|
1
|
Yu YL, Chou RH, Liang JH, Chang WJ, Su KJ,
Tseng YJ, Huang WC, Wang SC and Hung MC: Targeting the EGFR/PCNA
signaling suppresses tumor growth of triple-negative breast cancer
cells with cell-penetrating PCNA peptides. PLoS One. 8:e613622013.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Metzger-Filho O, Tutt A, de Azambuja E,
Saini KS, Viale G, Loi S, Bradbury I, Bliss JM, Azim HA Jr, et al:
Dissecting the heterogeneity of triple-negative breast cancer. J
Clin Oncol. 30:1879–1787. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ojo D, Wei F, Liu Y, Wang E, Zhang H, Lin
X, Wong N, Bane A and Tang D: Factors promoting tamoxifen
resistance in breast cancer via stimulating breast cancer stem cell
expansion. Curr Med Chem. 22:2360–2374. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Spring L, Bardia A and Modi S: Targeting
the cyclin D-cyclin-dependent kinase (CDK) 4/6-retinoblastoma
pathway with selective CDK 4/6 inhibitors in hormone
receptor-positive breast cancer: Rationale, current status, and
future directions. Discov Med. 21:65–74. 2016.PubMed/NCBI
|
|
5
|
Lumachi F, Chiara GB, Foltran L and Basso
SM: Proteomics as a guide for personalized adjuvant chemotherapy in
patients with early breast cancer. Cancer Genomics Proteomics.
12:385–390. 2015.PubMed/NCBI
|
|
6
|
Williams CB, Soloff AC, Ethier SP and Yeh
ES: Perspectives on epidermal growth factor receptor regulation in
triple-negative breast cancer: Ligand-mediated mechanisms of
receptor regulation and potential for clinical targeting. Adv
Cancer Res. 127:253–281. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hudis CA and Gianni L: Triple-negative
breast cancer: An unmet medical need. Oncologist. 16:(Suppl 1).
1–11. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Perou CM, Sørlie T, Eisen MB, van de Rijn
M, Jeffrey SS, Rees CA, Pollack JR, Ross DT, Johnsen H, Akslen LA,
et al: Molecular portraits of human breast tumours. Nature.
406:747–752. 2000. View
Article : Google Scholar : PubMed/NCBI
|
|
9
|
Schofield RC, Ramanathan LV, Murata K,
