Introduction
Malignant tumors of the smooth muscle can occur
anywhere in the body, particularly with higher frequency in the
gastrointestinal tract and in the uterus. In the genitourinary
tract, this type of tumor affects the kidney more commonly than the
ureter. Leiomyosarcoma of the ureter is an extremely rare neoplasm;
in fact, ~95% of ureteral tumors are primitive epithelial tumors,
which are generally transitional cell carcinomas. In
non-transitional cell carcinoma, the most common type is squamous
cell carcinoma (0.7–7%) and adenocarcinoma (1%). Sarcomas are
rapidly growing tumors, with the ability to invade the adjacent
structures. In the case of leiomyosarcomas, early metastasis to the
mesentery, lungs, liver and regional lymph nodes are common
(1–4). Generally, these tumors don't cause
hematuria due to the lack of involvement of the ureteral mucosa
(5,6) while, in 2/3 of cases, the typical sign
is the ureteric obstruction. With regard to leiomyosarcoma of the
ureter, a limited number of reports have been reported in the
literature. The first case of a leiomyosarcoma arising in the
genitourinary tract (exactly in the renal pelvis) was reported by
Ribbert in 1886 in a 4-year-old girl (7). To the best of our knowledge, from 1886
until 2022, only 13 cases of primary leiomyosarcoma have been
described as reported in Table I
(8–19). In particular, in the case reported
by John E. Kraus, metastasis to the pituitary gland from
leiomyosarcoma of the ureter is shown (9). In the present study, the clinical
features, histological details, imaging and treatment of ureteral
