Introduction
Gastric cancer is the fourth most common cancer and
is considered one of the most deadly cancers worldwide (1–4).
Although the incidence of gastric cancer has decreased recently,
the mortality rate remains high due to late diagnosis and a lack of
understanding of molecular pathogenesis. In South Korea, the
survival of gastric cancer patients has increased due to early
detection. The 5-year survival rate for stage I gastric cancer is
>90% in Korea (4,5). However, in the West, the 5-year
survival rate is generally <50% for stage II and 20% for stage
III cancer (4,6,7). Thus,
early diagnosis of gastric cancer and preventive treatment are
urgently needed to control the high mortality of this disease.
Diet is suggested to be crucial in gastrointestinal
cancer development and progression (8). Epidemiological studies show a strong
inverse correlation between vegetable intake and the risk of cancer
including gastric cancer (9–15).
Turati et al (12) and
Guercio et al (16) reported
that high allium vegetable consumption reduces gastric cancer risk,
and a high intake of cruciferous vegetables was found to be
inversely associated with the risk of gastric cancer in humans in a
study by Wu et al (15). The
compound 3,3′-diindolylmethane (DIM) is a component of cruciferous
vegetables that inhibits tumor growth through induction of
apoptosis in various types of cancer cells (17–20).
Our previous study demonstrated that DIM suppressed gastric cancer
cell growth via activation of the Hippo signaling pathway (17). DIM was found to inhibit gastric
cancer cell growth by modulating the aryl hydrocarbon receptor
(21). However, the function of DIM
in gastric cancer cells has not been clearly elucidated.
Forkhead box M1 (FOXM1) is an oncogenic FOX
transcription factor (22,23). Increased expression of FOXM1 has
been noted in a variety of aggressive human cancers (24,25),
suggesting that FOXM1 is important in oncogenesis. In gastric
cancer, FOXM1 is highly expressed and strongly correlated with poor
prognosis associated with drug resistance (26–29).
Although FOXM1 is important in gastric cancer, no studies have
investigated DIM and the regulation of FOXM1 in gastric cancer.
Moreover, the molecular mechanisms by which DIM contributes to
Akt/FOXM1 signaling pathway regulation in gastric cancer are not
fully understood. We tested whether DIM potentiated the efficacy of
chemotherapeutic agents such as paclitaxel in gastric cancer cells.
Our results showed that DIM inhibited Akt/FOXM1 signaling, which
led to the chemosensitization of gastric cancer cells and
potentiation of the efficacy of chemotherapeutic agents such as
paclitaxel. Our findings also demonstrated that the Akt/FOXM1
pathway is a novel molecular target of DIM, and that targeting this
pathway by combination treatment with DIM and paclitaxel is a new
strategy for gastric cancer treatment.
Materials and methods
Cell lines and experimental reagents
The gastric cancer cell line SNU638 was obtained
from the Korean Cell Line Bank (Seoul National University, Seoul,
Korea). Primary antibodies for Akt, p-Akt, p-GSK-3β, cleaved-PARP,
cleaved-caspase-9 and caspase-3 were obtained from Cell Signaling
Technology (Beverly, MA, USA), and antibodies to FOXM1 and GAPDH
were from Santa Cruz Biotechnology Inc. (Santa Cruz, CA, USA). DIM
was purchased from LKT Laboratories (St. Paul, MN, USA), and
paclitaxel was dissolved in dimethyl sulfoxide (DMSO) (both from
Sigma Chemical Co., St. Louis, MO, USA).
Cell proliferation assay
SNU638 cells were seeded in 96-well plates. After 24
h, the cells were treated with DIM (0, 50, 75 or 100 μM), followed
by 72 h of growth with or without paclitaxel (0, 50, 75 or 100 nM).
Cell growth was studied using
3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT)
assays as previously described (30,31).
MTT (50 μl) was added to the culture medium of growing cells at the
indicated time points, and the cells were incubated for a further 3
h. DMSO (200 μl) was added and the absorbance was measured at 540
nM using a model Epoch microplate reader (BioTek, Winooski, VT,
USA) Three independent experiments were performed in
triplicates.
Soft agar colony formation assay
Colony formation assays were performed as previously
described (17,19). Cells were seeded at 5×104
cells/plate with or without DIM and paclitaxel, grown until visible
colonies appeared and observed under microscopy to count colonies.
Experiments were performed >3 times.
Western blot analysis
SNU638 cells were treated with DIM (0, 50, 75 or 100
μM), followed by 72 h of growth with or without paclitaxel (0, 50,
75 or 100 nM). Cells with or without DIM and paclitaxel were
harvested and suspended in lysis buffer (Intron Biotechnology,
Inc.) as previously described (17,19,31).
The protein concentration was determined using BSA protein assay
kits (Pierce, Rockford, IL, USA). Whole lysates were resolved on
SDS-PAGE gels, transferred to PVDF membranes (Bio-Rad, Hercules,
CA, USA), and probed with specific primary antibodies for
cleaved-PARP, cleaved-caspase-9, caspase-3, p-Akt, Akt, FOXM1,
cyclin D1, CDK4, p53 and p-GSK-3β and then incubated with a
horseradish peroxidase-conjugated goat anti-rabbit or anti-mouse
secondary antibody (Cell Signaling Technology). Immunodetection was
performed with an enhanced chemiluminescent kit (Amersham,
Arlington Heights, IL, USA).
Statistical analysis
Experiments were repeated >3 times. Data are
expressed as mean ± SE. Comparisons between groups were evaluated
using the Student’s t-test or one-way ANOVA where appropriate. A
p-value <0.05 was considered to indicate a statistically
significant result.
