Introduction
Colorectal cancer (CRC) is the second most commonly
diagnosed gastrointestinal malignant neoplasm, and one of the
leading causes of cancer-associated mortality all over the world in
2015 (1). There were ~1.4 million
new cases and 0.7 million deaths worldwide in 2012 (2). The recurrence rate is higher than 11
and 40–50% in postoperative patients with stage II and III CRC,
respectively (3). The high
recurrence rate of CRC is a major contributor to poor prognosis,
and poor prognosis in patients with CRC is associated with tumor
invasion and metastasis (4,5). The development of metastasis is
complex, and includes proliferation, angiogenesis, invasion,
detachment, migration, adhesion and extravasation into target
organs (4). Research investigating
the mechanism into the origin and development of CRC has identified
a high number of biomarkers, as well as identifying signaling
pathways that are vital for tumorigenesis and progression of CRC
(5). However, only a few of the
identified biomarkers have clinicopathological significance in CRC.
Therefore, it is important to identify additional master genes that
are associated with the progression and metastasis of CRC, which
may provide more reliable molecular targets for therapy and improve
the prognosis of CRC patients.
Protein/nucleic acid deglycase DJ-1 (DJ-1) is a
20-kDa conserved protein, which belongs to the DJ-1/ThiJ/Pfp I
protein superfamily. DJ-1 is widely expressed in various tissues,
and previous studies have shown that DJ-1 is associated with
early-onset Parkinson's disease (6). Subsequent research has found that DJ-1
is associated with numerous types of cancer, such as lung and
pancreatic cancer (7–9). DJ-1 promotes the active efflux of
drugs and enhances the anti-apoptotic ability of multidrug
resistant gastric cancer cells by upregulating P-gp and Bcl-2
(10). As an oncogene, DJ-1 was
found to promote tumor cell migration and invasion through the
PI3K/Akt/mTOR and SRC/ERK/uPA signaling pathways in pancreatic
cancer (11,12). DJ-1 is suggested to promote the
survival of human CRC cells through the PTEN-AKT, PLAGL2/Wnt/BMP4
or PI3K-AKT pathways (13–15). In addition, a number of studies have
investigated treatment and diagnosis in clinical cancer.
Overexpression of DJ-1 has been reported in numerous types of
cancer, including breast cancer (9), melanoma (16), pancreatic cancer (17), astrocytic gliomas (18) and endometrial cancer (19). However, the precise role of DJ-1 in
the occurrence and development, and clinical treatment of CRC
remains unknown.
In the present study, DJ-1 was identified as a novel
biomarker to predict the prognosis of patients with CRC. DJ-1 may
predict the effect of chemotherapy based on clinical samples from
CRC database, but further investigation is required to identify how
DJ-1 regulates CRC cell proliferation, migration, invasion in
vitro and in vivo.
Materials and methods
Patient specimens and tissue
samples
The tissue microarray (TMA) cohort consisted of 470
CRC surgical samples from Yixing Hospital (Jiangsu, China)
recruited between January 2000 to December 2006. These patients
were followed up for at least 5 years. Overall survival (OS) was
the primary endpoint of the analysis, and survival time was
calculated from the date of surgery to the date of death or to the
last follow-up. The median follow-up time was 59.3 months. In the
CRC database, the mean age of all patients was 63 years. The age
range was 30–88 years. There were 281 male and 189 female patients.
The clinicopathological characteristics of the patients are
summarized in Table SI.
A total of 8-paired fresh samples that were
collected most recently were frozen in liquid nitrogen immediately
for western blot analysis. The present study was granted ethical
approval by the Institutional Review Board of Yixing Hospital
Affiliated to Medical College of Yangzhou University (Yixing,
Jiangsu). All patients provided written informed consent and all
acquired data were assured of anonymity and confidentiality.
Construction of TMA
The CRC samples and matched non-cancerous colon
tissues of patients with CRC were collected to construct the TMA.
All tissue sections were fixed in formalin and embedded in
paraffin. The CRC TMAs included 940 cores and were constructed by
the Shanghai National Engineering Center for Biochip. Each sample
was punched to a 1.0-mm diameter from the paraffin tumor block and
the corresponding non-tumoral tissues. The thickness of each slide
was 4-µm.
Immunohistochemistry (IHC)
The standard protocol used for the immunostaining
was used as previously described (20). The TMA was heated at 55°C for 20 min
and then washed with xylene 3 times to remove the paraffin.
Following which, the chip was washed with absolute ethyl alcohol.
Antigen retrieval step was then performed using 10 mmol/l sodium
citrate (pH 6.0) and the samples were incubated at 95°C for 30 min.
Serum blocking was subsequently performed for 30 min. The
monoclonal mouse anti-DJ-1 (dilution 1:200; cat. no. sc-55572;
Santa Cruz Biotechnology, Inc.), monoclonal rabbit anti-cyclin E
(dilution 1:200; cat. no. 4136; Cell Signaling Technology, Inc.),
anti-phosphorylated(p)-PI3K (dilution 1:200; cat. no. 17366; Cell
Signaling Technology, Inc.), anti-p-Akt (dilution 1:200; cat. no.
4060; Cell Signaling Technology, Inc.), anti-p-mTOR (dilution
1:200; cat. no. 5536; Cell Signaling Technology, Inc.), anti-p27
(dilution 1:200; product code ab32034; Epitomics; Abcam),
anti-cyclin E (dilution 1:200; product code ab32103; Epitomics;
Abcam), anti-NF-κB (dilution 1:200; cat. no. 8242; Cell Signaling
Technology, Inc.), anti-Snail (dilution 1:200; cat. no. 3879; Cell
Signaling Technology, Inc.), anti-N-cadherin (dilution 1:200; cat.
no. 13116; Cell Signaling Technology, Inc.), anti-E-cadherin
(dilution 1:200; cat. no. 14472; Cell Signaling Technology, Inc.)
and anti-vimentin (dilution 1:200; product code ab92547; Epitomics;
Abcam) antibodies were used for primary antibody incubation
overnight at 4°C. The samples were incubated with the respective
rabbit or mouse secondary antibody (dilution 1:200; product codes
150077 or 150177; Epitomics; Abcam) for 30 min followed by
hematoxylin staining using a 3,3′-diamido-plate. Dehydration was
subsequently performed and sample sections were sealed by cover
glasses. Once the tissue microarray was detected by
immunohistochemistry, the dot array tissue would surely fall off.
Thus, we could not acquire the data of 470 cases. We controlled the
stripping rate to less than 5%.
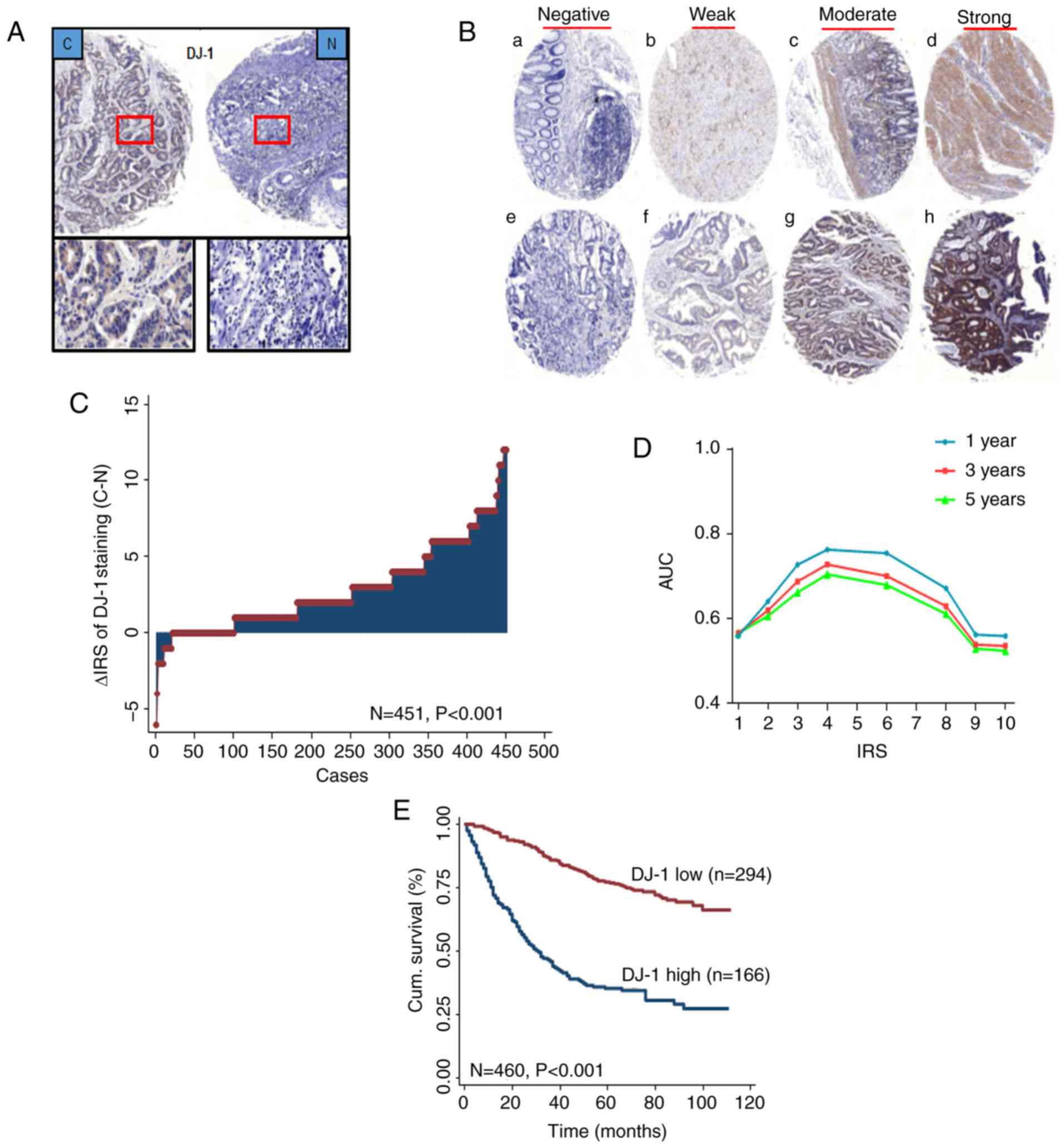
Assessment of IHC
A semi-quantitative immunoreactivity score (IRS) was
applied as previously described (21,22). A
total of two independent pathologists, blinded to the study data,
analyzed the staining of DJ-1 in the tissues, as shown in Fig. 2B. The receiver operator
characteristic (ROC) analysis was used to determine the optimum
cut-off value of IRS. The optimal cut-off value of DJ-1 IRS was 4,
as it had the best predictive value for survival (Fig. 2D). The tissues with IRS 0–3 and 4–12
were classified as low or high expression of DJ-1 in tumors,
respectively. In TMA, there were 465 plots in 470 tumor tissues.
The few discrepancies were resolved by consensus using a multihead
microscope.
