Introduction
Molecular-targeted approaches using antibodies have
attracted tremendous interest for early diagnosis and new
therapeutic options for cancer, such as antibody-drug conjugate
(ADC) therapy, radioimmunotherapy (RIT) and photoimmunotherapy
(PIT). Molecular imaging techniques with certain monoclonal
antibody-based probes are being developed to distinguish tumors
from normal tissues by exploiting tumor-specific molecules.
Expression levels of the target molecules, however, may differ due
to the intrinsic heterogeneity of tumors, even among those derived
from similar organs. A better understanding of these
characteristics through non-invasive nuclear medicine imaging would
facilitate patient selection, improve selection of treatment
strategies, and help to predict treatment sensitivity.
Pancreatic cancer is a major life-threatening
disease with a 5-year survival rate of 8% for all stages combined
(1). It is predicted to be the
second leading cause of cancer-related deaths by 2030 (2). Therefore, there is an urgent need to
explore suitable target molecules and their related imaging and
therapeutic agents to facilitate early diagnosis and the selection
of an effective treatment for pancreatic cancer. Patients with
malignancies, including pancreatic cancer, have a higher risk of
venous thromboembolism than patients without malignancy (3,4).
Cancer coagulopathy is triggered by tissue factor (TF) (5–7). TF is
a transmembrane glycoprotein (47-kDa) present on the cell surface
that mediates a variety of physiologically and pathophysiologically
relevant functions. Its overexpression is associated with
thrombogenicity, tumor angiogenesis, cell signaling, tumor cell
proliferation and metastasis (7–9). TF is
a key element in the initiation of the extrinsic coagulation
cascade (10–12). Although TF normally safeguards
vascular integrity by inducing hemostasis upon injury, abnormal
expression of TF in various tumors is related to the malignant
cycle of blood coagulation (13–15).
Therefore, the malignant blood coagulation cycle is postulated to
generate versatile cancer stroma, leading to cancer invasion into
vessels, tumor proliferation, metastasis, hemorrhage, fibrin clot
formation and replacement with collagenous tissue (8,9,16,17).
A wide variety of malignancies, including pancreatic cancer,
exhibit aberrant TF expression (18–20).
In addition, high TF expression in pancreatic cancer has been
revealed to be correlated with tumor grade, extent, metastasis and
invasion, in contrast to normal pancreas with low TF expression
(12,19,21,22).
Haas et al evaluated TF expression in eight human pancreatic
cancer cell lines, including BxPC-3, and reported aberrant TF
expression at both the RNA and protein levels (5). In parallel with TF expression in the
cell lines, they also demonstrated that most of the tissue
specimens from pancreatic cancer patients had highly variable TF
expression when determined by immunofluorescence staining (5). Furthermore, TF was expressed not only
on the tumor cell surface, but also in the tumor stroma (11) and on tumor-associated vascular
endothelial cells (23).
TF is a potential target for cancer diagnostic
imaging or therapy, and high-affinity anti-TF antibodies have been
developed (24). Application of
anti-TF monoclonal antibody 1849 (rat IgG2b), which
reacts with human TF antigen, to ADC demonstrated superior
antitumor activity in pancreatic cancer xenograft models (25). In addition, we successfully
visualized TF-expressing orthotopic glioma in a mouse xenograft
model using an 111In-labeled anti-TF antibody 1849
(111In-1849) probe (26). The relationship between tumor uptake
of the probe and TF expression levels, however, has not yet been
analyzed.
In the present study, we investigated the in
vitro binding of the 111In-1849 probe to five
pancreatic cancer cell lines, BxPC-3, BxPC-3-TF-knockout
(BxPC-3-TFKO), Capan-1, PSN-1 and SUIT-2, which have different TF
expression profiles. We also evaluated the in vivo uptake of
the probe in xenograft tumors derived from these cell lines in
biodistribution studies. The relationship of TF expression with
cell binding and tumor uptake of 111In-1849 was
evaluated by regression analysis.
Materials and methods
Cells
Human pancreatic cancer cell lines (BxPC-3, Capan-1
and PSN-1) were obtained from the American Type Culture Collection
(ATCC; Manassas, VA, USA). SUIT-2 cells were obtained from the
Japanese Collection of Research Bioresources Cell Bank (Osaka,
Japan) (27). The TF gene of BxPC-3
was disrupted using the CRISR/Cas9 system with a CRISPR plasmid
(U6-gRNA/CMV-Cas9-GFP; Sigma-Aldrich; Merck KGaA, Darmstadt,
Germany) and Lipofectamine LTX and PLUS reagent (Thermo Fisher
Scientific, Inc., Waltham, MA, USA) according to the manufacturer's
protocol, and the established cell line was named BxPC-3-TFKO.
BxPC-3 and BxPC-3-TFKO were maintained in RPMI-1640 medium (Wako
Pure Chemical Industries, Ltd., Osaka, Japan) supplemented with 10%
fetal bovine serum (FBS; Sigma-Aldrich; Merck KGaA) in a humidified
incubator maintained at 37°C with 5% CO2. PSN-1 and
SUIT-2 were maintained in Dulbecco's modified Eagle's medium (DMEM;
Wako Pure Chemical Industries, Ltd.) supplemented with 10% FBS.
Capan-1 was maintained in Iscove's modified Dulbecco's medium
(IMDM; Wako Pure Chemical Industries, Ltd.) supplemented with 20%
FBS.
TF protein expression analysis by
immunofluorescence staining
Immunofluorescence staining was conducted as
previously described (28,29). Briefly, cells were grown on glass
coverslips and fixed in cold methanol for 5 min. Non-specific
binding was blocked by applying Block Ace reagent (Dainippon
Pharmaceutical Co., Ltd., Osaka, Japan) with 10% goat serum for 30
min at room temperature. Cells were incubated with anti-TF antibody
1849 (rat IgG2b) (26,30) as
a primary antibody overnight at 4°C. A secondary anti-rat antibody
conjugated with Cy3 (diluted 1:1,000; cat. no. 109-165-003; Jackson
ImmunoResearch Laboratories, West Grove, PA, USA) was applied for
30 min at room temperature. Nuclei were stained with
4′,6-diamidino-2-phenylindole (DAPI) in mounting medium (Vector
Laboratories, Inc., Burlingame, CA, USA). Images were obtained with
an exposure time of 0.017 sec for detecting TF using a fluorescence
microscope (Olympus Corp., Tokyo, Japan). Signal intensities of
fifteen cells of each cell line's image were measured using ImageJ
software (ver. 1.46r; NIH; National Institutes of Health, Bethesda,
MD, USA). The mean ± SD value was used as an index of TF protein
expression.
Radiolabeling of the antibody
To label the single-photon emission computed
tomography (SPECT) tracer 111In-labeled anti-TF antibody
1849 (111In-1849), the antibody was first conjugated
with a chelating agent, p-SCN-Bn-CHX-A″-DTPA (DTPA)
(Macrocyclics, Inc., Dallas, TX, USA) as previously described
(31). The DTPA-conjugated antibody
was purified using a Sephadex G-50 (GE Healthcare, Little Chalfont,
UK) column (centrifuged once at 700 × g for 2 min). The conjugation
ratio of DTPA to the antibody was estimated to be ~1.5 based on
cellulose acetate electrophoresis. Typically, the DTPA-conjugated
antibody (50 µg) was mixed with 1.48 MBq of indium-111 chloride
(111InCl3; Nihon Medi-Physics, Tokyo, Japan)
in 0.5 M acetate buffer (pH 6.0) and the mixture was incubated for
30 min at room temperature. The radiolabeled antibody was separated
from free 111In using a Sephadex G-50 column
(centrifuged at 700 × g for 2 min). The labeling yield of
111In-1849 ranged from 82.4 to 85.8%, the radiochemical
purity was 100%, and the specific activity was 24.2–25.4
kBq/µg.