Results
Inhibition of cell growth by DIM and
paclitaxel
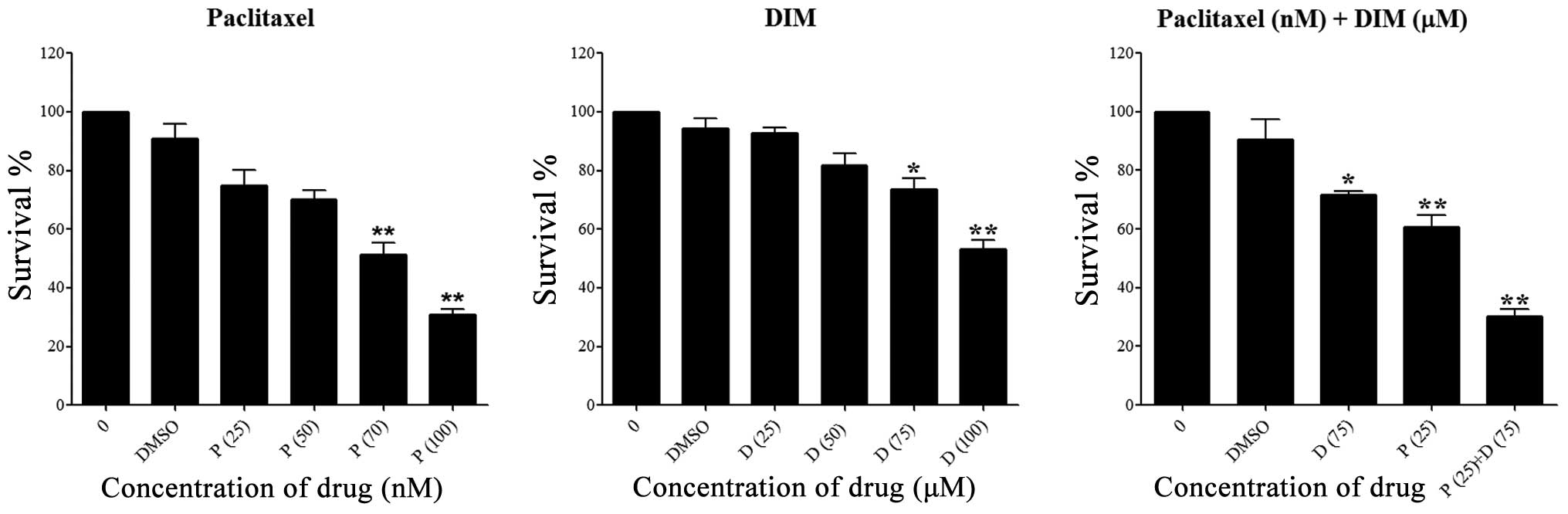
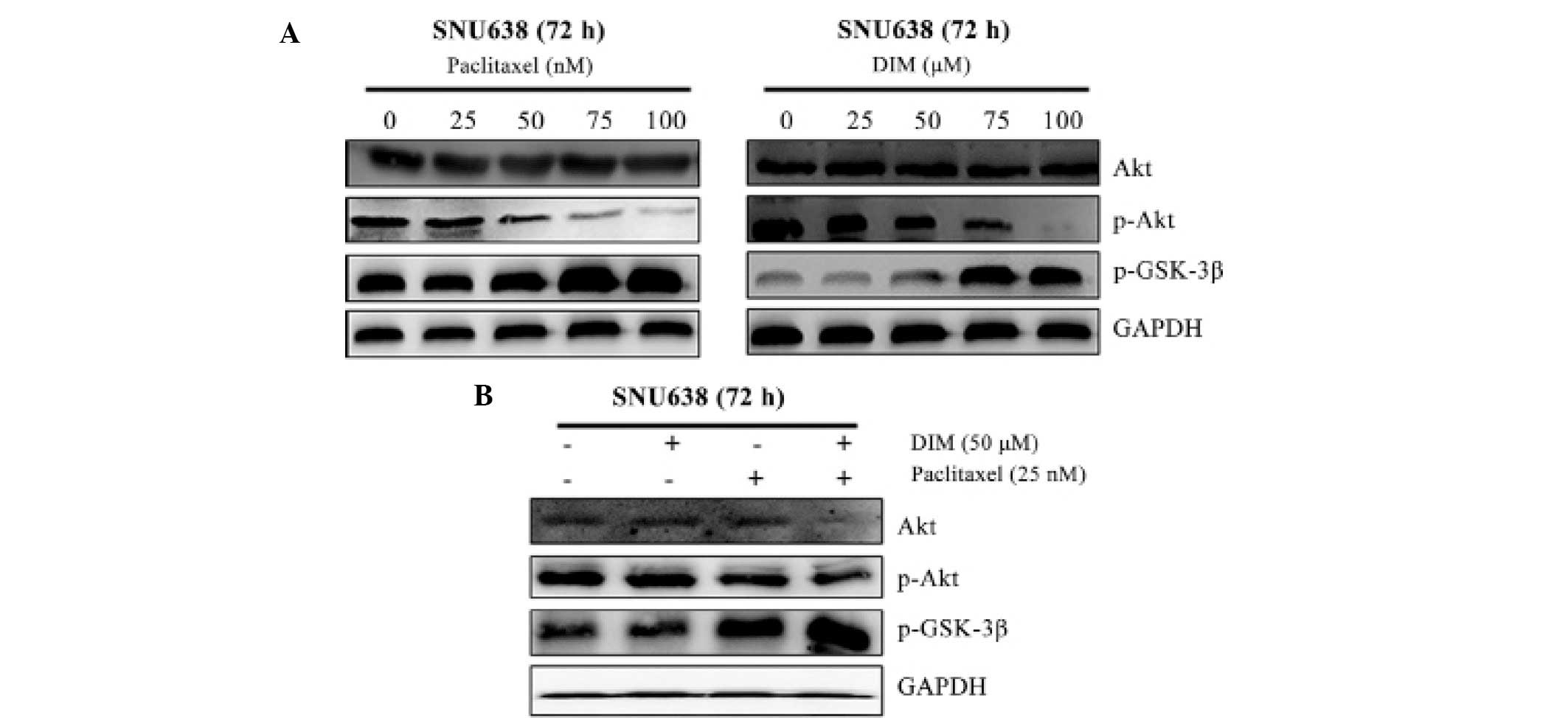
SNU638 gastric cancer cells were treated with the
indicated doses of DIM and paclitaxel for 72 h. DIM and paclitaxel
dose-dependently inhibited gastric cancer cell viability at 72 h.
As shown in Fig. 1, treatment with
75 μM DIM or 25 nM paclitaxel caused 30–50% growth inhibition of
SNU638 cells. However, a combination of DIM and paclitaxel resulted
in 70–80% growth inhibition of the SNU638 cells at 72 h, suggesting
a greater inhibitory effect of the combination treatment. Our
results revealed that a combination of DIM with a low-dose of
paclitaxel had substantially greater inhibition of cancer cell
growth compared with either agent alone.
 | Figure 1Cell growth inhibition after DIM and
paclitaxel treatment. Human gastric cancer SNU638 cells were
treated with DIM (0, 25, 50, 75 and 100 μM), paclitaxel (0, 25, 50,
70 and 100 nM) or a combination of DIM 75 μM and paclitaxel 25 nM.