leiomyosarcoma were reported in a 59-year-old female patient;
moreover, a systematic review of the literature was performed.
 | Table I.PubMed search for previous
publications of primary leiomyosarcoma of the ureter in humans from
1886. |
Table I.
PubMed search for previous
publications of primary leiomyosarcoma of the ureter in humans from
1886.
| First author/s,
year | Number of cases | Sex of patient | Ethnicity of
patient | Patient age,
years | Site of
malignancy | (Refs.) |
|---|
| Ribbert, 1886 | 1 | Female | Caucasian | 4 | Renal pelvis | (7) |
| Rademaker, 1943 | 1 | Female | Caucasian | 59 | Ureter | (8) |
| Rossien and Russel,
1946 | 1 | Female | Caucasian | 55 | Ureter | (10) |
| Alznauer, 1955 | 1 | Female | Caucasian | 60 | Ureter | (11) |
| Werner et al,
1959 | 1 | Female | Caucasian | 60 | Ureter | (12) |
| Rushton et al,
1983 | 1 | Female | African-American | 53 | Ureter | (13) |
| Márquez-Moreno et
al, 2003 | 1 | Female | Caucasian
(Spanish) | 38 | Ureter (pelvic
tract) | (14) |
| Shirotake et
al, 2006 | 1 | Female | Caucasian
(Japanese) | 60 | Ureter | (15) |
| Lv et al,
2008 | 1 | Female | Caucasian
(Japanese) | Middle aged | Ureter | (16) |
| Aubert et al,
2012 | 1 | Female | Caucasian | 57 | Ureter | (17) |
| Aboutaleb et
al, 2022 | 1 | Male | Pakistani | 57 | Ureter | (18) |
| Gan et al,
2022 | 1 | Male | Caucasian | 59 | Ureter | (19) |
Case report
A 59-year-old Caucasian woman presented to our
hospital (Umberto I Hospital in Nocera Inferiore) with an acute
pain in the right lumbar fossa. The patient exhibited a functional
single kidney, due to left renal atrophy for a long-standing
