Introduction
Pregnancy-induced hypertension syndrome (PIH)
(1) is an idiopathic disease prone
to occur in late pregnancy. At present, incidence of PIH in China
is approximately 10%, and has become the most common serious
complication of pregnancy. PIH as one of the top 3 leading causes
of death in pregnant women seriously affecting maternal and infant
health and safety (1–4). Clinical manifestations of PIH include
edema, hypertension and urinary protein (5,6).
Intervention in the early phase can effectively prevent the
occurrence of severe symptoms. Microalbuminuria (mALb) is a
macromolecule protein that can be used as a marker for early
glomerular injury (7). C-reactive
protein (CRP) is a non-specific inflammatory-related protein
produced by the liver and regulated by plasma interleukin-6 (IL-6)
(8). Qiu et al (9) discovered that serum CRP was
significantly elevated in patients with PIH. Another study showed
that postpartum PIH patients had higher levels of high sensitivity
CRP (hs-CRP) than non-PIH patients (10). The goal of this study was to
investigate the predictive value of serum hs-CRP for PIH patients
and to explore its clinical diagnostic value.
Patients and methods
Patient information
PIH patients treated in The First People's Hospital
of Chengdu from June 2013 to December 2015 were selected into this
study. Among them, 60 patients had mild preeclampsia and the other
60 had severe preeclampsia. Sixty women with normal pregnancy
during the same time period were included as control group. The PIH
patients had varying degrees of edema, headache, high blood
pressure, blurred vision; and their symptoms were in accordance
with the PIH diagnostic criteria. Patients with tumors, blood
diseases, essential hypertension, contagious diseases and severe
liver and kidney diseases were excluded. Patients were divided into
three groups: mild preeclampsia group, severe preeclampsia group
and normal control group. Patients in the PIH group were aged from
22 to 43 years, and the average was 26.7±8.4 years, and they had
given 1–3 births, and the average age was 2.4±0.6. Their
gestational ages were 32–41 weeks, and the mean was 32.4±4.1 weeks.
Patients in the control group were aged from 20 to 47 years, and
the mean age was 25.7±8.1 years, and they had given 1–3 births, and
the average was 2.1±0.5. Their gestational ages were 32–41 weeks,
and the average was 33.6±3.7 weeks. There were no significant
differences in age, number of previous birth and gestational age
between the two groups (P>0.05). All pregnant women and their
families were informed and signed the informed consent. This study
was approved by the Ethics Committee of The First People's Hospital
of Chengdu (Chengdu, China).
Inclusion and exclusion criteria
Inclusion criteria: Patients had not recently
received irritant drug treatment, patients without family genetic
disease, patients without memory and hearing impairment, patients
who cooperated with follow-up and patients with compete clinical
record.
Exclusion criteria: Patients below 18 years,
patients with respiratory system disease, patients with blood
relationship with other patients, patients who recently received
blood transfusion therapy, patients with mental disease or physical
insufficiency.
Diagnostic methods
Diagnostic methods refer to the ‘Chinese
Hypertension Prevention Guidelines’ (11). Diagnostic criteria for PIH patients:
blood pressure ≥140/90 mmHg after 20 weeks of pregnancy, and
patients with urine protein ≥0.3 g/24 h or positive random urine
protein, clinical manifestations of abdominal discomfort, headaches
and other symptoms. Severe patients with blood pressure ≥160/110
mmHg, urinary protein ≥2.0 g/24 h or a strong positive random urine
protein, serum creatinine >1,061 µmol/l, platelets
<100×109/l, microangiopathic hemolysis (blood LDH
elevating), stent headaches or other neurological or visual
disturbances and persistent epigastric discomfort.
