Introduction
Soft tissue sarcoma (STS) is a group of rare
malignant tumors that occur in the connective tissue and account
for ~10% of cancers in children and <1% of all adult solid
malignant cancers (1). These tumors
can originate throughout the human body, particularly in the
extremities and the trunk. Although STS accounts for no >1% of
all malignancies, it appears to be part of a heterogeneous disease,
as >50 different histological subtypes have been identified
(2,3). Recurrence occurs in ~50% of
high-grade, advanced, and metastatic STSs. For patients in relapse
or with a delayed diagnosis, few long-term effective agents are
available. Advanced STS presents poor overall survival (OS) with
the median OS being no >2 years (4,5).
Meanwhile, molecular biomarkers to optimize therapy strategies and
overcome disease resistance remain unknown (6). Multidisciplinary approaches and
specific molecular targeting therapies are recommended for STS
patients, but the clinical impact of these therapies in certain
common STS subtypes are unclear. Additional molecular pathway
targets and treatment strategies are required to improve the
outcomes of this confounding disease.
Drug repurposing involves the application of
clinical drugs to different diseases in order to reduce the
development time and cost. It has become a fast and effective way
to identify drug candidates (7).
Drug repurposing can be facilitated by an established and
searchable database that collects drug-gene interactions from
various sources (8–10).
The Connectivity Map (CMap; http://portals.broadinstitute.org/cmap/) is a
web-based computational drug-repurposing tool that allows users to
screen bioactive small molecules through genome-wide transcription
expression data (8). The current
version (build 02) of CMap includes >7,000 gene expression
profiles from five human cell lines and reflects treatment with
1,309 bioactive small molecules at different doses (11). Screening is achieved by comparing
the reference profiles stored in the database with the
significantly differentially expressed genes of the user's targeted
disease using a pattern-matching algorithm. The screening results
in a list of small molecule connectivity scores that range from −1
to +1. A small molecule-expression profile that presents a strong
negative correlation to a disease-relevant gene expression
signature indicates that the molecule may have a potentially
therapeutic effect on the disease (12). CMap has successfully identified
bioactive small molecules and combination therapies that have shown
promise in the treatment of a variety of diseases (13–19).
The Drug Gene Interaction Database (DGIdb;
http://www.dgidb.org), another drug repurposing
web-based application, contains >40,000 genes and >10,000
drugs that are involved in >15,000 drug-gene interactions
(9). These drug-gene interactions
were collected using expert curation and text-mining from the
drug-related databases DrugBank, Therapeutic Target Database,
PharmGKB, Guide to Pharmacology, and ClinicalTrials.gov. In addition, bioinformatic
analyses, such as gene ontology and pathway analysis, were used to
categorize potentially druggable genes.
The L1000 Fireworks Display (L1000 FWD; http://amp.pharm.mssm.edu/L1000FWD) is another
web-based application that provides interactive visualization of
>16,000 drug and gene expression signatures (10). In this database, potential drugs or
bioactive small molecules can be easily identified when users enter
the differentially expressed gene sets of a specific disease into
the search box.
The present study sought to identify novel drug
candidates for the treatment of several common histologic subtypes
of STS (58 dedifferentiated liposarcoma, 99 leiomyosarcoma, 8
malignant peripheral nerve sheath tumors, 25 myxofibrosarcoma, 10
synovial sarcoma and 49 undifferentiated pleomorphic sarcoma).
According to previous studies (6,20–23),
these six common STS subtypes may have collective biological
targets that can be recognized by one or more drugs. STS
survival-associated genes were identified using The Cancer Genome
Atlas (TCGA) data and then applied to the CMap, DGIdb and L1000 FWD
databases. The repetitions from the predicted drugs obtained from
these three drug-gene interaction databases were removed and
over-lapped in order to identify the final drug candidates for the
STS histologic subtypes, thus providing more reliable results. A
pathway analysis and molecular docking were conducted to evaluate
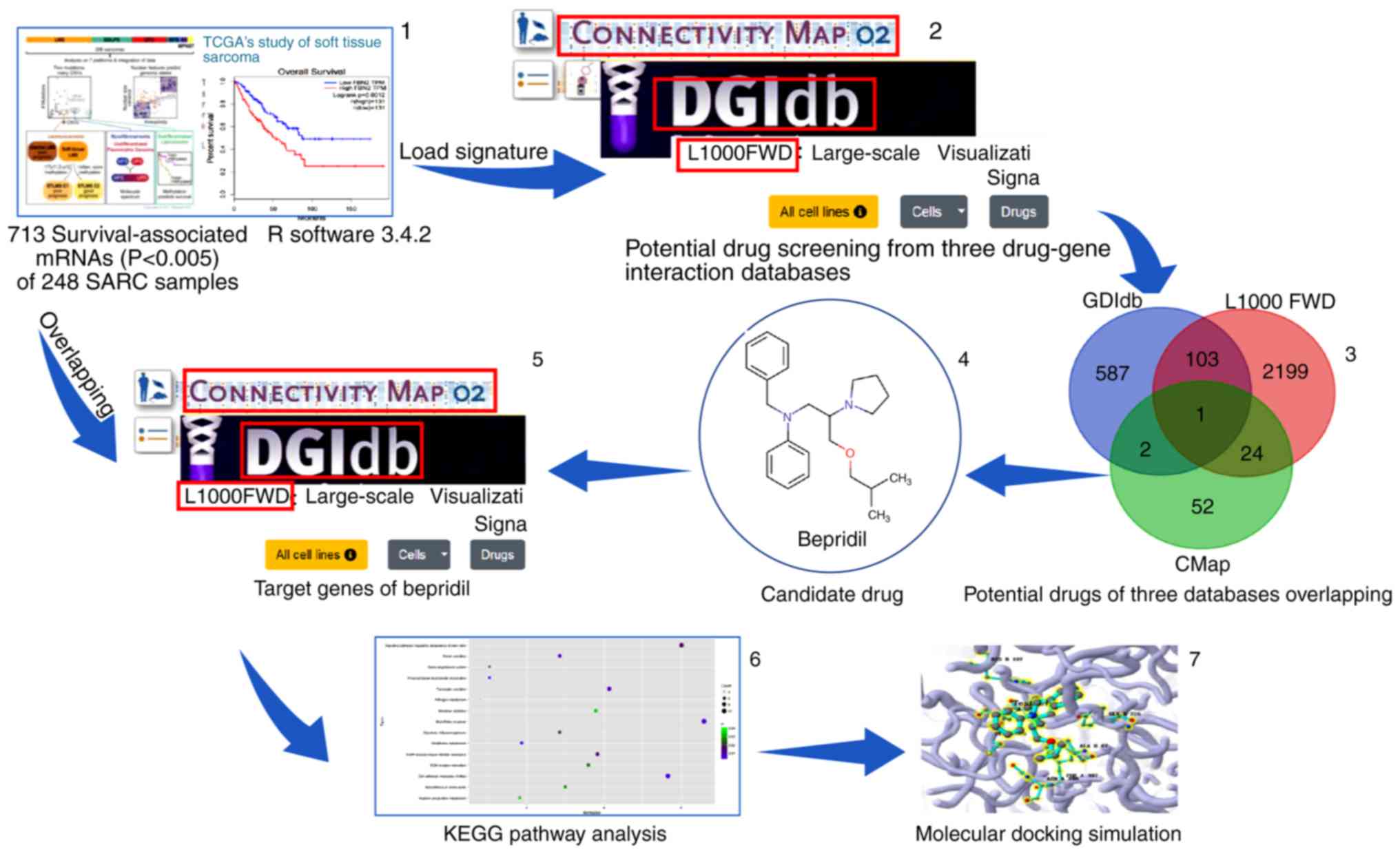
the molecular mechanism of the candidate drug. Fig. 1 presents a schematic of the study
design concept.
Materials and methods
STS survival-associated mRNA
screening
mRNA-sequence data (Level 3) was downloaded from the
STS samples in the TCGA database (http://cancergenome.nih.gov/). A total of 261 STS
samples were collected (including 59 dedifferentiated liposarcoma,
105 leiomyosarcoma, 9 malignant peripheral nerve sheath tumors, 25
myxofibrosarcoma, 10 synovial sarcoma and 51 undifferentiated
pleomorphic sarcomas, as well as 2 desmoid tumors). Subsequently,
edgeR, a BioconductoR software package, was used to normalize the
expression profile (24). To obtain
more reliable data, 2 desmoid tumors and 9 tumor samples with
survival times <90 days were excluded. Then, a univariate Cox
regression was conducted using R software (3.4.2 version; R
Foundation for Statistical Computing, Vienna, Austria) to obtain
the STS survival-associated genes. The eligible genes were divided
into two groups (risk and protective) according to their hazard
ratio values. The cut-off value was 1.
Potential drug predictions
The STS survival-associated genes were separated
into two files (risk factors and protective factors) in order to
query the CMap, DGIdb, and L1000 FWD databases. As the total number
of upload tags cannot be >1,000 for CMap, only STS
survival-associated genes with P-values <0.005 were selected.
Prior to querying CMap, all of the gene symbols were converted to
Affymetrix probe IDs using the Affymetrix site (https://www.affymetrix.com/site/mainPage.affx). A
total of 535 genes with a negative correlation with STS survival,
and 178 genes with a positive correlation with STS survival were
separately uploaded to CMap. In the CMap database, drugs with
significantly negative scores were expected to be putative novel
therapeutic indications for STS. The connectivity scores were
calculated using the gene-set-enrichment analysis algorithm
(9). A mean score of ≤0.65 was used
to identify potential drug candidates.
For DGIdb, all of the STS survival-associated gene
symbols were pasted directly into the search box using the ‘Search
Drug-Gene Interactions’ function button, and then the predictive
drug list, TSV, was downloaded. For the L1000 FWD database, all of
the STS survival-associated gene symbols were divided into
differential expression gene sets (up and down) before querying the
potential drugs. As with the CMap database, drugs with negative
scores were expected to have putative novel therapeutic indications
for STS.
To increase the reliability of the results, the
candidate drugs were selected by overlapping the results from the
three databases.