Cell proliferation was assessed using MTT assays. Data are mean
(SE) of >3 independent experiments with triplicate dishes. D,
DIM; P, paclitaxel, *p<0.05 and
**p<0.01 compared to the control. DIM,
3,3′-diindolylmethane. |
Inhibition of colony formation by DIM and
paclitaxel
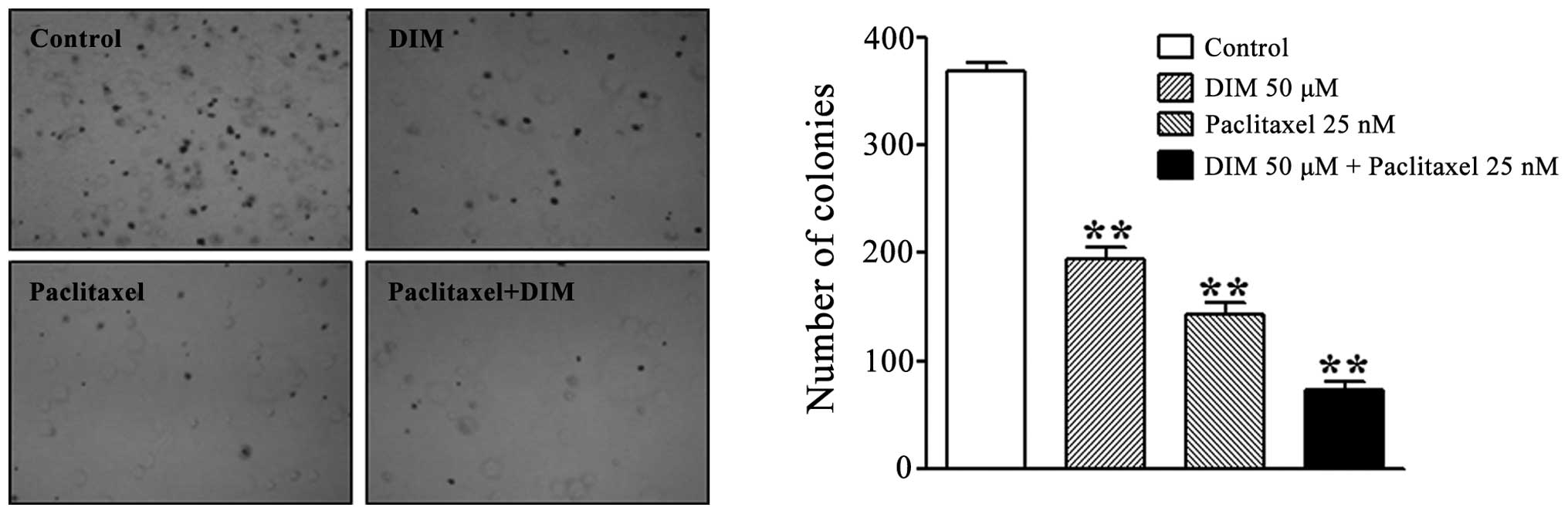
We further investigated the antitumor effects of DIM
and paclitaxel using colony formation assays. As shown in Fig. 2, treatment with 50 μM DIM and 25 nM
paclitaxel significantly inhibited the colony formation of the
SNU638 cells. Moreover, the combination treatment with DIM and
paclitaxel at the indicated doses resulted in greater inhibition of
the colony formation of the SNU638 cells than treatment with a
single agent (Fig. 2).
Induction of apoptosis by DIM and
paclitaxel
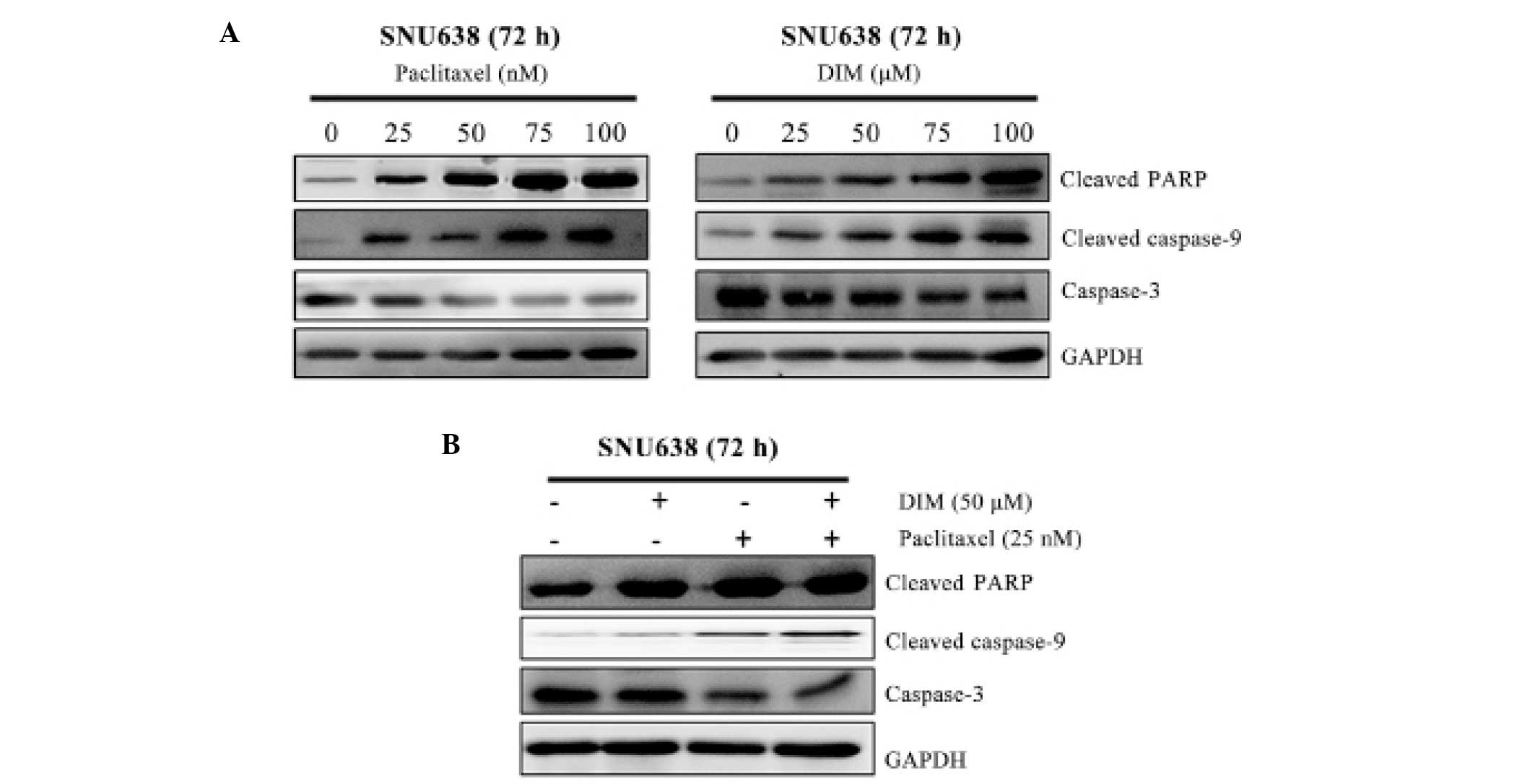
To elucidate the apoptotic effects of DIM and
paclitaxel on SNU638 cells, we measured levels of the apoptotic
factors: cleaved-PARP, cleaved caspase-9 and caspase-3. As shown in
Fig. 3A, treatment with 50 μM DIM
or 25 nM paclitaxel alone dose-dependently increased cleaved-PARP
and cleaved caspase-9 proteins, whereas expression of caspase-3 was
significantly decreased. The combination treatment of DIM and
paclitaxel at the indicated doses significantly induced
cleaved-PARP and cleaved caspase-9, while caspase-3 was
significantly suppressed (Fig. 3B).