Methods
A total of 3 ml of intravenous blood was extracted
from the PIH patients in the morning and stored in test tubes with
anticoagulant. Fasting blood was obtained from the patients in the
control group during their regular checkups. Level of hs-CRP in
blood was measured by immunosorbent assay. Morning urine (3 ml) was
collected to measure levels of mALb by immunoturbidimetry. hs-CRP
and mALb kits were provided by Beijing Strong Biotechnology Co.,
Ltd. (Beijing, China). All tests were carried out by using Beckman
Kurt AU5800 automatic biochemical analyzer. Standards and controls
were provided by the manufacturers, and all operations were
performed in strict accordance with the manufacturer's
instructions.
Statistical analysis
SPSS 20.0 statistical software (IBM SPSS, Armonk,
NY, USA) was used for data analysis. Measurement data were
expressed as mean ± standard error and underwent normal
distribution test. Non-normal distribution data were converted to
normal distribution data before comparisons. ANOVA analysis was
used for the comparisons among multiple groups and the post hoc
test was Dunnetts test. ROC curve was used to analyze the
predictive value of hs-CRP for PIH. P<0.05 was considered to
indicate a statistically significant difference.
Results
Comparison of clinical data
Clinical data of three groups of patients were
compared. Results showed no significant differences in age,
gestational age, number of birth, fasting blood glucose,
electrolytes, and blood lipids among 3 groups (P>0.05) (Table I).
 | Table I.Comparisons of clinical data of the
three groups (mean ± standard error). |
Table I.
Comparisons of clinical data of the
three groups (mean ± standard error).
| Group | Mild preeclampsia
(n=60) | Severe preeclampsia
(n=60) | Control (n=60) | F-value | P-value |
|---|
| Age (years) |
27.1±7.4 |
26.8±7.9 |
25.7±8.1 | 0.535 | 0.587 |
| Gestational age
(weeks) |
32.7±4.5 |
32.1±4.7 |
33.6±3.7 | 1.831 | 0.163 |
| No. of births
(n) |
2.3±0.7 |
2.5±0.5 |
2.3±0.6 | 2.182 | 0.116 |
| Fasting blood glucose
(mmol/l) |
5.2±0.6 |
5.1±0.5 |
5.2±0.4 | 0.779 | 0.460 |
| Na+
(mmol/l) |
140.7±4.8 |
143.1±5.4 |
142.5±5.2 | 1.121 | 0.328 |
| K+
(mmol/l) |
4.2±0.5 |
4.3±0.7 |
4.2±0.6 | 0.546 | 0.581 |
| Total cholesterol
(mmol/l) |
4.8±0.8 |
4.7±0.6 |
4.7±0.9 | 0.332 | 0.718 |
| Triglycerides
(mmol/l) |
1.6±0.8 |
1.7±0.7 |
1.6±0.8 | 0.339 | 0.713 |
Comparison of the levels of hs-CRP and
mALb
Compared with the control group, the mild
preeclampsia group and the severe preeclampsia group showed
significantly higher hs-CRP and mALb levels (P<0.05). There were
significant differences in levels of hs-CRP and mALb between the
two preeclampsia groups (P<0.05) (Table II).
 | Table II.Comparison of hs-CRP and mALb in
peripheral blood among 3 groups (mean ± standard error). |
Table II.
Comparison of hs-CRP and mALb in
peripheral blood among 3 groups (mean ± standard error).