Identified target genes of the
candidate drug
Genes regulated by the candidate drug were
subsequently identified in the three databases using an in
silico analysis. For the CMap database, the identified gene
symbols were converted into Affymetrix probe identifiers and then
tagged with the ‘up’ and ‘down’ files in. grp format prior to being
uploaded to the CMap ‘quick query’ separately (25). Significantly aberrantly expressed
probes with amplitude values ≤0.67 or >0.67 were selected (an
amplitude of ±0.67 l represents a two-fold change between the
treatment and the control). All of the predicted targets were
included for the DGIdb and L1000 FWD databases as no threshold was
provided.
Pathways analysis
The Kyoto Encyclopedia of Genes and Genomes (KEGG)
pathway analysis was performed for the significantly aberrantly
expressed probes of the candidate drugs using the WebGestalt
database (http://www.webgestalt.org/option.php) (26). The P-value of each pathway was
adjusted using the Hochberg (BH) procedure (27), and pathways with P<0.05 were
considered significant. Furthermore, target genes in pathways that
previously been reported to be involved in tumor genesis or
progression were uploaded to cBioPortal database (http://www.cbioportal.org/) to analyze their genetic
alterations.
Molecular docking
Molecular docking is an efficient computational
method which can rapidly calculate the binding potential of a small
molecule (drug candidate) to a target protein. It has been widely
used in computer-aided drug discovery due to its speed and low cost
(28,29). SystemsDock (http://systemsdock.unit.oist.jp/) is a web server for
network pharmacology-based prediction and analysis, which employs
two machine learning systems (Machine Learning Systems A and B) and
integrates curated signaling networks, bioinformatics databases and
molecular virtual docking simulation to comprehensively and rapidly
evaluate potential binding affinities of drug candidates against
target proteins (30). Compared
with other docking programs (31,32),
it provides a major advance in quality and reliability of assessing
protein-ligand interaction. However, systemsDock taking protein
structure availability and binding site certainty into
consideration, and the protein residues involved in the binding
interaction are automatically identified by exploring the position
where the biggest native ligand is bound. Ducking score, the
indication of binding strength, is a negative logarithm of the
experimental dissociation/inhibition constant (pKd/pKi) that ranges
from 0–10 (i.e., from weak to strong). A good accuracy level
(80–83%) was observed when the cut-off scores were in the range of
4.82–6.11 (pKd), which is conventionally used to classify ligand
binding activity.
In the present study, molecular docking was singly
performed on the proteins of several KEGG pathways with the
candidate drug using systemsDock to check whether the candidate
drug may have an anti-STS function. The docking simulation was
carried out in three steps: i) Specifying the proteins and binding
sites by uploading the names or Protein Data Bank (PDB; http://www.rcsb.org/) IDs of the proteins; ii)
preparing the small molecules (drugs) for the test by uploading
their structure files in 2D/3D SDF, Mol2 or SMILES formats; and
iii) clicking the ‘run’ button.
Results
Identification of STS
survival-associated genes in the TCGA database
A total of 2,842 survival-associated genes were
extracted from 248 sample (58 dedifferentiated liposarcoma, 99
leiomyosarcoma, 7 malignant peripheral nerve sheath tumors, 25
myxofibrosarcoma, 10 synovial sarcoma and 49 undifferentiated
pleomorphic sarcomas) mRNA profiles in the TCGA database using a
univariate Cox regression. As the CMap database could not process
>1,000 uploaded tags, SPS survival-associated genes with
P<0.005 were selected to screen the small molecules. Among those
genes, 535 were demonstrated to be risk factors for STS, while 178
were protective factors.
STS-targeted screening for candidate
drugs
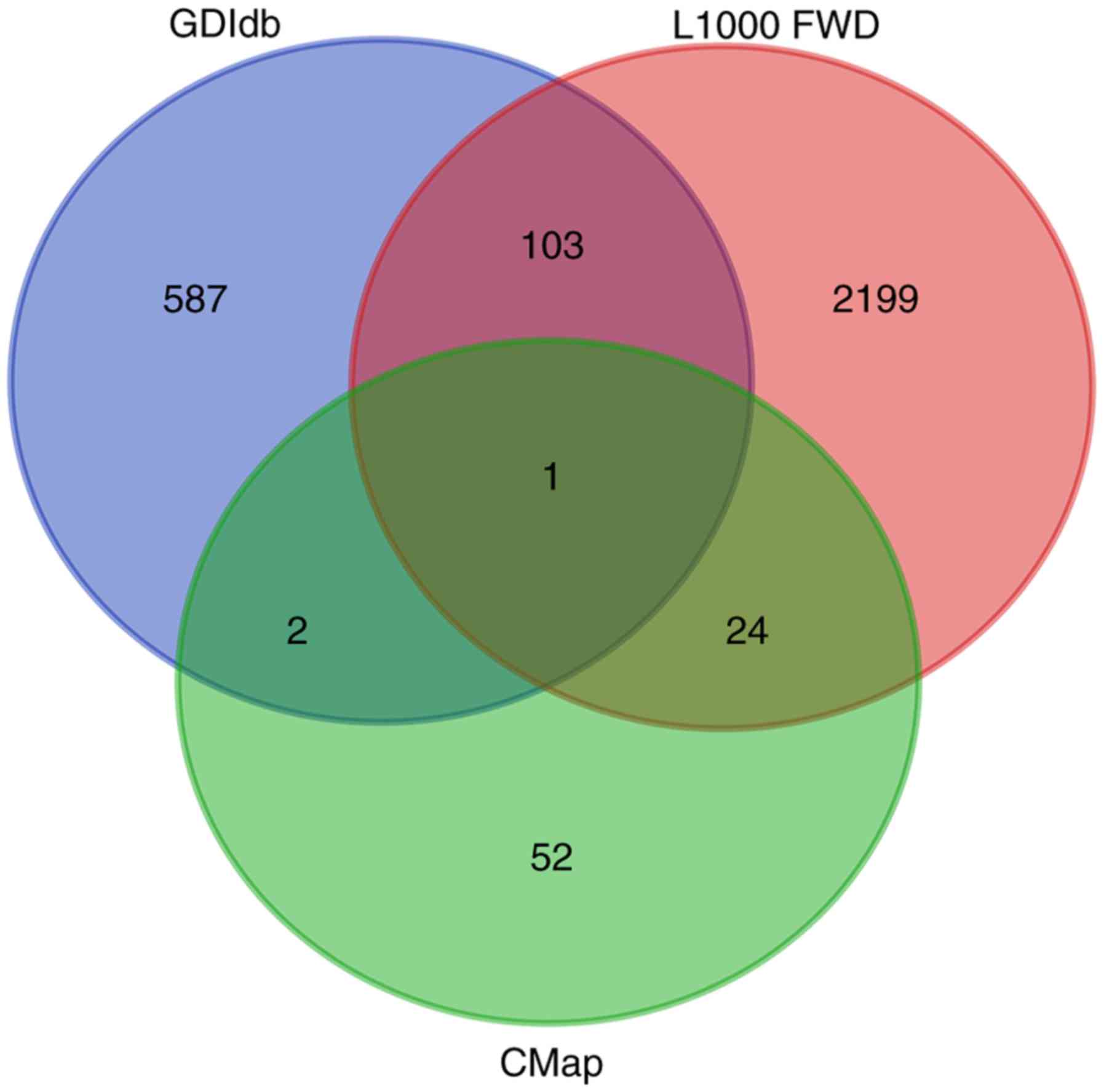
According to the screening conditions mentioned in
the methods above, 79, 693 and 2,327 potential drugs were screened
from the CMap, DGIdb and L1000 FWD databases, respectively. When
the results of this screening were overlapped, only Bepridil was
identified in all three databases simultaneously (Fig. 2). For the CMap database,
gene-expression changes in three kinds of human cell lines that
were treated with Bepridil partially matched those in the STS
survival-associated genes. For the L1000 FWD database, similar
findings were identified for two human cell lines (Table I). In the DGIdb database, Bepridil
was identified by mapping the STS survival-associated genes with
the Guide to Pharmacology database.
 | Table I.Cell lines treated with Bepridil in
the CMap and L1000 FWD databases. |
Table I.
Cell lines treated with Bepridil in
the CMap and L1000 FWD databases.
| Database | Mean score | Cell line | Dose (µm) | Score | n | P-value |
|---|
| CMap | −0.659 |
|
|
| 4 | 0.071 |
|
|
| MCF7 | 10 | −0.677 | 2 | 0.101 |
|
|
| PC3 | 10 | −0.756 | 1 | – |
|
|
| HL60 | 10 | −0.525 | 1 | – |
| L1000FWD | −0.0167 |
|
|
| 2 | – |
|
|
| HCC515 | 10 | N/A | 1 | 0.001 |
|
|
| VCaP | 10 | N/A | 1 | 0.002 |
Bepridil is a long-acting, non-selective
calcium-channel blocker with significant antianginal activity. As
Bepridil has been demonstrated to cause ventricular arrhythmias, it
is no longer used in clinical practice (33). To determine whether Bepridil could
be repurposed for the treatment of STS, specific targets were
identified for further analysis. As a result, 57, 19 and 434 genes
were reported to be regulated by Bepridil in the CMap, DGIdb and
L1000 FWD databases, respectively. In total, 510 potential Bepridil
targets were gathered for subsequent pathway analysis.