These results revealed that the combination of DIM and paclitaxel
induced greater apoptotic effects in the SNU638 cells than the
single agents alone, supporting DIM enhancement of
paclitaxel-induced cell growth inhibition in gastric cancer
cells.
Downregulation of FOXM1 levels by DIM and
paclitaxel
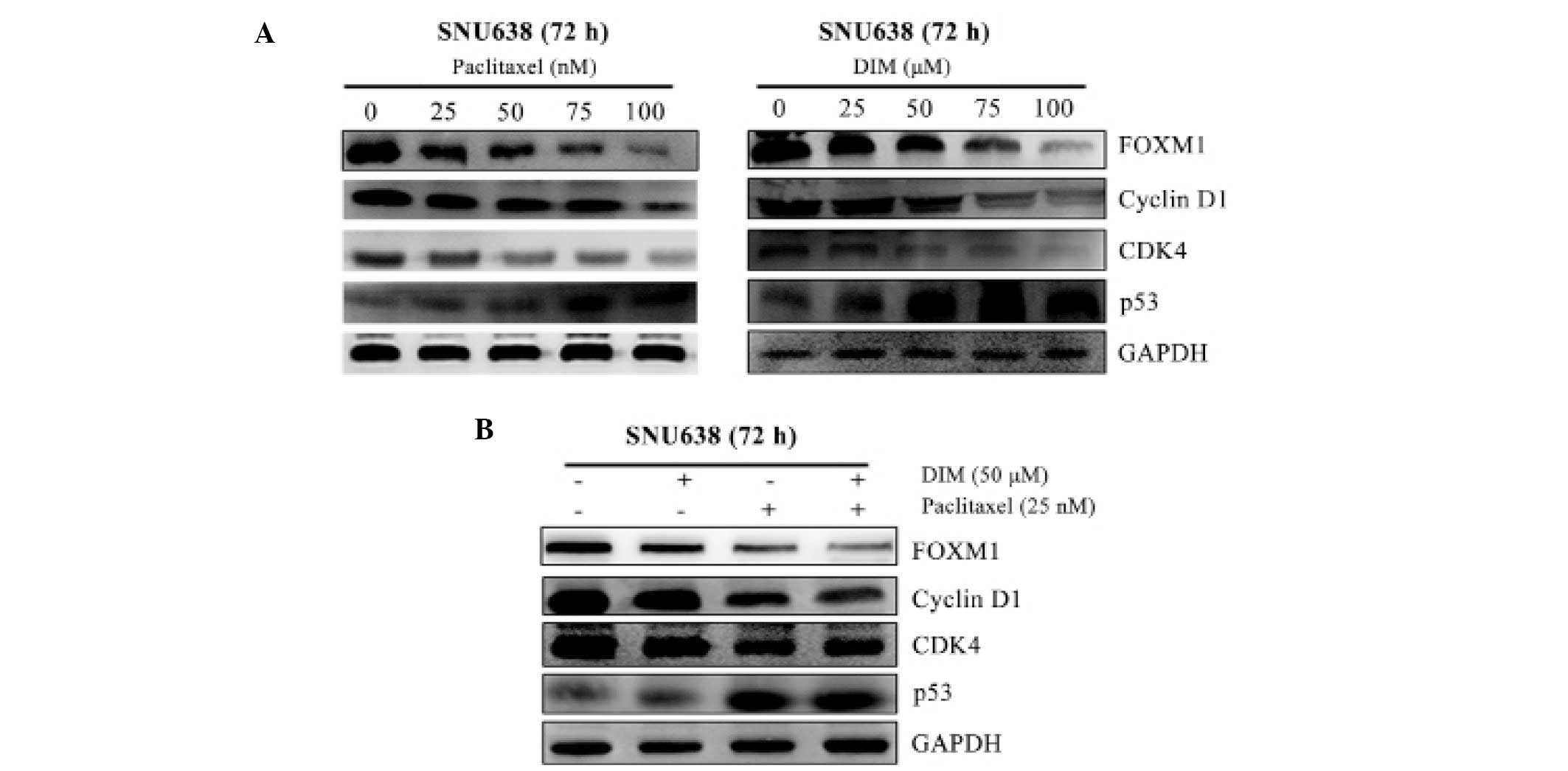
FOXM1 is an important transcription factor for
cancer cell growth (22).
Therefore, we examined whether DIM and paclitaxel have a functional
impact on FOXM1 expression in gastric cancer oncogenesis. After
treatment of the SNU638 cells with DIM or paclitaxel alone, FOXM1
expression decreased dose-dependently at 72 h (Fig. 4A). Expression of FOXM1 was reduced
after treatment with a combination of DIM and paclitaxel compared
to treatment with either agent alone (Fig. 4B). Levels of the cyclin-dependent
kinase inhibitor p53 which is a downstream gene affected by FOXM1,
increased dose-dependently after DIM or paclitaxel treatment, and
combination treatment with these two drugs increased the levels of
p53 at 72 h (Fig. 4B). CDK4 and
CDK6 protein significantly and dose-dependently decreased after a
72 h treatment with DIM or paclitaxel (Fig. 4A), and the combination treatment
significantly downregulated CDK4 protein level (Fig. 4B). These results revealed that the
combination of DIM and paclitaxel induced more marked
downregulation of FOXM1, which induced cell cycle inhibition in the
SNU638 cells, when compared with treatment with each single agent
alone. These findings support that DIM effectively potentiates
paclitaxel cytotoxicity.