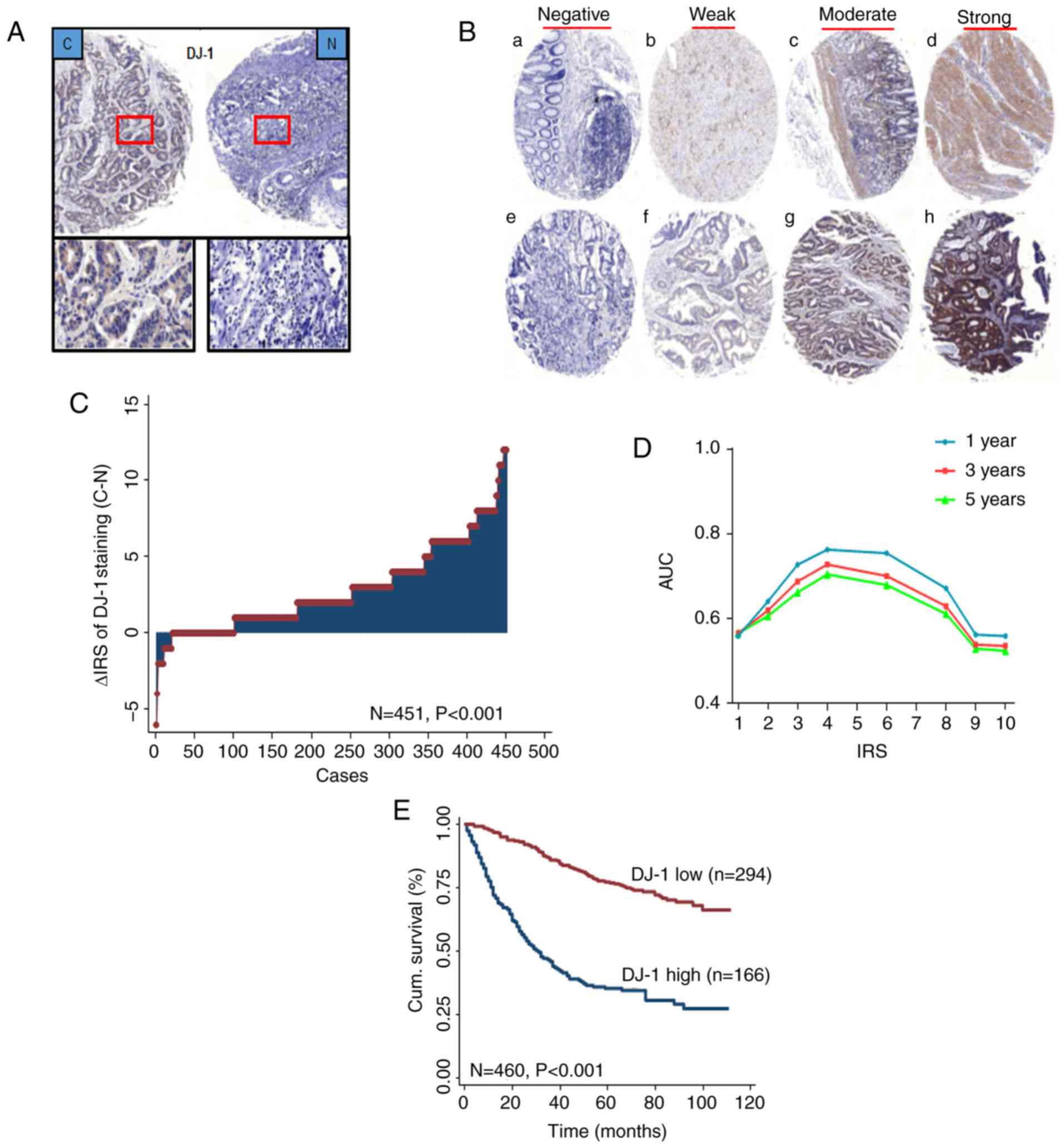 | Figure 2.DJ-1 is elevated in CRC and
associated with poor prognosis of CRC patients. (A) Representative
images of DJ-1 immunohistochemical staining in TMA are shown: Top
panels, original magnification, ×40; bottom panels, ×200. (B)
Representative images of DJ-1 immunohistochemical staining in CRC
cancer and adjacent normal tissues. (a-d) Adjacent normal tissue
and (e-h) cancer tissue. (a and e) Negative staining, (b and f)
weak staining, (c and g) moderate staining and (d and h) strong
staining. All panels, original magnification, ×40. (C) Distribution
of the difference in DJ-1 staining in CRC compared with that in the
paired normal tissues in the TMA. The expression of DJ-1 was higher
in cancer tissues than normal tissues (P<0.001). (D) Area under
the curve (AUC) at different cut-off values for DJ-1
immunoreactivity score (IRS) for 1-, 3- and 5-year OS. The optimal
cut-off point of DJ-1 IRS was 4. (E) Kaplan-Meier curves of the
patients with low/high DJ-1 expression. CRC patients with high DJ-1
expression had a worse OS than the patients with low expression
(P<0.001). CRC, colorectal cancer; TMA, tumor microarray; OS,
overall survival. |
Animals and cell lines
Forty-eight female BALB/c nude mice were purchased
from the Comparative Medicine Laboratory Animal Center (license no.
scxk (SU) 2012-0004) of Yangzhou University. The mice, aged 6–8
weeks, 18–26 g, were maintained in specific pathogen-free
conditions and cared for in accordance with the National Institutes
of Health Guide for the Care and Use of Laboratory Animals
(https://www.ncbi.nlm.nih.gov/books/NBK54050/). The
protocols were approved by the Institutional Animal Care and Use
Committee of Yangzhou University. The human SW620, DLD-1, RKO,
HCT116, SW480, HT29, HCT15 CRC and normal FHC cell lines were
purchased from the Shanghai Institute of Biochemistry and Cell
Biology, Chinese Academy of Sciences. Cells were cultured in
RPMI-1640 medium containing 100 U/ml penicillin, 100 µg/ml
streptomycin and 10% fetal bovine serum (FBS) and maintained at
37°C in a humidified incubator with 5% CO2.
Lentiviral infection and generation of
stable cell lines
The HCT116 cells were infected with lentivirus
(LV)-DJ-1, LV-DJ-1-control (ctrl), LV-DJ-1-RNA interference (RNAi)
and LV-DJ-1-RNAi-ctrl with a multiplicity of infection (MOI) 20 and
10 µg/ml polybrene (Shanghai GeneChem Co., Ltd.). A total of 8 h
after lentiviral infection, the HCT116 cells were maintained in
RPMI-1640 medium. Subsequently after 24 h, the cells were selected
using puromycin (Gibco; Thermo Fisher Scientific, Inc.) at a final
concentration of 2 µg/ml. The transgenic efficiency was detected
using fluorescence microscopy according to the GFP of the
lentivirus. The knockdown and overexpression efficiency of DJ-1 was
further analyzed using western blot analysis.
Cell Counting Kit (CCK)-8 assay
The LV-DJ-1 and LV-DJ-1-RNAi HCT116 cells and the
corresponding controls were seeded at a density of 8×103
cells/100 µl culture medium per well in 96-well plates. The cell
proliferation ability was analyzed 12, 24, 48, 60 and 72 h after
cell culture using a CCK-8 solution (Dojindo Molecular
Technologies, Inc.) according to the manufacturer's instructions.
An automatic microplate reader measured the optical density of each
well at 450 nm.
EdU immunofluorescence assay
The LV-DJ-1 and LV-DJ-1-RNAi HCT116 cells and the
corresponding controls were seeded in 96-well plates at a density
of 5×103 cells/100 µl culture medium. After 24 h of
culture, EdU immunofluorescence analysis was performed using the
EdU kit according to manufacturer's protocol (Guangzhou RiboBio
Co., Ltd.).
Cell cycle analysis
The LV-DJ-1 and LV-DJ-1-RNAi HCT116 cells and the
corresponding controls were fixed with 70% cold ethanol overnight
at 4°C and stained with 20 µg/ml propidium iodide (PI) in 0.1%
Triton X-100 for 15 min. Samples were subsequently analyzed using a
flow cytometer (BD Biosciences).
Transwell and Matrigel assays
The LV-DJ-1 and LV-DJ-1-RNAi HCT116 cells and the
corresponding controls (5×105 cells/100 µl serum-free
RPMI-1640) were seeded onto the upper chamber of Transwell filters
(8-µm pore size; EMD Millipore; Merck KGaA). The Transwell filter
inserts were coated with or without Matrigel (EMD Millipore; Merck
KGaA) for the cell invasion and migration assays, respectively. The
bottom chamber was filled with 500 µl RPMI-1640 medium containing
10% FBS. After incubation for 24 h the cells on the upper surface
of the filters were removed with a cotton swab. The cells that had
traversed the membrane were fixed with 4% paraformaldehyde and
stained with 0.4% crystal violet solution for 30 min at room
temperature. The number of invaded and migrated tumor cells was
counted under an inverted microscope (original magnification, ×40)
and images were captured by the 1X73 inverted fluorescence
microscope.
Wound healing assay
The LV-DJ-1 and LV-DJ-1-RNAi HCT116 cells and the
corresponding controls (2×105 cells) were cultured in
6-well plates and grown to 80% confluence. The wound was scratched
using a 10-µl pipette tip across the entire diameter of the well,
and rinsed with PBS to remove all cellular debris. RPMI-1640 medium
containing 2% FBS was then added to maintain cell growth during the
assay. The process of tumor cell migration was observed and images
were obtained at a low-power field (×50) under the 1X73 inverted
fluorescence microscope at 0, 24 and 48 h after the wound was
created. The closure rate reflected the migratory ability of the
tumor cells. Three random measurements were made per photographed
sample at every time point, which was used as baseline. AxioVision
Rel. 4.8 software was used for the measurements.
Western blot analysis
Cells or tissues were lysed with cold lysis buffer
supplemented with a protease inhibitor mixture on ice for 30 min.
The total protein concentration was measured using the
Bicinchoninic Acid Protein assay kit (Thermo Fisher Scientific,
Inc.). Western blots were performed as previously described
(23). The monoclonal mouse
anti-DJ-1 (dilution 1:1,000; Santa Cruz Biotechnology, Inc.),
monoclonal rabbit anti-cyclin E (dilution 1:1,000; Cell Signaling
Technology, Inc.), anti-PI3K (dilution 1:1,000; Cell Signaling
Technology, Inc.), anti-Akt (dilution 1:1,000, Cell Signaling
Technology, Inc.), anti-p-PI3K (dilution 1:1,000; Cell Signaling
Technology, Inc.), anti-p-Akt (dilution 1:1,000; Cell Signaling
Technology, Inc.), anti-mTOR (dilution 1:1,000; Cell Signaling
Technology, Inc.), anti-p-mTOR (dilution 1:1,000; Cell Signaling
Technology, Inc.), anti-P27 (dilution 1:2,000; Epitomics; Abcam),
anti-cyclin E (dilution 1:2,000; Epitomics; Abcam), anti-NF-κB
(dilution 1:1,000; Cell Signaling Technology, Inc.), anti-Snail
(dilution 1:1,000; Cell Signaling Technology, Inc.),
anti-N-cadherin (dilution 1:1,000; Cell Signaling Technology,
Inc.), anti-E-cadherin (dilution 1:1,000; Cell Signaling
Technology, Inc.) and anti-vimentin (dilution 1:1,000, Epitomics;
Abcam) antibodies were used for antibody incubation overnight at
4°C. The polyclonal mouse anti-actin (dilution 1:2,000; cat. no.
CSB-PA007670HA01; Wuhan Boster Biological Technology, Ltd.) was
used for the protein loading control. Each blot was repeated three
times. The intensity of the protein bands was analyzed using
densitometry by Image J software (National Institutes of Health,
Bethesda, MD, USA) after normalization to the corresponding protein
controls.
Reverse transcription-quantitative PCR
(RT-qPCR)
The total RNAs from CRC and FHC cells were extracted
using RNeasy Mini kit (Invitrogen; Thermo Fisher Scientific, Inc.)
according to the manufacturer's instructions using RNase-free
conditions. The purified RNAs were reversely transcribed to first
strand cDNA using a RevertAid RT reverse transcription kit (Thermo
Fisher Scientific, Inc.). SYBR Green Real-Time qPCR analysis was
performed using an Applied Biosystems 7500 Real-Time PCR System
(Roche Applied Science). The thermocycling conditions are as
follows: Pre-denaturation temperature: 95°C, 6 min; melting
temperature: 95°C, 10 sec, 65°C, 60 sec, 97°C, 1 sec; amplification
temperature: 95°C, 10 sec, 60°C, 10 sec, 72°C, 10 sec; then went
through 40 cycles.
Human DJ-1 and GAPDH specific primers (DJ-1 forward,
5′-CCATATGATGTGGTGGTTCTAC-3′ and reverse,
5′-CGTCTGGGCTGTAGTCGGAT-3′; GAPDH forward,
5′-ACGGATTTGGTCGTATTGGG-3′ and reverse, 5′-CGCTCCTGGAAGATGGTGAT-3′)
(Sangon Biotechnology Inc.) were used. The relative expression
level of DJ-1 mRNA was normalized to GAPDH internal control and
analyzed using the 2−ΔΔCq method (24). All reactions were performed in
duplicate.
Tumor xenograft and abdominal
metastasis model
In the tumor xenograft model, the LV-DJ-1 and
LV-DJ-1-RNAi HCT116 cells and the corresponding controls (0.2 ml
1×107 cells/mouse; 5 mice/group) were injected
subcutaneously into the flanks of BALB/c nude mice. The tumor size
was measured using a caliper upon palpable every 3 days. The
following equation was used to calculate the tumor volume: V = L ×
W2 × π/6 (V, volume; L, length; W, width). After 24
days, the mice were sacrificed by cervical dislocation. The tumors
were removed and images were obtained. Each tumor was divided into
2 pieces and fixed in 10% buffered formalin.