Fleisher M, Pessin MS and Carlow DC: Development of an assay for
methotrexate and its metabolites 7-hydroxy methotrexate and DAMPA
in serum by LC-MS/MS. Methods Mol Biol. 1383:213–222. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hara A, Taguchi A, Aoki H, Hatano Y, Niwa
M, Yamada Y and Kunisada T: Folate antagonist, methotrexate induces
neuronal differentiation of human embryonic stem cells transplanted
into nude mouse retina. Neurosci Lett. 477:138–143. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pavy S, Constantin A, Pham T, Gossec L,
Maillefert JF, Cantagrel A, Combe B, Flipo RM, Goupille P, Le Loët
X, et al: Methotrexate therapy for rheumatoid arthritis: clinical
practice guidelines based on published evidence and expert opinion.
Joint Bone Spine. 73:388–395. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Whittle SL and Hughes RA: Folate
supplementation and methotrexate treatment in rheumatoid arthritis:
A review. Rheumatology (Oxford). 43:267–271. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cho KM, Kim YJ, Kim SH, Kim JW, Lee JO,
Han JH, Lee KW, Kim JH, Kim CY, Bang SM, et al: Salvage treatment
with intracerebrospinal fluid thiotepa in patients with
leptomeningeal metastasis after failure of methotrexate-based
treatment. Anticancer Res. 35:5631–5638. 2015.PubMed/NCBI
|
|
14
|
van der Plas E, Nieman BJ, Butcher DT,
Hitzler JK, Weksberg R, Ito S and Schachar R: Neurocognitive late
effects of chemotherapy in survivors of acute lymphoblastic
leukemia: Focus on methotrexate. J Can Acad Child Adolesc
Psychiatry. 24:25–32. 2015.PubMed/NCBI
|
|
15
|
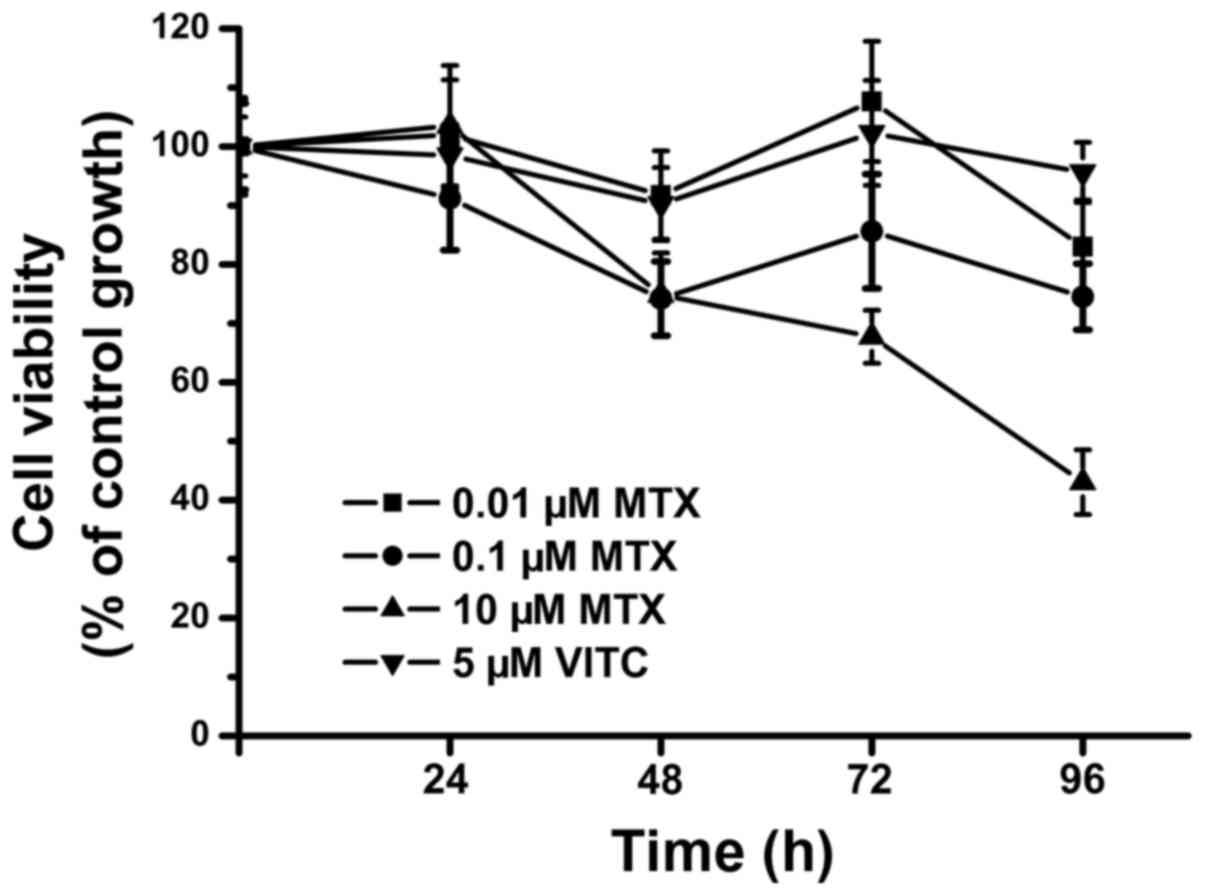
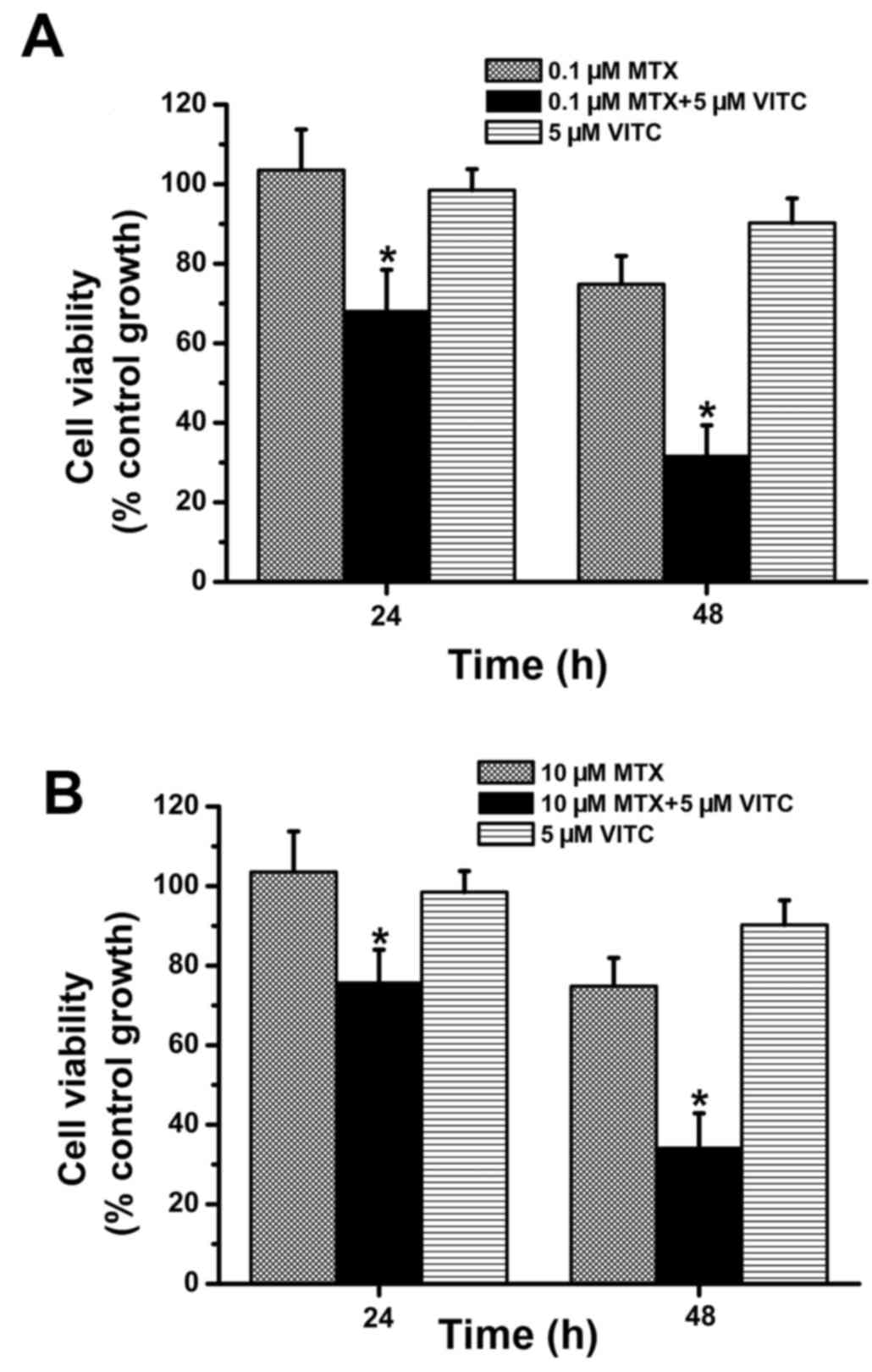
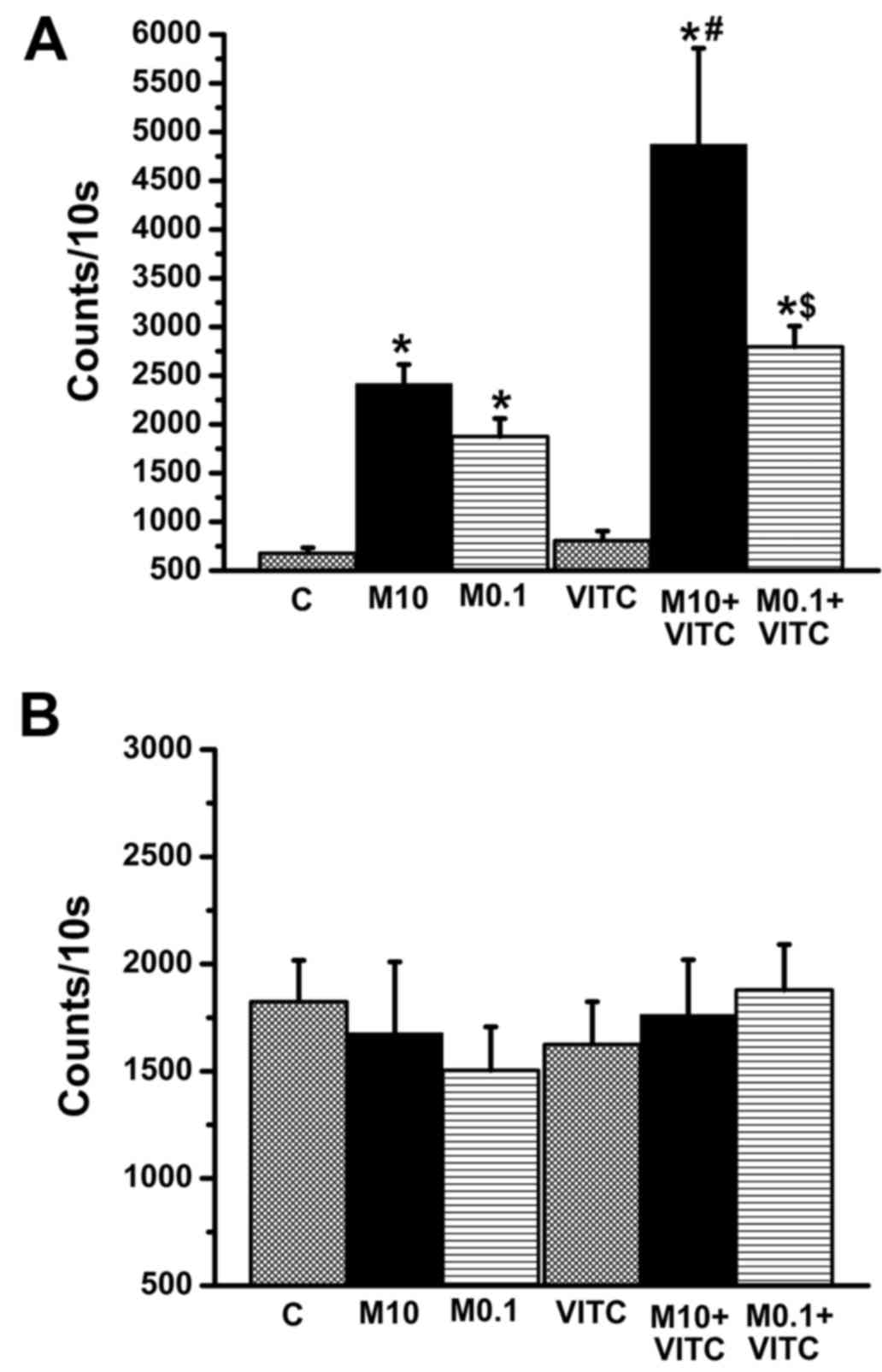
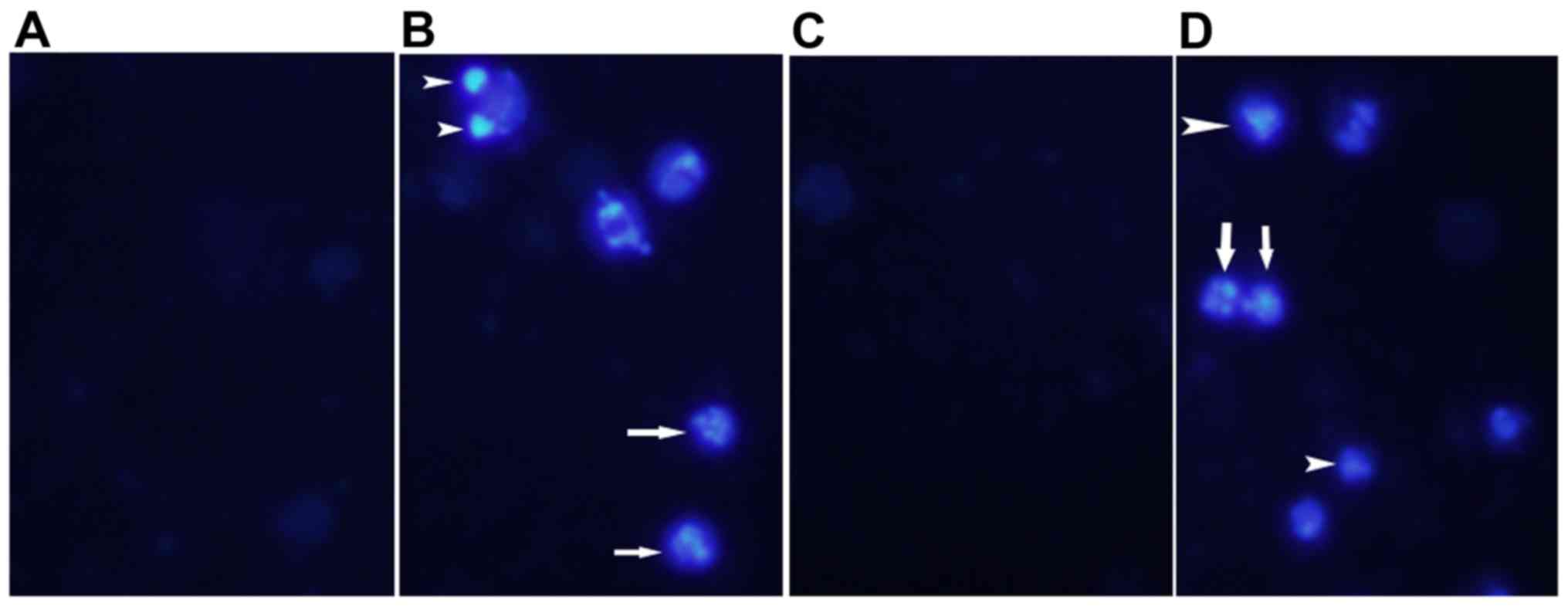
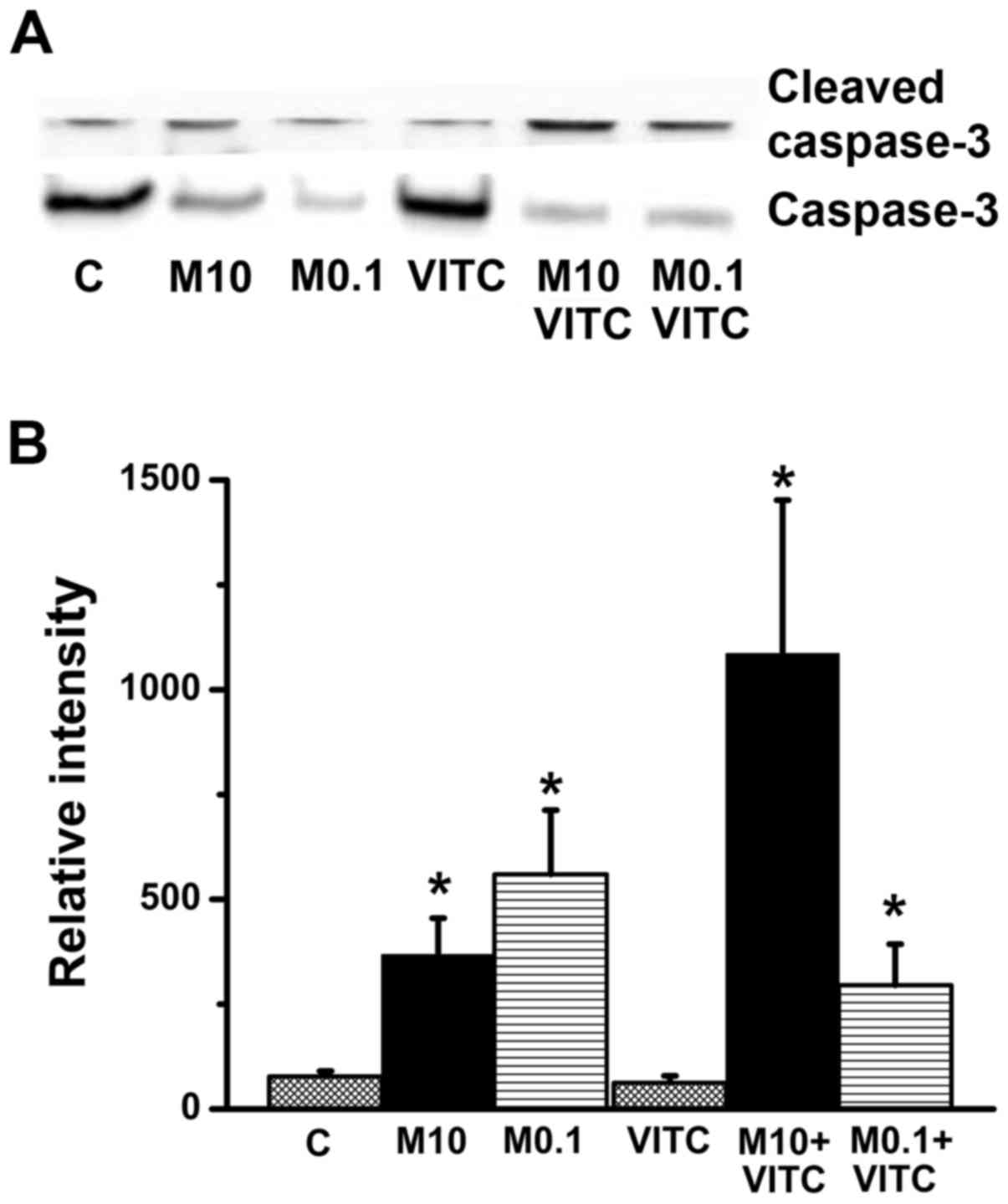
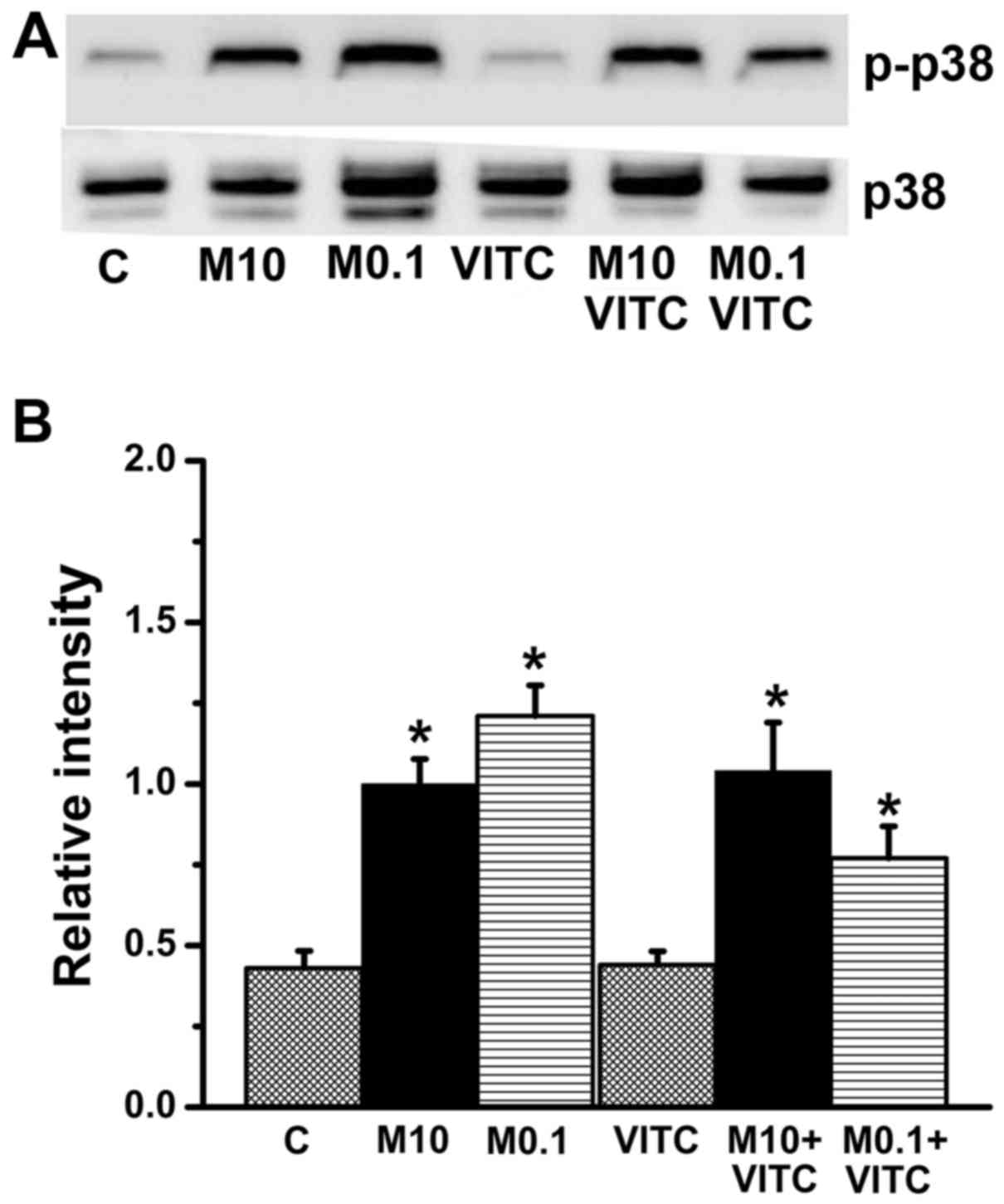
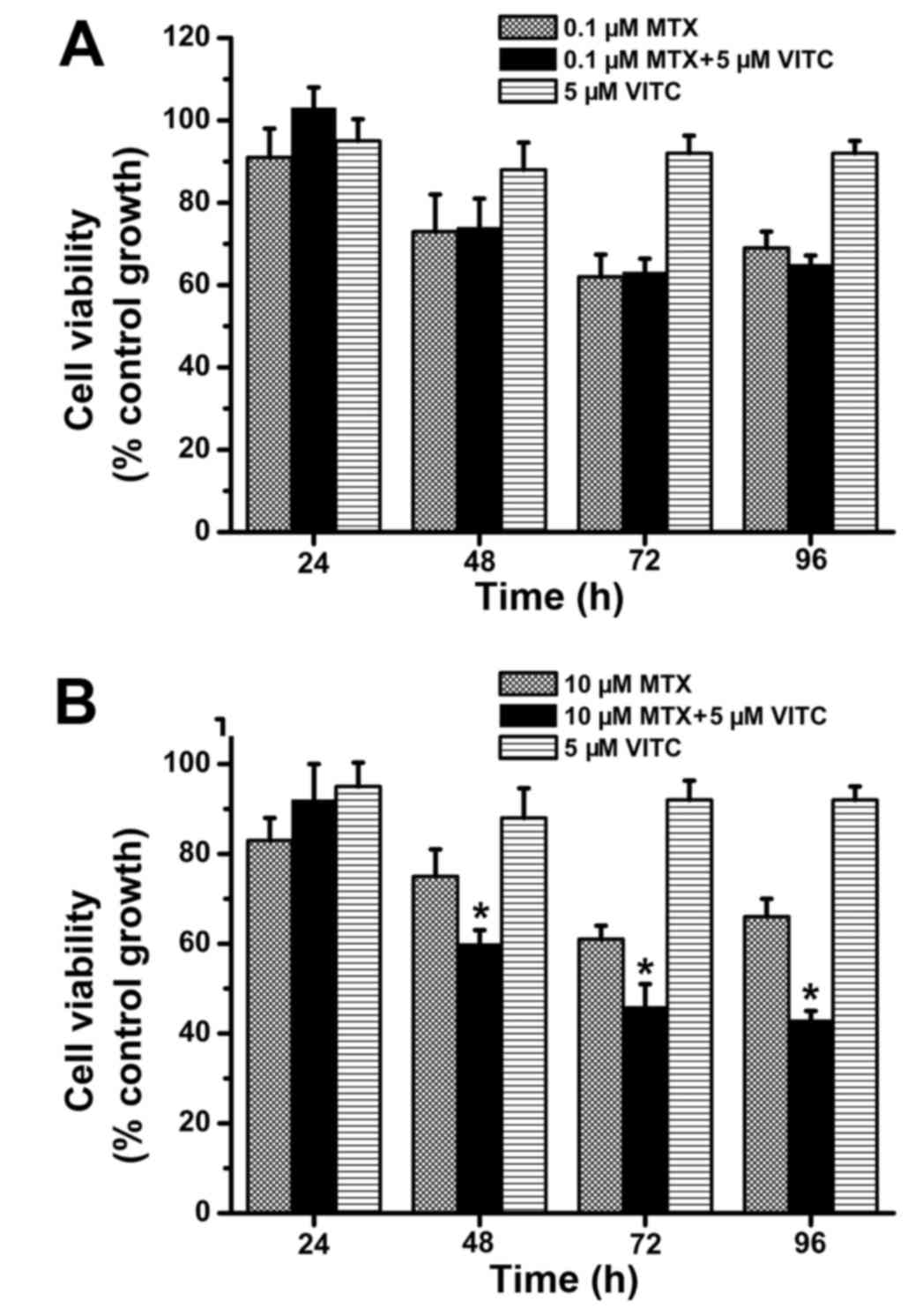
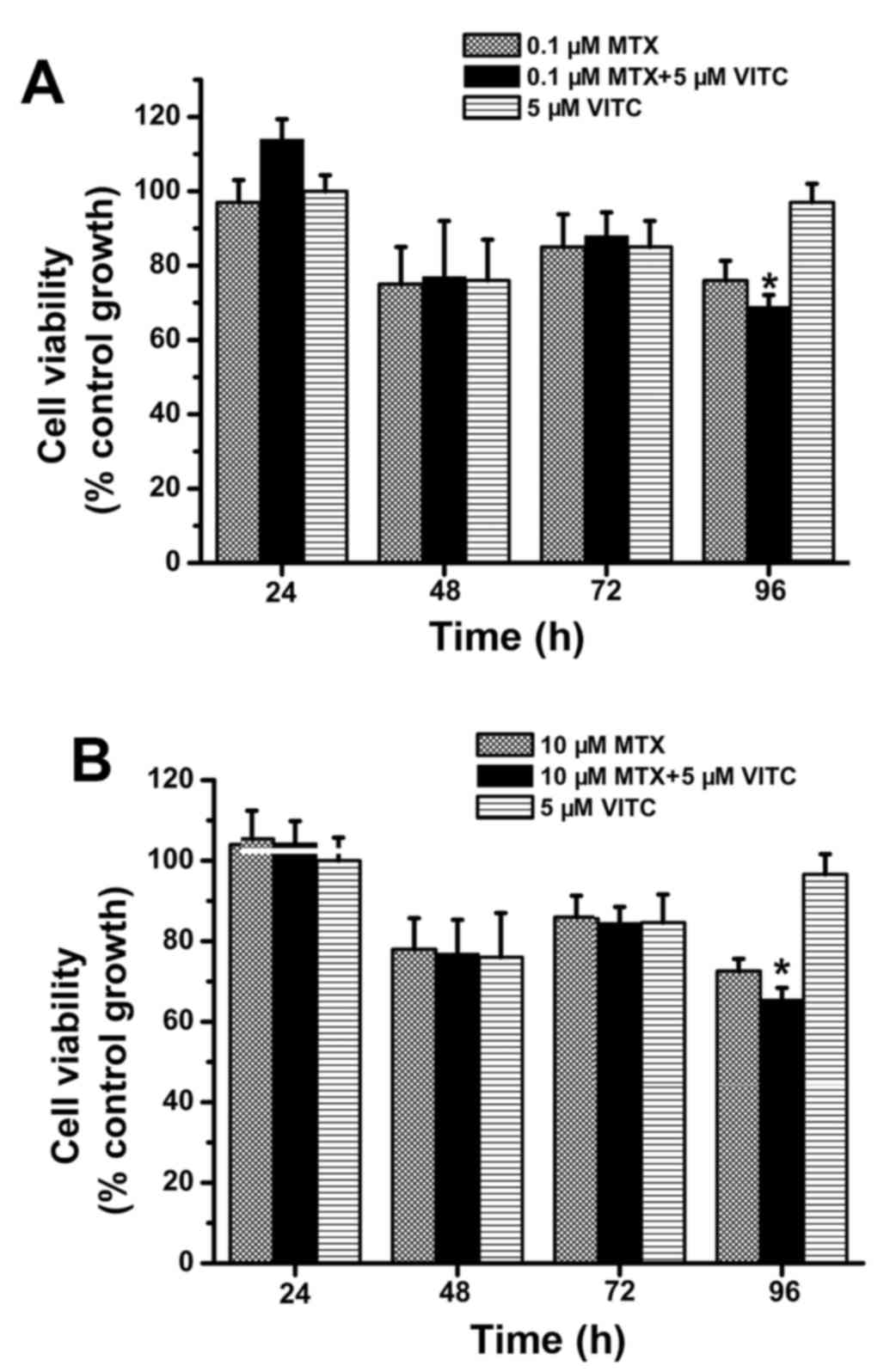
Yiang GT, Chou PL, Hung YT, Chen JN, Chang
WJ, Yu YL and Wei CW: Vitamin C enhances anticancer activity in
