|
1
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. 68:394–424. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
The Chinese standard of care for
colorectal cancer (2020 edition). Chin J Surg. 58:561–585.
2020.PubMed/NCBI
|
|
3
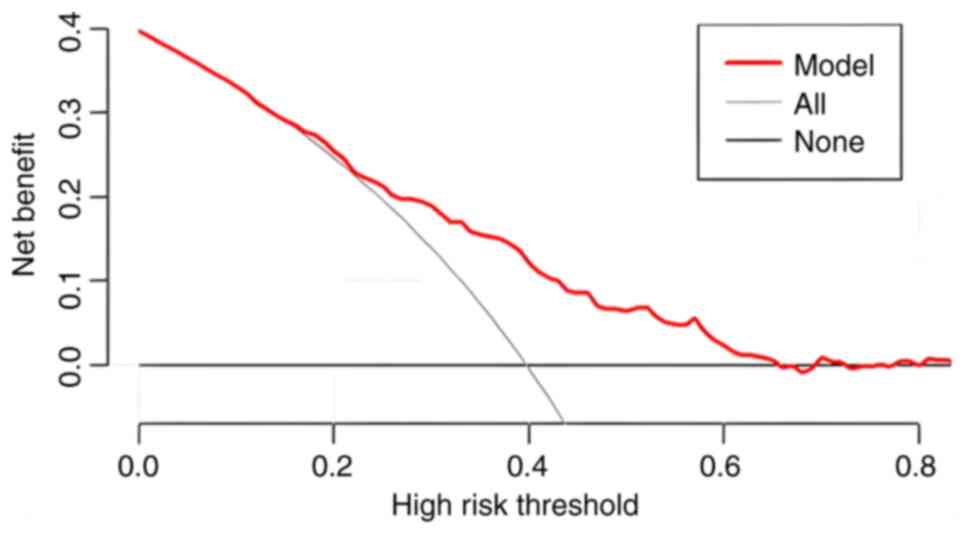
|
Hui YF, Li C and Guo TH: Colorectal
adenomas in TCM syndrome distribution laws and its clinical
intervention study. China's Basic Med J Traditional Chin Med.
29:1866–1870. 2023.(In Chinese).
|
|
4
|
Yu M, Liu XB, Zhou M, Zhu ZD, Pan JG and
WQ: Change trend of colorectal malignant tumors detected by
electronic colonoscopy from 2015 to 2020. J Clin Gastroenterol.
34:361–364. 2022.
|
|
5
|
Courtney RJ, Paul CL, Carey ML,
Sanson-Fisher RW, Macrae FA, D'Este C, Hill D, Barker D and Simmons
J: A population-based cross-sectional study of colorectal cancer
screening practices of first-degree relatives of colorectal cancer
patients. BMC Cancer. 13:132013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rex DK, Boland CR, Dominitz JA, Giardiello
FM, Johnson DA, Kaltenbach T, Levin TR, Lieberman D and Robertson
DJ: Colorectal cancer screening: Recommendations for physicians and
patients from the U.S. Multi-society task force on colorectal
cancer. Gastroenterology. 153:307–323. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bretthauer M, Kaminski MF, Løberg M,
Zauber AG, Regula J, Kuipers EJ, Hernán MA, McFadden E, Sunde A,
Kalager M, et al: Population-based colonoscopy screening for
colorectal cancer: A randomized clinical trial. JAMA Intern Med.
176:894–902. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Li P, Wang CJ and Chen GY: Consensus on
screening and diagnosis of early colorectal cancer and precancerous
lesions in China. Chin J Practical Internal Med. 35:211–227.