In vitro binding assay
Cell binding of five cell lines (BxPC-3,
BxPC-3-TFKO, Capan-1, PSN-1 and SUIT-2) was examined as previously
described (32). Briefly, in the
cell binding assay, 3–4 days after seeding, the cells were detached
and cell suspensions prepared (1.0×107,
5.0×106, 2.6×106, 1.3×106,
6.3×105, 3.1×105, 1.6×105,
7.8×104 and 3.9×104) in phosphate-buffered
saline (PBS) with 1% bovine serum albumin (BSA; Sigma-Aldrich;
Merck KGaA). The suspension was incubated with
111In-1849 on ice for 60 min. After washing, the
radioactivity bound to cells was assessed with a gamma counter
(ARC-370; Aloka Medical, Ltd., Tokyo, Japan). The association
between cell binding at 5×106 cells and TF expression
was evaluated by simple regression analysis using GraphPad Prism 6
(GraphPad Software, Inc., La Jolla, CA, USA).
Subcutaneous tumor mouse model
The animal experimental protocol was approved by the
Animal Care and Use Committee of the National Institute of
Radiological Sciences (Chiba, Japan), and all animal experiments
were conducted in accordance with the Guidelines Regarding Animal
Care and Handling of the National Institute of Radiological
Sciences. Thirty BALB/cA Jcl-nu/nu male mice (5 weeks old, 18–20 g;
CLEA Japan, Inc., Tokyo, Japan) were maintained under specific
pathogen-free conditions. Mice (6 mice/each model) were
subcutaneously inoculated in the left shoulder with BxPC-3
(4×106), BxPC-3-TFKO (1×106), Capan-1
(1×106), PSN-1 (1×106) and SUIT-2
(1×106) cells under isoflurane anesthesia. Animals were
maintained at controlled temperature (23±3°C) and humidity (50±20%)
under a 12/12-h light/dark cycle. Animals were provided food and
water ad libitum. We employed mice in which subcutaneous
tumors reached a diameter of ~9 mm.
In vivo SPECT/CT imaging with
111In-1849
For SPECT imaging, a mouse (n=1/tumor model) was
injected with ~1.85 MBq of 111In-1849 into a tail vein.
