|
1
|
Kamisawa T, Kaneko K, Itoi T and Ando H:
Pancreaticobiliary maljunction and congenital biliary dilatation.
Lancet Gastroenterol Hepatol. 2:610–618. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ono A, Arizono S, Isoda H and Togashi K:
Imaging of pancreaticobiliary maljunction. Radiographics.
40:378–392. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Nikolaidis P, Hammond NA, Day K, Yaghmai
V, Wood CG III, Mosbach DS, Harmath CB, Taffel MT, Horowitz JM,
Berggruen SM and Miller FH: Imaging features of benign and
malignant ampullary and periampullary lesions. Radiographics.
34:624–641. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zulfiqar M, Chatterjee D, Yoneda N,
Hoegger MJ, Ronot M, Hecht EM, Bastati N, Ba-Ssalamah A, Bashir MR
and Fowler K: Imaging features of premalignant biliary lesions and
predisposing conditions with pathologic correlation. Radiographics.
42:1320–1337. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhu D, Yang K, Li Y, Ye X, Zhang H, Long
Q, Ding X, Dong F and Xu J: Differential diagnostic value of
periampullary mass: A nomogram established by random forest based
on clinical characteristics and contrast-enhanced ultrasound. J
Clin Ultrasound. 50:918–928. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Al-Hawary MM, Kaza RK and Francis IR:
Optimal imaging modalities for the diagnosis and staging of
periampullary masses. Surg Oncol Clin N Am. 25:239–253. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chen XP, Liu J, Zhou J, Zhou PC, Shu J, Xu
LL, Li B and Su S: Combination of CEUS and MRI for the diagnosis of
periampullary space-occupying lesions: A retrospective analysis.
BMC Med Imaging. 19:772019. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fang C, Zhang P and Qi X: Digital and
intelligent liver surgery in the new era: Prospects and dilemmas.
EBioMedicine. 41:693–701. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rizzo A and Brandi G: Neoadjuvant therapy
for cholangiocarcinoma: A comprehensive literature review. Cancer
Treat Res Commun. 27:1003542021. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rizzo A and Brandi G: Pitfalls,
challenges, and updates in adjuvant systemic treatment for resected
biliary tract cancer. Expert Rev Gastroenterol Hepatol. 15:547–554.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Di Federico A, Mosca M, Pagani R, Carloni
R, Frega G, De Giglio A, Rizzo A, Ricci D, Tavolari S, Di Marco M,
et al: Immunotherapy in pancreatic cancer: why do we keep failing?
A focus on tumor immune microenvironment, Predictive biomarkers and
treatment outcomes. Cancers (Basel). 14:24292022. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Guven DC, Sahin TK, Erul E, Rizzo A, Ricci
AD, Aksoy S and Yalcin S: The association between albumin levels
and survival in patients treated with immune checkpoint inhibitors:
A systematic review and meta-analysis. Front Mol Biosci.
9:10391212022. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Di Federico A, Tateo V, Parisi C, Formica
F, Carloni R, Frega G, Rizzo A, Ricci D, Di Marco M, Palloni A and
Brandi G: Hacking pancreatic cancer: Present and future of
personalized medicine. Pharmaceuticals (Basel). 14:6772021.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Padilla-Thornton AE, Willmann JK and
Jeffrey RB: Adenocarcinoma of the uncinate process of the pancreas:
MDCT patterns of local invasion and clinical features at
presentation. Eur Radiol. 22:1067–1074. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Loi M, Magallon-Baro A, Suker M, van Eijck
C, Sharma A, Hoogeman M and Nuyttens J: Pancreatic cancer treated
with SBRT: Effect of anatomical interfraction variations on dose to
organs at risk. Radiother Oncol. 134:67–73. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gaballah AH, Kazi IA, Zaheer A, Liu PS,
Badawy M, Moshiri M, Ibrahim MK, Soliman M, Kimchi E and Elsayes
KM: Imaging after pancreatic surgery: Expected findings and
postoperative complications. Radiographics. 44:e2300612024.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bello HR, Sekhar A, Filice RW, Radmard AR
and Davarpanah AH: Pancreaticoduodenal groove: Spectrum of disease
and imaging features. Radiographics. 42:1062–1080. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sah SK, Panth H and Wang YX: Morphometric
analysis of common bile duct: A cadaveric study. J Biomed Res
Environ Sci. 2:64–68. 2021. View Article : Google Scholar
|
|
19
|
Bhutia KD, Lachungpa T and Lamtha SC:
Etiology of obstructive jaundice and its correlation with the
ethnic population of Sikkim. J Family Med Prim Care. 10:4189–4192.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Okano K, Oshima M, Suto H, Ando Y, Asano
E, Kamada H, Kobara H, Masaki T and Suzuki Y: Ampullary carcinoma
of the duodenum: Current clinical issues and genomic overview. Surg
Today. 52:189–197. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hou C, Zhang H, Wang X and Yang Z: The
‘Hand as Foot’ teaching method in the duodenum anatomy. Asian J
Surg. 45:1768–1769. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wu X, Niu R and Wu Y: The ‘Hand as Foot’
teaching method in pancreas-duodenum anatomy. Asian J Surg.
46:1448–1449. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Pickhardt PJ and Bhalla S: Intestinal
malrotation in adolescents and adults: Spectrum of clinical and
imaging features. AJR Am J Roentgenol. 179:1429–1435. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Johnson LN, Moran SK, Bhargava P, Revels
JW, Moshiri M, Rohrmann CA and Mansoori B: Fluoroscopic evaluation
of duodenal diseases. Radiographics. 42:397–416. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhang JY, Huang J and Yang ZY: Abdominal
pain after subtotal gastrectomy: A first report of accessory
pancreatic fistula. J Pain Res. 13:431–435. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Apurva Abdul Sattar RS, Ali A, Nimisha
Kumar Sharma A, Kumar A, Santoshi S and Saluja SS: Molecular
pathways in periampullary cancer: An overview. Cell Signal.
100:1104612022. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Perri G, Bortolato C, Marchegiani G,
Holmberg M, Romandini E, Sturesson C, Bassi C, Sparrelid E,
Ghorbani P and Salvia R: Pure biliary leak vs pancreatic fistula
associated: Non-identical twins following pancreatoduodenectomy.