2015.(In Chinese). View Article : Google Scholar
|
|
9
|
Wu XL, Wang LK and Huang XT: A
retrospective study on the epidemiological characteristics of
colorectal cancer. China Med Herald. 16:60–63. 2019.(In
Chinese).
|
|
10
|
Li QQ, Wang J and Zhao Y: Current status
of research on risk factors associated with the development of
colorectal polyps. Med Rev. 26:3196–3200. 2020.
|
|
11
|
Huang D, Zhu XZ and Sheng WQ:
Interpretation of the gastrointestinal epithelial tumors of 2019
edition of <WHO classification of tumors of the digestive
system>. Chin J Pathol. 49:209–213. 2020.
|
|
12
|
Fang SG, Wei JG and Chen ZW: WHO
classification of tumours of the digestive system (2019). J Diagn
Pathol. 26:865–870. 2019.(In Chinese).
|
|
13
|
Tibshirani R: Regression shrinkage and
selection via the lasso: A ret-rospective. J Royal Statistical Soc.
58:273–282. 2011. View Article : Google Scholar
|
|
14
|
Sninsky JA, Shore BM, Lupu GV and Crockett
SD: Risk factors for colorectal polyps and cancer. Gastrointest
Endosc Clin N Am. 32:195–213. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
von Elm E, Altman DG, Egger M, Pocock SJ,
Gøtzsche PC and Vandenbroucke JP; STROBE Initiative, : The
strengthening the reporting of observational studies in
epidemiology (STROBE) statement: Guidelines for reporting
observational studies. Lancet. 370:1453–1457. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fang R: Construction of a mult-icenter
sleep database and a risk prediction modeling of moderate to severe
obstructive sleep apnea in the population with sleep disorders
(unpublished PhD thesis). Southern Medical University; 2024, (In
Chinese).
|
|
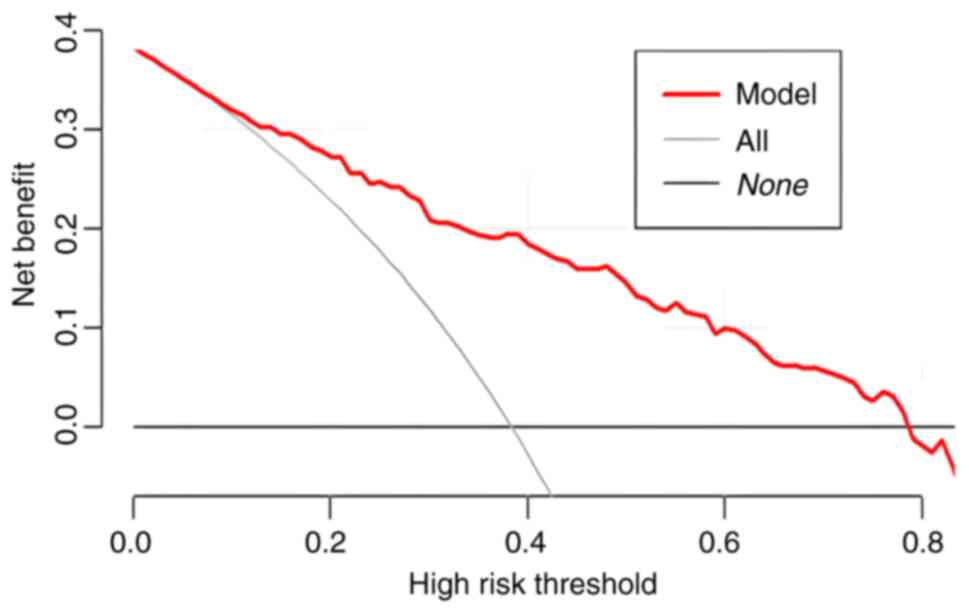
17
|
Zhao L, Leng Y, Hu Y, Xiao J, Li Q, Liu C
and Mao Y: Understanding decision curve analysis in clinical
prediction model research. Postgrad Med J. 100:512–515. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Vickers AJ and Holland F: Decision curve
analysis to evaluate the clinical benefit of prediction models.