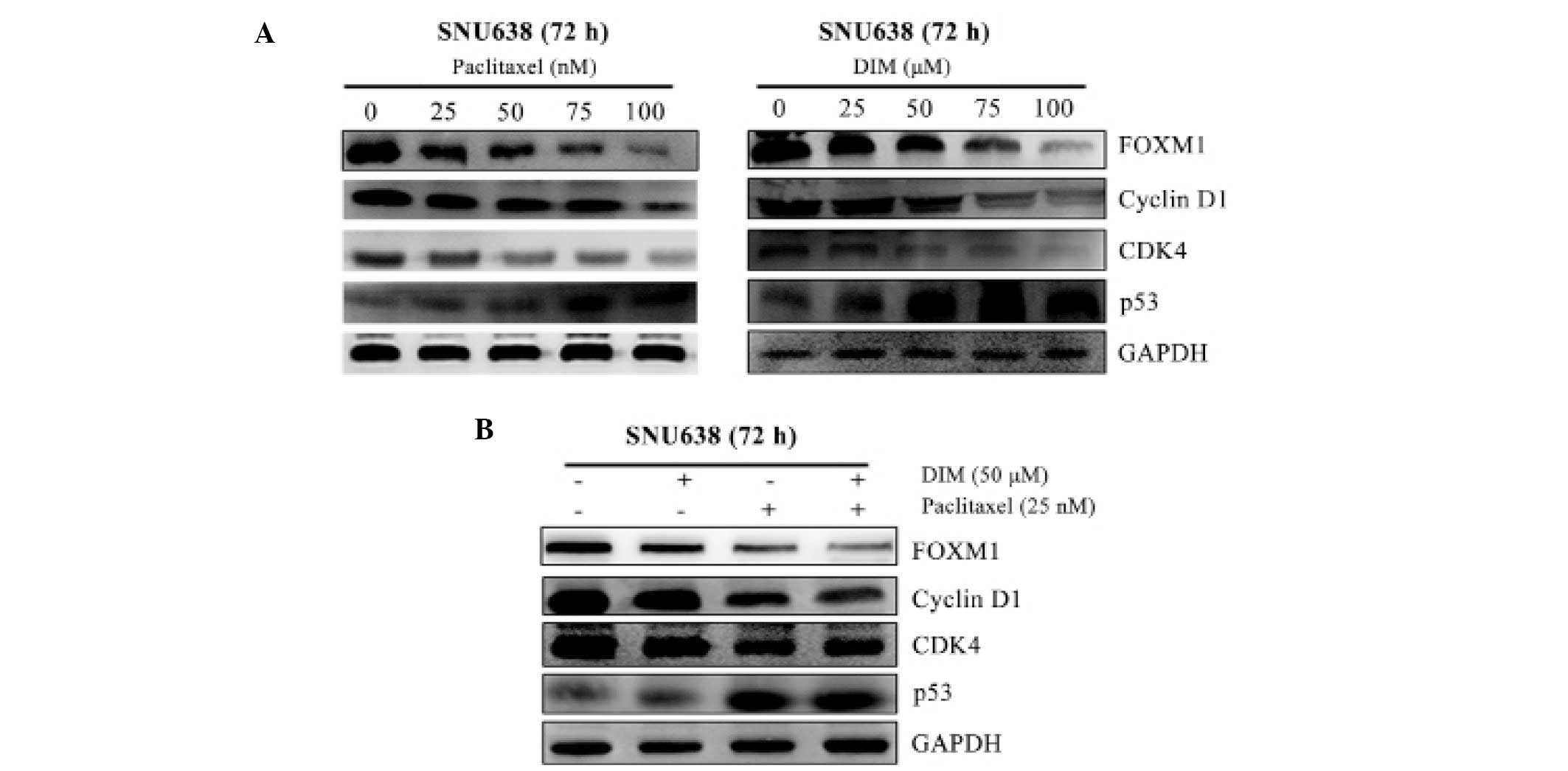 | Figure 4Effects of DIM and paclitaxel on
FOXM1 and effector cell cycle regulators. FOXM1, CDK4, cyclin D1
and p53 were measured by western blot analysis of SNU638 cells
after treatment with (A) DIM (0, 25, 50, 75 and 100 μM) or
paclitaxel (0, 25, 50, 75 and 100 nM) alone or (B) in combination.