HPB (Oxford). 24:1474–1481. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Pecorelli N, Capretti G, Sandini M,
Damascelli A, Cristel G, De Cobelli F, Gianotti L, Zerbi A and
Braga M: Impact of sarcopenic obesity on failure to rescue from
major complications following pancreaticoduodenectomy for cancer:
Results from a multicenter study. Ann Surg Oncol. 25:308–317. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Skórzewska M, Kurzawa P, Ciszewski T, Pelc
Z and Polkowski WP: Controversies in the diagnosis and treatment of
periampullary tumours. Surg Oncol. 44:1018532022. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Amr B, Shahtahmassebi G, Briggs CD, Bowles
MJ, Aroori S and Stell DA: Assessment of the effect of interval
from presentation to surgery on outcome in patients with
peri-ampullary malignancy. HPB (Oxford). 18:354–359. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Khan IA, Singh N, Gunjan D, Nayak B, Dash
NR, Pal S, Lohani N, Yadav R, Gupta S and Saraya A: Serum
miR-215-5p, miR-192-5p and miR-378a-5p as novel diagnostic
biomarkers for periampullary adenocarcinoma. Pathol Res Pract.
260:1554172024. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ilic M and Ilic I: Epidemiology of
pancreatic cancer. World J Gastroenterol. 22:9694–9705. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Groot VP, Gemenetzis G, Blair AB,
Rivero-Soto RJ, Yu J, Javed AA, Burkhart RA, Rinkes IHMB, Molenaar
IQ, Cameron JL, et al: Defining and predicting early recurrence in
957 patients with resected pancreatic ductal adenocarcinoma. Ann
Surg. 269:1154–1162. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Groot VP, Rezaee N, Wu W, Cameron JL,
Fishman EK, Hruban RH, Weiss MJ, Zheng L, Wolfgang CL and He J:
Patterns, timing, and predictors of recurrence following
pancreatectomy for pancreatic ductal adenocarcinoma. Ann Surg.
267:936–945. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Wood LD, Canto MI, Jaffee EM and Simeone
DM: Pancreatic cancer: Pathogenesis, screening, diagnosis, and
treatment. Gastroenterology. 163:386–402.e1. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
El Hakim BA, Caid N, Saoudi L, Benemla R,
Ramoul R, Rekkache S and Smaili F: Clinical characteristic of
pancreatic cancer. Ann Oncol. 29 (Suppl 5):S502018. View Article : Google Scholar
|
|
37
|
Hessmann E, Buchholz SM, Demir IE, Singh
SK, Gress TM, Ellenrieder V and Neesse A: Microenvironmental
determinants of pancreatic cancer. Physiol Rev. 100:1707–1751.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Malsy M, Hackl C, Graf B, Bitzinger D and
Bundscherer A: The effects of analgesics on the migration of
pancreatic cancer cells. In Vivo. 36:576–581. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Morita S, Onaya H, Kishi Y, Hiraoka N and
Arai Y: Multiple intraglandular metastases in a patient with
invasive ductal carcinoma of the pancreas. Intern Med.
54:1753–1756. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Nakase A, Koizumi T, Fujita N, Ono H and
Matsumoto Y: Studies of the growth and infiltration of experimental
tumor of the pancreas in rabbits. Am J Surg. 133:590–592. 1977.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Mizrahi JD, Surana R, Valle JW and Shroff
RT: Pancreatic cancer. Lancet. 395:2008–2020. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Burke EE, Marmor S, Virnig BA, Tuttle TM
and Jensen EH: Lymph node evaluation for pancreatic adenocarcinoma
and its value as a quality metric. J Gastrointest Surg.
19:2162–2170. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Shang S, Wang J, Chen S, Tian R, Zeng H,
Wang L, Xia M, Zhu H and Zuo C: Exosomal miRNA-1231 derived from
bone marrow mesenchymal stem cells inhibits the activity of
pancreatic cancer. Cancer Med. 8:7728–7740. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Selvaggi F, Melchiorre E, Casari I,
Cinalli S, Cinalli M, Aceto GM, Cotellese R, Garajova I and Falasca
M: Perineural invasion in pancreatic ductal adenocarcinoma: From
molecules towards drugs of clinical relevance. Cancers (Basel).
14:57932022. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Wang J, Chen Y, Li X and Zou X: Perineural
invasion and associated pain transmission in pancreatic cancer.
Cancers (Basel). 13:45942021. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Yang MW, Tao LY, Jiang YS, Yang JY, Huo
YM, Liu DJ, Li J, Fu XL, He R, Lin C, et al: Perineural invasion
reprograms the immune microenvironment through cholinergic
signaling in pancreatic ductal adenocarcinoma. Cancer Res.
80:1991–2003. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Bapat AA, Hostetter G, Von Hoff DD and Han
H: Perineural invasion and associated pain in pancreatic cancer.
Nat Rev Cancer. 11:695–707. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Tan X, Sivakumar S, Bednarsch J,
Wiltberger G, Kather JN, Niehues J, de Vos-Geelen J, Valkenburg-van
Iersel L, Kintsler S, Roeth A, et al: Nerve fibers in the tumor
microenvironment in neurotropic cancer-pancreatic cancer and
cholangiocarcinoma. Oncogene. 40:899–908. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Banales JM, Marin JJG, Lamarca A,
Rodrigues PM, Khan SA, Roberts LR, Cardinale V, Carpino G, Andersen
JB, Braconi C, et al: Cholangiocarcinoma 2020: The next horizon in
mechanisms and management. Nat Rev Gastroenterol Hepatol.
17:557–588. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Zaccari P, Cardinale V, Severi C, Pedica
F, Carpino G, Gaudio E, Doglioni C, Petrone MC, Alvaro D,
Arcidiacono PG and Capurso G: Common features between neoplastic
and preneoplastic lesions of the biliary tract and the pancreas.
World J Gastroenterol. 25:4343–4359. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Felsenstein M, Hruban RH and Wood LD: New
developments in the molecular mechanisms of pancreatic
tumorigenesis. Adv Anat Pathol. 25:131–142. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Banales JM, Cardinale V, Carpino G,
Marzioni M, Andersen JB, Invernizzi P, Lind GE, Folseraas T, Forbes
SJ, Fouassier L, et al: Expert consensus document:
Cholangiocarcinoma: Current knowledge and future perspectives
consensus statement from the European network for the study of
cholangiocarcinoma (ENS-CCA). Nat Rev Gastroenterol Hepatol.