KEGG functional pathway analysis of
Bepridil targets
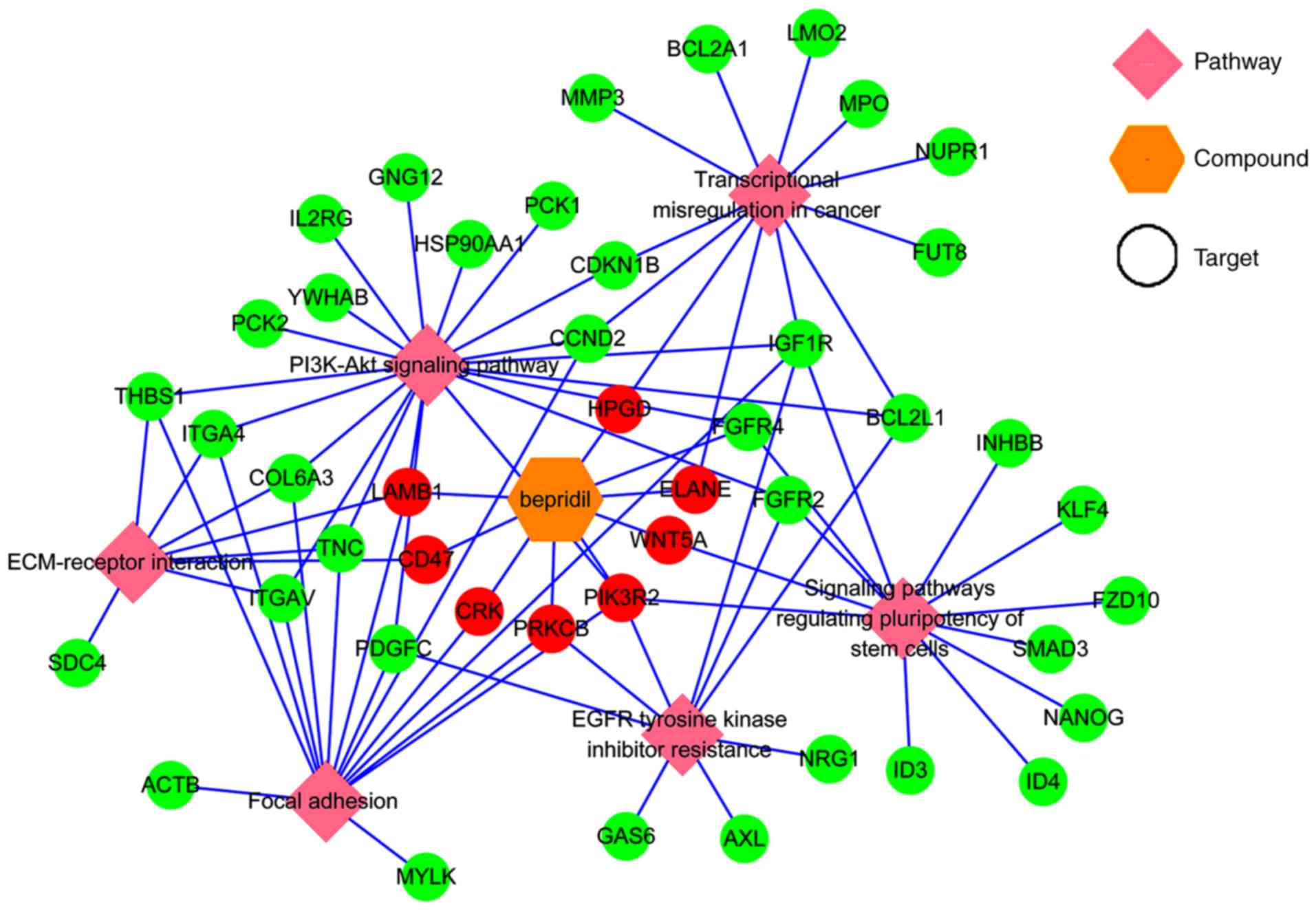
Next, the KEGG pathways in which the Bepridil target
genes were likely involved were explored. WebGestalt, a functional
enrichment analysis web tool, was used to conduct the pathway
analysis. Thirty pathways were identified as associated with the
Bepridil targets (Table II).
Several of these pathways were previously reported to be involved
in tumor genesis or progression (34–36),
including epidermal growth factor receptor (EGFR) tyrosine kinase
inhibitor resistance (hsa01521), signaling pathways regulating stem
cell pluripotency (hsa04550), extracellular matrix (ECM)-receptor
interaction (hsa04512), focal adhesion (hsa04510), transcriptional
misregulation in cancer (hsa05202) and the phosphatidylinositol 3
kinase-protein kinase B (PI3K-Akt) signaling pathway (hsa04151).
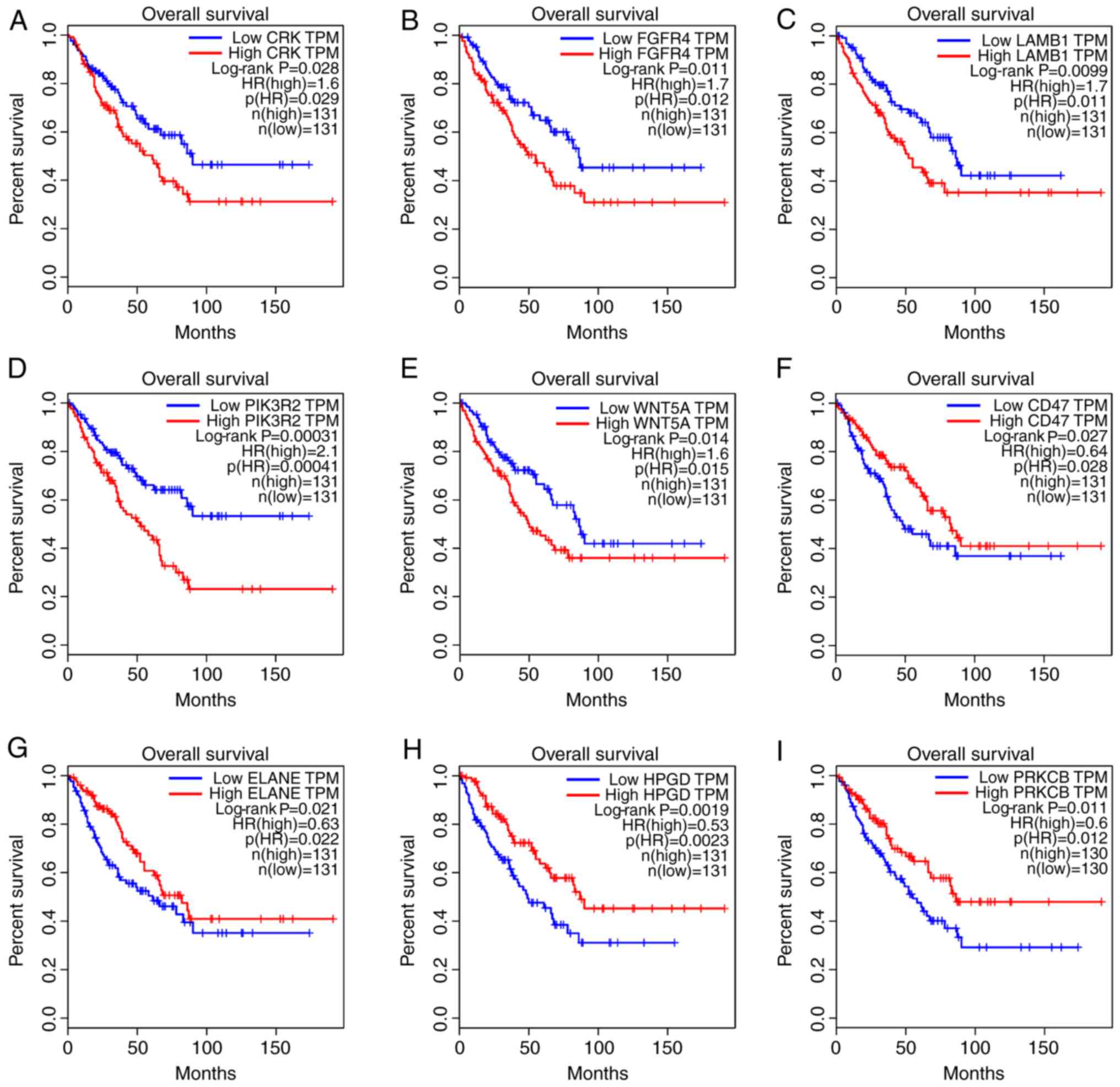
Overall survival analysis of the genes clustered in the above-noted
pathways revealed that CRK, fibroblast growth factor
receptor 4 (FGFR4), laminin subunit β1 (LAMB1),
phosphoinositide-3-kinase regulatory subunit 2 (PIK3R2) and
WNT5A were likely STS risk factors, while overexpression of
cluster of differentiation 47 (CD47), elastase, neutrophil
expressed (ELANE), 15-hydroxyprostaglandin dehydrogenase
(HPGD) and protein kinase cβ (PRKCB) was correlated
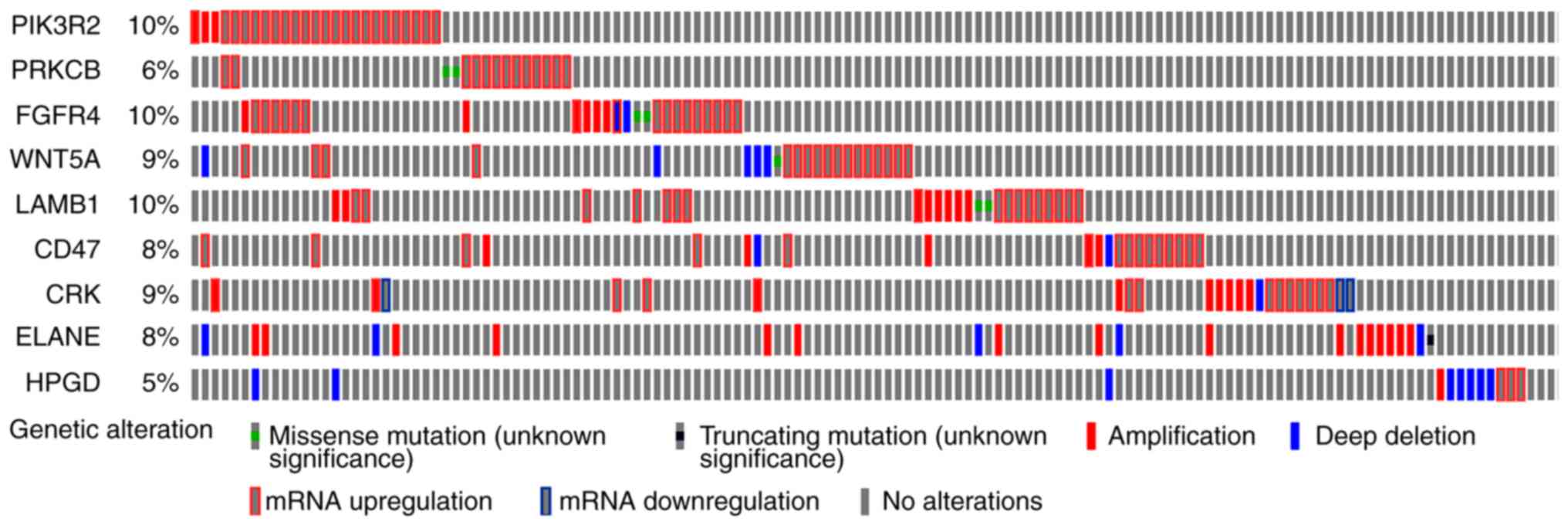
with a better prognosis in STS tissues (Fig. 3). The genetic alteration of these 9
genes was also evaluated using one TCGA dataset (with 265 STS
samples) in order to explore how they may function in STS. The
results demonstrated that the alterations in the other genes mainly
appeared as mRNA upregulation (Fig.