GAPDH was the internal control. DIM, 3,3′-diindolylmethane. |
Downregulation of Akt by DIM and
paclitaxel
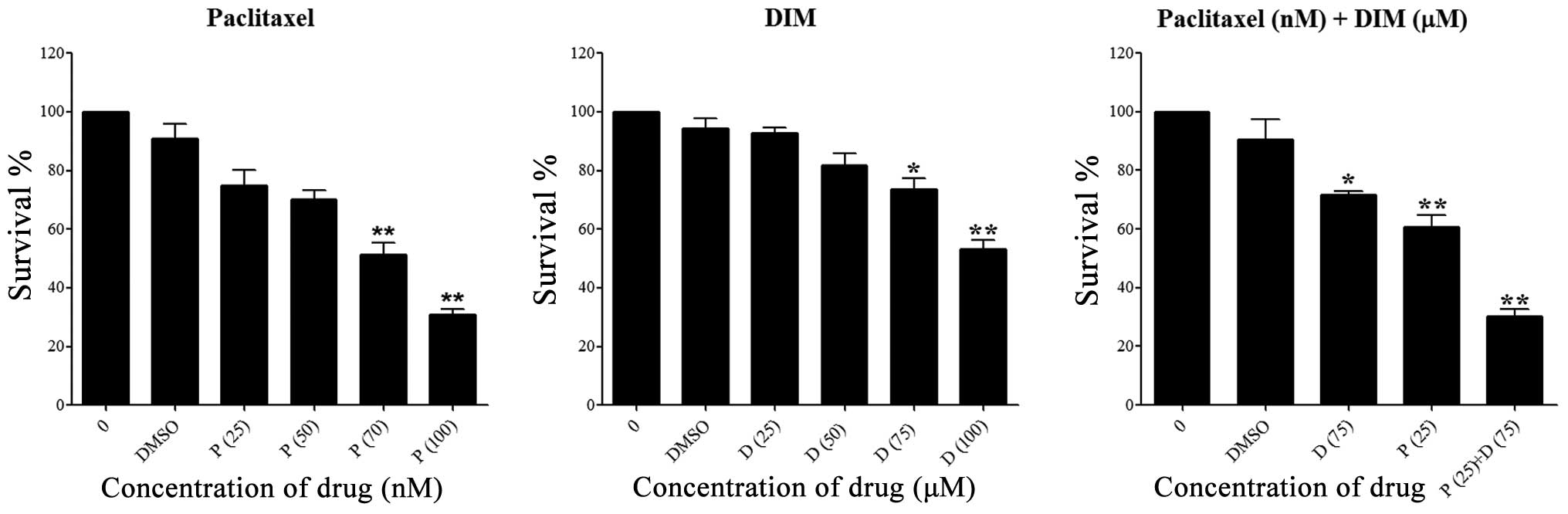
To study the functional relevance of alteration of
Akt expression in gastric cancer cells mediated by DIM or
paclitaxel, we measured p-Akt, Akt and p-GSK-3β protein in the
SNU638 cells. DIM significantly and dose-dependently decreased the
p-Akt level, while the Akt protein level was unchanged (Fig. 5A). Paclitaxel also significantly and
dose-dependently inhibited expression of p-Akt at 72 h (Fig. 5A). Furthermore, the combination
treatment with DIM (50 μM) and paclitaxel (25 nM) resulted in
significantly greater reduction in p-Akt protein at 72 h compared
with treatment with either agent alone (Fig. 5B). In addition, the p-GSK-3β protein
level was significantly and dose-dependently increased by DIM or
paclitaxel treatment, and treatment with the combination of the two
drugs induced higher expression of p-GSK-3β protein in the gastric
cancer cells than did either agent alone.
Discussion
The present study was performed to investigate the
molecular mechanisms by which DIM contributes to Akt/FOXM1
signaling pathway regulation and to determine whether DIM
potentiates the efficacy of chemotherapeutic agents such as
paclitaxel in gastric cancer cells. We determined the effects of
DIM on Akt/FOXM1 and its signaling pathway in gastric cancer cells.
Our results showed that DIM can function as a FOXM1 suppressor in
gastric cancer cells. Inactivation of Akt by DIM resulted in the
downregulation of FOXM1 and caused suppression of the FOXM1
downstream signaling pathways of the cell cycle and apoptotic
induction. In addition, we found that DIM effectively potentiated
the efficacy of chemotherapeutic agent paclitaxel by downregulation
of the Akt/FOXM1 signaling cascade in gastric cancer cells.
Therefore, our results suggest that DIM enhances the therapeutic
efficacy of paclitaxel in gastric cancer and is a potential
clinical anticancer agent for prevention and/or treatment of
gastric cancer.
DIM, a non-toxic dietary chemopreventive agent, has
been investigated for preventing, inhibiting and reversing the
progression of various types of cancer (32). Many studies have suggested that DIM
is strongly associated with tumor growth suppression mediated by
several signaling pathways in human carcinomas (9,17–20,24,32).
We found that DIM significantly inhibited gastric cancer cell
growth in a dose-dependent manner and potentiated the antitumor
effects of paclitaxel in gastric cancer cells. Colony formation was
also significantly attenuated by treatment of SNU638 cells with DIM
and paclitaxel, and DIM notably potentiated paclitaxel’s colony
formation inhibition in SNU638 cells compared to treatment with a
single agent. In addition, treatment with DIM plus paclitaxel
significantly increased apoptosis as indicated by increased levels
of cleaved PARP and caspase-9 proteins. These observations are
similar to the findings of previous studies demonstrating that DIM
enhances taxotere-induced growth inhibition of breast cancer cells
(24). Therefore, our findings
provide strong evidence in support of the enhancement by DIM of
paclitaxel-induced cell growth inhibition and apoptosis in gastric
cancer cells.
Accumulating evidence shows that activation of FOXM1
is associated with the development of human cancers (33–35).
FOXM1 is a FOX transcription factor that regulates a number of cell
cycle regulators (33,34,36,37).
Several studies have shown that FOXM1 is overexpressed in tumors
including lung, liver and breast cancers and is associated with
prognosis (38–40). In addition, suppression of FOXM1 by
genetic or pharmaceutical approaches significantly inhibited the
proliferation and migration of cancers in in vitro and in
vivo studies (41–44). FOXM1 is highly expressed in gastric
tumor tissue compared to normal gastric epithelium and is
associated with the prognosis of gastric cancer patients (27). In addition, Qian et al
demonstrated that FOXM1 promotes gastric cancer cell proliferation
through activation of twist 1 (45). FOXM1 was shown to be overexpressed
in human gastric cancers in previously published studies (27,45),
thus it appears to be an attractive potential target for prevention
and therapeutic intervention in gastric cancer. It is of interest
to examine how DIM effects FOXM1 regulation in gastric cancer
cells. We found that DIM sensitized gastric cancer cells through
dose-dependent downregulation of FOXM1 and potentiated the effects
of paclitaxel, which significantly suppressed FOXM1 expression in
gastric cancer cells. FOXM1 and its effector genes, CDK4, p53 and
cyclin D1, were significantly downregulated in the gastric cancer
cells by combination treatment with DIM and paclitaxel. Our results
confirm the hypothesis that inactivation of FOXM1 is one of the
molecular methods by which drug combinations potentiate cell cycle
arrest and inhibition of proliferation of gastric cancer cells.
Since FOXM1 is a downstream gene in the Akt
signaling pathway that modulates cell survival and metastasis
(22,23), we examined whether DIM affects the
Akt signaling pathway that is associated with FOXM1 in gastric
cancer cells. DIM significantly and dose-dependently inhibited
phosphorylation of Akt, which is the active form of Akt and
significantly increased phosphorylation of GSK-3β with paclitaxel
in gastric cancer cells. DIM significantly potentiated
paclitaxel-induced inhibition of Akt function and induced
activation of GSK-3β in gastric cancer cells. In agreement with our
findings concerning gastric cancer cells, studies have demonstrated
that DIM modulates PI3K/Akt signaling, which induces cell cycle
arrest and apoptosis in various types of cancers (19,32,46–48).
