Introduction
Hypopharyngeal squamous cell carcinoma (HSCC)
accounts for ~5–15% (1,2) of all head and neck cancers. This
neoplasm occurs most commonly in the pyriform sinus, followed by
the posterior wall of the hypopharynx; it occurs less commonly in
the postcricoid region (3). Smoking
cigarettes and drinking alcohol are the main risk factors for HSCC
(4). HSCC is the most aggressive
head and neck cancer and has the worst prognosis (5). Treating HSCC is one of the most
formidable challenges in the care of patients diagnosed with
malignancies (1). Even though
surgical resection, radiotherapy and neoadjuvant chemotherapy have
continuously improved over the past few decades, HSCC patients
remain exceedingly vulnerable to disease relapse and death
(6,7), and the 5-year survival rate remains no
higher than 40% (5).
Because of the close proximity of anatomical
structures of HSCC tumors, reconstruction of the upper digestive
tract and larynx after HSCC resection is a difficult problem. It is
important to offer a safe single-stage reconstruction with low
morbidity and mortality, as well as good functional rehabilitation
(8). Since 1978, curative
hypopharyngectomy with laryngeal function (LF) preservation and
reconstruction has been used at our institution to maintain
deglutition, respiration, and speech function as well as improve
quality of life (QOL). In the present study, we retrospectively
reviewed the oncologic and functional outcomes of 580 patients with
HSCC who were treated at our institution over 15 years and compared
the survival of patients with or without LF preservation.
Materials and methods
Patients and data
We retrospectively searched and reviewed the patient
database of the Department of Otolaryngology, Qilu Hospital of
Shandong University, Jinan, China, and identified patients with
HSCC who were surgically treated from January 1996 to December
2010. A total of 580 patients with biopsy-proven squamous cell
carcinoma with or without local lymph node metastases were eligible
for the study. We recorded and analyzed the following data: patient
and tumor characteristics, diagnosis and disease stage, excision
and reconstruction methods, adjuvant treatment, swallowing
outcomes, respiration, and speech function, complications, and
survival. All patients signed written informed consent, and this
consent procedure was approved by the Institutional Review Board
(IRB) of the Ethics Boards of Qilu Hospital and the study followed
the Declaration of Helsinki.
Treatment summary
All patients were treated as follows. The
preoperative workup included a barium esophagogram, endoscopic
examination and biopsy, enhanced cervical computed tomography (CT)
and full blood count with routine serum chemistry. Tumor staging
was in accordance with the International Union against Cancer
(UICC, 2002) TNM classification. None of the patients received any
preoperative treatment.
Surgical procedures were performed as described
previously by us (3,8–12).
Briefly, the thyroid cartilage cornu superius approach was chosen
for primary lesions located in the pyriform sinus. The epiglottic
vallecular cervical esophageal approach was chosen when the
patients had advanced pyriform sinus carcinoma. The thyroid
cartilage cornu superius and hyoid bone approaches were used to
resect primary lesions located in the posterior wall of the
hypopharynx. The thyrohyoid membrane and pyriform sinus approaches
were chosen to resect postcricoid area carcinoma. A tumor margin of
≥1.5 cm was considered optimal. If the esophagus was invaded, the
optimal distance between the tumor and the esophageal incisal edge
was >3 cm. Among the patients with LF preservation, epiglottal
tissue, sternohyoid myofascial flaps, thyroid perichondrium, or
platysma myocutaneous flaps were most commonly used to reconstruct
the larynx. Local skin flaps, pectoralis major musculocutaneous
flaps, laryngotracheal flaps, stomach or colon relocation was used
to reconstruct the hypopharyngoesophagus. All patients underwent
neck dissection. If the primary carcinoma invaded the midline of
the pharynx or a clear diagnosis of contralateral lymph node
metastasis was confirmed by physical examination or imaging
presurgically, a bilateral neck dissection was performed.
All 580 patients received adjuvant radiotherapy for
20 days to 2 months after surgery. The dosage of the postoperative
radiation was 50–60 Gy in 478 cases and 75 Gy in the other 102
cases who had advanced cancer or extra-capsular invasion of lymph
nodes.
Follow-up
Follow-up data were obtained by phone, letter and
the outpatient clinical database. Medical record review to
determine the follow-up status of all patients was performed under
the direct supervision of the staff head and neck surgeon. All
patients were subjected to close follow-up observation every 3
months for the first year, and every 6 months thereafter. The
primary endpoint in this study was overall survival (OS), which was
defined as the time from first diagnosis to death or last
follow-up. The time of follow-up was completely followed up for
>5 years. Participants who were alive at the end of the study
period or lost to follow-up were considered censored.
Statistical analysis
SPSS 17.0 (SPSS Inc., Chicago, IL, USA) statistical
software was used for the analyses. The association between
categorical variables was analyzed using Pearson Chi-square tests
or continuous correction Chi-square tests as appropriate. OS curves
were drawn using the Kaplan-Meier method, and the differences
between the survival curves were examined using the log-rank test.
Cox univariate and multivariate analyses were performed to explore
the influences of prognostic factors on OS time. The significant
variables in the univariate analyses (P<0.05) were then put into
the multivariate analysis. Hazard ratios (HRs) with 95% confidence
intervals (CIs) were measured to estimate the hazard of death for
the individual factors. In all analyses, a two-sided P<0.05 was
considered to indicate a statistically significant difference.
