Introduction
Epithelial ovarian cancer (EOC) is a major cause of
cancer-related mortality among gynecologic malignancies. Based on
the fact that EOC frequently remains clinically silent, most
patients have microscopically or macroscopically metastatic
peritoneal lesions at diagnosis (1). However, EOC is in general a
heterogeneous tumor that contains various histologic types,
including serous, clear-cell, endometrioid, mucinous and other
types of adenocarcinoma. The clinical outcomes and biological
hallmarks are different among these histological subtypes. This
diversity makes it complicated to understand and analyze EOC
(2). Ovarian clear-cell carcinoma
(CCC) is a comparatively rare tumor in Western countries,
representing less than 10% of all epithelial ovarian cancer (EOC)
cases diagnosed (3). However, the
incidence of this tumor was estimated to make it a common
pathological type among EOC cases in East Asia (4). In particular, CCC is the second most
frequent subtype of EOC, accounting for 24.8% of all malignant
ovarian neoplasms diagnosed in Japan (5). Clinically, this tumor is known to be
diagnosed at an early stage, and shows frequent unilateral
occurrence, association with endometriosis, and comorbidity with
thromboembolism (3,6–8). In
addition, based on recent larger-scale studies, a poorer oncologic
outcome is exhibited by patients with advanced-stage CCC compared
with those with a serous histology, reflecting its potential
chemoresistance to conventional platinum-based compounds (9,10).
Therefore, it is crucial to determine prognostic biomarkers of CCC
to develop strategies for improving the clinical outcome and/or
monitoring the tumor status.
Kinesin family member 20A (KIF20A), a member of the
kinesin superfamily-6, is a microtubule-associated motor protein
that is required for cell cycle mitosis (11,12).
This molecule was initially revealed to localize to the Golgi
apparatus and participate in organelle dynamics by interacting with
the GTP-bound form of Rab6 (13).
In non-cancerous normal tissues, KIF20A is reported to be expressed
in fetal liver, adult bone marrow and thymus, whereas low levels
are found in the placenta and heart (14,15).
On the other hand, according to previous studies, it was shown to
be overexpressed in various malignancies, including lung and breast
cancer (15,18). With regard to malignant cellular
functions, KIF20A has been reported to be involved in
proliferation, migration, invasiveness and angiogenesis (15,19–21).
In addition, a recent study also demonstrated the possible
involvement of KIF20A in the resistance of breast cancer to
paclitaxel (22). From the clinical
point of view, KIF20A expression was found to be associated with
poor oncologic outcome in a number of human malignancies, including
breast, nasopharyngeal, hepatocellular and uterine cervical
carcinoma (23–26).
To the best of our knowledge, no published study has
examined KIF20A expression in ovarian CCC. These clinical and
molecular backgrounds led us to hypothesize that KIF20A plays a
central role in the progression of CCC, and that positive KIF20A
expression may be a valuable indicator to predict an unfavorable
oncologic outcome in patients with CCC. In the present study, we
explored the relationship between KIF20A expression and the
prognosis of ovarian CCC patients, and we analyzed the functions of
KIF20A in CCC cell growth.
Materials and methods
Cell culture
One human pancreatic cancer cell line (PANC1:
positive control) (15) and seven
EOC cell lines (ES-2, TOV-21G, RMG-I, RMG-II, SKOV3, OV-90 and
KOC-7C) were maintained in RPMI-1640 medium with 10% fetal bovine
serum (FBS) and penicillin/streptomycin. These cell lines except
for RMG-I and RMG-II cells were purchased from the American Type
Culture Collection (ATCC; Manassas, VA, USA) in 2012-2013. RMG-I
and RMG-II cells were generously donated by Fujita Health
University (Toyoake, Japan). These cell lines were maintained in
RPMI-1640 medium (Sigma-Aldrich; Merck KGaA, Darmstadt, Germany)
supplemented with 10% FBS and penicillin-streptomycin at 37°C in a
humidified atmosphere of 5% CO2.
Inhibition of KIF20A by small
interfering RNA (siRNA)
To produce KIF20A-knockdown cells, ES-2 and SKOV3
cells were transfected with either a pool of small interfering RNA
(siRNA) oligonucleotides specific to human KIF20A (final
concentration, 50 nmol/l; sc-91657; Santa Cruz Biotechnology, Santa
Cruz, CA, USA) or control siRNA (5′-CUUACGCUGAGUACUUCGATT-3′:
Sigma-Aldrich; Merck KGaA) using GenePORTER 2 Transfection reagent
(Gene Therapy Systems Inc., San Diego, CA, USA). KIF20A siRNA
(sc-91657) is a pool of 3 different siRNA duplexes: sc-91657A
(sense, 5′-CUGUGAAGGAGAUGGUAAATT-3′), sc-91657B (sense,
5′-GCAAUCCCUAUGUGAAAGATT-3′) and sc-91657C (sense,
5′-GUUCCUGCAUGAUUGUCAATT-3′). After overnight incubation at 37°C,
the culture medium was replaced with fresh complete medium
containing 10% FBS. Cells were harvested after 48 h and solubilized
for western blot analysis of KIF20A silencing.
Western blot analysis
To examined the expression of KIF20A in seven EOC
cell lines (CCC: ES-2, TOV-21G, RMG-I, RMG-II, KOC-7C cells:
non-CCC SKOV3, OV-90 cells) or knockdown efficacy of the siRNA
experiment (ES-2 and SKOV3 cells), western blotting was performed.
The experimental procedure of western blotting was previously
described (27). As primary
antibodies, we used anti-KIF20A (diluted 1:100; cat. no. sc-374508;
Santa Cruz Biotechnology) and anti-β-actin antibodies (diluted
1:3,000; cat. no. 017-24573; Wako Pure Chemical Industries Ltd.,
Osaka, Japan). The primary antibodies were washed in 0.05%
Tween-20/PBS, and then incubated with horseradish
peroxidase-conjugated secondary antibody (diluted 1:3,000; cat. no.
A90-116P; Bethyl Laboratories Inc., Montgomery, TX, USA). Proteins
were visualized using enhanced chemiluminescence reagent (Amersham
Pharmacia Biotech, Piscataway, NJ, USA). The ratio of the intensity
of KIF20A-positive bands to the intensity of β-actin-positive ones
was used to compare the relative expression levels of these
proteins in the KIF20A- and control-siRNA transfected lines. The
intensities of the bands were semi-quantified by ImageJ software
(version 1.51k; National Institutes of Health, Bethesda, MD, USA)
(https://imagej.nih.gov/ij/).
Cell proliferation assay
To determine the effect of KIF20A on cell
proliferation, ES2 and SKOV3 cells transfected with KIF20A-siRNA or
control siRNA were seeded onto 96-well plates at a density of
1×103 cells/well. Then, at time-points of 0, 24, 48 and
72 h, the cell viability rate was assessed using Cell Counting
Kit-8 (CCK-8; Dojindo Molecular Technologies, Inc., Rockville, MD,
USA). Ten microliters of CCK-8 solution was added to each well and
the cells were incubated for another 2 h and then a microplate
reader (ELx808; BioTek Instruments Japan, Tokyo, Japan) was used to
measure the absorbance of each well at 450 nm. All experiments were
independently repeated three times. Paprotrain (Tocris Bioscience,
Bristol, UK) is a cell-permeable acrylonitrile compound that
inhibits the kinesin-6 family member KIF20A. We investigated the
effect of Paprotrain on cell proliferation using pretreatment at
doses of 0, 25 and 100 µM in the ES2 and SKOV3 cells.
Apoptosis assay
The percentage of apoptotic cells was assayed using
the Annexin V-FLUOS Staining kit (Roche Life Science, Indianapolis,
IN, USA). Briefly, 1×105 ES-2 cells were seeded in
6-well plates and cultured for 24 h. The cells were collected and
resuspended in 100 µl of binding buffer. Then, the cells were
incubated with 5 µl of FITC-Annexin V in the dark for 15 min at
room temperature. Subsequently, 5 µl of PI was added and incubated
with the cells for 20 min at room temperature in the dark. Finally,
the cell samples were examined in a flow cytometer. Each assessment
of proliferation and apoptosis was repeated three times.
