|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2019. CA Cancer J Clin. 69:7–34. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Villanueva A: Hepatocellular carcinoma. N
Engl J Med. 380:1450–1462. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kulik L and El-Serag HB: Epidemiology and
management of hepatocellular carcinoma. Gastroenterology.
56:477–491. 2019. View Article : Google Scholar
|
|
4
|
Miller KD, Nogueira L, Mariotto AB,
Rowland JH, Yabroff KR, Alfano CM, Jemal A, Kramer JL and Siegel
RL: Cancer treatment and survivorship statistics, 2019. CA Cancer J
Clin. 69:363–385. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Roayaie S, Jibara G, Tabrizian P, Park JW,
Yang J, Yan L, Schwartz M, Han G, Izzo F, Chen M, et al: The role
of hepatic resection in the treatment of hepatocellular cancer.
Hepatology. 62:440–451. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tabrizian P, Jibara G, Shrager B, Schwartz
M and Roayaie S: Recurrence of hepatocellular cancer after
resection: Patterns, treatments, and prognosis. Ann Surg.
261:947–955. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
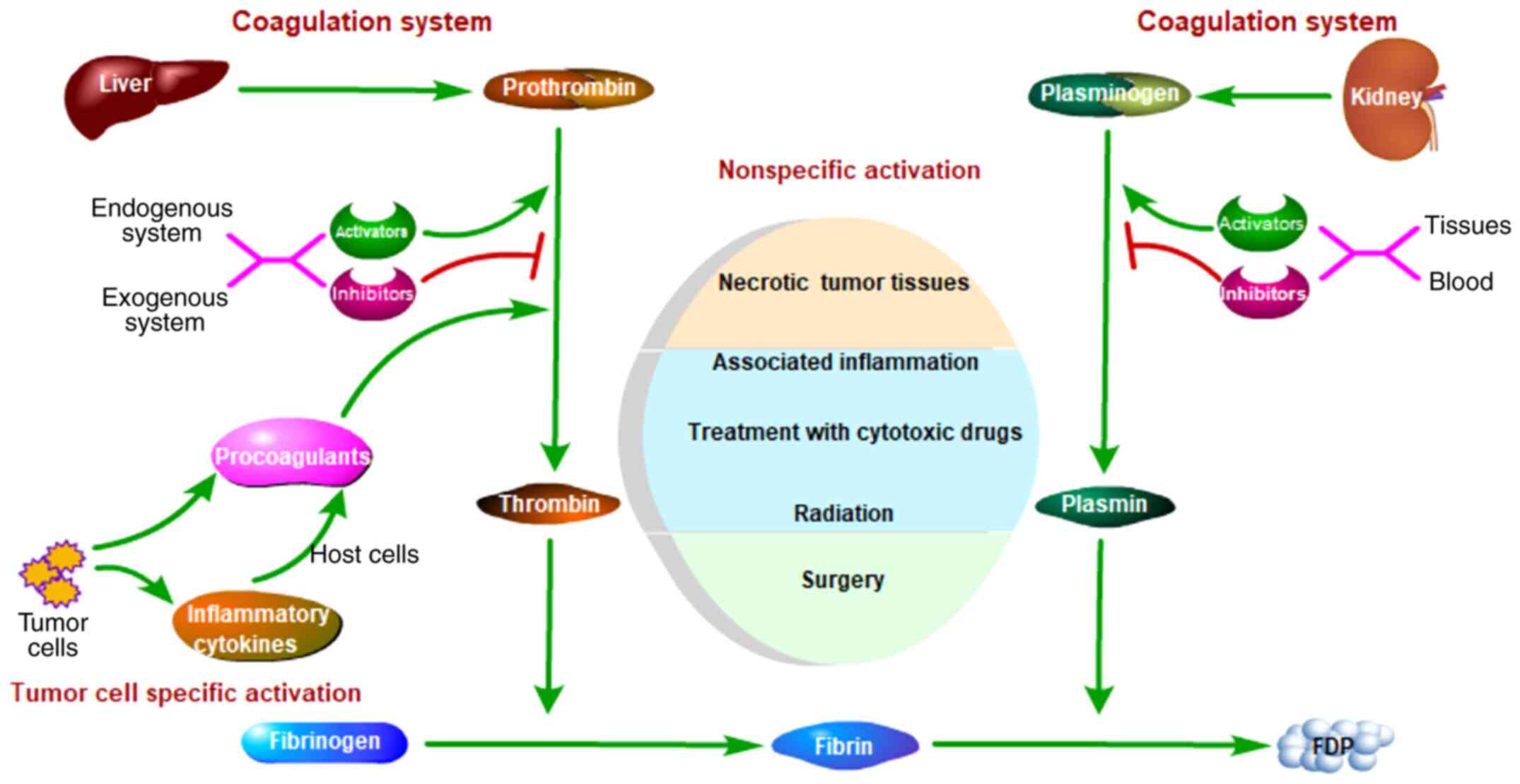
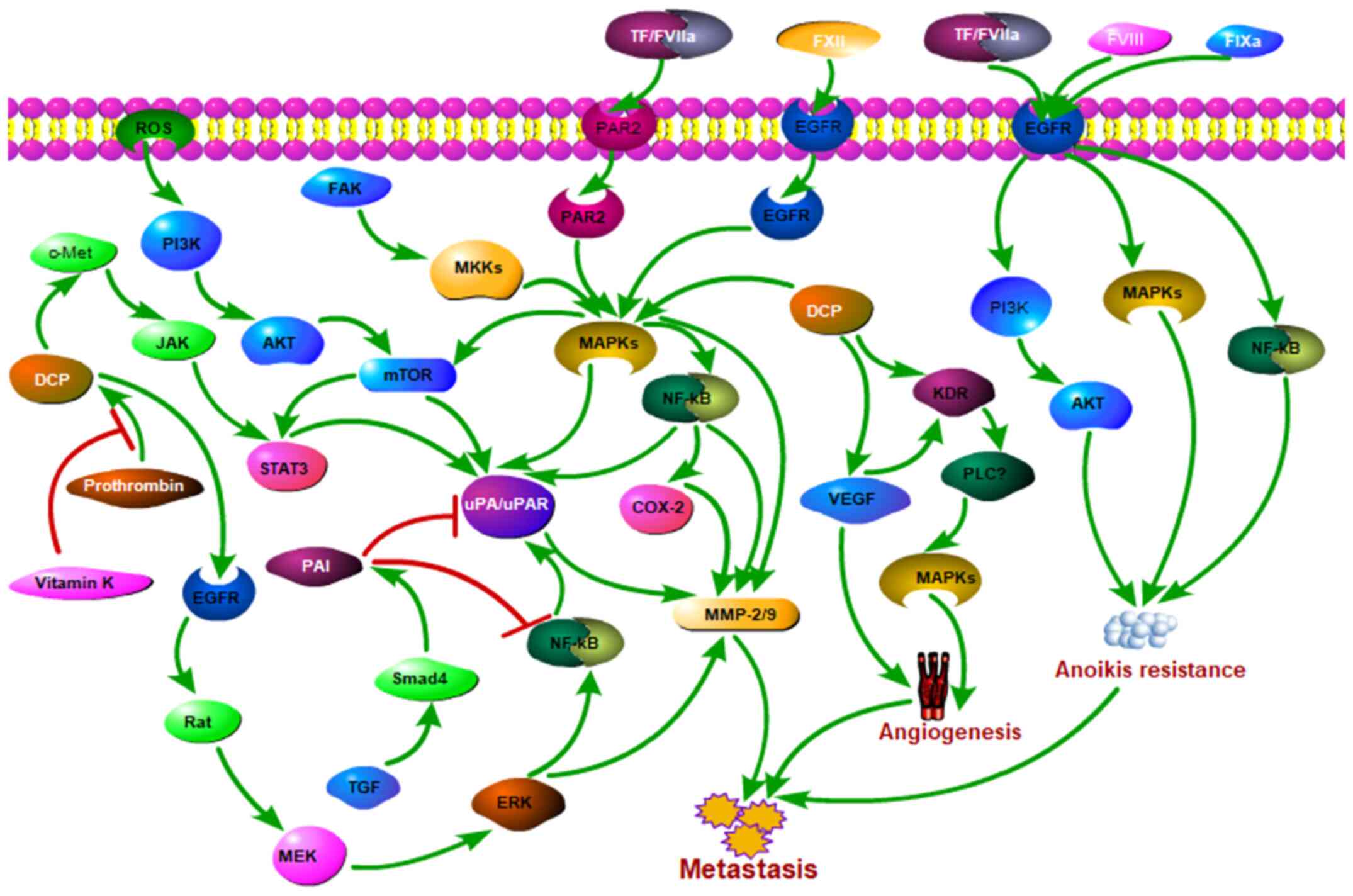
Kanoh Y: Coagulation and fibrinolytic
system. Nihon Rinsho. 74 (Suppl 4):S301–S305. 2016.(In
Japanese).