Results
Patient clinicopathological and demographic data are
shown in Table I. In summary, the
study cohort mainly consisted of male patients (526, 90.7%), with a
median age of 59.0 years (range, 26–82 years). All the tumors
originated from the pyriform sinus (452, 77.9%), posterior
pharyngeal wall (97, 16.7%), and postcricoid area (31, 5.4%) and
most patients had advanced T-stage disease (T3–T4, 65.2%), lymph
node metastasis (81.7%), and advanced clinical stage disease (stage
III and IV, 89.2%). There were no cases of distant metastasis.
Pathological studies confirmed that 114 cases (19.7%) were well
differentiated, 242 cases (41.7%) were moderately differentiated
and 224 cases (38.6%) were poorly differentiated.
 | Table IPatient clinicopathological
information and demographic data (n=580). |
Table I
Patient clinicopathological
information and demographic data (n=580).
| Variables | No. (%) |
|---|
| Age at presentation
(years) | |
| Median | 59.0 |
| Range | 26–82 |
| Gender | |
| Female | 54 (9.3) |
| Male | 526 (90.7) |
| Primary location | |
| Pyriform sinus | 452 (77.9) |
| Posterior pharyngeal
wall | 97 (16.7) |
| Postcricoid
area | 31 (5.4) |
| T category | |
| T1 | 73 (12.6) |
| T2 | 129 (22.2) |