stenosis of the pyeloureteric joint. With the exception of this
condition and hypertension (under medical therapy), the patient was
in excellent clinical condition (with a history of previous surgery
of cholecystectomy); furthermore, she was not a smoker. In the
emergency room the functional tests indicated acute renal failure,
with an important increase in the creatinine and urea blood levels
(creatinine: 3,9 mg/dl; urea: 95 mg/dl). Ultrasound examination
indicated moderate right hydronephrosis [transverse diameter (DT)
of renal pelvis: 30 mm]. Due to this reason, the patient underwent
right percutaneous nephrostomy placement under local anesthesia, in
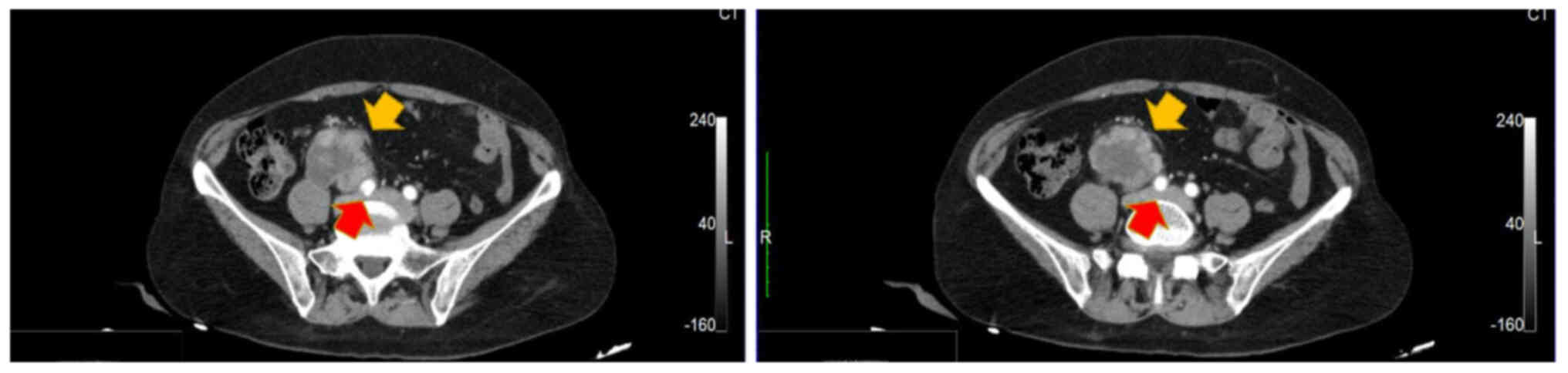
order to improve the kidney function. Computed tomography (CT) of
the abdomen and pelvis (Fig. 1)
indicated the presence of a voluminous formation, with polylobed
margins, with maximum axial dimensions of 45×52 mm (dAP × dT), with
a cranio-caudal extension of 46 mm, with a peripheral rim featuring
intense post-contrastographic impregnation and a hypodense central
core, as per necrotic-colliquative phenomena; this formation
appeared inseparable from the right ureter in its mid-distal
section and indicated a cleavage plane posteriorly with the
anterior margin of the psoas muscle and with the right common iliac
artery. The appearance of the bladder was normal. Therefore, the
diagnosis was performed between the following two pathological
entities: retroperitoneal adenomegaly extrinsically compressing the
ureter or an urothelial tumor developing extrinsically. Cystoscopy
indicated lack of abnormality; diagnostic ureteroscopy revealed a