Spine J. 21:1643–1648. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kerr KF, Brown MD, Zhu K and Janes H:
Assessing the clinical impact of risk prediction models with
decision curves: Guidance for correct interpretation and
appropriate use. J Clin Oncol. 34:2534–2540. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
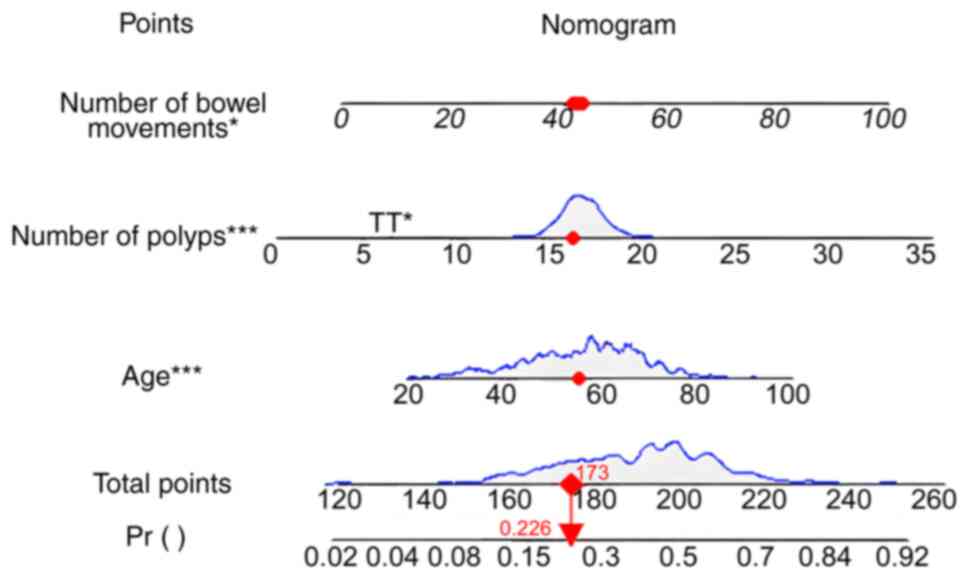
20
|
Iasonos A, Schrag D, Raj GV and Panageas
KS: How to build and interpret a nomogram for cancer prognosis. J
Clin Oncol. 26:1364–1370. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Balachandran VP, Gonen M, Smith JJ and
DeMatteo RP: Nomograms in oncology: More than meets the eye. Lancet
Oncol. 16:e173–e180. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gafita A, Calais J, Grogan TR, Hadaschik
B, Wang H, Weber M, Sandhu S, Kratochwil C, Esfandiari R, Tauber R,
et al: Nomograms to predict outcomes after 177Lu-PSMA therapy in
men with metastatic castration-resistant prostate cancer: An
international, multicentre, retrospective study. Lancet Oncol.
22:1115–1125. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Liu H, Li J, Guo J, Shi Y and Wang L: A
prediction nomogram for neonatal acute respiratory distress
syndrome in late-preterm infants and full-term infants: A
retrospective study. EClinicalMedicine. 50:1015232022. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Pietrantonio F, Lonardi S, Corti F,
Infante G, Elez ME, Fakih M, Jayachandran P, Shah AT, Salati M,
Fenocchio E, et al: Nomogram to predict the outcomes of patients
with microsatellite instability-high metastatic colorectal cancer
receiving immune checkpoint inhibitors. J Immunother Cancer.
9:e0033702021. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Viswanathan AN, Hankinson SE and
Schernhammer ES: Night shift work and the risk of endometrial
cancer. Cancer Res. 67:10618–10622. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Thompson CL, Larkin EK, Patel S, Berger
NA, Redline S and Li L: Short duration of sleep increases risk of
colorectal adenoma. Cancer. 117:841–8747. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Um K, Park CS, Yoo C, Ahn YS, Kim M and
Jeong KS: Risk factors including night shift work of colorectal
polyp. Ann Occup Environ Med. 32:e262020. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Alpert O, Begun L, Issac T and Solhkhah R:
The brain-gut axis in gastrointestinal cancers. J Gastrointest
Oncol. 12 (Suppl 2):S301–S331. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wang X, Wang S and Cao K: Prevention and
treatment of colorectal cancer by ‘brain-intestinal axis’ of
traditional Chinese medicine. World TCM. 18:3085–3089. 2023.
|
|
30
|
Cryan JF, O'Riordan KJ, Cowan CSM, Sandhu
KV, Bastiaanssen TFS, Boehme M, Codagnone MG, Cussotto S, Fulling
C, Golubeva AV, et al: The microbiota-gut-brain axis. Physiol Rev.