4), except for the alterations in ELANE and HPGD,
which were either amplifications or deep deletions. This suggests
that changes in gene expression may allow these 9 genes to function
in STS. In addition, mutually exclusive analysis revealed 18 gene
pairs with mutually exclusive alterations, and 18 gene pairs with
co-occurrent alterations; however, they were all non-significant
(adjusted P>0.05; data not shown).
 | Figure 3.Significant prognostic values of
genes that are reportedly involved in tumor genesis or progression
pathways. (A) CRK (B) FGFR4. (C) LAMB1. (D)
PIK3R2. (E) WNT5A. (F) CD47. (G) ELANE.
(H) HPGD. (I) PRKCB. FGFR4, fibroblast growth
factor receptor 4; LAMB1, laminin subunit β1; PIK3R2,
phosphoinositide-3-kinase regulatory subunit 2; CD47,
cluster of differentiation 47; ELANE, elastase, neutrophil
expressed; HPGD, 15-hydroxyprostaglandin dehydrogenase;
PRKCB, protein kinase cβ; TPM, trans per million; HR, hazard
ratio. |
 | Table II.KEGG functional annotation of the
Bepridil targets. |
Table II.
KEGG functional annotation of the
Bepridil targets.
| Gene set | Description | Count | P-value | Gene |
|---|
| hsa00480 | Glutathione
metabolism | 7 | 0.0022 | GPX1;
GPX4; ANPEP; GSTA1; GSTA4;
GSTP1; ODC1 |
| hsa04964 | Proximal tubule
bicarbonate reclamation | 5 | 0.0029 | ATP1A1;
PCK1; PCK2; CA2; SLC4A4 |
| hsa04514 | Cell adhesion
molecules | 13 | 0.0040 | VCAN; CADM1;
HLADQB1; ITGA4; ITGAV; CD99; NCAM1; CLDN18; PTPRM; SDC2; SDC4;
CD58; CDH1 |
| hsa05206 | microRNAs in
cancer | 14 | 0.0058 | SPRY2; CDKN1B;
CRK; E2F2; DICER1; TNC; MARCKS; ABCB1; SERPINB5; PIK3R2; PRKCB;
SOX4; THBS1; CCND2 |
| hsa04924 | Renin
secretion | 8 | 0.0069 | ADCYAP1R1;
CLCA1; AGT; PDE1A; PDE1C; PDE1B; PTGER4; CLCA2 |
| hsa04972 | Pancreatic
secretion | 10 | 0.0077 | CLCA1; SLC26A3;
KCNQ1; ATP1A1; PLA2G2A; PRKCB; SLC12A2; CA2; SLC4A4; CLCA2 |
| hsa01521 | EGFR tyrosine
kinase inhibitor resistance | 9 | 0.0136 | FGFR2; GAS6;
NRG1; IGF1R; PIK3R2; PRKCB; AXL; PDGFC; BCL2L1 |
| hsa04550 | Signaling pathways
regulating pluripotency of stem cells | 12 | 0.0161 | FZD10; FGFR2;
FGFR4; ID3; ID4; IGF1R; INHBB; SMAD3; PIK3R2; WNT5A; NANOG;
KLF4 |
| hsa04614 | Renin-angiotensin
system | 4 | 0.0176 | CTSG; AGT;
ANPEP; CTSA |
| hsa00010 |
Glycolysis/gluconeogenesis | 7 | 0.0225 | ALDH2; ALDOB;
HK2; PCK1; PCK2; PFKP; PGK1 |
| hsa04512 | ECM-receptor
interaction | 8 | 0.0259 | COL6A3; TNC;
ITGA4; ITGAV; LAMB1; SDC4; THBS1; CD47 |
| hsa01230 | Biosynthesis of
amino acids | 7 | 0.0289 | ALDOB; IDH3G;
PFKP; PGK1; PSPH; BCAT1; PYCRL |
| hsa00330 | Arginine and
proline metabolism | 5 | 0.0332 | ALDH2; OAT;
ODC1; SMOX; PYCRL |
| hsa05032 | Morphine
addiction | 8 | 0.0343 | GABRP; PDE1A;
PDE1C; PDE2A; PDE1B; PRKCB; GNG12; CACNA1A |
| hsa00910 | Nitrogen
metabolism | 3 | 0.0409 | CA1; CA2;
CA12 |
| hsa05215 | Prostate