narrowing of the lumen of the ureter, without any mass noted in the
ureteric lumen. Ureteric washings were inconclusive due to
insufficient number of cells. Therefore, under general anesthesia
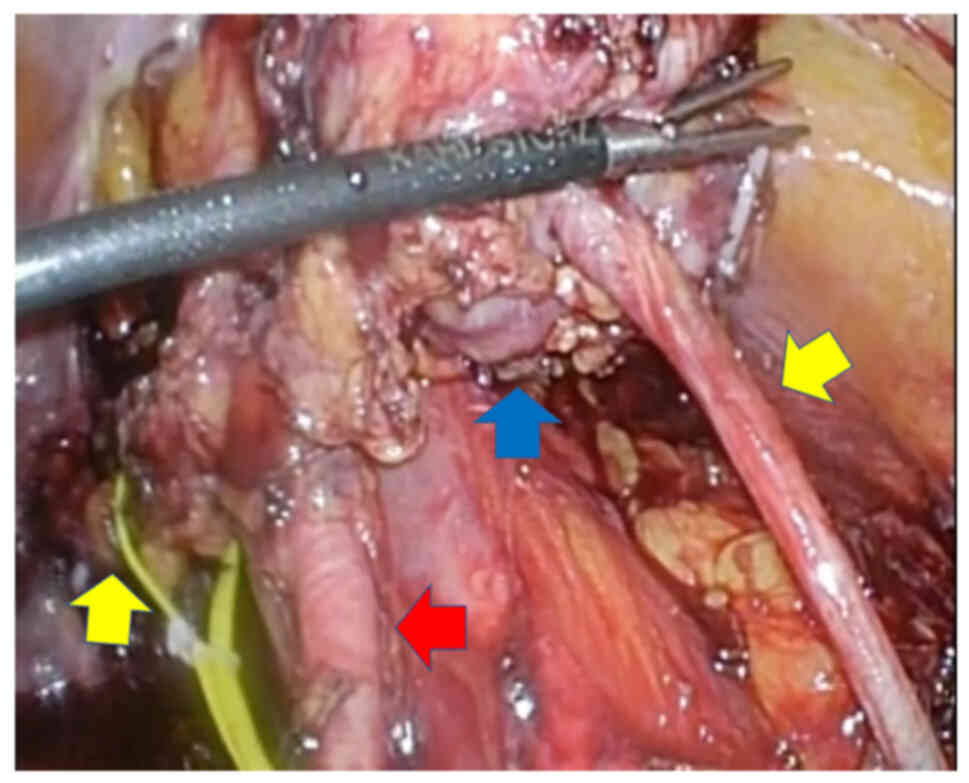
in the lithotomy position, an arrangement of trocars similar to
that used during radical prostatectomy was achieved with
transperitoneal access; based on this arrangement, a mass was
identified which incorporated the portion of the ureter at the
junction with the iliac vessels resembling a ‘sleeve’. A blunt
dissection released the tumor from the right common iliac vessel
(Fig. 2), due to the presence of a
definite line of cleavage between the mass and the common right
iliac vessel. Therefore, this tumor was resected with a safety
margin of 1 cm. Subsequently, an optimal ureteric length was
mobilized and a tension free end-to-end anastomosis between the two
stumps of the ureter was performed without complication. In the
same session of the surgery, a double J stent 7 Fr/24 cm was placed
retrogradely. The patient was discharged following 5 days
post-surgery and during the recovery she underwent medical therapy
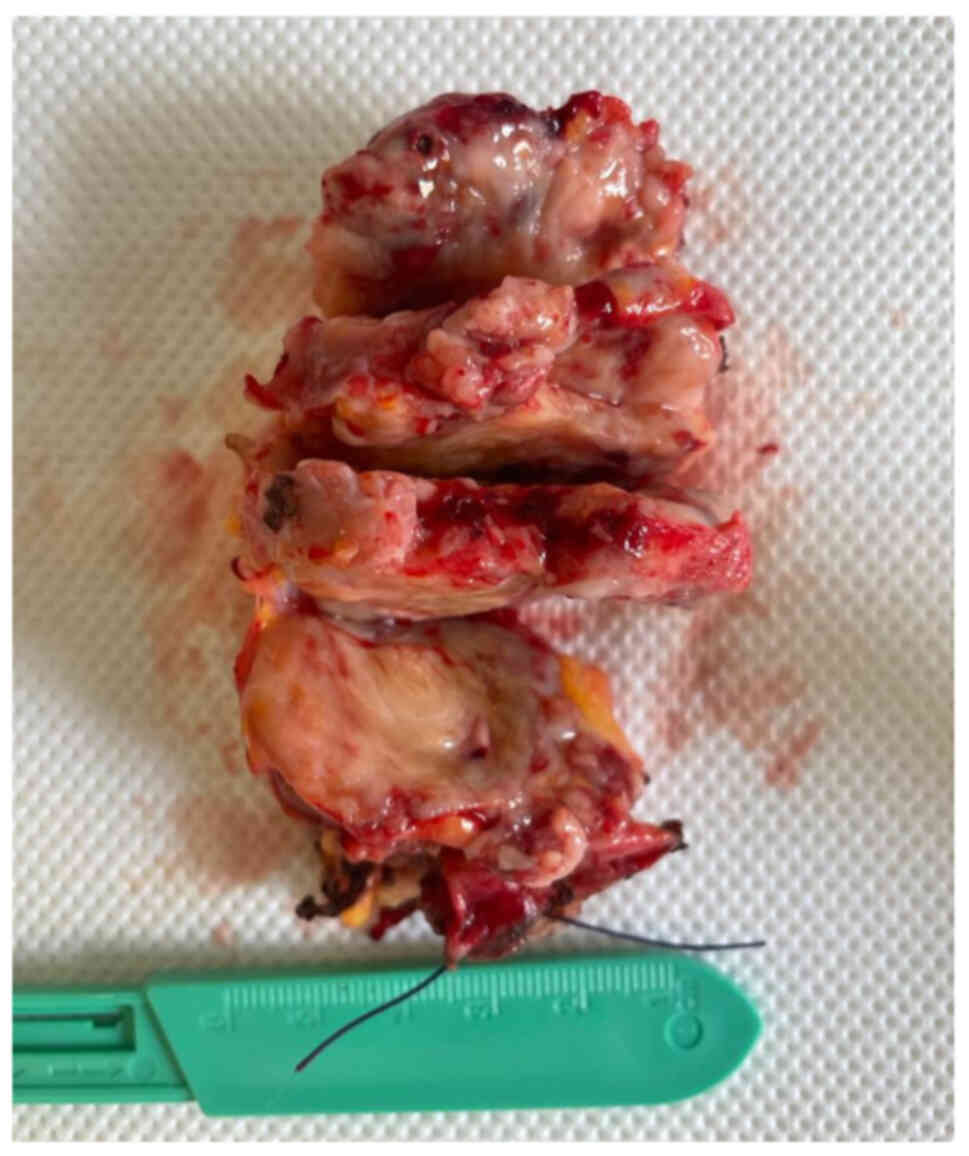
with ceftriaxone. At pathologic examination a diagnosis of a
high-grade leiomyosarcoma of the right ureteral wall, extensively
infiltrating the peri-ureteral tissues and the ureter itself (2017
UICC classification: pT2a) was made (Fig. 3), with a strong staining for smooth
muscle actin (SMA) at immunohistochemistry (Actin+, S100-, CK-,
CD117-, HMB45-). The cutting margins of the ureter were negative.