| Group | n | hs-CRP (mg/l) | mALb (mg/l) |
|---|
| Control | 60 | 2.1±1.2 | 6.4±4.1 |
| Mild
preeclampsia | 60 | 3.3±0.7a | 30.6±6.3a |
| Severe
preeclampsis | 60 | 5.4±1.6a | 35.4±4.2a |
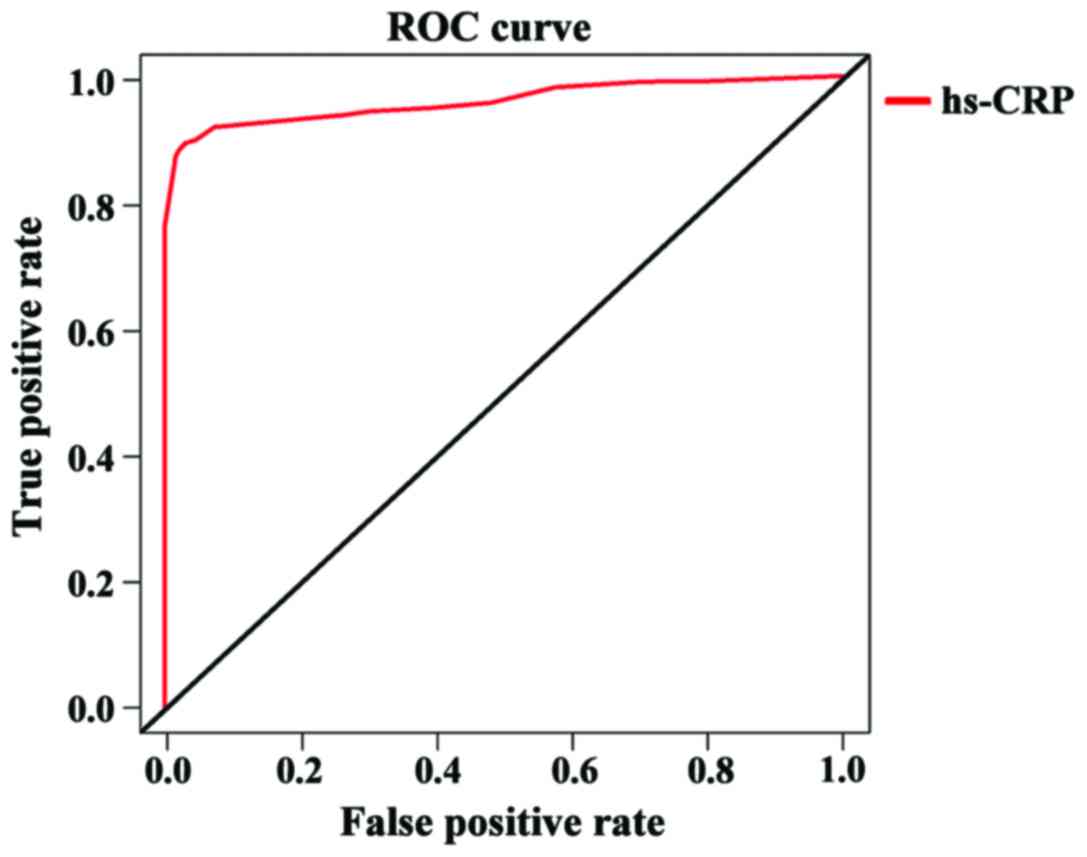
Analysis of diagnostic value of hs-CRP
for PIH by ROC curve analysis
Potential diagnostic value of hs-CRP for PIH was
analyzed by using ROC curve analysis. Results showed that hs-CRP
had high predictive value for PIH with an AUC of 0.943 and 95%
confidence interval (CI): 0.848–0.974. These data suggested that
hs-CRP can be used as a potential diagnostic marker for PIH
(Fig. 1).
Discussion
PIH is a unique disease in pregnant women that
mainly affects women after 20 weeks of gestation and/or two weeks
postpartum. Major symptoms include protein in urine and
hypertension, and PIH occurs in 5% of pregnant women (12). Studies have shown that (9) PIH not only cause serious complications
during perinatal period, but also increase the incidence of
cardiovascular and cerebrovascular diseases, seriously affecting
the health and safety of pregnant women.
Currently, it is thought that inflammatory response
may participate in the occurrence and development of PIH, and PIH
may be the first step of the onset of cardiovascular disease in
women (13). Clinically, PIH is
primarily diagnosed by quantification of 24 h urine protein and
monitoring blood pressure, but those two indicators are susceptible
to other factors (14). Increasing
number of studies have shown that CRP plays an important role in
the occurrence and development of PIH. CRP as an acute phase
reaction protein is synthesized in liver cells, and detection of
hs-CRP is more sensitive than CRP. hs-CRP is a sensitive marker
reflecting low-level inflammation, and it is specifically expressed
in cardiovascular disease (10).
hs-CRP is an indicator for atherosclerosis, and is also one of the
risk factors for hypertension. In a serum of healthy people, hs-CRP
content is low, while its level increases dramatically in
non-infectious inflammation (15).