methotrexate-treated Hep3B hepatocellular carcinoma cells. Oncol
Rep. 32:1057–1063. 2014.PubMed/NCBI
|
|
16
|
Shirao K, Boku N, Yamada Y, Yamaguchi K,
Doi T, Goto M, Nasu J, Denda T, Hamamoto Y, Takashima A, et al:
Gastrointestinal Oncology Study Group of the Japan Clinical
Oncology Group: Randomized Phase III study of 5-fluorouracil
continuous infusion vs. sequential methotrexate and 5-fluorouracil
therapy in far advanced gastric cancer with peritoneal metastasis
(JCOG0106). Jpn J Clin Oncol. 43:972–980. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Takemura Y and Jackman AL: Folate-based
thymidylate synthase inhibitors in cancer chemotherapy. Anticancer
Drugs. 8:3–16. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Fukuda T, Tanabe M, Kobayashi K, Fukada I,
Takahashi S, Iwase T and Ito Y: Combination chemotherapy with
mitomycin C and methotrexate is active against metastatic
HER2-negative breast cancer even after treatment with
anthracycline, taxane, capecitabine, and vinorelbine. Springerplus.
4:3762015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Leone JP, Leone J, Vallejo CT, Pérez JE,
Romero AO, Machiavelli MR, Romero Acuña L, Domínguez ME, Langui M,
Fasce HM, et al: Sixteen years follow-up results of a randomized
phase II trial of neoadjuvant fluorouracil, doxorubicin, and
cyclophosphamide (FAC) compared with cyclophosphamide,
methotrexate, and 5-fluorouracil (CMF) in stage III breast cancer:
GOCS experience. Breast Cancer Res Treat. 143:313–323. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wu CE, Chen SC, Lin YC, Lo YF, Hsueh S and
Chang HK: Identification of patients with node-negative,
triple-negative breast cancer who benefit from adjuvant
cyclophosphamide, methotrexate, and 5-fluorouracil chemotherapy.
Anticancer Res. 34:1301–1306. 2014.PubMed/NCBI
|
|
21
|
Shea B, Swinden MV, Ghogomu ET, Ortiz Z,
Katchamart W, Rader T, Bombardier C, Wells GA and Tugwell P: Folic
acid and folinic acid for reducing side effects in patients
receiving methotrexate for rheumatoid arthritis. J Rheumatol.