In the peritoneal metastasis model, the same cells
and groups were used as in the xenograft model, and inoculated into
the peritoneal cavity of BALB/c nude mice. The weight of each mouse
was recorded every 2 days. Mice were euthanized and examined
macroscopically for the presence of peritoneal metastasis after 22
days. Intraperitoneal metastatic tumors were displayed, images were
obtained and fixed in 10% formalin.
All experimental animal procedures were performed in
compliance with the institutional ethics requirements and approved
by the Institutional Animal Care and Use Committee of Yangzhou
University.
Statistical analysis
The significance of associations between DJ-1
staining patterns and clinicopathological data was evaluated using
Fisher's exact test. The paired Wilcoxon test (raw scores) was used
to assess the significance of the difference of DJ-1 staining
levels in tumor samples compared with that in the paired non-tumor
samples. We used ANOVA (Tukey's) method to compare CRC cells with
FHC cells, and the DJ-1 transfection groups with the control group.
Kaplan-Meier survival analysis was performed to calculate OS and
evaluate the prognostic value of patients with DJ-1 expression. Cox
proportional hazards model was performed to analyze DJ-1 expression
as a potential biomarker for predicting patient survival. All the
statistical analyses were performed using STATA software (version
10.1; StataCorp LP). P<0.05 was considered to indicate a
statistically significant difference.
Results
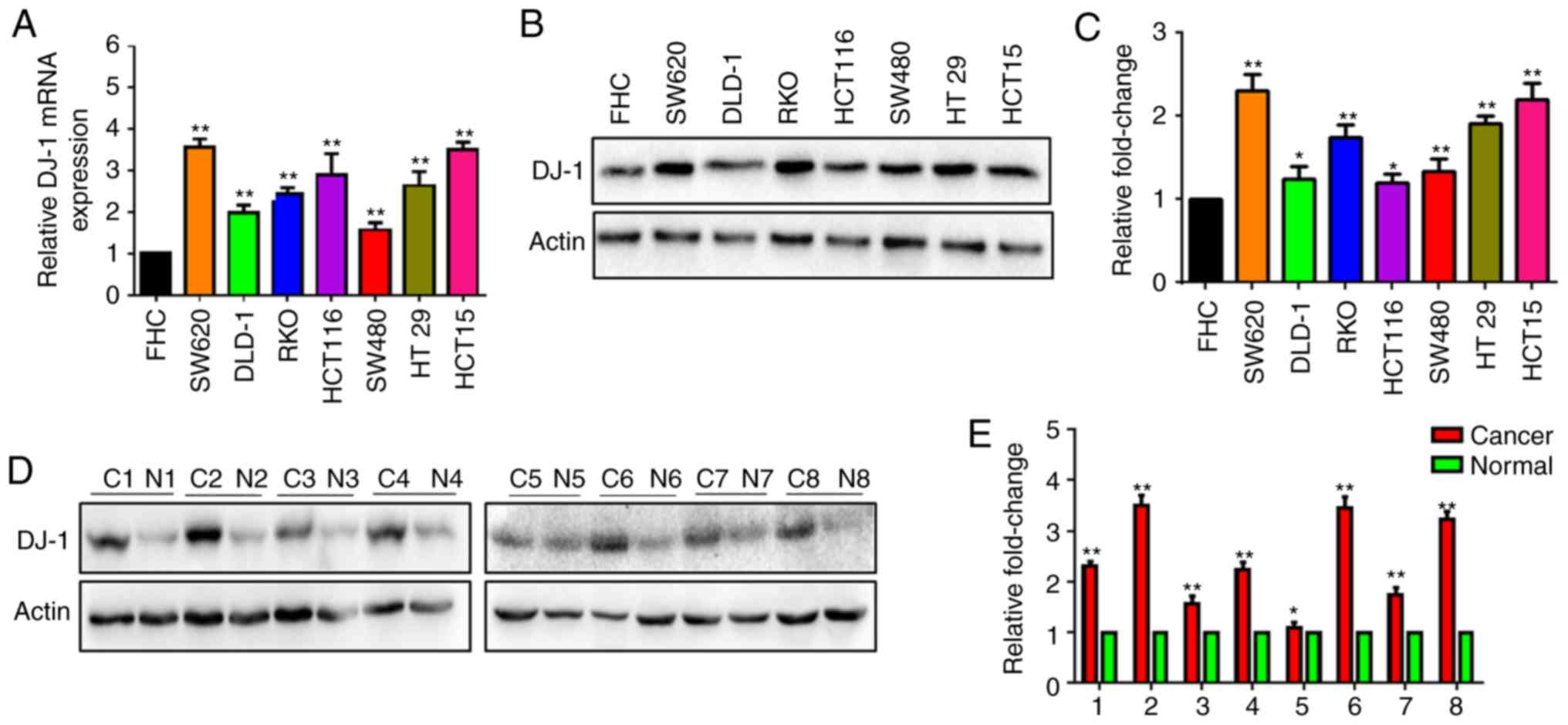
DJ-1 expression is increased in human
CRC cells and tissues
The DJ-1 mRNA level was determined in human CRC and
FHC cells using RT-qPCR. The DJ-1 mRNA level was significantly
higher in the SW620, DLD-1, RKO, HCT116, SW480, HT29 and HCT15
cells compared with that in normal FHC cells (Fig. 1A). Simultaneously, DJ-1 protein
expression was determined in six CRC cell lines and FHC using
western blot analysis. The results revealed that DJ-1 protein
expression was increased in the CRC cells compared with that in FHC
(Fig. 1B). The expression of DJ-1
protein was further detected in 8 CRC tissues (C1-C8) and
corresponding normal tissues (N1-N8). The expression of DJ-1
protein was increased in the CRC tissues (Fig. 1D). A statistical analysis indicated
that DJ-1 strip gray value was significantly overexpressed in the
CRC cells or tumor tissues, respectively (Fig. 1C and E). These results indicated
that DJ-1 expression was increased in CRC.
Increased DJ-1 expression in CRC is
associated with metastasis and poor OS in patients with CRC
To further reveal the role of DJ-1 in CRC, IHC was
used to detect the expression of DJ-1 in a CRC TMA. Strong DJ-1
cytoplasm and nuclear staining was primarily found in CRC tissues
and corresponding normal tissues (Fig.
2A). As shown in Fig. 2B,
representative images of immunostaining revealed negative, weak,
moderate, and strong expression levels in CRC tissues and
corresponding normal tissues, and DJ-1 expression was upregulated
in 351 of 451 (77.8%) tumors compared with that in the paired
normal tissues (P<0.001; Fig.
2C).
In the CRC cohort, there was a significant
association between high DJ-1 expression in cancerous tissues and
depth of invasion (P<0.001), lymph node metastasis (P<0.001),
and TNM stages (P<0.001; Table
I). DJ-1 expression had a trend with age (P=0.050). There was
no association between DJ-1 expression and sex, pathological
classification, and tumor diameter (Table I). In addition, Kaplan-Meier
survival curves were used to determine 5-year overall cumulative
survival in patients with high and low DJ-1 expression levels.
Patients with high DJ-1 expression levels had a worse OS compared
with patients with low expression (P<0.001; Fig. 2E) and DJ-1 expression had the best
predictive value for survival (Fig.
2D) upon assessment of IHC.
 | Table I.Association between expression levels
of DJ-1 and clinicopathological features in the CRC patients
(N=460). |
Table I.
Association between expression levels
of DJ-1 and clinicopathological features in the CRC patients
(N=460).
|
| DJ-1
expression |
|
|---|
|
|
|
|
|---|
| Variables | Low, n (%) | High, n (%) |
P-valuea |
|---|
| All patients | 294 (63.9) | 166 (36.1) |
|
| Age (years) |
|
| 0.050 |
|
≤65 | 177 (67.3) | 86 (32.7) |
|
|
>65 | 117 (59.4) | 80 (40.6) |
|
| Sex |
|
| 0.229 |
|
Male | 180 (65.5) | 95 (34.5) |
|
|
Female | 114 (61.6) | 71 (38.4) |
|
| Pathological
classificationb |
|
| 0.454 |
| I | 3 (60.0) | 2 (40.0) |
|
| II | 267 (64.3) | 148 (35.7) |
|
|
III | 19 (54.3) | 16 (45.7) |
|
| Depth of
invasionb |
|
| <0.001 |
|
T1/T2 | 78 (78.8) | 21 (21.2) |
|
|
T3/T4 | 211 (59.3) | 145 (40.7) |
|
| Lymph node
metastasisb |
|
| <0.001 |
| N0 | 204 (75.8) | 65 (24.2) |
|
|
N1/N2 | 86 (46.0) | 101 (54.0) |
|
| TNM
stageb |
|
| <0.001 |
| I | 68 (80.0) | 17 (20.0) |
|
| II | 133 (76.0) | 42 (24.0) |
|
|
III | 82 (46.3) | 95 (53.7) |
|
| IV | 6 (35.3) | 11 (64.7) |
|
| Tumor
diameterb |
|
| 0.529 |
| ≤5
cm | 237 (63.9) | 134 (36.1) |
|
| >5
cm | 56 (63.6) | 32 (36.4) |
|
| Distant
metastasis |
|
| <0.001 |
| M0 | 288 (65.2) | 154 (34.8) |
|
| M1 | 6 (33.3) | 12 (66.7) |
|
| Adjuvant
therapy |
|
| 0.071 |
| LFP
regimen | 60 (71.4) | 24 (28.6) |
|
| Surgery
alone | 234 (66.7) | 142 (33.3) |
|
From the univariate and multivariate Cox regression
analysis, DJ-1 expression was found to be an independent risk
factor for the prognosis of CRC. The univariate Cox regression
analysis revealed that age, pathological classification, depth of
invasion, lymph node metastasis, TNM stage, distant metastasis and
DJ-1 expression were associated with OS in patients with CRC
(Table II). Subsequently,
multivariate Cox regression analysis was used to verify the effect
of DJ-1 expression, and the clinical parameters (sex, pathological
classification, TNM stage and tumor diameter). The results
indicated that DJ-1 expression was an independent and unfavorable
prognostic factor in patients with CRC (HR, 0.301; 95% CI,
0.224–0.405; P<0.001; Table
II).
 | Table II.Univariate and multivariate Cox
regression analysis of DJ-1 expression and clinicopathological
variables predicting survival in CRC patients. |
Table II.
Univariate and multivariate Cox
regression analysis of DJ-1 expression and clinicopathological
variables predicting survival in CRC patients.
|
| N=470 cases |
|---|
|
|
|
|---|
| Variables | HR (95% CI) | P-value |
|---|
| Univariate Cox
regression analysis |
|
|
| Age (≤65 vs. >65
years) | 1.607
(1.215–2.126) | 0.001 |
| Sex (male vs.
female) | 1.013
(0.762–1.347) | 0.927 |
| Pathological
classification (I/II vs. III) | 2.475
(1.587–3.860) | <0.001 |
| Depth of invasion
(T1/T2 vs. T3/T4) | 3.687
(2.270–5.990) | <0.001 |
| Lymph node
metastasis (N0 vs. N1/N2) | 2.807
(2.112–3.731) | <0.001 |
| TNM stage (I/II vs.
III/IV) | 3.214
(2.407–4.291) | <0.001 |
| Distant metastasis
(M0 vs. M1) | 8.150
(4.849–13.699) | <0.001 |
| Tumor diameter (≤5
cm vs. >5 cm) | 1.196
(0.848–1.688) | 0.307 |
| DJ-1 expression
(low vs. high) | 0.255
(0.191–0.340) | <0.001 |
| Multivariate Cox
regression analysisa |
|
|
| Sex (male vs.
female) | 0.914
(0.684–1.222) | 0.544 |
| Pathological
classification (I/II vs. III) | 2.301
(1.420–3.731) | 0.001 |
| TNM stage (I/II vs.