| T3 | 207 (35.7) |
| T4 | 171 (29.5) |
| Node metastasis | |
| N0 | 106 (18.3) |
| N1 | 282 (48.6) |
| N2 | 160 (27.6) |
| N3 | 32 (5.5) |
| M category | |
| M0 | 580 (100.0) |
| M1 | 0 (0.0) |
| Clinical stage | |
| I | 32 (5.5) |
| II | 31 (5.3) |
| III | 236 (40.7) |
| IV | 281 (48.5) |
| Histologic
differentiation | |
| Well | 114 (19.7) |
| Moderate | 242 (41.7) |
| Poor | 224 (38.6) |
| Treatment | |
| Surgery plus
radiotherapy | 580 (100.0) |
| Death | |
| Yes | 393 (67.8) |
| No | 159 (27.4) |
| Lost to
follow-up | 28 (4.8) |
LF was preserved in 403 cases and not preserved in
177 cases. All the patients underwent modified neck dissection,
including both unilateral (412 patients) and bilateral (168
patients) dissections. As shown in Table II, pharyngoesophageal defect
reconstruction methods in cases with LF preserved were as follows:
direct suture in 262 patients, pectoralis major musculocutaneous
flap in 77, split graft in 4, pectoralis major musculocutaneous
flap combined with the split graft in 7, stomach pulling-up in 17,
and colon interposition in 36 patients. In cases without LF
preservation the methods included: direct suture in 51 patients,
pectoralis major musculocutaneous flap in 11, laryngotracheal flap