The injected protein dose was adjusted to 50 µg/mouse by adding the
intact antibody. At 1, 2, 3 and 4 day(s) after the injection, the
mice were anesthetized by isoflurane inhalation and imaged using a
VECTor/CT SPECT/CT Pre-Clinical Imaging system with a multi-pinhole
collimator (MILabs, Utrecht, The Netherlands). SPECT data were
acquired for 15 min on day 1, 20 min on day 2, 25 min on day 3, and
30 min on day 4 after injection, taking into account the half-life
of In-111. SPECT images were reconstructed using a pixel-based
ordered-subsets expectation maximization algorithm with eight
subsets and two iterations on a 0.8-mm voxel grid without
attenuation correction. Computed tomography data were acquired with
an X-ray source set at 60 kVp and 615 µA after SPECT scan and
images were reconstructed using a filtered back-projection
algorithm for cone beam. Merged images were obtained using PMOD
software (ver. 3.6; PMOD Technologies GmbH, Zürich, Switzerland).
The region of interest was manually drawn over tumors and tracer
uptake was quantified as the percentage of injected dose per gram
of tissue (%ID/g) using the PMOD software.
Biodistribution of
111In-1849
When subcutaneous tumors reached a diameter of ~10
mm, the mice (n=5/tumor model) were intravenously injected with 37
kBq of 111In-1849. The total injected protein dose was
adjusted to 50 µg/mouse by adding the intact antibody.
Biodistribution experiments for 111In-1849 were
conducted on day 4 after the injection because the largest
difference in tumor uptake of 111In-1849 was observed on
day 4 in the immuno-SPECT imaging studies. Five mice for each tumor
model were sacrificed by isoflurane inhalation and blood was
obtained from the heart. Tumors and organs of interest (blood,
brain, heart, lung, liver, spleen, pancreas, stomach, intestine,
kidney, muscle and bone) were removed and weighed, and