13:261–280. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Razumilava N and Gores GJ:
Cholangiocarcinoma. Lancet. 383:2168–2179. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Kato Y, Takahashi S, Gotohda N and Konishi
M: The likely sites of nodal metastasis differs according to the
tumor extent in distal bile duct cancer. J Gastrointest Surg.
20:1618–1627. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Min SK, You Y, Choi DW, Han IW, Shin SH,
Yoon S, Jung JH, Yoon SJ and Heo JS: Prognosis of pancreatic head
cancer with different patterns of lymph node metastasis. J
Hepatobiliary Pancreat Sci. 29:1004–1013. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Kwon HJ, Kim SG, Chun JM, Lee WK and Hwang
YJ: Prognostic factors in patients with middle and distal bile duct
cancers. World J Gastroenterol. 20:6658–6665. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Zheng-Pywell R and Reddy S: Ampullary
cancer. Surg Clin North Am. 99:357–367. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Williams JL, Chan CK, Toste PA, Elliott
IA, Vasquez CR, Sunjaya DB, Swanson EA, Koo J, Hines OJ, Reber HA,
et al: Association of histopathologic phenotype of periampullary
adenocarcinomas with survival. JAMA Surg. 152:82–88. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Nakeeb A, Pitt HA, Sohn TA, Coleman J,
Abrams RA, Piantadosi S, Hruban RH, Lillemoe KD, Yeo CJ and Cameron
JL: Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and
distal tumors. Ann Surg. 224:463–475. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Khan SA, Davidson BR, Goldin R, Pereira
SP, Rosenberg WM, Taylor-Robinson SD, Thillainayagam AV, Thomas HC,
Thursz MR and Wasan H; British Society of Gastroenterology, :
Guidelines for the diagnosis and treatment of cholangiocarcinoma:
Consensus document. Gut. 51 (Suppl 6):VI1–VI9. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Jiang S, Zhao R, Li Y, Han X, Liu Z, Ge W,
Dong Y and Han W: Prognosis and nomogram for predicting
postoperative survival of duodenal adenocarcinoma: A retrospective
study in China and the SEER database. Sci Rep. 8:79402018.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Nishio K, Kimura K, Murata A, Ohira G,
Shinkawa H, Kodai S, Amano R, Tanaka S, Shimizu S, Takemura S, et
al: Comparison of clinicopathological characteristics between
resected ampullary carcinoma and carcinoma of the second portion of
the duodenum. World J Gastrointest Surg. 14:1219–1229. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Burasakarn P, Higuchi R, Nunobe S, Kanaji
S, Eguchi H, Okada KI, Fujii T, Nagakawa Y, Kanetaka K, Yamashita
H, et al: Limited resection vs pancreaticoduodenectomy for primary
duodenal adenocarcinoma: A systematic review and meta-analysis. Int
J Clin Oncol. 26:450–460. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Zhao Z, Zhang J, Li C, Liu T and Li W:
Surgical treatment and survival analysis of primary duodenal
malignant tumor: A retrospective cohort study. J Gastrointest
Oncol. 13:1733–1745. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Xue Y, Vanoli A, Balci S, Reid MM, Saka B,
Bagci P, Memis B, Choi H, Ohike N, Tajiri T, et al:
Non-ampullary-duodenal carcinomas: Clinicopathologic analysis of 47
cases and comparison with ampullary and pancreatic adenocarcinomas.
Mod Pathol. 30:255–266. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Zhang S, Cui Y, Zhong B, Xiao W, Gong X,
Chao K and Chen M: Clinicopathological characteristics and survival
analysis of primary duodenal cancers: A 14-year experience in a
tertiary centre in South China. Int J Colorectal Dis. 26:219–226.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Yabuuchi Y, Yoshida M, Kakushima N, Kato
M, Iguchi M, Yamamoto Y, Kanetaka K, Uraoka T, Fujishiro M and Sho
M; Japan Duodenal Cancer Committee, : Risk factors for
non-ampullary duodenal adenocarcinoma: A systematic review. Dig
Dis. 40:147–155. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Overman MJ, Hu CY, Kopetz S, Abbruzzese
JL, Wolff RA and Chang GJ: A population-based comparison of
adenocarcinoma of the large and small intestine: Insights into a
rare disease. Ann Surg Oncol. 19:1439–1445. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Kakushima N, Ono H, Yoshida M, Takizawa K,
Tanaka M, Kawata N, Ito S, Imai K, Hotta K, Ishiwatari H and
Matsubayashi H: Characteristics and risk factors for sporadic
non-ampullary duodenal adenocarcinoma. Scand J Gastroenterol.
52:1253–1257. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Woo SM, Ryu JK, Lee SH, Yoo JW, Park JK,
Kim YT, Jang JY, Kim SW, Kang GH and Yoon YB: Recurrence and
prognostic factors of ampullary carcinoma after radical resection:
Comparison with distal extrahepatic cholangiocarcinoma. Ann Surg
Oncol. 14:3195–3201. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Secchi M, Leonardo R, Esteban M, Mario C
and Alejandro A: Periampullary malignant tumors. Management and
prognostic. Pancreatology. 17:S162017. View Article : Google Scholar
|
|
72
|
Ma Y, Jiang Q, Zhang Z, Xiao P, Yan Y, Liu
J, Li Q and Wang Z: Diagnosis of hirschsprung disease by
hydrocolonic sonography in children. Eur Radiol. 32:2089–2098.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Limberg B: Diagnosis and staging of
colonic tumors by conventional abdominal sonography as compared
with hydrocolonic sonography. N Engl J Med. 327:65–69. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Wang L, Wang X, Kou H, He H, Lu M, Zhou L
and Yang Y: Comparing single oral contrast-enhanced ultrasonography
and double contrast-enhanced ultrasonography in the preoperative
Borrmann classification of advanced gastric cancer. Oncotarget.