cancer | 8 | 0.0531 | CDKN1B; E2F2;
FGFR2; GSTP1; HSP90AA1; IGF1R; PIK3R2; PDGFC |
| hsa04974 | Protein digestion
and absorption | 7 | 0.0585 | COL5A2; COL6A3;
COL10A1; COL13A1; KCNQ1; ATP1A1; SLC1A1 |
| hsa04310 | Wnt signaling
pathway | 10 | 0.0609 | FZD10; DKK1;
SMAD3; PRKCB; SFRP1; SFRP4; TBL1X; WNT5A; TBL1XR1; CCND2 |
| hsa04510 | Focal adhesion | 14 | 0.0629 | COL6A3; CRK;
TNC; IGF1R; ITGA4; ITGAV; LAMB1; MYLK; PIK3R2; PRKCB; PDGFC; ACTB;
THBS1; CCND2 |
| hsa04068 | FoxO signaling
pathway | 10 | 0.0730 | CDKN1B; PRMT1;
IGF1R; SMAD3; FOXO4; PCK1; PCK2; PIK3R2; S1PR4; CCND2 |
| hsa04350 | TGF-β signaling
pathway | 7 | 0.0742 | ID3; ID4; INHBB;
SMAD3; BMP6; TFDP1; THBS1 |
| hsa05205 | Proteoglycans in
cancer | 14 | 0.0751 | FZD10; ANK1;
IGF1R; ITGAV; PIK3R2; PRKCB; PTCH1; ACTB; SDC2; SDC4; THBS1;
TWIST1; WNT5A; NANOG |
| hsa05020 | Prion diseases | 4 | 0.0764 | HSPA1A; NCAM1;
PRNP; C7 |
| hsa05130 | Pathogenic
Escherichia coli infection | 5 | 0.0849 | ARPC1A; KRT18;
ACTB; TUBB6; CDH1 |
| hsa05222 | Small cell lung
cancer | 7 | 0.0874 | CDKN1B; CKS2;
E2F2; ITGAV; LAMB1; PIK3R2; BCL2L1 |
| hsa04971 | Gastric acid
secretion | 6 | 0.0877 | KCNQ1; MYLK;
ATP1A1; PRKCB; ACTB; CA2 |
| hsa05202 | Transcriptional
misregulation in cancer | 12 | 0.0906 | CDKN1B; ELANE;
FUT8; NUPR1; HPGD; IGF1R; LMO2; MMP3; MPO; BCL2A1; BCL2L1;
CCND2 |
| hsa04151 | PI3K-Akt signaling
pathway | 20 | 0.0920 | CDKN1B; COL6A3;
FGFR2; FGFR4; HSP90AA1; TNC; IGF1R; IL2RG; ITGA4; ITGAV; LAMB1;
PCK1; PCK2; PIK3R2; GNG12; PDGFC; BCL2L1; THBS1; YWHAB;
CCND2 |
| hsa03320 | PPAR signaling
pathway | 6 | 0.0930 | PLIN2; FABP1;
FABP5; ACSL1; PCK1; PCK2 |
| hsa04110 | Cell cycle | 9 | 0.0986 | CDKN1B; CDKN1C;
E2F2; SMAD3; MCM4; TFDP1; YWHAB; CCND2; CDC20 |
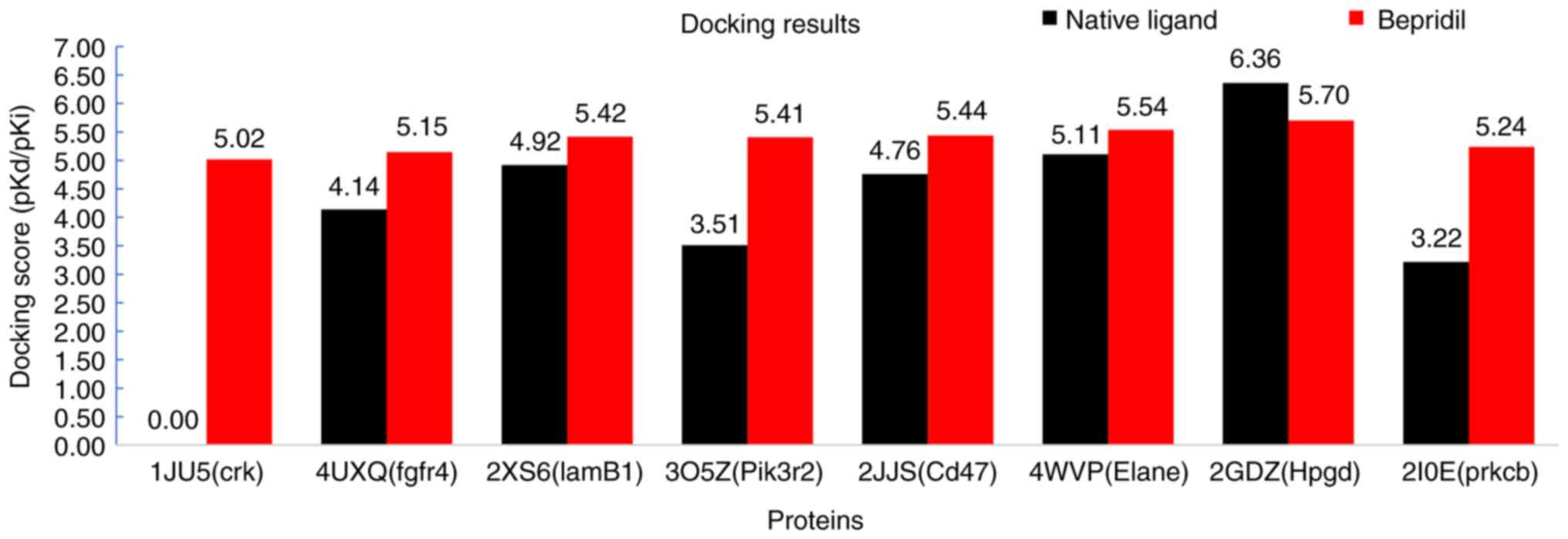
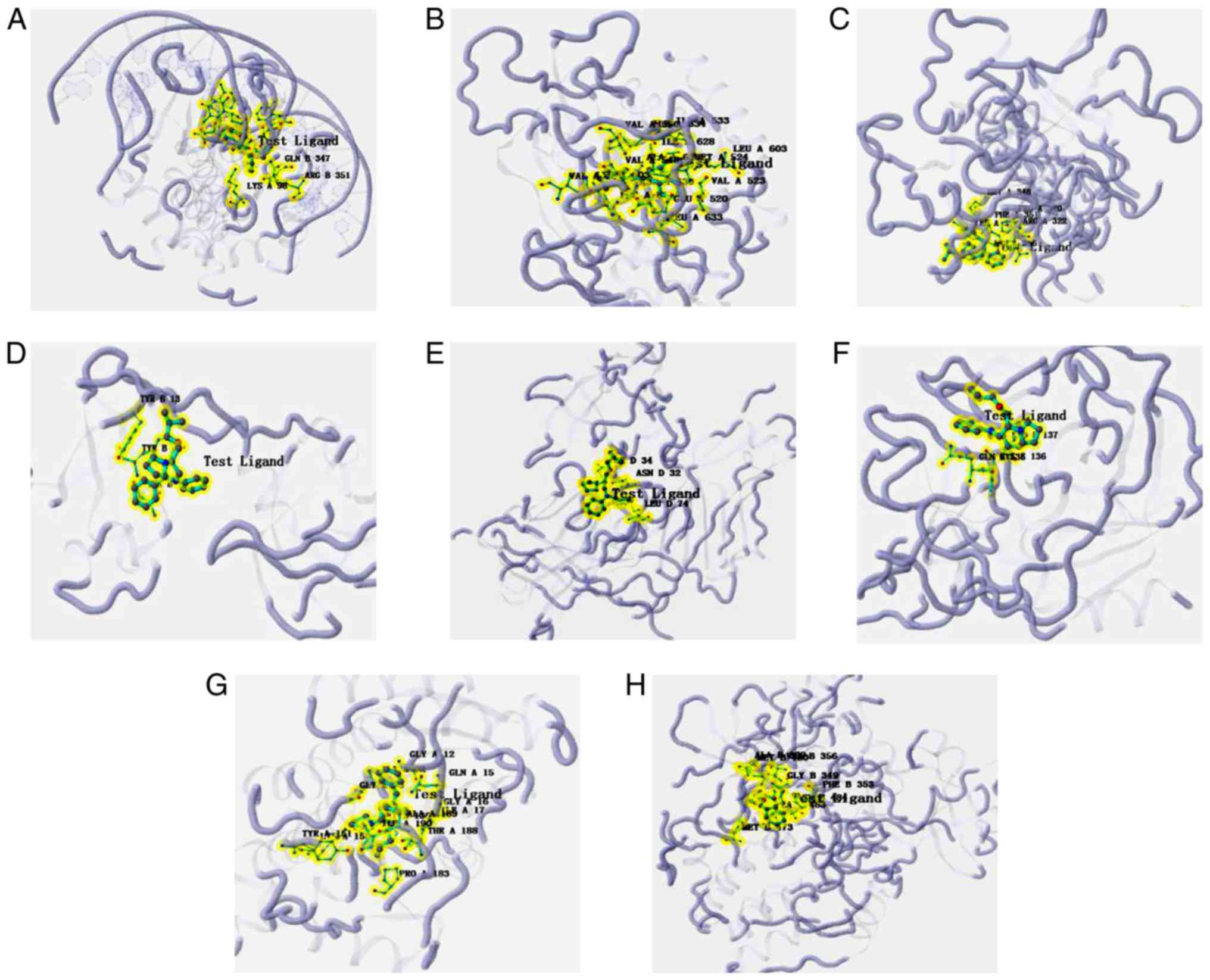
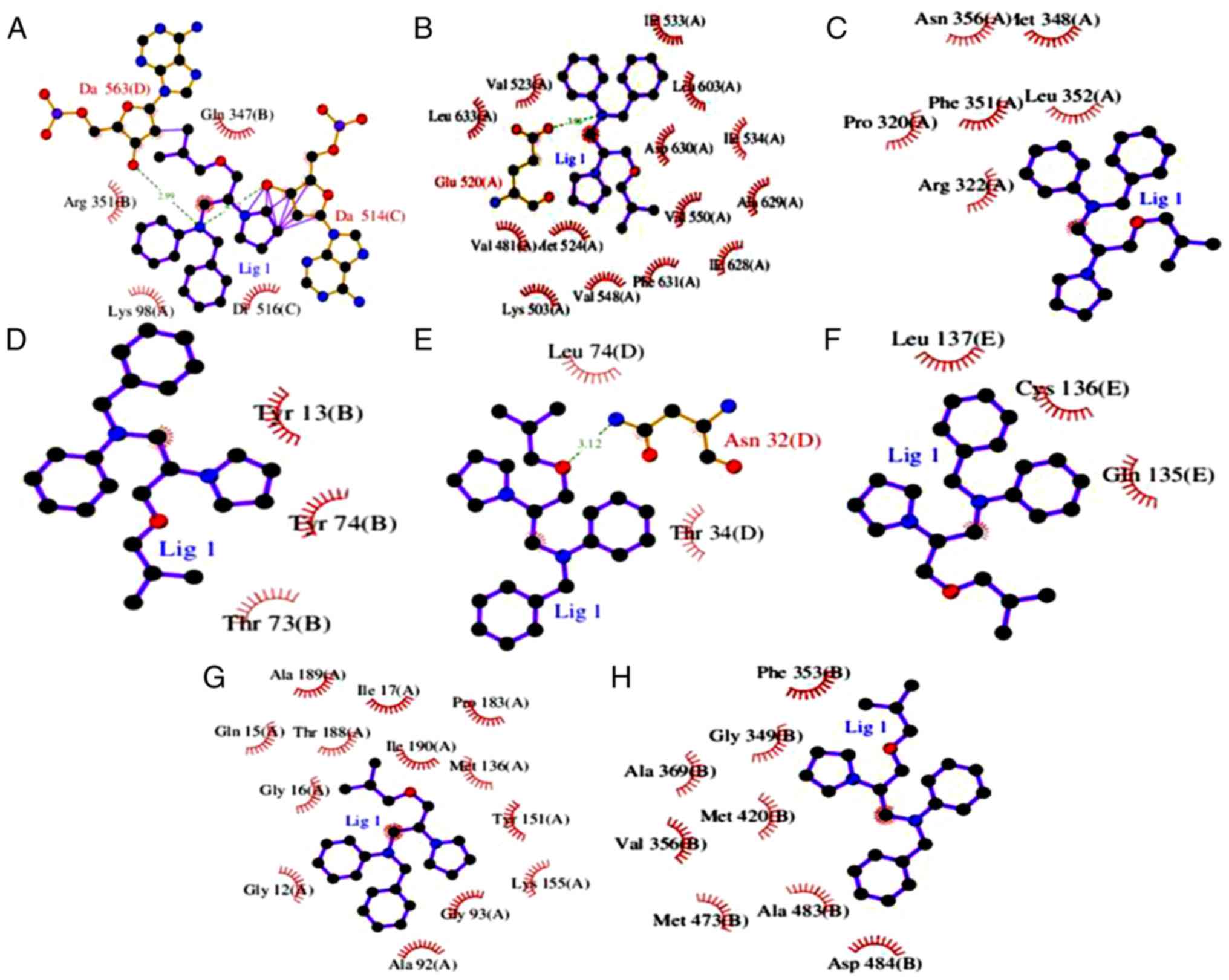
Molecular docking
Finally, to explore how Bepridil suppresses or
prevents carcinogenic progression, the proteins of 8 STS
survival-associated genes (CRK, FGFR4, LAMB1, PIK3R2, WNT5A,
CD47, ELANE, HPGD and PRKCB) were analyzed further using
molecular docking. Notably, compared with the cut-off scores
(4.82–6.11), except the protein of WNT5A, another 8 proteins all
exhibited stable docking (medium-to-good binding) results with
Bepridil. The lowest docking score was 5.017 for CRK, while the
other protein-ligand interaction scores were >5.1. The highest
docking simulation was found between HPGD and Bepridil (docking
score, 5.702). The PDB IDs, docking compound, and docking scores
are presented in Table III and
Fig. 5. The detailed protein-ligand
interactions of the docking pose (3D and 2D structures) are
presented in Figs. 6 and 7. Finally, a network was constructed to
display the association between the pathways, targets and candidate
drug Bepridil (Fig. 8).