radioactivity counts were measured using the gamma counter. The
data were expressed as %ID/g normalized to a 20-g body weight
mouse. Tumor uptake data were analyzed by two-way repeated-measures
ANOVA, followed by Student-Newman-Keuls (SNK) test. The association
between tumor uptake and TF expression was evaluated by simple
regression analysis using GraphPad Prism 6 (GraphPad Software,
Inc).
Results
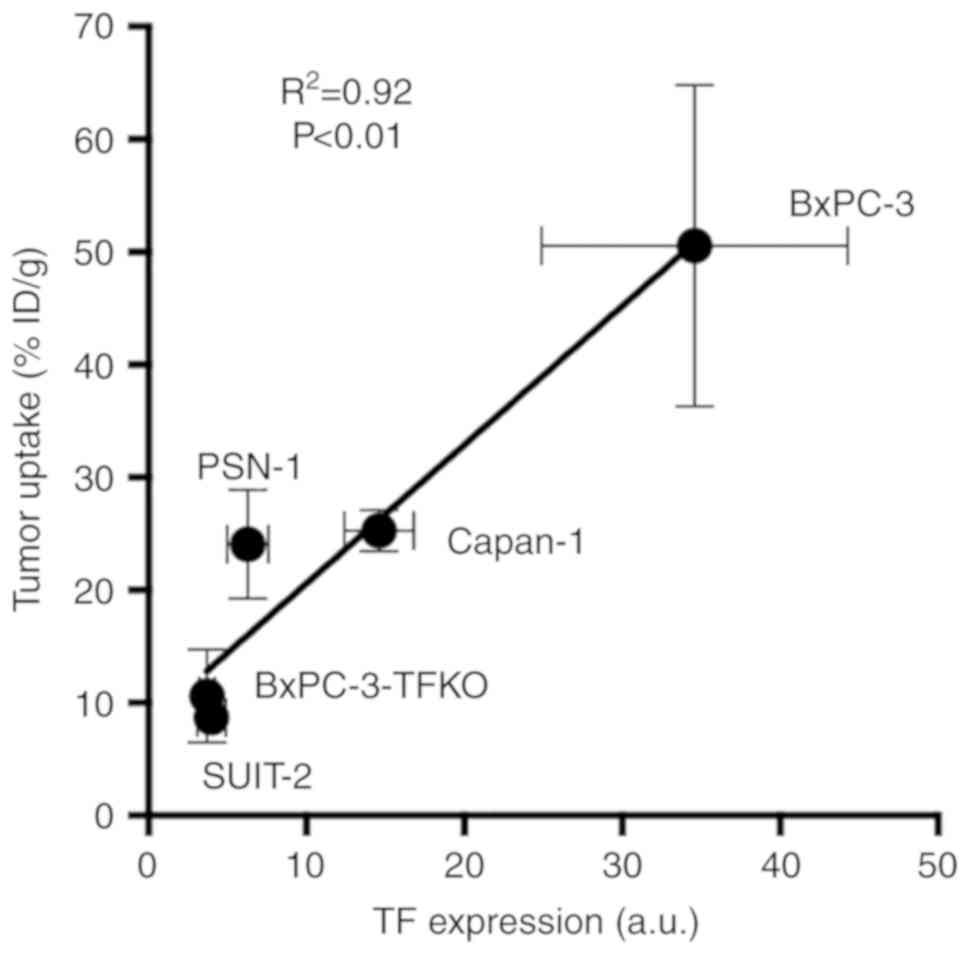
TF protein expression in pancreatic
cancer cells
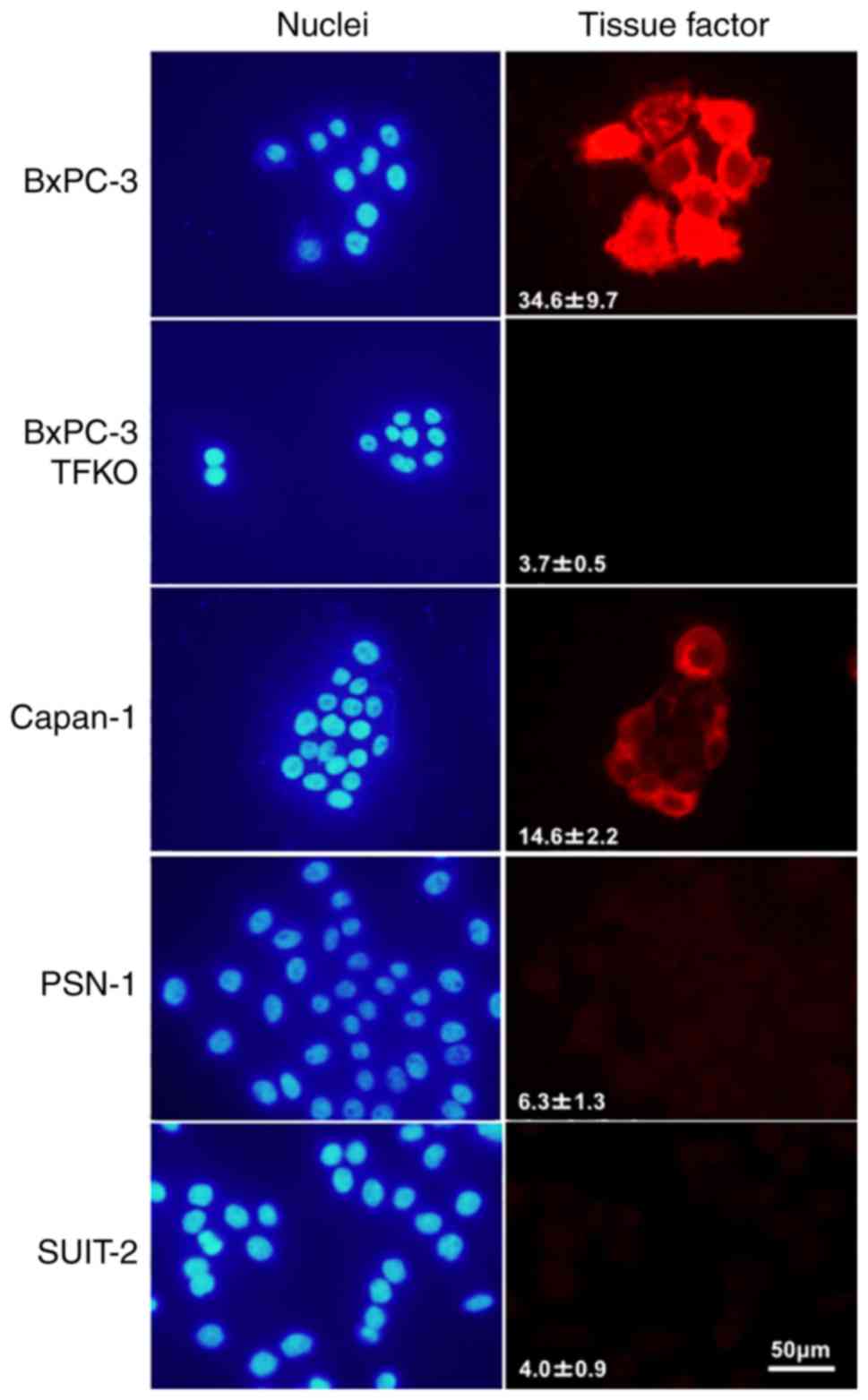
TF protein expression levels in five human
pancreatic cancer cell lines (BxPC-3, BxPC-3-TFKO, Capan-1, PSN-1
and SUIT-2) were determined by measuring the signal intensities of
the cells visualized by immunofluorescence. BxPC-3 had the highest
expression, followed by Capan-1, PSN-1, SUIT-2 and BxPC-3-TFKO
(Fig. 1).
 | Figure 1.TF protein expression analysis of
pancreatic cancer cells, BxPC-3, BxPC-3-TFKO, Capan-1, PSN-1 and
SUIT-2. TF protein expression was determined based on the mean
fluorescence signal intensities of five cells from each cell line
after immunofluorescence staining with the anti-TF antibody (red,
right panels). Signal intensity of TF staining (arbitrary unit) is
displayed in the right panels. DAPI stained nuclei (blue, left
panels). Scale bar, 50 µm. TF, tissue factor; BxPC-3-TFKO,
BxPC-3-TF-knockout; DAPI, 4′,6-diamidino-2-phenylindole. |
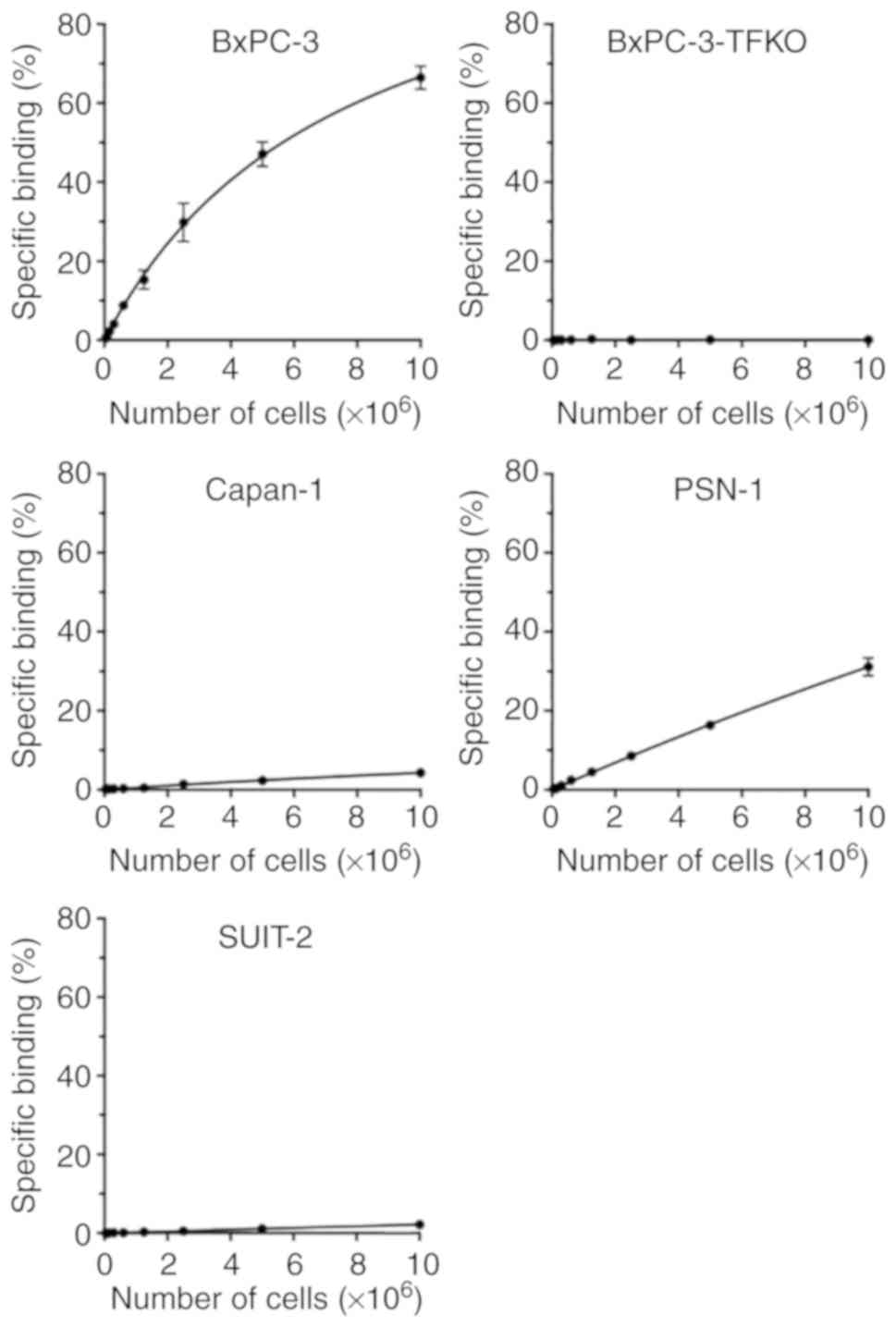
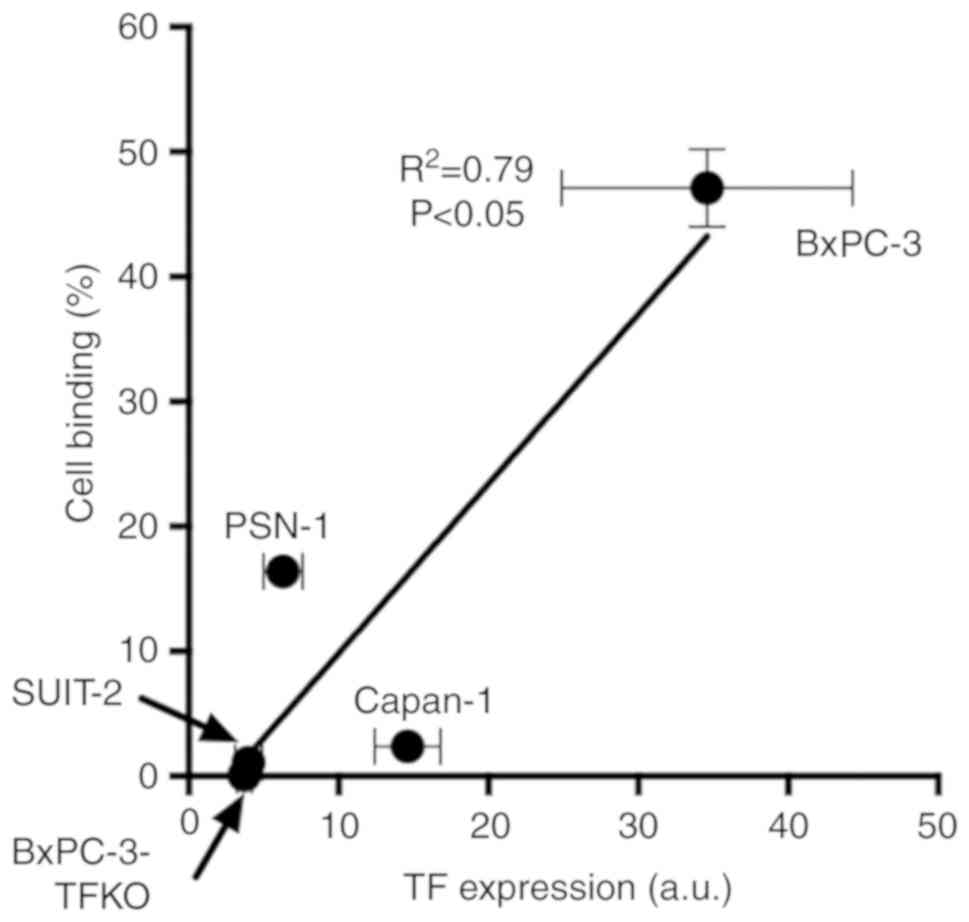
Cell binding of
111In-labeled anti-TF antibody 1849
Of the five cell lines, 111In-1849 had
the highest binding to BxPC-3 cells, followed by PSN-1, Capan-1 and
SUIT-2 (Fig. 2). No cell binding
was observed in BxPC-3-TFKO cells (Fig.
2). TF protein expression was significantly associated with the
cell binding when cell preparations seeded at 5×106
cells were used for the regression analysis (R2=0.79,
P<0.05; Fig. 3).