9:8716–8724. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Zhang T, Su ZZ, Wang P, Wu T, Tang W, Xu
EJ, Ju JX, Quan XY and Zheng RQ: Double contrast-enhanced
ultrasonography in the detection of periampullary cancer:
Comparison with B-mode ultrasonography and MR imaging. Eur J
Radiol. 85:1993–2000. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Li T, Lu M, Song J, Wu P, Cheng X and
Zhang Z: Improvement to ultrasonographical differential diagnosis
of gastric lesions: The value of contrast enhanced sonography with
gastric distention. PLoS One. 12:e01823322017. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Maconi G, Radice E, Bareggi E and Porro
GB: Hydrosonography of the gastrointestinal tract. AJR Am J
Roentgenol. 193:700–708. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Trikudanathan G, Njei B, Attam R, Arain M
and Shaukat A: Staging accuracy of ampullary tumors by endoscopic
ultrasound: Meta-analysis and systematic review. Dig Endosc.
26:617–626. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Kitano M, Yoshida T, Itonaga M, Tamura T,
Hatamaru K and Yamashita Y: Impact of endoscopic ultrasonography on
diagnosis of pancreatic cancer. J Gastroenterol. 54:19–32. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Archibugi L, Petrone MC, Tamburrino D,
Crippa S, Dabizzi E, Mariani A, Nicoletti R, Doglioni C, Capurso G,
Falconi M, et al: EUS versus CT scan in establishing the T stage in
surgically resected pancreatic cancer based on the new TNM 8th
edition. Pancreatology. 18 (Suppl):S130–S131. 2018. View Article : Google Scholar
|
|
81
|
Chen CH, Yang CC, Yeh YH, Chou DA and Nien
CK: Reappraisal of endosonography of ampullary tumors: Correlation
with transabdominal sonography, CT, and MRI. J Clin Ultrasound.
37:18–25. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
De Moura DTH, Moura EGH, Bernardo WM, De
Moura ETH, Baraca FI, Kondo A, Matuguma SE and Almeida Artifon EL:
Endoscopic retrograde cholangiopancreatography versus endoscopic
ultrasound for tissue diagnosis of malignant biliary stricture:
Systematic review and meta-analysis. Endosc Ultrasound. 7:10–19.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Oppong KW, Bekkali NLH, Leeds JS, Johnson
SJ, Nayar MK, Darné A, Egan M, Bassett P and Haugk B: Fork-tip
needle biopsy versus fine-needle aspiration in endoscopic
ultrasound-guided sampling of solid pancreatic masses: A randomized
crossover study. Endoscopy. 52:454–461. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Yeo SJ, Cho CM, Jung MK, Seo AN and Bae
HI: Comparison of the diagnostic performances of same-session
endoscopic ultrasound- and endoscopic retrograde
cholangiopancreatography-guided tissue sampling for suspected
biliary strictures at different primary tumor sites. Korean J
Gastroenterol. 73:213–218. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Jo JH, Cho CM, Jun JH, Chung MJ, Kim TH,
Seo DW, Kim J and Park DH; Research Group for Endoscopic
Ultrasonography in KSGE, : Same-session endoscopic
ultrasound-guided fine needle aspiration and endoscopic retrograde
cholangiopancreatography-based tissue sampling in suspected
malignant biliary obstruction: A multicenter experience. J
Gastroenterol Hepatol. 34:799–805. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
De Moura DTH, Ryou M, De Moura EGH,
Ribeiro IB, Bernardo WM and Thompson CC: Endoscopic
ultrasound-guided fine needle aspiration and endoscopic retrograde
cholangiopancreatography-based tissue sampling in suspected
malignant biliary strictures: A meta-analysis of same-session
procedures. Clin Endosc. 53:417–428. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Raman SP and Fishman EK: Abnormalities of