|
|
8
|
Tsai MC, Yen YH, Chang KC, Hung CH, Chen
CH, Lin MT and Hu TH: Elevated levels of serum urokinase
plasminogen activator predicts poor prognosis in hepatocellular
carcinoma after resection. BMC Cancer. 19:11692019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wei L, Lun Y, Zhou X, He S, Gao L, Liu Y,
He Z, Li B and Wang C: Novel urokinase-plasminogen activator
inhibitor SPINK13 inhibits growth and metastasis of hepatocellular
carcinoma in vivo. Pharmacol Res. 143:73–85. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zacharski LR: Anticoagulants in cancer
treatment: Malignancy as a solid phase coagulopathy. Cancer Lett.
186:1–9. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lip GY, Chin BS and Blann AD: Cancer and
the prothrombotic state. Lancet Oncol. 3:27–34. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zacharski LR, Wojtukiewicz MZ, Costantini
V, Ornstein DL and Memoli VA: Pathways of coagulation/fibrinolysis
activation in malignancy. Semin Thromb Hemost. 18:104–116. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Falanga A, Marchetti M and Vignoli A:
Coagulation and cancer: Biological and clinical aspects. J Thromb
Haemost. 11:223–233. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Thodiyil PA and Kakkar AK: Variation in
relative risk of venous thromboembolism in different cancers.
Thromb Haemost. 87:1076–1077. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Nadir Y: Decreasing tumor growth and
angiogenesis by inhibition of coagulation. Semin Thromb Hemost.
45:622–628. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sun H, Cao D, Liu Y, Wang H, Ke X and Ci
T: Low molecular weight heparin-based reduction-sensitive
nanoparticles for antitumor and anti-metastasis of orthotopic
breast cancer. Biomater Sci. 6:2172–2188. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Furie B and Furie BC: The molecular basis
of blood coagulation. Cell. 53:505–518. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhou Q, Huang T, Wang YF, Zhou XB, Liang
LJ and Peng BG: Role of tissue factor in hepatocellular carcinoma
genesis, invasion and metastasis. Chin Med J (Engl). 124:3746–3751.
2011.PubMed/NCBI
|
|
19
|
Huang SZ, Wei MN, Huang JR, Zhang ZJ,
Zhang WJ, Jiang QW, Yang Y, Wang HY, Jin HL, Wang K, et al:
Targeting TF-AKT/ERK-EGFR pathway suppresses the growth of
hepatocellular carcinoma. Front Oncol. 9:1502019. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dupuy E, Hainaud P, Villemain A,
Bodevin-Phèdre E, Brouland JP, Briand P and Tobelem G: Tumoral
angiogenesis and tissue factor expression during hepatocellular
carcinoma progression in a transgenic mouse model. J Hepatol.