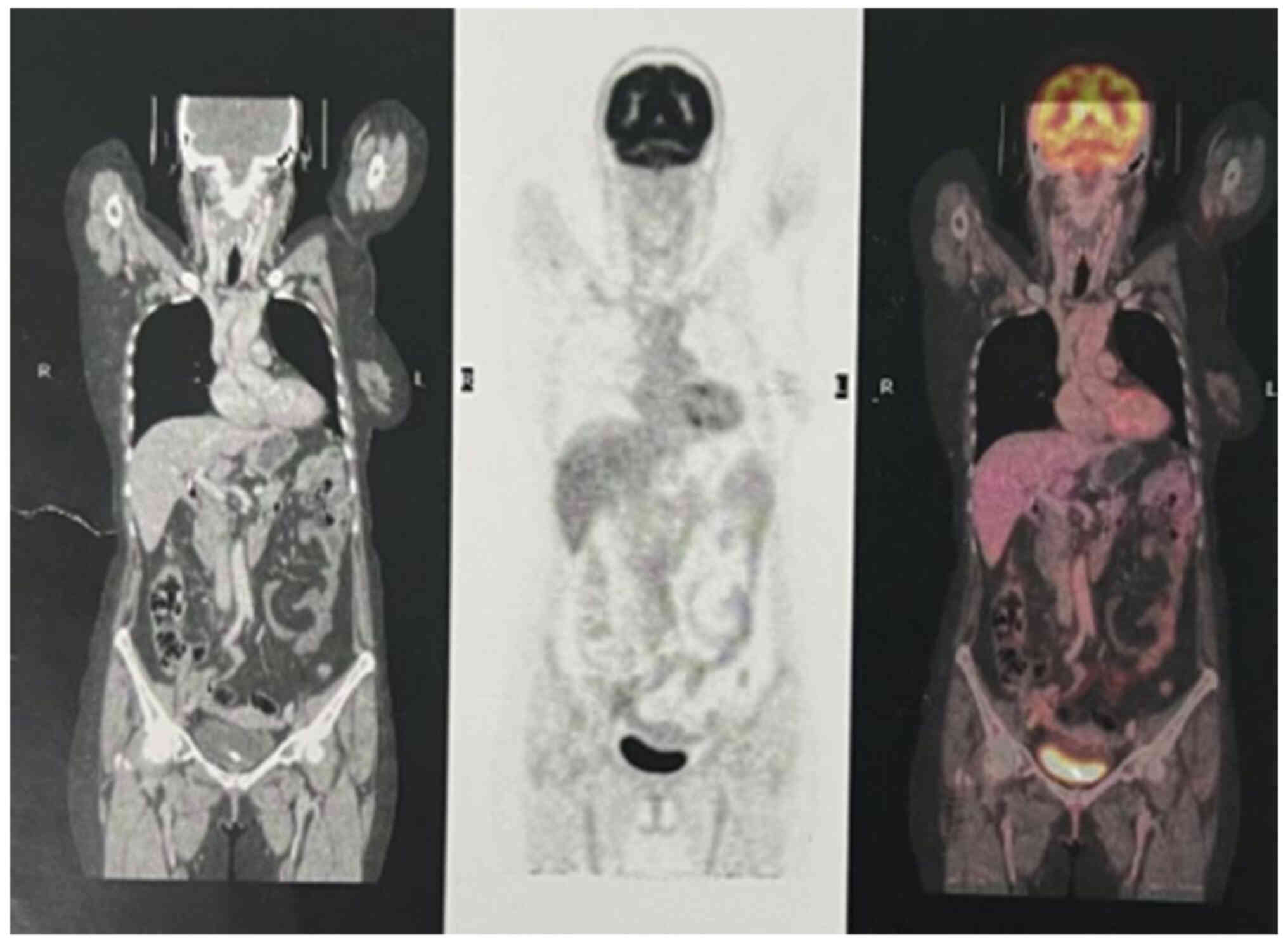
Following surgery, adjuvant chemotherapy was performed although the
positron emission tomography CT scan did not demonstrate distant
metastasis (Fig. 4). The patient
did not exhibit recurrence at 3, 6 and 9 months following the CT
scan examination. After the operation, the renal function was
normal and, at the removal of DJ PV stent, the patient didn't
suffer from stenosis of uretero-ureteral anastomosis which is a
complication of this type of surgery. Almost 2 years have passed
since the operation and the follow-up program shows no signs of
recovery of the disease.