Cell cycle distribution
For cell cycle analysis, ES2 and SKOV3 cells were
treated with or without S109 for 24 h. Then, the cells were
collected, fixed in 70% ethanol, washed twice with
phosphate-buffered saline (PBS), and then stained with propidium
iodide (PI) solution containing 25 µg/ml of RNAse and 50 µg/ml of
PI in the dark for 30 min. Subsequently, the cells were assayed
with FACSCalibur (Becton-Dickinson, Franklin Lakes, NJ, USA) and
analyzed using CellQuest Pro software (Becton-Dickinson).
Patients and immunohistochemical
staining
Forty-three human ovarian CCC tissues were obtained
from patients who underwent surgical treatment at the Nagoya
University Hospital between 1993 and 2006 after providing informed
consent. To ascertain the histological types, we adopted the World
Health Organization (WHO) classification criteria. The clinical
stage was assigned according to the International Federation of
Gynecology and Obstetrics (FIGO) staging system (28,29).
This study was approved by the Ethics Committee of Nagoya
University.
Formalin-fixed, paraffin-embedded tissue sections
were cut at a thickness of 4 µm. For heat-induced epitope
retrieval, deparaffinized sections in 0.01 M citrate buffer (Target
Retrieval Solution, pH 6.1; Dako, Tokyo Japan) were heated three
times at 90°C for 5 min using a microwave oven. Sections were
incubated at 4°C for 12 h with primary antibody (anti-rabbit KIF20A
polyclonal, at a 1:100 dilution; Santa Cruz Biotechnology). The
sections were rinsed and incubated for 30 min with biotinylated
anti-rabbit IgG antibody (cat. no. 424022; Nichirei Biosciences
Inc., Tokyo, Japan). The immunoreactive staining was processed
using the peroxidase-anti-peroxidase method according to the
manufacturer's instructions (Dako GmbH, Hamburg, Germany). To
detect the reaction, 3,3′-diaminobenzidine tetrachloride (DAB)
chromogen solution was used. After rinsing in water for 30 min, the
sections were counterstained with hematoxylin and then dehydrated.
Finally, they were mounted in mounting medium for examination. The
specificity of the antibody was determined using a non-specific
immunoglobulin IgG (diluted 1:100; cat. no. sc-2025; Santa Cruz
Biotechnology) at the same concentration.
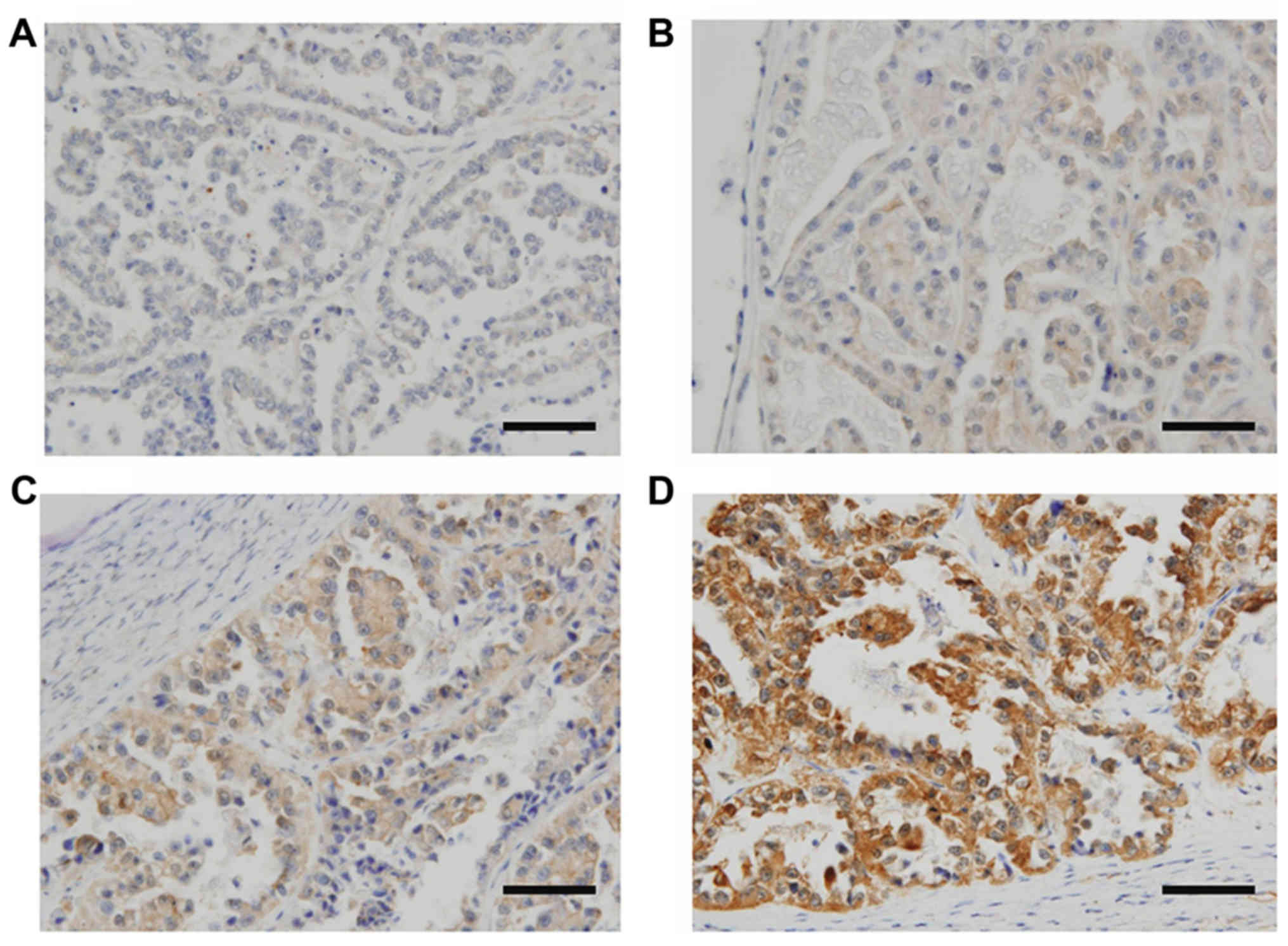
Evaluation of immunohistochemical
staining
For the evaluation of the results of
immunohistochemical staining, 10 fields of each specimen were
selected and evaluated with both low- (magnification, ×100) and
high-power microscopy (magnification, ×400). Two investigators
assessed the slides without knowledge of the clinicopathological
features and were blinded to each other's evaluation. The two
investigators were in agreement on all the slides examined. Based
on the immunostaining activity, a semi-quantitative score was
assigned according to the intensity and area of the stained cells,
as previously described (30). For
the evaluation of KIF20A expression, the staining intensity was
scored as 0 (negative-weak), 1 (medium), 2 (strong), or 3 (very
strong). The percentage of the staining area was scored as 0
(0–10%), 1 (11–50%), and 2 (51–100%) relative to the total tumor
area. The sum of the staining intensity and area scores was
calculated as the final score (0–5) for KIF20A. Tumors with a final
score of 0–1 and 2–5, were classified as showing low and high
expression, respectively.
Survival analyses
The distributions of clinicopathological factors
were statistically assessed using the Chi-square test or the
Fisher's exact test. The progression-free survival (PFS) was
defined as the time interval between the date of surgery and the
date of the last follow-up or recurrence/progression. The overall
survival (OS) was defined as the time interval between the date of
surgery and the date of the last follow-up or death from any cause.
The survival curves were compared employing the log-rank test.