PIH occurs through systemic arteriolar spasms. The underlying
mechanism is the injury and activation of endothelial cells, which
causes placental ischemia and hypoxia. With those pathological
changes, a series of cytotoxic factors will be released into the
maternal body and lead to increased intravascular permeability.
Finally, PIH patients will show prethrombotic symptoms and
excessive coagulation substances will be released, which in turn
lead to elevated blood hs-CRP level (16,17).
In this study, we investigated the expression of
hs-CRP and clinical data of 120 patients with PIH and 60 normal
pregnant women. The results showed that there were no significant
differences among the three groups in clinical data, indicating
that fasting blood glucose, electrolytes and lipids have no obvious
impact on PIH. However, significant differences in peripheral blood
hs-CRP and mALb were found between preeclampsia patients and normal
pregnant women, and their levels increased when the eclampsia
became more severe. These two indicators could be used as markers
for the diagnosis of PIH. A study showed that (18) PIH patients had significantly higher
mALb level than pregnant women without PIH, and elevated mALb
excretion proceeded other clinical manifestations. Another study by
Ertas et al (19) showed that
e treatment of PIH patients. Finally, ROC curve analysis showed
that hs-CRP had an AUC =0.943 and 95% CI: 0.848–0.974 in the
diagnosis of PIH, which suggested that hs-CRP can be used to
effectively predict PIH. Wang et al (20) suggested that hs-CRP can be used as a
standard for the diagnosis of PIH, which is consistent with our
conclusions.
ROC curve analysis used in this study increased the
reliability of our data. However, there are still some drawbacks.
The small sample size and regional differences might lead to bias
of our results. Moreover, this is only a clinical study and no
further study was performed. Therefore, more studies with larger
sample size are needed to confirm the conclusions in the
future.
In conclusion, peripheral blood hs-CRP increased
with the development of PIH, and it could be used as a potential
diagnostic marker for PIH. Monitoring hs-CRP closely can
effectively control the development of this disease and timely
intervene, which can effectively inhibit the progression of
disease. Sufficient attention should be paid to its clinical
value.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
HC drafted and finalized this manuscript. JZ and FQ
were devoted to collecting and interpreting the data. XC and XJ
revised it critically for important intellectual content. HC, JZ,
FQ, XC and XJ contributed to the conception and design of the
study. All authors read and approved the final study.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
The First People's Hospital of Chengdu (Chengdu, China). Signed
informed consents were obtained from the patients or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kappelle PJ, de Boer JF, Perton FG, Annema
W, de Vries R, Dullaart RP and Tietge UJ: Increased LCAT activity
and hyperglycaemia decrease the antioxidative functionality of HDL.
Eur J Clin Invest. 42:487–495. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kintiraki E, Papakatsika S, Kotronis G,
Goulis DG and Kotsis V: Pregnancy-induced hypertension. Hormones
(Athens). 14:211–223. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Andrews L and Patel N: Correlation of
serum lactate dehydrogenase and pregnancy induced hypertension with
its adverse outcomes. Int J Res Med Sci. 4:1347–1350. 2016.
View Article : Google Scholar
|
|
4
|
George JN and Amaresh A: Neonatal
mortality and morbidity in pregnancy induced hypertension: A
prospective observational study. J Evol Med Dent Sci. 3:5238–5246.
2014. View Article : Google Scholar
|
|
5
|
Sibai BM and Stella CL: Diagnosis and
management of atypical preeclampsia-eclampsia. Am J Obstet Gynecol.