in 62, laryngotracheal flap combined with pectoralis major
musculocutaneous flap in 12, stomach reposition in 37 and colon
interposition in 4 patients. Among the 403 cases with LF
preservation, 122 cases did not need laryngeal reconstruction since
the laryngeal integrity was maintained; the other 281 cases were
reconstructed using the epiglottis (170 cases), sternohyoid
myofascial flap (48 cases), thyroid perichondrium (42 cases), or
platysma myocutaneous flap (21 cases). Laryngeal functions (voice,
respiration and deglutition) were completely restored in 286
(71.0%) patients and partially restored (voice and deglutition) in
117 (29.0%) patients.
 | Table IIPharyngoesophageal defect
reconstruction methods in cases with and without LF preservation
(n=580). |
Table II
Pharyngoesophageal defect
reconstruction methods in cases with and without LF preservation
(n=580).
| Methods | Patient no. (LF
preserved)
| Total | Patient no. (LF not
preserved)
| Total |
|---|
| Pyriform sinus | Posterior pharyngeal
wall | Postcricoid area | Pyriform sinus | Posterior pharyngeal
wall | Postcricoid area |
|---|
| Direct suture | 234 | 23 | 5 | 262 | 51 | – | – | 51 |
| PMMF | 65 | 12 | – | 77 | 11 | – | – | 11 |