Survival analysis was conducted using the Kaplan-Meier method. The
prognostic significance of KIF20A expression concerning other
clinicopathological variables was assessed using the univariable
and multivariable Cox's proportional hazard's analyses. All
statistical analyses were performed with the JMP Pro Ver. 10.0 (SAS
Institute Japan Ltd., Tokyo, Japan). A P<0.05 was considered to
indicate a statistically significant result.
Statistical analysis
All data are expressed as the mean ± SD. Data were
calculated from at least three independent experiments. The
significance of differences was analyzed by Student's t-test or
one-way ANOVA. A value of P<0.05 was considered to indicate a
statistically significant result.
Results
Patient characteristics
We first explored KIF20A expression and its possible
involvement in the oncologic outcome of patients with ovarian CCC
using immunohistochemical analysis. Patient characteristics are
detailed in Table I. The median
(range) age was 52 (27–71) years. The distributions of the FIGO
stage were 58.1% (25/43) stage I, 18.6% (8/43) stage II, 18.6%
(8/43) stage III, and 4.7% (2/43) stage IV. Of all patients, 31
(72.1%) underwent complete surgery with surgical staging, and 37
(86.0%) had no residual tumor at the initial surgery. Thirty-seven
patients (86.0%) were administered postoperative chemotherapy. Six
patients did not undergo postoperative chemotherapy owing to their
strong wishes or severe complications. Of the 43 CCC patients, the
distributions of KIF20A staining expression was as follows: 7
(score, 0), 11 (score, 1), 7 (score, 2), 6 (score, 3), 6 (score, 4)
and 6 (score, 5). KIF20A immunoexpression was classified into the
two scoring groups as described above [low (score 0–1) and high
(score 2–5)]. Representative images of tissue samples for each
immunohistochemical staining score are shown in Fig. 1. For the distribution of age and
chemotherapy frequency, there was a significant difference between
the two groups (Table I).
 | Table I.Relationship between the expression
of KIF20A and clinicopathologic parameters. |
Table I.
Relationship between the expression
of KIF20A and clinicopathologic parameters.
|
| KIF20A
expression |
|
|---|
|
|
|
|
|---|
|
| Total | Low | High |
|
|---|
|
|
|
|
|
|
|---|
|
| N | N | % | N | % | P-value |
|---|
| Total no. of
cases | 43 | 18 |
| 25 |
|
|
| Age (years) |
|
|
|
|
|
|
|
≤50 | 21 | 14 | 77.8 | 7 | 28.0 | 0.001 |
|
>50 | 22 | 4 | 22.2 | 18 | 72.0 |
|
| FIGO stage |
|
|
|
|
|
|
| I | 25 | 12 | 66.7 | 13 | 52.0 | 0.697 |
| II | 8 | 3 | 16.7 | 5 | 20.0 |
|
|
III | 8 | 2 | 11.1 | 6 | 24.0 |
|
| IV | 2 | 1 | 5.6 | 1 | 4.0 |
|
| Preoperative CA-125
value (U/ml) |
|
|
|
|
|
|
|
≤35 | 32 | 12 | 66.7 | 20 | 80.0 | 0.323 |
|
>35 | 11 | 6 | 33.3 | 5 | 20.0 |
|
| Ascites volume
(ml) |
|
|
|
|
|
|
|
<100 | 23 | 11 | 61.1 | 12 | 48.0 | 0.245 |
|
100–1,000 | 5 | 0 | 0.0 | 5 | 20.0 |
|
|
>1,000 | 7 | 3 | 16.7 | 4 | 16.0 |
|
| NA | 8 | 4 | 22.2 | 4 | 16.0 |
|
| Surgery |
|
|
|
|
|
|
|
Standard surgery + full
staging | 31 | 14 | 77.8 | 17 | 68.0 | 0.417 |
|
Standard surgerya | 6 | 2 | 11.1 | 4 | 16.0 |
|
| USO/BSO
± OM | 2 | 1 | 5.6 | 1 | 4.0 |
|
|
Debulking surgery | 1 | 1 | 5.6 | 0 | 0.0 |
|
|
Exploratory | 3 | 0 | 0.0 | 3 | 12.0 |
|
| Residual tumor |
|
|
|
|
|
|
| No | 37 | 17 | 94.4 | 20 | 80.0 | 0.178 |
|
Yes | 6 | 1 | 5.6 | 5 | 20.0 |
|
| Chemotherapy |
|
|
|
|
|
|
|
None | 6 | 5 | 27.8 | 1 | 4.0 | 0.0149 |
|
Platinum-based | 10 | 6 | 33.3 | 4 | 16.0 |
|
| Taxane
plus platinum | 27 | 7 | 38.9 | 20 | 80.0 |
|
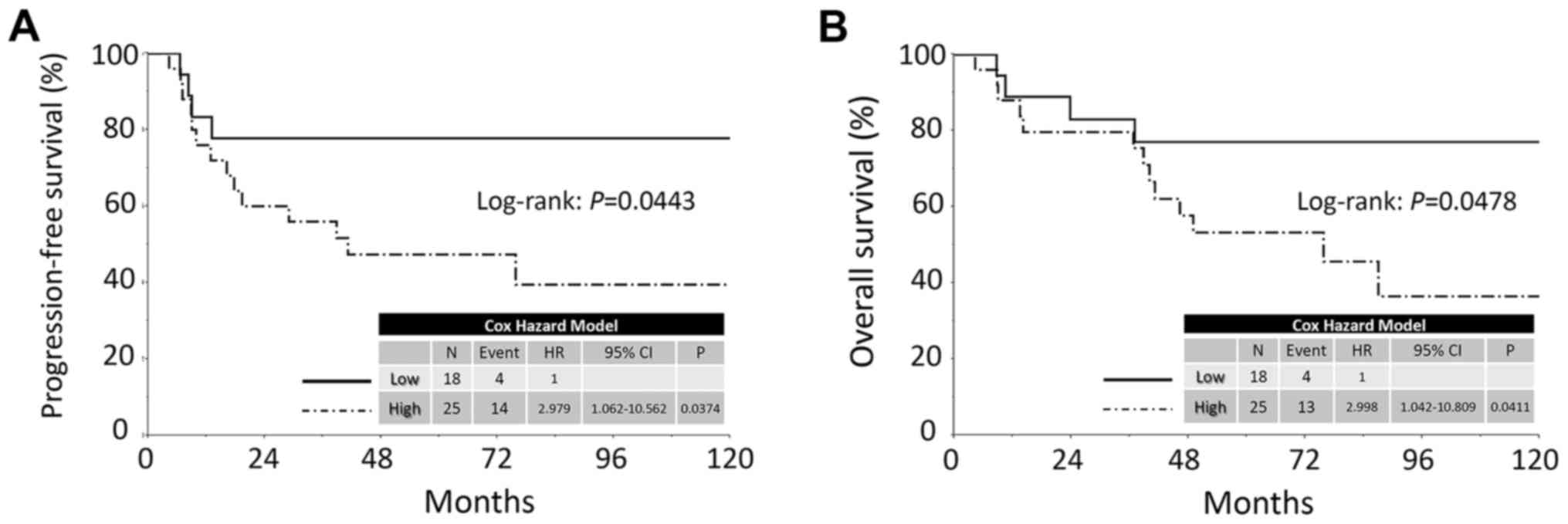
Oncologic outcome according to KIF20A
expression
The median follow-up duration was 64.9, ranging from
4.3 to 159.3 months in all patients. During this period, 18
patients (41.9%) developed recurrence. The median time to
recurrence was 11.5 months. The 5-year PFS and OS rates of all CCC
patients were 60.0 and 63.5%, respectively. Patients in the high
KIF20A expression group showed poorer PFS and OS than those in the
low expression group [PFS (log-rank: P=0.0443; Cox hazard:
P=0.0374) and OS (log-rank: P=0.0478, Cox hazard: P=0.0411),
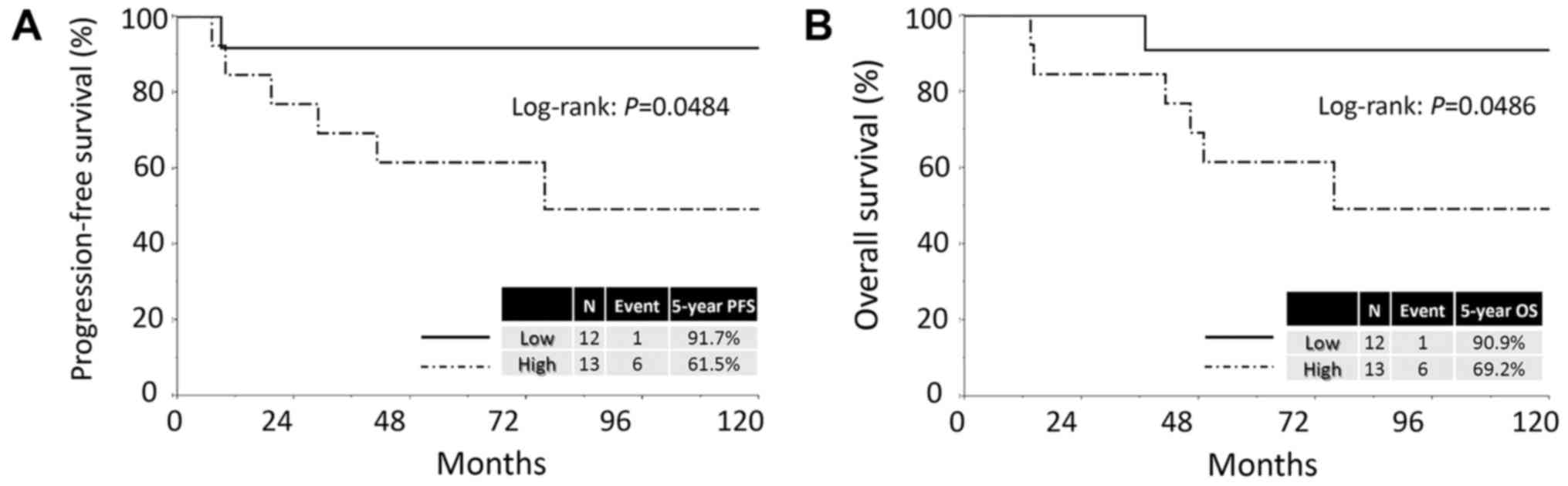
respectively] (Fig. 2). Confining
analysis to stage I patients with CCC, similar prognostic
tendencies were observed (PFS: P=0.0484; OS: P=0.0486) (Fig. 3).
Univariable and multivariable
analyses
We subsequently performed univariable and
multivariable Cox proportional analyses regarding PFS/OS, including
age (≤50 vs. >50 years), FIGO stage (I+II vs. III+IV),
preoperative CA-125 values (≤35 vs. >35 U/ml), volume of ascites
(≤100 vs. >100 ml), type of surgery (standard surgery with full
staging vs. other surgery), residual tumor (yes vs. no),
chemotherapy (platinum-based vs. taxane plus platinum) and KIF20A
immunoreactivity (low vs. high) (Table
II). In the univariable analyses, the preoperative CA-125
value, volume of ascites, FIGO stage, residual tumor presence and
KIF20A expression were significant prognostic indicators of a poor
PFS. In addition, KIF20A expression was found to be a marginally
significant prognostic indicator of a poor OS (P=0.0512). In
general, age was considered to be an important clinical factor
influencing patient survival. On the other hand, the preoperative
CA-125 value, volume of ascites, and residual tumor were strongly
correlated with the stage. To avoid multicollinearity, we entered
the age, stage and KIF20A expression factors into the multivariable
analyses. In multivariable analyses, the KIF20A expression was also
a significantly independent indicator for PFS and a
marginal-significant indicator for OS [PFS: HR (high vs. low),
5.488; 95% CI, 1.410–24.772 (P=0.0136); OS: HR, 2.835; 95% CI,
0.854–11.035 (P=0.0897)] (Table
II).
 | Table II.Univariable and multivariable
analyses. |
Table II.
Univariable and multivariable
analyses.
|
| PFS | OS |
|---|
|
|
|
|
|---|
|
| Univariable | Multivariable | Univariable | Multivariable |
|---|
|
|
|
|
|
|
|---|
|
| HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value |
|---|
| Age (years) |
|
|
|
|
|
|
|
|
|
≤50 | Referent | 0.619 | Referent | 0.1984 | Referent | 0.567 | Referent | 0.9678 |
|
>50 | 1.265
(0.498–3.324) |
| 0.454
(0.141–1.540) |
| 1.322
(0.502–3.542) |
| 1.022
(0.348–3.225) |
|
| Preoperative CA-125
value (U/ml) |
|
|
|
|
|
|
|
|
|
≤35 | Referent | 0.0052 | – |
| Referent | 0.0078 | – |
|
|
>35 | 8.163
(1.671–147.183) |
|
|
| 7.646
(1.553–138.162) |
|
|
|
| Ascites volume
(ml) |
|
|
|
|
|
|
|
|
|
≤100 | Referent | 0.0054 | – |
| Referent | 0.0079 | – |
|
|
>100 | 4.558
(1.570–14.866) |
|
|
| 4.501
(1.491–14.981) |
|
|
|
| FIGO stage |
|
|
|
|
|
|
|
|
|
I–II | Referent | 0.0031 | Referent | 0.0014 | Referent | 0.0106 | Referent | 0.0111 |
|
III–IV | 4.564
(1.720–11.731) |
| 5.696
(2.018–116.282) |
| 3.970
(1.405–10.280) |
| 3.978
(1.397–10.865) |
|
| Surgery |
|
|
|
|
|
|
|
|
|
Standard surgery+full
staging | Referent | 0.3686 | – |
| Referent | 0.457 | – |
|
| Other
surgery | 1.589
(0.552–4.097) |
|
|
| 1.505
(0.477–4.076) |
|
|
|
| Residual tumor |
|
|
|
|
|
|
|
|
| No | Referent | 0.0229 | – |
| Referent | 0.0302 | – |
|
|
Yes | 3.888
(1.233–10.472) |
|
|
| 4.227
(1.170–12.241) |
|
|
|
| Chemotherapy |
|
|
|
|
|
|
|
|
|
Platinum-based | Referent | 0.830 | – |
| Referent | 0.9344 | – |
|
| Taxane
plus platinum | 0.890
(0.329–2.808) |
|
|
| 0.956
(0.344–3.060) |
|
|
|
| KIF20A
expression |
|
|
|
|
|
|
|
|
|
Low | Referent | 0.0374 | Referent | 0.0136 | Referent | 0.0512 | Referent | 0.0897 |
|
High | 2.979
(1.061–10.562) |
| 5.488
(1.410–24.772) |
| 2.833
(0.995–10.117) |
| 2.835
(0.854–11.035) |
|
KIF20A expression in the deceased
ovarian CCC patients
Table III shows
the clinical backgrounds of the 17 deceased patients. The
high-level expression of KIF20A was observed in 13 of the 17
patients (76.5%). In the majority of deceased patients, the most
frequent site of recurrence was the peritoneal cavity and/or
distant parenchymal organs (14/17: 82.4%).
 | Table III.Clinical features and KIF20A
immunoexpression in the deceased ovarian CCC patients. |
Table III.