38:793–802. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Poon RT, Lau CP, Ho JW, Yu WC, Fan ST and
Wong J: Tissue factor expression correlates with tumor angiogenesis
and invasiveness in human hepatocellular carcinoma. Clin Cancer
Res. 9:5339–5345. 2003.PubMed/NCBI
|
|
22
|
Panasiuk A, Zak J, Panasiuk B and
Prokopowicz D: Increase in expression of monocytic tissue factor
(CD142) with monocytes and blood platelet activation in liver
cirrhosis. Blood Coagul Fibrinolysis. 18:739–744. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Tian M, Wan Y, Tang J, Li H, Yu G, Zhu J,
Ji S, Guo H, Zhang N, Li W, et al: Depletion of tissue factor
suppresses hepatic metastasis and tumor growth in colorectal cancer
via the downregulation of MMPs and the induction of autophagy and
apoptosis. Cancer Biol Ther. 12:896–907. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Li H, Tian ML, Yu G, Liu YC, Wang X, Zhang
J, Ji SQ, Zhu J, Wan YL and Tang JQ: Hyperthermia synergizes with
tissue factor knockdown to suppress the growth and hepatic
metastasis of colorectal cancer in orthotopic tumor model. J Surg
Oncol. 106:689–695. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zerbib P, Grimonprez A, Corseaux D,
Mouquet F, Nunes B, Petersen LC, Susen S, Ung A, Hebbar M, Pruvot
FR, et al: Inhibition of tissue factor-factor VIIa proteolytic
activity blunts hepatic metastasis in colorectal cancer. J Surg
Res. 153:239–245. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Neaud V, Hisaka T, Monvoisin A, Bedin C,
Balabaud C, Foster DC, Desmoulière A, Kisiel W and Rosenbaum J:
Paradoxical pro-invasive effect of the serine proteinase inhibitor
tissue factor pathway inhibitor-2 on human hepatocellular carcinoma
cells. J Biol Chem. 275:35565–35569. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Tsai MC, Chen KD, Wang CC, Huang KT, Wu
CH, Kuo IY, Chen LY, Hu TH, Goto S, Nakano T, et al: Factor VII
promotes hepatocellular carcinoma progression through ERK-TSC
signaling. Cell Death Discov. 1:150512015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chen KD, Wang CC, Tsai MC, Wu CH, Yang HJ,
Chen LY, Nakano T, Goto S, Huang KT, Hu TH, et al: Interconnections
between autophagy and the coagulation cascade in hepatocellular
carcinoma. Cell Death Dis. 5:e12442014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lin CC, Wu CH, Chen LY, Tsai MC, Elsarawy
AM and Huang KT: Coagulation factor VII gene polymorphisms are not
associated with the occurrence or the survival of hepatocellular
carcinoma: A report of 37 cases. Cancer Biol Med. 15:275–281. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Li Y, Wang X, Cheng S, Du J, Deng Z, Zhang
Y, Liu Q, Gao J, Cheng B and Ling C: Diosgenin induces G2/M cell
cycle arrest and apoptosis in human hepatocellular carcinoma cells.
Oncol Rep. 33:693–698. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zhuang M, Xin G, Wei Z, Li S, Xing Z, Ji
C, Du J, Niu H and Huang W: Dihydrodiosgenin inhibits endothelial
cell-derived factor VIII and platelet-mediated hepatocellular
carcinoma metastasis. Cancer Manag Res. 11:4871–4882. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Yoo BK, Chen D, Su ZZ, Gredler R, Yoo J,
Shah K, Fisher PB and Sarkar D: Molecular mechanism of
chemoresistance by astrocyte elevated gene-1. Cancer Res.
70:3249–3258. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Srivastava J, Siddiq A, Emdad L,
Santhekadur PK, Chen D, Gredler R, Shen XN, Robertson CL, Dumur CI,
Hylemon PB, et al: Astrocyte elevated gene-1 promotes
hepatocarcinogenesis: Novel insights from a mouse model.
Hepatology. 56:1782–1791. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Danø K, Andreasen PA, Grøndahl-Hansen J,
Kristensen P, Nielsen LS and Skriver L: Plasminogen activators,
tissue degradation, and cancer. Adv Cancer Res. 44:139–266. 1985.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Liotta LA, Tryggvason K, Garbisa S, Hart
I, Foltz CM and Shafie S: Metastatic potential correlates with
enzymatic degradation of basement membrane collagen. Nature.