the distal common bile duct and ampulla: Diagnostic approach and
differential diagnosis using multiplanar reformations and 3D
imaging. AJR Am J Roentgenol. 203:17–28. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Hashemzadeh S, Mehrafsa B, Kakaei F,
Javadrashid R, Golshan R, Seifar F, Hajibonabi F and Salmannezhad
Khorami F: Diagnostic accuracy of a 64-slice multi-detector CT scan
in the preoperative evaluation of periampullary neoplasms. J Clin
Med. 7:912018. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Liang H, Zhou Y, Zheng Q, Yan G, Liao H,
Du S, Zhang X, Lv F, Zhang Z and Li YM: Dual-energy CT with virtual
monoenergetic images and iodine maps improves tumor conspicuity in
patients with pancreatic ductal adenocarcinoma. Insights Imaging.
13:1532022. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
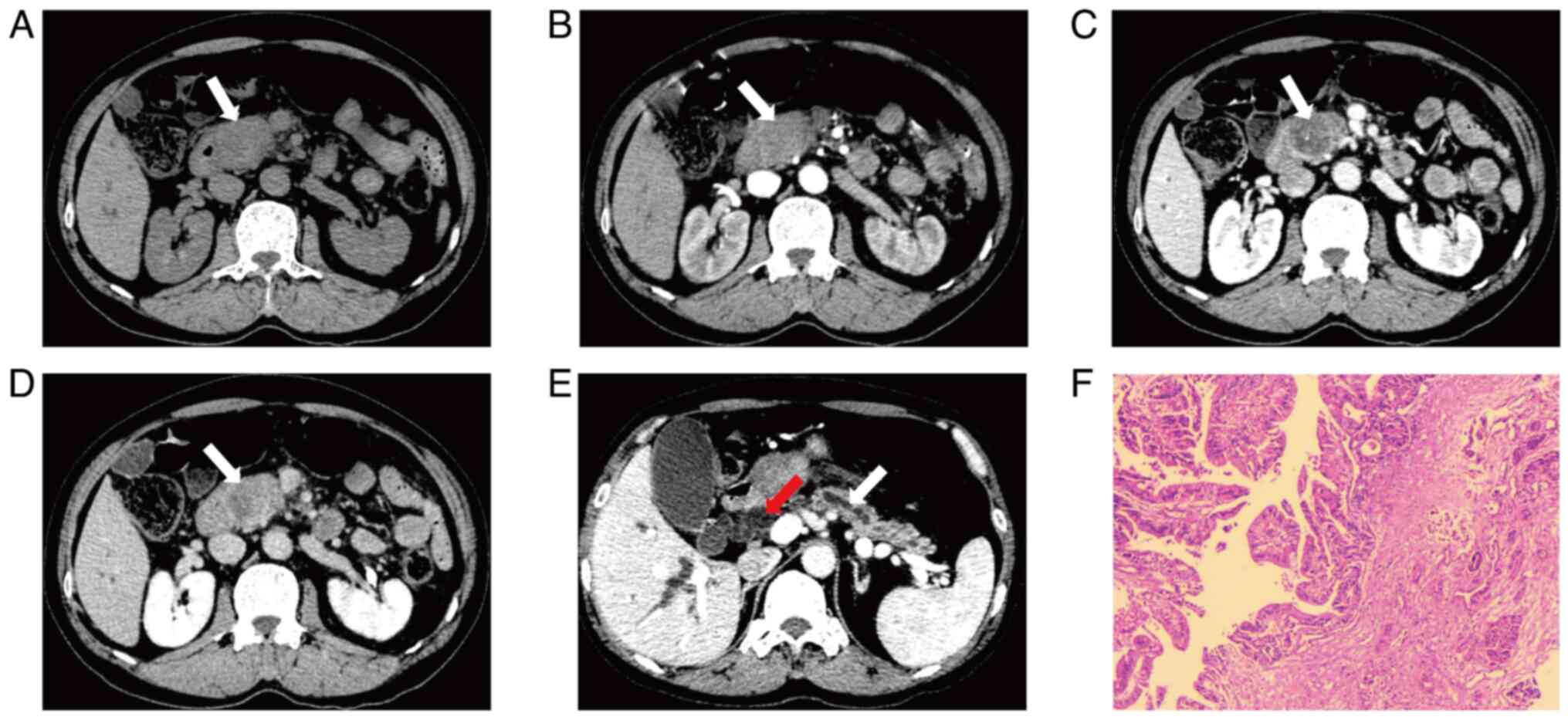
Wang FB, Ni JM, Zhang ZY, Zhang L, Wu WJ,
Wang D, Ji Y and Gong L: Differential diagnosis of periampullary
carcinomas: Comparison of CT with negative-contrast CT
cholangiopancreatography versus MRI with MR
cholangiopancreatography. Abdom Imaging. 39:506–517. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Li B, Zhang L, Zhang ZY, Ni JM, Lu FQ, Wu
WJ and Jiang CJ: Differentiation of noncalculous periampullary
obstruction: Comparison of CT with negative-contrast CT
cholangiopancreatography versus MRI with MR
cholangiopancreatography. Eur Radiol. 25:391–401. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Zhao DZ, Guo Y, Sun YP, Liu HM, Zhang Z,
Ma QL, Wang YS and Chen CL: Multi-detector spiral CT diagnosis of
common bile duct ampullary carcinoma. Eur Rev Med Pharmacol Sci.
21:3549–3553. 2017.PubMed/NCBI
|
|
93
|
Jang SK, Kim JH, Joo I, Jeon JH, Shin KS,
Han JK and Choi BI: Differential diagnosis of pancreatic cancer
from other solid tumours arising from the periampullary area on
MDCT. Eur Radiol. 25:2880–2888. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Angthong W, Jiarakoop K and Tangtiang K:
Differentiation of benign and malignant ampullary obstruction by
multi-row detector CT. Jpn J Radiol. 36:477–488. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Lee JE, Choi SY, Lee MH, Lim S, Min JH,
Hwang JA, Lee S and Kim JH: Differentiating between benign and
malignant ampullary strictures: A prediction model using a nomogram
based on CT imaging and clinical findings. Eur Radiol.
32:7566–7577. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Lambin P, Leijenaar RTH, Deist TM,
Peerlings J, De Jong EEC, Van Timmeren J, Sanduleanu S, Larue RTHM,
Even AJG, Jochems A, et al: Radiomics: The bridge between medical
imaging and personalized medicine. Nat Rev Clin Oncol. 14:749–762.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Lim CY, Min JH, Hwang JA, Choi SY and Ko
SE: Assessment of main pancreatic duct cutoff with dilatation, but
without visible pancreatic focal lesion on MDCT: A novel diagnostic
approach for malignant stricture using a CT-based nomogram. Eur
Radiol. 32:8285–8295. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Jang SY, Kim JS, Baek SY, Lee HA and Lee
JK: Proposed nomogram predicting neoplastic ampullary obstruction
in patients with a suspected ampulla of Vater lesion on CT. Abdom
Radiol (NY). 46:3128–3138. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Lu J, Hu D, Tang H, Hu X, Shen Y, Li Z,
Peng Y and Kamel I: Assessment of tumor heterogeneity:
Differentiation of periampullary neoplasms based on CT whole-lesion
histogram analysis. Eur J Radiol. 115:1–9. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Radojkovic M, Stojanovic M, Radojković D,
Jeremic L, Mihailovic D and Ilic I: Histopathologic differentiation