Clinical features and KIF20A
immunoexpression in the deceased ovarian CCC patients.
| Case | Age (years) | KIF20A
expression | FIGO stage | Ascites volume
(ml) | CA-125 (U/ml) | Chemotherapy | Residual tumor | Recurrence
site | Time to relapse
(mo) | OS (mo) |
|---|
| 1 | 49 | High | IIIc | ≤100 | 54 | P-based | None | Pelvis | 6.7 | 88.2 |
| 2 | 49 | High | Ic | ≥1,000 | 373 | P-based | None | Distant | 41.7 | 64.7 |
| 3 | 52 | High | Ic | 100–1,000 | 41 | P-based | None | PC + distant | 76.8 | 103.3 |
| 4 | 53 | Low | IIc | ≤100 | 60 | None | None | PC | 6.6 | 10.6 |
| 5 | 40 | High | Ic | 100–1,000 | 55 | TP | None | PC+RPN | 7.1 | 13.7 |
| 6 | 38 | Low | IIb | ≤100 | 52 | TP | None | PC | 13.3 | 24.1 |
| 7 | 38 | High | IIc | ≤100 | 328 | TP | None | Pelvis | 16.4 | 40.6 |
| 8 | 49 | Low | Ic | 100–1,000 | 67 | P-based | None | Pelvis +
distant | 9.1 | 37.5 |
| 9 | 27 | Low | IV | ≤100 | NA | P-based | None | PC | 8.4 | 8.8 |
| 10 | 52 | High | Ic | ≤100 | 10 | TP | None | Distant | 29.4 | 46.9 |
| 11 | 54 | High | IV | ≥1,000 | 890 | TP | ≥5 cm | Distant | 8.9 | 8.9 |
| 12 | 53 | High | Ic | ≤100 | 111 | TP | None | PC + distant | 10.0 | 14.3 |
| 13 | 55 | High | IIIc | ≤100 | NA | TP | ≥5 cm | PC | 9.1 | 9.1 |
| 14 | 55 | High | IIIc | 100–1,000 | 920 | TP | None | PC | 17.9 | 37.3 |
| 15 | 39 | High | Ia | ≤100 | 53 | TP | None | Pelvis | 19.6 | 49.7 |
| 16 | 59 | High | IIIc | ≥1,000 | 3,149 | TP | None | PC | 39.4 | 39.4 |
| 17 | 58 | High | IIIc | ≥1,000 | 1,012 | TP | ≤1 cm | PC | 4.3 | 4.3 |
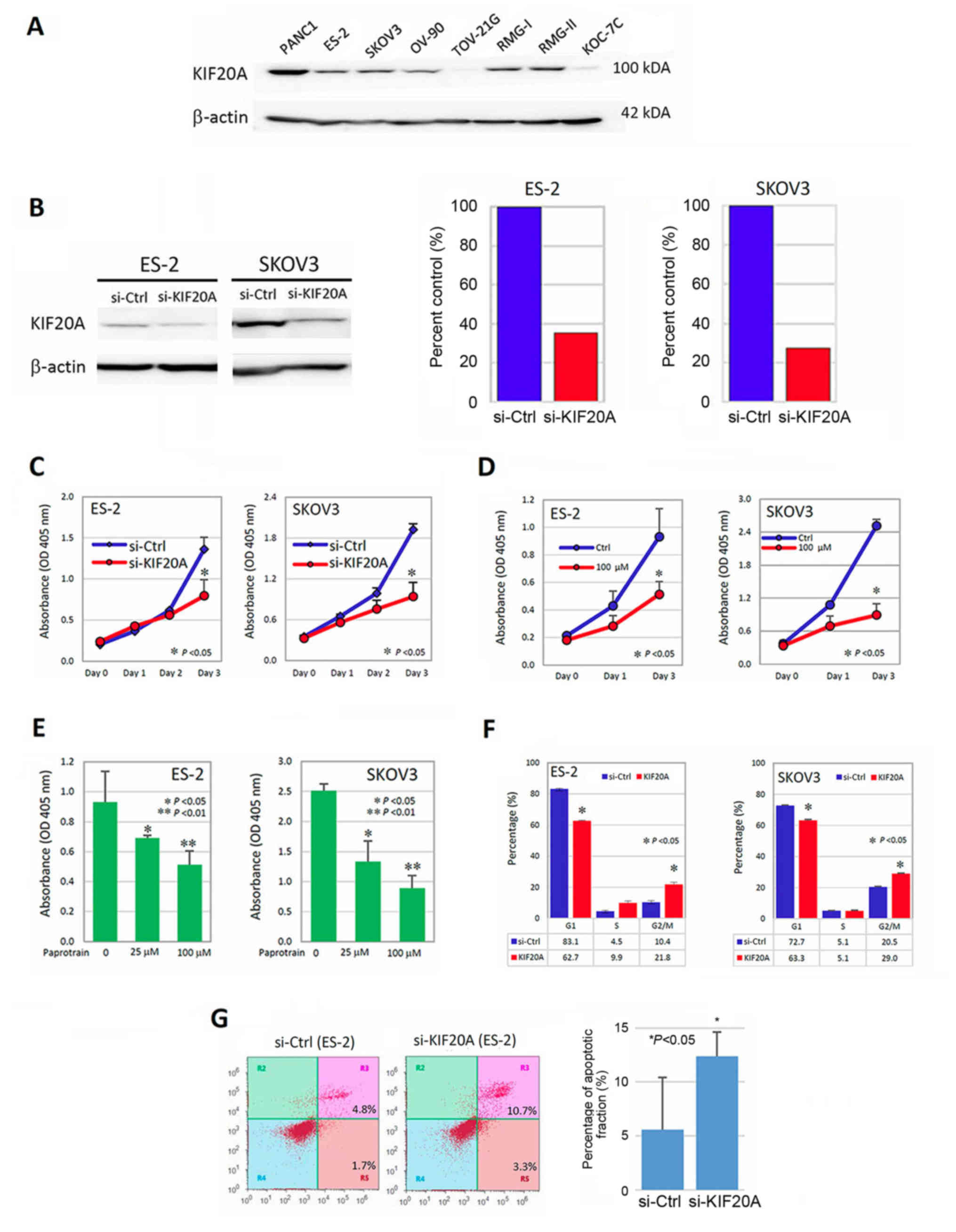
Association between KIF20A expression
and the proliferation-promoting effect
We subsequently investigated the role of KIF20A in
the malignant characteristics of CCC cells using several in
vitro experiments. We initially examined the expression of
KIF20A in various CCC and non-CCC cells. KIF20A was expressed in
RMG-I, RMG-II and ES-2 cells, but lower-level expression of KIF20A
was observed in KOC-7C and TOV-21G cells (these lines are all CCC
cells). As non-CCC/EOC cells, KIF20A was expressed in SKOV-3 and
OV-90 cells (Fig. 4A). We further
examined whether KIF20A was associated with the
proliferation-promoting effect in vitro. ES-2 and SKOV3
cells were successfully transfected with siRNAs (si-KIF20A)
(Fig. 4B) and were assessed by the
cell proliferation assay (CCK-8 assay) as described above. KIF20A
knockdown significantly decreased the cell proliferation (Fig. 4C) (P<0.05). To further confirm
that KIF20A was involved in cell proliferation, we again performed
the CCK-8 assay using Paprotrain, which is a cell-permeable
acrylonitrile compound that inhibits KIF20A. As a result, treatment
with 100 µM of Paprotrain led to an ~50% decrease in the
proliferation ability (Fig. 4D)
(P<0.05) in the ES-2 and SKOV3 cells. In addition, we confirmed
that this proliferation-inhibitory effect was observed in a
concentration-dependent manner (Fig.
4E).
