Psoriasis is a common immune-mediated skin disease.
The prevalence of psoriasis in adults ranges between 0.91 and 8.5%
worldwide and the incidence of psoriasis is higher in adults than
in children (1). Psoriasis is
characterized by symptoms of plaque, pustular and other skin
lesions. Chronic plaque psoriasis accounts for 90% of all psoriasis
cases (2,3).
A number of biological therapies are used to treat
moderate to severe psoriasis, including etanercept, briakinumab,
ustekinumab, adalimumab and infliximab (4–8).
Etanercept, adalimumab and infliximab are monoclonal antibodies
against tumor necrosis factor (TNF), which function by neutralizing
the biological activity of TNF for treating the TNF-mediated
inflammation (5,9). By contrast, ustekinumab and briakinumab
are human monoclonal antibodies against interleukin (IL)-12/23p40
(8). These biological therapies are
used to treat psoriasis and improved clinical outcomes have been
observed. However, the efficacy of these therapies has been not
systematically reviewed.
In the present study, a network meta-analysis was
performed to review and compare the efficacy of these
aforementioned biological therapies of psoriasis. The Psoriasis
Area and Severity Index (PASI) response (10) was used as an indicator for assessing
the effect of treatment on the severity of psoriasis. PASI 50, PASI
75 and PASI 90 responses for the therapies were systematically
assessed. The pooled results provide further information on
selecting the most suitable treatments for moderate to severe
psoriasis.
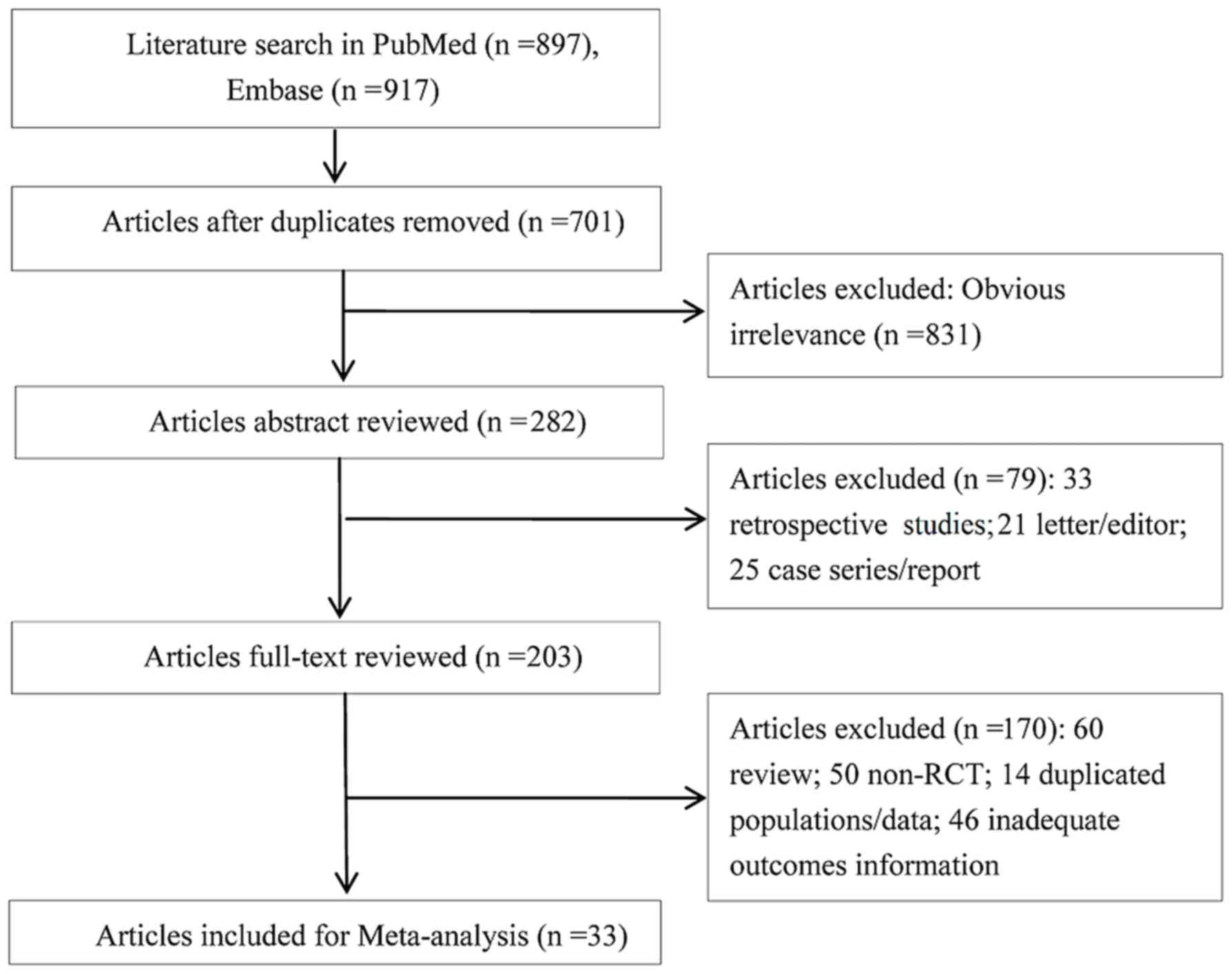
Studies with the following characteristics were
included in the current meta-analysis: i) Randomized controlled
trials (RCTs) reporting the treatment of moderate to severe
psoriasis with the aforementioned drugs. Moderate to severe
psoriasis is defined as body surface area >10 or psoriasis area
and severity index >10 and dermatology life quality index >10
(11); ii) studies including the
adults as participants; and iii) studies reporting the PASI
response rate (50, 75 and 90%). Any reviews, case reports and
letters were excluded from the meta-analysis. Any studies
investigating patients with mild psoriasis and those written in a
language other than English were also excluded.
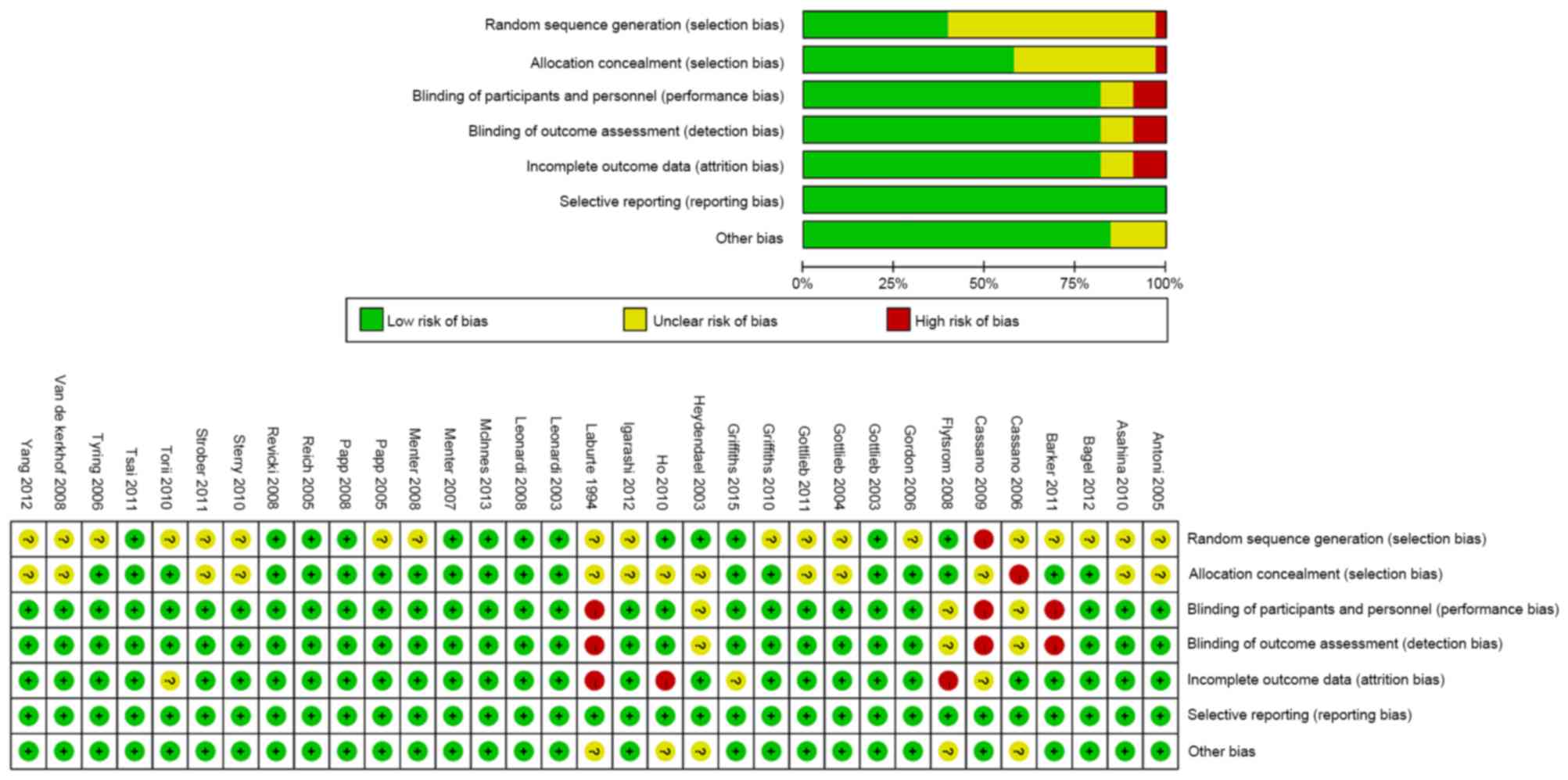
Two reviewers independently extracted the following
data: The name of the first author, publication year, sample size,
intervention, demographic characteristics of the included patients
and PASI response rate. The controversies were discussed with a
third reviewer to reach consensus. The methodological quality of
the included studies was evaluated by the Cochrane Collaboration