41:1049–1060. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lee HJ, Hong SK, Seo JK, Lee D and Sung
HS: A case of cutaneous side effect of methotrexate mimicking
Behçets disease. Ann Dermatol. 23:412–414. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Colomer Gallardo A, Martínez Rodríguez R,
Castillo Pacheco C, González Satue C and Ibarz Servio L:
Dermatological side effects of intravesical mitomycin C: Delayed
hypersensitivity. Arch Esp Urol. 69:89–91. 2016.PubMed/NCBI
|
|
24
|
Elazzazy S, Mohamed AE and Gulied A:
Cyclophosphamide-induced symptomatic hyponatremia, a rare but
severe side effect: A case report. Onco Targets Ther. 7:1641–1645.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sun W, Yan C, Jia S and Hu J: Correlation
analysis of peripheral DPYD gene polymorphism with 5-fluorouracil
susceptibility and side effects in colon cancer patients. Int J
Clin Exp Med. 7:5857–5861. 2014.PubMed/NCBI
|
|
26
|
Rietjens IM, Boersma MG, Haan L,
Spenkelink B, Awad HM, Cnubben NH, van Zanden JJ, Woude H, Alink GM
and Koeman JH: The pro-oxidant chemistry of the natural
antioxidants vitamin C, vitamin E, carotenoids and flavonoids.
Environ Toxicol Pharmacol. 11:321–333. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Mason SA, Gatta PA Della, Snow RJ, Russell
AP and Wadley GD: Ascorbic acid supplementation improves skeletal
muscle oxidative stress and insulin sensitivity in people with type
2 diabetes: Findings of a randomized controlled study. Free Radic
Biol Med. 93:227–238. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lee WJ: The prospects of vitamin C in
cancer therapy. Immune Netw. 9:147–152. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Nagappan A, Park KI, Park HS, Kim JA, Hong
GE, Kang SR, Lee DH, Kim EH, Lee WS, Won CK, et al: Vitamin C
induces apoptosis in AGS cells by down-regulation of 14-3-3σ via a
mitochondrial dependent pathway. Food Chem. 135:1920–1928. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Guerriero E, Sorice A, Capone F,
Napolitano V, Colonna G, Storti G, Castello G and Costantini S:
Vitamin C effect on mitoxantrone-induced cytotoxicity in human
breast cancer cell lines. PLoS One. 9:e1152872014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Vetvicka V and Vetvickova J: Combination
of glucan, resveratrol and vitamin C demonstrates strong anti-tumor
potential. Anticancer Res. 32:81–87. 2012.PubMed/NCBI
|
|
32
|
Nagao T, Warnakulasuriya S, Nakamura T,
Kato S, Yamamoto K, Fukano H, Suzuki K, Shimozato K and Hashimoto
S: Treatment of oral leukoplakia with a low-dose of beta-carotene
and vitamin C supplements: A randomized controlled trial. Int J
Cancer. 136:1708–1717. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Tokarski S, Rutkowski M, Godala M, Mejer A
and Kowalski J: The impact of ascorbic acid on the concentrations
of antioxidative vitamins in the plasma of patients with non-small
cell lung cancer undergoing first-line chemotherapy. Pol Merkur
Lekarski. 35:136–140. 2013.(In Polish). PubMed/NCBI
|
|
34
|
Nechuta S, Lu W, Chen Z, Zheng Y, Gu K,
Cai H, Zheng W and Shu XO: Vitamin supplement use during breast
cancer treatment and survival: A prospective cohort study. Cancer
Epidemiol Biomarkers Prev. 20:262–271. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Subramani T, Yeap SK, Ho WY, Ho CL, Omar
AR, Aziz SA, Rahman NM and Alitheen NB: Vitamin C suppresses cell
death in MCF-7 human breast cancer cells induced by tamoxifen. J
Cell Mol Med. 18:305–313. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Hong SW, Jin DH, Hahm ES, Yim SH, Lim JS,
Kim KI, Yang Y, Lee SS, Kang JS, Lee WJ, et al: Ascorbate (vitamin
C) induces cell death through the apoptosis-inducing factor in
human breast cancer cells. Oncol Rep. 18:811–815. 2007.PubMed/NCBI
|
|
37
|
Uetaki M, Tabata S, Nakasuka F, Soga T and
Tomita M: Metabolomic alterations in human cancer cells by vitamin
C-induced oxidative stress. Sci Rep. 5:138962015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
van der Reest J and Gottlieb E:
Anti-cancer effects of vitamin C revisited. Cell Res. 26:269–270.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Mense SM, Singh B, Remotti F, Liu X and
Bhat HK: Vitamin C and alpha-naphthoflavone prevent
estrogen-induced mammary tumors and decrease oxidative stress in
female ACI rats. Carcinogenesis. 30:1202–1208. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Yiang GT, Yu YL, Lin KT, Chen JN, Chang WJ
and Wei CW: Acetaminophen induces JNK/p38 signaling and activates
the caspase-9-3-dependent cell death pathway in human mesenchymal
stem cells. Int J Mol Med. 36:485–492. 2015.PubMed/NCBI
|
|
41
|
Yu YL, Yiang GT, Chou PL, Tseng HH, Wu TK,
Hung YT, Lin PS, Lin SY, Liu HC, Chang WJ, et al: Dual role of
acetaminophen in promoting hepatoma cell apoptosis and kidney
fibroblast proliferation. Mol Med Rep. 9:2077–2084. 2014.PubMed/NCBI
|
|
42
|
Lin BR, Yu CJ, Chen WC, Lee HS, Chang HM,
Lee YC, Chien CT and Chen CF: Green tea extract supplement reduces
D-galactosamine-induced acute liver injury by inhibition of
apoptotic and proinflammatory signaling. J Biomed Sci. 16:352009.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Kolli VK, Abraham P, Isaac B and
Selvakumar D: Neutrophil infiltration and oxidative stress may play
a critical role in methotrexate-induced renal damage. Chemotherapy.
55:83–90. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Ohgidani M, Komizu Y, Goto K and Ueoka R:
Residual powders from Shochu distillation remnants induce apoptosis
in human hepatoma cells via the caspase-independent pathway. J
Biosci Bioeng. 114:104–109. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Yu VW and Ho WS: Tetrandrine inhibits
hepatocellular carcinoma cell growth through the caspase pathway
and G2/M phase. Oncol Rep. 29:2205–2210. 2013.PubMed/NCBI
|
|
46
|
Wu Y, van der Schaft DW, Baaijens FP and
Oomens CW: Cell death induced by mechanical compression on
engineered muscle results from a gradual physiological mechanism. J
Biomech. 49:1071–1077. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Chen J, Li Y, Hao H, Li C, Du Y, Hu Y, Li
J, Liang Z, Li C, Liu J, et al: Mesenchymal stem cell conditioned
medium promotes proliferation and migration of alveolar epithelial
cells under Septic conditions in vitro via the JNK-P38 signaling
pathway. Cell Physiol Biochem. 37:1830–1846. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Lee K, Chung YH, Ahn H, Kim H, Rho J and
Jeong D: Selective regulation of MAPK signaling mediates
RANKL-dependent osteoclast differentiation. Int J Biol Sci.