as a prognostic factor in patients with carcinoma of the
hepatopancreatic ampulla of Vater. J Int Med Res. 46:4634–4639.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Zimmermann C, Wolk S, Aust DE, Meier F,
Saeger HD, Ehehalt F, Weitz J, Welsch T and Distler M: The
pathohistological subtype strongly predicts survival in patients
with ampullary carcinoma. Sci Rep. 9:126762019. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
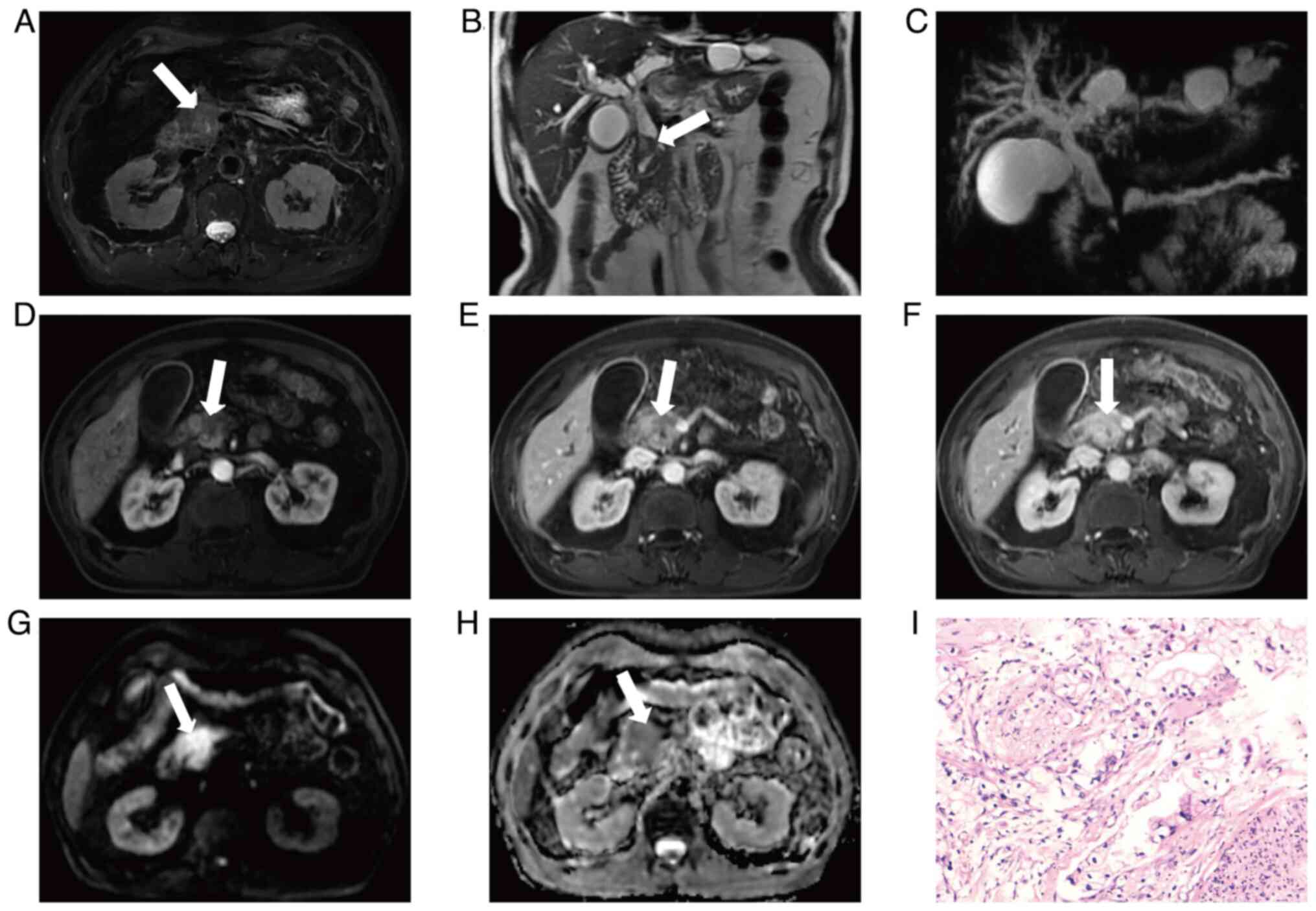
Ivanovic AM, Alessandrino F, Maksimovic R,
Micev M, Ostojic S, Gore RM and Mortele KJ: Pathologic subtypes of
ampullary adenocarcinoma: Value of ampullary MDCT for noninvasive
preoperative differentiation. AJR Am J Roentgenol. 208:W71–W78.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Bi L, Yang L, Ma J, Cai S, Li L, Huang C,
Xu J, Wang X and Huang M: Dynamic contract-enhanced CT-based
radiomics for differentiation of pancreatobiliary-type and
intestinal-type periampullary carcinomas. Clin Radiol. 77:e75–e83.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Chen WX, Xie QG, Zhang WF, Zhang X, Hu TT,
Xu P and Gu ZY: Multiple imaging techniques in the diagnosis of
ampullary carcinoma. Hepatobiliary Pancreat Dis Int. 7:649–653.
2008.PubMed/NCBI
|
|
105
|
Bi L, Dong Y, Jing C, Wu Q, Xiu J, Cai S,
Huang Z, Zhang J, Han X, Liu Q and Lv S: Differentiation of
pancreatobiliary-type from intestinal-type periampullary carcinomas
using 3.0T MRI. J Magn Reson Imaging. 43:877–886. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Nalbant MO, Inci E, Akinci O, Aygan S,
Gulturk U and Boluk Gulsever A: Evaluation of imaging findings of
pancreatobiliary and intestinal type periampullary carcinomas with
3.0T MRI. Acad Radiol. 30:1846–1855. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Dillman JR, Patel RM, Lin TK, Towbin AJ
and Trout AT: Diagnostic performance of magnetic resonance
cholangiopancreatography (MRCP) versus endoscopic retrograde
cholangiopancreatography (ERCP) in the pediatric population: A
clinical effectiveness study. Abdom Radiol (NY). 44:2377–2383.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Park MS, Kim TK, Kim KW, Park SW, Lee JK,
Kim JS, Lee JH, Kim KA, Kim AY, Kim PN, et al: Differentiation of
extrahepatic bile duct cholangiocarcinoma from benign stricture:
Findings at MRCP versus ERCP. Radiology. 233:234–240. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Suthar M, Purohit S, Bhargav V and Goyal
P: Role of MRCP in differentiation of benign and malignant causes
of biliary obstruction. J Clin Diagn Res. 9:TC08–TC012.
2015.PubMed/NCBI
|
|
110
|
Wang GX, Ge XD, Zhang D, Chen HL, Zhang QC
and Wen L: MRCP combined with CT promotes the differentiation of
benign and malignant distal bile duct strictures. Front Oncol.
11:6838692021. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Wu DS, Chen WX, Wang XD, Acharya R and
Jiang XH: Pancreaticobiliary duct changes of periampullary
carcinomas: Quantitative analysis at MR imaging. Eur J Radiol.
81:2112–2117. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Zhang L, Sanagapalli S and Stoita A:
Challenges in diagnosis of pancreatic cancer. World J
Gastroenterol. 24:2047–2060. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Wang S, Liu X and Zhao J, Liu Y, Liu S,
Liu Y and Zhao J: Computer auxiliary diagnosis technique of
detecting cholangiocarcinoma based on medical imaging: A review.
Comput Methods Programs Biomed. 208:1062652021. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Dusunceli Atman E, Erden A, Ustuner E,
Uzun C and Bektas M: MRI findings of intrinsic and extrinsic
duodenal abnormalities and variations. Korean J Radiol.