99:1877–2013. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Xiao W, Su J, Gao X, Yang H, Weng R, Ni W
and Gu Y: The microbiota-gut-brain axis participates in chronic
cerebral hypoperfusion by disrupting the metabolism of short-chain
fatty acids. Microbiome. 10:622022. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wu S, Liu X, Jiang R, Yan X and Ling Z:
Roles and mechanisms of gut microbiota in patients With Alzheimer's
disease. Front Aging Neurosci. 13:6500472021. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ma C, Li Y, Mei Z, Yuan C, Kang JH,
Grodstein F, Ascherio A, Willett WC, Chan AT and Huttenhower C:
Association between bowel movement pattern and cognitive function:
Prospective cohort study and a metagenomic analysis of the gut
microbiome. Neurology. 101:e2014–e2025. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Polimeno L, Barone M, Mosca A, Viggiani
MT, Joukar F, Mansour-Ghanaei F, Mavaddati S, Daniele A, Debellis
L, Bilancia M, et al: Soy Metabolism by gut microbiota from
patients with precancerous intestinal lesions. Microorganisms.
8:4692020. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Wei H: Theoretical connotation and
biological mechanism of ‘The Lung is Connected with the Large
Intestine, and the Large Intestine Corresponds to the Skin’. J
Beijing Univ Traditional Chin Med. 46:1350–1356. 2023.
|
|
36
|
Liu B, Yu Y, Zhao M, Xiao K, Yan P, Duan
Z, Wang K, Zhao N, Cao J, Wang J and Xie L: Correlation analysis of
the microbiome and immune function in the lung-gut axis of
critically Ill patients in the ICU. Front Med (Lausanne).
9:8083022022. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Zhao M, Shao F, Yu D, Zhang J, Liu Z, Ma
J, Xia P and Wang S: Maturation and specialization of group 2
innate lymphoid cells through the lung-gut axis. Nat Commun.
13:76002022. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Mazumder MHH, Gandhi J, Majumder N, Wang
L, Cumming RI, Stradtman S, Velayutham M, Hathaway QA, Shannahan J,
Hu G, et al: Lung-gut axis of microbiome alterations following
co-exposure to ultrafine carbon black and ozone. Part Fibre
Toxicol. 20:152023. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Zorn AM and Wells JM: Vertebrate endoderm
development and organ formation. Annu Rev Cell Dev Biol.
25:221–251. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Rankin SA, Han L, McCracken KW, Kenny AP,
Anglin CT, Grigg EA, Crawford CM, Wells JM, Shannon JM and Zorn AM:
A retinoic acid-hedgehog cascade coordinates mesoderm-inducing
signals and endoderm competence during lung specification. Cell
Rep. 16:66–78. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Liu S, Liu XY, Li LH, Wang X, Cui YF, Sun
GZ and Guo XZ: Histology and cytology basic research on'Lung and
Large Intestine being interior-exteriorly Related'. Chin J Trad
Chin Med Pharm. 27:1167–1170. 2012.(In Chinese).
|
|
42
|
Li LH: ‘Biological mechanism of the
relationship between the lung and the large intestine: A study on
the physiological mechanism of the correlation between lung and
intestinal tissues in a rat]. Beijing: Beijing University of
Chinese Medicine; pp. 1–4. 2012
|
|
43
|
Tulic MK, Piche T and Verhasselt V:
Lung-gut cross-talk: Evidence, mechanisms and implications for the
mucosal inflammatory diseases. Clin Exp Allergy. 46:519–528. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Tan XD, Chen YH, Liu QP, Gonzalez-Crussi F
and Liu XL: Prostanoids mediate the protective effect of trefoil
factor 3 in oxidant-induced intestinal epithelial cell injury: Role
of cyclooxygenase-2. J Cell Sci. 113:2149–2155. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Ganguly K and Schulz H: Association
studies of lung function in mice. Dtsch Tierarztl Wochenschr.
