM,
Fave GD and Marignani M: Sarcopenia predicts reduced survival in
patients with hepatocellular carcinoma at first diagnosis. Ann
Hepatol. 16:107–114. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Dong D, Shi JY, Shang X, Liu B, Xu WL, Cui
GZ and Wang NY: Prognostic significance of sarcopenia in patients
with hepatocellular carcinoma treated with lenvatinib: A
retrospective analysis. Medicine (Baltimore). 101:e286802022.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Guichet PL, Taslakian B, Zhan C, Aaltonen
E, Farquharson S, Hickey R, Horn CJ and Gross JS: MRI-derived
sarcopenia associated with increased mortality following yttrium-90
radioembolization of hepatocellular carcinoma. Cardiovasc Intervent
Radiol. 44:1561–1569. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ha Y, Kim D, Han S, Chon YE, Lee YB, Kim
MN, Lee JH, Park H, Rim KS and Hwang SG: Sarcopenia predicts
prognosis in patients with newly diagnosed hepatocellular
carcinoma, independent of tumor stage and liver function. Cancer
Res Treat. 50:843–851. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hirota K, Kawaguchi T, Koya S, Nagamatsu
A, Tomita M, Hashida R, Nakano D, Niizeki T, Matsuse H, Shiba N and
Torimura T: Clinical utility of the liver frailty index for
predicting muscle atrophy in chronic liver disease patients with
hepatocellular carcinoma. Hepatol Res. 50:330–341. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Imai K, Takai K, Watanabe S, Hanai T,
Suetsugu A, Shiraki M and Shimizu M: Sarcopenia impairs prognosis
of patients with hepatocellular carcinoma: The role of liver
functional reserve and tumor-related factors in loss of skeletal
muscle volume. Nutrients. 9:10542017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kim YR, Park S, Han S, Ahn JH, Kim S, Sinn
DH, Jeong WK, Ko JS, Gwak MS and Kim GS: Sarcopenia as a predictor
of post-transplant tumor recurrence after living donor liver
transplantation for hepatocellular carcinoma beyond the Milan
criteria. Sci Rep. 8:71572018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kobayashi A, Kaido T, Hamaguchi Y, Okumura
S, Shirai H, Yao S, Kamo N, Yagi S, Taura K, Okajima H and Uemoto
S: Impact of sarcopenic obesity on outcomes in patients undergoing
hepatectomy for hepatocellular carcinoma. Ann Surg. 269:924–931.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kobayashi T, Kawai H, Nakano O, Abe S,
Kamimura H, Sakamaki A, Kamimura K, Tsuchiya A, Takamura M,
Yamagiwa S and Terai S: Rapidly declining skeletal muscle mass
predicts poor prognosis of hepatocellular carcinoma treated with
transcatheter intra-arterial therapies. BMC Cancer. 18:7562018.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kotoh Y, Saeki I, Yamasaki T, Sasaki R,
Tanabe N, Oono T, Matsuda T, Hisanaga T, Matsumoto T, Hidaka I, et
al: Effect of handgrip strength on clinical outcomes of patients
with hepatocellular carcinoma treated with lenvatinib. Appl Sci.
10:54032020. View Article : Google Scholar
|
|
28
|
Kroh A, Uschner D, Lodewick T, Eickhoff
RM, Schöning W, Ulmer FT, Neumann UP and Binnebösel M: Impact of
body composition on survival and morbidity after liver resection in
hepatocellular carcinoma patients. Hepatobiliary Pancreat Dis Int.
18:28–37. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lanza E, Masetti C, Messana G, Muglia R,
Pugliese N, Ceriani R, Lleo de Nalda A, Rimassa L, Torzilli G,
Poretti D, et al: Sarcopenia as a predictor of survival in patients
undergoing bland transarterial embolization for unresectable
hepatocellular carcinoma. PLoS One. 15:e02323712020. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Lee J, Cho Y, Park S, Kim JW and Lee IJ:
Skeletal muscle depletion predicts the prognosis of patients with
hepatocellular carcinoma treated with radiotherapy. Front Oncol.