16:1240–1252. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Kim JH, Kim MJ, Chung JJ, Lee WJ, Yoo HS
and Lee JT: Differential diagnosis of periampullary carcinomas at
MR imaging. Radiographics. 22:1335–1352. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Baiu I and Visser B: Endoscopic retrograde
cholangiopancreatography. JAMA. 320:20502018. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Nakagawa K, Sho M, Fujishiro M, Kakushima
N, Horimatsu T, Okada KI, Iguchi M, Uraoka T, Kato M, Yamamoto Y,
et al: Clinical practice guidelines for duodenal cancer 2021. J
Gastroenterol. 57:927–941. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Yamamoto K, Itoi T, Sofuni A, Tsuchiya T,
Tanaka R, Tonozuka R, Honjo M, Mukai S, Fujita M, Asai Y, et al:
Expanding the indication of endoscopic papillectomy for T1a
ampullary carcinoma. Dig Endosc. 31:188–196. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Hanada K, Shimizu A, Kurihara K, Ikeda M,
Yamamoto T, Okuda Y and Tazuma S: Endoscopic approach in the
diagnosis of high-grade pancreatic intraepithelial neoplasia. Dig
Endosc. 34:927–937. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Ergul N, Gundogan C, Tozlu M, Toprak H,
Kadıoglu H, Aydin M and Cermik TF: Role of (18)F-fluorodeoxyglucose
positron emission tomography/computed tomography in diagnosis and
management of pancreatic cancer; comparison with multidetector row
computed tomography, magnetic resonance imaging and endoscopic
ultrasonography. Rev Esp Med Nucl Imagen Mol. 33:159–164.
2014.PubMed/NCBI
|
|
121
|
Yeh R, Dercle L, Garg I, Wang ZJ, Hough DM
and Goenka AH: The role of 18F-FDG PET/CT and PET/MRI in pancreatic
ductal adenocarcinoma. Abdom Radiol (NY). 43:415–434. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Pu Y, Wang C, Zhao S, Xie R, Zhao L, Li K,
Yang C, Zhang R, Tian Y, Tan L, et al: The clinical application of
18F-FDG PET/CT in pancreatic cancer: A narrative review.
Transl Cancer Res. 10:3560–3575. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Wolske KM, Ponnatapura J, Kolokythas O,
Burke LMB, Tappouni R and Lalwani N: Chronic pancreatitis or
pancreatic tumor? A problem-solving approach. Radiographics.
39:1965–1982. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Krishnaraju VS, Kumar R, Mittal BR, Sharma
V, Singh H, Nada R, Bal A, Rohilla M, Singh H and Rana SS:
Differentiating benign and malignant pancreatic masses: Ga-68 PSMA
PET/CT as a new diagnostic avenue. Eur Radiol. 31:2199–2208. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Ruan Z, Jiao J, Min D, Qu J, Li J, Chen J,
Li Q and Wang C: Multi-modality imaging features distinguish
pancreatic carcinoma from mass-forming chronic pancreatitis of the
pancreatic head. Oncol Lett. 15:9735–9744. 2018.PubMed/NCBI
|
|
126
|
Gnanasegaran G, Agrawal K and Wan S:
18F-Fluorodeoxyglucose-PET-computerized tomography and
non-fluorodeoxyglucose PET-computerized tomography in hepatobiliary
and pancreatic malignancies. PET Clin. 17:369–388. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Michalski CW, Liu B, Heckler M, Roth S,
Sun H, Heger U, Büchler MW and Hackert T: Underutilization of
surgery in periampullary cancer treatment. J Gastrointest Surg.
23:959–965. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Zhang JZ, Yang CX, Gao S, Bu JF, Li QQ,
Wang HL, Yang KN, Tong SS, Qian LJ, Zhang J, et al:
Three-dimensional visualization and evaluation of hilar
cholangiocarcinoma resectability and proposal of a new
classification. World J Surg Oncol. 21:2392023. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Lin C, Gao J, Zheng H, Zhao J, Yang H, Lin
G, Li H, Pan H, Liao Q and Zhao Y: Three-dimensional visualization
technology used in pancreatic surgery: A valuable tool for surgical
trainees. J Gastrointest Surg. 24:866–873. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Rozenblatt-Rosen O, Regev A, Oberdoerffer
P, Nawy T, Hupalowska A, Rood JE, Ashenberg O, Cerami E, Coffey RJ,
Demir E, et al: The human tumor atlas network: Charting tumor
transitions across space and time at single-cell resolution. Cell.
181:236–249. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Fang C, An J, Bruno A, Cai X, Fan J,
Fujimoto J, Golfieri R, Hao X, Jiang H, Jiao LR, et al: Consensus
recommendations of three-dimensional visualization for diagnosis
and management of liver diseases. Hepatol Int. 14:437–453. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Higuchi K, Kaise M, Noda H, Kirita K,
Koizumi E, Umeda T, Akimoto T, Omori J, Akimoto N, Goto O, et al:
Three-dimensional visualization improves the endoscopic diagnosis
of superficial gastric neoplasia. BMC Gastroenterol. 21:2422021.
View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Ahmed TM, Rowe SP, Fishman EK, Soyer P and
Chu LC: Three-dimensional CT cinematic rendering of adrenal masses:
Role in tumor analysis and management. Diagn Interv Imaging.
105:5–14. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Almagro J, Messal HA, Zaw Thin M, van
Rheenen J and Behrens A: Tissue clearing to examine tumour
complexity in three dimensions. Nat Rev Cancer. 21:718–730. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Kang SH, Won Y, Lee K, Youn SI, Min SH,
Park YS, Ahn SH and Kim HH: Three-dimensional (3D) visualization
provides better outcome than two-dimensional (2D) visualization in
single-port laparoscopic distal gastrectomy: A propensity-matched
analysis. Langenbecks Arch Surg. 406:473–478. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Jang W, Song JS, Kim SH and Yang JD:
Comparison of compressed sensing and gradient and spin-echo in
breath-hold 3D MR cholangiopancreatography: Qualitative and
quantitative analysis. Diagnostics (Basel). 11:6342021. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Chen Z, Xue Y, Wu Y, Duan Q, Zheng E, He
Y, Li G, Song Y and Sun B: Feasibility of 3D breath-hold MR
cholangiopancreatography with a spatially selective radiofrequency
excitation pulse: Prospective comparison with parallel imaging
technique and compressed sensing method. Acad Radiol. 29:e289–e295.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Huber T, Huettl F, Tripke V, Baumgart J
and Lang H: Experiences with three-dimensional printing in complex
liver surgery. Ann Surg. 273:e26–e27. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Yang J, Fang CH, Fan YF, Xiang N, Liu J,
Zhu W, Bao SS and Wang HZ: To assess the benefits of medical image
three-dimensional visualization system assisted
pancreaticoduodenctomy for patients with hepatic artery variance.