284:67–68. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Sun BS, Dong QZ, Ye QH, Sun HJ, Jia HL,
Zhu XQ, Liu DY, Chen J, Xue Q, Zhou HJ, et al: Lentiviral-mediated
miRNA against osteopontin suppresses tumor growth and metastasis of
human hepatocellular carcinoma. Hepatology. 48:1834–1842. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Cao X, Zhang L, Shi Y, Sun Y, Dai S, Guo
C, Zhu F, Wang Q, Wang J, Wang X, et al: Human tumor necrosis
factor (TNF)-alpha-induced protein 8-like 2 suppresses
hepatocellular carcinoma metastasis through inhibiting Rac1. Mol
Cancer. 12:1492013. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Tsai JP, Hsiao PC, Yang SF, Hsieh SC, Bau
DT, Ling CL, Pai CL and Hsieh YH: Licochalcone a suppresses
migration and invasion of human hepatocellular carcinoma cells
through downregulation of MKK4/JNK via NF-κB mediated urokinase
plasminogen activator expression. PLoS One. 9:e865372014.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Weng CJ, Chou CP, Ho CT and Yen GC:
Molecular mechanism inhibiting human hepatocarcinoma cell invasion
by 6-shogaol and 6-gingerol. Mol Nutr Food Res. 56:1304–1314. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Lee KH, Choi EY, Hyun MS, Jang BI, Kim TN,
Lee HJ, Eun JY, Kim HG, Yoon SS, Lee DS, et al: Role of hepatocyte
growth factor/c-Met signaling in regulating urokinase plasminogen
activator on invasiveness in human hepatocellular carcinoma: A
potential therapeutic target. Clin Exp Metastasis. 25:89–96. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Sun H and Liu GT: Inhibitory effect of
anti-hepatitis drug bicyclol on invasion of human hepatocellular
carcinoma MHCC97-H cells with high metastasis potential and its
relative mechanisms. J Asian Nat Prod Res. 11:576–583. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Blasi F and Carmeliet P: uPAR: A versatile
signalling orchestrator. Nat Rev Mol Cell Biol. 3:932–943. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Sakakibara T, Hibi K, Koike M, Fujiwara M,
Kodera Y, Ito K and Nakao A: Plasminogen activator inhibitor-1 as a
potential marker for the malignancy of colorectal cancer. Br J
Cancer. 93:799–803. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Zhou L, Jin Y, Cui QC, Jin KM, Zhou WX and
Xing BC: Low expression of PAI-2 as a novel marker of portal vein
tumor thrombosis and poor prognosis in hepatocellular carcinoma.
World J Surg. 37:608–613. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Weng CJ, Tsai CM, Chen YC, Hsieh YH, Lin
CW, Liu YF, Su SC, Chen MK and Yang SF: Evaluation of the
association of urokinase plasminogen activator system gene
polymorphisms with susceptibility and pathological development of
hepatocellular carcinoma. Ann Surg Oncol. 17:3394–3401. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Chen H, Peng H, Liu W, Sun Y, Su N, Tang
W, Zhang X, Wang J, Cui L, Hu P, et al: Silencing of plasminogen
activator inhibitor-1 suppresses colorectal cancer progression and
liver metastasis. Surgery. 158:1704–1713. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Divella R, Daniele A, Abbate I, Savino E,
Casamassima P, Sciortino G, Simone G, Gadaleta-Caldarola G, Fazio
V, Gadaleta CD, et al: Circulating levels of PAI-1 and SERPINE1
4G/4G polymorphism are predictive of poor prognosis in HCC patients
undergoing TACE. Transl Oncol. 8:273–278. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Wang X, Wang N, Li H, Liu M, Cao F, Yu X,
Zhang J, Tan Y, Xiang L and Feng Y: Up-Regulation of PAI-1 and
down-regulation of uPA are involved in suppression of invasiveness
and motility of hepatocellular carcinoma cells by a natural
compound berberine. Int J Mol Sci. 17:5772016. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Jin Y, Liang ZY, Zhou WX and Zhou L:
Plasminogen activator inhibitor 2 (PAI2) inhibits invasive
potential of hepatocellular carcinoma cells in vitro via uPA- and
RB/E2F1-related mechanisms. Hepatol Int. 13:180–189. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Pang RW, Joh JW, Johnson PJ, Monden M,
Pawlik TM and Poon RT: Biology of hepatocellular carcinoma. Ann
Surg Oncol. 15:962–971. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Kudo A, Shinoda M, Ariizumi S, Kumamoto T,
Katayama M, Otsubo T, Endo I, Kitagawa Y, Tanabe Y, Yamamoto M, et
al: Des-gamma-carboxy prothrombin affects the survival of HCC
patients with marginal liver function and curative treatment:
ACRoS1402. J Cancer Res Clin Oncol. 2020.(Epub ahead of print).
View Article : Google Scholar
|
|
52
|
Li Y and Chen J: Serum des-gamma-carboxy
prothrombin for diagnosis of adult primary cancer in liver. J Coll
Physicians Surg Pak. 29:972–976. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Cai Z, Chen G, Zeng Y, Dong X, Li Z, Huang
Y, Xin F, Qiu L, Xu H, Zhang W, et al: Comprehensive liquid
profiling of circulating tumor DNA and protein biomarkers in
long-term follow-up patients with hepatocellular carcinoma. Clin
Cancer Res. 25:5284–5294. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Tang W, Miki K, Kokudo N, Sugawara Y,
Imamura H, Minagawa M, Yuan LW, Ohnishi S and Makuuchi M:
Des-gamma-carboxy prothrombin in cancer and non-cancer liver tissue
of patients with hepatocellular carcinoma. Int J Oncol. 22:969–975.