III/IV) | 2.452
(1.810–3.324) | <0.001 |
| Tumor diameter (≤5
cm vs. >5 cm) | 0.978
(0.675–1.415) | 0.904 |
| DJ-1 expression
(low vs. high) | 0.301
(0.224–0.405) | <0.001 |
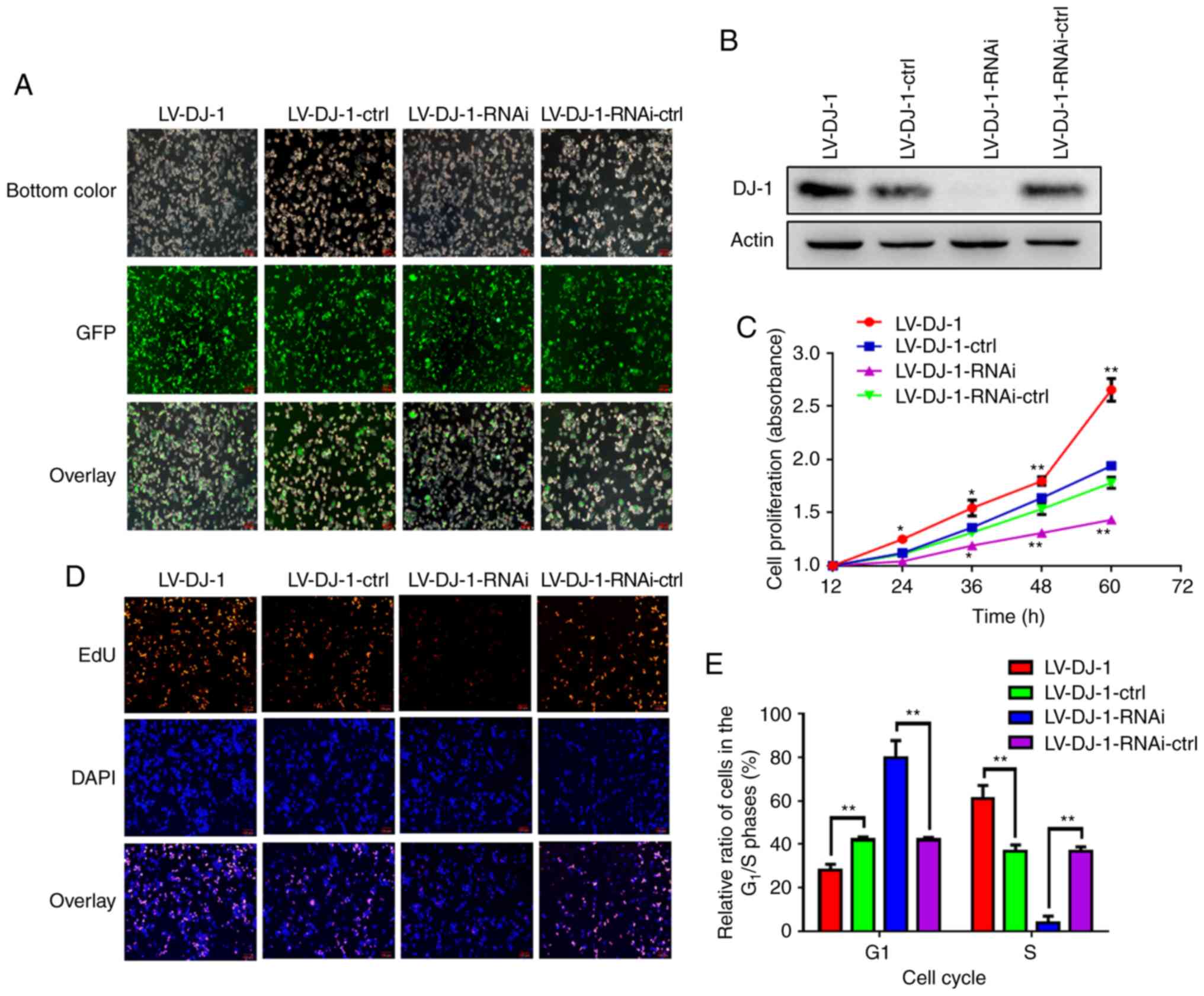
Lentivirus-mediated DJ-1
overexpression and knockdown in CRC cells
HCT116 cells transfected with either LV-DJ-1 or
LV-DJ-1-RNAi exhibited increased or knocked down DJ-1 expression
levels, respectively, compared with that in the respective control
groups. As shown in Fig. 3A, the
transfection efficiency with lentivirus and GFP was high. The
lentivirus-mediated overexpression or knockdown of DJ-1 in HCT116
cells was subsequently analyzed using western blot analysis
(Fig. 3B) and the results were
consistent with fluorescence imaging.
Overexpression and knockdown of DJ-1
enhances and inhibits CRC cell proliferation
From the TMA data analysis, DJ-1 overexpression was
associated with TNM stage in patients with CRC. It is unknown
whether DJ-1 overexpression increases CRC cell growth. To
investigate the biological role of DJ-1 in CRC cell proliferation,
CCK-8 assay was used to observe the proliferation rate in
DJ-1-overexpressing and -knockdown HCT116 cells and the
corresponding control cells (Fig.
3C). Furthermore, the cell proliferation rate was investigated
using EdU immunofluorescence assay (Fig. 3D). The results indicated that the
cell proliferation ability was significantly increased after DJ-1
overexpression and significantly decreased when DJ-1 was knocked
down in the HCT116 cells, when compared with that in the respective
controls. To examine whether DJ-1 promoted CRC cell proliferation
through directly acceleration of the progression of the cell cycle,
cell cycle analysis was performed using PI and flow cytometry. As
shown in Figs. 3E and S1, there was a significantly lower number
of LV-DJ-1 cells in the G1 phase and a significantly
higher number in the S phase, whereas significantly higher and
lower numbers of LV-DJ-1-RNAi cells were observed in the
G1 and S phase, respectively, compared with those of the
corresponding control cells. The results indicate that DJ-1
promotes CRC cell proliferation and growth through regulation of
the cell cycle.
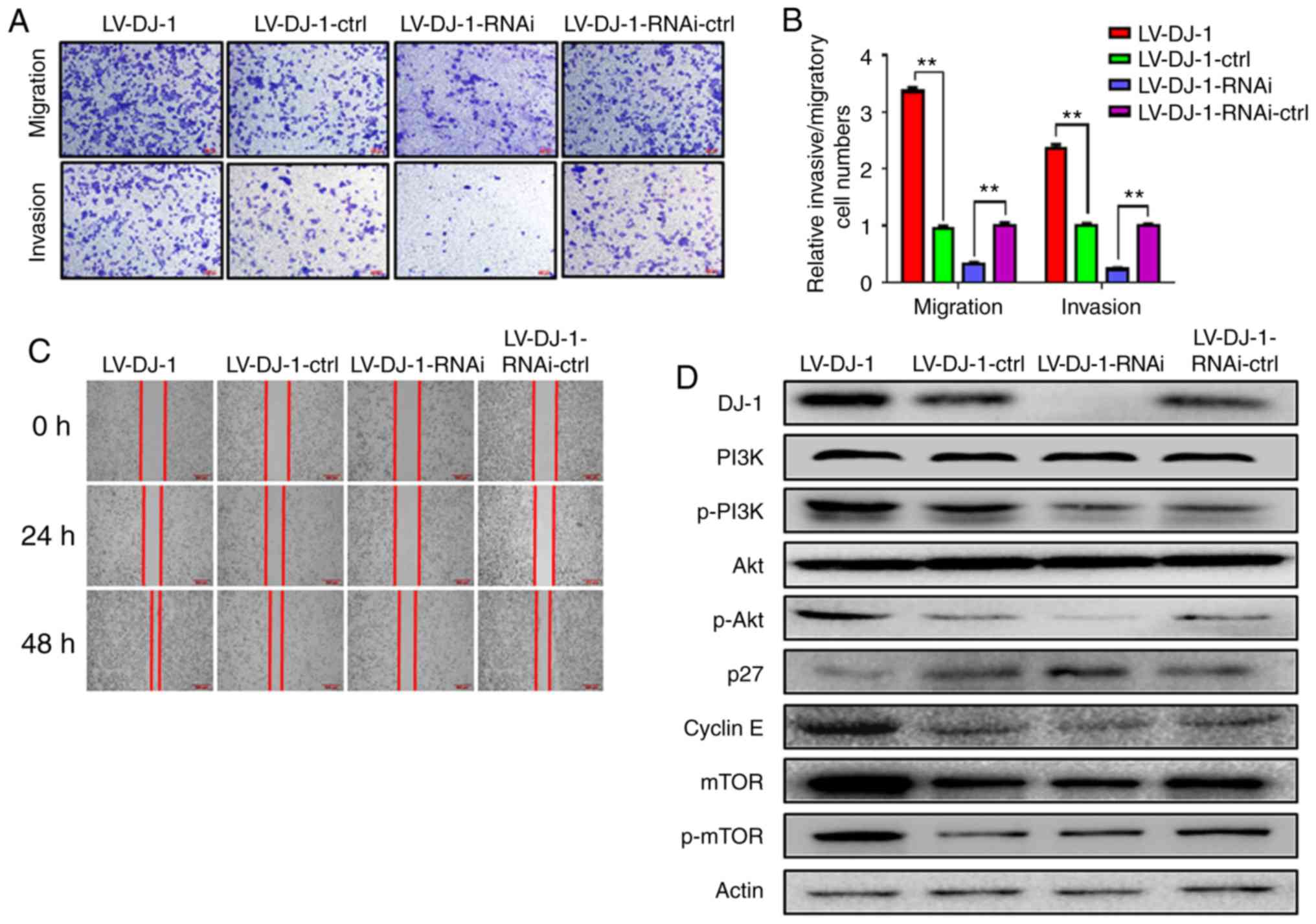
Overexpression and knockdown of DJ-1
promotes and inhibits CRC cell migration and invasion,
respectively
By analyzing the CRC database, DJ-1 expression was
associated with lymph node metastasis in patients with CRC. To
further clarify the role of DJ-1 in the metastasis of CRC, the
migration and invasion abilities of LV-DJ-1, LV-DJ-1-ctrl,
LV-DJ-1-RNAi and LV-DJ-1-RNAi-ctrl cell lines were observed using
Transwell and wound healing, and Matrigel assays respectively. As
shown in Fig. 4A, the results
revealed that the migration and invasion abilities of LV-DJ-1 cells
were increased, whereas the migration and invasion abilities of the
LV-DJ-1-RNAi cells were decreased when compared with that in the
corresponding controls, respectively. The mean number of migrated
and invaded cells in the LV-DJ-1 group was 3.36- and 2.37-fold,
respectively, whereas the number of migrated and invaded cells
decreased by 68.0 and 23.5%, respectively, in the LV-DJ-1-RNAi
cells compared with that in the control group (Fig. 4B; P<0.01). In addition, the wound
healing rate of LV-DJ-1 cells was higher compared with that in
LV-DJ-1-ctrl cells, and the rate of LV-DJ-1-RNAi cells was lower
compared with that in LV-DJ-1-RNAi-ctrl cells (Fig. 4C). These data indicated that DJ-1
promoted CRC cell migration and invasion.