12:235–245. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Tan CS, Gilligan D and Pacey S: Treatment
approaches for EGFR-inhibitor-resistant patients with
non-small-cell lung cancer. Lancet Oncol. 16:e447–e459. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Sato F, Kubota Y, Natsuizaka M, Maehara O,
Hatanaka Y, Marukawa K, Terashita K, Suda G, Ohnishi S, Shimizu Y,
et al: EGFR inhibitors prevent induction of cancer stem-like cells
in esophageal squamous cell carcinoma by suppressing
epithelial-mesenchymal transition. Cancer Biol Ther. 16:933–940.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Li X, Qin N, Wang J, Yang X, Zhang X, Lv
J, Wu Y, Zhang H, Nong J and Zhang Q: Clinical observation of
icotinib hydrochloride for advanced non-small cell lung cancer
patients with EGFR status identified. Zhongguo Fei Ai Za Zhi.
18:734–739. 2015.(In Chinese). PubMed/NCBI
|
|
52
|
Osarogiagbon RU, Cappuzzo F, Ciuleanu T,
Leon L and Klughammer B: Erlotinib therapy after initial platinum
doublet therapy in patients with EGFR wild type non-small cell lung
cancer: Results of a combined patient-level analysis of the NCIC
CTG BR.21 and SATURN trials. Transl Lung Cancer Res. 4:465–474.
2015.PubMed/NCBI
|
|
53
|
Montagna E, Cancello G, Bagnardi V,
Pastrello D, Dellapasqua S, Perri G, Viale G, Veronesi P, Luini A,
Intra M, et al: Metronomic chemotherapy combined with bevacizumab
and erlotinib in patients with metastatic HER2-negative breast
cancer: Clinical and biological activity. Clin Breast Cancer.
12:207–214. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Tolcher AW, LoRusso P, Arzt J, Busman TA,
Lian G, Rudersdorf NS, Vanderwal CA, Kirschbrown W, Holen KD and
Rosen LS: Safety, efficacy, and pharmacokinetics of navitoclax
(ABT-263) in combination with erlotinib in patients with advanced
solid tumors. Cancer Chemother Pharmacol. 76:1025–1032. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Evans MK, Tovmasyan A, Batinic-Haberle I
and Devi GR: Mn porphyrin in combination with ascorbate acts as a
pro-oxidant and mediates caspase-independent cancer cell death.
Free Radic Biol Med. 68:302–314. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Ohtani S, Iwamaru A, Deng W, Ueda K, Wu G,
Jayachandran G, Kondo S, Atkinson EN, Minna JD, Roth JA, et al:
Tumor suppressor 101F6 and ascorbate synergistically and
selectively inhibit non-small cell lung cancer growth by
caspase-independent apoptosis and autophagy. Cancer Res.
67:6293–6303. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Lin SY, Lai WW, Chou CC, Kuo HM, Li TM,
Chung JG and Yang JH: Sodium ascorbate inhibits growth via the
induction of cell cycle arrest and apoptosis in human malignant
melanoma A375.S2 cells. Melanoma Res. 16:509–519. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Nagao N, Nakayama T, Etoh T, Saiki I and
Miwa N: Tumor invasion is inhibited by phosphorylated ascorbate via
enrichment of intracellular vitamin C and decreasing of oxidative
stress. J Cancer Res Clin Oncol. 126:511–518. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Liu JW, Nagao N, Kageyama K and Miwa N:
Antimetastatic and anti-invasive ability of phospho-ascorbyl
palmitate through intracellular ascorbate enrichment and the
resultant antioxidant action. Oncol Res. 11:479–487.
1999.PubMed/NCBI
|
|
60
|
Pires AS, Marques CR, Encarnação JC,
Abrantes AM, Mamede AC, Laranjo M, Gonçalves AC, Sarmento-Ribeiro
AB and Botelho MF: Ascorbic acid and colon cancer: An oxidative
stimulus to cell death depending on cell profile. Eur J Cell Biol.
95:208–218. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Beck R, Pedrosa RC, Dejeans N, Glorieux C,
Levêque P, Gallez B, Taper H, Eeckhoudt S, Knoops L, Calderon PB,
et al: Ascorbate/menadione-induced oxidative stress kills cancer
cells that express normal or mutated forms of the oncogenic protein
Bcr-Abl. An in vitro and in vivo mechanistic study. Invest New
Drugs. 29:891–900. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Venturelli S, Sinnberg TW, Berger A, Noor
S, Levesque MP, Böcker A, Niessner H, Lauer UM, Bitzer M, Garbe C,
et al: Epigenetic impacts of ascorbate on human metastatic melanoma
cells. Front Oncol. 4:2272014. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Ma Y, Chapman J, Levine M, Polireddy K,
Drisko J and Chen Q: High-dose parenteral ascorbate enhanced
chemosensitivity of ovarian cancer and reduced toxicity of
chemotherapy. Sci Transl Med. 6:222ra182014. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Cieslak JA and Cullen JJ: Treatment of
pancreatic cancer with pharmacological ascorbate. Curr Pharm
Biotechnol. 16:759–770. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Presutti D, Santini S, Cardinali B, Papoff
G, Lalli C, Samperna S, Fustaino V, Giannini G and Ruberti G: MET
gene amplification and MET receptor activation are not sufficient
to predict efficacy of combined MET and EGFR inhibitors in EGFR
TKI-resistant NSCLC cells. PLoS One. 10:e01433332015. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
De S, Dermawan JK and Stark GR: EGF
receptor uses SOS1 to drive constitutive activation of NF-κB in
cancer cells. Proc Natl Acad Sci USA. 111:11721–11726. 2014.
View Article : Google Scholar : PubMed/NCBI
|