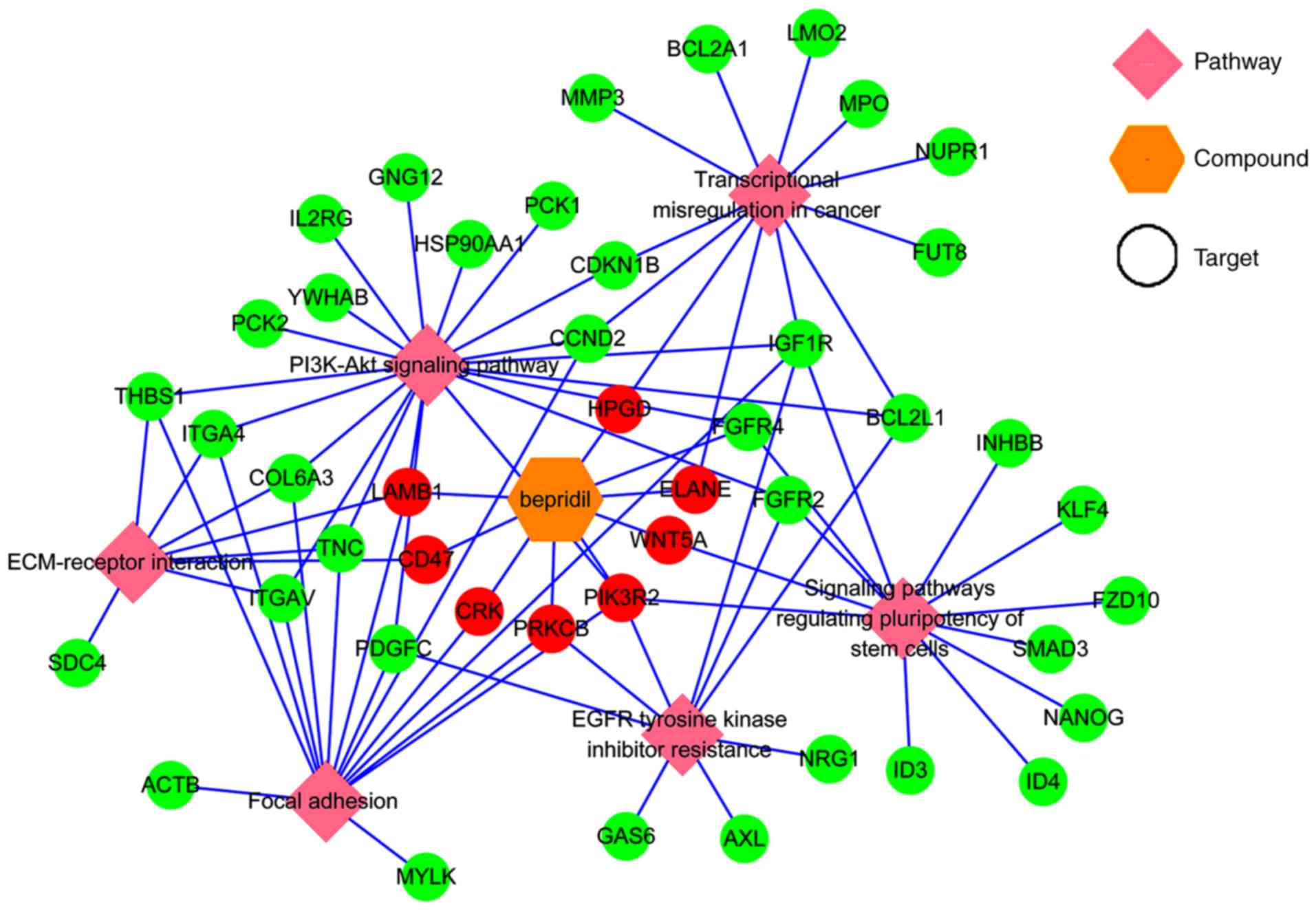 | Figure 8.A network visualization of the
association between the identified pathways, targets and candidate
drug. Green circles represent the genes clustered in different
pathways, red circles represent both the genes clustered in
different pathways and the Bepridil targets. FGFR4, fibroblast
growth factor receptor 4; LAMB1, laminin subunit β1; PIK3R2,
phosphoinositide-3-kinase regulatory subunit 2; CD47, cluster of
differentiation 47; ELANE, elastase, neutrophil expressed; HPGD,
15-hydroxyprostaglandin dehydrogenase; PRKCB, protein kinase
cβ. |
 | Table III.Docking simulation results for
Bepridil and proteins that are reportedly involved in tumor genesis
or progression. |
Table III.
Docking simulation results for
Bepridil and proteins that are reportedly involved in tumor genesis
or progression.
| Gene/protein
name | PDB ID | Docking scores
(pKd/pKi) |
|---|
| CRK/CRK | 1JU5 | 5.017 |
|
FGFR4/FGFR4 | 4UXQ | 5.146 |
|
LAMB1/LAMB1 | 5XAU | 5.417 |
|
PIK3R2/PIK3R2 | 2XS6 | 5.414 |
|
CD47/CD47 | 2JJS | 5.436 |
|
ELANE/ELANE | 4WVP | 5.539 |
|
HPGD/HPGD | 2GDZ | 5.702 |
|
PRKCB/PRKCB | 2I0E | 5.195 |
Discussion
Recent studies have tended to rely on a panel of
cancer-related genes to predict potential drugs for diseases
(12,14,17);
however, this has not yet been successfully performed for STS.
Therefore, the present study used a panel of cancer-related genes
to predict potential drugs for several STS subtypes. Previous
studies using this methodology have yielded several novel
candidates and several clinical drugs have been applied
successfully to different diseases using the drug-repurposing
strategy. To identify potential drug candidates, studies typically
focus on the genomic signatures that are available in electronic
patient records, as well as targets of drugs. For example, Paik
et al (37) used
computational methods to predict that terbutaline sulfate, an
anti-asthmatic, could be used to treat amyotrophic lateral
sclerosis. Similarly, Dudley et al (38) used an in silico computational
approach to discover a novel drug therapy for inflammatory bowel
disease that uses the public gene-expression profiles of the
disease and the potential targets of drugs. These results suggested
that using cancer-related genes to predict potential drugs may be a
promising method for drug repurposing. Changes in gene expression
are a significant factor in disease genesis and progression
Analyzing these changes can identify potential targets for
improving therapeutic intervention. In the present study,
survival-correlated gene expression signatures were used to make
in silico predictions of new indications for approved drugs.
Then, three drug-gene interaction databases (CMap, DGIdb, and L1000
FWD) were used to identify potential drugs for STS histologic
subtypes. Linking disease-drug profiles based on gene expression
signatures is a well-established modality for drug repurposing
(8,9,10).
CMap used several human tumor cell lines to generate
gene-expression profiles of >1,300 compounds, and the predicted
drugs were ranked by considering multiple parameters, such as the
mean score, enrichment score, match specificity and P-value, to
enhance the stability and reliability of the predicted results. The
developers of CMap and other groups (26,39)
have demonstrated that CMap is a potent tool for identifying
compounds with medicinal benefits for a wide range of diseases.
L1000 FWD is a similar drug-gene database, but its prediction
results only provide the drug name and similarity score. While
drug-gene interactions in the DGIdb database were collected using
expert curation and text-mining of data from the drug-related
database DrugBank, the Therapeutic Target Database, PharmGKB, and
ClinicalTrials.gov provide an alternative method
to predict drugs for STS histologic subtypes. Therefore, the
predicted drugs in these three databases were combined in order to
obtain more stable and reliable results. After mapping the targets
of these molecules in CMap and querying the DGIdb and L1000 FWD
databases with STS survival-associated genes, Bepridil was
discovered to be a drug candidate for several common histologic
subtypes of STS, which appeared simultaneously in all three
databases.
Bepridil is a long-acting, non-selective,
calcium-channel blocker that was once used as an antianginal
treatment. It induces significant coronary vasodilation and has
modest peripheral effects (40).
However, Bepridil is no longer used in clinical practice as it has
been implicated in ventricular arrhythmias. As novel drug discovery
is time consuming and risky, identifying novel indications for
known drugs (drug repurposing) has become an effective and
innovative method for disease therapy. Therefore, it was explored
in the present study whether Bepridil could be repurposed for tumor
therapy. A literature search revealed that in the 1990s, Bepridil
was revealed to be effective for treating different types of
tumors. For example, an early study conducted by van Kalken et
al (41) demonstrated that
Bepridil combined with anthracyclines could reverse anthracycline
resistance in cancer patients. Later, Lee et al (42) evaluated the effects of Bepridil
in vitro and similarly suggested that it could be combined
with Benzamil to effectively inhibit the growth of human brain
tumor cells. More recently, a study conducted by Baldoni et
al (43) demonstrated that
Bepridil could be used for anti-NOTCH1 targeted therapy for
patients with chronic lymphocytic leukemia. However, Bepridil has
not been reported as an anticancer agent for STS. The present study
combined the screening results of three drug-gene interaction
databases that used different algorithms. All three databases
indicated that Bepridil may act as an anticancer agent for several
common histologic subtypes of STS. If it was truly confirmed that
Bepridil could inhibit the proliferation of tumor cells in in
vitro STS cell lines and in vivo orthotopic PDX animal
models, or if it were used for similar clinical in the future,
further studies should be conducted to rationalize the potential
negative side-effects of Bepridil, such as by combining
antiarrhythmic agents and Bepridil. Further studies would then be
required to identify an appropriate method to overcome the
potential side-effects of Bepridil. As Bepridil has previously been
used in clinical practice, the time and cost of reintroducing this
compound into the market may be substantially reduced.
Potential Bepridil targets and pathways were
predicted in order to identify potential correlations between
Bepridil and other common therapies for STS histologic subtypes.
This analysis resulted in the identification of 510 targets and 30
pathways, several of which were reported to be involved in cancer
occurrence or progression. Using the TCGA data, the overall
survival analysis of the genes clustered in these pathways revealed
that CRK, FGFR4, LAMB1, PIK3R2 and WNT5A
(characterized by focal adhesion, signaling pathways regulating
stem cell pluripotency, EGFR tyrosine kinase inhibitor resistance,
ECM-receptor interaction and the PI3K-Akt signaling pathway) were
likely risk factors for STS, while CD47, ELANE, HPGD and
PRKCB (characterized by ECM-receptor interaction,
transcriptional misregulation in cancer, focal adhesion and EGFR
tyrosine kinase inhibitor resistance pathways) were likely
protective factors in STS tissues.
These 9 genes were reported to serve several roles
in malignances. For example, CRK is an adaptor protein that can
affect cancer cell migration and invasion (44,45).
The dysregulation of CRK expression has been implicated in various
aggressive human malignances, including synovial sarcoma, bladder
cancer and breast cancer (46–48).
These findings suggest that CRK may have targeted-therapy potential
in a wide range of tumors. The FGFR protein family is primarily
involved in angiogenesis, the activation of which regulates various
oncogenic processes (49). FGFR4,
one of the FGF receptors, was also demonstrated to be involved in
several important signaling pathways, including the WNT signaling
pathway, the MAPK signaling pathway and the PI3K-Akt signaling
pathway (50). FGFR-targeted
therapy is also considered a promising strategy in refractory
cancer treatment (51). Lin et
al (52) reported that LAMB1
performed better as a diagnostic antigen rather than a
carcino-embryonic antigen for colorectal cancer and may serve as a
potential serological biomarker for digestive cancer diagnosis.