2003.PubMed/NCBI
|
|
55
|
Suzuki M, Shiraha H, Fujikawa T, Takaoka
N, Ueda N, Nakanishi Y, Koike K, Takaki A and Shiratori Y:
Des-gamma-carboxy prothrombin is a potential autologous growth
factor for hepatocellular carcinoma. J Biol Chem. 280:6409–6415.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Gao FJ, Cui SX, Chen MH, Cheng YN, Sun LR,
Ward SG, Kokudo N, Tang W and Qu XJ: Des-gamma-carboxy prothrombin
increases the expression of angiogenic factors in human
hepatocellular carcinoma cells. Life Sci. 83:815–820. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Yue P, Gao ZH, Xue X, Cui SX, Zhao CR,
Yuan Y, Yin Z, Inagaki Y, Kokudo N, Tang W and Qu XJ:
Des-γ-carboxyl prothrombin induces matrix metalloproteinase
activity in hepatocellular carcinoma cells by involving the ERK1/2
MAPK signalling pathway. Eur J Cancer. 47:1115–1124. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Murata K and Sakamoto A: Impairment of
clathrin-mediated endocytosis via cytoskeletal change by epithelial
to fibroblastoid conversion in HepG2 cells: A possible mechanism of
des-gamma-carboxy prothrombin production in hepatocellular
carcinoma. Int J Oncol. 33:1149–1155. 2008.PubMed/NCBI
|
|
59
|
Murata K, Suzuki H, Okano H, Oyamada T,
Yasuda Y and Sakamoto A: Hypoxia-induced des-gamma-carboxy
prothrombin production in hepatocellular carcinoma. Int J Oncol.
36:161–170. 2010.PubMed/NCBI
|
|
60
|
Mizuta T, Ozaki I, Eguchi Y, Yasutake T,
Kawazoe S, Fujimoto K and Yamamoto K: The effect of menatetrenone,
a vitamin K2 analog, on disease recurrence and survival in patients
with hepatocellular carcinoma after curative treatment: A pilot
study. Cancer. 106:867–872. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Otsuka M, Kato N, Shao RX, Hoshida Y,
Ijichi H, Koike Y, Taniguchi H, Moriyama M, Shiratori Y, Kawabe T
and Omata M: Vitamin K2 inhibits the growth and invasiveness of
hepatocellular carcinoma cells via protein kinase A activation.
Hepatology. 40:243–251. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Shi CS, Shi GY, Hsiao HM, Kao YC, Kuo KL,
Ma CY, Kuo CH, Chang BI, Chang CF, Lin CH, et al: Lectin-like
domain of thrombomodulin binds to its specific ligand Lewis Y
antigen and neutralizes lipopolysaccharide-induced inflammatory
response. Blood. 112:3661–3670. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Suehiro T, Shimada M, Matsumata T,
Taketomi A, Yamamoto K and Sugimachi K: Thrombomodulin inhibits
intrahepatic spread in human hepatocellular carcinoma. Hepatology.
21:1285–1290. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Huang MT, Wei PL, Liu JJ, Liu DZ,
Huey-Chun H, An J, Wu CC, Wu CH, Ho YS, Yang YY and Chang YJ:
Knockdown of thrombomodulin enhances HCC cell migration through
increase of ZEB1 and decrease of E-cadherin gene expression. Ann
Surg Oncol. 17:3379–3385. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Hasegawa M, Nakoshi Y, Iino T, Sudo A,
Segawa T, Maeda M, Yoshida T and Uchida A: Thrombin-cleaved
osteopontin in synovial fluid of subjects with rheumatoid
arthritis. J Rheumatol. 36:240–245. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Xue YH, Zhang XF, Dong QZ, Sun J, Dai C,
Zhou HJ, Ren N, Jia HL, Ye QH and Qin LX: Thrombin is a therapeutic
target for metastatic osteopontin-positive hepatocellular
carcinoma. Hepatology. 52:2012–2022. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Liotta LA and Kohn E: Anoikis: Cancer and
the homeless cell. Nature. 430:973–974. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Kim YN, Koo KH, Sung JY, Yun UJ and Kim H:
Anoikis resistance: An essential prerequisite for tumor metastasis.