115:276–284. 2008.PubMed/NCBI
|
|
46
|
Pietrantonio F, Lonardi S, Corti F,
Infante G, Elez ME, Fakih M, Jayachandran P, Shah AT, Salati M,
Fenocchio E, et al: Nomogram to predict the outcomes of patients
with microsatellite instability-high metastatic colorectal cancer
receiving immune checkpoint inhibitors. J Immunother Cancer.
9:e0033702021. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Mao WX, Zhong ZS, Huang SP, Zhang W and
Wang J: Analysis of risk factors and TCM mechanism of adenomatous
polyps. Chin J Integr Tradit West Med Dig. 27:726–729,734.
2019.
|
|
48
|
Hao Y, Wang Y, Qi M, He X, Zhu Y and Hong
J: Risk factors for recurrent colorectal polyps. Gut Liver.
14:399–411. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Lucas C, Barnich N and Nguyen HTT:
Microbiota, inflammation and colorectal cancer. Int J Mol Sci.
18:13102017. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
He X, Wu K, Ogino S, Giovannucci EL, Chan
AT and Song M: Association between risk factors for colorectal
cancer and risk of serrated polyps and conventional adenomas.
Gastroenterology. 155:355–373.e18. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Yun GY, Moon HS, Kwon IS, Kim JS, Kang SH,
Lee ES, Kim SH, Sung JK, Lee BS and Jeong HY: Left-sided colectomy:
One of the important risk factors of metachronous colorectal
adenoma after colectomy for colon cancer. Dig Dis Sci.
63:1052–1061. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
International Society on Thrombosis and
Haemostasis (ISTH), . ISTH guidelines for coagulation testing.
2021.https://www.isth.org
|
|
53
|
Ren Y, Liang H, Huang Y, Miao Y, Li R,
Qiang J, Wu L, Qi J, Li Y, Xia Y, et al: Key candidate genes and
pathways in T lymphoblastic leukemia/lymphoma identified by
bioinformatics and serological analyses. Front Immunol.
15:13412552024. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Wu LL, Lin WK, Qian JY, Ma SS, Li MJ, Li
K, Li ZX, Lan G and Xie D: Prognostic assessment of lung
adenocarcinoma patients with early-staging diseases: A nomogram
based on coagulation-related factors. Eur J Cardiothorac Surg.
64:ezad3132023. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Wang HY, Xiu DR, Li ZF and Wang G:
Coagulation function in patients with pancreatic carcinoma. Chin
Med J (Engl). 122:697–700. 2009.PubMed/NCBI
|
|
56
|
Ward MP, E Kane L, Norris L, Mohamed BM,
Kelly T, Bates M, Clarke A, Brady N, Martin CM, Brooks RD, et al:
Platelets, immune cells and the coagulation cascade; friend or foe
of the circulating tumour cell? Mol Cancer. 20:592021. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Yin J and Zhu SS: Routine coagulation
molecules predict nasopharyngeal carcinoma and associated
metastases. Br J Biomed Sci. 76:178–183. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Peng PH, Wu CC, Liu SC, Chang KP, Chen CD,
Chang YT, Hsu CW, Chang YS and Yu JS: Quantitative plasma proteome
analysis reveals aberrant level of blood Coagulation-related
proteins in nasopharyngeal carcinoma. J Proteomics. 74:744–757.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Marinho FC and Takagaki TY:
Hypercoagulability and lung cancer. J Bras Pneumol. 34:312–322.