However, the role of LAMB1 in STS has not been reported. In the
present study, it was demonstrated that overexpression of LAMB1 was
correlated with poor prognosis in patients with STS. PIK3R2 is
involved in cell proliferation, migration and survival (53). PIK3R2 was recently reported to be
targeted by microRNA-126-3p and to suppress Kaposi's sarcoma cell
proliferation (54). WNT5A belongs
to the WNT gene family, which encodes secreted signaling
proteins and has been implicated in oncogenesis and several
developmental processes (55,56).
Ye et al (57) reported that
CD47 may be a prognostic marker for oral squamous cell carcinoma.
ELANE has been correlated with neutropenia outcomes (58). HPGD has been demonstrated to
participate in a variety of physiological and pathological
metabolic processes. It has also been identified as a novel
therapeutic target in prostate cancer (59,60)
and is involved in colorectal cancer progression (61). When these nine genes were queried in
the cBioPortal database, it was reported that nearly all were
genetically altered in patients with STS.
SystemsDock is a web-based tool for network
pharmacology-based prediction and analysis. Hsin et al
(30) applied the receiver
operating characteristic (ROC) to demonstrate that systemsDock
possesses a well-designed scoring function [area under the ROC
curve (AUC)=0.84] for molecular docking to evaluate protein-ligand
binding activity. According to the conventional rating, 0.9≤AUC≤1
is considered excellent, 0.80≤AUC<0.9 is good, 0.70≤AUC<0.8
is fair, 0.50≤AUC<0.7 is poor and AUC<0.5 represents failure.
This tool also considers protein structure availability and binding
site certainty, which allows the docking simulation of the
described proteins and their ligand selectivity to occur. According
to the software description, a cut-off score in the range of
4.82–6.11 indicates reliable accuracy (80–83%) when evaluating
protein-ligand binding activity. When systemsDock was applied to
test the protein-ligand binding activity of Bepridil and screen out
the 9 candidate proteins from the KEGG pathways, it was
demonstrated that the lowest docking score was 5.017, which
suggested that Bepridil had relatively stable binding selectivity
with all of the tested proteins. These results indicate that
Bepridil has the potential to become an STS candidate drug. This
theory should be confirmed with further in vitro and in
vivo experiments. If Bepridil could be repurposed for STS
treatment, this may provide a significant benefit to STS patients,
as well as reduce development time and cost.
In conclusion, the present study used a
computational method that combined three drug-gene interaction
databases and a gene-expression signature to explore drug
repositioning. As a result, Bepridil was identified as a potential
candidate for the treatment of STS. A KEGG pathway analysis
predicted that Bepridil may target CRK, FGFR4, LAMB1, PIK3R2, CD47,
ELANE, HPGD and PRKCB to suppress STS development. The pathways
associated with these targets were demonstrated to serve crucial
roles in cancer or cancer treatments. Molecular docking simulations
suggested that these proteins could combine with Bepridil in a
stable manner. These findings provide rationale that Bepridil may
be developed for the treatment of STS. However, the present study
has some limitations. For instance, it derives STS
survival-associated genes from the TCGA database alone; therefore,
it would be desirable to increase the power of the analysis by
including additional datasets. Furthermore, the present study was
simply based on computational approaches without using STS cell
lines and PDX models for further validation. Additionally, when
evaluating molecular docking, a control experiment by assessing the
binding strength of a known inhibitor and Bepridil was not set, as
inhibition constant was built-in in the systemsDock database. The
present authors intend to remedy this limitation in the future
using in vitro and in vivo methodologies. Although
drug repurposing using the computational approach does not
definitively measure the effects of a treatment, it allows the
safety profiling stage to be bypassed, which results in lower costs
and better time efficiency. Therefore, an initial genomics-based
recommendation may be made rapidly, and refinements or changes can
be made when further in vitro and in vivo results
become available.
Acknowledgments
Not applicable.
Funding
The present study was supported by the Guangxi
Medical University Training Program for Distinguished Young
Scholars (GC), the Medical Excellence Award funded by the Creative
Research Development Grant from the First Affiliated Hospital of
Guangxi Medical University (GC), the Guangxi Zhuang Autonomous
Region Health, the Family Planning Commission Self-Financed
Scientific Research Project (grant. no. Z20180979), and the
Innovation Project of Guangxi Graduate Education (grant no.
YCBZ2018038).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author upon reasonable
request.
Authors' contributions
XY, JM and GC were involved in the study design. XY
contributed to the preparation of the manuscript and data analysis.
WTH, HYW, RQH and AGL contributed to the data analysis and prepared
the figures and tables. JM and GC supervised and corrected the
manuscript. All authors read and approved the final manuscript and
agree to be accountable for all aspects of the work.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hoang NT, Acevedo LA, Mann MJ and Tolani
B: A review of soft-tissue sarcomas: Translation of biological
advances into treatment measures. Cancer Manag Res. 10:1089–1114.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Burningham Z, Hashibe M, Spector L and
Schiffman JD: The epidemiology of sarcoma. Clin Sarcoma Res.
2:142012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2018. CA Cancer J Clin. 68:7–30. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Koliou P, Karavasilis V, Theochari M,
Pollack SM, Jones RL and Thway K: Advances in the treatment of soft
tissue sarcoma: Focus on eribulin. Cancer Manag Res. 10:207–216.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bourcier K and Italiano A: Newer
therapeutic strategies for soft-tissue sarcomas. Pharmacol Ther.
188:118–123. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Recine F, Bongiovanni A, Riva N, Fausti V,
De Vita A, Mercatali L, Liverani C, Miserocchi G, Amadori D and
Ibrahim T: Update on the role of trabectedin in the treatment of
intractable soft tissue sarcomas. Onco Targets Ther. 10:1155–1164.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Oliveira IM, Borges A, Borges F and Simoes
M: Repurposing ibuprofen to control Staphylococcus aureus
biofilms. Eur J Med Chem. 166:197–205. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Qu XA and Rajpal DK: Applications of
connectivity map in drug discovery and development. Drug Discov
Today. 17:1289–1298. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cotto KC, Wagner AH, Feng YY, Kiwala S,
Coffman AC, Spies G, Wollam A, Spies NC, Griffith OL and Griffith
M: DGIdb 3.0: A redesign, and expansion of the drug-gene
interaction database. Nucleic Acids Res. 46:D1068–D1073. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wang Z, Lachmann A, Keenan AB and Ma'ayan
A: L1000FWD: Fireworks visualization of drug-induced transcriptomic
signatures. Bioinformatics. 34:2150–2152. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lamb J, Crawford ED, Peck D, Modell JW,
Blat IC, Wrobel MJ, Lerner J, Brunet JP, Subramanian A, Ross KN, et
al: The connectivity map: Using gene-expression signatures to
connect small molecules, genes, and disease. Science.
313:1929–1935. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hurle MR, Yang L, Xie Q, Rajpal DK,
Sanseau P and Agarwal P: Computational drug repositioning: From
data to therapeutics. Clin Pharmacol Ther. 93:335–341. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhong Y, Chen EY, Liu R, Chuang PY,
Mallipattu SK, Tan CM, Clark NR, Deng Y, Klotman PE, Ma'ayan A, et
al: Renoprotective effect of combined inhibition of
angiotensin-converting enzyme, and histone deacetylase. J Am Soc
Nephrol. 24:801–811. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Karube K, Tsuzuki S, Yoshida N, Arita K,
Kato H, Katayama M, Ko YH, Ohshima K, Nakamura S, Kinoshita T, et
al: Comprehensive gene expression profiles of NK cell neoplasms
identify vorinostat as an effective drug candidate. Cancer Lett.
333:47–55. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Dyle MC, Ebert SM, Cook DP, Kunkel SD, Fox
DK, Bongers KS, Bullard SA, Dierdorff JM and Adams CM:
Systems-based discovery of tomatidine as a natural small molecule
inhibitor of skeletal muscle atrophy. J Biol Chem. 289:14913–14924.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gao L, Zhao G, Fang JS, Yuan TY, Liu AL
and Du GH: Discovery of the neuroprotective effects of alvespimycin
by computational prioritization of potential anti-Parkinson agents.
FEBS J. 281:1110–1122. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chen YT, Xie JY, Sun Q and Mo WJ: Novel
drug candidates for treating esophageal carcinoma: A study on
differentially expressed genes, using connectivity mapping, and
molecular docking. Int J Oncol. 54:152–166. 2019.PubMed/NCBI
|
|
18
|
Drullion C, Marot G, Martin N, Desle J,
Saas L, Salazar-Cardozo C, Bouali F, Pourtier A, Abbadie C and
Pluquet O: Pre-malignant transformation by senescence evasion is
prevented by the PERK and ATF6alpha branches of the Unfolded
protein response. Cancer Lett. 438:187–196. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tang X, Xu Y, Lu L, Jiao Y, Liu J, Wang L
and Zhao H: Identification of key candidate genes, and small
molecule drugs in cervical cancer by bioinformatics strategy.
Cancer Manag Res. 10:3533–3549. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Christinat A and Leyvraz S: Role of
trabectedin in the treatment of soft tissue sarcoma. Onco Targets
Ther. 2:105–113. 2009.PubMed/NCBI
|
|
21
|
Demetri GD, von Mehren M, Jones RL,
Hensley ML, Schuetze SM, Staddon A, Milhem M, Elias A, Ganjoo K,
Tawbi H, et al: Efficacy and safety of trabectedin or dacarbazine
for metastatic liposarcoma or leiomyosarcoma after failure of
conventional chemotherapy: Results of a Phase III randomized
multicenter clinical trial. J Clin Oncol. 34:786–793. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Xie L, Guo W, Wang Y, Yan T, Ji T and Xu
J: Apatinib for advanced sarcoma: Results from multiple
institutions' off-label use in China. BMC Cancer. 18:3962018.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhu B, Li J, Xie Q, Diao L, Gai L and Yang
W: Efficacy and safety of apatinib monotherapy in advanced bone and
soft tissue sarcoma: An observational study. Cancer Biol Ther.
19:198–204. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Li S, Chen X, Liu X, Yu Y, Pan H, Haak R,
Schmidt J, Ziebolz D and Schmalz G: Complex integrated analysis of
lncRNAs-miRNAs-mRNAs in oral squamous cell carcinoma. Oral Oncol.