Other studies have shown that FOXM1 is regulated by FOXO3a, a
downstream gene in the PI3K/Akt/FOXO signaling pathway (22,49).
When PI3K/Akt signaling is activated, FOXO3a is inactivated and
does not suppress expression of FOXM1. Although we did not measure
FOXO3a expression, we assume that DIM inhibits activation of Akt
signaling, which leads to increased accumulation of FOXO3a. Thus,
increased FOXO3a may inhibit FOXM1 expression in gastric cancer
cells. Therefore, our findings suggest that inactivation of Akt by
DIM promotes inhibition of FOXM1 expression, further potentiating
paclitaxel-induced inactivation of Akt and FOXM1 in gastric cancer
cells. However, the underlying mechanisms by which Akt mediates
FOXO3a and FOXM1 by DIM in the nucleus and cytosol need to be
further explored.
In conclusion, we demonstrated the molecular
mechanism by which DIM suppresses gastric cancer cell growth by
inhibition of FOXM1 function via the Akt signaling pathway.
Combination treatment with DIM and paclitaxel is a potential
strategy for treating gastric cancer patients, although further
in-depth studies and testing of combinations of these two drugs are
required to support this therapy for gastric cancer.
Acknowledgements
This study was supported by a National Research
Foundation of Korea (NRF) grant funded by the Korean government
(MISP) (no. 2008-0062279).
References
|
1
|
do Pinheiro DR, Ferreira WA, Barros MB,
Araújo MD, Rodrigues-Antunes S and do Borges BN: Perspectives on
new biomarkers in gastric cancer: diagnostic and prognostic
applications. World J Gastroenterol. 20:11574–11585. 2014.
View Article : Google Scholar
|
|
2
|
Parkin DM, Bray F, Ferlay J and Pisani P:
Global cancer statistics, 2002. CA Cancer J Clin. 55:74–108. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cho JY, Lim JY, Cheong JH, et al: Gene
expression signature-based prognostic risk score in gastric cancer.
Clin Cancer Res. 17:1850–1857. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ahn HS, Jeong SH, Son YG, et al: Effect of
neoadjuvant chemotherapy on postoperative morbidity and mortality
in patients with locally advanced gastric cancer. Br J Surg.
101:1560–1565. 2014. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ahn HS, Lee HJ, Hahn S, et al: Evaluation
of the seventh American Joint Committee on Cancer/International
Union Against Cancer Classification of gastric adenocarcinoma in
comparison with the sixth classification. Cancer. 116:5592–5598.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wittekind C, Compton CC, Greene FL and
Sobin LH: TNM residual tumor classification revisited. Cancer.
94:2511–2516. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Edge SB and Compton CC: The American Joint
Committee on Cancer: the 7th edition of the AJCC Cancer Staging
Manual and the future of TNM. Ann Surg Oncol. 17:1471–1474. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Louis P, Hold GL and Flint HJ: The gut
microbiota, bacterial metabolites and colorectal cancer. Nat Rev
Microbiol. 12:661–672. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kong D, Li Y, Wang Z, Banerjee S and
Sarkar FH: Inhibition of angiogenesis and invasion by
3,3′-diindolylmethane is mediated by the nuclear factor-κB
downstream target genes MMP-9 and uPA that regulated
bioavailability of vascular endothelial growth factor in prostate
cancer. Cancer Res. 67:3310–3319. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kristal AR and Lampe JW: Brassica
vegetables and prostate cancer risk: a review of the
epidemiological evidence. Nutr Cancer. 42:1–9. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kim J, Cho YA, Choi WJ and Jeong SH:
Gene-diet interactions in gastric cancer risk: a systematic review.
World J Gastroenterol. 20:9600–9610. 2014.PubMed/NCBI
|
|
12
|
Turati F, Pelucchi C, Guercio V, La
Vecchia C and Galeone C: Allium vegetable intake and gastric
cancer: a case-control study and meta-analysis. Mol Nutr Food Res.
Sep 12–2014.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wu QJ, Xie L, Zheng W, et al: Cruciferous
vegetables consumption and the risk of female lung cancer: a
prospective study and a meta-analysis. Ann Oncol. 24:1918–1924.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wu QJ, Yang Y, Vogtmann E, et al:
Cruciferous vegetables intake and the risk of colorectal cancer: a
meta-analysis of observational studies. Ann Oncol. 24:1079–1087.
2013. View Article : Google Scholar :
|
|
15
|
Wu QJ, Yang Y, Wang J, Han LH and Xiang
YB: Cruciferous vegetable consumption and gastric cancer risk: a
meta-analysis of epidemiological studies. Cancer Sci.
104:1067–1073. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Guercio V, Galeone C, Turati F and La
Vecchia C: Gastric cancer and allium vegetable intake: a critical
review of the experimental and epidemiologic evidence. Nutr Cancer.
66:757–773. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li XJ, Park ES, Park MH and Kim SM:
3,3′-Diindolylmethane suppresses the growth of gastric cancer cells
via activation of the Hippo signaling pathway. Oncol Rep.
30:2419–2426. 2013.PubMed/NCBI
|
|
18
|
Saati GE and Archer MC: Inhibition of
fatty acid synthase and Sp1 expression by 3,3′-diindolylmethane in
human breast cancer cells. Nutr Cancer. 63:790–794. 2011.
View Article : Google Scholar
|
|
19
|
Li XJ, Leem SH, Park MH and Kim SM:
Regulation of YAP through an Akt-dependent process by 3,
3′-diindolylmethane in human colon cancer cells. Int J Oncol.
43:1992–1998. 2013.PubMed/NCBI
|
|
20
|
Kim SJ, Lee JS and Kim SM:
3,3′-Diindolylmethane suppresses growth of human esophageal
squamous cancer cells by G1 cell cycle arrest. Oncol Rep.