Risk of Bias Tool (12).
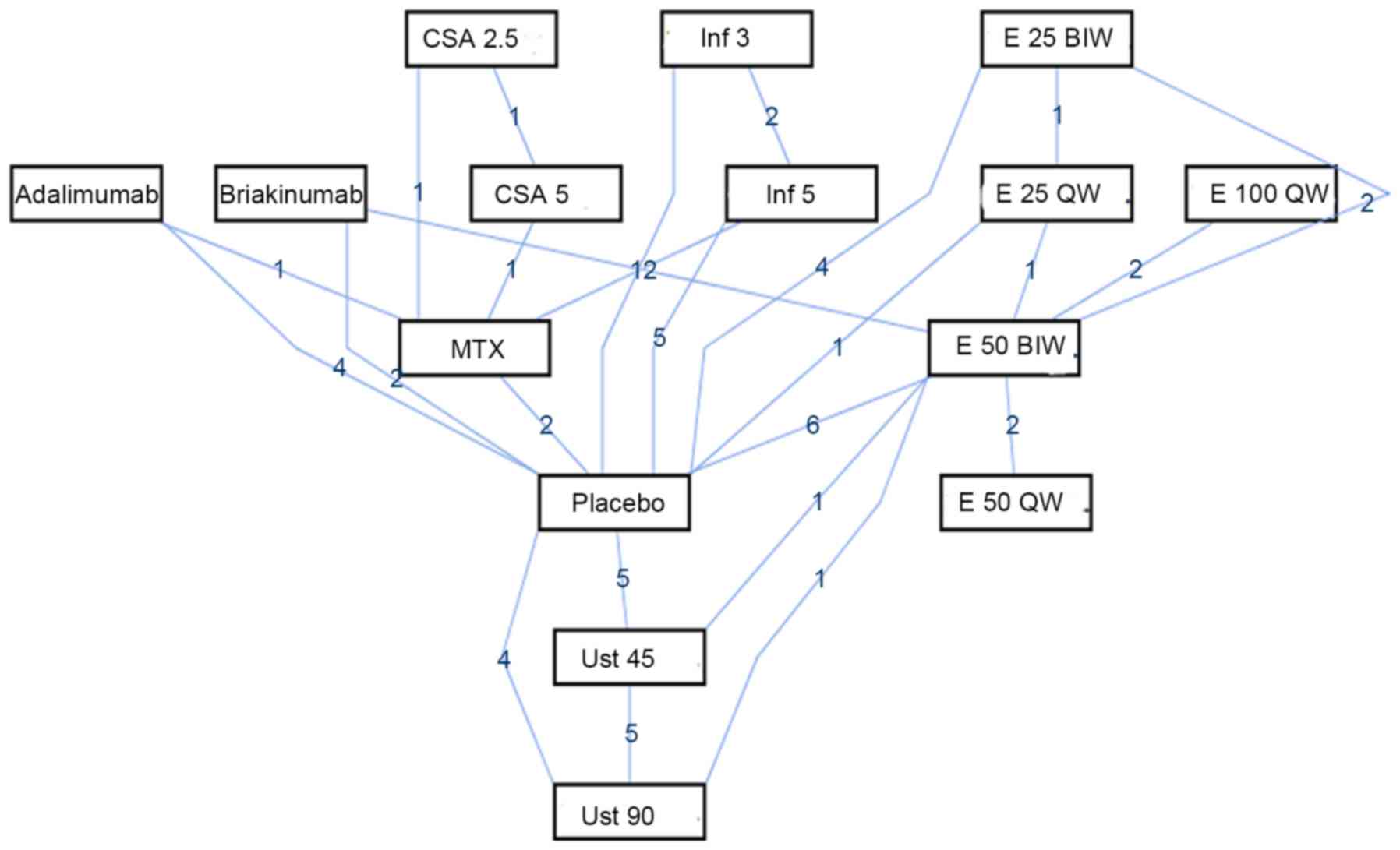
All analyses were performed using the ADDIS software
version 1.16.5 (Drug Information and Monitoring Systems, Groningen,
The Netherlands). Odds ratios (ORs) and their 95% confidence
intervals (CIs) were pooled. The network analysis performed was
based on the Bayesian framework. Data were evaluated by Markov
chain Monte Carlo methods and all analyses were performed using the
random effects model. The consistency of the RCTs was assessed by
Node-splitting analysis, and the consistency model was used if
P>0.05. Otherwise, the inconsistency model was used to pool the
odd ratios (13).
In the present study, a network meta-analysis was
performed to systematically review and compare the efficacy of
seven drugs used at different doses for treating moderate to severe
psoriasis. Based on the results of the network analysis, infliximab
(5 mg) may be an appropriate option to treat moderate to severe
psoriasis.
Psoriasis has been reported to be associated with a
high concentration of TNF-α (41)
and infliximab treatment can neutralize the biological activity of
TNF-α (42). However, the role of
the TNF-α in the pathogenesis of psoriasis remains unclear.
Previous studies have reported that TNF-α may serve an important
role in the upstream of the inflammatory responses of psoriasis
(43,44). An in vitro study determined
that infliximab was able to inhibit the activation of skin-homing T
cells and impair the antigen-presenting capacity of immature
dendritic cells in psoriasis patients (43). However, another TNF-α inhibitor,
etanercept, has been found to be effective in the treatment of
psoriasis by reducing the Th17 cell products, as well as the
production of IL-17, IL-22, IL-23 and inducible NO synthase from
dendritic cells (44). Thus, it has
been suggested that the infliximab may serve a different role with
other treatments on moderate to severe psoriasis.
Although the present meta-analysis indicated that
infliximab treatment had a high PASI score, a higher percentage of
adverse events were observed in infliximab-treated patients
compared with those in the placebo group (18), indicating that infliximab treatment
induces adverse effects. In addition, infliximab treatment
increases the incidence of infusion reactions (45). However, these outcomes were not
considered to be important due to the small sample size of each
study or the fact that the data were unavailable. Thus, the
therapeutic effect of the infliximab should be systematically
assessed in further studies. Besides, the dosage and treatment
duration of infliximab should be optimized according to the disease
severity of psoriasis.