9:10752019. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Levolger S, van Vledder MG, Muslem R, Koek
M, Niessen WJ, de Man RA, de Bruin RW and Ijzermans JN: Sarcopenia
impairs survival in patients with potentially curable
hepatocellular carcinoma. J Surg Oncol. 112:208–213. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Liao C, Li G, Bai Y, Zhou S, Huang L, Yan
M, Qiu F, Chen J, Wang Y, Tian Y and Chen S: Prognostic value and
association of sarcopenic obesity and systemic inflammatory indexes
in patients with hepatocellular carcinoma following hepatectomy and
the establishment of novel predictive nomograms. J Gastrointest
Oncol. 12:669–693. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Meister FA, Lurje G, Verhoeven S,
Wiltberger G, Heij L, Liu WJ, Jiang D, Bruners P, Lang SA, Ulmer
TF, et al: The role of sarcopenia and myosteatosis in short- and
long-term outcomes following curative-intent surgery for
hepatocellular carcinoma in a European cohort. Cancers (Basel).
14:7202022. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Meza-Junco J, Montano-Loza AJ, Baracos VE,
Prado CM, Bain VG, Beaumont C, Esfandiari N, Lieffers JR and Sawyer
MB: Sarcopenia as a prognostic index of nutritional status in
concurrent cirrhosis and hepatocellular carcinoma. J Clin
Gastroenterol. 47:861–870. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Salman A, Salman M, Moustafa A, Shaaban
HE, El-Mikkawy A, Labib S, Youssef A, Omar MG, Matter M and
Elkassar H: Impact of sarcopenia on two-year mortality in patients
with hcv-associated hepatocellular carcinoma after radiofrequency
ablation. J Hepatocell Carcinoma. 8:313–320. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Salman MA, Omar HSE, Mikhail HMS, Tourky
M, El-Ghobary M, Elkassar H, Omar MG, Matter M, Elbasiouny AM,
Farag AM, et al: Sarcopenia increases 1-year mortality after
surgical resection of hepatocellular carcinoma. ANZ J Surg.
90:781–785. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Shiba S, Shibuya K, Katoh H, Koyama Y,
Okamoto M, Abe T, Ohno T and Nakano T: No deterioration in clinical
outcomes of carbon ion radiotherapy for sarcopenia patients with
hepatocellular carcinoma. Anticancer Res. 38:3579–3586. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Takagi K, Yagi T, Yoshida R, Shinoura S,
Umeda Y, Nobuoka D, Kuise T, Watanabe N and Fujiwara T: Sarcopenia
and American society of anesthesiologists physical status in the
assessment of outcomes of hepatocellular carcinoma patients
undergoing hepatectomy. Acta Med Okayama. 70:363–370.
2016.PubMed/NCBI
|
|
39
|
Antonelli G, Gigante E, Iavarone M, Begini
P, Sangiovanni A, Iannicelli E, Biondetti P, Pellicelli AM,
Miglioresi L, Marchetti P, et al: Sarcopenia is associated with
reduced survival in patients with advanced hepatocellular carcinoma
undergoing sorafenib treatment. United European Gastroenterol J.
6:1039–1048. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Harimoto N, Shirabe K, Yamashita YI,
Ikegami T, Yoshizumi T, Soejima Y, Ikeda T, Maehara Y, Nishie A and
Yamanaka T: Sarcopenia as a predictor of prognosis in patients
following hepatectomy for hepatocellular carcinoma. Br J Surg.
100:1523–1530. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
41
|
Nishikawa H, Nishijima N, Enomoto H,
Sakamoto A, Nasu A, Komekado H, Nishimura T, Kita R, Kimura T,
Iijima H, et al: Prognostic significance of sarcopenia in patients
with hepatocellular carcinoma undergoing sorafenib therapy. Oncol
Lett. 14:1637–1647. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Chen BB, Liang PC, Shih TT, Liu TH, Shen
YC, Lu LC, Lin ZZ, Hsu C, Hsu CH, Cheng AL and Shao YY: Sarcopenia
and myosteatosis are associated with survival in patients receiving
immunotherapy for advanced hepatocellular carcinoma. Eur Radiol.
33:512–522. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Naganuma A, Hoshino T, Suzuki Y, Uehara D,
Kudo T, Ishihara H, Sato K, Kakizaki S, Yamada M and Takagi H:
Association between skeletal muscle depletion and sorafenib
treatment in male patients with hepatocellular carcinoma: A
retrospective cohort study. Acta Med Okayama. 71:291–299.