200:481.e1–7. 2009. View Article : Google Scholar
|
|
6
|
Pouta A, Hartikainen AL, Sovio U, Gissler
M, Laitinen J, McCarthy MI, Ruokonen A, Elliott P and Järvelin MR:
Manifestations of metabolic syndrome after hypertensive pregnancy.
Hypertension. 43:825–831. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhu H, Liu M, Yu H, Liu X, Zhong Y, Shu J,
Fu X, Cai G, Chen X, Geng W, et al: Glycopatterns of urinary
protein as new potential diagnosis indicators for diabetic
nephropathy. J Diabetes Res. 2017:57280872017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Volanakis JE: Human C-reactive protein:
Expression, structure, and function. Mol Immunol. 38:189–197. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Qiu C, Sorensen TK, Luthy DA and Williams
MA: A prospective study of maternal serum C-reactive protein (CRP)
concentrations and risk of gestational diabetes mellitus. Paediatr
Perinat Epidemiol. 18:377–384. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Paternoster DM, Fantinato S, Stella A,
Nanhornguè KN, Milani M, Plebani M, Nicolini U and Girolami A:
C-reactive protein in hypertensive disorders in pregnancy. Clin
Appl Thromb Hemost. 12:330–337. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liu LS: Writing Group of 2010 Chinese
Guidelines for the Management of Hypertension: 2010 Chinese
guidelines for the management of hypertension. Zhonghua Xin Xue
Guan Bing Za Zhi. 39:579–615. 2011.(In Chinese). PubMed/NCBI
|
|
12
|
García RG, Celedón J, Sierra-Laguado J,
Alarcón MA, Luengas C, Silva F, Arenas-Mantilla M and
López-Jaramillo P: Raised C-reactive protein and impaired
flow-mediated vasodilation precede the development of preeclampsia.
Am J Hypertens. 20:98–103. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Freeman DJ, McManus F, Brown EA, Cherry L,
Norrie J, Ramsay JE, Clark P, Walker ID, Sattar N and Greer IA:
Short- and long-term changes in plasma inflammatory markers
associated with preeclampsia. Hypertension. 44:708–714. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Watanabe K, Naruse K, Tanaka K, Metoki H
and Suzuki Y: Outline of definition and classification of
‘pregnancy induced hypertension (PIH)’. Hypertens Res Pregnancy.
1:3–4. 2013. View Article : Google Scholar
|
|
15
|
El Desh F, El Naggar G, Eid M and Ibrahim
E: Measurement of serum sex hormone-binding globulin as an early
marker for gestational diabetes. Tanta Med J. 45:14–20. 2017.
View Article : Google Scholar
|
|
16
|
Yousuf O, Mohanty BD, Martin SS, Joshi PH,
Blaha MJ, Nasir K, Blumenthal RS and Budoff MJ: High-sensitivity
C-reactive protein and cardiovascular disease: A resolute belief or
an elusive link? J Am Coll Cardiol. 62:397–408. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gaikwad KB, Joshi NG and Selkar SP: Study
of nitrosative stress in ‘Pregnancy Induced Hypertension’. J Clin
Diagn Res. 11:BC06–BC08. 2017.PubMed/NCBI
|
|
18
|
Niraula A, Lamsal M, Majhi S, Khan SA and
Basnet P: Significance of serum uric acid in pregnancy induced
hypertension. J Natl Med Assoc. 109:198–202. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ertas IE, Kahyaoglu S, Yilmaz B, Ozel M,
Sut N, Guven MA and Danisman N: Association of maternal serum high
sensitive C-reactive protein level with body mass index and
severity of pre-eclampsia at third trimester. J Obstet Gynaecol
Res. 36:970–977. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wang L, Liu ZQ, Huo YQ, Yao LJ, Wei XG and
Wang YF: Change of hs-CRP, sVCAM-1, NT-proBNP levels in patients
with pregnancy-induced hypertension after therapy with magnesium
sulfate and nifedipine. Asian Pac J Trop Med. 6:897–901. 2013.
View Article : Google Scholar : PubMed/NCBI
|