| Split graft | – | 4 | – | 4 | – | – | – | – |
| PMMF + split
graft | – | 7 | – | 7 | – | – | – | – |
| Laryngotracheal
flap | – | – | – | – | 30 | 18 | 14 | 62 |
| PMMF +
laryngotracheal flap | – | – | – | – | 7 | 5 | | 12 |
| Stomach
pulling-up | 17 | – | – | 17 | 19 | 11 | 7 | 37 |
| Colon
interposition | 22 | 9 | 5 | 36 | – | 4 | – | 4 |
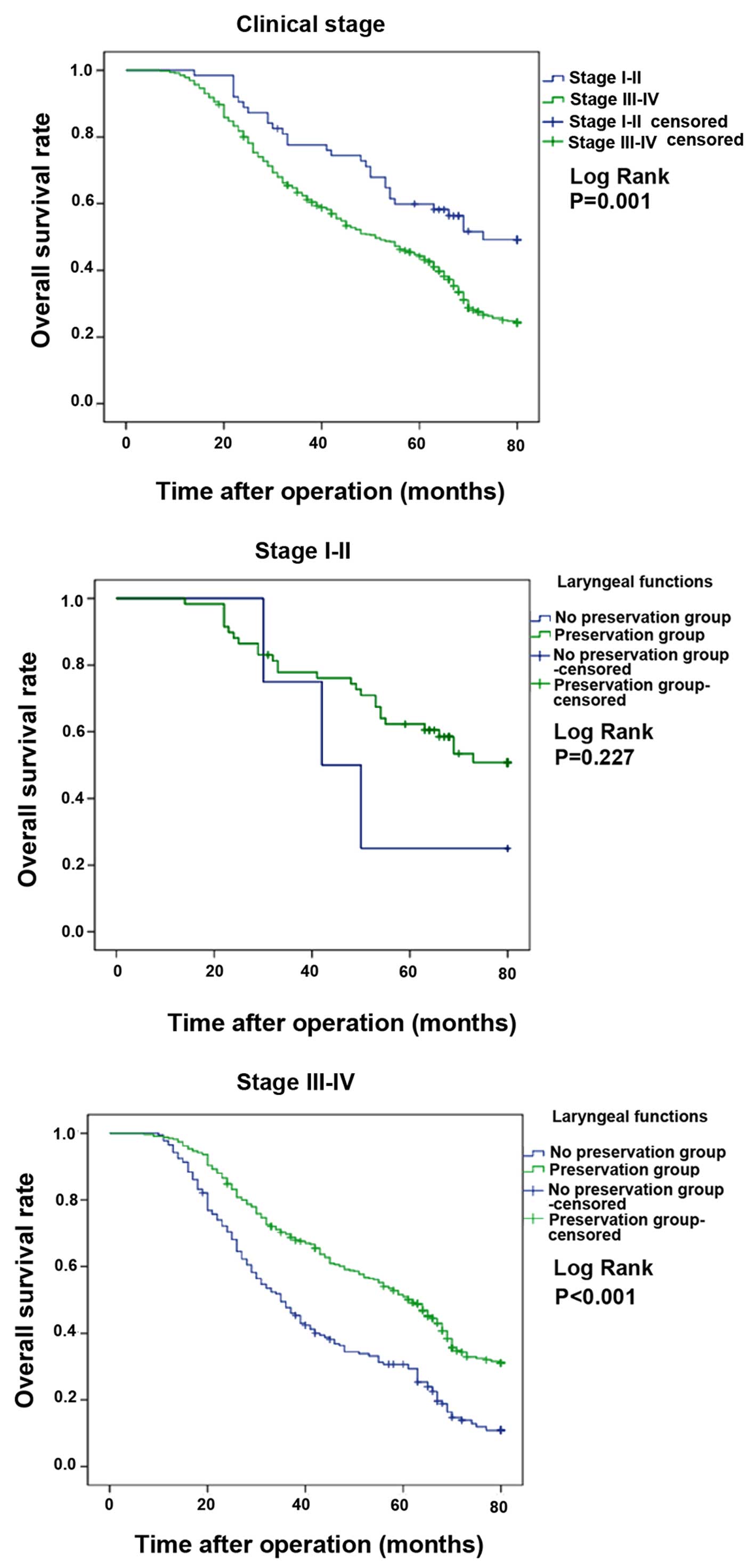
There were significant statistical differences
between the LF preservation group and the group without LF
preservation in regards to T stage (P<0.001), N stage (P=0.046),
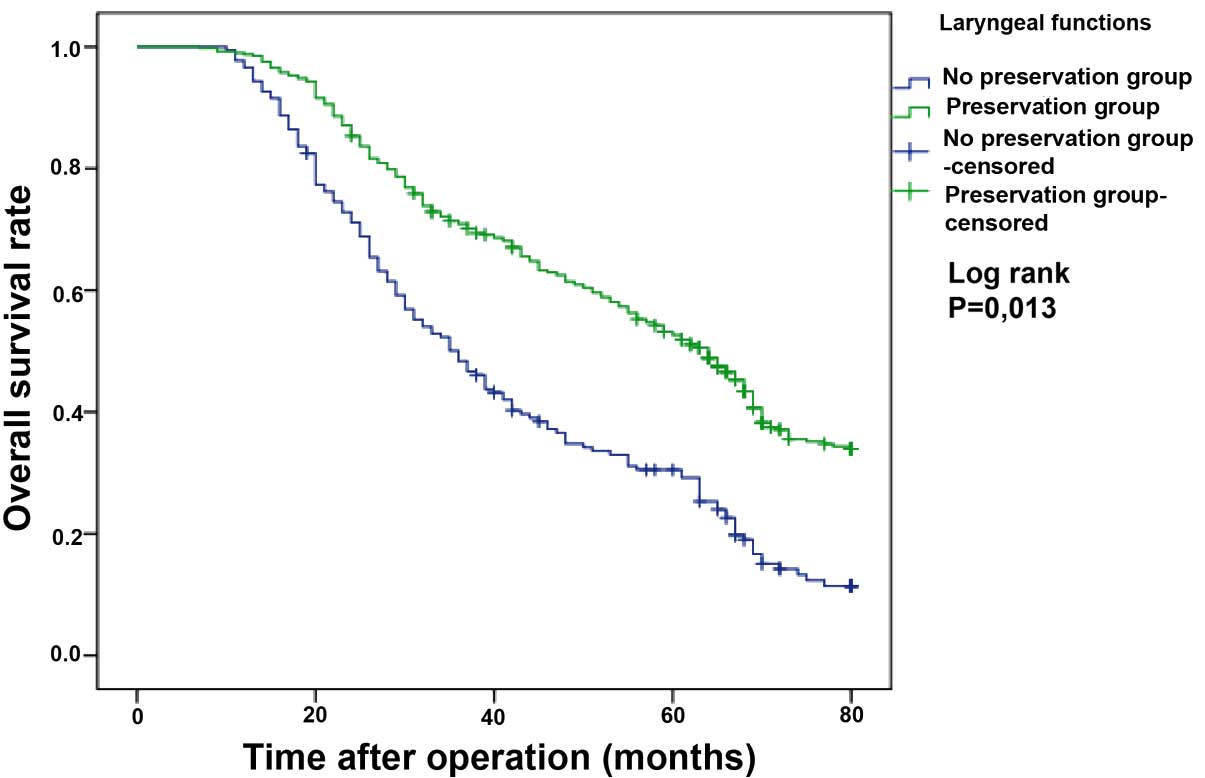
clinical stage (P<0.001) and tumor site (P<0.001) (Table III). The overall 3- and 5-year OS
rates were 64.0 and 45.9%, respectively. The 3- and 5-year OS rates
in the LF preservation group were 70.9 and 52.7%, respectively,
while in the group without LF preservation, the 3- and 5-year OS
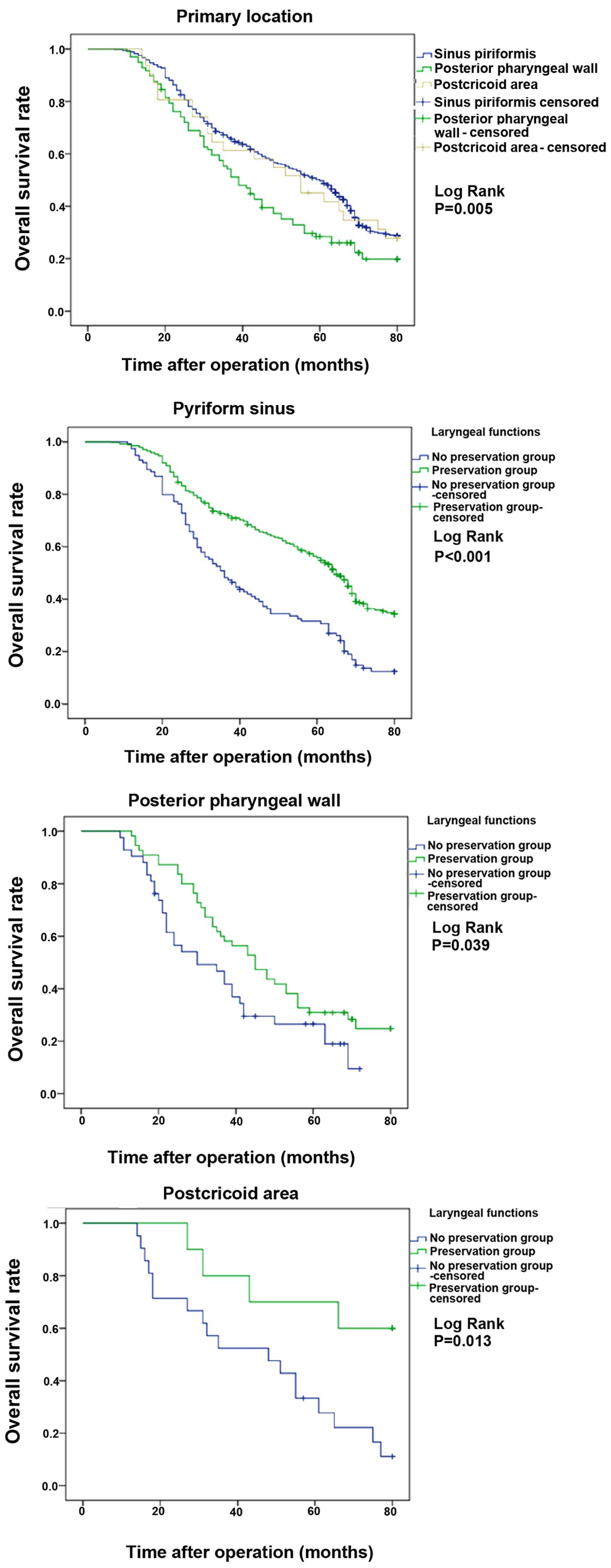
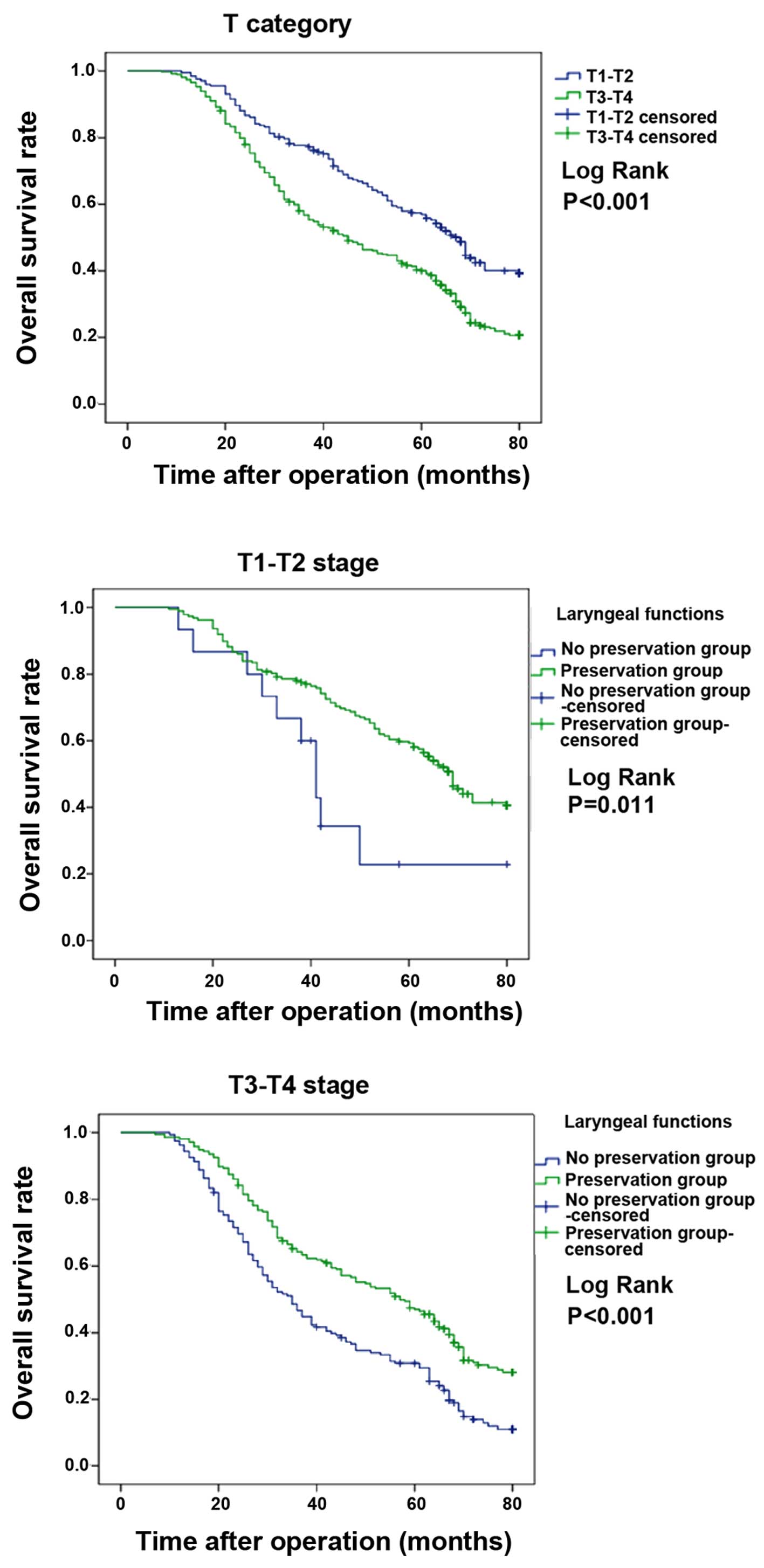
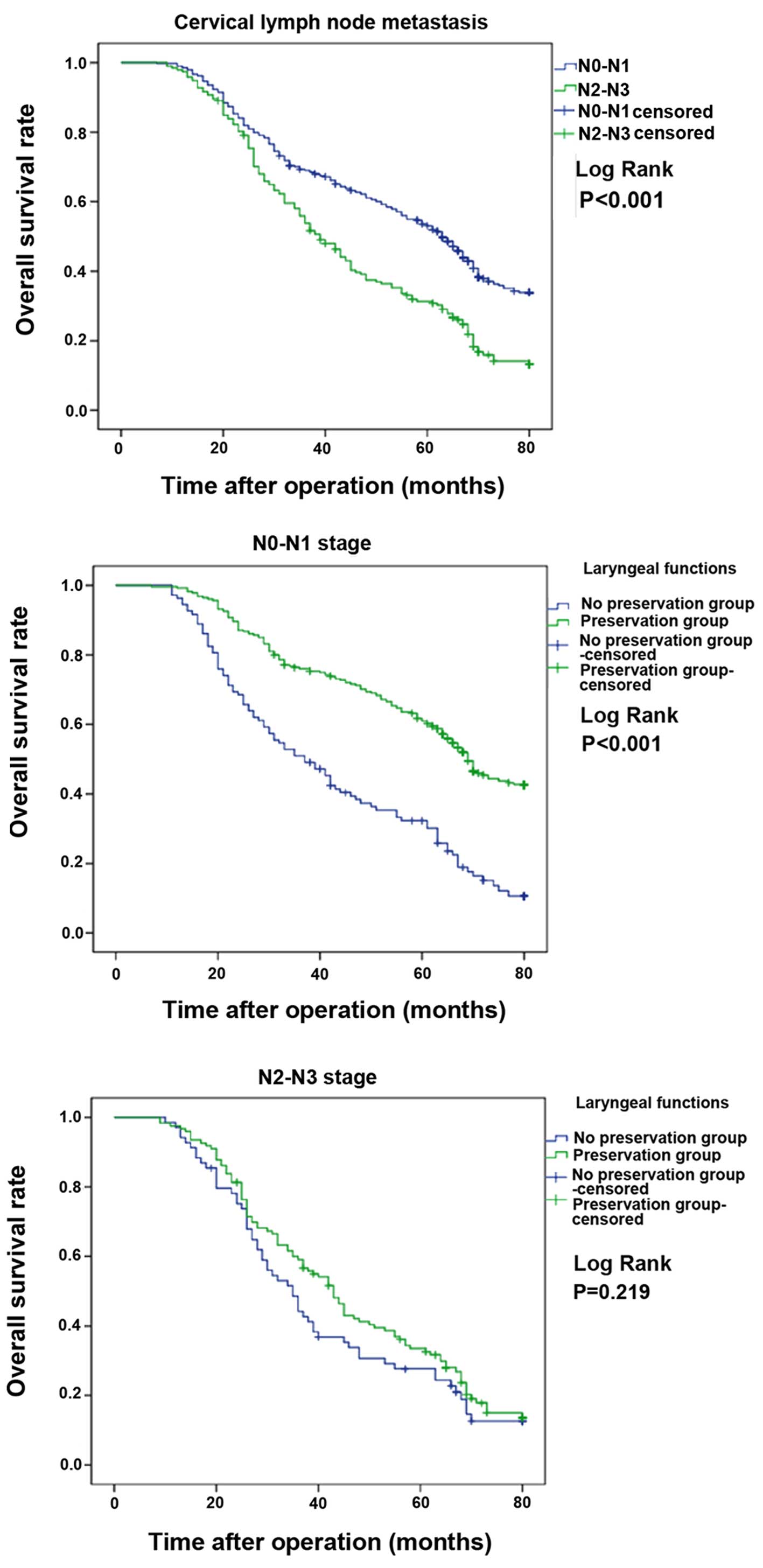
rates were 48.4 and 30.5%, respectively (Fig. 1). OS rates according to tumor site
(Fig. 2), T stage (Fig. 3), lymph node metastasis (Fig. 4) and clinical stage (Fig. 5) among patients with and without LF
preservation are shown in Table
IV.