Discussion
Leiomyosarcoma is a rare and highly malignant tumor,
accounting for 10–20% of soft-tissue sarcomas; its incidence is
generally noted in middle-age subjects; women are affected by this
neoplasm more commonly than men (16). The prognosis is extremely poor
(2,15–17,20,21)
due to the frequent tendency to develop secondary localizations,
which may already be present at diagnosis or appear at a subsequent
time. The mesentery, lung, liver and lymphatic vessels are
generally affected as the main areas of metastasis (2). To the best of our knowledge, a
literature review (performed with a PubMed search) has revealed
only 13 cases of primary leiomyosarcoma of the ureter from 1886 to
2022. Generally, the majority of the tumors arising from the ureter
are transitional cell carcinomas (17), with smooth muscle tumors being more
common in tumors of the bladder and kidney. No clinical pattern has
been associated with ureter leiomyosarcoma; however, patients
generally complain of flank or abdominal pain, urinary tract
infection and obstructive uropathy (22). As with the present case report,
diagnosis is based on the anatomopathological analysis with
immunohistochemical markers. The mass may be visualized on
ultrasound and has been described as cystic (3). Ureter leiomyosarcoma lacks a
characteristic enhancement pattern on the CT scan adequate to
derive a diagnosis (17), probably
due to the low number of cases studied. In general, this type of
tumor is derived from the wall of the ureter, which develops as
eccentric or circumferential parietal thickening (23). In the present case, a nodular mass
of the wall of the ureter was developing exophytically with ‘crown’
enhancement (a hypodense centre and highly enhanced periphery); the
hypodensity of the centre of the lesion is caused by necrosis
phenomena which are more visible depending on the voluminous nature
of the neoplastic mass and/or the higher degree of malignancy
(24). However, when a
retroperitoneal nodular mass is discovered, which is in contact
with the ureter, several diagnostic hypotheses must be
investigated. First of all, due to its frequency, a diagnosis of
urothelial carcinoma must be excluded, especially in case of
haematuria (25); however, the
patient did not exhibit this sign, directing clinical suspicion
towards other pathologies. Furthermore, in the case of urothelial
carcinoma, the lesions are readily multifocal and with synchronous
involvement of the bladder in ~40% of cases (23,25,26).
In the present case report, the lesion was single and the bladder
was free from any alteration. Furthermore, in lymphoproliferative
disease, secondary localization of a urogenital cancer or an
infection (tuberculosis) must also be excluded when the diagnosis
of leiomyosarcoma is suspected. In patients suffering from
lymphoproliferative disease, adenomegalies indicate the following
characteristic aspect: they are generally multiple, perivascular
and confluent (in the absence of contrastographic impregnation); in
the present case report, the clinical context will suggest the
diagnosis. In a patient suffering from tuberculosis the
adenopathies could mime the aspect discussed in the lesion noted in
the present study since they are much smaller than lymphomas and
poorly confluent; furthermore, following injection of the contrast
medium, the centre of these adenopathies is hypodense while the
peripheral contours indicate contrastographic enhancement (24). The analysis of the contact angles
may aid the differential diagnosis; in effect, the contact angles
are obtuse in the case of leiomyosarcoma, while they are acute when
an extrinsic site of the adenomegaly type compresses the ureter.
However, this is theoretical and in practice it is often difficult
to differentiate these two pathologies. However, patients of this
type may less commonly exhibit melanoma and lung cancer, which can
cause retroperitoneal metastases (24); therefore, their diagnosis must also
be excluded. A final pathology to consider is retroperitoneal
fibrosis which presents as an infiltration ‘sheathing’ the ureter,
usually medially, causing proximal (unilateral or bilateral)
hydronephrosis (24). In this case,
the clinical context is again a key element for the diagnosis.