2017.PubMed/NCBI
|
|
44
|
Mardian Y, Yano Y, Ratnasari N, Choridah
L, Wasityastuti W, Setyawan NH and Hayashi Y: ‘Sarcopenia and
intramuscular fat deposition are associated with poor survival in
Indonesian patients with hepatocellular carcinoma: A retrospective
study’. BMC Gastroenterol. 19:2292019. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Badran H, Elsabaawy MM, Ragab A, Aly RA,
Alsebaey A and Sabry A: Baseline sarcopenia is associated with lack
of response to therapy, liver decompensation and high mortality in
hepatocellular carcinoma patients. Asian Pac J Cancer Prev.
21:3285–3290. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Hou GM, Jiang C, Du JP and Yuan KF:
Sarcopenia predicts an adverse prognosis in patients with combined
hepatocellular carcinoma and cholangiocarcinoma after surgery.
Cancer Med. 11:317–331. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Imai K, Takai K, Miwa T, Taguchi D, Hanai
T, Suetsugu A, Shiraki M and Shimizu M: Rapid depletion of
subcutaneous adipose tissue during sorafenib treatment predicts
poor survival in patients with hepatocellular carcinoma. Cancers
(Basel). 12:17952020. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Endo K, Kuroda H, Kanazawa J, Sato T,
Fujiwara Y, Abe T, Sato H, Kooka Y, Oikawa T, Sawara K and Takikawa
Y: Impact of grip strength in patients with unresectable
hepatocellular carcinoma treated with lenvatinib. Cancers (Basel).
12:21462020. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Choi K, Jang HY, Ahn JM, Hwang SH, Chung
JW, Choi YS, Kim JW, Jang ES, Choi GH and Jeong SH: The association
of the serum levels of myostatin, follistatin, and interleukin-6
with sarcopenia, and their impacts on survival in patients with
hepatocellular carcinoma. Clin Mol Hepatol. 26:492–505. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Harimoto N, Yoshizumi T, Shimokawa M,
Sakata K, Kimura K, Itoh S, Ikegami T, Ikeda T, Shirabe K and
Maehara Y: Sarcopenia is a poor prognostic factor following hepatic
resection in patients aged 70 years and older with hepatocellular
carcinoma. Hepatol Res. 46:1247–1255. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Kamachi S, Mizuta T, Otsuka T, Nakashita
S, Ide Y, Miyoshi A, Kitahara K, Eguchi Y, Ozaki I and Anzai K:
Sarcopenia is a risk factor for the recurrence of hepatocellular
carcinoma after curative treatment. Hepatol Res. 46:201–208. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Zhang JX, Yan HT, Ding Y, Liu J, Liu S, Zu
QQ and Shi HB: Low psoas-muscle index is associated with decreased
survival in hepatocellular carcinoma treated with transarterial
chemoembolization. Ann Med. 54:1562–1569. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Yabusaki N, Fujii T, Yamada S, Suzuki K,
Sugimoto H, Kanda M, Nakayama G, Koike M, Fujiwara M and Kodera Y:
Adverse impact of low skeletal muscle index on the prognosis of
hepatocellular carcinoma after hepatic resection. Int J Surg.
30:136–142. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Fujiwara N, Nakagawa H, Kudo Y, Tateishi
R, Taguri M, Watadani T, Nakagomi R, Kondo M, Nakatsuka T, Minami
T, et al: Sarcopenia, intramuscular fat deposition, and visceral
adiposity independently predict the outcomes of hepatocellular
carcinoma. J Hepatol. 63:131–140. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Acosta LF, Galuppo R, García CR,
Villacorta E, Dugan A, Castellanos AL, Gedaly R and Lee JT:
Association between sarcopenia and AFP level in patients undergoing
liver transplantation for hepatocellular carcinoma. J Surg Res.
238:10–15. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Yang J, Chen K, Zheng C, Chen K, Lin J,
Meng Q, Chen Z, Deng L, Yu H, Deng T, et al: Impact of sarcopenia
on outcomes of patients undergoing liver resection for
hepatocellular carcinoma. J Cachexia Sarcopenia Muscle.