Int J Med Robot. 10:410–417. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Miyamoto R, Oshiro Y, Nakayama K and
Ohkohchi N: Impact of three-dimensional surgical simulation on
pancreatic surgery. Gastrointest Tumors. 4:84–89. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Miyamoto R, Oshiro Y, Sano N, Inagawa S
and Ohkohchi N: Three-dimensional remnant pancreatic volumetry
predicts postoperative pancreatic fistula in pancreatic cancer
patients after pancreaticoduodenectomy. Gastrointest Tumors.
5:90–99. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Javed AA, Young RWC, Habib JR,
Kinny-Köster B, Cohen SM, Fishman EK and Wolfgang CL: Cinematic
rendering: Novel tool for improving pancreatic cancer surgical
planning. Curr Probl Diagn Radiol. 51:878–883. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Barat M, Pellat A, Terris B, Dohan A,
Coriat R, Fishman EK, Rowe SP, Chu L and Soyer P: Cinematic
rendering of gastrointestinal stromal tumours: A review of current
possibilities and future developments. Can Assoc Radiol J.
75:359–368. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Cai W, Fan Y, Hu H, Xiang N, Fang C and
Jia F: Postoperative liver volume was accurately predicted by a
medical image three dimensional visualization system in hepatectomy
for liver cancer. Surg Oncol. 26:188–194. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Mise Y, Hasegawa K and Kokudo N: Response
to Comment on ‘the virtual hepatectomy changed the practice of
liver surgery: More details, more significance’. Ann Surg.
270:e332019. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Allan A, Kealley C, Squelch A, Wong YH,
Yeong CH and Sun Z: Patient-specific 3D printed model of biliary
ducts with congenital cyst. Quant Imaging Med Surg. 9:86–93. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Bati AH, Guler E, Ozer MA, Govsa F,
Erozkan K, Vatansever S, Ersin MS, Elmas ZN and Harman M: Surgical
planning with patient-specific three-dimensional printed
pancreaticobiliary disease models-cross-sectional study. Int J
Surg. 80:175–183. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Mise Y, Hasegawa K, Satou S, Shindoh J,
Miki K, Akamatsu N, Arita J, Kaneko J, Sakamoto Y and Kokudo N: How
has virtual hepatectomy changed the practice of liver surgery?:
Experience of 1194 virtual hepatectomy before liver resection and
living donor liver transplantation. Ann Surg. 268:127–133. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Uchida M: Recent advances in 3D computed
tomography techniques for simulation and navigation in
hepatobiliary pancreatic surgery. J Hepatobiliary Pancreat Sci.
21:239–245. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Liu Y, Wang Q, Du B, Wang X, Xue Q and Gao
W: A meta-analysis of the three-dimensional reconstruction
visualization technology for hepatectomy. Asian J Surg. 46:669–676.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Zhang J, Guo X, Wang H, Zhang J, Liu P,
Qiao Q and Wang X: The application of three-dimensional
visualization in preoperative evaluation of portal vein invasion in
hilar cholangiocarcinoma. Cancer Manag Res. 12:9297–9302. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Guo Q, Chen J, Pu T, Zhao Y, Xie K, Geng X
and Liu F: The value of three-dimensional visualization techniques
in hepatectomy for complicated hepatolithiasis: A propensity score
matching study. Asian J Surg. 46:767–773. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Zhao D, Lau WY, Zhou W, Yang J, Xiang N,
Zeng N, Liu J, Zhu W and Fang C: Impact of three-dimensional
visualization technology on surgical strategies in complex hepatic
cancer. Biosci Trends. 12:476–483. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Song JS, Kim SH, Kuehn B and Paek MY:
Optimized breath-hold compressed-sensing 3D MR
cholangiopancreatography at 3T: Image quality analysis and clinical
feasibility assessment. Diagnostics (Basel). 10:3762020. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Swaraj S, Mohapatra M, Sathpathy G,
Yalamanchi R, Sen K, Menon SM, Madhesia A, Kumaraswamy SM, Radha
Krishna K and Bobde DV: Diagnostic performance of ultrasonography
versus magnetic resonance cholangiopancreatography in biliary
obstruction. Cureus. 15:e339152023.PubMed/NCBI
|
|
156
|
Reddy S CT, Mohan VSK, Jeepalem SM,
Manthri R, Kalawat T, Reddy V V, Hulikal N and Devi B VL: Utility
of 18F-FDG PET/CT in management of pancreatic and periampullary
masses-prospective study from a tertiary care center. Indian J Surg
Oncol. 13:288–298. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Wen G, Gu J, Zhou W, Wang L, Tian Y, Dong
Y, Fu L and Wu H: Benefits of 18F-FDG PET/CT for the
preoperative characterisation or staging of disease in the
ampullary and duodenal papillary. Eur Radiol. 30:5089–5098. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Deng S, Luo J, Ouyang Y, Xie J, He Z,
Huang B, Bai F, Xiao K, Yin B, Wang J, et al: Application analysis
of omental flap isolation and modified pancreaticojejunostomy in
pancreaticoduodenectomy (175 cases). BMC Surg. 22:1272022.
View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Gugenheim J, Crovetto A and Petrucciani N:
Neoadjuvant therapy for pancreatic cancer. Updates Surg. 74:35–42.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Meijer LL, Alberga AJ, de Bakker JK, van
der Vliet HJ, Le Large TYS, van Grieken NCT, de Vries R, Daams F,
Zonderhuis BM and Kazemier G: Outcomes and treatment options for
duodenal adenocarcinoma: A systematic review and meta-analysis. Ann
Surg Oncol. 25:2681–2692. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Gössling GCL, Zhen DB, Pillarisetty VG and
Chiorean EG: Combination immunotherapy for pancreatic cancer:
Challenges and future considerations. Expert Rev Clin Immunol.
18:1173–1186. 2022. View Article : Google Scholar : PubMed/NCBI
|