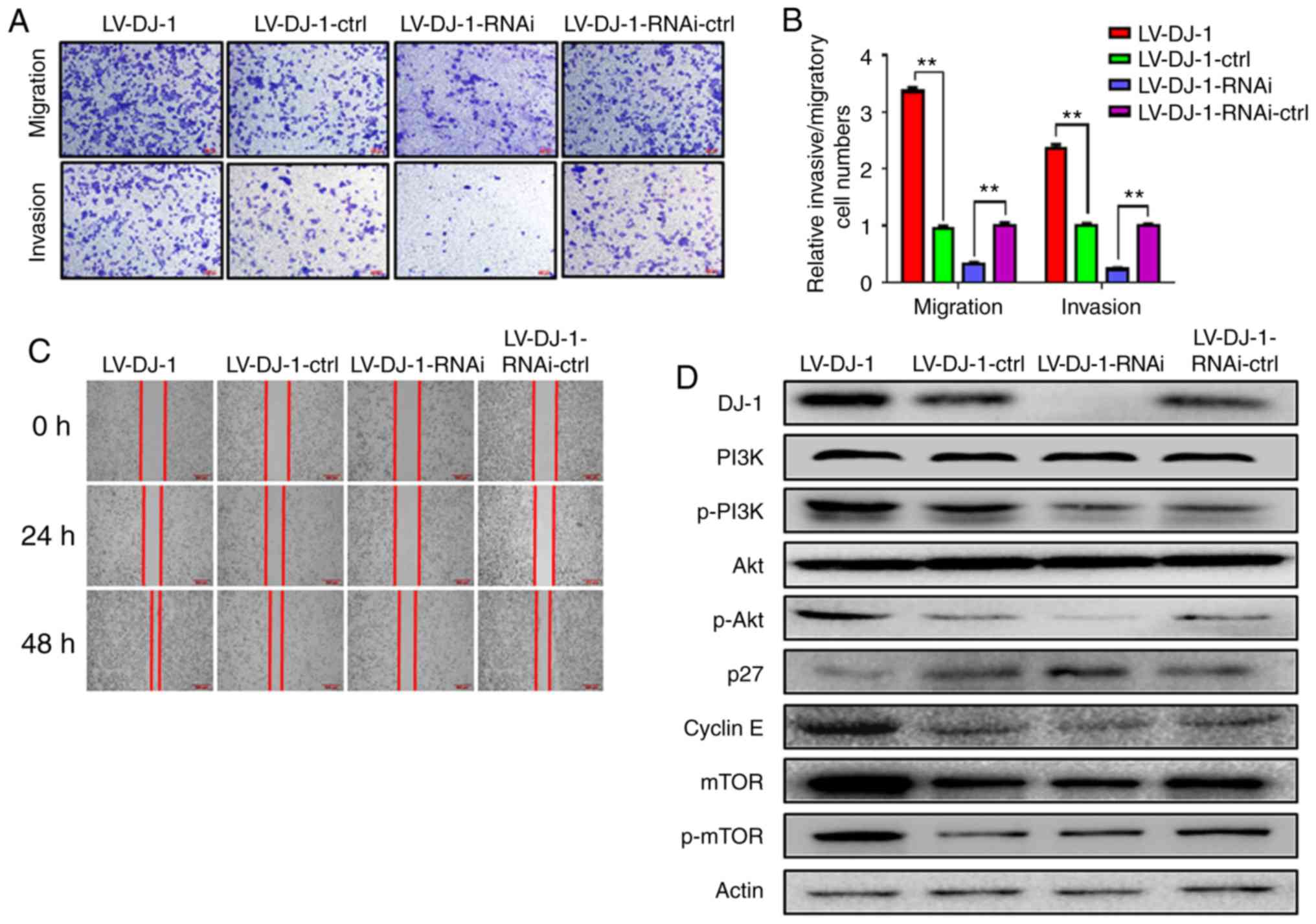 | Figure 4.DJ-1 positively regulates CRC cell
migration and invasion in vitro. (A and B) The cell
migration and invasion results of HCT116 cells with differential
DJ-1 expression levels. Numbers of cell migration and invasion per
field were counted in five random fields for the
DJ-1-overexpressing/knockout and control groups (n=3/group). The
ability of cell migration and invasion was increased after DJ-1
over-expression, whereas the ability of cell migration and invasion
was decreased after DJ-1 knockout (**P<0.01). (C) Wound healing
assay was used to detect the migratory ability of HCT116 cells with
differential DJ-1 expression levels. The wound healing rate of
LV-DJ-1 cells was higher than that of the LV-DJ-1-ctrl cells,
whereas the wound healing rate was lower in the LV-DJ-1-RNAi cells
compared with the control groups. (D and E) The expression of
PI3K/Akt downstream molecules such as p27, cyclin E, mTOR, p-mTOR
was detected by western blot analysis. DJ-1 regulated
PI3K/Akt/p27/cyclin E and PI3K/Akt/ mTOR signaling pathway to
promote CRC cell growth and metastasis. Densitometric analysis is
presented as mean ± SD of 3 separate experiments (**P<0.01). (F
and G) Nuclear transcription factors (NF-κB, Snail), EMT markers
(E-cadherin, N-cadherin, and vimentin) were evaluated by western
blot analysis. Densitometric analysis is presented as mean ± SD of
3 separate experiments (**P<0.01). DJ-1 was able to regulate the
NF-κB/Snail signaling pathway to induce EMT. CRC, colorectal
cancer; EMT, epithelial-mesenchymal transition. The HCT116 cells
were infected with lentivirus (LV)-DJ-1, LV-DJ-1-control (ctrl),
LV-DJ-1-RNA interference (RNAi) and LV-DJ-1-RNAi-ctrl. |
DJ-1 activates the PI3K/Akt signaling
pathway to promote CRC cell proliferation, migration and
invasion
To further explore the molecular mechanism of DJ-1
in promoting proliferation and metastasis in CRC, proliferation-
and metastasis-related proteins were detected using western blot
analysis. DJ-1 positively regulated p-PI3K and p-Akt expression
however, there was no difference in total PI3K and Akt protein
levels. The data indicate that DJ-1 is able to activate the
PI3K/Akt signaling pathway. The expression of PI3K/Akt downstream
molecules, such as p27, cyclin E, mTOR, p-mTOR were also analyzed
and the results revealed that DJ-1 negatively regulated p27 and
cyclin E expression and positively regulated mTOR and p-mTOR
expression (Fig. 4D and E). These
results from the present study suggest that DJ-1 regulates the
PI3K/AKT/p27/cyclin E and PI3K/Akt/mTOR signaling pathways to
promote CRC cell growth and metastasis.
DJ-1 induces CRC cell EMT to promote
migration and invasion
Previous studies have demonstrated that DJ-1 is
upregulated in renal fibrosis and DJ-1 mediates EMT by suppressing
cytoplasmic PTEN expression and Akt activation (25). Epithelial marker (E-cadherin) and
mesenchymal markers (N-cadherin and vimentin) are markers for the
occurrence of EMT. We investigated whether DJ-1 stimulates CRC
cells to induce EMT, which consequently promotes CRC cell invasion
and metastasis. The results from western blot analysis revealed
that protein expression level of E-cadherin was reduced following
DJ-1 overexpression, whereas E-cadherin was upregulated following
knockdown of DJ-1, when compared with the corresponding controls,
respectively. The expression of N-cadherin and vimentin was
inversely associated with DJ-1 expression. The data confirmed that
DJ-1 was able to induce CRC cell EMT to promote migration and
invasion. To investigate the related mechanism further, the effect
of DJ-1 on the NF-κB/Snail signaling pathway was examined (Fig. 4F and G). From these results, we
concluded that DJ-1 could regulate EMT signaling pathway through
NF-κB/Snail.
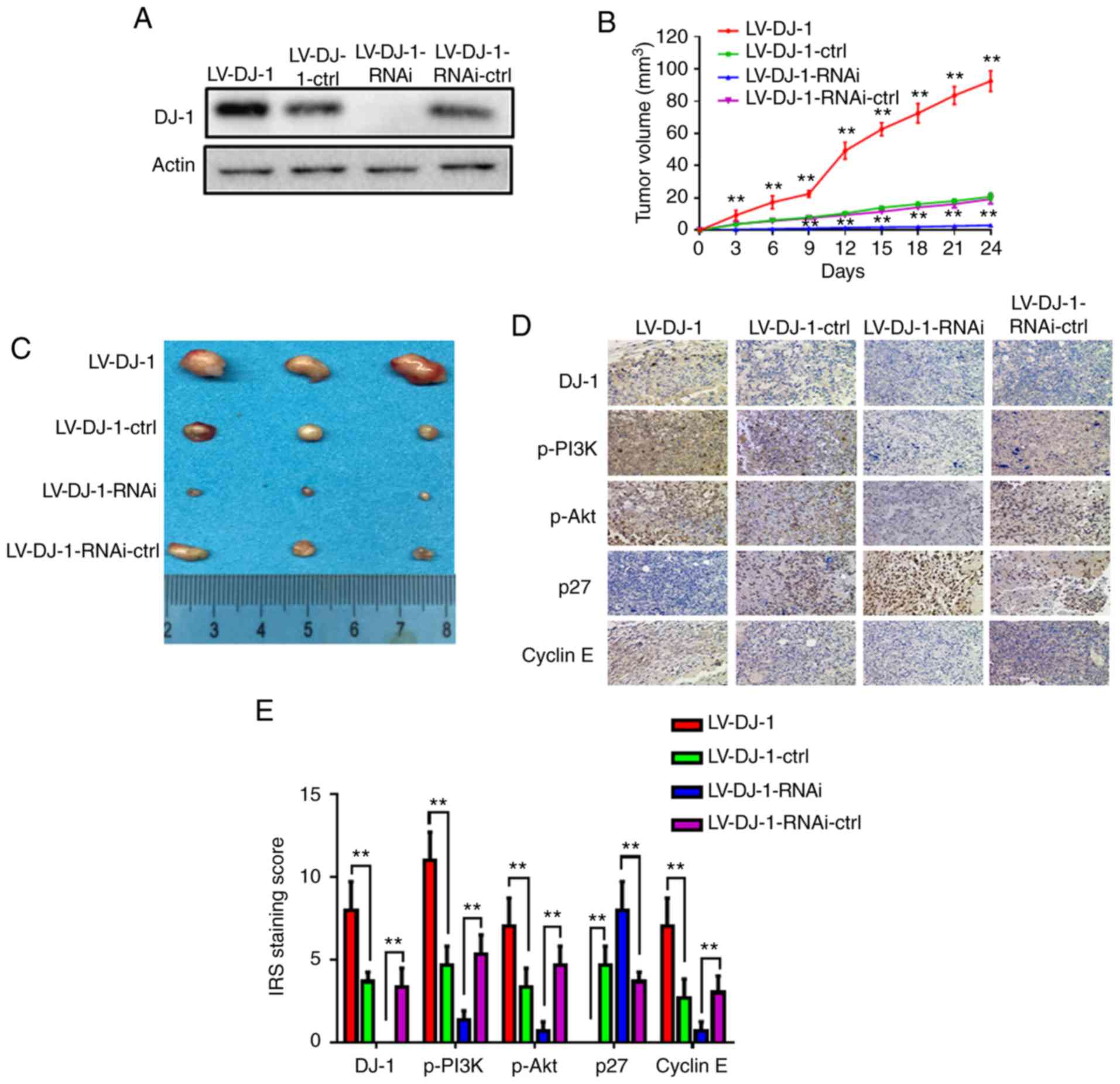
DJ-1 increases CRC cell growth and
induces CRC cell metastasis in vivo
LV-DJ-1, LV-DJ-1-ctrl, LV-DJ-1-RNAi and
LV-DJ-1-RNAi-ctrl cell lines exhibited differential levels of DJ-1
(Fig. 5A). These four groups cells
were injected subcutaneously into nude mice, and tumor growth was
monitored (Fig. 5B). Tumor volume
was increased in the LV-DJ-1 group, whereas it was decreased in
LV-DJ-1-RNAi group when compared with that in the respective
control groups (Fig. 5B and C).
Furthermore, the protein expression levels of DJ-1, p-PI3K, p-Akt,
p27 and cyclin E in the xenograft tumors were determined using IHC.