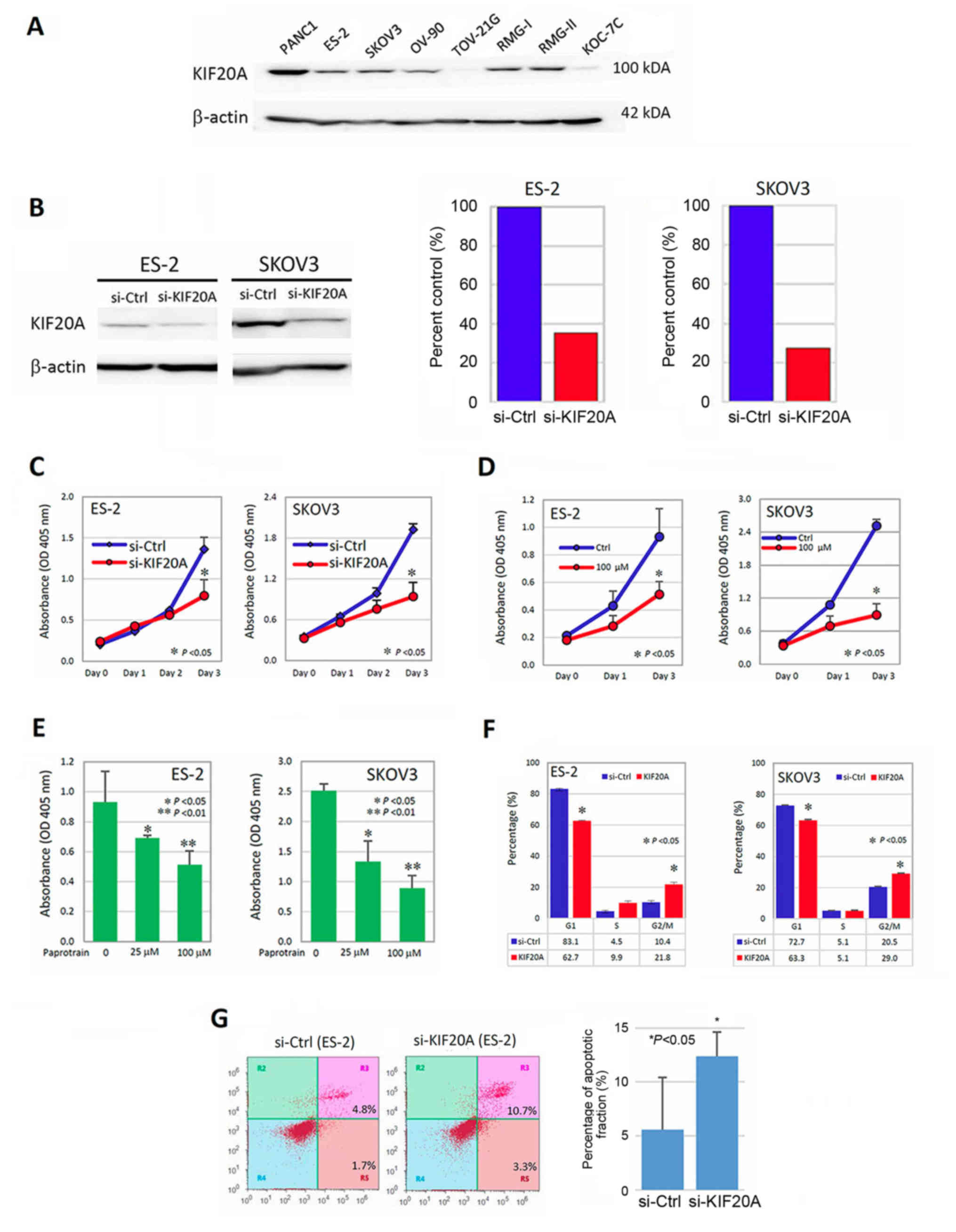 | Figure 4.Association between KIF20A expression
and the proliferation-promoting effect. (A) The expression of
KIF20A in various CCC or non-CCC cell lines. KIF20A was expressed
in ES-2, SKOV-3, OV-90, RMG-I and RMG-II cells. In TOV-21G and
KOC-7C cells, the expression of KIF20A was weak. PANC1 (pancreatic
cancer cells: positive control), ES-2, RMG-I, RMG-II, TOV-21G and
KOC-7C cells (CCC cells) and SKOV3, OV-90 (non-CCC ovarian
carcinoma cells) were used. (B) Western blotting and densitometric
analyses showing the inhibitory efficacy of KIF20A expressions by
siRNA (ES-2 and SKOV3). (C) The effect of KIF20A on cell
proliferation in ES2 and SKOV3 cells transfected with KIF20A-siRNA
(si-KIF20A) or control siRNA (si-ctrl) using Cell Counting Kit-8
(CCK-8). *P<0.05 indicates significance. (D) The
proliferation-inhibitory effect of Paprotrain, a cell-permeable
acrylonitrile compound that inhibits the kinesin-6 family member
KIF20A (time course). *P<0.05 indicates significance. (E) The
proliferation-inhibitory effect of Paprotrain was observed in a
concentration-dependent manner. *P<0.05, **P<0.01 indicate
significance. (F) Evaluation of the cell cycle distribution using
flow cytometric analysis. Suppression of KIF20A expression resulted
in an increase in the G2/M phase population and a decrease in the
G1 phase population, suggesting that knockdown of KIF20A induced
G2/M arrest (*P<0.05). (G) Enhancement of the apoptotic fraction
by the downregulation of KIF20A. In the si-KIF20A-transfected
cells, the apoptosis-induced fraction was higher than that in the
control-siRNA-transfected cells [(*P<0.05), respectively]. |
To determine the mitogenic effect of KIF20A, we then
performed cell-cycle analysis using ES2 and SKOV3 cells. The
distribution of the cell cycle was tested using flow cytometric
analysis. As shown in Fig. 4F, the
suppression of KIF20A expression led to the increase in the G2/M
phase population and decrease in the G1 phase population. This
observation suggested that knockdown of KIF20A induced the G2/M
arrest (P<0.05). We finally tested whether the downregulation of
KIF20A expression led to the enhanced apoptotic fraction using the
apoptosis assay. Consequently, in the si-KIF20A-transfected ES-2
cells, the apoptosis-induced fraction was higher than that in the
the control-siRNA transfected ES-2 cells [12.4±2.3 vs. 5.6±4.9%
(P<0.05), respectively] (Fig.
4G). These results indicate that KIF20A may be involved in the
mitogenic effect in CCC cells.
Discussion
In the present study, we first demonstrated that
KIF20A expression was significantly correlated with a poor
oncologic outcome in patients with ovarian CCC. Furthermore,
multivariate analyses demonstrated that a higher expression of
KIF20A was an independent prognostic indicator of a poorer PFS of
CCC patients. Up to the present, a number of studies have
demonstrated the important association between KIF20A expression
and aggressive phenotypes in several solid malignancies. Zhang
et al (24) demonstrated
that elevated KIF20A expression was associated with a number of
clinicopathological factors in cervical squamous cell carcinoma,
including HPV infection, stage, recurrence, lymphovascular space
involvement, nodal status, and poor outcome in patients with this
tumor, and concluded that aberrant KIF20A expression is a novel
independent unfavorable prognostic indicator that may be a
potential therapeutic target for cervical cancer. Liu et al
(25) reported that KIF20A was
aberrantly expressed in nasopharyngeal cancer, and that high KIF20A
protein expression was significantly correlated with poor 5-year OS
and PFS. The cumulative 5-year OS and PFS for the high
KIF20A-expressing group were 78.5 and 62.7%, respectively, and 95.9
and 90.8%, respectively, for the low or no KIF20A-expressing group.
In addition, Duan et al (31) reported the clinical effect of KIF20A
expression in 119 patients with glioma. They demonstrated that
patients with positive KIF20A expression showed significantly
poorer OS compared with patients with negative KIF20A expression
(median, 16.0 vs. 39.0 months, respectively). Our current results
are consistent with those of these previous studies. Similarly to
patients with EOC, those with CCC show an unfavorable prognosis,
principally attributable to its asymptomatic intraperitoneal
dissemination with or without distant metastases to parenchymal
organs (32). Our data were
obtained from a small number of patients, and therefore, the
prognostic significance of KIF20 needs to be confirmed in a larger
number of patients. At least, the present findings clarify that the
immunoreactive expression of KIF20A may be a critical indicator of
a poor prognosis in CCC patients, and its identification may result
in the selection of better strategic options.