Therefore, considering this abundance of pathologies, the
anatomopathological analysis of the mass following surgical
treatment (more specifically on the evaluation of the
immunohistochemical markers in the case of leiomyosarcoma of the
ureter) is mandatory for definitive diagnosis. Following
immunohistochemical analysis, leiomyosarcoma is negative with
regard to the expression levels of epithelial markers (cytokeratins
and epithelial membrane antigens) and positive for desmin and SMA
(indicating the smooth muscle origin of the tumor). Negative
expressions of myoglobin, cytokeratin and S-100 aid to rule out
rhabdomyosarcoma, sarcomatoid carcinoma and melanoma, respectively
(27,28). By noting the aggressive nature of
the condition, the choice of treatment has been reported as total
nephroureterectomy with en bloc resection of the tumor
(22,29). By contrast, certain cases have been
managed with tumor excision and ureteroureterostomy without signs
of recurrence, similar to those noted in the patient of the present
study. As noted in the present case, in the case by Kolhartkar
et al (29), the
nephroureterectomy was not performed because the tumor was derived
from the patient's only functioning kidney. Radiotherapy can be
considered for larger tumors and/or if the margins of the resection
are affected (16,21). Adjuvant chemotherapy (based on
doxorubicin, ifosfamide, gemcitabine and docetaxel) has not been
proven to be effective, having a role in the metastatic disease
(18). It is recommended that
adjuvant chemotherapy (based on Ifosfamide plus Epirubicin) should
be used in the patient of the present study hoping for an adequate
prognosis. Due to the rarity of the condition, the management is
not standardized and it is mainly based on modes of treatment of
epithelial tumors of the ureter. In the present case report,
surgical excision of the ureteric mass with safety margin was
performed.
Although leiomyosarcoma is rarely noted in the
urinary tract, it should be considered in the differential
diagnosis of ureteral stricture disease and tumors. For this
reason, it is important to report primary ureter leiomyosarcoma
cases to assist further studies investigating the condition and the
optimal approach to its treatment; in the present case report, no
malignant recurrence was observed 12 months following tumor
resection and uretero-ureterostomy.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study are included
in the figures and/or tables of this article.
Authors' contributions
RB was the major contributor in writing the
manuscript. RB and GM made substantial contributions to the
conception and design of the study. DF and RC assisted with imaging
acquisition. RB and GM confirm the authenticity of all the raw
data. RS, UDM, OI, TP, CB and GDL interpreted the patient data
regarding urological disease. All authors have read and approved
the final manuscript.
Ethics approval and consent to
participate
The present study was conducted according to the
guidelines of the Declaration of Helsinki. However, ethics approval
was not required because this was a case report that did not
include procedures outside of common and correct clinical practice.
Furthermore, the patient included in the study provided their
written informed consent for the processing of their medical
data.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present study and for processing
their medical data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Abeshouse BS: Primary benign and malignant
tumors of the ureter; a review of the literature and report of one
benign and twelve malignant tumors. Am J Surg. 91:237–271. 1956.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Griffin JH and Waters WB: Primary
leiomyosarcoma of the ureter. J Surg Oncol. 62:148–152. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Roemer CE, Pfister RC, Brodsky G and
Sacknoff EJ: Primary leiomyosarcoma of the ureter. Urology.
16:492–495. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Spiess PE, Leibovici D and Pisters LL:
PART X: Neoplasms of the upper urinary tract. Campbell-Walsh
Urology; 11th edition. pp. 1404–1412. 2016
|
|
5
|
Gislason T and Arnarson O: Primary
ureteral leiomyosarcoma. Scand J Urol Nephrol. 18:253–254. 1984.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mehraban D: Primary leiomyosarcoma of the
ureter. Med J Islam Repub Iran. 2:67–69. 1988.
|
|
7
|
Ribbert, . About an atriocellular
myosarcoma of the renal pelvis and the ureter. Virch Arch.
106:2821886.
|
|
8
|
Rademaker L: Primary sarcoma of the
ureter: Case report and review of the literature. Am J Surg.
62:402–406. 1943. View Article : Google Scholar
|
|
9
|
Kraus JE: Primary sarcoma of the ureter.
Urol Cutan Rev. 48:5221944.
|
|
10
|
Rossien AK and Russell TH: Leiomyosarcoma
involving the right ureter. Arch Pathol (Chic). 41:655–660.