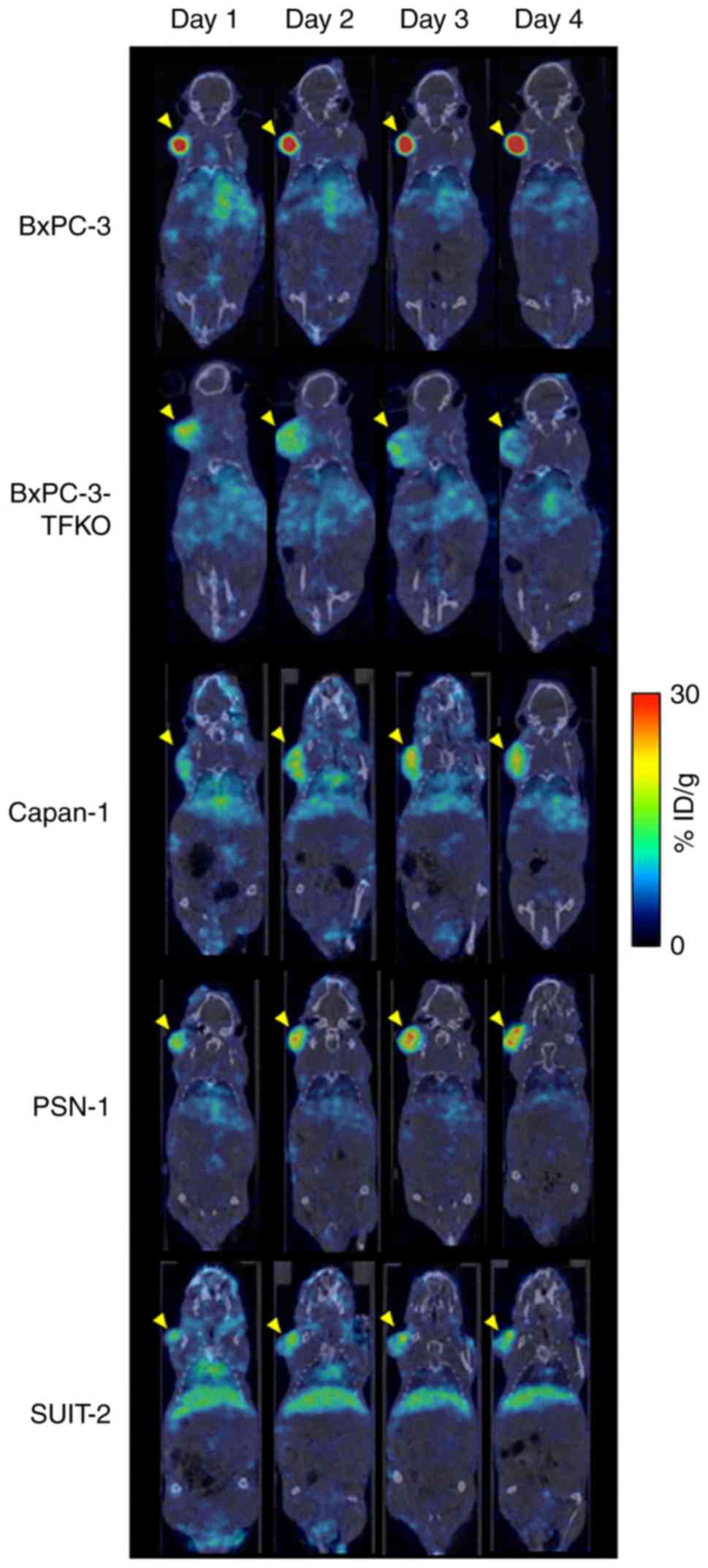
SPECT/CT imaging with
111In-1849 in tumor-bearing mice
SPECT/CT images in subcutaneous tumor mouse models
bearing BxPC-3, BxPC-3-TFKO, Capan-1, PSN-1 and SUIT-2 tumors were
obtained on days 1, 2, 3 and 4 after injection of
111In-1849. On day 1, high BxPC-3 tumor uptake of
24.9%ID/g was observed and thereafter the uptake increased with
time, whereas the background activity continued to decrease,
resulting in increased contrast of BxPC-3 tumors over time
(Fig. 4). On day 4, BxPC-3 tumor
uptake was highest (62.3%ID/g) and PSN-1 tumor uptake was second
highest (18.1%ID/g), followed by Capan-1 (15.2%ID/g), SUIT-2
(9.1%ID/g) and BxPC-3-TFKO tumor (9.1%ID/g; Fig. 4). Tumor uptake in PSN-1 and Capan-1
increased with time like BxPC-3, whereas that of BxPC-3-TFKO and
SUIT-2 decreased with time (Fig.
4).
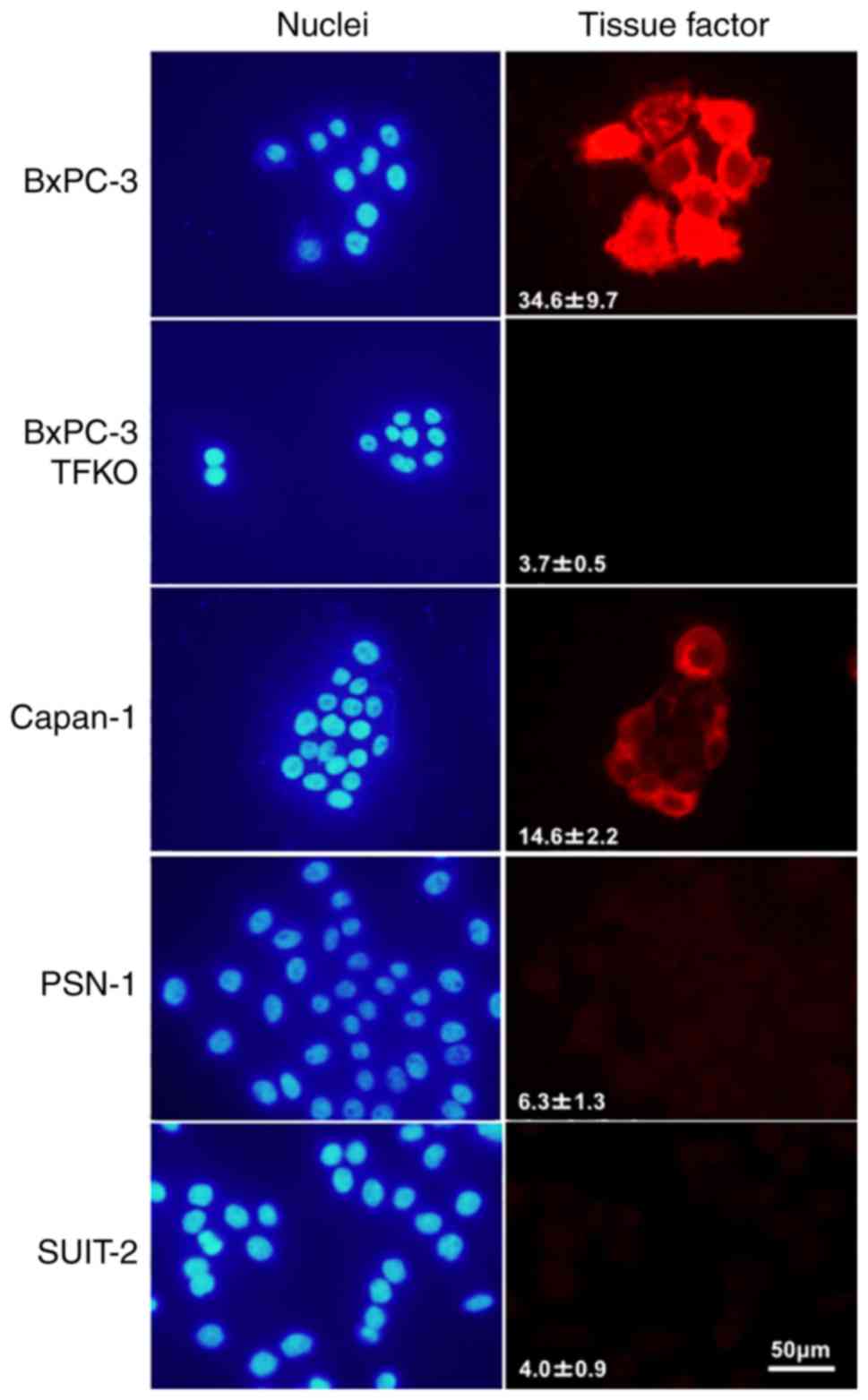
In vivo biodistribution of
111In-1849
Biodistribution experiments for
111In-1849 were conducted in nude mice bearing xenograft
tumors on day 4 after injection. Tumor uptake of
111In-1849 was 50.58±14.26%ID/g in BxPC-3,
10.59±4.15%ID/g in BxPC-3-TFKO, 25.26±1.84%ID/g in Capan-1,
24.05±4.86%ID/g in PSN-1, and 8.68±0.52%ID/g in SUIT-2 tumors
(Table I). BxPC-3 tumor uptake was
significantly higher than that of the others (P<0.01; Table I). In all mice, the uptake of
111In-1849 in the major normal organs, including the
liver and kidney, was relatively low (Table I). TF protein expression was
significantly associated with the tumor uptake (R2=0.92,
P<0.01; Fig. 5).
 | Table I.Biodistribution of
111In-1849 in mice bearing pancreatic cancer tumors on
day 4. |
Table I.