The results revealed that DJ-1 expression in tumors was higher in
the LV-DJ-1 group and lower in the LV-DJ-1-RNAi group compared with
that in the respective control groups. The DJ-1 expression was
positively associated with the expression of p-PI3K, p-Akt and
cyclin E, whereas it was negatively associated with p27 expression
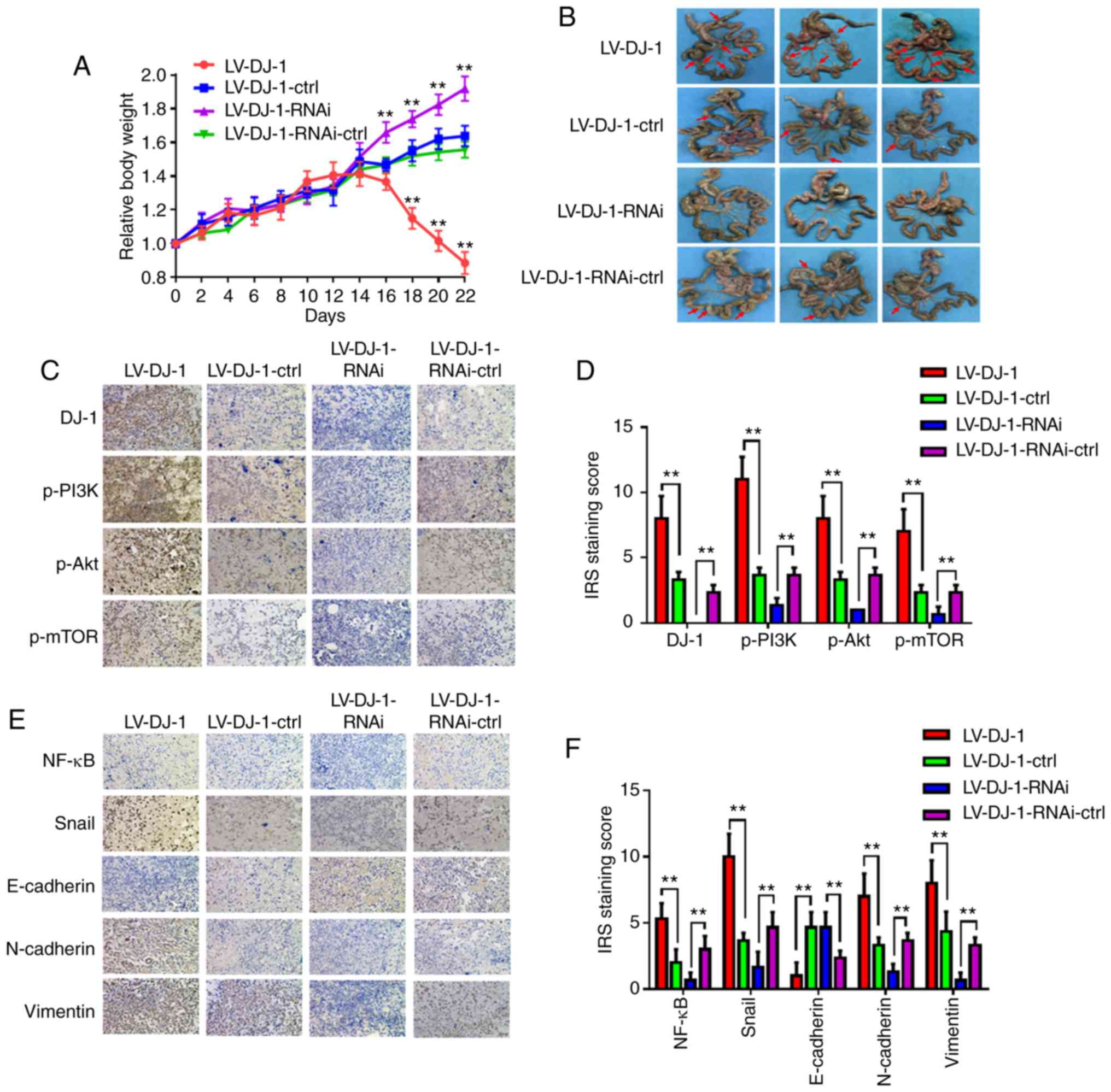
(Fig. 5D and E). In addition, the
aforementioned transfected cells were inoculated into the
peritoneal cavity of BALB/c nude mice. The weight of each mouse was
monitored every 2 days. The relative weight of the mice in the
LV-DJ-1 group was significantly reduced at days 18, 20 and 22
compared with that in the control group, whereas the weight of the
mice in the LV-DJ-1-RNAi group increased at days 16, 18, 20 and 22
compared with that in the control group (Fig. 6A). These mice were sacrificed by
cervical dislocation on day 22, and the number of metastatic
nodules was higher and lower in the LV-DJ-1 and LV-DJ-1-RNAi group,
respectively, compared with that in the corresponding control group
(Fig. 6B). Subsequently, the
protein expression of DJ-1, p-PI3K, p-Akt and p-mTOR in the
metastatic nodules of the peritoneum was determined using IHC. The
results indicated that DJ-1 expression was positively associated
with the expression levels of p-PI3K, p-Akt and p-mTOR (Fig. 6C and D). Furthermore, the expression
levels of EMT-related proteins (NF-κB, Snail, E-cadherin,
N-cadherin and vimentin) were also determined in intraperitoneal
metastasis. The expression levels of NF-κB, Snail, N-cadherin and
vimentin were positively regulated by the expression of DJ-1,
whereas E-cadherin was negatively associated with DJ-1 expression
(Fig. 6E and F). The data from the
present study revealed that DJ-1 was also capable of promoting CRC
cell growth and metastasis in vivo, which is consistent with
the results from CRC cell proliferation and invasion in
vitro.
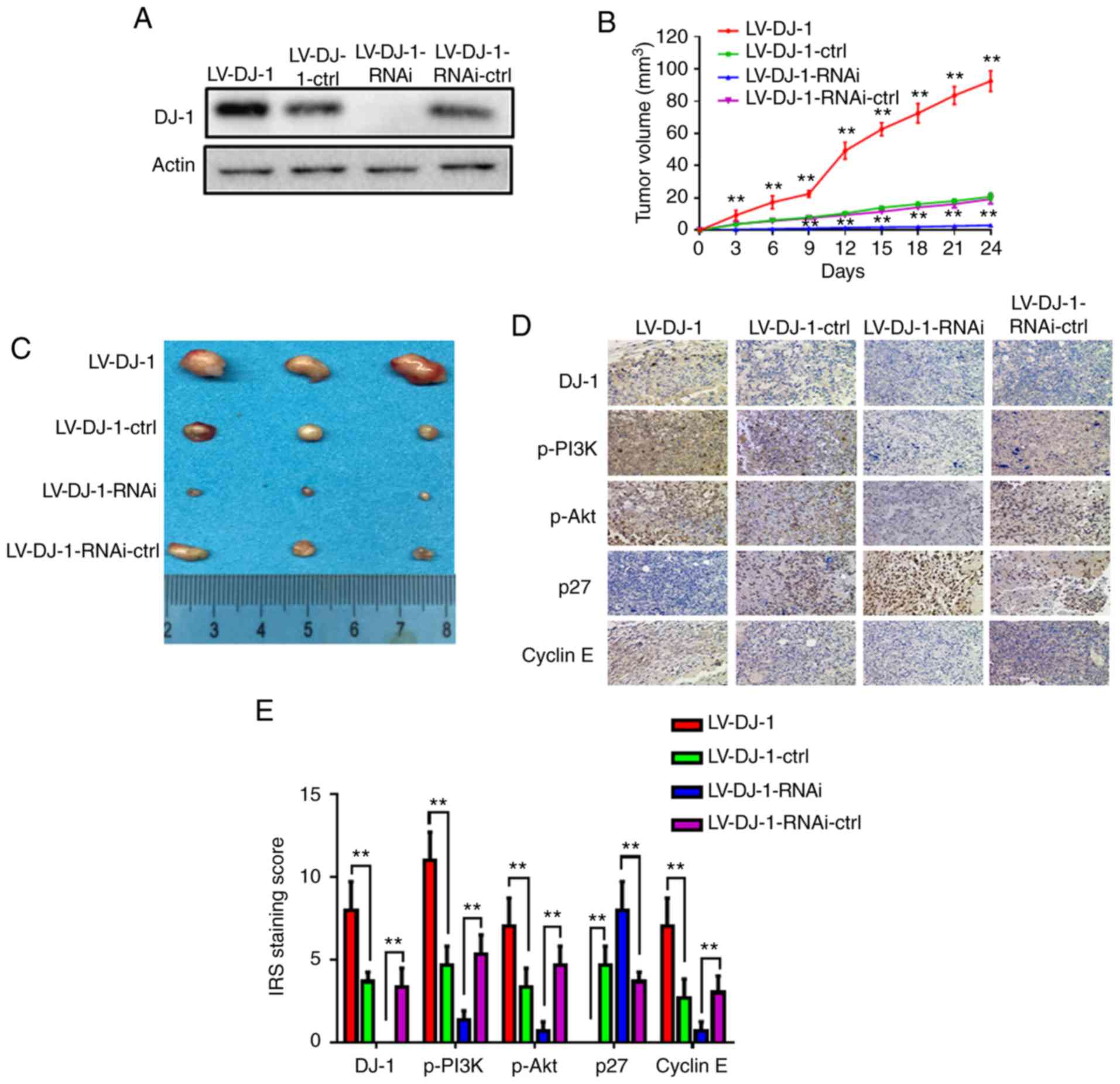 | Figure 5.DJ-1 induces CRC cell growth in
vivo. (A) Western blot analysis was used to validate the
expression of DJ-1. LV-DJ-1, LV-DJ-1-ctrl, LV-DJ-1-RNAi and
LV-DJ-1-RNAi-ctrl cell lines were generated. (B) The tumor volume
was calculated in the 4 groups every 3 days. The tumor volume was
significantly larger in the LV-DJ-1 group, and smaller in the
LV-DJ-1-RNAi group compared with the control group, respectively
(**P<0.01). (C) Images of the xenograft tumors in the stable
DJ-1-over-expression or knockout and the corresponding vector
control group. (D) The expression levels of DJ-1, p-PI3K, p-Akt,
p27, cyclin E in the xenograft tumors were tested by IHC. (E) The
IRS staining scores of DJ-1, p-PI3K, p-Akt, p27, cyclin E in the
xenograft tumors were evaluated (n=3). Data are presented as mean ±
SD (**P<0.01). CRC, colorectal cancer; IHC,
immunohistochemistry; IRS, immunoreactivity score. |
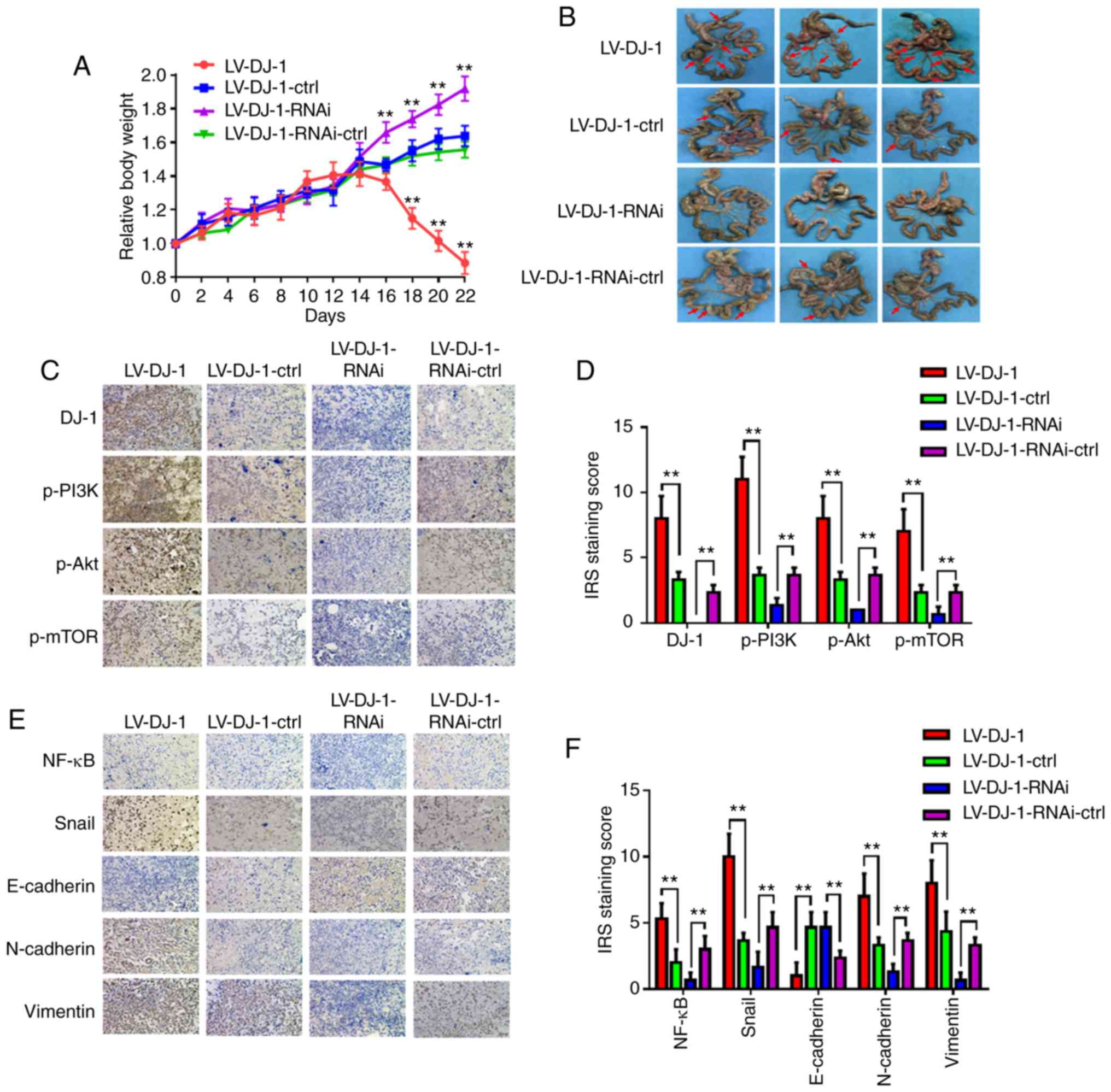 | Figure 6.DJ-1 promotes cell metastasis of CRC
cells in vivo. (A) The body weight of mice in the four
groups were monitored every 2 days. After 2 weeks, the mouse
weights in the LV-DJ-1 group were lower than that in the
LV-DJ-1-ctrl group; whereas in the LV-DJ-1-RNAi group, the opposite
phenomenon was observed. (B) Representative images of the
metastatic nodules of the peritoneal cavity in the four groups.