27:1669–1673. 2012.PubMed/NCBI
|
|
21
|
Yin XF, Chen J, Mao W, Wang YH and Chen
MH: A selective aryl hydrocarbon receptor modulator
3,3′-diindolylmethane inhibits gastric cancer cell growth. J Exp
Clin Cancer Res. 31:462012. View Article : Google Scholar
|
|
22
|
Wilson MS, Brosens JJ, Schwenen HD and Lam
EW: FOXO and FOXM1 in cancer: the FOXO-FOXM1 axis shapes the
outcome of cancer chemotherapy. Curr Drug Targets. 12:1256–1266.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yung MM, Chan DW, Liu VW, Yao KM and Ngan
HY: Activation of AMPK inhibits cervical cancer cell growth through
AKT/FOXO3a/FOXM1 signaling cascade. BMC Cancer. 13:3272013.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ahmad A, Ali S, Wang Z, et al:
3,3′-Diindolylmethane enhances taxotere-induced growth inhibition
of breast cancer cells through downregulation of FoxM1. Int J
Cancer. 129:1781–1791. 2011. View Article : Google Scholar
|
|
25
|
Adami GR and Ye H: Future roles for FoxM1
inhibitors in cancer treatments. Future Oncol. 3:1–3. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Li X, Qiu W, Liu B, et al: Forkhead box
transcription factor 1 expression in gastric cancer: FOXM1 is a
poor prognostic factor and mediates resistance to docetaxel. J
Transl Med. 11:2042013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Li X, Qi W, Yao R, Tang D and Liang J:
Overexpressed transcription factor FOXM1 is a potential diagnostic
and adverse prognostic factor in postoperational gastric cancer
patients. Clin Transl Oncol. 16:307–314. 2014. View Article : Google Scholar
|
|
28
|
Okada K, Fujiwara Y, Takahashi T, et al:
Overexpression of forkhead box M1 transcription factor (FOXM1) is a
potential prognostic marker and enhances chemoresistance for
docetaxel in gastric cancer. Ann Surg Oncol. 20:1035–1043. 2013.
View Article : Google Scholar
|
|
29
|
Zeng J, Wang L, Li Q, et al: FoxM1 is
up-regulated in gastric cancer and its inhibition leads to cellular
senescence, partially dependent on p27kip1. J Pathol.
218:419–427. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ye S, Lee KB, Park MH, Lee JS and Kim SM:
p63 regulates growth of esophageal squamous carcinoma cells via the
Akt signaling pathway. Int J Oncol. 44:2153–2159. 2014.PubMed/NCBI
|
|
31
|
Lee HH, Ye S, Li XJ, Lee KB, Park MH and
Kim SM: Combination treatment with paclitaxel and doxorubicin
inhibits growth of human esophageal squamous cancer cells by
inactivation of Akt. Oncol Rep. 31:183–188. 2014.
|
|
32
|
Banerjee S, Kong D, Wang Z, Bao B, Hillman
GG and Sarkar FH: Attenuation of multi-targeted
proliferation-linked signaling by 3,3′-diindolylmethane (DIM): from
bench to clinic. Mutat Res. 728:47–66. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Yu J, Deshmukh H, Payton JE, et al:
Array-based comparative genomic hybridization identifies CDK4 and
FOXM1 alterations as independent predictors of survival in
malignant peripheral nerve sheath tumor. Clin Cancer Res.
17:1924–1934. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Raychaudhuri P and Park HJ: FoxM1: a
master regulator of tumor metastasis. Cancer Res. 71:4329–4333.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Dai B, Kang SH, Gong W, et al: Aberrant
FoxM1B expression increases matrix metalloproteinase-2
transcription and enhances the invasion of glioma cells. Oncogene.
26:6212–6219. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Wang Z, Park HJ, Carr JR, et al: FoxM1 in
tumorigenicity of the neuroblastoma cells and renewal of the neural
progenitors. Cancer Res. 71:4292–4302. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Sun H, Teng M, Liu J, et al: FOXM1
expression predicts the prognosis in hepatocellular carcinoma
patients after orthotopic liver transplantation combined with the
Milan criteria. Cancer Lett. 306:214–222. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Xu N, Jia D, Chen W, et al: FoxM1 is
associated with poor prognosis of non-small cell lung cancer
patients through promoting tumor metastasis. PLoS One.
8:e594122013. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Qu K, Xu X, Liu C, et al: Negative
regulation of transcription factor FoxM1 by p53 enhances
oxaliplatin-induced senescence in hepatocellular carcinoma. Cancer
Lett. 331:105–114. 2013. View Article : Google Scholar
|
|
40
|
Kalin TV, Wang IC, Ackerson TJ, et al:
Increased levels of the FoxM1 transcription factor accelerate
development and progression of prostate carcinomas in both TRAMP
and LADY transgenic mice. Cancer Res. 66:1712–1720. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Chan DW, Yu SY, Chiu PM, et al:
Over-expression of FOXM1 transcription factor is associated with
cervical cancer progression and pathogenesis. J Pathol.
215:245–252. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Lok GT, Chan DW, Liu VW, et al: Aberrant
activation of ERK/FOXM1 signaling cascade triggers the cell
migration/invasion in ovarian cancer cells. PLoS One. 6:e237902011.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Chan DW, Hui WW, Cai PC, et al: Targeting
GRB7/ERK/FOXM1 signaling pathway impairs aggressiveness of ovarian
cancer cells. PLoS One. 7:e525782012. View Article : Google Scholar
|
|
44
|
Ahmad A, Wang Z, Kong D, et al: FoxM1
down-regulation leads to inhibition of proliferation, migration and
invasion of breast cancer cells through the modulation of
extra-cellular matrix degrading factors. Breast Cancer Res Treat.
122:337–346. 2010. View Article : Google Scholar
|
|
45
|
Qian J, Luo Y, Gu X, Zhan W and Wang X:
Twist1 promotes gastric cancer cell proliferation through
up-regulation of FoxM1. PLoS One. 8:e776252013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Gao N, Cheng S, Budhraja A, et al:
3,3′-Diindolylmethane exhibits antileukemic activity in vitro and
in vivo through a Akt-dependent process. PLoS One. 7:e317832012.
View Article : Google Scholar
|
|
47
|
Weng JR, Bai LY, Chiu CF, Wang YC and Tsai
MH: The dietary phytochemical 3,3′-diindolylmethane induces G2/M
arrest and apoptosis in oral squamous cell carcinoma by modulating
Akt-NF-κB, MAPK, and p53 signaling. Chem Biol Interact.
195:224–230. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Ahmad A, Biersack B, Li Y, et al: Targeted
regulation of PI3K/Akt/mTOR/NF-κB signaling by indole compounds and
their derivatives: mechanistic details and biological implications
for cancer therapy. Anticancer Agents Med Chem. 13:1002–1013. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Zhao F and Lam EW: Role of the forkhead
transcription factor FOXO-FOXM1 axis in cancer and drug resistance.
Front Med. 6:376–380. 2012. View Article : Google Scholar : PubMed/NCBI
|