Biodistribution of
111In-1849 in mice bearing pancreatic cancer tumors on
day 4.
|
| BxPC-3 | BxPC-3-TFKO | Capan-1 | PSN-1 | SUIT-2 |
|---|
| Blood | 10.12±2.67 | 12.48±1.99 | 13.95±1.89 | 10.68±4.56 | 11.86±2.44 |
| Brain | 0.33±0.08 | 0.36±0.15 | 0.39±0.14 | 0.31±0.13 | 0.40±0.12 |
| Heart | 3.29±0.65 | 3.37±0.62 | 3.74±0.56 | 2.83±0.88 | 3.30±0.79 |
| Lung | 4.96±1.07 | 5.10±1.35 | 6.39±0.86 | 4.54±1.62 | 5.19±1.07 |
| Liver | 6.30±0.87 | 6.99±0.77 | 6.42±0.80 | 5.87±0.32 | 7.85±1.89 |
| Spleen | 6.07±2.29 | 5.39±2.29 | 7.04±0.76 | 5.70±2.08 | 5.92±1.58 |
| Pancreas | 1.35±0.29 | 1.26±0.28 |
1.85±0.20a | 1.27±0.46 | 1.39±0.30 |
| Stomach | 1.31±0.30 | 1.44±0.28 | 1.75±0.37 | 1.19±0.39 | 1.40±0.22 |
| Intestine | 1.68±0.47 | 1.69±0.30 | 2.05±0.14 | 1.51±0.57 | 1.60±0.38 |
| Kidney | 4.17±0.95 | 3.89±0.64 | 4.55±0.57 | 3.28±1.10 | 3.74±0.46 |
| Muscle | 0.91±0.23 | 0.80±0.17 | 1.06±0.17 | 0.83±0.26 | 0.87±0.17 |
| Bone | 2.85±0.89 | 2.33±0.74 | 3.44±0.48 | 2.42±1.11 | 2.54±0.64 |
| Tumor | 50.58±14.26 |
10.59±4.15b | 25.26±1.84
b |
24.05±4.86b |
8.68±0.52b |
Discussion
Specific probes targeting specific molecules or
genetic abnormalities are highly desired for improving the
diagnostic and treatment efficiency of pancreatic cancer, which has
a dismal clinical outcome. Generally, to visualize cancer with a
targeted molecular imaging approach, tumor-specific targets with
sufficient expression are important for distinguishing lesions from
the surrounding environment, and antibodies are favorable
candidates due to their excellent specific binding affinity with
compatible antigens and slow rate of disassociation.
The present study aimed to evaluate whether tumor
uptake of our monoclonal antibody-based single-photon emission
computed tomography (SPECT) probe 111In-1849 could
reflect differences in the tissue factor (TF) expression levels in
certain pancreatic cancer models. Various expression levels of TF
have been detected in several human pancreatic cancer cell lines
(5). In the present study, the TF
expression profiles of five human pancreatic cancer cell lines
[BxPC-3, BxPC-3-TF-knockout (BxPC-3-TFKO), Capan-1, PSN-1 and
SUIT-2] were analyzed by immunofluorescence examination. In good
agreement with previous studies, BxPC-3 had the highest signal
intensity indicating the highest TF expression among the five cell
lines, followed by Capan-1, PSN-1, SUIT-2 and BxPC-3-TFKO (Fig. 1). These cell lines are considered
suitable for the purposes of the present study. The cell binding of
111In-labeled anti-TF antibody 1849
(111In-1849) to each cell line (Fig. 2) related to the TF expression
measured from the signal intensities of cells visualized by
immunofluorescence (Fig. 3).
SPECT/CT studies in tumor-bearing mice were
conducted to evaluate the temporal change in 111In-1849
uptake and to determine the temporal kinetics of the
biodistribution. The largest difference in tumor uptake was
observed on day 4. Therefore, the biodistribution studies were
conducted at that time-point. In the biodistribution studies, tumor
uptake ranged from 8.68 to 50.58% ID/g; BxPC-3 had the highest
uptake and SUIT-2 the lowest (Table
I). TF protein expression was significantly associated with the
tumor uptake (Fig. 5). Moreover,
the biodistribution studies revealed that 111In-1849
uptake in the surrounding normal organs, including the liver,
spleen and kidneys, which are the major organs involved in the
elimination of the probe, and the pancreas, was relatively low
(Table I). Therefore, the
pharmacokinetics of 111In-1849 produced minimal
background, providing a high-contrast image of tumors with
111In-1849 in mice bearing pancreatic cancer
xenografts.
Higher TF-expressing cancer tissue may be more
accessible to administered 111In-1849 than lower
TF-expressing tumors. The present findings suggest that
111In-1849 will be an excellent probe for non-invasive
imaging of TF-expression. 111In-1849 accumulates in
tumors with TF expression based on both active and passive
targeting. BxPC-3-TFKO tumors exhibited a little accumulation of
111In-1849, probably due to passive enhanced
permeability and retention in tumors (33).
We previously proposed TF as an alternative
potential target for the diagnosis and treatment of cancer. The
Alexa Fluor®−647-labeled anti-TF antibody 1849 probe was
used for fluorescence imaging in a pancreatic cancer xenograft
model (24), and the
111In-1849 probe for immuno-SPECT imaging in a glioma
model (26). Hong et al
developed a radiotracer, 64Cu-labeled chimeric
anti-human TF monoclonal antibody, for immuno-positron emission
tomography (PET) imaging of in vivo TF expression in
pancreatic cancer models (34). PET
has higher sensitivity (10−11−10−12 mole/l)
than SPECT (10−10−10−11 mole/l) (35). A gamma-emitting radionuclide such as
111In for immuno-SPECT is easier to obtain than a
positron-emitting radionuclide, such as 64Cu or
89Zr for PET because 111In is widely used in
routine clinical nuclear medicine practice. The higher sensitivity
of PET allows for the detection of smaller tumors compared with
SPECT (36), whereas SPECT provides
sufficient quality images to interpret disease in routine use and
can be more easily conducted in clinics. Both SPECT and PET have
potential application in many clinical situations, and further
clinical studies are needed to clarify the role of
111In-1849 immuno-SPECT in clinical oncology
imaging.
Some research groups (19,22)
evaluated the correlations between the expression of TF and
clinicopathologic characteristics. Nitori et al reported
that TF expression is a useful prognostic marker in pancreatic
cancer patients, and that the identification of molecules that
could predict a poor prognosis is critical for selecting patients
who would benefit from radical treatment or molecular targeting
therapy (22). Mainly
immunohistochemical examination of tumor tissue sections has been
performed to assess target expression. The technique is limited to
measuring the expression in a whole tumor region, however, due to
biopsy-associated pitfalls and the requirement of multiple invasive
procedures. Moreover, target expression may change over time as a
result of tumor growth and therapy and thus differ between primary
lesions and metastatic foci, and these variabilities are difficult
to capture utilizing techniques other than non-invasive imaging.
Nuclear medicine imaging using target-specific and sensitive probes
offers accurate and real-time measurement of protein expression in
a whole tumor because the imaging is sensitive for quantitative
assessment of heterogeneous expression and spatiotemporal variance
in target expression. Therefore, our radiolabeled anti-TF antibody
1849 has potential utility as a novel probe for predicting which
patients are most likely to respond to TF-targeted therapeutic
approaches.