 | Table IIIClinical characteristics of the
patients with and without LF preservation (n=580). |
Table III
Clinical characteristics of the
patients with and without LF preservation (n=580).
| Characteristics | Total | Patients (LF
preserved) n (%) | Patients (LF not
preserved) n (%) | P-value |
|---|
| T category | | | | |
| T1–T2 | 202 | 187 (92.6) | 15 (7.4) | <0.001a |
| T3–T4 | 378 | 216 (57.1) | 162 (42.9) | |
| Node metastasis | | | | |
| N0–N1 | 388 | 280 (72.2) | 108 (27.8) | 0.046a |
| N2–N3 | 192 | 123 (64.1) | 69 (35.9) | |
| Clinical stage | | | | |
| I–II | 63 | 59 (93.7) | 4 (6.3) | <0.001a |
| III–IV | 517 | 344 (66.5) | 173 (33.5) | |
| Primary
location | | | | |
| Pyriform
sinus | 452 | 338 (74.8) | 114 (25.2) | <0.001a |
| Posterior
pharyngeal wall | 97 | 55 (56.7) | 42 (43.3) | |
| Postcricoid
area | 31 | 10 (32.3) | 21 (67.7) | |
 | Table IVOverall survival rates according to
tumor site, T stage, lymph node metastasis, and clinical stage
among the patients with and without LF preservation (n=580). |
Table IV
Overall survival rates according to
tumor site, T stage, lymph node metastasis, and clinical stage
among the patients with and without LF preservation (n=580).
| Variables | 3-year survival
rate (%)
| Total | 5-year survival
rate (%)
| Total |
|---|
| LF preserved | LF not
preserved | LF preserved | LF not
preserved |
|---|
| Primary
location | | | | | | |
| Pyriform
sinus | 72.4 | 48.2 | 66.3 | 55.8 | 31.7 | 49.7 |
| Posterior
pharyngeal wall | 60.0 | 46.7 | 54.3 | 30.9 | 26.5 | 28.5 |
| Postcricoid
area | 80.0 | 52.4 | 61.3 | 70.0 | 33.3 | 45.2 |
| T category | | | | | | |
| T1–T2 | 78.6 | 66.7 | 77.7 | 59.2 | 22.9 | 56.9 |
| T3–T4 | 64.2 | 46.6 | 56.7 | 47.0 | 30.8 | 40.0 |
| Node
metastasis | | | | | | |
| N0–N1 | 76.0 | 50.9 | 69.0 | 61.0 | 32.3 | 53.0 |
| N2–N3 | 59.1 | 44.2 | 53.8 | 33.5 | 27.6 | 31.4 |
| Clinical stage | | | | | | |
| I–II | 77.9 | 75.0 | 77.7 | 62.3 | 25.0 | 59.9 |
| III–IV | 69.7 | 47.7 | 62.4 | 51.0 | 30.7 | 44.2 |
Multivariable Cox proportional hazards regression
analysis was performed to evaluate the association between LF
preservation and overall risk of death in the patients with HSCC.
The adjusted confounders were T stage, N stage, clinical stage,
differentiation and treatment. As shown in Table V, compared with the patients without
LF preservation, patients with LF preservation had a significantly
reduced risk of overall death (HR=0.633, 95% CI: 0.503–0.797).
 | Table VResults of the univariate and
multivariate Cox regression analyses in 580 patients with and
without LF preservation. |
Table V
Results of the univariate and
multivariate Cox regression analyses in 580 patients with and
without LF preservation.
| | Univariate analysis
| Multivariate
analysis
|
|---|
| Parameters | Comparison | HR | 95% CI | P-value | HRa | 95% CI | P-value |
|---|
| Age (years) | <60 vs. ≥60 | 1.12 | 0.92–1.37 | 0.249 | | | |
| Gender | Male vs.
female | 1.37 | 0.99–1.89 | 0.056 | | | |
| T stage | T1–T2 vs.
T3–T4 | 1.71 | 1.37–2.13 | <0.001b | 1.32 | 1.03–1.67 | 0.026b |
| Node
metastasis | N0–N1 vs.
N2–N3 | 1.90 | 1.55–2.33 | <0.001b | 1.62 | 1.31–2.00 | <0.001b |
|
Differentiation | Poor vs. well and
moderate | 1.20 | 1.05–1.37 | 0.007b | 1.15 | 1.00–1.32 | 0.047b |
| Clinical stage | I–II vs.