Our current data indicated that KIF20A participated
in the growth of CCC cells. Furthermore, we demonstrated that
KIF20A regulates cell division, and the knockdown of KIF20A induced
apoptosis and cell cycle arrest via nuclear localization. In
addition, the present study showed that the inhibition of KIF20A
induced the multinucleation of cells, which ensures the inhibition
of cell division. KIF20A is required during mitosis exit for the
final step of cytokinesis, and its inhibitor, Paprotrain, inhibits
the recruitment of the surviving chromosome passenger proteins and
aurora B to the central spindle during the anaphase (33). A previous report demonstrated that
KIF20A plays a crucial role in the proliferation and tumor growth
of hepatocellular carcinoma as a novel downstream target of
glioma-associated oncogene 2 (Gli2) (26). This evidence prompted us to
hypothesize that the growth-inhibitory effect in KIF20A silencing
CCC cells may be partly attributable to the inhibition of activity
to drive the cell cycle. Moreover, tumor invasion and migration are
representative steps in the peritoneal dissemination of this tumor
(34,35). Stangel et al (15) reported that KIF20A silencing with
small interfering RNA molecules resulted in the inhibition of
motility and invasion of pancreatic cancer cell lines, as well as
the growth-promoting effect of KIF20A. It is possible that KIF20A
is involved in these multiple steps of the peritoneal metastasis of
CCC. We hope to clarify these unelucidated mechanisms of KIF20A in
CCC in our next investigation.
Additionally, CCC patients generally showed a very
low chemoresponse rate to platinum-based compounds, leading to
intrinsic chemoresistance (9–36). In
the present study, the majority of patients showing a higher
expression of KIF20A died of the disease [13/17 (76.4%)]. In
general, the remaining chemoresistant clone may be a cause of the
high rate of recurrence and/or cancer-related mortality. Thus, one
of the mainstream mechanisms leading to patients with KIF20A
expression showing an unfavorable clinical outcome may be based on
the chemoresistant hallmark as well as the growth-promoting effect
of KIF20A. Actually, Khongkow et al (22) revealed that paclitaxel targets the
FOXM1-KIF20A axis to drive abnormal mitotic spindle formation and
mitotic catastrophe, and that deregulations of FOXM1 and KIF20A
expression may be involved in the resistance to paclitaxel. Based
on our current result that silencing KIF20A expression induced the
upregulation of apoptosis in CCC cells, its knockdown may lead to
enhancement of the chemosusceptibility of this tumor, although we
did not investigate the direct correlation between KIF20A
expression and chemoresistance. Also, we hope to verify this
hypothesis in the next study in order to clarify the CCC-specific
biological hallmarks.
To the best of our knowledge, the present study is
the first to report that the expression of KIF20A was closely
associated with a poor oncologic outcome of patients with CCC. The
current findings may be based on the growth- and/or
chemoresistant-promoting effects of KIF20A, although further
investigation is needed to clarify its molecular mechanism.
Furthermore, KIF20A could be considered as an ideal cancer-testis
antigen and the KIF20A peptide may be a cancer vaccine for
pancreatic cancer. A phase I/II clinical trial using a peptide
vaccine derived from KIF20A revealed that patients with advanced
pancreatic cancer vaccinated with KIF20A-derived peptide had a
better prognosis than control patients (37,38).
From this point of view, the present study demonstrated the
possibility of using KIF20A-derived peptide vaccine for the
treatment of advanced CCC.
In summary, we identified KIF20A as a prognostic
indicator and therapeutic target in patients with CCC. However, the
detailed functions of KIF20A remain unclear. Particularly, we think
that the present study was preliminary because overexpression or
restoration assays and animal experiments have not been performed
to conclude the possible implication of KIF20A in the proliferation
of CCC. Further studies are needed in order to realize therapeutic
application. We believe that the mechanistic clarification of
KIF20A will help improve treatment for CCC patients by adding
criteria for the administration of systematic therapy in the
future.
Acknowledgements
The authors thank Mrs. Mai Sugiyama for her
technical support.
Funding
The present study was supported by the Japan Society
for the Promotion of Science (JSPS) Grant-in-Aid for Scientific
Research (24592512 and 15K10714 to KS).
Availability of data and materials
The datasets used during the present study are
available from the corresponding author upon reasonable
request.
Authors' contributions
KS and TS conceived and designed the study. YK
performed the experiments. YK and HK wrote the manuscript. KS
reviewed and edited the manuscript. SS, FU, KN and RS performed
data acquisition and curation. Supervision throughout this
manuscript was done by FK and TS. All authors read and approved the
manuscript and agree to be accountable for all aspects of the
research in ensuring that the accuracy or integrity of any part of
the work are appropriately investigated and resolved.
Ethics approval and consent to
participate
Patient's consent protocol was approved by the
Ethics Committee of Nagoya University (Nagoya, Japan).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
EOC
|
epithelial ovarian cancer
|
|
CCC
|
clear-cell carcinoma
|
|
FIGO
|
International Federation of Gynecology
and Obstetrics
|
|
OS
|
overall survival
|
|
PFS
|
progression-free survival
|
References
|
1
|
Kikkawa F, Nawa A, Ino K, Shibata K,
Kajiyama H and Nomura S: Advances in treatment of epithelial
ovarian cancer. Nagoya J Med Sci. 68:19–26. 2006.PubMed/NCBI
|
|
2
|
Brun JL, Feyler A, Chêne G, Saurel J, Brun
G and Hocké C: Long-term results and prognostic factors in patients
with epithelial ovarian cancer. Gynecol Oncol. 78:21–27. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chan JK, Teoh D, Hu JM, Shin JY, Osann K
and Kapp DS: Do clear cell ovarian carcinomas have poorer prognosis
compared to other epithelial cell types? A study of 1411 clear cell
ovarian cancers. Gynecol Oncol. 109:370–376. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ryu SY, Park SI, Nam BH, Kim I, Yoo CW,
Nam JH, Lee KH, Cho CH, Kim JH, Park SY, et al: Prognostic
significance of histological grade in clear-cell carcinoma of the
ovary: A retrospective study of Korean gynecologic oncology group.
Ann Oncol. 20:1032–1036. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gynecology JSoOa: Annual patient report.
Acta Obstet Gynaecologia Japonica. 68:1117–1160. 2016.
|
|
6
|
Jenison EL, Montag AG, Griffiths CT, Welch
WR, Lavin PT, Greer J and Knapp RC: Clear cell adenocarcinoma of
the ovary: A clinical analysis and comparison with serous
carcinoma. Gynecol Oncol. 32:65–71. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kennedy AW, Biscotti CV, Hart WR and
Webster KD: Ovarian clear cell adenocarcinoma. Gynecol Oncol.
32:342–349. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Satoh T, Oki A, Uno K, Sakurai M, Ochi H,
Okada S, Minami R, Matsumoto K, Tanaka YO, Tsunoda H, et al: High
incidence of silent venous thromboembolism before treatment in
ovarian cancer. Br J Cancer. 97:1053–1057. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sugiyama T, Kamura T, Kigawa J, Terakawa
N, Kikuchi Y, Kita T, Suzuki M, Sato I and Taguchi K: Clinical
characteristics of clear cell carcinoma of the ovary: A distinct
histologic type with poor prognosis and resistance to
platinum-based chemotherapy. Cancer. 88:2584–2589. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mizuno M, Kikkawa F, Shibata K, Kajiyama
H, Ino K, Kawai M, Nagasaka T and Nomura S: Long-term follow-up and
prognostic factor analysis in clear cell adenocarcinoma of the
ovary. J Surg Oncol. 94:138–143. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yan GR, Zou FY, Dang BL, Zhang Y, Yu G,
Liu X and He QY: Genistein-induced mitotic arrest of gastric cancer
cells by downregulating KIF20A, a proteomics study. Proteomics.