TF-targeted therapeutic approaches can be applied to
antibody-drug conjugate (ADC) therapy, radioimmunotherapy (RIT) and
photoimmunotherapy (PIT). Active targeting of a specific antibody
to tumor antigens would enhance the delivery of anticancer
candidates (drugs, radionuclides and photosensitizers) to tumor
tissues and promote the therapeutic effect. We as well as other
groups have reported the usefulness of anti-TF monoclonal antibody
in cancer therapy (25,37,38).
The anticancer effect of TF-specific ADCs comprising anti-TF
antibodies linked to the cytotoxic agent monomethyl auristatin E
was demonstrated in pancreatic tumor xenografts (25) and a broad range of solid tumors
xenograft models (37). In
contrast, RIT using an antibody labeled with a suitable
radionuclide that emits β- or α-radiation to produce cytotoxic
effects in target cells is increasingly used for internal
radiotherapy (39); Wang et
al labeled the anti-TF antibody with a β-emitter yttrium-90 and
reported its radiotherapeutic effect on human xenograft non-small
cell lung cancer tumors in nude mice (38). PIT is also an advanced alternative
molecular-targeted cancer therapy exerting highly selective cancer
cell death after systemic administration of a
photosensitizer-conjugated antibody targeting tumor-associated
innate antigens and subsequent exposure of light with an
appropriate wavelength. We recently investigated the
photoimmunotherapeutic effect induced by anti-TF antibody 1849
conjugated to a photosensitizer, indocyanine green, in a
TF-expressing BxPC-3 pancreatic cancer model (40). TF-targeted therapies such as ADC,
RIT and PIT have desirable prospects, and patient selection for
these therapeutic options may be based on TF expression. Our
immuno-SPECT imaging helps to reliably visualize and even quantify
the expression of the target molecule TF in a non-invasive and
repeatable manner. This could ultimately be translated to clinical
use, and would enable physicians to make more informed decisions
regarding treatment options, patient entry and follow-up. Although
the potential utility of 111In-1849 as a novel probe in
preclinical studies was demonstrated, some modifications, such as
the development of a humanized form of the antibody, are desirable
to facilitate adoption of this imaging technique and its success in
clinical use.
The present study has some limitations: Only one
mouse per tumor model was used for SPECT imaging. The clinical
effect of anti-TF antibody 1849 on normal tissue could not be
accurately assessed since 1849 does not recognize murine TF.
Associations between 111In-1849 uptake and
histopathological characteristics or neoplastic tumor grade were
not evaluated. Further studies are required to resolve these
issues.
In summary, this proof-of-concept study with in
vitro and in vivo experiments demonstrated that
immuno-SPECT using 111In-labeled anti-TF antibody 1849
could become a unique imaging modality for non-invasive
visualization of the TF expression profile in pancreatic cancer.
This novel imaging strategy will likely have an important role in
the diagnosis and selection of therapeutic strategies for
personalized therapy in the clinic.
Acknowledgements
We thank Yuriko Ogawa and Naoko Kuroda (QST-NIRS)
for technical assistance, and staff at the Laboratory Animal
Sciences section for animal management in QST-NIRS.
Funding
The present study was supported in part by KAKENHI
17K10497 and 18H02774.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
WA, ABT, TS and TH were involved in the conception
and design of the study. AS, ABT and HS performed the experiments;
AS, ABT and HS analyzed the data; WA, ABT, TS and TH interpreted
data; HT, MY and YM provided the anti-TF antibody; AS, WA and MY
drafted and wrote the manuscript; ABT, HT, YM, TS and TH reviewed
and edited the manuscript. All authors read and approved the
manuscript and agree to be accountable for all aspects of the
research in ensuring that the accuracy or integrity of any part of
the work are appropriately investigated and resolved.
Ethics approval and consent to
participate
The animal experimental protocol was approved by the
Animal Care and Use Committee of the National Institute of
Radiological Sciences (Chiba, Japan), and all animal experiments
were conducted in accordance with the Guidelines Regarding Animal
Care and Handling of the National Institute of Radiological
Sciences.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
ADC
|
antibody-drug conjugate
|
|
DAPI
|
4′,6-diamidino-2-phenylindole
|
|
PBS
|
phosphate-buffered saline
|
|
PET
|
positron emission computed
tomography
|
|
PIT
|
photoimmunotherapy
|
|
RIT
|
radioimmunotherapy
|
|
SD
|
standard deviation
|
|
SPECT
|
single-photon emission computed
tomography
|
|
TF
|
tissue factor
|
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2018. CA Cancer J Clin. 68:7–30. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rahib L, Smith BD, Aizenberg R, Rosenzweig
AB, Fleshman JM and Matrisian LM: Projecting cancer incidence and
deaths to 2030: The unexpected burden of thyroid, liver, and
pancreas cancers in the United States. Cancer Res. 74:2913–2921.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Stein PD, Beemath A, Meyers FA, Skaf E,
Sanchez J and Olson RE: Incidence of venous thromboembolism in
patients hospitalized with cancer. Am J Med. 119:60–68. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Woei-A-Jin FJ, Tesselaar ME, Garcia
Rodriguez P, Romijn FP, Bertina RM and Osanto S: Tissue
factor-bearing microparticles and CA19.9: Two players in pancreatic
cancer-associated thrombosis? Br J Cancer. 115:332–338. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Haas SL, Jesnowski R, Steiner M, Hummel F,
Ringel J, Burstein C, Nizze H, Liebe S and Löhr JM: Expression of
tissue factor in pancreatic adenocarcinoma is associated with
activation of coagulation. World J Gastroenterol. 12:4843–4849.
2006.PubMed/NCBI
|
|
6
|
Steffel J, Luscher TF and Tanner FC:
Tissue factor in cardiovascular diseases: Molecular mechanisms and
clinical implications. Circulation. 113:722–731. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
van den Berg YW, Osanto S, Reitsma PH and
Versteeg HH: The relationship between tissue factor and cancer
progression: Insights from bench and bedside. Blood. 119:924–932.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Leppert U and Eisenreich A: The role of
tissue factor isoforms in cancer biology. Int J Cancer.
137:497–503. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kasthuri RS, Taubman MB and Mackman N:
Role of tissue factor in cancer. J Clin Oncol. 27:4834–4838. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Drake TA, Morrissey JH and Edgington TS:
Selective cellular expression of tissue factor in
human-tissues-implications for disorders of hemostasis and
thrombosis. Am J Pathol. 134:1087–1097. 1989.PubMed/NCBI
|
|
11
|
Vrana JA, Stang MT, Grande JP and Getz MJ:
Expression of tissue factor in tumor stroma correlates with
progression to invasive human breast cancer: Paracrine regulation
by carcinoma cell-derived members of the transforming growth factor
beta family. Cancer Res. 56:5063–5070. 1996.PubMed/NCBI
|
|
12
|
Khorana AA, Ahrendt SA, Ryan CK, Francis
CW, Hruban RH, Hu YC, Hostetter G, Harvey J and Taubman MB: Tissue
factor expression, angiogenesis, and thrombosis in pancreatic
cancer. Clin Cancer Res. 13:2870–2875. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Matsumura Y, Kimura M, Yamamoto T and
Maeda H: Involvement of the kinin-generating cascade in enhanced
vascular permeability in tumor tissue. Jpn J Cancer Res.