73:1–9. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Brum AM, van de Peppel J, Nguyen L, Aliev
A, Schreuders- Koedam M, Gajadien T, van der Leije CS, van Kerkwijk
A, Eijken M, van Leeuwen JPTM, et al: Using the connectivity map to
discover compounds influencing human osteoblast differentiation. J
Cell Physiol. 233:4895–4906. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wang J, Vasaikar S, Shi Z, Greer M and
Zhang B: WebGestalt 2017: A more comprehensive, powerful, flexible,
and interactive gene set enrichment analysis toolkit. Nucleic Acids
Res. 45:W130–W137. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yoav Benjamini and Yosef Hochberg:
Controlling the false discovery rate: A practical and powerful
approach to multiple testing. J R Stat Soc Series B. 57:289–300.
1995.
|
|
28
|
Vilar S, Sobarzo-Sanchez E, Santana L and
Uriarte E: Molecular docking and drug discovery in beta-Adrenergic
receptors. Curr Med Chem. 24:4340–4359. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Eswari JS, Dhagat S, Kaser S and Tiwari A:
Homology modeling and molecular docking studies of bacillomycin and
iturin synthetases with novel ligands for the production of
therapeutic lipopeptides. Curr Drug Discov Technol. 15:132–141.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hsin KY, Matsuoka Y, Asai Y, Kamiyoshi K,
Watanabe T, Kawaoka Y and Kitano H: systemsDock: A web server for
network pharmacology-based prediction and analysis. Nucleic Acids
Res. 44:W507–W513. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Jain AN: Surflex: Fully automatic flexible
molecular docking using a molecular similarity-based search engine.
J Med Chem. 46:499–511. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Zsoldos Z, Reid D, Simon A, Sadjad BS and
Johnson AP: eHiTS: An innovative approach to the docking and
scoring function problems. Curr Protein Pept Sci. 7:421–435. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ma F, Takanari H, Masuda K, Morishima M
and Ono K: Short- and long-term inhibition of cardiac
inward-rectifier potassium channel current by an antiarrhythmic
drug bepridil. Heart Vessels. 31:1176–1184. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Vitiello PP, Cardone C, Martini G,
Ciardiello D, Belli V, Matrone N, Barra G, Napolitano S, Della
Corte C, Turano M, et al: Receptor tyrosine kinase-dependent PI3K
activation is an escape mechanism to vertical suppression of the
EGFR/RAS/MAPK pathway in KRAS-mutated human colorectal cancer cell
lines. J Exp Clin Cancer Res. 38:412019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Ge W, Wang SH, Sun B, Zhang YL, Shen W,
Khatib H and Wang X: Melatonin promotes Cashmere goat (Capra
hircus) secondary hair follicle growth: A view from integrated
analysis of long non-coding and coding RNAs. Cell Cycle.
17:1255–1267. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Doi T, Yang JC, Shitara K, Naito Y, Cheng
AL, Sarashina A, Pronk LC, Takeuchi Y and Lin CC: Phase I study of
the focal adhesion kinase inhibitor BI 853520 in Japanese and
Taiwanese patients with advanced or metastatic solid tumors. Target
Oncol. Feb 6–2019.(Epub ahead of print). doi:
10.1007/s11523-019-00620-0. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Paik H, Chung AY, Park HC, Park RW, Suk K,
Kim J, Kim H, Lee K and Butte AJ: Repurpose terbutaline sulfate for
amyotrophic lateral sclerosis using electronic medical records. Sci
Rep. 5:85802015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Dudley JT, Sirota M, Shenoy M, Pai RK,
Roedder S, Chiang AP, Morgan AA, Sarwal MM, Pasricha PJ and Butte
AJ: Computational repositioning of the anticonvulsant topiramate
for inflammatory bowel disease. Sci Transl Med. 3:96ra762011.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Musa A, Ghoraie LS, Zhang SD, Glazko G,
Yli-Harja O, Dehmer M, Haibe-Kains B and Emmert-Streib F: A review
of connectivity map, and computational approaches in
pharmacogenomics. Brief Bioinform. 19:506–523. 2018.PubMed/NCBI
|
|
40
|
Gaspar T, Kis B, Snipes JA, Lenzsér G,
Mayanagi K, Bari F and Busija DW: Neuronal preconditioning with the
antianginal drug, bepridil. J Neurochem. 102:595–608. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
van Kalken CK, van der Hoeven JJ, de Jong
J, Giaccone G, Schuurhuis GJ, Maessen PA, Blokhuis WM, van der
Vijgh WJ and Pinedo HM: Bepridil in combination with anthracyclines
to reverse anthracycline resistance in cancer patients. Eur J
Cancer. 27:739–744. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Lee YS, Sayeed MM and Wurster RD:
Intracellular Ca2+ mediates the cytotoxicity induced by
Bepridil, and benzamil in human brain tumor cells. Cancer Lett.
88:87–91. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Baldoni S, Del Papa B, Dorillo E, Aureli
P, De Falco F, Rompietti C, Sorcini D, Varasano E, Cecchini D, Zei
T, et al: Bepridil exhibits anti-leukemic activity associated with
NOTCH1 pathway inhibition in chronic lymphocytic leukemia. Int J
Cancer. 143:958–970. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Li C, Zeng X, Liu Z, Li F, Wang K and Wu
B: BDNF VAL66MET polymorphism elevates the risk of bladder cancer
via MiRNA-146b in Micro-Vehicles. Cell Physiol Biochem. 45:366–377.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Gong XH, Chen C, Hou P, Zhu SC, Wu CQ,
Song CL, Ni W, Hu JF, Yao DK, Kang JH, et al: Overexpression of
miR-126 inhibits the activation, and migration of HSCs through
targeting CRK. Cell Physiol Biochem. 33:97–106. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Watanabe T, Tsuda M, Tanaka S, Ohba Y,
Kawaguchi H, Majima T, Sawa H and Minami A: Adaptor protein Crk
induces Src-dependent activation of p38 MAPK in regulation of
synovial sarcoma cell proliferation. Mol Cancer Res. 7:1582–1592.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Matsumoto R, Tsuda M, Wang L, Maishi N,
Abe T, Kimura T, Tanino M, Nishihara H, Hida K, Ohba Y, et al:
Adaptor protein CRK induces epithelial-mesenchymal transition, and
metastasis of bladder cancer cells through HGF/c-Met feedback loop.
Cancer Sci. 106:709–717. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Kumar S, Lu B, Davra V, Hornbeck P,
Machida K and Birge RB: Crk tyrosine phosphorylation regulates
PDGF-BB-inducible Src activation, and breast tumorigenicity, and
metastasis. Mol Cancer Res. 16:173–183. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Xu M, Chen S, Yang W, Cheng X, Ye Y, Mao
J, Wu X, Huang L and Ji J: FGFR4 links glucose metabolism, and
chemotherapy resistance in breast cancer. Cell Physiol Biochem.
47:151–160. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Katoh M and Nakagama H: FGF receptors:
Cancer biology, and therapeutics. Med Res Rev. 34:280–300. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Schelch K, Kirschner MB, Williams M, Cheng
YY, van Zandwijk N, Grusch M and Reid G: A link between the
fibroblast growth factor axis, and the miR-16 family reveals
potential new treatment combinations in mesothelioma. Mol Oncol.
12:58–73. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Lin Q, Lim HS, Lin HL, Tan HT, Lim TK,
Cheong WK, Cheah PY, Tang CL, Chow PK and Chung MC: Analysis of
colorectal cancer glyco-secretome identifies laminin β-1 (LAMB1) as
a potential serological biomarker for colorectal cancer.
Proteomics. 15:3905–3920. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Qi L, Sun K, Zhuang Y, Yang J and Chen J:
Study on the association between PI3K/AKT/mTOR signaling pathway
gene polymorphism, and susceptibility to gastric cancer. J BUON.
22:1488–1493. 2017.PubMed/NCBI
|
|
54
|
Wu XJ, Zhao ZF, Kang XJ, Wang HJ, Zhao J
and Pu XM: MicroRNA-126-3p suppresses cell proliferation by
targeting PIK3R2 in Kaposi's sarcoma cells. Oncotarget.
7:36614–36621. 2016.PubMed/NCBI
|
|
55
|
Kobayashi Y, Kadoya T, Amioka A, Hanaki H,
Sasada S, Masumoto N, Yamamoto H, Arihiro K, Kikuchi A and Okada M:
Wnt5a-induced cell migration is associated with the aggressiveness
of estrogen receptor-positive breast cancer. Oncotarget.
9:20979–20992. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Wang L, Yao M, Fang M, Zheng WJ, Dong ZZ,
Pan LH, Zhang HJ and Yao DF: Expression of hepatic Wnt5a, and its
clinicopathological features in patients with hepatocellular
carcinoma. Hepatobiliary Pancreat Dis Int. 17:227–232. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Ye X, Wang X, Lu R, Zhang J, Chen X and
Zhou G: CD47 as a potential prognostic marker for oral leukoplakia,
and oral squamous cell carcinoma. Oncol Lett. 15:9075–9080.
2018.PubMed/NCBI
|
|
58
|
Makaryan V, Zeidler C, Bolyard AA, Skokowa
J, Rodger E, Kelley ML, Boxer LA, Bonilla MA, Newburger PE,
Shimamura A, et al: The diversity of mutations, and clinical
outcomes for ELANE-associated neutropenia. Curr Opin Hematol.
22:3–11. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Vainio P, Gupta S, Ketola K, Mirtti T,
Mpindi JP, Kohonen P, Fey V, Perälä M, Smit F, Verhaegh G, et al:
Arachidonic acid pathway members PLA2G7, HPGD, EPHX2, and
CYP4F8 identified as putative novel therapeutic targets in
prostate cancer. Am J Pathol. 178:525–536. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Qi X, Wang Y, Hou J and Huang Y: A Single
nucleotide polymorphism in HPGD gene is associated with
prostate cancer risk. J Cancer. 8:4083–4086. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Pereira C, Queiros S, Galaghar A, Sousa H,
Pimentel-Nunes P, Brandão C, Moreira-Dias L, Medeiros R and
Dinis-Ribeiro M: Genetic variability in key genes in prostaglandin
E2 pathway (COX-2, HPGD, ABCC4, and
SLCO2A1), and their involvement in colorectal cancer
development. PLoS One. 9:e920002014. View Article : Google Scholar : PubMed/NCBI
|