2008.(In English, Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Hammouda A, Souilah S, Ferhat-Hamida MY,
Amir ZC, Aouichat-Bouguerra S and Hariti G: Activation of
coagulation in patients with lung cancer. Ann Biol Clin (Paris).
77:272–280. 2019.(In French). PubMed/NCBI
|
|
61
|
Repetto O and De Re V: Coagulation and
fibrinolysis in gastric cancer. Ann N Y Acad Sci. 1404:27–48. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Wang B, Zou D, Wang N, Wang H, Zhang T,
Gao L, Ma C, Zheng P, Gu B, Li X, et al: Construction and
validation of a novel coagulation-related 7-gene prognostic
signature for gastric cancer. Front Genet. 13:9576552022.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Chuang IW, Cho YH, Ahn MJ, Lee MJ, Kim GM,
Chung CS and Bang OY: Association of cancer cell type and
extracellular vesicles with coagulopathy in patients with lung
cancer and stroke. Stroke. 49:1282–1285. 2018. View Article : Google Scholar
|
|
64
|
Kessler CM: The link between cancer and
venous thromboembolism: A review. Am J Clin Oncol. 32 (4
Suppl):S2–S7. 2009. View Article : Google Scholar
|
|
65
|
Guo Q, Zhang B, Dong X, Xie Q, Guo E,
Huang H and Wu Y: Elevated levels of plasma fibrinogen in patients
with pancreatic cancer: Possible role of a distant metastasis
predictor. Pancreas. 38:e75–e79. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Tang L, Liu K, Wang J, Wang C, Zhao P and
Liu J: High preoperative plasma fibrinogen levels are associated
with distant metastases and impaired prognosis after curative
resection in patients with colorectal cancer. J Surg Oncol.
102:428–432. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Sahni A, Simpson-Haidaris PJ, Sahni SK,
Vaday GG and Francis CW: Fibrinogen synthesized by cancer cells
augments the prolifrative effect of fibroblast growth factor-2. J
Thromb Haemost. 6:176–183. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Junsheng L, Ziling Y and Zhengyuan H:
Construction of a prediction model to distinguish colorectal
adenoma from colorectal cancer based on conventional test
indicators. Tumor Control Res. 51:353–360. 2024.(In Chinese).
|
|
69
|
Liu ZH, Zhang N, Li FX, Li SX and Liu JT:
Correlation between homocysteine, coagulation function indicators
and the risk of colorectal cancer incidence: a case-control study.
Chin J Clin Oncol. 50:654–660. 2023.(In Chinese).
|
|
70
|
Chen ZH, Sun SB, Wang XM, Yu SS, Wu XF,
Chen XS, Geng T, Liu H, Liu XM and Nan Q: Abnormal Coagulation
Parameters in Patients with Early Colorectal Cancer and Its
Clinical Significance. Journal of Kunming Medical University.
42:96–100. 2021.(In Chinese).
|
|
71
|
Negro S, Bao QR, Scarpa M, Scognamiglio F,
Pucciarelli S, Remo A, Agostini M, D'Angelo E, Mammi I, Schiavi F,
et al: Multiple colorectal adenomas syndrome: The role of MUTYH
mutation and the polyps' number in clinical management and
colorectal cancer risk. Dig Liver Dis. 56:1087–1094. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Wang W and Wang XR: Exploring Risk Factors
for Colorectal Polyp Malignant Transformation in Middle-Aged and
Elderly Patients Based on Multivariate Logistic Regression
Analysis. Modern Medicine and Health Research Electronic Journal.
9:122–124. 2025.(In Chinese).
|
|
73
|
Kim SE, Shim KN, Jung SA, Yoo K and Moon
IH: An association be-tween obesity and the prevalence of colonic
adenoma according to age and gender. J Gastroenterol. 42:616–623.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Meester RGS, Mannalithara A,
Lansdorp-Vogelaar I and Ladabaum U: Trends in incidence and stage
at diagnosis of colorectal cancer in adults aged 40 through 49
years, 1975–2015. JAMA. 321:1933–1934. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Chen XY and Kong LB: Progress of research
on factors and mechanisms associated with carcinogenesis of
colorectal adenomatous polyps. Chin J Cancer Prevention Treatment.