12:2391–2399. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhang Y, Liu J, Peng X, Zhu CC, Han J, Luo
J and Rui R: KIF20A regulates porcine oocyte maturation and early
embryo development. PLoS One. 9:e1028982014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Echard A, Jollivet F, Martinez O, Lacapere
JJ, Rousselet A, Janoueix-Lerosey I and Goud B: Interaction of a
Golgi-associated kinesin-like protein with Rab6. Science.
279:580–585. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lai F, Fernald AA, Zhao N and Le Beau MM:
cDNA cloning, expression pattern, genomic structure and chromosomal
location of RAB6KIFL, a human kinesin-like gene. Gene. 248:117–125.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Stangel D, Erkan M, Buchholz M, Gress T,
Michalski C, Raulefs S, Friess H and Kleeff J: Kif20a inhibition
reduces migration and invasion of pancreatic cancer cells. J Surg
Res. 197:91–100. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ho JR, Chapeaublanc E, Kirkwood L, Nicolle
R, Benhamou S, Lebret T, Allory Y, Southgate J, Radvanyi F and Goud
B: Deregulation of Rab and Rab effector genes in bladder cancer.
PLoS One. 7:e394692012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Imai K, Hirata S, Irie A, Senju S, Ikuta
Y, Yokomine K, Harao M, Inoue M, Tomita Y, Tsunoda T, et al:
Identification of HLA-A2-restricted CTL epitopes of a novel
tumour-associated antigen, KIF20A, overexpressed in pancreatic
cancer. Br J Cancer. 104:300–307. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kikuchi T, Daigo Y, Katagiri T, Tsunoda T,
Okada K, Kakiuchi S, Zembutsu H, Furukawa Y, Kawamura M, Kobayashi
K, et al: Expression profiles of non-small cell lung cancers on
cDNA microarrays: Identification of genes for prediction of
lymph-node metastasis and sensitivity to anti-cancer drugs.
Oncogene. 22:2192–2205. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Taniuchi K, Furihata M and Saibara T:
KIF20A-mediated RNA granule transport system promotes the
invasiveness of pancreatic cancer cells. Neoplasia. 16:1082–1093.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gasnereau I, Boissan M, Margall-Ducos G,
Couchy G, Wendum D, Bourgain-Guglielmetti F, Desdouets C, Lacombe
ML, Zucman-Rossi J and Sobczak-Thépot J: KIF20A mRNA and its
product MKlp2 are increased during hepatocyte proliferation and
hepatocarcinogenesis. Am J Pathol. 180:131–140. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Exertier P, Javerzat S, Wang B, Franco M,
Herbert J, Platonova N, Winandy M, Pujol N, Nivelles O, Ormenese S,
et al: Impaired angiogenesis and tumor development by inhibition of
the mitotic kinesin Eg5. Oncotarget. 4:2302–2316. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Khongkow P, Gomes AR, Gong C, Man EP,
Tsang JW, Zhao F, Monteiro LJ, Coombes RC, Medema RH, Khoo US and
Lam EW: Paclitaxel targets FOXM1 to regulate KIF20A in mitotic
catastrophe and breast cancer paclitaxel resistance. Oncogene.
35:990–1002. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zou JX, Duan Z, Wang J, Sokolov A, Xu J,
Chen CZ, Li JJ and Chen HW: Kinesin family deregulation coordinated
by bromodomain protein ANCCA and histone methyltransferase MLL for
breast cancer cell growth, survival, and tamoxifen resistance. Mol
Cancer Res. 12:539–549. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhang W, He W, Shi Y, Gu H, Li M, Liu Z,
Feng Y, Zheng N, Xie C and Zhang Y: High expression of KIF20A is
associated with poor overall survival and tumor progression in
early-stage cervical squamous cell carcinoma. PLoS One.
11:e01674492016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Liu SL, Lin HX, Qiu F, Zhang WJ, Niu CH,
Wen W, Sun XQ, Ye LP, Wu XQ, Lin CY, et al: Overexpression of
Kinesin family member 20A correlates with disease progression and
poor prognosis in human nasopharyngeal cancer: A retrospective
analysis of 105 patients. PLoS One. 12:e01692802017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Shi C, Huang D, Lu N, Chen D, Zhang M, Yan
Y, Deng L, Lu Q, Lu H and Luo S: Aberrantly activated Gli2-KIF20A
axis is crucial for growth of hepatocellular carcinoma and predicts
poor prognosis. Oncotarget. 7:26206–26219. 2016.PubMed/NCBI
|
|
27
|
Hosono S, Kajiyama H, Terauchi M, Shibata
K, Ino K, Nawa A and Kikkawa F: Expression of Twist increases the
risk for recurrence and for poor survival in epithelial ovarian
carcinoma patients. Br J Cancer. 96:314–320. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zeppernick F and Meinhold-Heerlein I: The
new FIGO staging system for ovarian, fallopian tube, and primary
peritoneal cancer. Arch Gynecol Obstet. 290:839–842. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chen VW, Ruiz B, Killeen JL, Cote TR, Wu
XC and Correa CN: Pathology and classification of ovarian tumors.
Cancer. 97:2631–2642. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Sakata J, Kajiyama H, Suzuki S, Utsumi F,
Niimi K, Sekiya R, Shibata K, Senga T and Kikkawa F: Impact of
positive ZEB1 expression in patients with epithelial ovarian
carcinoma as an oncologic outcome-predicting indicator. Oncol Lett.
14:4287–4293. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Duan J, Huang W and Shi H: Positive
expression of KIF20A indicates poor prognosis of glioma patients.
Onco Targets Ther. 9:6741–6749. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kajiyama H, Shibata K, Mizuno M, Yamamoto
E, Fujiwara S, Umezu T, Suzuki S, Nakanishi T, Nagasaka T and
Kikkawa F: Postrecurrent oncologic outcome of patients with ovarian
clear cell carcinoma. Int J Gynecol Cancer. 22:801–806. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Tcherniuk S, Skoufias DA, Labriere C, Rath
O, Gueritte F, Guillou C and Kozielski F: Relocation of Aurora B
and survivin from centromeres to the central spindle impaired by a
kinesin-specific MKLP-2 inhibitor. Angew Chem Int Ed Engl.
49:8228–8231. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kajiyama H, Shibata K, Terauchi M, Ino K,
Nawa A and Kikkawa F: Involvement of SDF-1alpha/CXCR4 axis in the
enhanced peritoneal metastasis of epithelial ovarian carcinoma. Int
J Cancer. 122:91–99. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Terauchi M, Kajiyama H, Yamashita M, Kato
M, Tsukamoto H, Umezu T, Hosono S, Yamamoto E, Shibata K, Ino K, et
al: Possible involvement of TWIST in enhanced peritoneal metastasis
of epithelial ovarian carcinoma. Clin Exp Metastasis. 24:329–339.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Shimada M, Kigawa J, Ohishi Y, Yasuda M,
Suzuki M, Hiura M, Nishimura R, Tabata T, Sugiyama T and Kaku T:
Clinicopathological characteristics of mucinous adenocarcinoma of
the ovary. Gynecol Oncol. 113:331–334. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Suzuki N, Hazama S, Ueno T, Matsui H,
Shindo Y, Iida M, Yoshimura K, Yoshino S, Takeda K and Oka M: A
phase I clinical trial of vaccination with KIF20A-derived peptide
in combination with gemcitabine for patients with advanced
pancreatic cancer. J Immunother. 37:36–42. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Asahara S, Takeda K, Yamao K, Maguchi H
and Yamaue H: Phase I/II clinical trial using HLA-A24-restricted
peptide vaccine derived from KIF20A for patients with advanced
pancreatic cancer. J Transl Med. 11:2912013. View Article : Google Scholar : PubMed/NCBI
|