In the present study, briakinumab and ustekinumab
(90 mg) treatments were superior to other treatments for PASI 90
response. Thus, anti-IL-12/23 monoclonal antibodies appear to be
more appropriate compared with anti-TNF-α treatment for treating
moderate to severe psoriasis. However, briakinumab and ustekinumab
showed no significantly improved therapeutic effect in PASI 75 and
PASI 50 responses when compared with the anti-TNF-α treatments. In
addition, the long-term safety profile, including severe infections
and cardiac disorders, should be evaluated in further studies with
large sample sizes and strict study design.
To the best of our knowledge, the present study is
the first network meta-analysis for evaluating the efficacy of
various treatments for moderate to severe psoriasis. The current
results may provide information for clinician and patients on the
selection of the suitable treatment for moderate to severe
psoriasis. However, there were also several limitations in the
present meta-analysis. Firstly, due to unavailable data in certain
included studies, confounding variables could not be adjusted and
subgroup analysis was not performed to reduce the effect of the
confounding variables. Secondly, due to unknown bias, the network
analyses of PASI 75 and PASI 50 responses were performed using an
inconsistency model. Finally, the results of the network
meta-analysis should be pooled only by a random effects model.
Thus, the pooled results may be conservative and certain borderline
significant effects may have been ignored (46).
In conclusion, the present meta-analysis results
suggested that infliximab (5 mg) may be a superior option compared
with other drugs for treating moderate to severe psoriasis due to
the relatively high PASI scores of patients. However, despite the
high PASI 90 responses, the efficacy of ustekinumab (90 mg) and
briakinumab were also high and therefore should be investigated in
further studies.
|
1
|
Parisi R, Symmons DP, Griffiths CE and
Ashcroft DM; Identification and Management of Psoriasis and
Associated ComorbidiTy (IMPACT) project team, . Global epidemiology
of psoriasis: A systematic review of incidence and prevalence. J
Invest Dermatol. 133:377–385. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Menter A, Gottlieb A, Feldman SR, Van
Voorhees AS, Leonardi CL, Gordon KB, Lebwohl M, Koo JY, Elmets CA,
Korman NJ, et al: Guidelines of care for the management of
psoriasis and psoriatic arthritis: Section 1. Overview of psoriasis
and guidelines of care for the treatment of psoriasis with
biologics. J Am Acad Dermatol. 58:826–850. 2008.
|
|
3
|
Griffiths CE and Barker JN: Pathogenesis
and clinical features of psoriasis. Lancet. 370:263–271. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Antoni CE, Kavanaugh A, Kirkham B, Tutuncu
Z, Burmester GR, Schneider U, Furst DE, Molitor J, Keystone E,
Gladman D, et al: Sustained benefits of infliximab therapy for
dermatologic and articular manifestations of psoriatic arthritis:
Results from the infliximab multinational psoriatic arthritis
controlled trial (IMPACT). Arthritis Rheum. 52:1227–1236. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Asahina A, Nakagawa H, Etoh T and Ohtsuki
M; Adalimumab M04-688 Study Group, . Adalimumab in Japanese
patients with moderate to severe chronic plaque psoriasis: Efficacy
and safety results from a Phase II/III randomized controlled study.
J Dermatol. 37:299–310. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Griffiths C, Sterry W, Brock F, Dilleen M,
Stefanidis D, Germain JM and Mallbris L: Pattern of response in
patients with moderate-to-severe psoriasis treated with etanercept.