13:2383–2392. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Hamaguchi Y, Kaido T, Okumura S, Kobayashi
A, Shirai H, Yao S, Yagi S, Kamo N, Seo S, Taura K, et al:
Preoperative visceral adiposity and muscularity predict poor
outcomes after hepatectomy for hepatocellular carcinoma. Liver
Cancer. 8:92–109. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Uojima H, Chuma M, Tanaka Y, Hidaka H,
Nakazawa T, Iwabuchi S, Kobayashi S, Hattori N, Ogushi K, Morimoto
M, et al: Skeletal muscle mass influences tolerability and
prognosis in hepatocellular carcinoma patients treated with
lenvatinib. Liver Cancer. 9:193–206. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Takada H, Kurosaki M, Nakanishi H,
Takahashi Y, Itakura J, Tsuchiya K, Yasui Y, Tamaki N, Takaura K,
Komiyama Y, et al: Impact of pre-sarcopenia in sorafenib treatment
for advanced hepatocellular carcinoma. PLoS One. 13:e01988122018.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Tan Y, Duan T, Li B, Zhang B, Zhu Y, Yan
K, Song J, Lv T, Yang J, Jiang L, et al: Sarcopenia defined by
psoas muscle index independently predicts long-term survival after
living donor liver transplantation in male recipients. Quant
Imaging Med Surg. 12:215–228. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Kim N, Yu JI, Park HC, Yoo GS, Choi C,
Hong JY, Lim HY, Lee J, Choi MS, Lee JE and Kim K: Incorporating
sarcopenia and inflammation with radiation therapy in patients with
hepatocellular carcinoma treated with nivolumab. Cancer Immunol
Immunother. 70:1593–1603. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Iritani S, Imai K, Takai K, Hanai T, Ideta
T, Miyazaki T, Suetsugu A, Shiraki M, Shimizu M and Moriwaki H:
Skeletal muscle depletion is an independent prognostic factor for
hepatocellular carcinoma. J Gastroenterol. 50:323–232. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Voron T, Tselikas L, Pietrasz D, Pigneur
F, Laurent A, Compagnon P, Salloum C, Luciani A and Azoulay D:
Sarcopenia impacts on short- and long-term results of hepatectomy
for hepatocellular carcinoma. Ann Surg. 261:1173–1183. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Bischoff-Ferrari HA, Orav JE, Kanis JA,
Rizzoli R, Schlögl M, Staehelin HB, Willett WC and Dawson-Hughes B:
Comparative performance of current definitions of sarcopenia
against the prospective incidence of falls among community-dwelling
seniors age 65 and older. Osteoporos Int. 26:2793–2802. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Williams GR, Dunne RF, Giri S, Shachar SS
and Caan BJ: Sarcopenia in the older adult with cancer. J Clin
Oncol. 39:2068–2078. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Giallauria F, Cittadini A, Smart NA and
Vigorito C: Resistance training and sarcopenia. Monaldi Arch Chest
Dis. 84:7382016. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Fan J, Kou X, Yang Y and Chen N:
MicroRNA-regulated proinflammatory cytokines in sarcopenia.
Mediators Inflamm. 2016:14386862016. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Sinclair M, Grossmann M, Angus PW,
Hoermann R, Hey P, Scodellaro T and Gow PJ: Low testosterone as a
better predictor of mortality than sarcopenia in men with advanced
liver disease. J Gastroenterol Hepatol. 31:661–667. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Phillips T and Leeuwenburgh C: Muscle
fiber specific apoptosis and TNF-alpha signaling in sarcopenia are
attenuated by life-long calorie restriction. FASEB J. 19:668–670.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Anderson LJ, Liu H and Garcia JM: Sex
differences in muscle wasting. Adv Exp Med Biol. 1043:153–197.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Janssen I, Heymsfield SB, Wang ZM and Ross
R: Skeletal muscle mass and distribution in 468 men and women aged
18–88 yr. J Appl Physiol (1985). 89:81–88. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Llovet JM, Kelley RK, Villanueva A, Singal
AG, Pikarsky E, Roayaie S, Lencioni R, Koike K, Zucman-Rossi J and
Finn RS: Hepatocellular carcinoma. Nat Rev Dis Primers. 7:62021.
View Article : Google Scholar : PubMed/NCBI
|