III–IV | 1.89 | 1.30–2.75 | 0.001b | 1.23 | 0.81–1.87 | 0.331 |
| Treatment | LF not preserved
vs. LF preserved | 0.49 | 0.40–0.61 | <0.001b | 0.63 | 0.50–0.80 | <0.001b |
Discussion
In the present study, we found that patients with LF
preservation had significantly higher OS rates than did patients
without LF preservation, and LF preservation significantly reduced
the risk of overall death. The 3- and 5-year OS rates were 70.9 and
52.7%, respectively, in the LF preservation group and 48.4 and
30.5%, respectively, in the group without LF preservation. Although
LF preservation is often performed in cases of relatively less
advanced tumors, however, as the Cox multivariate analysis
confirmed, LF preservation itself can improve survival. This may be
due to the relatively high QOF after surgery.
LFs (voice, respiration and deglutition) were
completely restored in 286 (71.0%) patients and partially restored
(voice and deglutition) in 117 (29.0%) patients with LF
preservation. The success of organ preservation relies not only on
favorable survival and preservation rates but also on adequate
function of the remaining organ. Before the decision to attempt LF
preservation is made, X-ray barium meal examination, enhanced
cervical CT and laryngoscopy are used to determine the optimal
range of surgery. The complete resection of the tumor and the
preservation of a maximum amount of laryngeal tissue are the key
factors considered when we consider the feasibility of LF
preservation. We think that patients with at least one movable
arytenoid cartilage and a normal contralateral pyriform sinus can
undergo LF preservation. However, during surgery, tumors should be
fully exposed to the naked eye, and it is unwise to reduce the
scope of surgery for the protection of LF. In addition, respiratory
function tests and cardiologic examination are also important. For
elderly or weak patients and those with poor cardiopulmonary
function, LF preservation is unsuitable, even if there is enough
remnant laryngeal tissue. Four patients in the present study,
although with clinical stage I–II disease, were unable to undergo
LF preservation owing to their poor cardiopulmonary function.
The main purpose of reconstruction of LF is to
prevent aspiration after surgery. In our previous study, we
reported several LF reconstruction methods in detail (3): i) if the epiglottis was resected
completely, the tongue flap covered the laryngeal inlet and the
pyriform sinus was capacious to help the food pass the laryngeal
inlet as quickly as possible to avoid aspiration; ii) if the
majority of the supraglottic tissues on the same side as the tumor
were resected, the epiglottis was pulled downward or rotated
outwards in order to suture it with the surgical margin of
subglottic tissues and to re-shape the lateral wall of the residual
larynx; iii) if the edge of the epiglottis was involved by tumor,
the remnant epiglottis was pulled downward to reconstruct the
lateral wall of the laryngeal vestibule and to cover the laryngeal
inlet effectively; iv) because LF preservation in the postcricoid
area is troublesome, if the bilateral arytenoid cartilage is
movable and the interarytenoid notch is not infiltrated, the
carcinoma can be resected completely without total laryngectomy and
v) the sternohyoid myofascial flap, thyroid perichondrium, or
platysma myocutaneous flap could be inverted into the laryngeal
cavity to repair the defects of the larynx.
The most important aspect of pharyngo-esophageal
defect reconstruction is to create/maintain a spacious cavity in
the hypopharynx so that food can pass more quickly and smoothly and
aspiration will be less likely. It is important to deal
appropriately with the laryngeal inlet rather than to rebuild the
affected ipsilateral part of the pyriform sinus. For early stage
tumors, the remnant mucosa can be sutured directly to close the
hypopharyngeal cavity. However, for advanced-stage tumors, if the
excised tissue exceeds the ipsilateral area in the pyriform sinus
and extends to the posterior wall of the hypopharynx, postcricoid
area, or cervical esophagus, reconstruction of the hypopharynx
should involve use of a local skin flap, pectoralis major
musculocutaneous flap, or stomach reposition or colon interposition
with vessel pedicles. In cases with removal of one side of the
lateral wall of the cervical esophagus and tumor involvement
limited to within 3 cm below the inlet of the esophagus, a
pectoralis major musculocutaneous flap is still suitable to repair
the defect. However, the anastomotic orifice should be formed
obliquely to prevent anastomosis from stenosis (13). If the cervical esophagus is involved
more than 3 cm below the inlet of the esophagus, the use of a
pectoralis major musculocutaneous flap is difficult because the
esophageal incisal margin is below the superior aperture of the
thorax. In that case, stomach repositioning or colon tissue
interposition with vessel pedicles is more appropriate in our
experience (12). For elderly or
weak patients and those with poor cardiopulmonary function, LF
preservation is unsuitable. Thus, in those cases, the hypopharynx
can be reconstructed using a laryngotracheal flap.
Pharyngocutaneous fistulas were observed in 34
patients in our study. After postoperative nutrition and wound
dressing were improved, 26 patients healed spontaneously within 4
weeks; 4 patients healed by two-stage suture, and 4 patients
underwent reconstruction with a pectoralis major musculocutaneous
flap. Pharyngocutaneous fistula is the most common complication
occurring after head and neck surgery. It may lead to high surgical
morbidity and mortality rates, prolonged hospital stays, high
hospital costs, and increased emotional distress. It may also
prevent or delay the onset of radiation therapy and patient
rehabilitation. In our experience, the occurrence of
pharyngocutaneous fistula can be prevented by: i) using negative
pressure drainage; ii) ensuring that the remnant mucosa is fixed to
the submucosal tissue and/or posterior part of the ipsilateral
thyroid cartilage, which can prevent suture dehiscence and iii)
reducing the tissue defect lateral to the anastomotic orifice by
using a thyroid gland, unipedicled sternohyoid myofascial, or
unipedicled sternocleidomastoid myofascial flap.