Br J Dermatol. 172:230–238. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sterry W, Ortonne JP, Kirkham B, Brocq O,
Robertson D, Pedersen RD, Estojak J, Molta CT and Freundlich B:
Comparison of two etanercept regimens for treatment of psoriasis
and psoriatic arthritis: PRESTA randomised double blind multicentre
trial. BMJ. 340:c1472010. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Strober BE, Crowley JJ, Yamauchi PS, Olds
M and Williams DA: Efficacy and safety results from a phase III,
randomized controlled trial comparing the safety and efficacy of
briakinumab with etanercept and placebo in patients with moderate
to severe chronic plaque psoriasis. Br J Dermatol. 165:661–668.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bagel J, Lynde C, Tyring S, Kricorian G,
Shi Y and Klekotka P: Moderate to severe plaque psoriasis with
scalp involvement: A randomized, double-blind, placebo-controlled
study of etanercept. J Am Acad Dermatol. 67:86–92. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Schäfer I, Hacker J, Rustenbach SJ, Radtke
M, Franzke N and Augustin M: Concordance of the psoriasis area and
severity index (PASI) and patient-reported outcomes in psoriasis
treatment. Eur J Dermatol. 20:62–67. 2010.PubMed/NCBI
|
|
11
|
Mrowietz U, Kragballe K, Reich K, Spuls P,
Griffiths CE, Nast A, Franke J, Antoniou C, Arenberger P, Balieva
F, et al: Definition of treatment goals for moderate to severe
psoriasis: A European consensus. Arch Dermatol Res. 303:1–10. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Higgins JP, Altman DG, Gøtzsche PC, Jüni
P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, et
al: The Cochrane Collaboration's tool for assessing risk of bias in
randomised trials. BMJ. 343:d59282011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dias S, Welton NJ, Caldwell DM and Ades
AE: Checking consistency in mixed treatment comparison
meta-analysis. Stat Med. 29:932–944. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Barker J, Hoffmann M, Wozel G, Ortonne JP,
Zheng H, van Hoogstraten H and Reich K: Efficacy and safety of
infliximab vs. methotrexate in patients with moderate-to-severe
plaque psoriasis: Results of an open-label, active-controlled,
randomized trial (RESTORE1). Br J Dermatol. 165:1109–1117.
2011.
|
|
15
|
Cassano N, Miracapillo A, Coviello C,
Loconsole F, Bellino M and Vena GA: Treatment of psoriasis vulgaris
with the two-compound product calcipotriol/betamethasone
dipropionate followed by different formulations of calcipotriol.
Clin Drug Investig. 26:227–233. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Flytstrom I, Stenberg B, Svensson A and
Bergbrant IM: Methotrexate vs. ciclosporin in psoriasis:
effectiveness, quality of life and safety. A randomized controlled
trial. Br J Dermatol. 158:116–121. 2008.
|
|
17
|
Gordon KB, Langley RG, Leonardi C, Toth D,
Menter MA, Kang S, Heffernan M, Miller B, Hamlin R, Lim L, et al:
Clinical response to adalimumab treatment in patients with moderate
to severe psoriasis: Double-blind, randomized controlled trial and
open-label extension study. J Am Acad Dermatol. 55:598–606. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gottlieb AB, Evans R, Li S, Dooley LT,
Guzzo CA, Baker D, Bala M, Marano CW and Menter A: Infliximab
induction therapy for patients with severe plaque-type psoriasis: A
randomized, double-blind, placebo-controlled trial. J Am Acad
Dermatol. 51:534–542. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gottlieb AB, Leonardi C, Kerdel F, Mehlis
S, Olds M and Williams DA: Efficacy and safety of briakinumab vs.
etanercept and placebo in patients with moderate to severe chronic
plaque psoriasis. Br J Dermatol. 165:652–660. 2011.
|
|
20
|
Gottlieb AB, Matheson RT, Lowe N, Krueger
GG, Kang S, Goffe BS, Gaspari AA, Ling M, Weinstein GD, Nayak A, et
al: A randomized trial of etanercept as monotherapy for psoriasis.