Overexpression of DJ-1 was found to promote the metastasis of CRC
cells. In the LV-DJ-1-RNAi group, metastasis of the CRC cells was
reduced much more than in the control group. (C) Expression of
DJ-1, p-PI3K, p-Akt and p-mTOR in the metastatic nodules was
assessed by IHC. (D) IRS staining scores of DJ-1, p-PI3K, p-Akt,
p-mTOR were evaluated (n=3). Data are presented as mean ± SD
(**P<0.01). (E) Protein expression of NF-κB, Snail, E-cadherin,
N-cadherin, and vimentin in the metastatic nodules was assessed by
IHC. (F) IRS staining scores of NF-κB, Snail, E-cadherin,
N-cadherin, and vimentin were evaluated (n=3). Data are presented
as mean ± SD (**P<0.01). The HCT116 cells used in the mouse
model were infected with lentivirus (LV)-DJ-1, LV-DJ-1-control
(ctrl), LV-DJ-1-RNA interference (RNAi) and LV-DJ-1-RNAi-ctrl. CRC,
colorectal cancer; IHC, immunohistochemistry. |
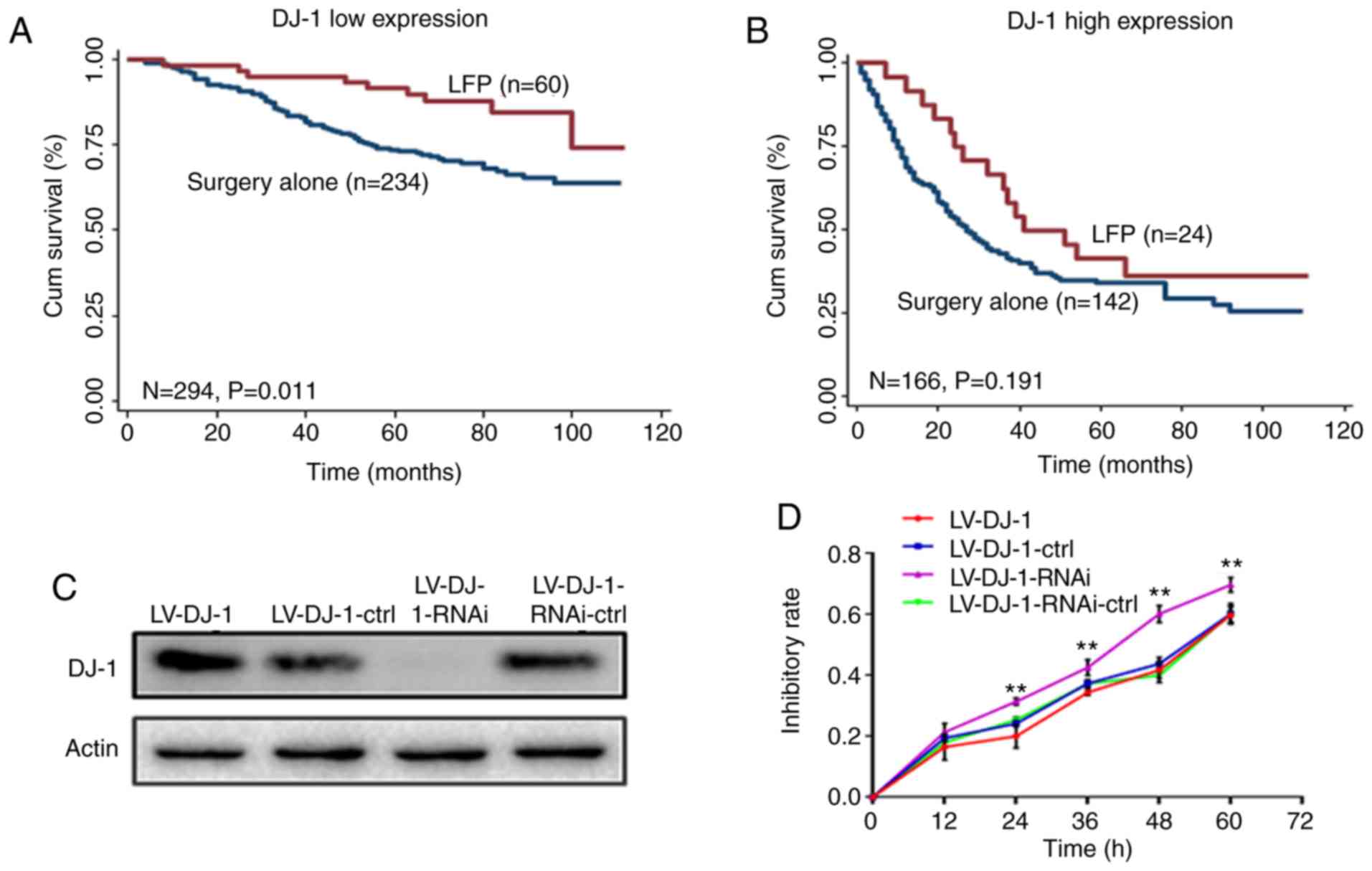
Patients with low DJ-1 expression
levels are more sensitive to adjuvant chemotherapy
In the CRC database, the postoperative chemotherapy
of each patient with CRC was recorded in detail. According to the
National Comprehensive Cancer Network guidelines at that time, the
recommended first-line postoperative adjuvant chemotherapy for
patients with CRC is the LFP regimen, which includes oxaliplatin,
5-FU and tetrahydrofolate (26).
Subsequently, the correlation between DJ-1 expression and the
therapeutic effect of chemotherapy was investigated. Kaplan-Meier
curve analysis revealed that patients who received LFP treatment
and had low DJ-l expression levels in tumor tissues had a
significantly longer survival time compared with that in patients
who received surgery alone (Fig.
7A; P=0.011). However, patients with high DJ-1 expression level
did not benefit from LFP treatment (Fig. 7B; P=0.191). Multivariate Cox
proportional hazard regression analysis, including 6 variables
(age, sex, TNM stage, pathological classification, tumor diameter
and adjuvant chemotherapy) was used to evaluate the benefit of
chemotherapy on OS. Notably, LFP treatment increased OS compared
with that with surgery alone in patients with low DJ-1 expression
levels (HR, 0.410; 95% CI, 0.200–0.837; P=0.014; Table III). However, this effect was not
observed in patients with high DJ-1 expression levels (HR, 0.634;
95% CI, 0.355–1.32; P=0.124; Table
III).
 | Table III.Multivariate Cox model analysis of
the effect of LFP therapy on OS of CRC patients with low/high DJ-1
expression. |
Table III.
Multivariate Cox model analysis of
the effect of LFP therapy on OS of CRC patients with low/high DJ-1
expression.
|
| DJ-1 low
expression | DJ-1 high
expression |
|---|
|
|
|
|
|---|
|
| HR (95% CI) | β |
P-valuea | HR (95% CI) | β |
P-valuea |
|---|
| Age (≤65 vs. >65
years) | 1.670
(1.072–2.604) | 2.27 | 0.023 | 1.552
(1.040–2.317) | 2.15 | 0.031 |
| Sex (male vs.
female) | 0.734
(0.464–1.161) | −1.32 | 0.186 | 1.056
(0.723–1.542) | 0.28 | 0.779 |
| Pathological
classification (I/II vs. III) | 1.037
(0.440–2.447) | 0.08 | 0.934 | 3.645
(1.948–6.819) | 4.05 | 0.001 |
| TNM stage (I/II vs.
III/IV) | 2.390
(1.536–3.718) | 3.86 | 0.001 | 3.260
(2.061–5.157) | 5.05 | 0.001 |
| Tumor diameter (≤5
cm vs. >5 cm) | 1.306
(0.763–2.236) | 0.97 | 0.331 | 0.853
(0.502–1.451) | −0.59 | 0.558 |
| Adjuvant therapy
(LFP vs. surgery alone) | 0.410
(0.200–0.837) | −2.45 | 0.014 | 0.634
(0.355–1.132) | −1.54 | 0.124 |
In addition, the association between DJ-1 expression
and chemosensitivity was investigated in vitro. A drug which
contains 5-FU (25 µg/ml) and L-OHP (20 µg/ml) was used to act on
LV-DJ-1, LV-DJ-1-ctrl, LV-DJ-1-RNAi and LV-DJ-1-RNAi-ctrl cell
lines. As in Fig. 7C, DJ-1
expression in these four groups was again verified by Western blot
analysis. The inhibition rate was determined using CCK-8 assay. The
results indicate that the inhibition rate in the LV-DJ-1-RNAi group
was significantly higher when compared with that in
LV-DJ-1-RNAi-ctrl group (P<0.01; Fig. 7D); however, the inhibition rate in
the LV-DJ-1 group was not statistically significant compared with
that in the control group (P>0.05; Fig. 7D). These results suggest that DJ-1
expression may predict the effect of LFP chemotherapy in patients
with CRC.
Discussion
The pathogenesis of colorectal cancer (CRC) is a
complex process, which is associated with the abnormal expression
of oncogenes and tumor-suppressor genes (27). In the progression of CRC, novel
molecular markers may be valuable as early diagnostic markers or
indicators of treatment efficacy (28). Our previous research revealed that
molecular markers can predict metastasis and prognosis in patients
with CRC (29,30). In the present study, protein/nucleic
acid deglycase DJ-1 (DJ-1) expression was found to be significantly
different between CRC and FHC cell lines, and between CRC tissues
and normal adjacent tissues. Furthermore, subsequent experiments
were performed to fully elucidate the underlying mechanisms and
clinical significance of DJ-1 in CRC.
DJ-1 is associated with the development of cancer.
Previous studies have revealed that DJ-1 promoted the invasion and
metastasis in numerous types of tumors, including liver cancer
(31), laryngeal carcinoma
(32), lung cancer (33), and breast cancer (33). The mechanism involved may be
associated with PI3K/Akt, SRC/ERK/uPA and other signaling pathways
(12,25,34).
Additionally, DJ-1 could induce apoptosis and promote cell EMT
(25,35). In the present study, patients with
CRC and high DJ-1 expression levels had a poorer disease-free
survival, and multivariate Cox proportional hazards regression
analysis revealed that DJ-1 expression was an independent negative
prognostic factor following adjustment by sex, pathological
classification, TNM stage and tumor diameter in CRC database
analysis.
To validate these results, LV-DJ-1, LV-DJ-1-ctrl,
LV-DJ-1-RNAi and LV-DJ-1-RNAi-ctrl cell lines were constructed to
investigate the biological function of DJ-1 in CRC. In
vitro, cell proliferation was significantly increased in
LV-DJ-1 and decreased in LV-DJ-1-RNAi cells when compared with that
in the respective controls. Moreover, the migration and invasion
abilities of the LV-DJ-1 cells were increased, whereas these
abilities were decreased in the LV-DJ-1-RNAi cells when compared
with those in the corresponding controls. Previous research
mechanisms have been clarified that DJ-1 could promote CRC cell
growth or metastasis through the PTEN-AKT, PLAGL2/Wnt/BMP4 pathways
(13,14). Subsequently, the related mechanisms
involved were investigated in the present study. The results
indicated that increased DJ-1 expression induced cell proliferation
by regulating PI3K/Akt/p27/cyclin E signaling, and promoted cell
invasion and metastasis by regulating PI3K/Akt/mTOR signaling or
induced EMT in vitro. In addition, two models of
subcutaneous implantation and peritoneal metastases were
constructed to investigate the role of DJ-1 in tumorigenesis. The
growth of tumors was observed and the regulation between DJ-1 and
p-PI3K, p-Akt, p27 and cyclin E protein expression in xenograft
tumor tissues was validated using IHC. In addition, the expression
levels of DJ-1, p-PI3K, p-Akt, p-mTOR, NF-κB, Snail, E-cadherin,
N-cadherin and vimentin were also analyzed in peritoneal metastasis
tumor tissues. The analysis of these results indicates that DJ-1
promotes CRC cell growth and metastasis in vivo, which is
consistent with the results from CRC cell proliferation and
invasion in vitro.