1946.PubMed/NCBI
|
|
11
|
Alznauer RL: Leiomyosarcoma of right
ureter; report of a case. AMA Arch Pathol. 59:94–99.
1955.PubMed/NCBI
|
|
12
|
Werner JR, Klingensmith W and Denko JV:
Leiomyosarcoma of the ureter: Case report and review of literature.
J Urol. 82:68–71. 1959. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Rushton HG, Sens MA, Garvin AJ and Turner
WR Jr: Primary leiomyosarcoma of the ureter: A case report with
electron microscopy. J Urol. 129:1045–1046. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Márquez-Moreno AJ, Julve-Villalta E,
Corral-García P, Gutiérrez-Chacón P and Blanes-Berenguel A: Primary
ureteral leiomyosarcoma: A rare cause of obstructive uropathy. Arch
Esp Urol. 56:169–172. 2003.(In Spanish). PubMed/NCBI
|
|
15
|
Shirotake S, Sumitomo M, Asakuma J, Asano
T, Aiko S and Hayakawa M: A case of primary leiomyosarcoma of the
ureter. Hinyokika Kiyo. 52:41–45. 2006.(In Japanese). PubMed/NCBI
|
|
16
|
Lv C, Chen N, Zhu X, Zhang X and Zhong Z:
Primary leiomyosarcoma of the ureter. Asian J Surg. 31:191–194.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Aubert E, Millet I, Serre I and Taourel P:
Leiomyosarcoma of the ureter: A rare case. Diagn Interv Imaging.
93:60–63. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Aboutaleb HA, Khurana P and El-Shahat YM:
Primary leiomyosarcoma of the middle ureter: A rare case report
with literature review. Clin Case Rep. 10:e054092022. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gan C, Attwell-Heap A and Clarke A: Left
distal ureter leiomyosarcoma: A case report. J Surg Case Rep.
2022:rjac5012022.PubMed/NCBI
|
|
20
|
Tzen CY, Wu CJ, Huang ZD and Wu TY: Poorly
differentiated transitional cell carcinoma versus leiomyosarcoma of
the ureter: Different defects in tumour suppressor genes.
Histopathology. 51:271–273. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kasper B, Gil T and Awada A: Treatment of
patients with advanced soft tissue sarcoma: Disappointment or
challenge? Curr Opin Oncol. 19:336–340. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Madgar I, Goldwasser B, Czerniak A and
Many M: Leiomyosarcoma of the ureter. Eur Urol. 14:487–489. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Browne RF, Meehan CP, Colville J, Power R
and Torreggiani WC: Transitional cell carcinoma of the upper
urinary tract: Spectrum of imaging findings. Radiographics.
25:1609–1627. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Merran S, Karila-Cohen P and Vieillefond
A: Primary retroperitoneal tumors in adults. J Radiol. 85:252–264.
2004.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Delomez J, Claudon M, Darmaillacq C,
Hubert J and Lemaître L: Imaging of upper excretory tract tumors. J
Radiol. 83:825–838. 2002.(In French). PubMed/NCBI
|
|
26
|
Vikram R, Sandler CM and Ng CS: Imaging
and staging of transitional cell carcinoma: Part 2, upper urinary
tract. AJR Am J Roentgenol. 192:1488–1493. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Miettinen M: Antibody specific to muscle
actins in the diagnosis and classification of soft tissue tumors.
Am J Pathol. 130:205–215. 1988.PubMed/NCBI
|
|
28
|
Iwata J and Fletcher CD:
Immunohistochemical detection of cytokeratin and epithelial
membrane antigen in leiomyosarcoma: A systematic study of 100
cases. Pathol Int. 50:7–14. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kolhartkar RK, Kulkarni SH, Phansopkar MA
and Thomas C: Leimyosarcoma of ureter presenting as acute renal
failure. Br J Urol. 51:3261979. View Article : Google Scholar : PubMed/NCBI
|