Arch Dermatol. 139:1627–1632. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Griffiths CE: Comparing biological
therapies in psoriasis: Implications for clinical practice. J Eur
Acad Dermatol Venereol. 24 (Suppl 6):S10–S14. 2010. View Article : Google Scholar
|
|
22
|
Heydendael VM, Spuls PI, Opmeer BC, de
Borgie CA, Reitsma JB, Goldschmidt WF, Bossuyt PM, Bos JD and de
Rie MA: Methotrexate versus cyclosporine in moderate-to-severe
chronic plaque psoriasis. N Engl J Med. 349:658–665. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ho SG, Yeung CK and Chan HH: Methotrexate
versus traditional Chinese medicine in psoriasis: A randomized,
placebo-controlled trial to determine efficacy, safety and quality
of life. Clin Exp Dermatol. 35:717–722. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Igarashi A, Kato T, Kato M, Song M and
Nakagawa H; Japanese Ustekinumab Study Group, . Efficacy and safety
of ustekinumab in Japanese patients with moderate-to-severe
plaque-type psoriasis: Long-term results from a phase 2/3 clinical
trial. J Dermatol. 39:242–252. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Laburte C, Grossman R, Abi-Rached J,
Abeywickrama K and Dubertret L: Efficacy and safety of oral
cyclosporin A (CyA; Sandimmun) for long-term treatment of chronic
severe plaque psoriasis. Br J Dermatol. 130:366–375. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Leonardi CL, Kimball AB, Papp KA, Yeilding
N, Guzzo C, Wang Y, Li S, Dooley LT and Gordon KB; PHOENIX 1 study
investigators, . Efficacy and safety of ustekinumab, a human
interleukin-12/23 monoclonal antibody, in patients with psoriasis:
76-week results from a randomised, double-blind, placebo-controlled
trial (PHOENIX 1). Lancet. 371:1665–1674. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Leonardi CL, Powers JL, Matheson RT, Goffe
BS, Zitnik R, Wang A and Gottlieb AB; Etanercept Psoriasis Study
Group, . Etanercept as monotherapy in patients with psoriasis. N
Engl J Med. 349:2014–2022. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
McInnes IB, Kavanaugh A, Gottlieb AB, Puig
L, Rahman P, Ritchlin C, Brodmerkel C, Li S, Wang Y, Mendelsohn AM,
et al: Efficacy and safety of ustekinumab in patients with active
psoriatic arthritis: 1 year results of the phase 3, multicentre,
double-blind, placebo-controlled PSUMMIT 1 trial. Lancet.
382:780–789. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Menter A, Feldman SR, Weinstein GD, Papp
K, Evans R, Guzzo C, Li S, Dooley LT, Arnold C and Gottlieb AB: A
randomized comparison of continuous vs. intermittent infliximab
maintenance regimens over 1 year in the treatment of
moderate-to-severe plaque psoriasis. J Am Acad Dermatol. 56(31):
e1–e15. 2007.PubMed/NCBI
|
|
30
|
Menter A, Tyring SK, Gordon K, Kimball AB,
Leonardi CL, Langley RG, Strober BE, Kaul M, Gu Y, Okun M and Papp
K: Adalimumab therapy for moderate to severe psoriasis: A
randomized, controlled phase III trial. J Am Acad Dermatol.
58:106–115. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Papp KA, Langley RG, Lebwohl M, Krueger
GG, Szapary P, Yeilding N, Guzzo C, Hsu MC, Wang Y, Li S, et al:
Efficacy and safety of ustekinumab, a human interleukin-12/23
monoclonal antibody, in patients with psoriasis: 52-week results
from a randomised, double-blind, placebo-controlled trial (PHOENIX
2). Lancet. 371:1675–1684. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Papp KA, Tyring S, Lahfa M, Prinz J,
Griffiths CE, Nakanishi AM, Zitnik R, van de Kerkhof PC and Melvin
L; Etanercept Psoriasis Study Group, . A global phase III
randomized controlled trial of etanercept in psoriasis: Safety,
efficacy and effect of dose reduction. Br J Dermatol.