26:354–358. 2019.
|
|
76
|
Wu H, Zhang J and Zhou B: Metabolic
syndrome and colorectal adenoma risk: A systematic review and
metaanalysis. Clin Res Hepatol Gastroenterol. 45:1017492021.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Han X, Qian W, Liu Y, Zheng T, Su XJ,
Zhang PP, Chen Y, Hu LH and Li ZS: Effects of age, sex and
pathological type on the risk of multiple polyps: A Chinese
teaching hospital study. J Dig Dis. 21:505–511. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Karsenti D, Tharsis G, Burtin P, Venezia
F, Tordjman G, Gillet A, Samama J, Nahon-Uzan K, Cattan P and
Cavicchi M: Adenoma and advanced neoplasia detection rates increase
from 45 years of age. World J Gastroen. 25:447–456. 2019.
View Article : Google Scholar
|
|
79
|
Lin G, Feng Z, Liu H, Li Y, Nie Y, Liang Y
and Li K: Mass screening for colorectal cancer in a population of
two million older adults in Guangzhou, China. Sci Rep. 9:104242019.
View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Hong W, Dong L, Stock S, Basharat Z, Zippi
M and Zhou M: Prevalence and characteristics of colonic adenoma in
mainland China. Cancer Manag Res. 10:2743–2755. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Sun DH: Clinical characteristics of 543
cases of tubular adenomatous polyps and their carcinogenesis of the
large intestine. Gansu Med. 36:705–707. 2017.
|
|
82
|
McCashland TM, Brand R, Lyden E and de
Garmo P; CORI Research Project, : Gender differences in colorectal
polyps and tumors. Am J Gastroenterol. 96:882–886. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Jin EH, Han K, Lee DH, Shin CM, Lim JH,
Choi YJ and Yoon K: Association between metabolic syndrome and the
risk of colorectal cancer diagnosed before age 50 years according
to tumor location. Gastroenterology. 163:637–648.e2. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Chen H, Li N, Ren J, Feng X, Lyu Z, Wei L,
Li X, Guo L, Zheng Z, Zou S, et al: Participation and yield of a
population-based colorectal cancer screening programme in China.
Gut. 68:1450–1457. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Soltani G, Poursheikhani A, Yassi M,
Hayatbakhsh A, Kerachian M and Kerachian MA: Obesity, diabetes and
the risk of colorectal adenoma and cancer. BMC Endocr Disord.
19:1132019. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Lin CC, Huang KW, Luo JC, Wang YW, Hou MC,
Lin HC, Lee FY and Chan WL: Hypertension is an important predictor
of recurrent colorectal adenoma after screening colonoscopy with
adenoma polypectomy. J Chin Med Assoc. 77:508–512. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Xing J, Ren J and Zhang Q: Analysis of
risk factors for the development of colorectal adenomatous polyps.
J Capital Med Univ. 42:601–608. 2021.
|
|
88
|
Liu ZH, Zhang GX, Zhang H, Jiang L, Deng
Y, Chan FSY and Fan JKM: Association of body fat distribution and
metabolic syndrome with the occurrence of colorectal adenoma: A
Case-control study. J Dig Dis. 22:222–229. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Blackett JW, Verna EC and Lebwohl B:
Increased prevalence of colorectal adenomas in patients with
nonalcoholic fatty liver disease: A Cross-sectional study. Dig Dis.
38:222–230. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Han X, Qian W, Liu Y, Zheng T, Su XJ,
Zhang PP, Chen Y, Hu LH and Li ZS: Effects of age, sex and
pathological type on the risk of multiple polyps: A Chinese
teaching hospital study. J Dig Dis. 21:505–511. 2020. View Article : Google Scholar : PubMed/NCBI
|