In conclusion, we retrospectively reviewed a series
of 580 HSCC patients who were treated with surgery followed by
radiotherapy at our institution. Although most patients presented
with advanced clinical stage disease, the majority of the patients
could be surgically treated with LF preservation. LF preservation
may affect prognosis and QOL: patients with LF preservation had
significantly better survival and QOL than those without LF
preservation. Although there is disagreement about which
multidisciplinary plan [radiotherapy followed by surgery, surgery
followed by radiotherapy, induction chemotherapy followed by
radiotherapy, or concurrent chemotherapy and radiotherapy (14,15)]
is best for HSCC patients, we recommend the comprehensive use of
surgery and radiotherapy. However, further investigations that take
into account early diagnosis and novel effective therapies are
still needed.
Acknowledgments
The present study was supported by the Taishan
Scholars Program (no. tshw20130950), Shandong and the Department of
Science and Technology of Shandong (nos. ZR2013HM107 and
ZR2014HM005) and Science Foundation of Qilu Hospital of Shandong
University and the Fundamental Research Funds of Shandong
University (no. 2014QLKY05).
References
|
1
|
Bradley PT and Bradley PJ: Treatment of
hypopharyngeal carcinoma with primary chemoradiotherapy: Functional
morbidity. Curr Opin Otolaryngol Head Neck Surg. 20:89–96. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cooper JS, Porter K, Mallin K, Hoffman HT,
Weber RS, Ang KK, Gay EG and Langer CJ: National Cancer Database
report on cancer of the head and neck: 10-year update. Head Neck.
31:748–758. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jin T, Li X, Lei D, Liu D, Yang Q, Li G
and Pan X: Preservation of laryngeal function improves outcomes of
patients with hypopharyngeal carcinoma. Eur Arch Otorhinolaryngol.
272:1785–1791. 2015. View Article : Google Scholar :
|
|
4
|
Zhou L: Standardization of the management
of laryngeal and hypopharyngeal carcinoma. Zhonghua Er Bi Yan Hou
Tou Jing Wai Ke Za Zhi. 44:705–706. 2009.In Chinese.
|
|
5
|
Hall SF, Groome PA, Irish J and O'Sullivan
B: The natural history of patients with squamous cell carcinoma of
the hypopharynx. Laryngoscope. 118:1362–1371. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chan JY and Wei WI: Current management
strategy of hypopharyngeal carcinoma. Auris Nasus Larynx. 40:2–6.
2013. View Article : Google Scholar
|
|
7
|
Takes RP, Strojan P, Silver CE, Bradley
PJ, Haigentz M Jr, Wolf GT, Shaha AR, Hartl DM, Olofsson J,
Langendijk JA, et al International Head and Neck Scientific Group:
Current trends in initial management of hypopharyngeal cancer: The
declining use of open surgery. Head Neck. 34:270–281. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pan XL, Lei DP, Liu DY, Xu FL, Wang HL,
Jin T, Xie G and Luan XY: Comprehensive treatment of 352 cases with
hypopharyngeal cancer. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za
Zhi. 44:710–715. 2009.In Chinese.
|
|
9
|
Li X, Zhang L, Pan X, Xie G, Luan X and
Wang T: Preservation of laryngeal function in surgical treatment of
posterior hypo-pharyngeal wall cancer. Lin Chuang Er Bi Yan Hou Ke
Za Zhi. 19:1109–11. 11152005.In Chinese.
|
|
10
|
Li XZ, Zhang LQ, Pan XL, Xie G, Luan XY
and Wang TD: Preservation of laryngeal function in surgical
treatment of pyriform sinus carcinoma. Zhonghua Er Bi Yan Hou Tou
Jing Wai Ke Za Zhi. 40:212–216. 2005.In Chinese. PubMed/NCBI
|
|
11
|
Li XZ, Zhang LQ, Pan XL, Xie G, Lei DP,
Luan XY and Wang TD: Surgical treatment of postcricoid carcinoma.
Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 40:427–430. 2005.In
Chinese. PubMed/NCBI
|
|
12
|
Lei DP, Pan XL, Xu FL, Liu DY, Zhang LQ,
Li XZ, Xie G and Luan XY: Surgical treatment of hypopharyngeal
cancer with cervical esophageal invasion. Zhonghua Er Bi Yan Hou
Tou Jing Wai Ke Za Zhi. 40:691–695. 2005.In Chinese. PubMed/NCBI
|
|
13
|
Chaturvedi P, Pai PS, Pathak KA, Chaukar
DA, Deshpande MS and D'Cruz AK: Simultaneous reconstruction of
large skin and mucosal defect following head and neck surgery with
a single skin paddle pectoralis major myocutaneous flap. J Laryngol
Otol. 119:303–305. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lefebvre JL, Rolland F, Tesselaar M,
Bardet E, Leemans CR, Geoffrois L, Hupperets P, Barzan L, de
Raucourt D, Chevalier D, et al EORTC Head and Neck Cancer
Cooperative Group; EORTC Radiation Oncology Group: Phase 3
randomized trial on larynx preservation comparing sequential vs
alternating chemotherapy and radiotherapy. J Natl Cancer Inst.
101:142–152. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lefebvre JL, Pointreau Y, Rolland F,
Alfonsi M, Baudoux A, Sire C, de Raucourt D, Malard O, Degardin M,
Tuchais C, et al: Induction chemotherapy followed by either
chemoradiotherapy or bioradiotherapy for larynx preservation: The
TREMPLIN randomized phase II study. J Clin Oncol. 31:853–859. 2013.
View Article : Google Scholar : PubMed/NCBI
|