152:1304–1312. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Reich K, Nestle FO, Papp K, Ortonne JP,
Evans R, Guzzo C, Li S, Dooley LT and Griffiths CE: EXPRESS study
investigators: Infliximab induction and maintenance therapy for
moderate-to-severe psoriasis: A phase III, multicentre,
double-blind trial. Lancet. 366:1367–1374. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Revicki D, Willian MK, Saurat JH, Papp KA,
Ortonne JP, Sexton C and Camez A: Impact of adalimumab treatment on
health-related quality of life and other patient-reported outcomes:
Results from a 16-week randomized controlled trial in patients with
moderate to severe plaque psoriasis. Br J Dermatol. 158:549–557.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Torii H and Nakagawa H; Japanese
Infliximab Study investigators, . Infliximab monotherapy in
Japanese patients with moderate-to-severe plaque psoriasis and
psoriatic arthritis. A randomized, double-blind, placebo-controlled
multicenter trial. J Dermatol Sci. 59:40–49. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Tsai TF, Ho JC, Song M, Szapary P, Guzzo
C, Shen YK, Li S, Kim KJ, Kim TY, Choi JH, et al: Efficacy and
safety of ustekinumab for the treatment of moderate-to-severe
psoriasis: A phase III, randomized, placebo-controlled trial in
Taiwanese and Korean patients (PEARL). J Dermatol Sci. 63:154–163.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Tyring S, Gottlieb A, Papp K, Gordon K,
Leonardi C, Wang A, Lalla D, Woolley M, Jahreis A, Zitnik R, et al:
Etanercept and clinical outcomes, fatigue, and depression in
psoriasis: Double-blind placebo-controlled randomised phase III
trial. Lancet. 367:29–35. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
van de Kerkhof PC, Segaert S, Lahfa M,
Luger TA, Karolyi Z, Kaszuba A, Leigheb G, Camacho FM, Forsea D,
Zang C, et al: Once weekly administration of etanercept 50 mg is
efficacious and well tolerated in patients with moderate-to-severe
plaque psoriasis: A randomized controlled trial with open-label
extension. Br J Dermatol. 159:1177–1185. 2008.PubMed/NCBI
|
|
39
|
Yang HZ, Wang K, Jin HZ, Gao TW, Xiao SX,
Xu JH, Wang BX, Zhang FR, Li CY, Liu XM, et al: Infliximab
monotherapy for Chinese patients with moderate to severe plaque
psoriasis: A randomized, double-blind, placebo-controlled
multicenter trial. Chin Med J (Engl). 125:1845–1851.
2012.PubMed/NCBI
|
|
40
|
Cassano N, Loconsole F, Miracapillo A,
Travaglini M, Digiuseppe MD, Congedo M, Galluccio A, Buquicchio R,
Mastrandrea V, Filieri M, et al: Treatment of psoriasis with
different dosage regimens of etanercept: Preliminary results from
the Tαranta plastic study group. Int J Immunopathol Pharmacol.
23:797–802. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Mussi A, Bonifati C, Carducci M, D'Agosto
G, Pimpinelli F, D'Urso D, D'Auria L, Fazio M and Ameglio F: Serum
TNF-alpha levels correlate with disease severity and are reduced by
effective therapy in plaque-type psoriasis. J Biol Regul Homeost
Agents. 11:115–118. 1997.PubMed/NCBI
|
|
42
|
Cooper C, Shafran S, Greenbloom S, Enns R,
Farley J, Hilzenrat N, Williams K, Elkashab M, Abadir N and Neuman
M: Single-dose infliximab in hepatitis C genotype 1 treatment-naive
patients with high serum tumour necrosis factor-alpha does not
influence the efficacy of pegylated interferon alpha-2b/ribavirin
therapy. Can J Gastroenterol Hepatol. 28:35–40. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Bedini C, Nasorri F, Girolomoni G, Pità Od
and Cavani A: Antitumour necrosis factor-alpha chimeric antibody
(infliximab) inhibits activation of skin-homing CD4+ and CD8+ T
lymphocytes and impairs dendritic cell function. Br J Dermatol.
157:249–258. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Gottlieb AB, Chamian F, Masud S, Cardinale
I, Abello MV, Lowes MA, Chen F, Magliocco M and Krueger JG: TNF
inhibition rapidly down-regulates multiple proinflammatory pathways
in psoriasis plaques. J Immunol. 175:2721–2729. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Steenholdt C, Svenson M, Bendtzen K,
Thomsen OØ, Brynskov J and Ainsworth MA: Severe infusion reactions
to infliximab: aetiology, immunogenicity and risk factors in
patients with inflammatory bowel disease. Aliment Pharmacol Ther.
34:51–58. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Van Valkenhoef G, Tervonen T, Zwinkels T,
de Brock B and Hillege H: ADDIS: A decision support system for
evidence-based medicine. Decis Support Syst. 55:459–475. 2013.
View Article : Google Scholar
|