Notably, the CRC database, which contains samples
from 470 patients, was used to investigate the association between
DJ expression and postoperative adjuvant chemotherapy. In the CRC
database, 86 patients with CRC were treated with LFP chemotherapy.
Using the Kaplan-Meier curve method and multivariate Cox
proportional hazard regression, LFP treatment increased the overall
survival (OS) compared with that in patients who underwent surgery
alone and with low DJ-1 expression levels, whereas a lower OS was
found in patients with high DJ-1 expression levels. To confirm this
conclusion, the drugs 5-FU and L-OHP were used to act on LV-DJ-1,
LV-DJ-1-ctrl, LV-DJ-1-RNAi and LV-DJ-1-RNAi-ctrl cell lines. The
results indicate that the inhibition rate of the LV-DJ-1-RNAi group
was higher compared with that in the LV-DJ-1-RNAi-ctrl group, but
not in the LV-DJ-1 group.
In conclusion, DJ-1 was the most unfavorable
prognostic factor for patients with CRC. High DJ-1 expression
levels are positively associated with poorer survival in patients
with CRC. The investigations into the molecular mechanisms revealed
that DJ-1 increased cell proliferation by regulating the
PI3K/Akt/p27/cyclin E signaling pathway and induced CRC metastasis
via regulating the PI3K/Akt/mTOR signaling pathway or by inducing
EMT in vitro and in vivo. DJ-1 may play a role as an
oncogene in CRC tumorigenesis and may be involved in the
progression of CRC. Therefore, DJ-1 appears to be a significant
prognostic indicator for patients with CRC and an effective marker
for predicting the efficacy of chemotherapy. However, the results
from the present study require validation in larger retrospective
and prospective CRC cohorts.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant no. 81773944), the Young
Medicine Focus Talent Foundation of Jiangsu Province (grant no.
QNRC2016206), the Postgraduate Research by Practice Innovation
Program of Jiangsu Province (grant nos. KYCX18_2382 and
KYCX17_1892), the Wuxi City Health Planning Commission project
(grant no. MS201815), and the Natural Science Foundation of Jiangsu
Province of China (grant no. BK20191149).
Availability of data and materials
The datasets used during the present study are
available from the corresponding author upon reasonable
request.
Authors' contributions
YuZ and YL conceived and coordinated the project.
WW, HW, LX, TN and FJ performed experiments and collected the data.
WW and LX performed overall data interpretation. JD, YaZ, and IS
interpreted the data and critically reviewed the manuscript. WW
wrote the manuscript. All authors read and approved the manuscript
and agree to be accountable for all aspects of the research in
ensuring that the accuracy or integrity of any part of the work are
appropriately investigated and resolved.
Ethics approval and consent to
participate
The present study was granted ethics approval by the
Institutional Review Board of Yixing Hospital Affiliated to Medical
College of Yangzhou University (Yixing, Jiangsu). All patients
provided written informed consent and all acquired data were
assured of anonymity and confidentiality. All experimental animal
procedures were performed in compliance with the institutional
ethics requirements and approved by the Institutional Animal Care
and Use Committee of Yangzhou University.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kang D, Park JM, Jung CK, Lee BI, Oh ST
and Choi MG: Prognostic impact of membranous ATP-binding cassette
Sub-family G member 2 expression in patients with colorectal
carcinoma after surgical resection. Cancer Biol Ther. 16:1438–1444.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tsikitis VL, Larson DW, Huebner M, Lohse
CM and Thompson PA: Predictors of recurrence free survival for
patients with stage II and III colon cancer. BMC Cancer.
14:3362014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zuo J, Ishikawa T, Boutros S, Xiao Z,
Humtsoe JO and Kramer RH: Bcl-2 overexpression induces a partial
epithelial to mesenchymal transition and promotes squamous
carcinoma cell invasion and metastasis. Mol Cancer Res. 8:170–182.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Erstad DJ, Tumusiime G and Cusack JC Jr:
Prognostic and predictive biomarkers in colorectal cancer:
Implications for the clinical surgeon. Ann Surg Oncol.
22:3433–3450. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bonifati V, Rizzu P, Squitieri F, Krieger
E, Vanacore N, van Swieten JC, Brice A, van Duijn CM, Oostra B,
Meco G and Heutink P: DJ-1( PARK7), a novel gene for autosomal
recessive, early onset parkinsonism. Neurol Sci. 24:159–160. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhang HJ, Siu MK, Jiang LL, Mak VC, Ngan
HY and Cheung AN: Overexpression of the Parkinson disease protein
DJ-1 and its regulator PTEN in gestational trophoblastic disease.
Int J Gynecol Pathol. 29:468–475. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bai J, Guo C, Sun W, Li M, Meng X, Yu Y,
Jin Y, Tong D, Geng J, Huang Q, et al: DJ-1 may contribute to
metastasis of non-small cell lung cancer. Mol Biol Rep.
39:2697–2703. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chen Y, Kang M, Lu W, Guo Q, Zhang B, Xie
Q and Wu Y: DJ-1, a novel biomarker and a selected target gene for
overcoming chemoresistance in pancreatic cancer. J Cancer Res Clin
Oncol. 138:1463–1474. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Liu HY, Duan GL, Xu RY, Li XR, Xiao L,
Zhao L, Ma ZX, Xu XW, Qiu LJ, Zhu ZM and Chen HP: DJ-1
overexpression confers the multidrug resistance phenotype to
SGC7901 cells by upregulating P-gp and Bcl-2. Biochem Biophys Res
Commun. 519:73–80. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Aleyasin H, Rousseaux MW, Marcogliese PC,
Hewitt SJ, Irrcher I, Joselin AP, Parsanejad M, Kim RH, Rizzu P,
Callaghan SM, et al: DJ-1 protects the nigrostriatal axis from the
neurotoxin MPTP by modulation of the AKT pathway. Proc Natl Acad
Sci USA. 107:3186–3191. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
He X, Zheng Z, Li J, Ben Q, Liu J, Zhang
J, Ji J, Yu B, Chen X, Su L, et al: DJ-1 promotes invasion and
metastasis of pancreatic cancer cells by activating SRC/ERK/uPA.
Carcinogenesis. 33:555–562. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lin Y, Chen Q, Liu QX, Zhou D, Lu X, Deng
XF, Yang H, Zheng H and Qiu Y: High expression of DJ-1 promotes
growth and invasion via the PTEN-AKT pathway and predicts a poor
prognosis in colorectal cancer. Cancer Med. 7:809–819. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhou J, Liu H, Zhang L, Liu X, Zhang C,
Wang Y, He Q, Zhang Y, Li Y, Chen Q, et al: DJ-1 promotes
colorectal cancer progression through activating PLAGL2/Wnt/BMP4
axis. Cell Death Dis. 9:8652018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zheng H, Zhou C, Lu X, Liu Q, Liu M, Chen
G, Chen W, Wang S and Qiu Y: DJ-1 promotes survival of human colon
cancer cells under hypoxia by modulating HIF-1α expression through
the PI3K-AKT pathway. Cancer Manag Res. 10:4615–4629. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Pardo M, García A, Thomas B, Piñeiro A,
Akoulitchev A, Dwek RA and Zitzmann N: The characterization of the
invasion phenotype of uveal melanoma tumour cells shows the
presence of MUC18 and HMG-1 metastasis markers and leads to the
identification of DJ-1 as a potential serum biomarker. Int J
Cancer. 119:1014–1022. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kawate T, Iwaya K, Koshikawa K, Moriya T,
Yamasaki T, Hasegawa S, Kaise H, Fujita T, Matsuo H, Nakamura T, et
al: High levels of DJ-1 protein and isoelectric point 6.3 isoform
in sera of breast cancer patients. Cancer Sci. 106:938–943. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Haapasalo J, Nordfors K, Granberg KJ,
Kivioja T, Nykter M, Haapasalo H and Soini Y: NRF2, DJ1 and SNRX1
and their prognostic impact in astrocytic gliomas. Histol
Histopathol. 33:791–801. 2018.PubMed/NCBI
|
|
19
|
Benati M, Montagnana M, Danese E, Paviati
E, Giudici S, Ruzzenente O, Franchi M and Lippi G: The clinical
significance of DJ-1 and HE4 in patients with endometrial cancer. J
Clin Lab Anal. 32:e222232018. View Article : Google Scholar
|
|
20
|
Wang S, Wu X, Zhang J, Chen Y, Xu J, Xia
X, He S, Qiang F, Li A, Shu Y, et al: CHIP functions as a novel
suppressor of tumour angiogenesis with prognostic significance in
human gastric cancer. Gut. 62:496–508. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bai J, Zhou Y, Chen G, Zeng J, Ding J, Tan
Y, Zhou J and Li G: Overexpression of Cullin1 is associated with
poor prognosis of patients with gastric cancer. Hum Pathol.
42:375–383. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wang W, Chen Y, Deng J, Zhou J, Gu X, Tang
Y, Zhang G, Tan Y, Ge Z, Huang Y, et al: Cullin1 is a novel
prognostic marker and regulates the cell proliferation and
metastasis in colorectal cancer. J Cancer Res Clin Oncol.
141:1603–1612. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wang S, Wu X, Chen Y, Zhang J, Ding J,
Zhou Y, He S, Tan Y, Qiang F, Bai J, et al: Prognostic and
predictive role of JWA and XRCC1 expressions in gastric cancer.
Clin Cancer Res. 18:2987–2996. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Yao Y, Wei H, Liu L, Liu L, Bai S, Li C,
Luo Y, Zeng R, Han M, Ge S and Xu G: Upregulated DJ-1 promotes
renal tubular EMT by suppressing cytoplasmic PTEN expression and
Akt activation. J Huazhong Univ Sci Technolog Med Sci. 31:4692011.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Benson AB, Venook AP, Al-Hawary MM,
Cederquist L, Chen YJ, Ciombor KK, Cohen S, Cooper HS, Deming D,
Engstrom PF, et al: NCCN Guidelines Insights: Colon Cancer, Version
2.2018. J Natl Compr Canc Netw. 16:359–369. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Papachristou DJ, Korpetinou A,
Giannopoulou E, Antonacopoulou AG, Papadaki H, Grivas P, Scopa CD
and Kalofonos HP: Expression of the ribonucleases Drosha, Dicer,
and Ago2 in colorectal carcinomas. Virchows Arch. 459:431–440.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Oldenhuis CN, Oosting SF, Gietema JA and
de Vries EG: Prognostic versus predictive value of biomarkers in
oncology. Eur J Cancer. 44:946–953. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Deng J, Chen W, Du Y, Wang W, Zhang G,
Tang Y, Qian Z, Xu P, Cao Z and Zhou Y: Synergistic efficacy of
Cullin1 and MMP-2 expressions in diagnosis and prognosis of
colorectal cancer. Cancer Biomark. 19:57–64. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wang W, Deng J, Wang Q, Yao Q, Chen W, Tan
Y, Ge Z, Zhou J and Zhou Y: Synergistic role of Cul1 and c-Myc:
Prognostic and predictive biomarkers in colorectal cancer. Oncol
Rep. 38:245–252. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Liu S, Yang Z, Wei H, Shen W, Liu J, Yin
Q, Li X and Yi J: Increased DJ-1 and its prognostic significance in
hepatocellular carcinoma. Hepatogastroenterology. 57:1247–1256.
2010.PubMed/NCBI
|
|
32
|
Shen Z, Ren Y, Ye D, Guo J, Kang C and
Ding H: Significance and relationship between DJ-1 gene and
surviving gene expression in laryngeal carcinoma. Eur J Histochem.
55:e92011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kim RH, Peters M, Jang Y, Shi W, Pintilie
M, Fletcher GC, DeLuca C, Liepa J, Zhou L, Snow B, et al: DJ-1, a
novel regulator of the tumor suppressor PTEN. Cancer Cell.
7:263–273. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Vasseur S, Afzal S, Tardivel-Lacombe J,
Park DS, Iovanna JL and Mak TW: DJ-1/PARK7 is an important mediator
of hypoxia-induced cellular responses. Proc Natl Acad Sci USA.
106:1111–1116. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Vasseur S, Afzal S, Tomasini R,
Guillaumond F, Tardivel-Lacombe J, Mak TW and Iovanna JL:
Consequences of DJ-1 upregulation following p53 loss and cell
transformation. Oncogene. 31:664–670. 2012. View Article : Google Scholar : PubMed/NCBI
|