79:1327–1334. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Fernandez PM, Patierno SR and Rickles FR:
Tissue factor and fibrin in tumor angiogenesis. Semin Thromb
Hemost. 30:31–44. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Dvorak HF: Tumors: Wounds that do not
heal. Similarities between tumor stroma generation and wound
healing. N Engl J Med. 315:1650–1659. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hisada Y, Yasunaga M, Hanaoka S, Saijou S,
Sugino T, Tsuji A, Saga T, Tsumoto K, Manabe S, Kuroda J, et al:
Discovery of an uncovered region in fibrin clots and its clinical
significance. Sci Rep. 3:26042013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Saito Y, Hashimoto Y, Kuroda J, Yasunaga
M, Koga Y, Takahashi A and Matsumura Y: The inhibition of
pancreatic cancer invasion-metastasis cascade in both cellular
signal and blood coagulation cascade of tissue factor by its
neutralisation antibody. Eur J Cancer. 47:2230–2239. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ueda C, Hirohata Y, Kihara Y, Nakamura H,
Abe S, Akahane K, Okamoto K, Itoh H and Otsuki M: Pancreatic cancer
complicated by disseminated intravascular coagulation associated
with production of tissue factor. J Gastroenterol. 36:848–850.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kakkar AK, Lemoine NR, Scully MF, Tebbutt
S and Williamson RC: Tissue factor expression correlates with
histological grade in human pancreatic cancer. Br J Surg.
82:1101–1104. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Callander NS, Varki N and Rao LV:
Immunohistochemical identification of tissue factor in solid
tumors. Cancer. 70:1194–1201. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hobbs JE, Zakarija A, Cundiff DL, Doll JA,
Hymen E, Cornwell M, Crawford SE, Liu N, Signaevsky M and Soff GA:
Alternatively spliced human tissue factor promotes tumor growth and
angiogenesis in a pancreatic cancer tumor model. Thromb Res. 120
(Suppl 2):S13–S21. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nitori N, Ino Y, Nakanishi Y, Yamada T,
Honda K, Yanagihara K, Kosuge T, Kanai Y, Kitajima M and Hirohashi
S: Prognostic significance of tissue factor in pancreatic ductal
adenocarcinoma. Clin Cancer Res. 11:2531–2539. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Contrino J, Hair G, Kreutzer DL and
Rickles FR: In situ detection of tissue factor in vascular
endothelial cells: Correlation with the malignant phenotype of
human breast disease. Nat Med. 2:209–215. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Tsumura R, Sato R, Furuya F, Koga Y,
Yamamoto Y, Fujiwara Y, Yasunaga M and Matsumura Y: Feasibility
study of the Fab fragment of a monoclonal antibody against tissue
factor as a diagnostic tool. Int J Oncol. 47:2107–2114. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Koga Y, Manabe S, Aihara Y, Sato R,
Tsumura R, Iwafuji H, Furuya F, Fuchigami H, Fujiwara Y, Hisada Y,
et al: Antitumor effect of antitissue factor antibody-MMAE
conjugate in human pancreatic tumor xenografts. Int J Cancer.
137:1457–1466. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Takashima H, Tsuji AB, Saga T, Yasunaga M,
Koga Y, Kuroda JI, Yano S, Kuratsu JI and Matsumura Y: Molecular
imaging using an anti-human tissue factor monoclonal antibody in an
orthotopic glioma xenograft model. Sci Rep. 7:123412017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Iwamura T, Katsuki T and Ide K:
Establishment and characterization of a human pancreatic cancer
cell line (SUIT-2) producing carcinoembryonic antigen and
carbohydrate antigen 19-9. Jpn J Cancer Res. 78:54–62.
1987.PubMed/NCBI
|
|
28
|
Sogawa C, Tsuji AB, Sudo H, Sugyo A,
Yoshida C, Odaka K, Uehara T, Arano Y, Koizumi M and Saga T:
C-kit-targeted imaging of gastrointestinal stromal tumor using
radiolabeled anti-c-kit monoclonal antibody in a mouse tumor model.
Nucl Med Biol. 37:179–187. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Sudo H, Tsuji AB, Sugyo A, Ogawa Y, Sagara
M and Saga T: ZDHHC8 knockdown enhances radiosensitivity and
suppresses tumor growth in a mesothelioma mouse model. Cancer Sci.
103:203–209. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Sugaya A, Hyodo I, Koga Y, Yamamoto Y,
Takashima H, Sato R, Tsumura R, Furuya F, Yasunaga M, Harada M, et
al: Utility of epirubicin-incorporating micelles tagged with
anti-tissue factor antibody clone with no anticoagulant effect.
Cancer Sci. 107:335–340. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yoshida C, Tsuji AB, Sudo H, Sugyo A,
Kikuchi T, Koizumi M, Arano Y and Saga T: Therapeutic efficacy of
c-kit-targeted radioimmunotherapy using 90Y-labeled anti-c-kit
antibodies in a mouse model of small cell lung cancer. PLoS One.
8:e592482013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Sugyo A, Tsuji AB, Sudo H, Nagatsu K,
Koizumi M, Ukai Y, Kurosawa G, Zhang MR, Kurosawa Y and Saga T:
Evaluation of 89Zr-labeled human anti-CD147 monoclonal
antibody as a positron emission tomography probe in a mouse model
of pancreatic cancer. PLoS One. 8:e612302013. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Matsumura Y and Maeda H: A new concept for
macromolecular therapeutics in cancer chemotherapy: Mechanism of
tumoritropic accumulation of proteins and the antitumor agent
smancs. Cancer Res. 46:6387–6392. 1986.PubMed/NCBI
|
|
34
|
Hong H, Zhang Y, Nayak TR, Engle JW, Wong
HC, Liu B, Barnhart TE and Cai W: Immuno-PET of tissue factor in
pancreatic cancer. J Nucl Med. 53:1748–1754. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Massoud TF and Gambhir SS: Molecular
imaging in living subjects: Seeing fundamental biological processes
in a new light. Genes Dev. 17:545–580. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Gnanasegaran G and Ballinger JR: Molecular
imaging agents for SPECT (and SPECT/CT). Eur J Nucl Med Mol
Imaging. 41 (Suppl 1):S26–S35. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Breij EC, de Goeij BE, Verploegen S,
Schuurhuis DH, Amirkhosravi A, Francis J, Miller VB, Houtkamp M,
Bleeker WK, Satijn D, et al: An antibody-drug conjugate that
targets tissue factor exhibits potent therapeutic activity against
a broad range of solid tumors. Cancer Res. 74:1214–1226. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Wang B, Berger M, Masters G, Albone E,
Yang Q, Sheedy J, Kirksey Y, Grimm L, Wang B, Singleton J and
Soltis D: Radiotherapy of human xenograft NSCLC tumors in nude mice
with a 90Y-labeled anti-tissue factor antibody. Cancer
Biother Radiopharm. 20:300–309. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Jain M, Gupta S, Kaur S, Ponnusamy MP and
Batra SK: Emerging trends for radioimmunotherapy in solid tumors.
Cancer Biother Radiopharm. 28:639–650. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Aung W, Tsuji AB, Sugyo A, Takashima H,
Yasunaga M, Matsumura Y and Higashi T: Near-infrared
photoimmunotherapy of pancreatic cancer using an indocyanine
green-labeled anti-tissue factor antibody. World J Gastroenterol.
24:5491–5504. 2018. View Article : Google Scholar : PubMed/NCBI
|