Int J Cell Biol. 2012:3068792012. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Frisch SM and Francis H: Disruption of
epithelial cell-matrix interactions induces apoptosis. J Cell Biol.
124:619–626. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Zhang X, Cheng SL, Bian K, Wang L, Zhang
X, Yan B, Jia LT, Zhao J, Gammoh N, Yang AG and Zhang R:
MicroRNA-26a promotes anoikis in human hepatocellular carcinoma
cells by targeting alpha5 integrin. Oncotarget. 6:2277–2289. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Jia Q, Xue T, Zhang Q, Cheng W, Zhang C,
Ma J, Bu Y, Yu S and Liu Q: CCN3 is a therapeutic target relating
enhanced stemness and coagulation in hepatocellular carcinoma. Sci
Rep. 7:138462017. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Ishikawa T, Kitano H, Mamiya A, Kokubun S
and Hidai C: The first EGF domain of coagulation factor IX
attenuates cell adhesion and induces apoptosis. Biosci Rep.
36:e003402016. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Versteeg HH, Spek CA, Richel DJ and
Peppelenbosch MP: Coagulation factors VIIa and Xa inhibit apoptosis
and anoikis. Oncogene. 23:410–417. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Das S and Johnson DB: Immune-related
adverse events and anti-tumor efficacy of immune checkpoint
inhibitors. J Immunother Cancer. 7:3062019. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
El-Khoueiry AB, Sangro B, Yau T, Crocenzi
TS, Kudo M, Hsu C, Kim TY, Choo SP, Trojan J, Welling TH Rd, et al:
Nivolumab in patients with advanced hepatocellular carcinoma
(CheckMate 040): An open-label, non-comparative, phase 1/2 dose
escalation and expansion trial. Lancet. 389:2492–2502. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Herbst RS, Soria JC, Kowanetz M, Fine GD,
Hamid O, Gordon MS, Sosman JA, McDermott DF, Powderly JD, Gettinger
SN, et al: Predictive correlates of response to the anti-PD-L1
antibody MPDL3280A in cancer patients. Nature. 515:563–567. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Zhang J, Bu X, Wang H, Zhu Y, Geng Y,
Nihira NT, Tan Y, Ci Y, Wu F, Dai X, et al: Cyclin D-CDK4 kinase
destabilizes PD-L1 via cullin 3-SPOP to control cancer immune
surveillance. Nature. 553:91–95. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Casey SC, Tong L, Li Y, Do R, Walz S,
Fitzgerald KN, Gouw AM, Baylot V, Gütgemann I, Eilers M and Felsher
DW: MYC regulates the antitumor immune response through CD47 and
PD-L1. Science. 352:227–231. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Li N, Wang J, Zhang N, Zhuang M, Zong Z,
Zou J, Li G, Wang X, Zhou H, Zhang L and Shi Y: Cross-talk between
TNF-α and IFN-γ signaling in induction of B7-H1 expression in
hepatocellular carcinoma cells. Cancer Immunol Immunother.
67:271–283. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Xiang J, Zhang N, Sun H, Su L, Zhang C, Xu
H, Feng J, Wang M, Chen J, Liu L, et al: Disruption of SIRT7
increases the efficacy of checkpoint inhibitor via MEF2D regulation
of programmed cell Death 1 Ligand 1 in hepatocellular carcinoma
cells. Gastroenterology. 158:664–678.e24. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Zhou J, Liu M, Sun H, Feng Y, Xu L, Chan
AWH, Tong JH, Wong J, Chong CCN, Lai PBS, et al: Hepatoma-intrinsic
CCRK inhibition diminishes myeloid-derived suppressor cell
immunosuppression and enhances immune-checkpoint blockade efficacy.
Gut. 67:931–944. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Nakagawa H, Umemura A, Taniguchi K,
Font-Burgada J, Dhar D, Ogata H, Zhong Z, Valasek MA, Seki E,
Hidalgo J, et al: ER stress cooperates with hypernutrition to
trigger TNF-dependent spontaneous HCC development. Cancer Cell.
26:331–343. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Febbraio MA, Reibe S, Shalapour S, Ooi GJ,
Watt MJ and Karin M: Preclinical models for studying NASH-Driven
HCC: How useful are they? Cell Metab. 29:18–26. 2019. View Article : Google Scholar : PubMed/NCBI
|